Abstract
Why have some countries done significantly better than others in fighting the Covid-19 pandemic? Had some countries been better prepared than others? This paper attempts to shed light on these questions by examining the role of climate risk and culture in explaining the cross-country variation in the Covid-19 mortality, while controlling for other potential drivers. In our analysis, we consider climate risk, readiness to climate change and individualism as main indicators reflecting the climate and culture status of individual countries. Using data from 110 countries, we find that the greater the climate risk; the lower the readiness to climate change and the more individualistic the society, the higher the pandemic mortality rate. We also present a series of sensitivity checks and show that our findings are robust to different specifications, alternative definitions of the mortality rate; and different estimation methods. One policy implication arising from our results is that countries that were better prepared for the climate emergency were also better placed to fight the pandemic. Overall, countries in which individuals look after each other and the environment, creating sustainable societies, are better able to cope with climate and public health emergencies.
Keywords: Covid-19, Mortality rate, Climate risk, Readiness, Individualism
1. Introduction
The Covid-19 crisis is unquestionably the greatest global public health emergency, at least since the influenza pandemic of 1918. As the virus has been transmitted across the globe with alarming pace and catastrophic consequences, exposing significant cross-country variation in the mortality rates, several key questions have emerged. Why have some countries done significantly better than others in fighting the Covid-19 pandemic? Were some countries more exposed than others to the virus? Had some countries been better prepared against such a health crisis than others?
In this paper, we attempt to shed some light on these questions, by exploring the links between the Covid-19 crisis, climate change and culture. Scientists have long established deep links between climate change and pandemics (Colwell, 1996, Epstein, 2002, Harvell et al., 2009, Semenza and Menne, 2009, Altizer et al., 2013, Ficetola and Rubolini, 2020). Specifically, climate change is known to drive wild-life closer to people, resulting in extensive interactions between wild animals, domestic animals and humans. This, in turn, paves the way for viruses that are harmless in wild animals to be transmitted to humans with deadly consequences (Kamradt-Scott, 2012, Vora, 2012). Indeed, around 75 percent of all major diseases affecting humans, including Aids, Sars, H5N1 avian flu and the H1N1 flu now originate in animals (USAID). It is also widely agreed that frequent extreme weather events have played a major role in the range and spread of diseases, increasingly turning them into epidemics and pandemics (Loevinsohn, 1994, McMichael, 2015, Tosepu et al., 2020).
Since the outbreak of the pandemic early in 2020, there has been much discussion on how learning from the coronavirus would help tackle the impending climate crisis (Jacobsen, 2020). It is argued that responding to the pandemic can teach policy-makers important lessons towards fighting other global threats, including climate change. Increasing national and international resilience against future epidemics and pandemics is highlighted as required preparation towards future climate change (Djalante, Shaw, & DeWit, 2020).
In this paper, we approach this issue in reverse order by exploring whether countries that are vulnerable to climate risk suffered more in the face of the Covid-19 pandemic. We hence have more specific questions to consider, namely (1) had countries been better prepared for climate change, would they have fared better in their fight against the Covid-19 pandemic? (2) Did cultural traits such as individualism that are closely linked to climate action, play any role in the human cost of the Covid-19? To establish whether a country’s standing with regard to climate change and its cultural traits impact its fight against the pandemic, we examine the link between climate risk, culture and the Covid-19 outcomes. Our choice of metric for the pandemic outcomes is the Covid-19 mortality rate – defined as the number of pandemic related deaths as a proportion of the total number of cases – widely referred to as the case-fatality ratio.
The relationship between climate conditions and mortality has long been recognized; through the impact of both extreme hot and cold weather increasing mortality (Curriero et al., 2002, Deschênes and Greenstone, 2011, Barreca, 2012); through warmer climates and spread of diseases (Altizer et al., 2013); and through changes in weather patterns, adaptation and mortality (Deschênes and Greenstone, 2011, Hajat et al., 2014). Given such significant role of climate change in health outcomes, and particularly in mortality, one would expect climate risk to play a significant role in influencing the Covid-19 fatality rate. Indeed, Ma et al. (2020) documents the effect of temperature and humidity on the Covid-19 mortality in Wuhan province, China, the pandemic has originated in. Similarly, Araujo and Naimi, 2020, Ficetola and Rubolini, 2020 establish how the spread of the coronavirus is likely to be impacted by climate.1 Yet, there is no formal analysis of climate risk as a potential factor underlying the cross-country variation in Covid-19 mortality rates. To the best of our knowledge, this is the first paper formally establishing the link between climate risk, culture and the Covid-19 mortality rate.2
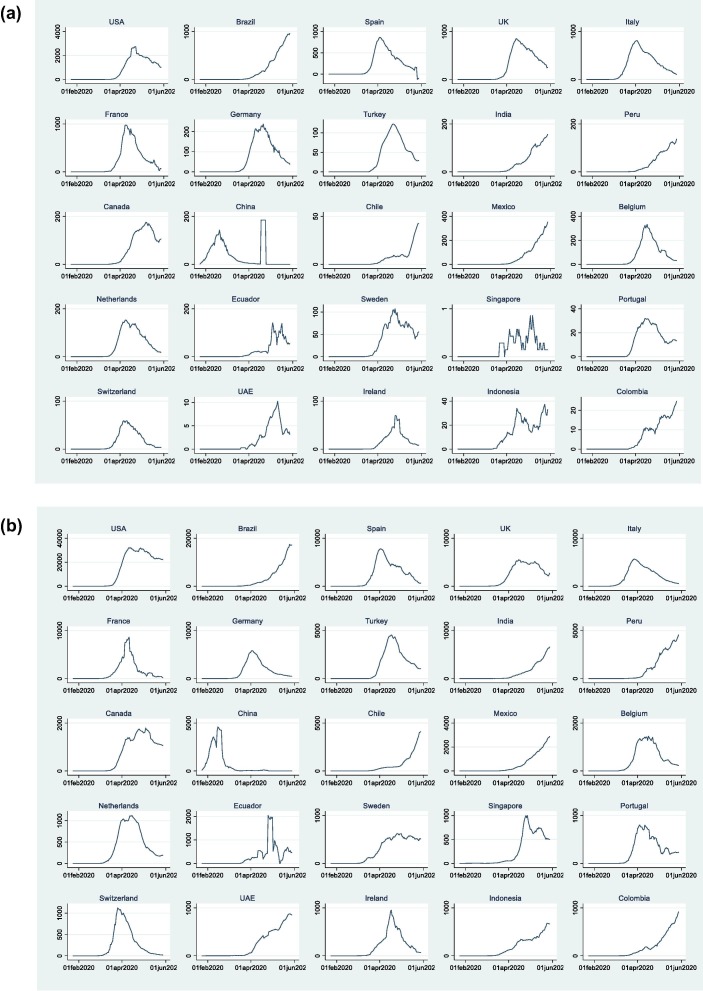
While it is true that a definitive cross-country comparison is difficult until after the full set of data are available – naturally after the pandemic is all but eradicated – there is now sufficient information enabling us to examine the link between climate risk, the preparedness of countries and the Covid-19 mortality rates. As is widely observed, the great majority of the worst-affected countries appear to have passed the peak of first wave of pandemic in terms of both the number of cases and the number of deaths, allowing comparability of the fatality rates (see, for example, Jinjarak, et al., 2020).3 This is clearly seen in Fig. 1 that displays the seven-day rolling averages of the number of deaths and the number of cases over January-May 2020, for 25 countries with highest number of deaths.4 Another difficulty in cross-country comparisons of mortality rates arises from potential biases in reporting fatalities and the number of infections. The former is caused by under-reporting and the latter arises from the wide variation in testing ability across countries. Using the case-fatality rate is likely to moderate this bias given both the numerator and the denominator are likely to be lower than their true unobserved values.
