Abstract
Background and aim
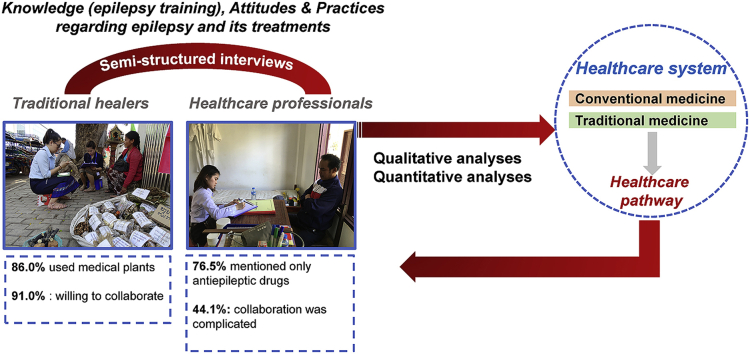
Traditional practices are deeply rooted in Lao people’s perceptions and beliefs about health and illness.
The objective of the study was to understand the perceptions of healthcare professionals and traditional healers regarding the management of epilepsy in Laos, and their reciprocal views.
Experimental procedure
An observational study was carried out in two areas of Laos from February to May 2017. Semi directive questionnaires were used to collect quantitative and qualitative data. Semiotic square was carried out to highlight relationships between attitudes of traditional healers and healthcare professionals. For quantitative approach, the proportions were reported, and the test used was Fisher’s test for nominal variables. The mean and standard deviation expressed the continuous variables and the Student’s t-test was used.
Results and conclusion
Epilepsy was cited by 90.9% of traditional healers as a convulsive disease with saliva or urine, and herbal medicines were predominantly used (86.4%) to treat it. Few healthcare professionals (26.5%) pointed out that they knew remedies to treat epilepsy other than antiepileptic drugs (AEDs), and 76.5% of healthcare professionals mentioned that epilepsy was a disease which only AEDs could treat. On the other hand, 54.5% of traditional healers confirmed a traditional remedy could cure completely epilepsy through long-term use. Ninety percent of traditional healers said the collaboration with healthcare professionals was a good idea and 44.1% of the healthcare professionals group said was complicated.
The combination of these medicines for the management of epilepsy needs to be adapted to Lao’s medical context.
Keywords: Epilepsy, Traditional medicine, Conventional medicine, Traditional healer, Treatment gap
Graphical abstract
Highlights of the findings and novelties
-
•
Understanding the perceptions and reciprocal views of care providers.
-
•
Study the combination of traditional and conventional medicine for epilepsy.
-
•
Public health policies: integration of traditional medicine in the care of patients.
List of abbreviations
- AEDs
antiepileptic drugs
- CAM
complementary and alternative medicine
- DHeVeLoP
Domestic Health Visitors for improving access to care for people with epilepsy in Lao PDR
- Lao APE
Lao Association for Patients living with Epilepsy
- Lao PDR
Lao People’s Democratic Republic
- PWEs
people living with epilepsy
1. Introduction
Epilepsy is a chronic brain disorder that affects about 70 million people worldwide.1 Epilepsy affects about 1% of the population in Southeast Asia region; thus, there are approximately 15 million people with epilepsy in the region. Only 10–20% of all people living with epilepsy (PWEs) receive appropriate treatment; communities in Southeast Asia continue to believe in many myths and misconceptions about epilepsy.2 In Eastern and South Eastern Asian languages, such as Chinese, Japanese, Korean, Malay, Lao, Thai, Burmese, and Khmer (Cambodia) epilepsy is associated with madness.3 In many cultures, including in Africa and Asia, people with epilepsy (PWEs) are viewed with hostility and denied access to medical and social care. PWEs are excluded from society: exposed to social and religious taboos, isolated, sometimes with no right to have children or marry,4 are excluded from jobs, and are not allowed to have contact or to share meals with other people.5
Epilepsy is a controllable disease in the majority of PWEs. The goal of treatment is to maintain a healthy lifestyle, ideally by complete seizure control with no or minimal side effects. Antiepileptic drugs (AEDs) are the main treatment,6 and are the usual first line step in the management of epilepsy for the majority of PWEs.7 In Asian countries, the treatment gap is 64.0%,8 and higher in rural areas than in urban areas, particularly because of a lack of knowledge on epilepsy and the low availability of AEDs.9
In developing countries, traditional healthcare systems compete or complement conventional medicine.10 Faith healers have strong social and religious connections; they also play an essential role in the management of epilepsy in some countries. Especially in communities in Southeast Asia, where PWEs are sometimes more likely to consult traditional healers than conventional doctors.2
Despite a lack of national policy program on epilepsy in Laos, recent research studies in collaboration with several centers provided an overview of the state of knowledge.11 The overall prevalence of epilepsy was 7.7 cases per thousand inhabitants in 2006.12 The treatment gap was 90% or more, the low level of knowledge of epilepsy on the part of health workers may be contributing to the wide treatment gap in Laos.12 A low availability of AEDs throughout the country was reported with an annual importation of phenobarbital allowing to treat around 2% of PWEs and a price of annual treatment 4- to 10-fold higher than the international price.13 Only a mean of one PWE per month per hospital is being cared in Lao hospitals.11 PWEs face many challenges to get access to appropriate healthcare: a study in 2013 showed that PWEs combined conventional and traditional medicines treatments.14 Traditional practices are deeply rooted in Lao people’s perceptions and beliefs about health and illness. The use of traditional medicine has recently become more popular and accessible, and in response, the Ministry of Health has launched a policy in support of integrating traditional medicine with Western medicine. The Centre for Research on Medicinal Plants and Traditional Medicine was upgraded to a national institute in 2009. In 2014, the Food and Drug Department provided a census of traditional medicines but guidelines for the safe use have not yet been formulated. The first national traditional medicine policy and strategy are under discussion.15
Our study aimed to understand the perceptions of healthcare professionals and traditional healers regarding the management of epilepsy in Laos, and their reciprocal views on traditional and conventional medicines, in order to improve the management of epilepsy.
