Abstract
Background
The SARS-CoV-2 pandemic has caused mental stress in a number of ways: overstrain of the health care system, lockdown of the economy, restricted opportunities for interpersonal contact and excursions outside the home and workplace, and quarantine measures where necessary. In this article, we provide an overview of psychological distress in the current pandemic, identifying protective factors and risk factors.
Methods
The PubMed, PsycINFO, and Web of Science databases were systematically searched for relevant publications (1 January 2019 – 16 April 2020). This study was registered in OSF Registries (osf.io/34j8g). Data on mental stress and resilience in Germany were obtained from three surveys carried out on more than 1000 participants each in the framework of the COSMO study (24 March, 31 March, and 21 April 2020).
Results
18 studies from China and India, with a total of 79 664 participants, revealed increased stress in the general population, with manifestations of depression and anxiety, post-traumatic stress, and sleep disturbances. Stress was more marked among persons working in the health care sector. Risk factors for stress included patient contact, female sex, impaired health status, worry about family members and significant others, and poor sleep quality. Protective factors included being informed about the increasing number of persons who have recovered from COVID, social support, and a lower perceived infectious risk. The COSMO study, though based on an insufficiently representative population sample because of a low questionnaire return rate (<20%), revealed increased rates of despondency, loneliness, and hopelessness in the German population as compared to norm data, with no change in estimated resilience.
Conclusion
Stress factors associated with the current pandemic probably increase stress by causing anxiety and depression. Once the protective factors and risk factors have been identified, these can be used to develop psychosocial interventions. The informativeness of the results reported here is limited by the wide variety of instruments used to acquire data and by the insufficiently representative nature of the population samples.
The SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) pandemic has led to over 11.5 million confirmed cases and more than 540 000 deaths worldwide since the end of 2019/beginning of 2020) (as of 10.07.2020) (1, 2). A pandemic on this scale causes stress and mental health burdens in the population (3, 4). These include:
The fear that one/others might fall ill or die due to the virus
-
Psychological distress as a result of:
Isolation or quarantine measures
Financial difficulties (for example, due to job loss)
Responses to the pandemic on a state level (for example, school closures) (5).
In addition, healthcare workers are exposed to further stressors, such as increased risk of infection, the distress caused by triage decision-making, or stigmatization (5, 6).
The aim of this article is to provide an overview of studies from China and other countries on stress and mental burden in the general population as well as in healthcare workers. The results of three cross-sectional surveys conducted in the German population on psychological distress and resilience are also presented. By describing identified risk and protective factors, it is our intention to inform scientists and decision-makers in the healthcare system as to where psychosocial interventions to cope with the pandemic could be deployed.
Methods
Systematic literature analysis
The approach to the systematic literature analysis is described in detail in the eMethods and eBox. Parallel to this, a protocol was developed according to PRISMA guidelines (7) and registered in OSF Registries (osf.io/34j8g). The present analysis included studies that met the criteria listed in Table 1. A systematic literature search was conducted in the electronic databases PubMed, PsycINFO, and Web of Science (Core Collection) for publications in the period 01.01.2019 to 16.04.2020. Study selection and data extraction of included studies, as well as quality assessments using a modified version of the NIH-NHLBI instrument for cross-sectional studies and cohort studies (8), were carried out by two pairs of independent reviewers (NR, MB and NR, JSW). Any disagreement was resolved through discussion or by involving a third assessor (KL) at each stage of the literature analysis. There was high inter-rater reliability (κ1= 0.875; κ2= 1) on the title/abstract and full-text screening levels. The data extracted for each study included are presented in the eMethods. For five areas of psychological distress (anxiety and worry, depression, posttraumatic stress, sleep disorders, stress), the respective proportion of a sample showing elevated values (>cut-off) on an appropriate scale was extracted, if indicated. Comparisons with norm data were also taken into consideration for the data extraction. Due to the heterogeneity of the studies included, no quantitative synthesis of study results was carried out.
eBOX. Search strategies.
