Abstract
Background
Healthcare workers, who are at the forefront of the fight against COVID-19, are particularly susceptible to physical and mental health consequences such as anxiety and depression. The aim of this umbrella review of meta-analyses is to determine the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic.
Methods
Using relevant keywords, data resources including PubMed, Scopus, Web of Science, Cochrane, ProQuest, Science Direct, Google Scholar and Embase were searched to obtain systematic reviews and meta-analyses reporting the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic from the beginning of January to the end of October 2020. The random effects model was used for meta-analysis, and the I2 index was employed to assess heterogeneity among studies. Data was analyzed using STATA 14 software.
Results
In the primary search, 103 studies were identified, and ultimately 7 studies were included in the umbrella review. The results showed that the overall prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic was 24.94% (95% CI: 21.83–28.05, I2 = 0.0%, P = 0.804) and 24.83% (95% CI: 21.41–28.25, I2 = 0.0%, P = 0.897), respectively.
Conclusion
This umbrella review shows that the prevalence of anxiety and depression is relatively high among healthcare workers during the COVID-19 pandemic. Healthcare workers should be provided with resources to minimize this risk.
Keywords: COVID-19, Mental disorder, Health personnel, Systematic review, Meta-analysis
1. Introduction
In December 2019, a novel type of coronavirus started to spread from China, ravaging all countries around the world within a few months. On February 12, 2020, the World Health Organization (WHO) recognized the disease as coronavirus disease 2019 (COVID-19) (Vardanjani et al., 2020; Mallet et al., 2020). The COVID-19 pandemic has been linked to a great deal of anxiety, exacerbation of mental illnesses (Mallet et al., 2020; da Silva and Neto, 2020), social isolation, and feelings of helplessness and abandonment in various populations (Ornell et al., 2020; Khademi et al., 2020). In one study, 53.8% of respondents perceived the psychological impacts of COVID-19 as moderate to severe with the prevalence of related depression and anxiety as 16.5% and 28.8%, respectively(Wang et al., 2020). During epidemics, healthcare workers are susceptible to significant psychological stress related to exposure to disease, concerns about transmitting the infection to family members, shortages in personal protective equipment (PPE), longer working hours, and challenging decisions regarding the allocation of limited resources to patients (Pfefferbaum and North, 2020; Shaukat et al., 2020; Mokhtari et al., 2020). The COVID-19 pandemic has placed healthcare workers around the world in an unprecedented situation. The risk of adverse psychological outcomes among healthcare workers has been particularly high (Rajkumar, 2020). Healthcare workers are facing difficult conditions and limited resources to take care of COVID-19 patients, placing them at higher risk for depression, anxiety, and insomnia. It is vital to assess the mental health of healthcare workers who are at the frontlines of this pandemic. One study in China reported a high prevalence of depression (50.4%), anxiety (44.6%), insomnia (34%), and psychological distress (71.5%) among frontline healthcare providers (Lai et al., 2020).
The first step to providing mental health services and implementing effective psychological interventions, is to screen the mental health status of at-risk groups (Goldmann and Galea, 2014). Healthcare workers are recognized as a high-risk group for whom the psychological consequences of COVID-19 are significant and sustained (Fiorillo and Gorwood, 2020). Numerous studies have been conducted on the mental health of healthcare workers during the pandemic, but there has not been a comprehensive study to pool the results of published systematic reviews and meta-analyses to ascertain the prevalence of depression and anxiety among them. We conducted an umbrella review on the meta-analyses reporting the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic. The results of this study can provide important data to support policymaking and the allocation mental health services for healthcare workers.
2. Materials and methods
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) protocol was used (Liberati et al., 2009). The protocol was registered with the international prospective register of systematic reviews (PROSPERO) under the code of CRD42020216550.