2. Method
2.1. Study area
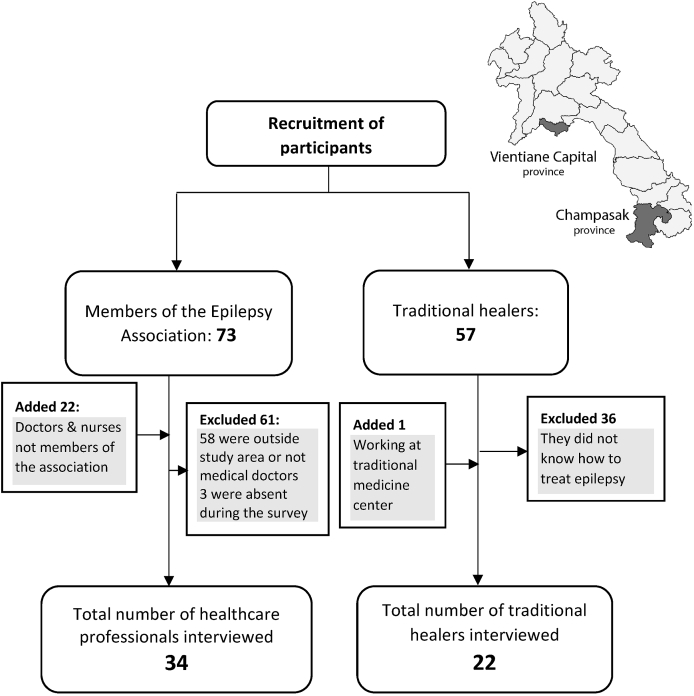
An observational descriptive study was carried out from February to May 2017 by using semi directive questionnaires. The selection procedure of participants was concentrated in 2 areas of Laos. First, in Vientiane Capital (Fig. 1), a well-known area included in the Domestic Health Visitors for improving access to care for people with epilepsy in Laos (DHeVeLoP project 2014–2016).16 Most of participants were the members of the Lao Association for Patients with Epilepsy (APE), and lived in the capital. The APE was established in 2011 with four main activities: organizing scientific conferences on epilepsy, providing three days training on epilepsy to health personal at both provincial and district levels, supporting the provision of antiepileptic drugs through a revolving drug fund at provincial and district hospitals, and promoting the dissemination of information on epilepsy to the public.15 There are also market trade centers for traditional medicine (sellers of medicinal plants). The second area was Champasak Province, which located in the South of Laos, it is about 700 kms away from Vientiane Capital (Fig. 1). This province has a strong cultural and religious environment, the largest number of traditional healers, and there is a Traditional Medicine Centre site in the Provincial Hospital.
Fig. 1.
Flow chart of healthcare professionals & traditional healers interviewed and localization of study areas in Lao PDR.
2.2. Participants
2.2.1. Healthcare professionals
The participants in the conventional group were selected from the list of healthcare professionals from the Lao Association for Patient with Epilepsy.17
We performed an exhaustive sampling: all healthcare professionals (nurses and general practitioners) of the list from the association for people living with epilepsy that have been found in both study areas (Vientiane Capital and Champasak Province) were included. Then, we also automatically included health personnel in the neurology and mental health services who provided epilepsy treatment although they were not a member of the association.
2.2.2. Traditional healers
With the assistance of the Provincial and District Health Units, and especially the Provincial Hospital Traditional Medicine Centre, as well as through the herbal market, we were able to identify traditional healers. In addition, a snowball sampling technique was used, allowing recruiting traditional healers who were familiar and lived in the same villages as PWEs.