PubMed
| #1 | “Mental health”[mh] |
| #2 | “mental health”[tw] |
| #3 | psychological[tw] |
| #4 | Resilience, psychological[mh] |
| #5 | resilien*[tiab] or hardiness*[tiab] |
| #6 | “post-traumatic growth”[tiab] or “posttraumatic growth”[tiab] or “stress-related growth”[tiab] |
| #7 | “resilience factor*”[tiab] or “protective factor*”[tiab] or resource*[tiab] |
| #8 | burden[tiab] |
| #9 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 |
| #10 | SARS [tiab] OR influenza[tiab] or flu[tiab] or MERS[tiab] or ebola[tiab] |
| #11 | Pandemic[mh] or pandem*[tw] |
| #12 | coronavirus[tw] or COVID-19[tw] or 2019-nCoV[tw] or SARS-CoV-2[tw] |
| #13 | Quarantine[mh] or quarantine[tw] |
| #14 | #10 or #11 or #12 or #13 |
| #15 | #9 and #14 |
| #16 | “health personnel”[mh] |
| #17 | “health* personnel”[tiab] or “health* profession*”[tiab] or “health* worker*”[tiab] or “health* practitioner*”[tiab] or “health* provider*”[tiab] or “health* staff”[tiab] |
| #18 | “care personnel”[tiab] or “care profession*”[tiab] or “care worker*”[tiab] or “care practitioner*”[tiab] or “care provider*”[tiab] or “care staff”[tiab] |
| #19 | “intensive care”[tiab] or ICU[tiab] |
| #20 | emergency[tiab] |
| #21 | ambulance[tiab] or paramedic*[tiab] |
| #22 | “hospital personnel” [tiab] or “hospital staff” [tiab] |
| #23 | physician*[tiab] or doctor*[tiab] |
| #24 | nurse*[tiab] or “nursing staff”[tiab] |
| #25 | #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 |
| #26 | Patients[mh] or patients[tiab] |
| #27 | older[tiab] or geriatric[tiab] |
| #28 | #26 or #27 |
| #29 | “population health”[mh] |
| #30 | public[tiab] |
| #31 | society[tiab] or social[tiab] |
| #32 | community[tiab] |
| #33 | “general population”[tiab] |
| #34 | nationwide[tiab] |
| #35 | #29 or #30 or #31 or #32 or #33 or #34 |
| #36 | #25 or #28 or #35 |
| #37 | #15 and #36 |
PsycINFO
| S1 | MA Mental health |
| S2 | TX Mental Health |
| S3 | TX psychological |
| S4 | MA Resilience, psychological |
| S5 | TI resilien* OR AB resilien* OR TI hardiness* OR AB hardiness* |
| S6 | TI posttraumatic growth OR AB posttraumatic growth OR TI post-traumatic growth OR AB post-traumatic growth OR TI stress-related growth OR AB stress-related growth |
| S7 | TI resilience factor* OR AB resilience factor* OR TI protective factor* OR AB protective factor* OR TI resource* OR AB resource* |
| S8 | TI burden OR AB burden |
| S9 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 |
| S10 | TI SARS OR AB SARS OR TI Influenza OR AB Influenza OR TI Flu OR AB Flu OR TI MERS OR AB MERS OR TI Ebola OR AB Ebola |
| S11 | MA pandemic OR TX pandem* |
| S12 | TX coronavirus OR TX COVID-19 OR TX 2019-nCoV OR TX SARS-CoV-2 |
| S13 | MA quarantine OR TX quarantine |
| S14 | S10 OR S11 OR S12 OR S13 |
| S15 | S9 AND S14 |
| S16 | MA health personnel |
| S17 | TI health* personnel OR AB health* personnel OR TI health* profession* OR AB health* profession* OR TI health* worker* OR AB health* worker* OR TI health* practitioner OR AB health* practitioner OR TI health* provider* OR AB health* provider* OR TI health* staff OR AB health* staff |
| S18 | TI care personnel OR AB care personnel OR TI care profession* OR AB care profession* OR TI care worker* OR AB care worker* OR TI care practitioner* OR AB care practitioner* OR TI care provider* OR AB care provider* OR TI care staff OR AB care staff |
| S19 | TI intensive care OR AB intensive care OR TI ICU OR AB ICU |
| S20 | TI emergency OR AB emergency |
| S21 | TI ambulance OR AB ambulance OR TI paramedic* OR AB paramedic* |
| S22 | TI hospital personnel OR AB hospital personnel OR TI hospital staff OR AB hospital staff |
| S23 | TI physician* OR AB physician* OR TI doctor* OR AB doctor* |
| S24 | TI nurse* OR AB nurse* OR TI nursing staff OR AB nursing staff |
| S25 | S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 |
| S26 | MA patients OR TI patients OR AB patients |
| S27 | TI older OR AB older OR TI geriatric OR AB geriatric |
| S28 | S26 OR S27 |
| S29 | MA population health |
| S30 | TI public OR AB public |