2.1. Search strategy
The data resources of PubMed, Embase, Scopus, Web of Science, Cochrane, ProQuest, Science Direct and Google Scholar were searched using valid keywords which were extracted from terms in related articles and medical subject headings (MeSH). A search strategy was designed for each database using key words, operators and search fields. For example, the following search strategy was applied in the PubMed database: ((Anxiety OR “Anxiety Disorder*” OR “Mental health Disorder*” OR “Psychiatric Disorder*”) AND (Depression* OR “Depressive Symptom*” OR “Emotional Depression*”) AND (“2019 novel coronavirus disease” OR COVID19 OR “COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “COVID-19 virus disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “Coronavirus disease 2019” OR “2019-nCoV disease” OR “COVID-19 virus infection”) AND (“Health Personnel” OR “Health Care Provider*” OR “Health worker*” OR “Healthcare Provider*” OR “Healthcare Worker*” OR “Health care professional*” OR “medical staff” OR “Medical worker*”) AND (“Systematic review”) AND (“meta-analysis” OR “meta-analytic”)). Finally, searches were performed by designing combinations of the keywords to gather the studies published from the beginning of January to the end of October 2020. The search strategy in each database has been noted in Appendix A.
2.2. Study eligibility criteria
Systematic reviews and meta-analyses reporting the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic were included. Studies reporting mean scores for anxiety and depression, narrative reviews, systematic literature review, scoping review, rapid review, literature review and interventional and cross-sectional studies were excluded.
2.3. Study selection
Studies obtained after the primary literature search were inserted into EndNote X7 software. After removing duplicates, two researchers (AS and MG) independently reviewed the texts and selected the qualifying studies. Any disagreement between the two researchers was resolved through group discussions.
2.4. Study qualification and data extraction
Researchers (AS and MG) independently used the Assessment of Multiple Systematic Reviews v2 (AMSTAR-2) tool to check the methodological qualities of the selected studies(Shea et al., 2017). In the data extraction phase, the research team first designed a checklist in Microsoft Word software, and then two researchers independently recorded the required data including first authors' names, prevalence of anxiety, prevalence of depression, country, sample size, heterogeneity, publication bias, group study and age average into the checklist.
2.5. Statistical analysis
The I2 index was used to investigate heterogeneity among the studies. I2 values of <25%, 25 to 75%, and > 75% indicate low, moderate, and high heterogeneity, respectively (Kazemzadeh et al., 2019). The random effects model was utilized to perform the meta-analysis. Publication bias was assessed by the Egger's linear regression test, Begg's and Mazumdar's rank correlation tests. The significance level of the two tests is different, it is 0.05 in Egger's test and 0.1 in Begg's and mazumdar rank correlation test(Orlewski and Orlewska, 2015). Data analysis was performed in STATA software (version 14).
3. Results
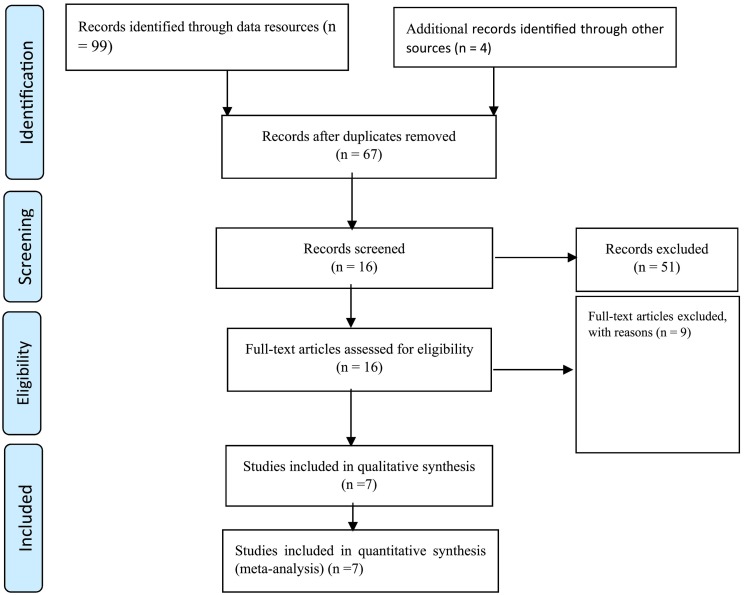
After the comprehensive literature search, 103 studies were initially identified. After removing duplicates, 67 studies were further screened, and 16 of these were subjected to the full-text review. Following quality assessment, seven studies were included in the umbrella review phase. The study selection process is shown in Fig. 1 .