All participants had to know at least one traditional remedy for treating epilepsy. We included all types of traditional medicine players (traditional healers and sellers of medicinal plants). They had to be present at the time of our survey and willing to participate.
2.3. Semi-structured interviews
We organized individual interviews using two semi-structured questionnaires and interview guides, one for healthcare professionals and one for traditional healers. The questionnaire for healthcare professionals consisted of four sections: sociodemographics, knowledge (epilepsy training), attitudes and practices regarding epilepsy and its treatments. It included seven questions in total, two closed questions, and five open-ended questions. The questionnaire for traditional healers consisted of five sections: sociodemographic data, experience with conventional medicine, knowledge, attitudes, and practices regarding epilepsy and its treatments. There were in total eight open-ended questions to allow a good free expression on these topics.
Questionnaires were initially developed in English with the agreement of the research team, and then they were translated in Lao language. The Lao questionnaires were field tested in Vientiane capital with 10 participants prior to conducting field work.
Before starting the interview, the researcher explained in detail the topic and the objective of the discussion. All individual interviews were conducted by the first author (bilingual, native of Laos) at the residence of participant from the traditional healers’ group. For the conventional group, they could choose the place where it was most convenient for them. The researcher allowed participants to share their opinions without influencing the answers. If necessary, more specific questions were then asked. We worked closely with local healthcare professionals (who acted as mediators) for better communicating and comprehensive of a local term, so the participants would be able to provide rich information. Each individual interview would take a minimum of 50 min; interviews were recorded after seeking authorization from the participants. Interviews recorded in Lao were then translated in English.
2.4. Ethical considerations
Written consent was systematically obtained before the interviews. Our study was authorized by the Lao National County of Ethics for Health Research (No 032/NIOPH/NECHE and No044/NECHR) and the Ministry of Health, Laos (Agreement No 0397 dated 04/03/2016).
2.5. Data analysis
Our main objective was focused on understanding the perceptions of traditional healers and healthcare professionals on epilepsy management by using two different analytical approaches.
2.5.1. Qualitative analyses
Thirteen open-ended questions, reverse translations, and transcriptions were carried out by the bilingual interviewer, a native of Laos (1st author). We used the thematic analysis methodology, first identifying key themes within data, and encoding before interpretation. The lexical analysis was based on semantic occurrences, which allowed coding (in qualitative value) according to the most frequently cited modalities and was presented by a proportion. The validity of the coding was based on the consensual coding of two researchers (1st and 2nd author). When differences emerged, a consensus was sought with a third researcher. These questions were then analyzed as closed multiple-choice questions by proportion analysis.
We used semiotic square in order to highlight relationships between attitudes of traditional healers and healthcare professionals through the negative and positive answers.
2.5.2. Quantitative analyses
Transcriptions and coding of the lexical segments of interest were carried out using the functionalities of the Word software; then the coded data were stored in Microsoft Excel. The statistical analyses were performed using STATA 13 software. For dichotomous and closed-ended questions, the proportions were reported, and the tests used were Chi2 or Fisher’s test. Their mean and standard deviation expressed the quantitative variables, and the Student’s t-test was used. The significance threshold for all analyses was set at 0.05.
3. Results
3.1. Sociodemographic data
Fifty-six participants were interviewed: 34 healthcare professionals and 22 traditional healers (Fig. 1). Women represented 61.8% in the group of healthcare professionals in contrast with the traditional healers’ group, where the male population was predominant (95.5%); the difference between two groups was significant (p < 0.0001). The participants were mostly Buddhists (98.2%) and in the traditional healers’ group, they were significantly older than in the conventional group (p < 0.0001). Only one traditional healer (4.6%) had completed a university degree compared to 100% of subject in the healthcare professionals’ group (p < 0.0001) (Table 1).
Table 1.
Sociodemographic characteristics of participants interviewed.
| Overall N = 56 | Healthcare professionals N = 34 | Traditional healers N = 22 | P value | |
|---|---|---|---|---|
| Sex | ||||
| Male | 34 (60.7%) | 13 (38.2%) | 21 (95.5%) | <0.0001a |
| Female | 22 (39.3%) | 21 (61.8%) | 1 (4.6%) | |
| Mean age ± SD (Min-Max) | 50.4 ± 13.9 (24–80) | 43.1 ± 9.1 (24–61) | 61.8 ± 12.3 (34–80) | <0.0001b |
| Religion | ||||
| Buddhism | 55 (98.2%) | 34 (100.0%) | 21 (95.5%) | 0.393a |
| Animism | 1 (1.8%) | 0 | 1 (4.6%) | |
| Education level | ||||
| Special education system | 2 (3.6%) | 0 | 2 (9.1%) | <0.0001a |
| Primary school | 10 (17.9%) | 0 | 10 (45.5%) | |
| Secondary and higher | 9 (16.1%) | 0 | 9 (40.9%) | |
| University degree | 35 (62.5%) | 34 (100.0%) | 1 (4.6%) | |
| Family status | ||||
| Single | 5 (8.9%) | 5 (14.7%) | 0 | 0.145a |
| Married | 51 (91.1%) | 29 (85.3%) | 22 (100.0%) | |
= fisher’s exact test, b = student’s T-Test.