Fig. 1.
(a) 7-day rolling average of number of deaths, Jan-May 2020. (b) 7-day rolling average of number of cases, Jan-May 2020.
In addition, as is also noted in Atkeson (2020), the difficulty in estimating Covid-19 case-fatality rate at the earlier stages of the pandemic is significantly alleviated as large scale testing becames available, as has been the case at the time of recording of our data in late May 2020. Notwithstanding these arguments, we re-estimate our model using different dates and an alternative definition of mortality – the number of deaths per capita – as part of our robustness tests. We also provide an informal analysis of our key relationships using excess death data, which are available only for a limited number of countries.
We conduct our analysis by empirically linking the Covid-19 mortality rates and a set of country-specific factors, consisting of pre-Covid-19 characteristics and a set of social, economic and health responses to the outbreak of the virus. Among the pre-Covid-19 factors are climate indicators and cultural traits, as well as a set of controls combining other potential drivers of the pandemic related mortality.
Our findings yield some important insights. First, we establish that climate risk has been a major determinant of the Covid-19 mortality. That is, countries that face a greater climate risk are found to have suffered a higher mortality. This is a robust result that prevails whether we measure climate risk on past outcomes such as deaths and income losses from weather related events in the past, or on current exposure and capacity to respond to climate change. Second, we also find that greater preparedness to climate risk is consistently associated with a lower Covid-19 mortality rate. Third, we find that collectivist societies are associated with consistently lower fatalities in the face of the Covid-19. Finally, our results suggest that public health capacity in terms of both health expenditures and number of hospital beds; the share of the elderly population; and economic resilience are important factors in fighting a pandemic. We present a range of robustness checks and show that our findings on the relationship between climate risk, culture and the mortality rate is remarkably consistent across all specifications.
By formally establishing the link between climate-related risks and the Covid-19 mortality, this paper contributes to several strands in the literature. First, by quantifying additional costs of climate risks and inaction, we contribute to the debate on climate change. Second, by identifying climate and culture as additional sources of the cross-country variation in the pandemic-related mortality, we contribute to the fast-developing literature on the Covid-19 and efforts to develop our understanding of pandemics. Our findings clearly point to the crucial need for investment in both climate action and public health infrastructure as key lessons from the Covid-19 crisis, and hence towards better preparation for similar disasters in future.
The rest of this paper is organized as follows. Section 2 outlines our empirical methodology. Section 3 describes the data and the variables used in the analysis. Section 4 presents and discusses our empirical findings, including a set of robustness checks. Finally, Section 5 concludes.
2. Methodology
To examine the link between climate risk, culture and the Covid-19 mortality rate, we estimate the following specification:
| (1) |
where DR is death rate and i denotes country. In our benchmark case, DR corresponds to the cumulative number of deaths as a ratio of the cumulative number of cases, as recorded on the 26th of May 2020 (data on other dates are used as part of the robustness checks in Section 4). in Eq. (1) consists of two sets of variables: (1) climate and cultural factors; and (2) control variables that are likely to impact the Covid-19 mortality rate. Both sets of variables relate to the pre-Covid-19 period. In contrast, contains policy measures taken during the pandemic, including a wide range of containment measures, economic responses and health measures, taken in response to the onset of the virus, combined in an aggregate index, Stringency. In addition, denotes controls for time-invariant regional characteristics.
3. Data and variables
In this section, we briefly discuss data on variables that are our focus in this paper – climate risk, readiness and individualism – and other controls containing factors that are also likely to influence the pandemic-related mortality. We also provide the reasoning for including each variable in our analysis. Full definitions of the variables used in the analysis and the sources of data are given in Table A1 in the Appendix A.
Death rate – Our choice of mortality rate, DR, is the ratio of the number of confirmed Covid-19 deaths to the total number of confirmed cases – widely referred to as the case-fatality rate (DR1). It is a measure of how deadly the pandemic is in individual countries. As part of our robustness checks, we also use crude fatality rate (DR2), defined as the number of deaths per 100,000 of the population, as well as excess death, given by the number of deaths over and above the historical average over the same period. The analysis of excess death rate is provided only descriptively due to limited data availability.
3.1. Climate indicators
We utilize three separate climate-related indicators; Climate Risk; ND-Gain; and Readiness.
Climate Risk – This is a country-specific measure of climate risk defined as the scale of damage from extreme weather-related events in the past, such as storms, floods, heat waves. Climate Risk is a combined measure incorporating four indicators; number of deaths; number of deaths per 100,000; total losses of income; and total income losses per unit of GDP. The resulting index reflects the vulnerability of a country against similar events, and as such is branded as climate risk and is measured for the 1999–2018 period.
ND-Gain – This measure, provided by the Notre Dame Global Adaptation Initiative, is a composite index combining an extensive set of both vulnerabilities to and resilience against climate change and other global challenges, quantifying the net readiness to climate change. Its components reflect exposure to climate change and contain country-specific measures of dependence on sectors susceptible to climate emergencies; capacity of adaptation; economic ability to adapt in the face of climate change; institutional readiness for adaptation; and social readiness incorporating factors such as infrastructure, education and innovation adaptation actions. ND-Gain is calculated as net readiness and is normalized to lie between [0–100], with a higher score indicating a greater readiness and/or lower vulnerability to climate change.
Readiness – This measure, a component of ND-Gain index, combines economic, governance and social adaptability in the face of climate change, hence indicating how prepared individual countries are against the climate emergencies.
3.2. Culture variable
Individualism – A widely used measure of cultural traits is the degree of individualism, reflecting the prevailing cultural worldviews. Individualism is defined as the strength of ‘preference for a loosely-knit social framework in which individuals are expected to take care of only themselves and their immediate families’, with a higher score indicating a greater degree individualism (Hofstede, 2001).
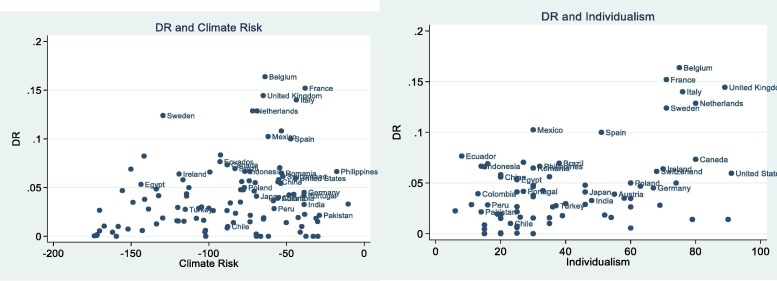
Before we formally establish the impact of climate change and culture variables on the pandemic mortality rate, we present bivariate relationships between mortality and Climate Risk; and mortality and Individualism, respectively in Fig. 2 . The clustering of countries with high climate risk corresponding to high pandemic-mortality rate is clearly visible from Fig. 2, while low climate risk countries are associated with low mortality rates. Similarly, Fig. 2 suggests that as individualism increases so does pandemic-mortality, with highly individualistic countries exhibiting highest mortality rates.