Fig. 1.
Flowchart of the Selection of Studies Based on PRISMA.
The final seven meta-analyses subjected to the umbrella review consisted of 108 articles and 433,800 healthcare workers. Table 1 shows the characteristics of the included studies investigating the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic.
Table 1.
The Specifications of Studies Included in the Umbrella Review.
| First Author | Prevalence of depression | Prevalence of anxiety | Country | sample size (HCW) | Heterogeneity% I2 | Publication bias | Group study |
|---|---|---|---|---|---|---|---|
| (Ren et al., 2020) | 25% (95% CI: 4–45) | 27% (95% CI: 12–43) | China | 6098 | Anxiety: 99.4 Depression: 99.7 |
Anxiety: *0.721 and **0.925 Depression: *0.348 and **0.594 |
healthcare workers |
| (de Pablo et al., 2020) | 17.9% (95% CI: 6.7–40.1) | 22.2% (95% CI: 12.7–35.8) | United Kingdom | 19,307 | Anxiety: 99.091 Depression: 99.621 |
NA | nurses, physicians, medical students, social workers |
| (Dutta et al., 2020) | 25.9% (95% CI: 18.4–34.1) | 24.5% (95% CI: 17.9–31.9) | India | 34,021 | Anxiety: 99.1 Depression: 99.5 |
NA | Doctors, nurses Other healthcare workers |
| (Krishnamoorthy et al., 2020) | 25% (95% CI: 19–32) | 24% (95% CI: 16–32) | India | 171,571 | Anxiety: 99.6 Depression: 99.4 |
Anxiety: *0.83 Depression: *0.89 |
healthcare workers |
| (Luo et al., 2020) | 25% (95% CI: 17–33) | 26% (95% CI:18–34) | China | 162,639 | Anxiety= 98.94 Depression = 99.19 |
NA | healthcare workers |
| (Pappa et al., 2020) | 22.8% (95% CI: 15.1–31.51) | 23.21% (95% CI: 17.77–29.13) | United Kingdom | 33,062 | Anxiety= 99 Depression = 99.62 |
NA | Physicians, nurses Other healthcare workers |
| (da Silva and Neto, 2020) | 36% (95% CI: 19–58) | 33% (95% CI: 24–45) | Brazil | 7102 | NA | funnel plot (asymmetric) | Physicians, nurses Other healthcare workers |
* = Egger's Test, ** = Begg's tests, NA = Not Applicable, HCW = Healthcare workers.
