Abstract
Background
Cancer-related fatigue (CRF) is a common psychosomatic problem in breast cancer patients. Traditional Chinese medicine (TCM) has been used to address symptoms in patients with CRF. Identification of the specific constitution in TCM is essential for personalized care.
Aim
To explore the relationship between fatigue and specific constitutions in breast cancer.
Experimental procedure
We conducted a cross-sectional study in all breast cancer patients at Kaohsiung Chang Gung Memorial Hospital in Taiwan. The severity of fatigue was determined using the Brief Fatigue Inventory-Taiwanese (BFI-T) form. TCM patterns were determined using the Body Constitution Questionnaire (BCQ). The relationship between constitution and fatigue was analyzed using logistic regression.
Results
We recruited 110 breast cancer patients with fatigue (mean age: 55 ± 11 years). The mean duration of breast cancer was 17.4 months. The major constitution among these patients with fatigue was Yang-Qi deficiency (50%). Phlegm-Stasis syndrome was correlated with a duration of breast cancer of more than 18 months (p = 0.02). Out of all participants, 42.7% (n = 47) reported clinically significant fatigue (BFI-T score ≥4). According to logistic regression, the score of Yang-Qi deficiency [odds ratio (OR): 3.5, 95% confidence interval (CI): 1.49–8.21, p < 0.01] was also associated with clinically significant fatigue.
Conclusion
Yang-Qi deficiency is associated with clinically significant fatigue in breast cancer patients. However, the association of Phlegm-Stasis syndrome and fatigue as disease duration increases cannot be ignored. Further studies are needed to determine whether treating both constitutions integrating TCM treatment can alleviate patients’ fatigue symptoms.
Keywords: Breast cancer, Chemotherapy, Constitution, Fatigue, Traditional Chinese medicine
Abbreviations: BCQ, Body Constitution Questionnaire; BFI-T, Brief Fatigue Inventory–Taiwan; BMI, body mass index; CAM, complementary and alternative medicine; CRF, Cancer-related fatigue; CI, confidence interval; Hb, hemoglobin; OR, odds ratio; TCM, traditional Chinese medicine; VAS, visual analogue scale; WBC, white blood cell
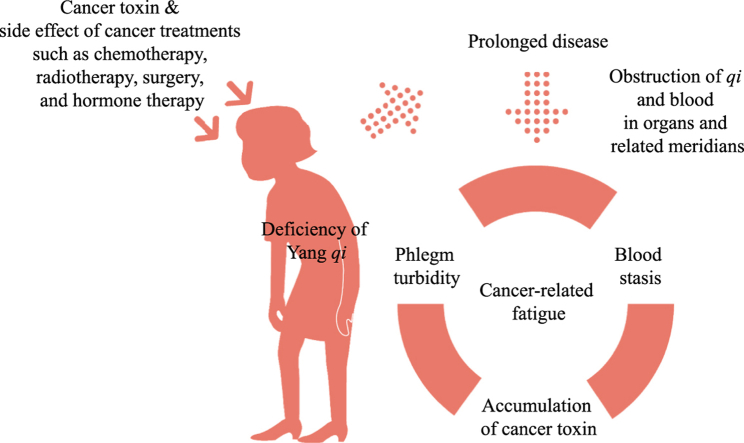
Graphical abstract
Highlights of the findings and novelties
-
•
Cancer-related fatigue is a common distressing symptom in patients with breast cancer.
-
•
Accurate Traditional Chinese medicine pattern diagnosis would provide objective and precise medical interventions.
-
•
The Yang-Qi deficiency constitution was associated with significant fatigue in breast cancer patients.
-
•
Phlegm-Stasis syndrome was correlated with a longer duration of breast cancer.
1. Introduction
Cancer-related fatigue (CRF) is a distressing symptom experienced by patients during the course of cancer and its treatment. Fatigue presents as sensations ranging from tiredness to exhaustion that affect the survivor’s physical, emotional, and/or cognitive functioning.1 The majority of patients will experience varying levels of fatigue during cancer treatment.2 Fatigue is the most common psychosomatic disorder in breast cancer patients,3 with an estimated prevalence of 40%.4 Furthermore, fatigue is associated with shorter survival, discontinuation of treatment, and all-cause mortality in cancer patients.5, 6, 7 The therapeutic strategies of CRF tends to focus on education, cognitive-behavioral therapy, psychostimulants, physical exercise, and treatment of comorbid conditions (e.g., insomnia, pain, emotional distress, anemia, and hypothyroidism).8,9 However, the effectiveness of current CRF approaches is limited because the pathogenesis of CRF has not been thoroughly explored.10
Complementary and alternative medicine (CAM) therapies such as herbal medicine,11,12 acupuncture,13 moxibustion,14 and qigong15 have been used in cancer patients with fatigue. Nearly 36% of breast cancer patients in Taiwan use traditional Chinese medicine (TCM), including herbal medicine and acupuncture, for their unmet needs such as reducing the side effects of conventional treatment, alleviating clinical symptoms, preventing recurrence and metastasis, and prolonging survival time.16,17 A high proportion of them believe that TCM has a positive impact on their quality of life (QOL) and improves their clinical status.18 In TCM, diseases are classified into different patterns (or ZHENG, syndrome, body constitutions) through assessment of each patient’s symptoms, tongue coating, and pulse.19 Qi (vital energy), Xue (blood) and Yin (body fluid) are the fundamental substances which make up the human body and maintain its normal physiological functioning. Once qi cannot govern the energy flow of the body to maintain blood circulation or warm and nourish the body, blood stasis or phlegm will develop, affecting the entire body and producing pathological symptoms and signs.20 Therefore, Yang-Qi deficiency, Yin-Xue deficiency, and Phlegm-Stasis syndrome are the most common TCM constitutions for patients, according to TCM theory. Balancing the disharmonious condition toward a gentleness type of constitution is more important than treating the specific disease.21 Precise TCM classification is the priority principle in treatment, and improper classification may entail serious consequences.