Fig. 2.
Covid-19 mortality, climate risk, and individualism.
3.3. Control variables
Clearly, mortality rates during a public health emergency such as the Covid-19 are likely to be closely linked with public health capacity. We incorporate two controls as measures of the public health infrastructure, namely the level of health expenditure expressed as a percentage of total public spending, Health Exp; and the number of hospital beds available per 100,000 people in the population, Hospital Beds. Both measures feature widely in the existing work on pandemics including the Covid-19 episode, with the number of hospital beds consistently emerging as a key driver of mortality (see, for example, Morens and Fauci, 2007, Favero, 2020, Sussman, 2020).
Two other control variables relate to population characteristics. The age distribution of population has already been established as an important risk factor in the fight against the Covid-19 (see, for example, Dowd and Andriano, 2020, Vincent and Taccone, 2020). We use Pop65, the ratio of those aged 65 and above as a proportion of total population, to capture the role of population age in mortality rates. Countries with higher population density are also known to be at greater risk in the face of an infectious disease as the transmission of the virus is much faster in densely populated areas (Rocklöv & Sjödin, 2020). To capture this effect, we use a density proxy, Density, defined as the number of people per square kilometre.
In addition, we control for economic conditions prevailing at the time the country in question is hit by the pandemic by using both the latest pre-Covid-19 GDP growth rates, GDP Growth, and GDP per capita figures, GDP per capita.
Finally, we also control for the regional effects that are common for countries in the same region, by incorporating regional dummy variables for seven distinct regions following the World Bank classification, as reported in Appendix A.
3.4. Post-Covid-19 policy measures
We control for the policy response to the pandemic as a potential determinant of the resulting fatalities, through the use of Stringency Index (see, for example, Acemoglu et al., 2020, Anderson et al., 2020, Lin and Meissner, 2020). This index taken from the Coronavirus government response tracker at the University of Oxford, reflecting the number and strictness of government policies in response to the pandemic. The attributes in the index include containment and closure policies; economic policies and healthcare responses such as testing regime; and emergency investment into healthcare.
Table 1 presents the descriptive statistics of the variables used in the analysis. There is significant variation in the average values of the variables. For example, the sample mean (median) value of the case fatality ratio, DR1, in the sample is about 3.90 (2.94), with the highest ratio observed in Belgium as 16.24. There are 6 countries in the sample where the mortality rate is recorded as zero. On the other hand, the mean (median) value of DR2, the number of deaths per 100,000 in population, is about 6.38 (0.8), with the highest deaths per capita is observed in Belgium as 81.45. Table 1 offers several other observations. The mean value of Pop65 is 10.28, with significant variation ranging from 1.09 (United Arab Emirates) to 27.58 (Japan). There are also significant differences in health measures across countries, with the lowest (highest) health expenditures ratio, Health Exp, being recorded in Iraq (Mozambique); while the mean value of Health Exp is 17.40. Furthermore, the average number of Hospital Beds is 31.20 where the lowest (highest) number of beds is observed in Mali (Japan).
Table 1.
Descriptive statistics.
| Variable | Obs. | Mean | Median | Std. dev. | Min. | Max. |
|---|---|---|---|---|---|---|
| DR1 | 110 | 3.897 | 2.944 | 3.579 | 0 | 16.239 |
| DR2 | 110 | 6.382 | 0.807 | 13.794 | 0 | 81.445 |
| GDP Growth | 110 | 3.080 | 2.775 | 2.249 | −4.200 | 9.350 |
| GDP per capita | 110 | 9.052 | 9.115 | 1.443 | 5.605 | 11.667 |
| Density | 110 | 4.430 | 4.574 | 1.421 | 0.713 | 8.981 |
| Pop65 | 110 | 10.277 | 8.305 | 6.723 | 1.090 | 27.580 |
| Health Exp | 110 | 17.399 | 13.904 | 11.780 | 1.783 | 69.523 |
| Hospital Beds | 110 | 31.209 | 26 | 24.082 | 1 | 134 |
| Stringency | 110 | 84.371 | 85.710 | 13.007 | 28.570 | 100 |
| Climate Risk | 110 | −87.903 | −79.165 | 41.395 | −173.670 | −10.330 |
| Readiness | 110 | 45.893 | 43.339 | 15.487 | 20.520 | 80.135 |
| ND-Gain | 110 | 52.334 | 50.892 | 11.356 | 30.952 | 76.052 |
| Individualism | 81 | 39.840 | 30 | 22.941 | 6 | 91 |
Notes: This table reports the descriptive statistics for the variables used in the analysis. Variable definitions are presented in Appendix A.
There are also significant differences across countries with respect to the values of the climate and culture indices. The values of Climate Risk (Readiness) range from −173.67 to −10.33 (20.52 to 80.14), with a mean value of −87.90 (45.89). The highest (lowest) value for Climate Risk is observed in Myanmar (Qatar) and highest (lowest) value for Readiness is observed in Singapore (Zimbabwe). Finally, the average value of Individualism is 39.84, with a range of values from 6 to 91. The most (least) individualistic country in our sample is United States (Guatemala).
4. Covid-19 mortality rate, climate risk and culture
4.1. The main results
Table 2 presents the first set of our empirical results from estimating Eq. (1). Column (1) reports our baseline specification that only includes the control variables, with estimated results mostly in line with predictions. Specifically, we find a negative and significant relation between the Covid-19 mortality rate (DR1) and GDP Growth, and GDP per capita, suggesting better outcomes for countries with greater economic resilience. In contrast, the percentage of population aged 65 and over (Pop65) is positively related to the Covid-19 death rate. This is not surprising given the widely observed higher likelihood of pandemic mortality among the elderly population5 . The estimated coefficient of Density is positive, but it is not statistically significant.
Table 2.
Covid-19 mortality and climate risk.
| (1) | (2) | (3) | |
|---|---|---|---|
| GDP Growth | −0.252* | −0.256* | −0.242* |
| (0.131) | (0.150) | (0.141) | |
| GDP per capita | −0.589** | −0.647** | −0.310 |
| (0.258) | (0.296) | (0.321) | |
| Density | 0.120 | 0.304 | 0.345* |
| (0.197) | (0.218) | (0.202) | |
| Pop65 | 0.434*** | 0.394*** | 0.312*** |
| (0.061) | (0.080) | (0.086) | |
| Health Exp | −0.016 | −0.054** | −0.074*** |
| (0.020) | (0.026) | (0.026) | |
| Hospital Beds | −0.044*** | −0.046*** | −0.038** |
| (0.014) | (0.017) | (0.017) | |
| Stringency | −0.003 | −0.013 | |
| (0.025) | (0.025) | ||
| Climate Risk | 0.022** | ||
| (0.009) | |||
| Region dummies | Yes | Yes | Yes |
| N | 110 | 110 | 110 |
| R2 | 0.328 | 0.366 | 0.403 |
Notes: This table reports the regression results to assess the impact of the control variables and climate risk on Covid-19 mortality rate (DR1). The specifications are estimated by OLS regression. Variable definitions are presented in Appendix A. Robust standard errors are in parentheses. ***, **, * denote the significance level at 1%, 5%, and 10%, respectively.