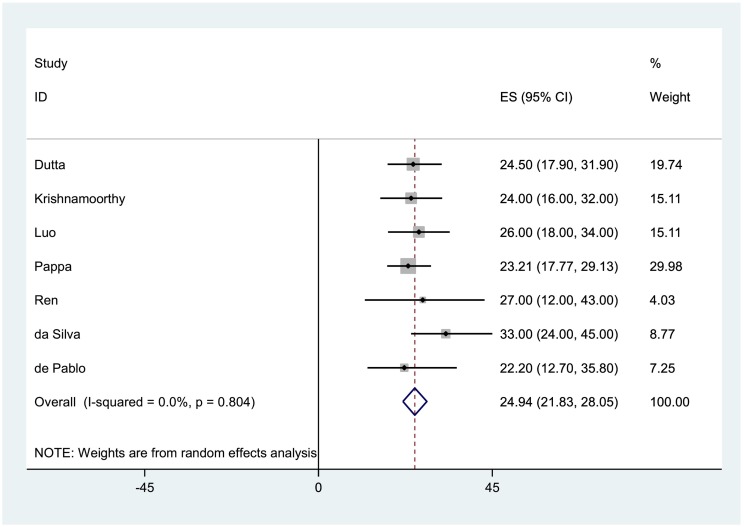
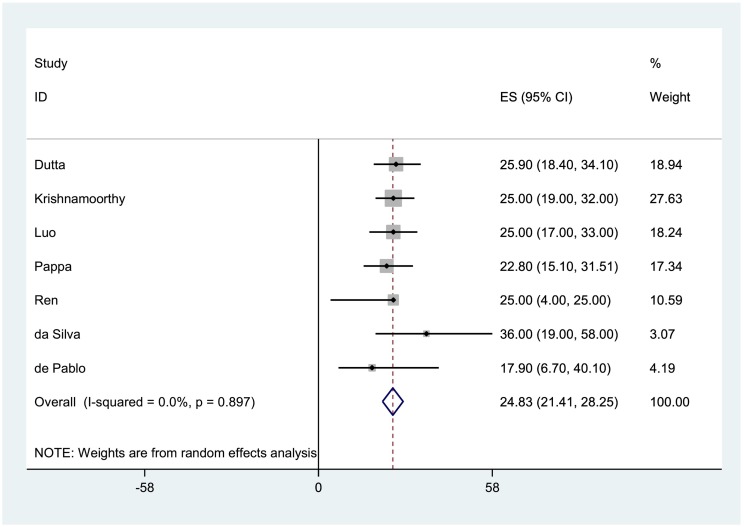
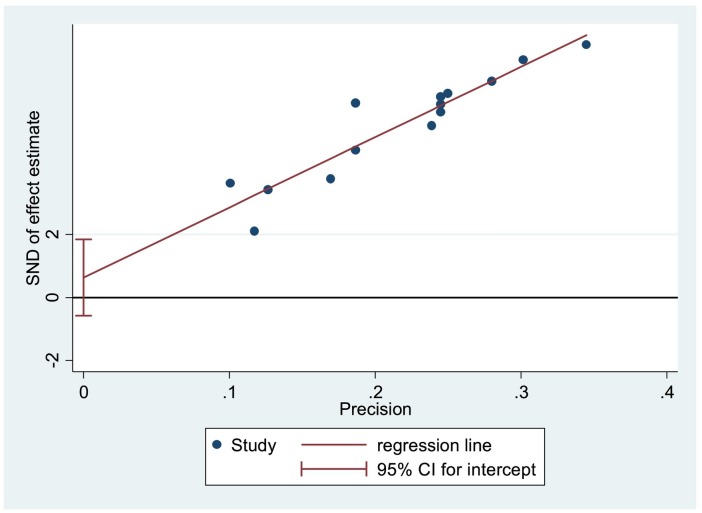
The prevalence of anxiety (Fig. 2 ) and depression (Fig. 3 ) among healthcare workers during the COVID-19 pandemic were 24.94% (95% CI: 21.83–28.05, I2 = 0.0%, P = 0.804) and 24.83% (95% CI: 21.41–28.25, I2 = 0.0%, P = 0.897), respectively. Based on the results of the Egger's (P = 0.279) and Begg's and Mazumdar's tests (P = 0.620) tests, publication bias was not significant in the present study (Fig. 4 ).
Fig. 2.
The Forest Plot of Overall and Individual Prevalence of anxiety in the Included Studies with 95% Confidence Interval.
Fig. 3.
The Forest Plot of Overall and Individual Prevalence of depression in the Included Studies with 95% Confidence Interval.
Fig. 4.
Publication Bias Based on Egger's Test.