3.2. Knowledge and practice of traditional healers on epilepsy
Epilepsy was cited by 91% of traditional healers as a convulsive disease with saliva or urine, followed by a neurological disease (41%). The perception of a supernatural disease was not found in the participants of the survey. Fifty-four percent had learned about traditional medicine from their family and they stated this practice was a Lao folk custom. When we questioned if the participant knew another remedy to treat epilepsy beside a traditional remedy, about 41% mentioned biomedical medicine as a treatment for epilepsy. Forty-one percent had no restriction if patient would like to combine antiepileptic drugs with traditional remedy.
3.3. Epilepsy remedy of traditional healers
Herbal medicines were predominantly used by traditional healers (86.4%) and 31.8% of them used bone or teeth from animals. The participant explained the reason of using traditional remedies by a familiarity and a tradition behavior (54.5%). Food restrictions were mentioned for PWEs being treated with traditional medicine (68.2%). For some traditional healers, the only advice given to PWEs was to be careful about epileptic seizures (31.2%). Regarding the combination of traditional and biomedical treatments, 45.5% of traditional healers said it was the patient’s decision. Forty-one percent stated that patients could combine a traditional remedy with AEDs with no restriction (Table 2).
Table 2.
Knowledge and practices towards epilepsy of traditional healers.
| Traditional healers N = 22 | |
|---|---|
| Knowledge on epilepsy and epilepsy remedy | |
| What is epilepsy, also called mad pig disease?(multiple answers) | |
| Convulsive disease with saliva/urine | 20 (90.9%) |
| Neurological disease | 9 (40.9%) |
| Disease of the blood system | 7 (31.8%) |
| Disease of nerve fibers/tendons | 6 (27.3%) |
| Hereditary disease | 6 (27.3%) |
| Do you know epilepsy remedies other than your epilepsy treatment methods? | |
| Yes | 11 (50.0%) |
| Biomedical medicine | 9 (40.9%) |
| Acupuncture | 2 (9.1%) |
| No | 11 (50.0%) |
| How did you learn about traditional medicine?(multiple answers) | |
| Family knowledge | 12 (54.5%) |
| Learned at the temple (learned with a monk) | 4 (18.2%) |
| Learned by ancient traditional healer | 3 (13.6%) |
| The only one remedy access to care in rural area | 3 (13.7%) |
| Have been chosen by a spirit to become a healer | 3 (13.7%) |
| Practices on epilepsy | |
| Which methods do you use to treat epilepsy?(multiple answers) | |
| Herbal medicines | 19 (86.4%) |
| Animals (bone, teeth) | 7 (31.8%) |
| Other | 4 (18.2%) |
| Why do you use traditional remedy?(multiple answers) | |
| This is a tradition/these traditions exist in Lao folk custom | 12 (54.5%) |
| Generation-to-generation knowledge | 8 (36.4%) |
| Fewest side effects | 7 (31.8%) |
| Restrictions?Yes | |
| Food diet | 15 (68.2%) |
| No restrictions, just advise him to be careful about the seizures | 7 (31.2%) |
| Drinking alcohol | 4 (18.2%) |
| Advice for PWEs who want to use antiepileptic drugs | |
| Patient’s preference | 10 (45.5%) |
| In association with no restriction | 9 (40.9%) |
| One after the other | 3 (13.6%) |
3.4. Attitudes of healthcare professionals on epilepsy care pathway
Thirty-four healthcare professionals were interviewed about their opinion on epilepsy management in Laos (Table 3). Only 21% reported that they received initial training in epilepsy as part of their medical curriculum. Sixty one percent mentioned that continuous training had improved their knowledge on epilepsy and 50% stated they had the capacity to diagnose and prescribe antiepileptic drugs (AEDs).
Table 3.
Opinion of healthcare professionals on epilepsy care.
