Abstract
Background
The only two preventive interventions available for COVID-19 have been social distancing and quarantine. These preventive measures challenge health care providers by causing cancelations of elective in-person outpatient clinic visits in many hospitals, particularly in otolaryngology clinics.
Objectives
To assess the applicability and feasibility of telemedicine in rhinology cases with a study of outcomes to guide rhinologists on indications of in-office visits. Assessment of patient satisfaction with telemedicine in the rhinology clinic was also investigated.
Methods
A retrospective review of electronic charts of all adult patients (>18 years) who were scheduled in the rhinology clinics of King Abdulaziz University Hospital, Riyadh, Saudi Arabia, and received a phone call as a part of telemedicine care from April through June 2020. Demographics (including age and gender), diagnosis, plan of treatment, and status of the visit (either new or follow-up) were collected. In addition, we used a special questionnaire to measure the satisfaction rate among patients who received telemedicine services.
Results
A total of 339 patients were included. The mean age was 41 years with 60.2% males. Only 5 cases (1.48%) were asked to attend to the clinic. The vast majority of cases were given a follow-up (n = 311, 91.7%). The most common diagnosis among the follow-up cases was chronic rhinosinusitis with nasal polyposis (n = 130, 38.3%). The satisfaction telephone survey had a total of 41 respondents out of 80 cases selected randomly. Most respondents (83.3%) were satisfied with telemedicine services.
Conclusion
We conclude that telemedicine proved its effectiveness in the efficient management and screening of rhinology cases during public health emergencies while providing sufficient protection for patients and medical practitioners. Telemedicine as a modality of care during the pandemic faced minor or no opposition given patients' understanding of the importance of social distancing.
Keywords: Rhinology, Telehealth, Telemedicine, COVID-19, Satisfaction, Pandemic, Otolaryngologists, Quarantine, Saudi Arabia, Retrospective
1. Introduction
On 31 December 2019, the World Health Organization (WHO) China Country Office was informed of pneumonia cases of unknown etiology detected in Wuhan City, Hubei Province, China [1]. This was the beginning of the story of COVID-19. Since that time the virus has spread worldwide at breathtaking speed, which led the WHO to declare COVID-19 a pandemic on 11 March 2020 [2]. To date there have been millions of confirmed cases and thousands of deaths with no effective treatment or vaccine for COVID-19. The only two preventive interventions available have been social distancing and quarantine. These preventive measures challenge health care providers by causing cancelations of elective in-person outpatient clinic visits in many hospitals, particularly in otolaryngology clinics, as otolaryngologists are at high risk for viral transmission due to the high viral load in the nasopharynx [3]. A result has been the rapid growth of telemedicine compared to the era before COVID-19, when its use was almost entirely limited to providing care for those in remote areas [4].
The WHO broadly describes telemedicine as: “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment, and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.” [5].
In Saudi Arabia, the first announced case of COVID-19 was in Qatif City on 2 March 2020 [6]. With an acceleration in the number of cases, the Ministry of Interior started implementing a lockdown policy throughout the kingdom on 5 April 2020 [7].
Following the new regulations, all otorhinolaryngology and head-and-neck surgery clinics started telemedicine service via phone calls. Therefore, in this study we aimed to assess the applicability and feasibility of telemedicine in rhinologic practice, studying the outcomes to guide rhinologists on indications of in-office visits during this pandemic or in any future pandemic. Furthermore, through a randomly distributed electronic survey, we assessed patients' satisfaction with telemedicine (by phone call) as a method of health care delivery.
2. Methods
2.1. Study design
This was a descriptive retrospective chart review to assess the efficacy of the telehealth service in the rhinology clinics at King Abdulaziz University Hospital from April to June 2020.
2.2. Study population/inclusion and exclusion criteria
All cases scheduled in the rhinology clinics and contacted by phone were included in the study. Patients were excluded if he or she had not received a phone call, pediatric cases (<18 years) and/or if the diagnosis/problem was not rhinologic in nature.