Regarding the role of the health-care capacity, the estimated coefficient of Hospital Beds is negative and statistically significant at the 1 percent level, in line with the prediction that the state of the pre-Covid-19 public health infrastructure has played a significant role in mortality rates (Favero, 2020, Sussman, 2020). This variable captures the extent to which countries were prepared to deal with the Covid-19 cases in providing the support to the infected to recover from the disease. In our second specification in Table 2, in addition to the pre-Covid-19 characteristics of countries, we incorporate Stringency, combining the extent and the strictness of government policies in response to the pandemic. We also include regional dummies to control for the common regional effects. The results suggest that Stringency is not significantly related to the Covid-19 mortality ratio. This may be due to the fact that Stringency is more likely to affect the number of infections rather than the number of deaths, resulting in an insignificant impact on the case-fatality rate.
In Column (3), we incorporate a measure of pre-Covid-19 country-specific Climate Risk, one of our key variables of interest. As can be seen, the estimated relation between the Covid-19 mortality rate and climate risk is positive and significant, indicating that countries that are susceptible to damage from climate change are likely to suffer a higher Covid-19 mortality. As specified above, Climate Risk measure is derived from the observed losses a country has suffered due to weather and climate conditions in the past, signalling its vulnerability to other global threats such as pandemics. Estimation results in Column (3) suggest that countries that suffered losses – both human and economic – from previous emergencies, have also suffered greater mortality in the face of the current coronavirus crisis.
In Table 3 , we further examine the relationship between climate risk and Covid-19 mortality by refining the way we measure climate risk. Our earlier measure, Climate Risk, is based on observed losses in the form of the number of actual deaths and economic losses arising from the past climate-related events in individual countries. We now consider an alternative measure of climate risk to capture a range of country-specific characteristics reflecting the ability and capacity of countries to deal with public health emergencies. Clearly, such ability and capacity would also be reflected in the success in reducing the Covid-19 related fatalities. Specifically, in our first specification in Table 3, we use ND-Gain as a proxy for climate risk. As explained earlier, this measure is derived from two opposing aspects of climate risk, encompassing both the vulnerability and readiness of countries in relation to climate change and the associated risks. A high value of ND-Gain represents the strength of readiness over vulnerability, and hence countries with the highest level of ND-Gain are the ones who have the highest level of readiness and/or the lowest level of vulnerability to climate change. As can be seen from the estimated coefficient in Column (1), a reduction in vulnerability and/or a strengthening of readiness against climate change is associated with a fall in the Covid-19 mortality rate.
Table 3.
Covid-19 mortality, climate risk, readiness, and individualism.
| (1) OLS |
(2) OLS |
(3) OLS |
(4) OLS |
(5) OLS |
|
|---|---|---|---|---|---|
| GDP Growth | −0.230* | −0.202 | −0.229 | −0.195 | −0.154 |
| (0.135) | (0.136) | (0.200) | (0.197) | (0.197) | |
| GDP per capita | 0.372 | 0.375 | −0.990** | −0.048 | 0.045 |
| (0.453) | (0.445) | (0.442) | (0.604) | (0.653) | |
| Density | 0.265 | 0.303 | 0.939*** | 0.761** | 0.818** |
| (0.200) | (0.193) | (0.319) | (0.336) | (0.320) | |
| Pop65 | 0.358*** | 0.359*** | 0.164 | 0.267** | 0.272** |
| (0.091) | (0.089) | (0.126) | (0.114) | (0.117) | |
| Health Exp | −0.056** | −0.052* | −0.116*** | −0.082** | −0.076** |
| (0.027) | (0.029) | (0.037) | (0.035) | (0.035) | |
| Hospital Beds | −0.038** | −0.039** | −0.027 | −0.027 | −0.028 |
| (0.017) | (0.017) | (0.022) | (0.023) | (0.024) | |
| Stringency | −0.012 | −0.013 | −0.012 | 0.006 | 0.007 |
| (0.025) | (0.024) | (0.037) | (0.039) | (0.037) | |
| Climate Risk | 0.019** | 0.019** | 0.017* | ||
| (0.009) | (0.009) | (0.010) | |||
| ND-Gain | −0.126* | −0.224** | |||
| (0.069) | (0.093) | ||||
| Readiness | −0.082** | −0.148** | |||
| (0.039) | (0.058) | ||||
| Individualism | 0.091*** | 0.107*** | 0.104*** | ||
| (0.026) | (0.027) | (0.027) | |||
| Region dummies | Yes | Yes | Yes | Yes | Yes |
| N | 110 | 110 | 81 | 81 | 81 |
| R2 | 0.417 | 0.419 | 0.505 | 0.521 | 0.527 |
Notes: This table reports the regression results to assess the impact of the control variables, climate risk, readiness of countries to climate change, and individualism on Covid-19 mortality rate (DR1). The specifications are estimated by OLS regression. Variable definitions are presented in Appendix A. Robust standard errors are in parentheses. ***, **, * denote the significance level at 1%, 5%, and 10%, respectively.
In Column (2) of Table 3, we replace ND-Gain with Readiness, a measure of economic, governance and social ability to adapt in the face of climate change. This enables us to evaluate, in isolation, how the extent of the pre-Covid-19 preparedness against climate change affects the mortality rate during the crisis. This specification also includes Climate Risk and hence the estimated coefficient of Readiness would reflect the impact of climate readiness on mortality, while controlling for the climate vulnerability of countries. In line with our predictions, the estimated relation is negative and significant. The extent to which countries were ready for the potential adverse effects of climate change prior to the Covid-19 period helps reduce the mortality rate during the pandemic, while the finding for Climate Risk remains unaffected.
4.2. Individualism, climate change and the Covid-19 mortality
An additional source of climate risk is related to societal attitudes to climate change, which in turn, is linked to cultural worldviews. It is widely agreed that a society’s worldview, defined as ‘its common values, shared beliefs and wisdom’ provides the basis for individual and societal behaviour, including those towards environmental action (Dunlap & Liere, 1984). A commonly used measure of cultural attitudes is the degree of individualism versus collectivism in a society. Emphasis on personal achievements and a strong sense of competition are among the key characteristics of individualist cultures. In contrast, in collectivist societies group or societal goals are above the individual needs and preferences. People in collectivist societies are ‘integrated into strong, cohesive in-groups, which through people’s lifetime continue to protect them in exchange for unquestioning loyalty’ (Hofstede, 1991). United States and Western Europe exemplify individualistic societies, while collectivist cultures are observed in Asia, Latin America and Middle East (see, for example, Triandis, 2018).
A large body of work has emerged on the relationship between cultural attitudes and climate policy, suggesting that individualistic societies are less likely to support environmental action due to: (1) lower perceived risks from climate change (Xue et al., 2016); (2) greater perceived intractability of environmental challenges (Xiang et al., 2019); and (3) greater scepticism about the environmental risks (Kahan et al., 2011).