| S31 | TI society OR AB society OR TI social OR AB social |
| S32 | TI community OR AB community |
| S33 | TI general population OR AB general population |
| S34 | TI nationwide OR AB nationwide |
| S35 | S29 OR S30 OR S31 OR S32 OR S33 OR S34 |
| S36 | S25 OR S28 OR S35 |
| S37 | S15 AND S36 |
-
Web of Science (Core Collection)
# 36 #33 AND #13
Refined by: WEB OF SCIENCE CATEGORIES: (PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR PSYCHOLOGY OR PSYCHOLOGY CLINICAL OR PRIMARY HEALTH CARE OR PSYCHIATRY OR NURSING OR PSYCHOLOGY MULTIDISCIPLINARY)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 35 #33 AND #13
Refined by: WEB OF SCIENCE CATEGORIES: (INFECTIOUS DISEASES OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR IMMUNOLOGY OR PSYCHOLOGY OR VIROLOGY OR PSYCHOLOGY CLINICAL OR PRIMARY HEALTH CARE OR PSYCHIATRY OR NURSING OR SOCIAL SCIENCES INTERDISCIPLINARY OR PSYCHOLOGY MULTIDISCIPLINARY OR SOCIAL WORK)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 34 #33 AND #13
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 33 #32 OR #25 OR #22
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 32 #31 OR #30 OR #29 OR #28 OR #27 OR #26
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 31 TS=nationwide
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 30 TS=“general population”
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 29 TS=community
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 28 TS=(society or social)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 27 TS=public
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 26 TS=“population health”
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 25 #24 OR #23
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 24 TS=(older or geriatric)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 23 TS=patients
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 22 #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 21 TS=(nurse* or “nursing staff”)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 20 TS=(physician* or doctor*)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 19 TS=(“hospital personnel” or “hospital staff”)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 18 TS=(ambulance or paramedic*)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 17 TS=emergency
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 16 TS=(“intensive care” or ICU)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 15 TS=(“care personnel” or “care profession*” or “care worker*” or “care practitioner*” or “care provider*” or “care staff”)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 14 TS=(“health* personnel” or “health* profession*” or “health* worker*” or “health* practitioner*” or “health* provider*” or “health* staff”)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 13 #12 AND #7
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 12 #11 OR #10 OR #9 OR #8
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 11 TS=quarantine
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 10 TS=(coronavirus or COVID-19 or 2019-nCoV or SARS-CoV-2)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 9 TS=pandem*
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 8 TS=(SARS or influenza or flu or MERS or ebola)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 7 #6 OR #5 OR #4 OR #3 OR #2 OR #1
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 6 TS=burden
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 5 TS=(“resilience factor*” or “protective factor*” or resource*)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 4 TS=(“post traumatic growth” or “posttraumatic growth” or “stress related growth”)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 3 TS=(resilien* or hardiness*)
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 2 TS=psychological
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
# 1 TS=“mental health”
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=1990–2020
191916.04.202085716.04.202012616.04.2020190
Table 1. Selection criteria for the systematic literature analysis.