2.3. Data collection and study tools
Data was extracted from the hospital's electronic records. Chart review was done for all patients fulfilling the study criteria. An electronic data extraction sheet was designed to collect the following: demographic information (including age and gender), diagnosis, plan of treatment, and status of the visit as either new or follow-up. In addition, using a special questionnaire we measured the satisfaction rate among patients who had received telemedicine services. The items on this questionnaire were adapted from a validated questionnaire [8] designed to assess the level of patient satisfaction with diabetes remote consultations via videoconferencing in a virtual outreach clinic. The original questionnaire contains 16 questions in 4 domains: equipment/technical issues (3 questions), communication and rapport (3 questions), clinical assessment (4 questions), and program evaluation (5 questions), with a final question for open comments. We made some modifications to make the questions suitable for a teleclinic using phone calls to address general medical conditions rather than a videoconference to assess diabetic patients. Furthermore, we omitted the first question because it is specific to videoconferencing. Finally, we had the questionnaire translated to the Arabic language and then back into English to highlight any discrepancies or inaccuracies in the original translation. The survey was conducted by phone. Considering the study population of 339 patient, the estimated representative sample size to conduct satisfactory survey is 80 with confidence level of 80%. Sample size of the survey was calculated using Centers for Disease Control and Prevention (CDC) epi-info ™ tool. The study protocol was approved by the appropriate institutional review board (reference number 20/0782/IRB). Participation in the study was voluntary. Verbal informed consent was obtained from all participants in the survey.
3. Results
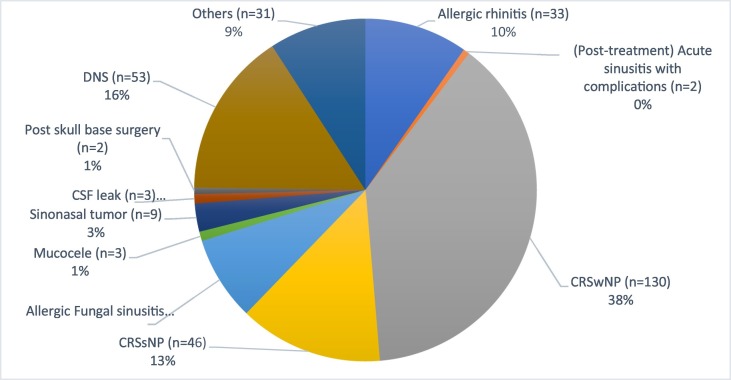
Of a total of 504 charts reviewed, 165 charts were discarded as the patient had not answered the phone call, pediatric cases and/or was not a rhinology case. The remaining 339 charts included 204 males (60.2%) and 135 females (39.8%). The age range was 18–70 years (mean: 41.333, SD: 14.417). Out of 339 cases, only 5 cases (1.48%) were asked to attend the clinic for further evaluation. One of these cases attended for nasal mass biopsy (suspected inverted papilloma recurrence). The other 4 were in their first post-operative visit (3 Functional Endoscopic Sinus Surgeries, 1 septoplasty). Although most cases were follow-up (n = 311, 91.7%), the new cases (n = 28, 8.3%) complained mainly (20 of 28, 71.4%) of nasal obstruction. The most common diagnosis among the follow-up cases was chronic rhinosinusitis with nasal polyposis (CRSwNP; n = 130, 38.3%), either post-operative or under medical treatment. The other diagnoses presented with variable percentages (Fig. 1 ).
Fig. 1.
Diagnosis of patients who were followed by telemedicine. CRSwNP: chronic rhinosinusitis with nasal polyp, CRSsNP: chronic rhinosinusitis without nasal polyp, DNS: deviated nasal septum, CSF: cerebrospinal fluid.
3.1. Patient satisfaction with telemedicine service
We had total of 41 respondents out of 80 cases that had been selected randomly. These 41 were called by phone and expressed their answers. The responses of patients to the satisfaction questionnaire are summarized in Table 1 . In general, responses were positive: 478 answers out of 574 (83.3%) for the 14 items in the questionnaire were agree or strongly agree. By contrast, an average of 7.75 out of 41 (18.9%) of the respondents showed concern (disagree or strongly disagree) about clinical assessment via telemedicine, as they believed that their conditions should be evaluated face to face in the clinic. The highest level of satisfaction was expressed about the quality of the voice call and technical equipment, on which all respondents (100%) gave agree or strongly agree answers. More than 27 of 41 (67%) respondents expressed their trust in telemedicine and would prefer to use it again in the future. Thirty-seven respondents (90.2%) agreed that telemedicine is cost and time efficient compared to conventional in-office visits. Of the 41 respondents, 35 (85.4%) patients thought it was easy to gain access to specialist care by telemedicine. Overall, the average total score among all respondents was 4.4 out of 5, which reflects the patients' acceptance of this new service.