| Healthcare professionals (N = 34) |
||
|---|---|---|
| Opinion on the epilepsy care system in Laos | ||
| Positive attitude | Continuous training enabling to increase knowledge | 21 (61.8%) |
| Capacity of diagnosis & prescription of AEDs | 17 (50.0%) | |
| Improvement of the patient’s quality of life | 8 (23.5%) | |
| Negative attitude | Difficulty of AEDs management and accessibility | 19 (55.9%) |
| Misunderstanding of patients and their families about epilepsy | 13 (38.2%) | |
| Poor knowledge of the medical staff | 8 (23.5%) | |
| Complexity of doctor-patient coordination | 5 (14.7%) | |
| Do you know any other remedy to treat epilepsy? | ||
| Yes (multiple answer) | 9 (26.5%) | |
| Traditional ceremony | 7 (20.6%) | |
| Herbal medicines | 4 (11.8%) | |
| Surgery | 1 (2.9%) | |
| No | 25 (67.6%) | |
| Advice for PWEs who want to use herbal medicine | ||
| Only AEDs, other remedies are not effective | 14 (41.2%) | |
| In association | 13 (38.2%) | |
| Patient’s preference | 7 (20.6%) | |
Very few participants pointed out that they knew treatments other than AEDs (26.5%): among those who knew, 20.6% mentioned traditional ceremonies and 11.5% herbal medicines, only one healthcare professional mentioned surgery. Otherwise, 41.2% of participants stated that only AEDs could treat epilepsy, and that traditional remedies or herbal medicine were ineffective. Anyhow, if PWEs would like to combine, they could (38.2%).
3.5. Conventional doctor and traditional healers’ attitudes on epilepsy treatment
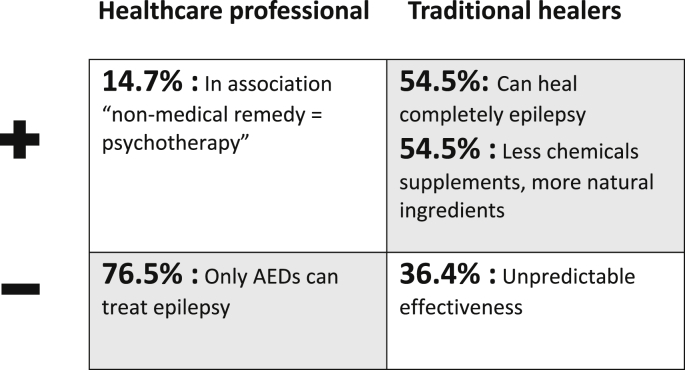
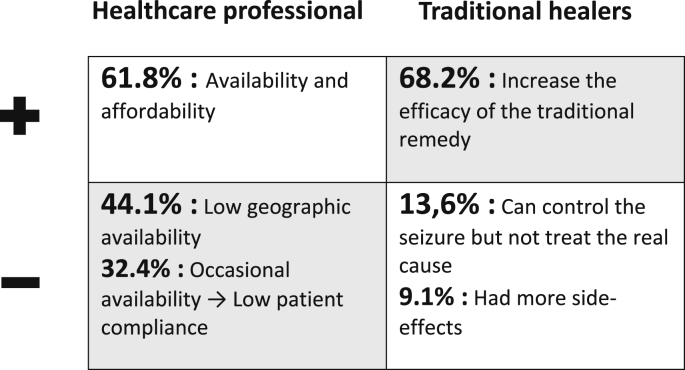
We synthesized participants’ attitudes according to semiotic squares in Fig. 2B, Fig. 2A(A and B). Regarding the opinions on AEDs, the figures were categorized in more positive and more negative attitudes for better understanding. In the conventional group, 61.8% mentioned that AEDs were available and affordable, but some of them (44.1%) stated AEDs geographical availability could be limited, potentially leading to low adherence to treatment for PWEs (32.4%). For the traditional healers’ group, AEDs were considered by 68.2% of participants to increase the pharmacological effect of traditional remedies. Although, 13.6% of participants thought AEDs were used to control the epileptic seizures, not to treat epilepsy cause.
Fig. 2B.
Opinion on traditional method for epilepsy treatment.
Fig. 2A.
Opinion on antiepileptic drugs (AEDs) for epilepsy treatment.
The second question was focused on the perception regarding traditional remedies. Participants in the conventional group had more negative attitudes on traditional medicine: 76.5% mentioned that epilepsy was a neurological disease which only AEDs could treat. Only 14.7% said it could be combined with AEDs as traditional medicine was about providing psychosocial support to PWEs. In the traditional healers’ group, traditional medicine was considered as more natural (organic means) and moreover, it could cure completely epilepsy when used over the long-term (54.5%). Thirty-six percent of traditional healers stated that the effectiveness of traditional remedies was unpredictable. For the collaboration between conventional and traditional medicine, 90.9% of traditional healers said it was a good idea. In contrast, with the conventional group in which 44.1% stating, it was complicated.