We, therefore, incorporate in our analysis a country-specific individualism score, Individualism, reflecting the differences in cultural worldviews prevailing in individual countries (taken from Hofstede database). A higher value of the index represents a more individualistic, and hence less collectivist, society. Including Individualism as an additional regressor in our estimation of the Covid-19 mortality serves two purposes. First, following from the above arguments on the link between individualism and climate change action, Individualism can be viewed as a proxy for climate inaction. In this respect, it can be taken as an alternative to the Climate Risk measure used earlier. Second, although the observation that collectivist countries have done better at fighting the Covid-19 pandemic has featured widely in the debates since the onset of the crisis, there is no formal evidence, as yet, on this relationship. Relatedly, the degree of individualism may impact on the pandemic-mortality rate through linkages other than the climate risk channel. For example, the relative success of Asian countries such as South Korea, Japan and China in controlling the Covid-19 is partly linked to the ability of these countries to impose surveillance on their citizens (Ahn, 2020). It is argued that such information exposure requires a culture that tolerates a certain level of surveillance, absent in most western societies which instead chose to restrict movements (Won Sonn, 2020).
Further to the role of individualism through the climate action channel, individualism may also impact on mortality through the link between national culture and social cohesiveness. High social cohesiveness, including a high degree of trust among people, and a less individualistic orientation, are, in turn, viewed as an important driver of overall health in a society (Marmot, 2004). Similarly, collectivism is viewed as an effective mechanism addressing health inequalities (Coburn & Coburn, 2007). In the context of Covid-19, individualistic societies may be less likely to engage with social distancing, handwashing and wearing masks since they may be less concerned about the favourable impacts of such actions on others. Indeed, Bian et al., (2020) finds that more individualist US counties complied less with social distancing over the period, January-April 2020. We, therefore, predict that in more individualistic societies the death rate is likely to be higher.
To formally test the impact of individualism on the Covid-19 mortality, we include Individualism as an additional country-specific regressor in Column (3) of Table 3. Individualism is estimated with a positive coefficient, significant at the 1 percent level. This finding points to an adverse impact of individualism on the Covid-19 outcomes, suggesting that mortality rates are higher in countries with greater (lower) levels of individualism (collectivism). Similar to our earlier specifications, Column (4) incorporates ND-GAIN in the empirical model together with Individualism. The estimated positive and highly significant relation between the Covid-19 mortality rate, DR1, and individualism prevails in Column (5) which combine both Individualism and Readiness. Overall, the results presented in Table 2, Table 3 clearly show that the climate indicators and cultural traits exert a significant influence on the Covid-19 mortality rate.
We now turn to the economic significance of the variables of interest that emerge as statistically significant drivers of the Covid-19 mortality rate. Given that the variables are measured in different units, we utilize results from estimating our specification with standardised values of the variables (not reported) to discuss the relative importance of the determinants of the mortality rate. The results suggest that the percentage of population over 65 (Pop65) is economically the most significant variable. Increasing it by one standard deviation increases the mortality rate by 0.674 standard deviations – holding the other variables constant. This corresponds to about 2.41 (0.674 × 3.579) deaths in 100 cases. The second most relevant variable in our analysis is Readiness. With an increase of one standard deviation in Readiness, mortality rate decreases by 0.35 deviations, or about 1.27 (−0.354 × 3.579) less deaths in 100 cases. Furthermore, one standard deviation increase in the number of hospital beds (Hospital Beds) decreases the mortality rate by 0.26 standard deviations. If Climate Risk, one of our main variables of interest, increases by one standard deviation, mortality rate is expected to increase by 0.22 standard deviations, which is about 0.79 (0.222 × 3.579) deaths in 100 cases. Finally, the effect of one standard deviation increase in total health expenditures reduces mortality rate by 0.16 standard deviations.
4.3. Robustness checks
4.3.1. Alternative measures of Covid-19 mortality and dates
In this section, we conduct several checks to test the robustness of our results. Starting with the measure of Covid-19 related deaths, we incorporate two additional measures in the analysis. First, we acknowledge that the number of reported cases, which is the denominator of our mortality rate, also depends on the ability of countries to carry out tests for the virus. We therefore use an alternative measure of Covid-19 related mortality rates, expressing the number of deaths in relation to population (per 100,000), rather than as a ratio of the number of observed cases. Second, given that countries are at different stages of the Covid-19 cycle, we carry out our empirical analysis using the cumulative death rates on two earlier dates: 30th of April and 13th of May.
The results corresponding to these different cases are reported in Table 4 . Panel A (Panel B) reports the results for 13th May (30th April). The Columns 1–3 in each panel display the estimation results based on the case mortality rate, DR1, whereas in Columns 4–6 we estimate the specifications incorporating the death per capita, DR2, in the model. Other control variables and regional dummies are included in all specifications. In Columns 1 and 4 (2 and 5), we include Climate Risk and Readiness (Individualism and Readiness) to test the impact of both climate risk and the preparedness of countries. Our estimation results are remarkably consistent across the alternative definitions of mortality; the death numbers recorded on different dates; and across different estimation methods.
Table 4.
Robustness checks.
|
Panel A. Mortality rates (13th of May), climate risk, readiness, and individualism. | ||||||
|---|---|---|---|---|---|---|
| (1) OLS (DR1) | (2) OLS (DR1) | (3) Tobit (DR1) | (4) OLS (DR2) | (5) OLS (DR2) | (6) Tobit (DR2) | |
| Climate Risk | 0.021** | 0.091*** | ||||
| (0.009) | (0.034) | |||||
| Readiness | −0.085** | −0.144** | −0.139** | −0.178 | −0.570* | −0.558** |
| (0.041) | (0.059) | (0.054) | (0.171) | (0.295) | (0.268) | |
| Individualism | 0.114*** | 0.117*** | 0.319*** | 0.330*** | ||
| (0.026) | (0.024) | (0.116) | (0.106) | |||
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| N | 110 | 81 | 81 | 109 | 80 | 80 |
| R2 | 0.397 | 0.525 | 0.447 | 0.524 | ||
| Panel B. Mortality rates (30th of April), climate risk, readiness, and individualism | ||||||
| Climate Risk | 0.021** | 0.082*** | ||||
| (0.009) | (0.029) | |||||
| Readiness | −0.079* | −0.121* | −0.117** | −0.164 | −0.516* | −0.507** |
| (0.044) | (0.061) | (0.056) | (0.150) | (0.261) | (0.237) | |
| Individualism | 0.119*** | 0.121*** | 0.277*** | 0.286*** | ||
| (0.026) | (0.024) | (0.099) | (0.091) | |||
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| N | 110 | 81 | 81 | 109 | 80 | 80 |
| R2 | 0.350 | 0.494 | 0.449 | 0.530 | ||
Notes: This table reports estimation results using alternative dates, mortality rate definitions and estimation methods. The results are reported only for the main variables of interest for brevity. Panel A (Panel B) gives the results for the Covid-19 mortality rate measured on 13th May (30th April). In Columns 1–3 (Columns 4–6) we define mortality by the ratio of the number of deaths to total cases (the number of deaths per 100,000 population). Variable definitions are presented in Appendix A. Robust standard errors are in parenthesis. ***, **, * denote the significance level at 1%, 5%, and 10%, respectively.