In TCM theory, it is generally believed that fatigue is an important characteristic of deficiency in qi. Despite the numerous attempts at prescribing qi tonifying agents to CRF patients,11,22 clinical treatment responses remain limited and the implementation of such treatment faces challenges. Thus, understanding the TCM patterns that are associated with fatigue in breast cancer patients may improve the efficacy and safety of treatment. The objective of this study was to analyze TCM patterns associated with fatigue in breast cancer patients.
2. Materials and methods
2.1. Recruitment
This was a cross-sectional study performed in a cancer center at Kaohsiung Chang Gung Hospital from October 2017 to March 2018. The inclusion criteria were female gender, a histologically diagnosis of breast cancer, current enrollment in standard neoadjuvant or adjuvant chemotherapy treatment in an inpatient setting, Eastern Cooperative Oncology Group (ECOG) performance score of 0–2, age of 20 years or older, and ability to provide informed consent. Patients with cognitive defects, heart disease, renal insufficiency, pregnancy, or lactation were excluded.
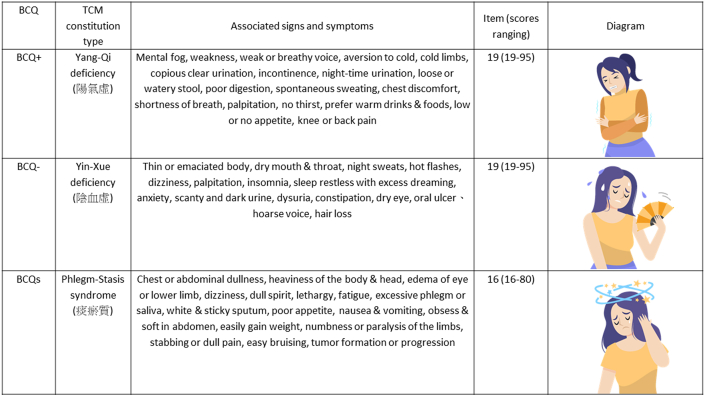
2.2. Data collection
The TCM pattern in the Body Constitution Questionnaire (BCQ), developed by Prof. Yi-Chang Su, was used to measure the psychological and physiological states of deviations in body constitution in each patient during the previous month.23,24 In 2007, the BCQ was recognized as a national standard measure that can be applied to clinical trials adopting TCM interventions in Taiwan. The reliability and validity were previously evaluated on 597 participants recruited from three different geographical districts in Taiwan. The results indicated good internal consistency, with Cronbach’s α of 0.93, and good test–retest reliability of 0.72–0.80 for the 3 subscales.23 The BCQ contains 44 items on the following three major constitution types as shown in Fig. 1: Yang-Qi deficiency (BCQ+, 19 Items), Yin-Xue deficiency (BCQ-, 19 Items), and Phlegm-Stasis syndrome (BCQs, 16 Items). Symptom frequency and intensity in the previous month are reported on a 5-point Likert-type scale (1, never; 2, occasionally; 3, sometimes; 4, often; 5, always). Scores of ≥31, 30, and 27 are respectively used as the thresholds for the 3 individual constitution types.24 A higher score indicates a more pronounced constitution. In the BCQ, the main three body constituents are calculated separately, so the subjects may have conditions ranging from none of the constitution types to all three constitution types. If a score indicates two or three of the constitution types, it is classified as a Mixed type. If a score indicates none of the three, then it is classified as the Gentleness type. However, both Mixed type and Gentleness are only classifications of the additional constitution type and cannot be used to quantify in degree.
Fig. 1.
The major three traditional Chinese medicine (TCM) patterns and clinical characteristics in the Body Constitution Questionnaire (BCQ).