4. Discussion
4.1. Conventional and traditional medicine for epilepsy management
Traditional medicine remains an important part of the health care system, particularly in Asian and African countries.18, 19, 20 Traditional healers showed a positive attitude regarding the collaboration with healthcare professionals for epilepsy treatment. Most of them said the cooperation was an excellent approach but only 13.0% of traditional healers recommend PWEs taking a traditional remedy and an AED at the same time. A study in Burkina Faso demonstrated that most healers (more than 90.0%) wished to be integrated into the modern healthcare system and considered that both kinds of treatments were complementary.21 A study conducted in Cape Town in 2015 showed that traditional healers were supportive of collaboration with western-trained practitioners.22 Conversely, the study in Ivory Coast highlighted that traditional healers would recommend the sudden discontinuation of modern medicines in preference to traditional treatment, this attitude reflecting their relative ignorance about modern treatments.23 In our study, almost half healthcare professionals thought that collaboration with traditional healers was complicated and only thirty-eight percent stated it was good. We noticed that they were likely to not recommend complementary treatment, unlike patients in Peru, in which it was showed the traditional medicine has been chosen by PWEs instead of conventional treatment (p = 0.024).24
It is interesting to discuss why they had a different perspective, especially because our study shows a contradictory perception between the two groups. First, if we consider sex and age, we observed that the participants’ traditional groups were significantly older than those of the conventional group. Older adults perceive pictures differently than younger adults; older adults focus more on positive affect.25 There was also a greater proportion of males in the group of traditional healers similar to the study in Burkina Faso by Abdullahi et al. (2011), regarding traditional healers’ knowledge and attitudes towards epilepsy, all traditional practitioners were male and most of them were above 50 years of age.21 In Lao context, men are considered culturally superior because of their ability to become monks. Men are generally recognized as the household head for religious and political purposes.26 Being a traditional healer in Laos means they have to respect many cultural rules, so it is not too different from being a religious leader.
4.2. Knowledge, attitudes and practices regarding on epilepsy care
Epilepsy was seen largely as a convulsive disease with saliva or urine flowing out by traditional healers. The perception that epilepsy has a supernatural origin was not found for traditional healers and healthcare professionals but was previously reached by PWE, their families and villagers.5 A study in Ivory Coast demonstrated that for more than 80.0% of traditional practitioners, epilepsy was a supernatural disease.23 Our results, and those of the study in Ivory Coast,23 suggest that herbal treatments are the main remedy used by traditional practitioners, 86.4% and 97.0% respectively. In Latin America, a study conducted in Peru showed the traditional healers were more frequently consulted than healthcare professionals for first-line antiepileptic treatment. More than 60.0% of PWEs and 80.0% of traditional healers, used herbal remedies in this survey, and supernatural etiologies were mentioned by 23.4% of PWEs.24 By contrast, in Malaysia in 2008, Razali et al. showed that 75.0% of epileptic patients used Holy water and only 12.5% herbal medicine.27
Awareness campaigns provided by healthcare system mentioned 38.2% of PWEs and their families had limited understanding about epilepsy and medicals staff in rural areas had poor knowledge on epilepsy (23.5%).28 More than half of healthcare professionals mentioned that continuous professional training could be applied to increase knowledge on epilepsy treatment and allowed them to have the ability to diagnose and prescribe antiepileptic drugs (AEDs). The professional training that they referred to was the activities of the program DHeVeLoP (2014–2016) and of the Lao Association for patients living with epilepsy (Lao APE).17 This suggested a positive outcome of the intervention activities compared to the previous study conducted in 2013 which indicated a low knowledge of epilepsy for healthcare workers in Laos.14 Two important changes in the management of epilepsy were made between the studies: the APE provided AEDs and the domestic health visitors were trained about the disease in the second study. A randomly selected health workers study conducted in 2009 reported only 2.5% of them recalled ever having received training on epilepsy and our study highlighted a poor knowledge of the medical staff for less than 25% of the healthcare professionals surveyed. The majority of the health workers (59.9%) were unaware of any available AEDs at the health facilities12 and 55.9% perceived difficulties of AEDs management and accessibility in the present study.
The availability of antiepileptic drugs (AEDs) seems to be a serious barrier to the management of epilepsy: participants in the conventional group mentioned that AEDs were available and affordable with some of them stating that their geographical availability across the country could be limited. Many studies in Laos already highlighted that AEDs had very low availability especially in rural areas.28,29 Traditional or herbal medicines were considered as ineffective (41.2%) but the study conducted in 2018 in Laos suggested that more than 50% of PWEs had already consulted a traditional practitioner to treat their epilepsy.30 Only thirty-eight percent agreed about the combination of conventional and traditional medicines based on patient’s needs.
4.3. Strengths and limitations
Our study was the first study in Laos conducted to understand the perceptions of healthcare professionals and traditional healers regarding epilepsy treatment. Exploratory research is effective in laying the foundation for future studies. All information collected was original data; individual interviews helped participants to discuss contentious issues in more depth, allowing flexibility, and adaptability to the local context.
A rather modest number of subjects in the samples, which may not adequately represent the target population, was surveyed. The identification of participants, especially traditional healers was not easy because not every Traditional Medicine Centre has a list of registered traditional healers resulting in a lower number of traditional healers answered in comparison with healthcare professionals. Thus our sample has a limited representativeness, which makes extrapolation of the results in the national context difficult. Additionally, it could have been interesting to interview traditional healers from the North of Laos who have different cultural background and medicine healthcare, influenced by Chinese traditional medicine.