Table 1.
The questionnaire for assessing patient satisfaction about telehealth services, with the survey results (figures represent the number of responses in each category).
| Domain | Question | Strongly disagree 1 |
Disagree 2 |
Undecided 3 |
Agree 4 |
Strongly agree 5 |
|---|---|---|---|---|---|---|
| Equipment and technical issues | 1. I was satisfied with the quality of the sound (audio) during the phone call. | 4 | 37 | |||
| 2. Experienced NO technical difficulties during the phone call (e.g. unexpected disconnections or loss of sound, etc.). | 6 | 35 | ||||
| Communication and rapport | 3. The phone call did not make me feel nervous and uncomfortable. | 1 | 3 | 37 | ||
| 4. I could easily explain my medical problems to the doctor in the phone call. | 2 | 1 | 4 | 9 | 25 | |
| 5. I took my doctor's advice given by phone call seriously. | 2 | 4 | 35 | |||
| Clinical assessment | 6. I was confident that the clinician could assess my condition via phone call as if I was there. | 1 | 2 | 10 | 12 | 16 |
| 7. I believe the doctor understood clinical situation during the phone call visit. | 2 | 1 | 1 | 11 | 26 | |
| 8. I was confident that the doctor could evaluate my medication requirements via phone call. | 2 | 2 | 7 | 30 | ||
| 9. The lack of physical contact in a phone call is NOT a problem for managing my condition. | 2 | 1 | 7 | 9 | 22 | |
| Program evaluation | 10. Telehealth enables me to save money and time. | 4 | 5 | 32 | ||
| 11.Telehealth improves my access to specialist care. | 1 | 5 | 6 | 29 | ||
| 12. I would like to use telehealth again in the future. | 3 | 3 | 10 | 5 | 20 | |
| 13. I believe that telehealth is good for achieving good control of my condition. | 2 | 3 | 13 | 7 | 16 | |
| 14. I prefer to have my next consultation via telehealth. | 1 | 1 | 9 | 8 | 22 | |
| Comment | 15. If you have any comments or suggestions about the telehealth service please note here. | |||||
3.2. Patient comments and suggestions on telemedicine
Comments were provided by 33 of 41 respondents. Most (20 of 33) expressed gratitude and appreciation, as the service saved them time and money, whereas 2 patients would have preferred a video consultation. In-office visits were preferred by 6 patients. Although patients' privacy and confidentiality were well protected, one patient was worried about the lack of privacy utilizing such a service. One patient suggested starting virtual clinics after the patient's first visit to the clinic. The remaining respondents provided no comments.
4. Discussion
While the first study discussing the application of telemedicine during outbreaks was published in 2015 [9], the Kingdom of Saudi Arabia started to consider telemedicine as a part of the health care system in August 2013 by initiating the National Health Information System, which connected an electronic network of health information with the Ministry of Health, medical services in the military bodies, university hospitals, and other relevant government agencies to create and supervise a national telemedicine network [10]. Although the infrastructure is available for video consultations, we kept in mind social and religious considerations, as many female patients commit to Islamic hijab. For this reason, we preferred to use the phone call as main method for virtual clinics. The virtual clinics were organized to be conducted by specialists, residents, or consultants from our department. They were to take a detailed patient history and prescribe the proper medication according to the patient's needs, which was then to be delivered to patients' residence by a national delivery company. However, depending on the condition of each case, patients were given rescheduled appointments after 2–6 months. No decision to discontinue follow-up was made among our cases.