| Criterion | Description |
| Population | Inclucion: General population. healthcare workers (e.g.. physicians. nurses). irrespective of age and health status; exposure to SARS-CoV-2 pandemic; all countries Exclusion: COVID-19 patients or other patient groups; other infections (e.g.. MERS. SARS. Ebola. HIV. influenza) |
| Endpoints | Inclusion: Assessment of psychological distress (e.g.. anxiety and worry. depression. posttraumatic stress. sleep. stress) and/or assessment of protective factors. including resilience or risk factors Exclusion: no exclusion criteria |
| Study design | Inclusion: Questionnaire-based cross-sectional and longitudinal studies (survey-based studies) Exclusion: Interventional studies |
| Publication language | All |
| Publication formats | Inclusion: Original articles Exclusion: Other publication formats (e.g.. reviews. letters to the editor. comments) |
| Publication status | Inclusion: Peer-reviewed publications |
COVID-19. coronavirus disease 2019; HIV. human immunodeficiency virus infection; MERS. Middle East respiratory syndrome; SARS. severe acute respiratory syndrome
Data collection on psychomorbidity and resilience in Germany
The COVID-19 Snapshot Monitoring (COSMO) study (9, 10) monitored perception of the current SARS-CoV-2 outbreak in quota samples of an online panel at three measurement points:
24./25.03.2020, wave 4
31.03./01.04.2020, wave 5
21./22.04.2020, wave 8.
The quotas match the German population in terms of age, sex (crossed), and German federal state (uncrossed). Due to the response rates of 19% (wave 4), 14% (wave 5), and 15% (wave 8), the results are representative of the German population to only a limited extent. Psychological distress was assessed on the basis of five items for the period of the previous 7 days:
“I felt nervous, anxious, or on edge” (item 1, GAD-7, [11])
“I felt depressed” (item 6, ADS [12])
“I felt lonely” (item 14, ADS [12])
“I felt hopeful about the future” (item 8, ADS [12])
“Thoughts about my experiences during the Coronavirus pandemic caused me to have physical reactions, such as sweating, trouble breathing, nausea or a pounding heart” (item 19, IES-R [13]).
To estimate the reported overall psychological burden, the mean value of the five items was determined. Suicidal tendency was not assessed. In order to estimate fear of SARS-CoV-2, the mean value of nine items tailored to the situation were recorded. The subjective assessment of resilience was surveyed with the Brief Resilience Scale (BRS [14, 15]). The results of the COSMO study were compared with the norm data of the Generalized Anxiety Disorder Screener (GAD-7) (11), the German General Depression Scale (Allgemeine Depressionsskala, ADS) (12), and the Brief Resilience Scale (BRS) (14, 15) for the German population before the outbreak of the SARS-CoV-2 pandemic.
Results
Systematic literature analysis
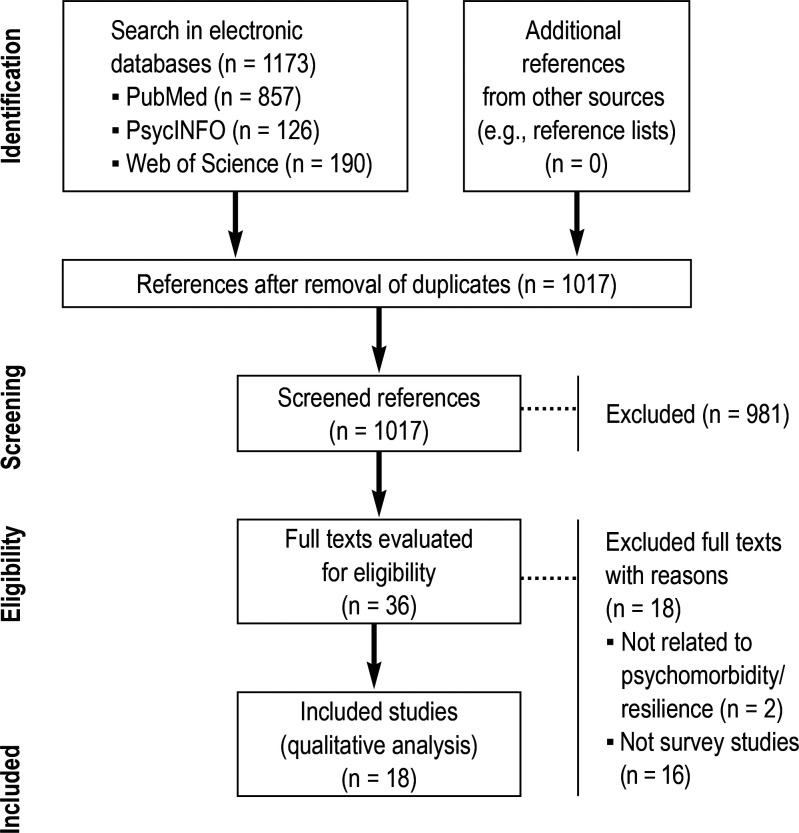
The literature search initially identified 1173 studies, of which n = 18 studies with i = 18 reported samples were included in the analysis according to the inclusion criteria (efigure).
eFigure.