Exploratory studies generate qualitative information and interpretation of such type of information is subject to biases. That is the reason why we combined qualitative and quantitative approaches: some qualitative answers were then categorized into quantitative variables (after consultation with several authors). Although it can lead to a loss of information from interviews, it has the benefit of allowing quantitative analyses.
The healthcare seeking behavior of mixing remedies has long been observed. It is time for healthcare professionals to be more willing to accept complementary and alternative remedies.
5. Implications for practice and conclusion
Most traditional healers said the collaboration with healthcare professionals was a good idea and nearly half of the healthcare professionals believed it would be complicated. Healthcare professionals reported than AEDs have a low compliance, mainly due to occasional availability. For them, traditional medicine could be used in association with AEDs as non-medical remedies and could play a psychotherapeutic role. Traditional healers mentioned that traditional medicine provides unpredictable effectiveness. Most of them indicated that AEDs will be interesting in order to increase the efficacy of the traditional remedy. For both groups of caregivers, it would be relevant to use the effects of traditional medicine coupled with those of AEDs.
Understanding the attitudes of the conventional doctor towards traditional medicine will be useful in implementing future integration of complementary and alternative medicine (CAM). The institutional recognition of traditional medicine, recommended by the WHO in its strategy 2014–2023, promote the safe and effective use of CAM through the regulation of products, practices, and practitioners. Healthcare professionals need to be aware of their presence and their role as a potential referral to healthcare, considering the holistic, humanitarian and individualized views of the traditional healer, and the interesting therapeutic and palliative effect of CAM in chronic diseases.
This study showed steps forward in epilepsy management in the Lao medical context. Further research on the combination of traditional and conventional medicine for epilepsy is required and will bring us closer to the patient. A better understanding of the care pathway will help reduce the treatment gap.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
We declare no competing interests. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtcme.2019.12.003.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Anthony K., Ngugi CB Immo Kleinschmidt. Sander Josemir W., Newton Charles R. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51(5):883–890. doi: 10.1111/j.1528-1167.2009.02481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epilepsy in the WHO South-East Asian Region: Bridging the Gap. The Global Campaign Against Epilepsy “Out of the Shadows.”; 2015. [Google Scholar]
- 3.Lim K.S., Li S.C., Casanova-Gutierrez J., Tan C.T. Name of epilepsy, does it matter? Neurol Asia. 2012;17(2):87–91. [Google Scholar]
- 4.Moselhy H.F. 2011. Psychosocial and Cultural Aspects of Epilepsy; pp. 1–11. [Google Scholar]
- 5.Tran D.S., Odermatt P., Singphuoangphet S. Epilepsy in Laos: knowledge, attitudes, and practices in the community. Epilepsy Behav. June 2007;10(4):565–570. doi: 10.1016/j.yebeh.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Prilipko L., Saxena S., Boer H. vol. 129. Programme for Neurological Diseases and Neuroscience Department of Mental Health and Substance Abuse World Health Organization Geneva; 2005. http://books.google.com/books?id=ZJfku__6BKMC&pgis=1 (Atlas : Epilepsy Care in the World). [Google Scholar]
- 7.Glauser T, Ben-Menachem E, Bourgeois B, et al ILAE treatment guidelines: evidence-based analysis of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 47(7):1094-1120.. [DOI] [PubMed]
- 8.Trinka E, Kwan P, Lee B, Dash A. Epilepsy in Asia: disease burden, management barriers, and challenges. Epilepsia.:1-15.. [DOI] [PubMed]
- 9.Mac T.L., Tran D.S., Quet F., Odermatt P., Preux P.M., Tan C.T. Epidemiology, aetiology, and clinical management of epilepsy in Asia: a systematic review. Lancet Neurol. 2007;6(6):533–543. doi: 10.1016/S1474-4422(07)70127-8. [DOI] [PubMed] [Google Scholar]
- 10.Danesi M.A., Adetunji J.B. Use of alternative medicine by patients with epilepsy - a survey of 265 epileptic patients in a developing-country. Epilepsia. 1994;35(2):344–351. doi: 10.1111/j.1528-1157.1994.tb02442.x. [DOI] [PubMed] [Google Scholar]
- 11.Barennes H., Souvong V., Chivorakoun P., Preux P.M., Odermatt P. Epilepsy: A Global Approach. 2017. The challenge of epilepsy in low-income countries insights from Laos; pp. 110–116. Cambridge. [Google Scholar]
- 12.Tran D.-S., Odermatt P., Le T.-O. Prevalence of epilepsy in a rural district of Central Lao PDR. Neuroepidemiology. 2006;26(4):199–206. doi: 10.1159/000092407. [DOI] [PubMed] [Google Scholar]
- 13.Barennes H., Tran D.-S., Latthaphasavang V., Preux P.M., Odermatt P. Epilepsy in Lao PDR: from research to treatment intervention. Neurology Asia. http://www.neurology-asia.org/articles.php Published June 2008.