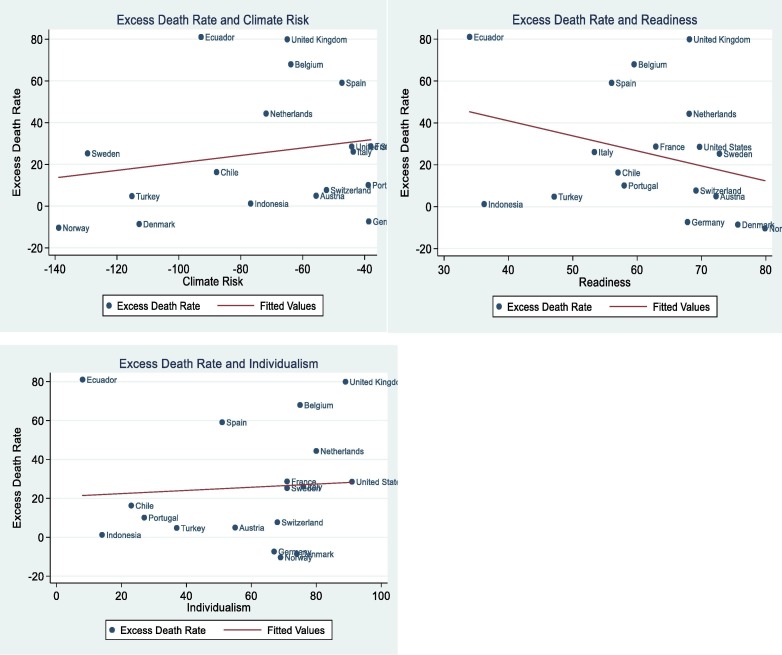
As is stated earlier, a good measure of cross-country mortality comparisons is excess death ratio, defined as the number of deaths in excess of historical averages for the corresponding period. Currently this is only available for a very small number of countries, insufficient for re-estimating our regression models. We collected data for 16 countries for which excess death numbers are available from a variety of sources (details are provided in Table A1 in the Appendix A). Bivariate relationships between the excess death ratio, defined as the number of excess deaths per 100,000, and our three measures of interest, namely climate risk, readiness and individualism are displayed in Fig. 3 . The relationships established earlier in our formal analysis between mortality, climate risk, readiness and individualism are also visible in these plots. Clearly, given the small size of the sample the displayed relationships are only suggestive rather than definitive at this stage.
Fig. 3.
Excess death rate, climate risk, readiness, and individualism.
Finally, we control for the possibility that countries may be at different stages of the pandemic by including a new regressor – the number of days since the first Covid-19 death was reported in each country. Including this variable does not change our findings regarding our main variables of interest while, not surprisingly, the relation between the number of days and the mortality is positive and significant at the 1 percent (the results are not reported for brevity).
4.3.2. Tobit regressions
As an additional robustness check, we have re-estimated our main specifications by utilizing a Tobit regression, as presented in Columns 3 and 6 in Table 4. The choice of Tobit regression is based on its ability to control for the observed number of zeros for the dependent variable. The presented coefficient estimates in Table 4 are marginal effects that are comparable to the coefficients of the OLS results presented in Columns 1–2 and 4–5. As is clear from Table 4, Tobit regressions produce very similar findings to the OLS results.
4.3.3. Further robustness checks
We have also carried out a number of other robustness checks by controlling for the potential impact of public debt levels; using alternative definitions of health expenditure (as a ratio of GDP and per capita health expenditure); and excluding the US and the UK from our sample. Our results under the alternative specifications are presented in Appendix B. As can be seen, our findings prevail under all three cases.
5. Conclusions
This paper investigates the role of climate risk, preparedness and culture in explaining the cross-country variation in the Covid-19 mortality rates. By using data from 110 countries, we estimate the relation between mortality rate and indicators of climate risk and culture, while controlling for a set of other determinants identified in the existing literature. To the best of our knowledge, this is the first paper formally exploring these interactions.
Our results show that the Covid-19 mortality rate is linked to the pre-Covid-19 levels of climate risk, individualism and the readiness of countries to climate change related adversities. The estimated relations are both statistically and economically significant. Specifically, the greater the climate risk and the lower the readiness to climate change, the higher the risk of mortality from the Covid-19. We also find that countries with more individualistic societies fare significantly worse than the collectivist ones in coping with the pandemic, displaying greater mortality rates. Put differently, countries in which individuals look after each other and the environment, key hallmarks of sustainable societies, are better able to cope with climate and public health emergencies.
In terms of our control variables, the findings reveal that the Covid-19 mortality rate is closely linked to public health capacity, measured by the share of health expenditure in GDP and the number of hospital beds; the share of those aged 65 and over in population; and economic resilience. We present a series of sensitivity checks and show that our findings are robust to different specifications, alternative definitions of the mortality rate as well as to different estimation methods.
Our findings suggest that (1) countries facing higher climate risk were also more exposed to Covid-19 and hence suffered greater pandemic-mortality; (2) countries that were better prepared for the climate emergency were also better placed to fight the coronavirus crisis; (3) collectivist societies did significantly better than individualistic ones in limiting the damage from the pandemic with consistently lower fatality rates. Taken together, our findings point to the crucial need for investment in both climate action and public health infrastructure.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Recent work has also documented the link between climate indicators such as weather and temperature changes and the spread of Covid-19 using country-level data for: Brazil (Prata et al., 2020); China (Shi et al., 2020); USA (Bashir et al., 2020); Spain (Briz-Redon & Serrano-Aroca, 2020) and Turkey (Sahin, 2020).
Clear parallels between the Covid-19 crisis and the climate emergency gave rise to a proliferation of studies drawing lessons from the former for the latter (Buscher et al., 2021; Botzen et al., 2020; Herrero & Thonton, 2020; Howarth et al., 2020; Klenert et al., 2020; and Manzanedo & Manning, 2020). It was argued that both types of crisis are less costly to prevent than cure and hence the early action is key (Klenert et al., 2020 and Manzanedo & Manning, 2020); climate emergency should be treated with the same urgency as the Covid-19 pandemic (Herrero & Thornton, 2020); and behavioural changes are essential for future climate action (Botzen et al., 2021; Howarth et al., 2020).
Excess mortality, the difference between number of deaths in excess of the historical average over the same period would be a better measure of mortality, yet this data is only available for a small number of countries, and for restricted periods at present (FT, 27 May 2020). We utilize the available data on excess death as part of our robustness analysis in Section 4.
It should be noted that several countries have witnessed a notable increase in the number of cases beyond our sample period, especially picking up from September 2020 - widely referred to as the second wave of the pandemic. While our analysis therefore focuses on the initial phase of the pandemic, most of the worst-hit countries in the first wave were also hit hard in the second wave, allowing us to generalize our findings.
There has been a clear age pattern in the Covid-19 deaths. For example, in England, those younger than 65 made up only the 12 percent of total Covid-19 deaths, in April 2020 (ONS, 2020, as documented at https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingCovid19englandandwales/deathsoccurringinapril2020.
Appendix A
Table A1.