Flow diagram on study selection (search period 01. 01. 2019 to 16. 04. 2020)
Table 2, etable 1, and etable 2 provide an overview of the included studies, their study populations, as well as the survey instruments and cut-off values used.
Table 2. Survey-based studies from China and India on the psychological effects of the SARS-CoV-2 pandemic (as of 16.04.2020).
| Country | Participants; female (%); age (M ± SD) [alternative data] |
Subgroups | Anxiety and worry | Depression | Posttraumatic stress | Sleep | Stress/other outcomes | |
| General population | ||||||||
| Cao et al. (2020) (e16) |
China | 7143; 4975 (69.65%); n. a. |
n. a. | GAD-7 | n. a. | n. a. | n. a. | n. a. |
| Liu et al. (2020) (e7) |
China | 285; 155 (54.4%); n. a. [47.7% <35 years] |
n. a. | n. a. | n. a. | PCL-5 (higher than norm*1) | n. a. | n. a. |
| Qiu et al. (2020) (e4) |
China. Hong Kong. Macao. Taiwan | 52 730; 34 131 (64.73%); n. a. |
n. a. | n. a. | n. a. | n. a. | n. a. | CPDI |
| Roy et al. (2020) (e17) |
India | 662; 339 (51.2%); 29.09 ± 8.83 |
n. a. | SD | n. a. | n. a. | SD | n. a. |
| Wang C et al. (2020) (16) |
China | 1210; 814 (67.3%); n. a. [53.1% 21.4–30.8 years] |
n. a. | DASS-21 subscale on anxiety |
DASS-21 subscale on depression |
IES-R | n. a. | DASS-21 subscale on stress |
| Wang Y et al. (2020) (e18) |
China | 600; 333 (55.5%); 34 ± 12 |
n. a. | SAS | SDS | n. a. | n. a. | n. a. |
| Zhang Y et al. (2020) (e19) |
China | 263; 157 (60%); 37.7± 14.0 |
n. a. | n. a. | n. a. | IES | n. a. | n. a. |
| Healthcare workers | ||||||||
| Cai et al. (2020) (e1) |
China | 534; 367 (68.7%); 36.4 ± 16.18 years |
P (n = 233). NS (n = 248) |
SD | n. a. | n. a. | n. a. | n. a. |
| Huang JZ et. al. (2020) (e9) |
China | 230; 187 (81.30%); n. a. [53% 30–39 years] |
P (n = 70). NS (n = 160) |
SAS | n. a. | PTSD-SS | n. a. | n. a. |
| Kang et al. (2020) (e20) |
China | 994; 850 (85.5%); n. a. [63.4% ca. 30–40 years] |
P (n = 183). NS (n = 811) |
GAD-7 | PHQ-9 | IES-R | ISI | n. a. |
| Lai et al. (2020) (6) |
China | 1257; 964 (76.7%); n. a. [64.7% 26–40 years] |
P (n = 493). NS (n = 764) |
GAD-7 | PHQ-9 | IES-R | ISI | n. a. |
| Mo et al. (2020) (e2) |
China | 180; 162 (90%); 129 (71.7%); 32.71 ± 6.52 |
n. a. | SAS (higher than norm*2) |
n. a. | n. a. | n. a. | SOS |
| Xiao et al. (2020) (e3) |
China | 180; 129 (71.7%); 32.31±4.88 |
P (n = 82). NS (n = 98) |
SAS (higher than norm*3) |
n. a. | n. a. | PSQI | SASR; GSES; SSRS |
| Mixed groups | ||||||||
| Huang Y et al. (2020) (e6) |
China | 7236; 3952 (54.6%); 35.3 ± 5.6 |
HW (n = 2250) | GAD-7 (higher than norm*4) |
CES-D (higher than norm*5) |
n. a. | PSQI | n. a. |
| Li et al. (2020) (e8) |
China | 740; 128 (59.81%); 25 [IQR: 22–38.3] |
GP (n = 214). NS (n = 526) |
n. a. | n. a. | VTQ | n. a. | n. a. |