- 14.Harimanana A., Chivorakul P., Souvong V., Preux P.-M., Barennes H. Is insufficient knowledge of epilepsy the reason for low levels of healthcare in the Lao PDR? BMC Health Serv Res. 2013;13:41. doi: 10.1186/1472-6963-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akkhavong K., Paphassarang C., Phoxay C., Vonglokham M., Phommavong C., Pholsena S. vol. 4. World Health Organization; 2014. http://apps.who.int/iris/bitstream/handle/10665/207762/9789290616481_eng.pdf;jsessionid=5923963A726B3C74C51FCA7295C0E8BD?sequence=1 (The Lao People’s Democratic Republic Health System Review). (on behalf of the Asia Pacific Observatory on Health Systems and Policies). Viroj Tangcharoensathien, Walaiporn Patcharanarumol International Health Policy Program, Ministry of Public Health, Thailand; 2014. [Google Scholar]
- 16.Boumédiène F., Chhour C., Chivorakoun P. Development of an interventional strategy for the management of epilepsy in South-east Asia. J Neurol Sci. 2017;381:374–375. [Google Scholar]
- 17.Chivorakoun P., Souvong V., Vorachit S., Latthaphasavang V., Phetsiriseng K., Naphayvong P. Lao association for patient with epilepsy: report of activity 2011-2014. Neurology Asia. http://www.neurology-asia.org/articles.php Published December 2015.
- 18.World Health Organization Geneva . 2002. Traditional Medicine Strategy 2002-2005. [Google Scholar]
- 19.Sydara K., Gneunphonsavath S., Wahlström R. Use of traditional medicine in Lao PDR. Complement Ther Med. 2005;13(3):199–205. doi: 10.1016/j.ctim.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Abdullahi A.A. Trends and challenges of traditional medicine in Africa. Afr J Tradit, Complementary Altern Med. 2011;8(5 Suppl):115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Millogo A., Ratsimbazafy V., Nubukpo P., Barro S., Zongo I., Preux P.M. Epilepsy and traditional medicine in Bobo-Dioulasso (Burkina Faso) Acta Neurol Scand. 2004;109(4):250–254. doi: 10.1111/j.1600-0404.2004.00248.x. [DOI] [PubMed] [Google Scholar]
- 22.Keikelame M.J., Swartz L. ‘A Thing Full of Stories’: traditional healers’ explanations of epilepsy and perspectives on collaboration with biomedical health care in Cape Town. Transcult Psychiatry. 2015;52(5):659–680. doi: 10.1177/1363461515571626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.François A.A., Elisée B.K., Christian T.A. Tradipraticiens et épilepsies en Côte d’Ivoire. Rev Neurol (Paris) 2014;170(8):508–511. doi: 10.1016/j.neurol.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Auditeau E., Moyano L.M., Bourdy G. Herbal medicine uses to treat people with epilepsy: a survey in rural communities of northern Peru. J Ethnopharmacol. 2018;215:184–190. doi: 10.1016/j.jep.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Neiss M.B., Leigland L.A., Carlson N.E., Janowsky J.S. Age differences in perception and awareness of emotion. Neurobiol Aging. 2009;30(8):1305–1313. doi: 10.1016/j.neurobiolaging.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leigh J. Lao culture and profile. 2012. http://www.diversicare.com.au/wp-content/uploads/2015/10/Profile_LaoSML.pdf Jennifer Leigh, J.Leigh & Associates.
- 27.Razali S.M., Yassin A.M. Complementary treatment of psychotic and epileptic patients in Malaysia. Transcult Psychiatry. 2008;45(3):455–469. doi: 10.1177/1363461508094676. [DOI] [PubMed] [Google Scholar]
- 28.Odermatt P., Ly S., Simmala C. Availability and costs of antiepileptic drugs and quality of phenobarbital in Vientiane municipality, Lao PDR. Neuroepidemiology. 2007;28(3):169–174. doi: 10.1159/000103270. [DOI] [PubMed] [Google Scholar]
- 29.Chivorakoun P., Harimanana A., Clavel S., Jousseaume S., Barennes H. Épilepsie au Laos : le difficile parcours d’un antiépileptique de première ligne contribue à la forte carence de traitement. Rev Neurol (Paris) 2012;168(3):221–229. doi: 10.1016/j.neurol.2012.01.584. [DOI] [PubMed] [Google Scholar]
- 30.Bounlu M., Auditeau E., Vorachit S. Explanatory factors of adherence to community-based management of epilepsy in Lao PDR. Epilepsy Behav. 2018;88:74–80. doi: 10.1016/j.yebeh.2018.08.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.