The Brief Fatigue Inventory–Taiwan (BFI-T) questionnaire was used to evaluate fatigue severity.25 The BFI-T consists of 9 questions, each scored on a scale of 0–10. The total score is obtained from the sum of the question scores and indicates one of 4 levels of fatigue severity as follows: 0, normal; 1–3, mild; 4–6, moderate; and 7–10, severe. The cutoff indicating clinically significant fatigue is 4, based on the results of previous studies, as a lower cut-off could lead to overestimation of the severity.26,27 Severity of pain and sleep disturbance were measured on a visual analogue scale (VAS). The subjects were informed that the scales increased in intensity from left to right, with 0 corresponding to “none” and 10 indicating “very severe”, and they were asked to record their severities of pain and sleep disturbance accordingly. All BCQ, BFI-T, and VAS questionnaires were administered by an assistant and completed at enrollment. Demographic characteristics, such as gender, age, body mass index (BMI), and comorbidities, were recorded. Patients’ information related to current treatment and their biochemistry data, including white blood cell and hemoglobin, were recorded in the same month of enrollment.
2.3. Ethical approval and informed consent
This study was approved by the Institutional Review Board of Chang Gung Medical Foundation (201701347B0). This study was conducted in accordance with the Helsinki Declaration. Informed consent was obtained from each subject.
2.4. Statistical analysis
Power analysis for a multiple regression with eight predictors was conducted in G∗Power version 3.1. The results indicated that a sample size of at least 107 patients would be sufficient for our study, using an alpha of 0.05 and power of 80%. Data are reported as mean ± standard deviation or frequency (percentage), as appropriate. Data were analyzed using Student’s t-test or chi-square test for continuous and categorical variables. The association between CRF and the scores of TCM body constitution pattern and other independent variables was analyzed using univariable logistic regression, which was followed by stepwise logistic regression with adjustments for confounders. A cutoff score for the CRF (≥4) was identified for clinically significant fatigue. The fatigue confounders were determined based on factors reported in the literature and the results of univariable regression. The confounders included duration of disease, chemotherapy cycle, pain, sleep disturbance, and three major TCM body constitutions. The odds ratio (OR) and 95% confidence interval (CI) were calculated. All analyses were performed in SPSS version 23, and p < 0.05 was considered statistically significant.
3. Results
All the breast cancer patients recruited in the study were females, and their mean age was 55.1 ± 11.1 years (Table 1). Most (79.1%) of the subjects were married, and 57.3% were housewives. Seventy-seven patients (70%) had early-stage disease (stages 0–II), while 33 (30%) had locally advanced or metastatic disease (stages III–IV). The mean duration (time at diagnosis of breast cancer) was 17.4 months, and the average number of cycles of chemotherapy was 4.3. Approximately 21% of the patients used TCM at least once during the standard treatment. The mean score of the BFI-T was 3.4, and 42.7% of the patients reported clinically significant fatigue (BFI-T score ≥ 4 points). The proportions of the TCM patterns were Mixed type, 49.1%; Gentleness type, 1.8%; Yang-Qi deficiency, 50%; Yin-Xue deficiency, 48.2%; and Phlegm-Stasis syndrome, 44.5%.
Table 1.
Characteristics of breast cancer patients at Kaohsiung Chang Gung Memorial Hospital from October 2017 to March 2018.
| Clinical characteristics | N = 110 |
|---|---|
| Age (years)a | 55.1 ± 11.1 |
| Marriage, n (%) | 87 (79.1) |
| Housewives, n (%) | 63 (57.3) |
| Duration of disease (months)a |
17.4 ± 33.9 |
| Chronic diseases, n (%) | |
| Hypertension | 30 (27.3) |
| Chronic liver disease |
11 (10.0) |
| Stage, n (%) | |
| 0-II | 77 (70) |
| III-IV | 33 (30) |
| Fatigue (BFI-T score)a | 3.4 ± 2.3 |
| VAS of sleep disturbancea | 3.3 ± 2.5 |
| VAS of paina | 2.1 ± 2.4 |
| Concurrent TCM user, n (%) | 23 (20.9) |
| Surgery, n (%) | 36 (32.7) |
| Chemotherapy cycle, n (%) | 4.3 ± 9.2 |
| ≤ 9 times | 104 (94.5) |
| > 10 time | 6 (5.5) |
| BMI (kg/m2)a | 24.3 ± 3.5 |
| White blood cell (mm3)a | 6530 ± 3405 |
| Hemoglobin (g/dl)a |
11.8 ± 1.45 |
| TCM patterna | |
| Gentleness | 2 (1.8) |
| Yang-Qi deficiency | 55 (50.0) |
| Yin-Xue deficiency | 53 (48.2) |
| Phlegm-Stasis syndrome | 49 (44.5) |
| Mixed type | 54 (49.1) |
BFI-T: Brief Fatigue Inventory–Taiwan; VAS: Visual analogue scale; TCM: traditional Chinese medicine; BMI: body mass index.
Mean ± SD.