4. Discussion
This umbrella review shows that the prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic were 24.94% and 24.83%, respectively. In the systematic review and meta-analysis conducted by Salari et al. (Salari et al., 2020), they reported the prevalence of anxiety and depression in the general population during the COVID-19 pandemic as 31.9% and 33.7% respectively. These numbers are close and highlight the possible impacts of COVID-19, on the mental health of people including patients, healthcare workers, children, students, and individuals in various sectors of the community (Bao et al., 2020; Ryu et al., 2020; Chen et al., 2020). Increased workload, burnout, inadequate PPE, the risk of contracting the disease, and the challenge of making difficult moral decisions about care priorities during the pandemic have exposed healthcare workers to severe psychological pressures leading to mental disorders such as anxiety and depression (Mokhtari et al., 2020). In a cross-sectional study of 939 healthcare workers during the COVID-19 pandemic by Shahin et al. (Şahin et al., 2020), the signs and symptoms of anxiety and depression were observed in 60.2% and 77.6% of participants, respectively. In the early stages of the pandemic in Italy, 10% of healthcare workers contracted Covid-19, of whom 3% died (Mokhtari et al., 2020). These high infectivity and mortality rates can lead to anxiety and depression among healthcare workers around the world. Furthermore, factors such as a high-risk workplace, a lack of clinical experience, young age, and a history of psychological disorders can contribute to the development of anxiety and depression among healthcare workers (Salari et al., 2020; Mokhtari et al., 2020; Şahin et al., 2020).
In their study, Khanal et al. reported that inadequate isolation precautions were significantly associated with signs of anxiety and depression among healthcare workers (Khanal et al., 2020). A shortage in preventive measures, such as insufficient PPE, can render the work environment dangerous, leading to a feeling of insecurity and vulnerability to the infection. Studies across the world (Du et al., 2020; Chen et al., 2020; Liu et al., 2020) have highlighted the need for providing healthcare workers with adequate PPE and psychological support to increase their resilience.
According to studies performed on healthcare workers during the severe acute respiratory syndrome (SARS) pandemic of 2003 and this current COVID-19 pandemic, nurses have poor outcomes in terms of mental health and anxiety disorders compared to other healthcare professionals. This may be because they spend more time caring for patients compared to other healthcare workers. A study in China also showed that nurses experienced more unfavorable mental health outcomes than other health staff (Khanal et al., 2020; Lai et al., 2020; Maunder et al., 2004). Of note, poor mental health in healthcare workers will affect the quality of the health care provided (Khanal et al., 2020; Brooks et al., 2018; Maharaj et al., 2019). Therefore, hospital leadership should pay special attention to the mental well-being of their employees, especially nurses, as the mismanagement of their mental health can lead to dire public health consequences. Future studies are needed to identify specific risk factors for psychological disorders such as anxiety and depression among healthcare workers in order to equip them with practical coping strategies.
5. Limitations
There are likely many non-English publications that we were not able to identify in our search. Additionally, the broad term “healthcare worker” does not allow us to make conclusions for specific subsets such as physicians or nurses. Similarly, some of the studies did not report the number of participants by gender.
6. Conclusion
This umbrella review shows that the prevalence of anxiety and depression is relatively high among healthcare workers during the COVID-19 pandemic. Healthcare workers should be provided with resources to minimize this risk. This can be done by identifying the risk factors of these disorders and taking appropriate measures such as emotional and mental support (via personal or group counseling sessions, lectures, mental health counseling hotlines, social networks, etc.). Due to the long duration of this pandemic, the lack of a definitive treatment, and the evidence indicating that we are many months away from mass-producing and distributing effective vaccines, health policy makers must consider preserving their human resources by implementing appropriate strategies. These may include redistributing individual workloads, recruiting new staff, providing sufficient PPE, providing financial and psychological support, and shortening shift lengths.
Funding
None.
Authors contributions
AS, KY, BN and MG designed the review, developed the inclusion criteria, screened titles and abstracts, appraised the quality of included papers, and drafted the manuscript. AS, SM, BN, MT and MG reviewed the study protocol and inclusion criteria and provided substantial input to the manuscript. AS, MG, SM, MS and KY reviewed the study protocol. AS, MG read and screened articles for inclusion. All authors critically reviewed drafts and approved the final manuscript.