Variable Definitions and Data Sources.
| Variables | Definition | Sources |
|---|---|---|
| DR1 (Mortality rate) | The ratio of the total number of deaths to total number of infections | John Hopkins CSSE GitHub Data Source |
|
DR2 (Mortality rate per 100,000 people) |
The ratio of total number of deaths to population Excess death is calculated as the difference between the observed that for the period and average deaths over the last 5 years for the same period. The ratio is defined as the number of excess deaths to the expected number of deaths for the corresponding period. |
John Hopkins CSSE GitHub Data Source The Economist The New York Times Human Mortality Database https://www.mortality.org/ |
| Excess death ratio | ||
| GDP Growth | Average GDP growth rate for 2018 and 2019 | IMF |
| GDP per capita | Gross Domestic Product per capita | World Bank |
| Density | Population density (people per square kilometre of land area) | World Bank |
| Pop65 | Population aged 65 and above as percentage of population | World Bank |
| Health Exp | Total health expenditure including government and external expenditure expressed as a ratio of total public spending | World Bank |
| Hospital Beds | Number of hospital beds expressed per 10,000 people | UNDP |
| Stringency | A composite index derived from information on 17 indicators of government responses; including containment and closure policies; economic policies; and health system policies | https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker |
| Climate Risk | Cumulative climate risk index based on the impact of extreme whether events both in terms of fatalities and economic losses from 1999 to 2018. | https://germanwatch.org/en/cri |
| ND-Gain | A measure of climate change adaptation based on the vulnerability and readiness of the country. Higher score indicates higher adaptation | Notre Dame Global Adaptation Initiative |
| Readiness | The country’s ability to leverage investments and convert them to adaptation actions considering three components: economic, social and governance readiness | Notre Dame Global Adaptation Initiative |
| Individualism | Individualism score of the countries which is defined as a preference of loosely-knit social framework | https://hi.hofstede-insights.com/national-culture |
| Regions |
|
World Bank |
Appendix B
Table B1.
Further Robustness Checks.
| Panel A. Estimation results when controlling for public debt | ||||||
|---|---|---|---|---|---|---|
| (1) OLS (DR1) | (2) OLS (DR1) | (3) Tobit (DR1) | (4) OLS (DR2) | (5) OLS (DR2) | (6) Tobit (DR2) | |
| Climate Risk | 0.024** | 0.098*** | ||||
| (0.010) | (0.036) | |||||
| Readiness | −0.084* | −0.141** | −0.138** | −0.114 | −0.502* | −0.497* |
| (0.044) | (0.061) | (0.055) | (0.154) | (0.278) | (0.251) | |
| Individualism | 0.114*** | 0.117*** | 0.326*** | 0.336*** | ||
| (0.027) | (0.024) | (0.119) | (0.108) | |||
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| N | 108 | 81 | 81 | 107 | 80 | 80 |
| R2 | 0.407 | 0.525 | 0.462 | 0.535 | ||
| Panel B. Estimation results when Health expenditure is defined in per capita terms | ||||||
| Climate Risk | 0.012 | 0.072** | ||||
| (0.009) | (0.031) | |||||
| Readiness | −0.154*** | −0.195*** | −0.192*** | −0.336* | −0.693*** | −0.690*** |
| (0.042) | (0.059) | (0.053) | (0.173) | (0.252) | (0.225) | |
| Individualism | 0.100*** | 0.102*** | 0.275** | 0.285*** | ||
| (0.028) | (0.025) | (0.113) | (0.101) | |||
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| N | 110 | 81 | 81 | 109 | 80 | 80 |
| R2 | 0.399 | 0.510 | 0.483 | 0.570 | ||
| Panel C. Estimation results when excluding the US and the UK | ||||||
| Climate Risk | 0.019** | 0.082** | ||||
| (0.009) | (0.033) | |||||
| Readiness | −0.097** | −0.155*** | −0.150*** | −0.219 | −0.605** | −0.592** |
| (0.040) | (0.058) | (0.053) | (0.161) | (0.287) | (0.259) | |
| Individualism | 0.106*** | 0.109*** | 0.281** | 0.294** | ||
| (0.027) | (0.025) | (0.123) | (0.112) | |||
| Controls | Yes | Yes | Yes | Yes | Yes | Yes |
| Region dummies | Yes | Yes | Yes | Yes | Yes | Yes |
| N | 110 | 81 | 81 | 109 | 80 | 80 |
| R2 | 0.380 | 0.497 | 0.407 | 0.477 | ||
Note: All other variables are as defined earlier.
References
- Acemoglu, D., V. Chernozhukov., Werning, I., & Whinston, M. D. (2020). A Multi-Risk SIR model with optimally targeted lockdown. NBER Working Paper No. 27102.
- Ahn, Michael. (2020). How South Korea flattened the coronavirus curve with technology. The Conversation, 21 April 2020.
- Altizer S., Ostfeld R.S., Johnson P.T., Kutz S., Harvell C.D. Climate change and infectious diseases: From evidence to a predictive framework. Science. 2013;341(6145):514–519. doi: 10.1126/science.1239401. [DOI] [PubMed] [Google Scholar]
- Anderson, R.M., Heesterbeek. H., Klinkenberg., D., & Hollingsworth, T. (2020). How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet, Mar21;395(10228):931-934. [DOI] [PMC free article] [PubMed]
- Araujo M.B., Naimi B. Spread of SARS-CoV-2 Coronavirus likely to be constrained by climate. MedRxiv. 2020 [Google Scholar]
- Atkeson, A. (2020). How deadly is Covid-19? Understanding the difficulties with estimation of its fatality rate. NBER Working Papers, No. 26965.