The patient characteristics according to fatigue status in the two groups are shown in Table 2. Disease duration was longer in group 1 than in group 2 (p < 0.01). The number of chemotherapy cycles was higher in group 1 than in group 2 (p < 0.05). Additionally analyzing the dichotomized body constitution revealed that the proportions of patients with Yang-Qi deficiency (p < 0.001), Yin-Xue deficiency (p < 0.05), and Phlegm-Stasis syndrome (p < 0.01) were higher in group 1 than in group 2. Pain (p < 0.001) and sleep disturbance (p < 0.01) scores were higher in group 1 than in group 2. There were no differences in age, surgery, TCM use, BMI, white blood count, or hemoglobin between the two groups.
Table 2.
Characteristics of patients with different degrees of fatigue.
| Characteristics | Group 1 (BFI-T: ≥ 4), n = 47 | Group 2 (BFI-T: < 4), n = 63 | P value |
|---|---|---|---|
| Age (years) | 54.8 ± 10.9 | 55.2 ± 11.2 | 0.83 |
| Marriage, n (%) | 36 (41.4) | 51 (58.6) | 0.63 |
| Duration of disease (months) |
28.5 ± 43.8 |
9.06 ± 20.8 |
0.006∗∗ |
| Chronic disease, n (%) | |||
| Hypertension | 13 (43.3) | 17 (56.7) | 1.00 |
| Chronic liver disease | 2 (18.2) | 9 (81.8) | 0.11 |
| Stage, n (%) | 0.51 | ||
| 0-II | 11 (36.7) | 19 (63.3) | |
| III-IV | 36 (45.0) | 44 (55.0) | |
| VAS of sleep disturbance | 4.2 ± 2.7 | 2.8 ± 2.3 | 0.006∗∗ |
| VAS of pain | 3.2 ± 2.9 | 1.5 ± 1.9 | 0.001∗∗∗ |
| Concurrent TCM user, n (%) | 11 (52.2) | 12 (47.8) | 0.63 |
| Surgery, n (%) | 11 (30.6) | 25 (69.4) | 1.00 |
| Chemotherapy cycle, n (%) | 0.03∗ | ||
| ≤ 9 times | 42 (40.4) | 62 (59.6) | |
| > 10 times | 5 (83.3) | 1 (16.7) | |
| BMI (kg/m2) | 24.2 ± 3.9 | 24.4 ± 3.1 | 0.74 |
| White blood cell (mm3) | 6876 ± 4389 | 6271 ± 2434 | 0.35 |
| Hemoglobin (g/dl) |
11.4 ± 1.41 |
11.9 ± 1.4 |
0.07 |
| TCM pattern, n (%)a | |||
| Gentleness | 1.00 | ||
| No | 46 (42.6) | 62 (57.4) | |
| Yes | 1 (50.0) | 1 (50.0) | |
| Yang-Qi deficiency | <0.001∗∗∗ | ||
| No | 14 (25.5) | 41 (74.5) | |
| Yes | 33 (60.0) | 22 (40.0) | |
| Yin-Xue deficiency | 0.02∗ | ||
| No | 18 (31.6) | 39 (68.4) | |
| Yes | 29 (54.7) | 24 (45.3) | |
| Phlegm-Stasis syndrome | 0.007∗∗ | ||
| No | 19 (31.1) | 42 (68.9) | |
| Yes | 28 (57.1) | 21 (42.9) | |
| Mixed Type | 0.07 | ||
| No | 17 (30.4) | 39 (69.6) | |
| Yes | 30 (55.6) | 24 (44.4) | |
∗p < 0.05. ∗∗p < 0.01. ∗∗∗p < 0.001.
BFI-T: Brief Fatigue Inventory–Taiwan; VAS: Visual analogue scale; TCM: traditional Chinese medicine; BMI: body mass index.
Chi-Squared Test.
The mean BCQ scores of breast cancer patients with Yang-Qi deficiency, Yin-Xue deficiency, and Phlegm-Stasis syndrome were 31.5, 29.8, and 25.9, respectively. The mean duration of disease (time since initial diagnosis of breast cancer) was 17.4 months. With respect to the duration of disease in the patients with fatigue, the BCQ scores of the TCM patterns changed over time. We found that Phlegm-Stasis syndrome was correlated with a duration of disease of more than 18 months (p < 0.05) (Table 3).
Table 3.
The Body Constitution Questionnaire scores of the major three traditional Chinese medicine patterns in patients with fatigue according to the duration of disease.