A small percentage (1.48%) of patients needed to be evaluated in the clinic, and most of them were in their first visit post-surgery. About (98.52%) of cases in our clinic could be managed remotely during the COVID-19 pandemic. This demonstrated that the rhinology specialty is amenable to the use of telemedicine during pandemic infections or as a screening tool but not on a regular basis. This is because the nose and in particular the sinuses are internal organs that require specific instruments (such as a nasal speculum or endoscope) to perform valid examinations or to take a biopsy [11]. Unlike other specialties that can examine patients effectively via video consultations, rhinologic practice requires further assessment in the clinic, which limits the hoped-for role of video consultations. Hence, the possibility of developing a guideline to triage those who need in-office consultations has been discussed in the literature [12] and some indicators were suggested for in-person visits during pandemics. We have also found that telemedicine could be utilized for other indications (Table 2 ). These suggested indications could be considered as a significant step to establish guidelines for in-office visits during pandemics. However, clinical judgment is still needed to distinguish the urgency and importance of an in-office visit in each case. All rhinology patients should know the worrisome symptoms that necessitate seeking immediate medical care. Therefore, community medical education is important before implementation of telemedicine. While the medical community has been enthusiastic in activating telemedicine, we have to consider patient opinions about such a step. Thus, we specified a portion of our study to assess patients' satisfaction with telemedicine. With the vast majority (84%) of patients satisfied or highly satisfied with telemedicine, we note that telemedicine as a modality of care during the pandemic faces minor or no opposition due to patients' understanding of the importance of social distancing. Generally, the main concern of these patients was clinical assessment via telemedicine, as they believed that their condition should be evaluated in the clinic. Therefore, to reassure patients, we rescheduled all patients 2–6 months later according to their condition.
Table 2.
Suggested indications for rhinologic in-office visits during pandemics.
| Indications for rhinologic in-office visits during pandemics |
|---|
|
We had some limitations in our study. Our virtual clinic depends exclusively on phone calls, which resulted in a lost opportunity to study telemedicine in Saudi Arabia from all aspects. Another limitation is the sizable number of patients who did not answer the phone call (n = 154) (due to connectivity issues, a closed phone, a wrong number, or simply not answering the call) and the retrospective nature of the study.
5. Conclusions
COVID-19 is the first worldwide pandemic in the technology era, and we know it will not be the last. We can conclude that we have to prepare our communities and health systems for such scenarios by establishing guidelines, facilities, and training. As a start, from this study we conclude that telemedicine proved its effectiveness in the efficient management and screening of rhinology cases during disasters and public health emergencies such as the COVID-19 pandemic while providing sufficient protection for patients and medical practitioners. Moreover, telemedicine as a modality of care during a pandemic faced minor or no opposition due to patients' understanding of the importance of social distancing.
Author's note
Saad Alsaleh is considered a co-first author and contributed equally to the first author.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.World Health Organization Pneumonia of unknown cause – China [internet] 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [cited 2020 Jul 18]. Available from:
- 2.World Health Organization WHO director-General's opening remarks at the media briefing on COVID-19-11 [internet] 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [cited 2020 Jul 18]. Available from:
- 3.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. New England Journal of Medicine. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Layfield E., Triantafillou V., Prasad A., Deng J., Shanti R.M., Newman J.G., et al. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42(7) doi: 10.1002/hed.26285. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryu S. Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth 2009 (global observatory for eHealth series, volume 2) Healthc Inform Res. 2012;18(2):153–155. [Google Scholar]
- 6.Ministry of Health MOH reports first case of coronavirus infection [internet] 2020. https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-03-02-002.aspx [cited 2020 Jul 21]. Available from:
- 7.Saudi Press Agency 24 hours lockdown policy all over the kingdom of Saudi Arabia Kingdom of Saudi Arabia [internet] 2020. www.spa.gov.sa/2070988 [cited 2020 Jul 21]. Available from:
- 8.Fatehi F., Martin-Khan M., Smith A.C., Russell A.W., Gray L.C. Patient satisfaction with video teleconsultation in a virtual diabetes outreach clinic. Diabetes Technol Ther. 2015;17(1):43–48. doi: 10.1089/dia.2014.0159. [DOI] [PubMed] [Google Scholar]
- 9.Ohannessian R. Telemedicine: potential applications in epidemic situations. European Research in Telemedicine/La Recherche Européenne en Télémédecine. 2015;4(3):95–98. Sep 1. [Google Scholar]
- 10.National Health Information System About the center [internet] 2013. https://nhic.gov.sa/AboutUs/Pages/default.aspx [cited 2020 Jul 23]. Available from:
- 11.K Maru Y., Gupta Y. Nasal endoscopy versus other diagnostic tools in Sinonasal diseases. Indian J Otolaryngol Head Neck Surg. 2016;68(2):202–206. doi: 10.1007/s12070-014-0762-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Setzen M., Svider P.F., Pollock K. COVID-19 and rhinology: a look at the future. Am J Otolaryngol. 2020;41(3):102491. doi: 10.1016/j.amjoto.2020.102491. Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]