| Lu et al. (2020) (e21) |
China | 2299; 1785 (77.6%); n. a. [78% <40 years] |
HW (n = 2042). AS (n = 257) |
HAMA. NRS on fear |
HAMD | n. a. | n. a. | n. a. |
| Yuan et al. (2020) (e22) |
China | 939; 582 (61.98%); n. a. [71.5% 18–39 years] |
HW (n = 249). S (n = 312) |
n. a. | n. a. | n. a. | n. a. | n. a. |
| Zhang W et al. (2020) (e23) |
China | 2182; 1401 (64.2%); n. a. [96.3% 18–60 years] |
HW (n = 927). GP (n = 1255) |
GAD-2 | PHQ-2 | n. a. | ISI | SCL-90-R |
*1 Prevalence: 7 versus 3.7%
*2 M ± SD: 32.19 ± 7.56 versus 29.78 ± 0.46; t = 4.27; p <0.001
*3 M ± SD: 8.583 ± 4.567 versus 7 (SD n. a.)
*4 Prevalence: 35.1 versus 5.0%; *5 prevalence: 20.3 versus 3.6%
IQR. interquartile range. M. mean value; n. a.. not available; t. value of the t-test for independent samples; SD. standard deviation
Subgroups: GP. general population; P. physicians; HW. healthcare workers; NS. nursing staff; S. students; AS. administrative staff
Measurement tools: CES-D. Center for Epidemiologic Studies Depression Scale to measure depressive symptoms; CPDI. COVID-19 Peritraumatic Distress Index; DASS-21. Depression. Anxiety and Stress Scale; GAD-2. Generalized Anxiety Disorder Scale-2 to measure symptoms of anxiety; GAD-7. Generalized Anxiety Disorder Scale-7 to measure symptoms of anxiety; GSES. General Self-Efficacy Scale to measure self-efficacy; HAMA. Hamilton Anxiety Scale to measure symptoms of anxiety; HAMD. Hamilton Depression Scale to measure depressive symptoms; IES. Impact of Event Scale to measure posttraumatic stress symptoms; IES-R. Impact of Event Scale—Revised to measure posttraumatic stress symptoms; ISI. Insomnia Severity Index to measure sleep disorders; NRS. Numeric Rating Scale; PCL-5. Posttraumatic Stress Disorder Checklist for DSM-5 for posttraumatic stress symptoms; PHQ-2. Personal Health Questionnaire-2 to measure depressive symptoms; PHQ-9. Personal Health Questionnaire-9 to measure depressive symptoms; PSQI. Pittsburgh Sleep Quality Index to measure sleep quality; PTSD-SS. PTSD Self-rating Scale to measure posttraumatic stress symptoms; SAS. Self-Rating Anxiety Scale to measure anxiety symptoms; SASR. Stanford Acute Stress Reaction questionnaire to measure stress reactions; SCL-90-R. symptom checklist 90—Revised to measure psychological distress; SDS. Self-Rating Depression Scale; SD. self-developed questionnaire; SOS. Stress Overload Scale to measure stress; SSRS. Social Support Rate Scale to assess social support; VTQ:. Vicarious Traumatization Questionnaire to assess secondary traumatization. based. e.g.. on the TSIB (Traumatic Stress Institute Belief Scale). VTS (Vicarious Trauma Scale). and IES
eTable 1. Extraction table for survey studies on psychological effects of the SARS-CoV-2 pandemic (as of April 16, 2020).