Conflicts of interest statement
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
The authors whose names are listed immediately below report the following details of affiliation or involvement in an organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript. Please specify the nature of the conflict on a separate sheet of paper if the space below is inadequate.
Ethical considerations
Not applicable.
Acknowledgements
None.
Appendix A
Table A1.
Using database-appropriate syntax, with parentheses, Boolean operators, and field codes.
| Data base | Syntax | Records Number |
|---|---|---|
| PubMed | ((Anxiety OR “Anxiety Disorder*” OR “Mental health Disorder*” OR “Psychiatric Disorder*”) AND (Depression* OR “Depressive Symptom*” OR “Emotional Depression*”) AND (“2019 novel coronavirus disease” OR COVID19 OR “COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “COVID-19 virus disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “Coronavirus disease 2019” OR “2019-nCoV disease” OR “COVID-19 virus infection”) AND (“Health Personnel” OR “Health Care Provider*” OR “Health worker*” OR “Healthcare Provider*” OR “Healthcare Worker*” OR “Health care professional*” OR “medical staff” OR “Medical worker*”) AND (“Systematic review” OR “systematic literature review” OR “scoping review” OR “rapid review” OR “literature review”) AND (“meta-analysis” OR “meta-analytic”)) | 11 |
| Scopus | ((ALL(Anxiety) OR ALL(“Anxiety Disorder*”) OR ALL(“Mental health Disorder*”) OR ALL(“Psychiatric Disorder*”)) AND (ALL(Depression*) OR ALL(“Depressive Symptom*”) OR ALL(“Emotional Depression*”)) AND (ALL(“2019 novel coronavirus disease”) OR ALL(COVID19) OR ALL(“COVID-19 pandemic”) OR ALL(“SARS-CoV-2 infection”) OR ALL(“COVID-19 virus disease”) OR ALL(“2019 novel coronavirus infection”) OR ALL(“2019-nCoV infection”) OR ALL(“Coronavirus disease 2019”) OR ALL(“2019-nCoV disease”) OR ALL(“COVID-19 virus infection”)) AND(ALL (“Health Personnel”) OR ALL(“Health Care Provider*”) OR ALL(“Health worker*”) OR ALL(“Healthcare Provider*”) OR ALL(“Healthcare Worker*”) OR ALL(“Health care professional*”) OR ALL(“medical staff”) OR ALL(“Medical worker*”)) AND (TITLE-ABS (“Systematic review”) OR ALL(“systematic literature review”) OR ALL(“scoping review”) OR ALL(“rapid review”) OR ALL(“literature review”)) AND (TITLE-ABS(“meta-analysis”) OR ALL(“meta-analytic”))) | 53 |
| Web Of science | ((TS = (Anxiety) OR TS = (“Anxiety Disorder*”) OR TS = (“Mental health Disorder*”) OR TS = (“Psychiatric Disorder*”)) AND (TS = (Depression*) OR TS = (“Depressive Symptom*”) OR TS = (“Emotional Depression*”)) AND (TS = (“2019 novel coronavirus disease”) OR TS = (COVID19) OR TS = (“COVID-19 pandemic”) OR TS = (“SARS-CoV-2 infection”) OR TS = (“COVID-19 virus disease”) OR TS = (“2019 novel coronavirus infection”) OR TS = (“2019-nCoV infection”) OR TS = (“Coronavirus disease 2019”) OR TS = (“2019-nCoV disease”) OR TS = (“COVID-19 virus infection”)) AND(TS = (“Health Personnel”) OR TS = (“Health Care Provider*”) OR TS = (“Health worker*”) OR TS = (“Healthcare Provider*”) OR TS = (“Healthcare Worker*”) OR TS = (“Health care professional*”) OR TS = (“medical staff”) OR TS = (“Medical worker*”)) AND (TS = (“Systematic review”) OR TS = (“systematic literature review”) OR TS = (“scoping review”) OR TS = (“rapid review”) OR TS = (“literature review”)) AND (TS = (“meta-analysis”) OR TS = (“meta-analytic”))) | 5 |
References
- Bao Y., Sun Y., Meng S., Shi J., Lu, L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Dunn R., Amlôt R., Rubin G.J., Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018;60:248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva F.C.T., Neto M.L.R. Psychological effects caused by the COVID-19 pandemic in health professionals: A systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2020:110062. doi: 10.1016/j.pnpbp.2020.110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Pablo G.S., Serrano J.V., Catalan A., Arango C., Moreno C., Ferre F., Shin J.I., Sullivan S., Brondino N., Solmi M. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 2020;275:48–75. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J., Dong L., Wang T., Yuan C., Fu R., Zhang L., Liu B., Zhang M., Yin Y., Qin J. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry. 2020;67:144–145. doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta A., Sharma A., Torres-Castro R., Pachori H., Mishra S. 2020. Mental Health Outcomes Among Healthcare Workers Dealing with COVID-19/SARS-CoV-2 Pandemic: A Systematic Review and Meta-Analysis. (Available at SSRN 3633225) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63 doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annu. Rev. Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Kazemzadeh M., Shafiei E., Jahangiri K., Yousefi K., Sahebi A. The preparedness of hospital emergency departments for responding to disasters in Iran; a systematic review and meta-analysis. Arch. Acad. Emerg. Med. 2019;7 [PMC free article] [PubMed] [Google Scholar]
- Khademi F., Moayedi S., Golitaleb M., Karbalaie N. The COVID-19 pandemic and death anxiety in the elderly. Int. J. Ment. Health Nurs. 2020 doi: 10.1111/inm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanal P., Devkota N., Dahal M., Paudel K., Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob. Health. 2020;16:1–12. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020;293:113382. doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. (e203976-e203976) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Liu C.-Y., Yang Y.-Z., Zhang X.-M., Xu X., Dou Q.-L., Zhang W.-W., Cheng A.S. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol. Infect. 2020:1–17. doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu, M. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020;113190 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj S., Lees T., Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int. J. Environ. Res. Public Health. 2019;16:61. doi: 10.3390/ijerph16010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallet J., Dubertret C., LE Strat Y. Addictions in the COVID-19 era: current evidence, future perspectives a comprehensive review. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2020;110070 doi: 10.1016/j.pnpbp.2020.110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K., Petryshen P., Steinberg R., Wasylenki D., Koh D. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66:938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- Mokhtari R., Moayedi S., Golitaleb M. COVID-19 pandemic and health anxiety among nurses of intensive care units. Int. J. Ment. Health Nurs. 2020;29(6):1275–1277. doi: 10.1111/inm.12800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlewski J., Orlewska E. Effects of genetic polymorphisms of glutathione S-transferase genes (GSTM1, GSTT1, GSTP1) on the risk of diabetic nephropathy: a meta-analysis. Pol. Arch. Med. Wewn. 2015;125:649–658. doi: 10.20452/pamw.3045. [DOI] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz. J. Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020;102066 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren X., Huang W., Pan H., Huang T., Wang X., Ma, Y. Mental health during the COVID-19 outbreak in China: a meta-analysis. Psychiatry Q. 2020:1–13. doi: 10.1007/s11126-020-09796-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu S., Chun B.C., Of Epidemiology, K. S An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol. Health. 2020;42 doi: 10.4178/epih.e2020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J. Community Health. 2020:1–10. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaukat N., Ali D.M., Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020;13:1–8. doi: 10.1186/s12245-020-00299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., Moher D., Tugwell P., Welch V., Kristjansson E. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. bmj. 2017;358 doi: 10.1136/bmj.j4008. (j4008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardanjani A.E., Ronco C., Rafiei H., Golitaleb M., Pishvaei M.H., Mohammadi M. Early hemoperfusion for cytokine removal may contribute to prevention of intubation in patients infected with COVID-19. Blood Purif. 2020:1–4. doi: 10.1159/000509107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]