- Barreca A.I. Climate change, humidity, and mortality in the United States. Journal of Environmental Economics and Management. 2012;63(1):19–34. doi: 10.1016/j.jeem.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir, M. F., Ma, B., Komal, B., Bashir, M. A., Tan, D., & Bashir, M. (2020). Correlation between climate indicators and COVID-19 pandemic in New York, USA. Science of the Total Environment, 138835. [DOI] [PMC free article] [PubMed]
- Bian B., Li J., Xu T., Foutz N. Individualism During Crises: Big Data Analytics of Collective Actions amid COVID-19. COVID Economics. 2020;48:46–93. [Google Scholar]
- Botzen W., Duijndam S., van Beukering P. Lessons for climate policy from behavioral biases towards COVID-19 and climate change risks. World Development. 2020;137 doi: 10.1016/j.worlddev.2020.105214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redón, Á. & Serrano-Aroca, Á., 2020. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Science of the Total Environment, p.138811. [DOI] [PMC free article] [PubMed]
- Buscher B., Feola G., Fischer A., Fletcher R., Gerber J.F., Harcourt W., Walstra V. Planning for a World beyond COVID-19: Five Pillars for Post-Neoliberal Development. World Development. 2021;105357 doi: 10.1016/j.worlddev.2020.105357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coburn D., Coburn E.S. In: The Economics of Health Equity. McIntyre D., Mooney G., editors. Cambridge University Press; Cambridge: 2007. Health and Health Inequalities in a Neo-liberal Global World; p. 2007. [Google Scholar]
- Colwell R.R. Global climate and infectious disease: The cholera paradigm. Science. 1996;274(5295):2025–2031. doi: 10.1126/science.274.5295.2025. [DOI] [PubMed] [Google Scholar]
- Curriero F.C., Heiner K.S., Samet J.M., Zeger S.L., Strug L., Patz J.A. Temperature and mortality in 11 cities of the eastern United States. American Journal of Epidemiology. 2002;155(1):80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- Deschênes O., Greenstone M. Climate change, mortality, and adaptation: Evidence from annual fluctuations in weather in the US. American Economic Journal: Applied Economics. 2011;3(4):152–185. [Google Scholar]
- Djalante R., Shaw R., DeWit A. Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai Framework. Progress in Disaster Science. 2020;100080 doi: 10.1016/j.pdisas.2020.100080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd, J.B., L. Andriano., D., Brazel, V. Rotondi, P. Block., X. Ding., Y. Liu, & Mills, M.C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences of the USA, April 2020. https://doi.org/10.1073/pnas.2004911117 [DOI] [PMC free article] [PubMed]
- Dunlap R.E., Liere K.D. Commitment to the dominant social paradigm and concern for environmental quality. Social Science Quarterly. 1984;65(4):1013. [Google Scholar]
- Epstein P.R. Climate change and infectious disease: Stormy weather ahead? Epidemiology. 2002;13(4):373–375. doi: 10.1097/00001648-200207000-00001. [DOI] [PubMed] [Google Scholar]
- Favero C. Mortality in Lombardy. COVID Economics. 2020;4:47–62. [Google Scholar]
- Ficetola G.F., Rubolini D. Climate affects global patterns of COVID-19 early outbreak dynamics. MedRxiv. 2020 [Google Scholar]
- Hajat S., Vardoulakis S., Heaviside C., Eggen B. Climate change effects on human health: Projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. Journal of Epidemiol Community Health. 2014;68(7):641–648. doi: 10.1136/jech-2013-202449. [DOI] [PubMed] [Google Scholar]
- Harvell D., Altizer S., Cattadori I.M., Harrington L., Weil E. Climate change and wildlife diseases: When does the host matter the most? Ecology. 2009;90(4):912–920. doi: 10.1890/08-0616.1. [DOI] [PubMed] [Google Scholar]
- Herrero M., Thornton P. What can COVID-19 teach us about responding to climate change? The Lancet Planetary Health. 2020;4(5) doi: 10.1016/S2542-5196(20)30085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstede G. McGrawHill; London/New York: 1991. Cultures and Organizations: Software of the Mind. [Google Scholar]
- Hofstede G. Second edition. Sage Publishers; 2001. Culture's consequences: Comparing Values, Behaviors, Institutions, and Organizations Across Nations. [Google Scholar]
- Howarth C., Bryant P., Corner A., Fankhauser S., Gouldson A., Whitmarsh L., Willis R. Building a social mandate for climate action: Lessons from COVID-19. Environmental and Resource Economics. 2020;76(4):1107–1115. doi: 10.1007/s10640-020-00446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen K.H. Will COVID-19 generate global preparedness? The Lancet. 2020;395(10229):1013–1014. doi: 10.1016/S0140-6736(20)30559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinjarak Y, R Ahmed, S Nair-Desai, W Xin., & Aizenman, J. (2020). Accounting for global Covid-19 diffusion patterns: January-April 2020. NBER Working Papers, No. 27185. [DOI] [PMC free article] [PubMed]
- Kahan D.M., Jenkins-Smith H., Braman D. Cultural cognition of scientific consensus. Journal of Risk Research. 2011;14(2):147–174. [Google Scholar]
- Kamradt-Scott A. Changing perceptions: Of pandemic influenza and public health responses. American Journal of Public Health. 2012;102(1):90–98. doi: 10.2105/AJPH.2011.300330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klenert D., Funke F., Mattauch L., O'Callaghan B. Five Lessons from COVID-19 for Advancing Climate Change Mitigation. Environmental and Resource Economics. 2020;76:751–778. doi: 10.1007/s10640-020-00453-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, Z., & Meissner, C. M. (2020). Health vs. wealth? Public health policies and the economy during COVID-19. NBER Working Paper No. 27099.
- Loevinsohn M.E. Climatic warming and increased malaria incidence in Rwanda. Lancet. 1994;343:714–800. doi: 10.1016/s0140-6736(94)91586-5. [DOI] [PubMed] [Google Scholar]
- Ma, Y., Zhao, Y., Liu, J., He, X., Wang, B., Fu, S., Yan, J., Niu, J., Zhou, J. and Luo, B. (2020). Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Science of The Total Environment, 138226. [DOI] [PMC free article] [PubMed]
- Manzanedo R.D., Manning P. COVID-19: Lessons for the climate change emergency. Science of the Total Environment. 2020;742 doi: 10.1016/j.scitotenv.2020.140563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. Bloomsbury; London: 2004. Status Syndrome: How Your Social Standing Directly Affects Your Health and Life Expectancy; p. 2004. [Google Scholar]
- McMichael A.J. Extreme weather events and infectious disease outbreaks. Virulence. 2015;6(6):543–547. doi: 10.4161/21505594.2014.975022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morens D.M., Fauci T.S. The 1918 Influenza Pandemic: Insights for the 21st Century. The Journal of Infectious Diseases. 2007;195(7):1018–1028. doi: 10.1086/511989. [DOI] [PubMed] [Google Scholar]
- ONS (2020) Deaths involving Covid-19, England and Wales: Deaths occurring in April 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingCovid19englandandwales/deathsoccurringinapril2020
- Prata D.N., Rodrigues W., Bermejo P.H. Science of the Total Environment. 2020. Temperature significantly changes COVID-19 transmission in (sub) tropical cities of Brazil; p. 138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocklöv J.M., Sjödin H. High population densities catalyse the spread of COVID-19. Journal of Travel Medicine. 2020:1–2. doi: 10.1093/jtm/taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin M. Impact of weather on COVID-19 pandemic in Turkey. Science of The Total Environment. 2020;138810 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza J.C., Menne B. Climate change and infectious diseases in Europe. The Lancet Infectious Diseases. 2009;9(6):365–375. doi: 10.1016/S1473-3099(09)70104-5. [DOI] [PubMed] [Google Scholar]
- Shi P., Dong Y., Yan H., Zhao C., Li X., Liu W., Xi S. Science of the Total Environment. 2020. Impact of temperature on the dynamics of the COVID-19 outbreak in China; p. 138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman N. Time for bed(s): Hospital capacity and mortality from COVID-19. COVID Economics. 2020;11:116–129. [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Science of the Total Environment. 2020. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia; p. 138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triandis H.C. Routledge; 2018. Individualism and collectivism. [Google Scholar]
- Vincent, J. & F. S. Taccone (2020). Understanding pathways to death in patients with COVID-19, Comment, The Lancet Respiratory Medicine, 8 (5), P430-432, May 01, 2020. [DOI] [PMC free article] [PubMed]
- Vora N. The viral storm: The dawn of a new pandemic age. The Lancet Infectious Diseases. 2012;12(3):190. [Google Scholar]
- Won Sonn, J. (2020). Coronavirus: South Korea’s success in controlling disease is due to its acceptance of surveillance, The Conversation, 19 March, 2020.
- Xue W., Hine D.W., Marks A.D., Phillips W.J., Zhao S. Cultural worldviews and climate change: A view from China. Asian Journal of Social Psychology. 2016;19(2):134–144. [Google Scholar]
- Xiang P., Zhang H., Geng L., Zhou K., Wu Y. Individualist-Collectivist Differences in Climate Change Inaction: The Role of Perceived Intractability. Frontiers in Psychology. 2019;10 doi: 10.3389/fpsyg.2019.00187. [DOI] [PMC free article] [PubMed] [Google Scholar]