| Characteristics | Duration of disease <18 months, n = 89 | Duration of disease ≥18 months, n = 21 | P value |
|---|---|---|---|
| Yang-Qi deficiency | 30.8 ± 7.88 | 34.4 ± 7.77 | 0.06 |
| Yin-Xue deficiency | 29.2 ± 7.15 | 32.0 ± 7.09 | 0.12 |
| Phlegm-Stasis syndrome | 25.2 ± 6.87 | 29.0 ± 7.49 | 0.02∗ |
In univariable logistic regression, the scores of Yang-Qi deficiency (OR: 4.39, 95% CI: 1.95–9.89, p < 0.001), Yin-Xue deficiency (OR 2.61, 95% CI: 1.20–5.69, p < 0.05) and Phlegm-Stasis syndrome (OR: 2.90, 95% CI: 1.34–6.45, p = 0.007) were associated with clinically significant fatigue (Table 4). Longer duration of disease (OR: 1.00, 95% CI: 1.00–1.03), higher VAS of pain (OR: 1.38, 95% CI: 1.15–1.67) and sleep disturbance (OR: 1.29, 95% CI: 1.10–1.52) were associated with a significantly increased risk of fatigue in breast cancer (p < 0.05). Stepwise logistic regression indicated that the score of Yang-Qi deficiency was associated with fatigue, but that the scores of other two types were not. The adjusted OR of Yang-Qi deficiency was 3.50 (95% CI: 1.49–8.21, p < 0.01). Duration of disease (adjusted OR: 1.02, 95% CI: 1.00–1.03, p < 0.05) and severity of pain (adjusted OR: 1.32, 95% CI: 1.09–1.60, p < 0.01) were independently associated with fatigue. Patients’ chemotherapy cycles and sleep disturbance were not associated with fatigue.
Table 4.
Odds ratio (ORs) of the traditional Chinese medicine (TCM) patterns for clinically significant fatigue according to logistic regression.
| Factors | Crude univariate |
Adjust multivariablea |
||||
|---|---|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | |||
| Duration of disease (months) | 1.00 | 1.00 | 1.03 | – | – | – |
| VAS of sleep disturbance | 1.29 | 1.10 | 1.52 | – | – | – |
| VAS of pain | 1.38 | 1.15 | 1.67 | 1.32 | 1.09 | 1.60 |
| Chemotherapy cycle ≤9 times/> 10 times |
0.11 |
0.01 |
0.94 |
– |
– |
– |
|
TCM pattern | ||||||
| Yang-Qi deficiency | 4.39 | 1.95 | 9.89 | 3.50 | 1.49 | 8.21 |
| Yin-Xue deficiency | 2.61 | 1.20 | 5.69 | – | – | – |
| Phlegm-Stasis syndrome | 2.90 | 1.34 | 6.45 | – | – | – |
VAS: Visual analogue scale, TCM: traditional Chinese medicine.
Stepwise logistic regression analysis with the application of a likelihood ratio test.
4. Discussion
The aim of this study was to explore the associations between the major TCM patterns and CRF in breast cancer patients. Approximately 88% of the patients in this cross-sectional study had experienced fatigue symptoms, and 42.7% had moderate to severe fatigue symptoms. A cut-off BFI-T score of 4 was used according to the results of previous studies,26,27 which demonstrated that scores of ≥4 are correlated with higher functional interference scores, lower QOL, and greater symptom distress. The clinical cut-off for measures of fatigue severity has been identified in cases of clinically significant CRF.28 Moreover, it can serve as an eligibility criterion for participants in intervention trials focused on treating clinically meaningful fatigue.29
We found that the degree of Yang-Qi deficiency in patients with breast cancer was associated with fatigue, according to the logistic regression. In TCM theory, Yang-Qi deficiency indicates an insufficiency of the primordial qi and is characterized by fatiguing easily, lack of energy, low appetite, poor circulation, and even cold symptoms.30 Yang-Qi deficiency contributes to the development of fatigue in patients with breast cancer.31,32 According to TCM theory, disease progression may lead to an imbalance of Yin and Yang, followed by weakness of Essence qi. Our findings showed that Yang-Qi deficiency was correlated with prolonged disease duration in the significant fatigue group, in accordance with TCM theory. As noted by Yeh et al., in cancer patients, Qi-deficiency and Yang-deficiency are independently associated with a higher risk of moderate-to-severe CRF.33 Many questionnaires try to classify TCM patterns according to individuals’ developmental, physiological, and psychological characteristics, which are innate or acquired over time, and to develop national standards for measurement. To date, few unified criteria have been published for TCM patterns, but the implications of either Yang- or Qi-deficiency types for fatigue in research settings have led to some consensus. If cancer patients lose the driving force of Yang-qi and reduce their daily amount of physical activity, they are more likely to have fatigue.34 Disruption of metabolic activity in the mitochondria may explain the association between fatigue and Yang-Qi deficiency in cancer patients. 34Additionally, elevated inflammatory cytokines, especially from radiotherapy or chemotherapy, may lead to fatigue by affecting the hypothalamus-pituitary-adrenal gland axis, resulting in Yang-Qi deficiency.8,35
In our study, Phlegm-Stasis syndrome was another significant constitution in breast cancer patients with a higher degree of fatigue and was associated with prolonged disease. According to TCM, Phlegm-Stasis syndrome is formed by phlegm turbidity or blood stasis in the body due to qi transport being impeded by external or environmental stimuli.20,36 It is characterized by numbness, pain, lack of appetite, nausea, vomiting, heavy body weight, and a purple tongue with a thick and greasy coating. An epidemiological study has revealed that Phlegm-Stasis is one of the prominent constitutions in patients with cancer, especially in those with liver, lung, and pancreatic cancer.37 Phlegm-Stasis is the main environment of cancer pathogenesis and has a strong statistical correlation with tumor metastasis.38,39 However, our results indicated only that the Phlegm-Stasis syndrome might be significantly associated with CRF if it is analyzed in a separate model. It is possible that these patients had Yang-Qi deficiency that was significantly correlated to fatigue scores, and that the BCQ score of Phlegm-Stasis increased after several months of cancer treatments. Further research is needed to explore this issue.
According to our clinical experience, the majority of patients have mixed TCM patterns. Our study found that nearly half of the breast cancer patients had mixed types. “Mixed type” is a term indicating that a patient displays a combination of two or three types of body constitutions and does not indicate greater severity of symptoms.24 In our Table 2 analysis, no significant difference between severity of fatigue and mixed type was found. However, some important issues deserve mentioning. We only emphasized that fatigue is the key point of Yang-Qi deficiency, and fatigue symptoms worsen with time in cancer patients. More complex factors, including age, nutrition, comorbid conditions (e.g., pain, anemia, diabetes, and hypothyroidism), and psychological and behavioral status, accompanied by cancer and/or its therapy, may influence the development of TCM patterns in CRF.8,9 Therefore, a diverse range of TCM treatment approaches, including nourishment of Yin and Xue, adjustment of abnormal sleep and emotion, and removal of heat, dampness, phlegm, or stasis pathogens, have been considered to address CRF during cancer treatment.35
Research on evidence-based medicine of TCM is greatly limited, mainly because TCM is to a certain extent empirical medicine, and many researchers lack objective and unified evaluation methods. Although TCM theory and practice indicate that a positive therapeutic response is dependent on proper syndrome differentiation,40 most of the classification or evaluation tools in use were designed on the basis of TCM doctors’ personal experiences, medical literature, or discussions among experts.24 The criteria applied in such evaluation tools are easily affected by a doctor’s educational background, the practice area, and the characteristics of his patients. The evolution of national standards for conveniently typing, or a more suitable instrument for use in guiding the treatment approach by TCM doctors during disease consultation, is an ongoing process with no end predicted in the near future.
The limitations of the present study were related to the cross-sectional study design. First, the study was conducted in a single medical center; therefore, the findings cannot be generalized. Second, we were unable to determine a definite relationship for TCM patterns and CRF. Additionally, it seems that weakness and other fatigue-related feelings are included in the classification of Yang-Qi deficiency. It is also possible that Yang-Qi deficiency is partially a description of chronic fatigue, which will make itself a confounder. Finally, these data are only applicable to inpatient settings and to patients requiring hours of continuous observation and drug administration. Limited data are available on targeted therapy, radiotherapy, and hormone therapy, which are usually performed at outpatient clinics. Further longitudinal studies should be conducted to clarify this issue.
5. Conclusion
These data draw to the attention of clinicians and clinical trialists the possibility that Yang-Qi deficiency could be associated with clinically meaningful fatigue in breast cancer patients undergoing chemotherapy. The relation of Phlegm-Stasis syndrome to the development of disease over time during treatment will need to be considered. The findings from our study may contribute to a better understanding of the potential of TCM patterns for supplementing modern therapeutic strategies for breast cancer. More studies are needed to determine whether treatment of both types of constitution effectively resolves fatigue in cancer patients.
Authors’ contributions
S.M. Deng and A.F. Chiu were responsible for the conception and design of the study and drafted the manuscript. S.M. Deng collected, analyzed, and interpreted the data. Y.C. Huang and S.Y. Chen assisted with the data analysis and interpretation of the data. S.C. Wu and S.C. Huang recruited the patients and participated in the study design. M.Y. Tsai conceived of the study, participated in the study design, supervised the study, and finalized the manuscript. S.M. Deng and A.F. Chiu contributed equally to this work and should be considered co-first authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have declared that no competing interests exist.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was supported by the Taiwan Ministry of Health and Welfare (MOHW107-CMAP-M-114-122111), and funded by Chang Gung Memorial Hospital with grant number CMRPG-8I038-1 & −0382. We thank all our colleagues from the breast surgery, oncology, and CM wards of Kaohsiung Chang Gung Memorial Hospital for their enthusiastic help in this work. We also thank Miss Hsiang-Yu Wang (UD Misi), Department of Visual Communication Design, Shu-Te University, for assisting with the procedure of patients’ enrollment and drawing a figure.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtcme.2020.08.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Network N.C.C. Cancer-related fatigue (version 2.2018) 2018. https://www.nccn.org/ [DOI] [PMC free article] [PubMed]
- 2.McFarland D.C., Shaffer K.M., Tiersten A., Holland J. Prevalence of physical problems detected by the distress thermometer and problem list in patients with breast cancer. Psycho Oncol. 2018;27(5):1394–1403. doi: 10.1002/pon.4631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stan D., Loprinzi C.L., Ruddy K.J. Breast cancer survivorship issues. Hematol/Oncol Clin. 2013;27(4):805–827. doi: 10.1016/j.hoc.2013.05.005. ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abraham J.E., Hiller L., Dorling L. A nested cohort study of 6,248 early breast cancer patients treated in neoadjuvant and adjuvant chemotherapy trials investigating the prognostic value of chemotherapy-related toxicities. BMC Med. 2015;13(1):306. doi: 10.1186/s12916-015-0547-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt M.E., Chang-Claude J., Seibold P. Determinants of long-term fatigue in breast cancer survivors: results of a prospective patient cohort study. Psycho Oncol. 2015;24(1):40–46. doi: 10.1002/pon.3581. [DOI] [PubMed] [Google Scholar]
- 6.Wang S.H., He G.P., Jiang P.L. Relationship between cancer-related fatigue and personality in patients with breast cancer after chemotherapy. Psycho Oncol. 2013;22(10):2386–2390. doi: 10.1002/pon.3303. [DOI] [PubMed] [Google Scholar]
- 7.Quinten C., Maringwa J., Gotay C.C. Patient self-reports of symptoms and clinician ratings as predictors of overall cancer survival. J Natl Cancer Inst. 2011;103(24):1851–1858. doi: 10.1093/jnci/djr485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bower J.E. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11(10):597–609. doi: 10.1038/nrclinonc.2014.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howell D., Keller-Olaman S., Oliver T.K. A pan-Canadian practice guideline and algorithm: screening, assessment, and supportive care of adults with cancer-related fatigue. Curr Oncol. 2013;20(3):e233–246. doi: 10.3747/co.20.1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sood A., Moynihan T.J. Cancer-related fatigue: an update. Curr Oncol Rep. 2005;7(4):277–282. doi: 10.1007/s11912-005-0051-8. [DOI] [PubMed] [Google Scholar]
- 11.Xu Y., Chen Y., Li P., Wang X.S. Ren Shen Yangrong Tang for fatigue in cancer survivors: a phase I/II open-label study. J Alternative Compl Med. 2015;21(5):281–287. doi: 10.1089/acm.2014.0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouyang M., Liu Y., Tan W. Bu-zhong-yi-qi pill alleviate the chemotherapy-related fatigue in 4 T1 murine breast cancer model. BMC Compl Alternative Med. 2014;14:497. doi: 10.1186/1472-6882-14-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng C.S., Chen L.Y., Ning Z.Y. Acupuncture for cancer-related fatigue in lung cancer patients: a randomized, double blind, placebo-controlled pilot trial. Support Care Canc. 2017;25(12):3807–3814. doi: 10.1007/s00520-017-3812-7. [DOI] [PubMed] [Google Scholar]
- 14.Mao H., Mao J.J., Guo M. Effects of infrared laser moxibustion on cancer-related fatigue: a randomized, double-blind, placebo-controlled trial. Cancer. 2016;122(23):3667–3672. doi: 10.1002/cncr.30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larkey L.K., Roe D.J., Smith L., Millstine D. Exploratory outcome assessment of Qigong/Tai Chi Easy on breast cancer survivors. Compl Ther Med. 2016;29:196–203. doi: 10.1016/j.ctim.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin Y.-H., Chiu J.-H. Use of Chinese medicine by women with breast cancer: a nationwide cross-sectional study in Taiwan. Compl Ther Med. 2011;19(3):137–143. doi: 10.1016/j.ctim.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Guo Q., Li J., Lin H. Effect and molecular mechanisms of traditional Chinese medicine on regulating tumor immunosuppressive microenvironment. BioMed Res Int. 2015;2015:261620. doi: 10.1155/2015/261620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Templeton A.J., Thurlimann B., Baumann M. Cross-sectional study of self-reported physical activity, eating habits and use of complementary medicine in breast cancer survivors. BMC Canc. 2013;13:153. doi: 10.1186/1471-2407-13-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konkimalla V.B., Efferth T. Evidence-based Chinese medicine for cancer therapy. J Ethnopharmacol. 2008;116(2):207–210. doi: 10.1016/j.jep.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Lin J.-D., Lin J.-S., Chen L.-L., Chang C.-H., Huang Y.-C., Su Y.-C. BCQs: a body constitution questionnaire to assess stasis in traditional Chinese medicine. Euro J Integrative Med. 2012;4(4):e379–e391. [Google Scholar]
- 21.Zhang H.J., Wang Z.X. Yin-yang, Zheng: exported from Chinese medicine. Chin J Integr Med. 2014;20(4):250–255. doi: 10.1007/s11655-014-1777-z. [DOI] [PubMed] [Google Scholar]
- 22.Jeong J.S., Ryu B.H., Kim J.S., Park J.W., Choi W.C., Yoon S.W. Bojungikki-tang for cancer-related fatigue: a pilot randomized clinical trial. Integr Canc Ther. 2010;9(4):331–338. doi: 10.1177/1534735410383170. [DOI] [PubMed] [Google Scholar]
- 23.Chen L.L., Lin J.D., Huang Y.C., Lin J.S., Huang C.H., Su Y.C. Scale descriptor selection for a Taiwan-version of a body constitution questionnaire in traditional Chinese medicine. Mid-Taiwan J Med. 2008;13(1):35–42. [Google Scholar]
- 24.Chen L.L., Lin J.S., Lin J.D. BCQ+: a body constitution questionnaire to assess Yang-Xu. Part II: evaluation of reliability and validity. Forsch Komplementmed. 2009;16(1):20–27. doi: 10.1159/000197770. [DOI] [PubMed] [Google Scholar]
- 25.Lin C.C., Chang A.P., Chen M.L., Cleeland C.S., Mendoza T.R., Wang X.S. Validation of the Taiwanese version of the Brief fatigue inventory. J Pain Symptom Manag. 2006;32(1):52–59. doi: 10.1016/j.jpainsymman.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 26.Tian L., Lin L., Li H.L. Prevalence and associated factors of cancer-related fatigue among cancer patients in eastern China. Oncol. 2016;21(11):1349–1354. doi: 10.1634/theoncologist.2015-0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hwang S.S., Chang V.T., Cogswell J., Kasimis B.S. Clinical relevance of fatigue levels in cancer patients at a Veterans administration medical center. Cancer. 2002;94(9):2481–2489. doi: 10.1002/cncr.10507. [DOI] [PubMed] [Google Scholar]
- 28.Dittner A.J., Wessely S.C., Brown R.G. The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res. 2004;56(2):157–170. doi: 10.1016/S0022-3999(03)00371-4. [DOI] [PubMed] [Google Scholar]
- 29.Donovan K.A., Jacobsen P.B., Small B.J., Munster P.N., Andrykowski M.A. Identifying clinically meaningful fatigue with the fatigue symptom inventory. J Pain Symptom Manag. 2008;36(5):480–487. doi: 10.1016/j.jpainsymman.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yao W., Yang H., Ding G. Mechanisms of Qi-blood circulation and Qi deficiency syndrome in view of blood and interstitial fluid circulation. J Tradit Chin Med. 2013;33(4):538–544. doi: 10.1016/s0254-6272(13)60162-4. [DOI] [PubMed] [Google Scholar]
- 31.Hsu C.H., Lee C.J., Chien T.J. The relationship between Qi deficiency, cancer-related fatigue and quality of life in cancer patients. J Tradit Chin Med. 2012;2(2):129–135. doi: 10.1016/s2225-4110(16)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chien T.J., Song Y.L., Lin C.P., Hsu C.H. The correlation of traditional Chinese medicine deficiency syndromes, cancer related fatigue, and quality of life in breast cancer patients. J Tradit Chin Med. 2012;2(3):204–210. doi: 10.1016/s2225-4110(16)30101-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang S.M., Chien L.Y., Tai C.J., Chen P.H., Lien P.J., Tai C.J. Effects of symptoms and complementary and alternative medicine use on the yang deficiency pattern among breast cancer patients receiving chemotherapy. Compl Ther Med. 2015;23(2):233–241. doi: 10.1016/j.ctim.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Leong P.K., Wong H.S., Chen J., Ko K.M. Yang/Qi invigoration: an herbal therapy for chronic fatigue syndrome with yang deficiency? Evid Based Complement Alternat Med. 2015;2015:945901. doi: 10.1155/2015/945901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen R., Moriya J., Yamakawa J., Takahashi T., Kanda T. Traditional Chinese medicine for chronic fatigue syndrome. Evid Based Complement Alternat Med. 2010;7(1):3–10. doi: 10.1093/ecam/nen017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rena J.-X., Chang D., Liu J.-X. Pathophysiological characteristics of phlegm-stasis cementation syndrome in coronary heart disease: a review and update. World J Tradit Chin Med. 2015;1(4):38–41. [Google Scholar]
- 37.Chen B., Li M.Y., Liu P.D., Guo Y., Chen Z.L. Alternative medicine: an update on cupping therapy. QJM. 2015;108(7):523–525. doi: 10.1093/qjmed/hcu227. [DOI] [PubMed] [Google Scholar]
- 38.Yh L., Yw Z., Gg L., Kq Y. Experimental and clinical study on tumor metastasis and microscopic blood stasis. 1996;4(33):224–228. Xian Dai Zhong Yi. [Google Scholar]
- 39.Liu S., Hua Y.Q., Sun Z.P., Tan S., Lu D.M. Breast cancer pathogenesis of stagnation of phlegm, poison and blood stasis: rationale and clinical application in traditional Chinese medicine. Zhong Xi Yi Jie He Xue Bao. 2007;5(2):122–125. doi: 10.3736/jcim20070203. [DOI] [PubMed] [Google Scholar]
- 40.Liu C.T., Chen Y.H., Huang Y.C., Chen S.Y., Tsai M.Y. Chemotherapy in conjunction with traditional Chinese medicine for survival of patients with early female breast cancer: protocol for a non-randomized, single center prospective cohort study. Trials. 2019;20(1):741. doi: 10.1186/s13063-019-3848-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.