| Country; participants; female (%); age (M ± SD) [alternative information] | Subgroup; assessment; survey period | Assessment tools or questions asked | Psychological distress | Stress/ other outcomes | Moderating factors | ||||
| Anxiety, fear, worries | Depressive symptoms | Posttraumatic stress | Sleep-related symptoms | ||||||
| General Population | |||||||||
| Cao et al. (2020) (e16) | China; 7,143; 4,975 (69.65%); NR | Medical students from Changzhi Medical College; Internet, no details on recruitment, cross-sectional; NR | GAD-7 | 24.9% affected; 0.9% severe, 2.7% moderate, 21.3% mild symptoms | NR | NR | NR | NR | for anxiety: infection of loved ones (+); worries about economic impact of the epidemic (+); concerns about study related disadvantages (+); influence of the epidemic on daily life (+); stability of family income (–); living in a urban area (–); living with parents (–); social support (–) |
| Liu et al. (2020) (e7) | China; 285; 155 (54.4%); NR [47.7%<35] | Current (n=124) or previous (n=188) stay in Wuhan; internet, no details on recruitment; January 30 - February 08, 2020 | PCL-5, PSQI | NR | NR | 7% according to PCL-5 (higher than norm data1) | NR | NR | For PTSD: Female sex (+); Risk groups (+); no current / previous stay in Wuhan (–); poor subjective sleep quality (+); sleep latency (+) |
| Qiu et al. (2020) (e4) | China, Hong Kong, Taiwan, Macao; 52,730; 34,131 (64.73%), NR | GP; internet, recruitment with QR code via Siuvo Intelligent Psychological Assessment Platform, cross-sectional; January 31 – February 10, 2020 | CPDI | NR | NR | NR | NR | 35% CPDI>27 | for psychological distress: female (+); age < 18 (–); migrant workers (+); being from hubei (+) |
| Roy et al. (2020) (e17) | India; 662; 339 (51.2%); 29.09±8.83 | GP; internet, snowball sampling method via e-mail, WhatsApp, other social media, cross-sectional; March 22 – 24, 2020 | multiple-choice-questions on awareness, attitudes, fear | 82.2% preoccupations about COVID-19; 37.8 % hypochondriac fear | NR | NR | 12.5% sleep disorders due to worries | NR | NR |
| Wang, C. et al. (2020) (16) | China; 1,210; 814 (67.3%); NR [53.1% age 21.4-30.8] | GP; internet, via snowball sampling to students, cross-sectional; January 31 - February 2, 2020 | IES-R, DASS-21 | 28.8% >9 in DASS-21 anxiety subscale | 16.5% >12 in DASS-21 depression subscale | 53.8% > 33 im IES-R; M±SD: 32.98± 15.42 | NR | Stress: 8.1%>18 in DASS-21stress subscale | For PTSD: male sex (–); students (+); respiratory symptoms (+); chronic diseases (+); discontent with information about COVID-19 (+); concerns about children (+); hygiene behavior (–); For stress: students (+); reduced perceived health (+); chronic diseases (+); discontent with information on COVID-19 (+); information about increase in cured (–); no trust in the doctor (+); low perceived risk of infection (–); perceived risk of death from infection (+); concerns about family (+); hygiene behavior (–) For fear: students (+); doctor's visits (+); hospital stays (+); reduced perceived health (+); chronic diseases (+); contact to person with COVID-19 (+); no confidence in the doctor (+); low perceived risk (–) of infection; concerns about children (+); hygiene behavior (–) for depressive symptoms: low educational level (+); reduced perceived health (+); chronic diseases (+); discontent with information on COVID-19 (+); information about increase in the number of people cured (–); no trust in the doctor (+); hygiene behavior (–) |
| Wang, Y et al. (2020) (e18) | China; 600; 333 (55.5%); 34 ± 12 | GP; internet, no details on recruitment, cross-sectional; February 6 - 9, 2020; | SAS, SDS | 0.67% SAS> 59 (36.92 ± 7.33) | 2.83% SDS>62 (40.50 ± 11.31) | NR | NR | NR | for anxiety: female sex (+); age > 40 (+) |
| Zhang, Y. et al. (2020) (e19) | China; 263; 157 (60%); 37.7± 14.0 | GP from Liaoning; internet, recruitment via WeChat, cross-sectional; January 28 – 5, 2020 | i. a. IES | NR | NR | 7.6% IES > 25 (13.6±7.7) | NR | NR | for PTSS: (–) rest |
| Healthcare Workers | |||||||||
| Cai et al. (2020) (e1) | China; 534; 367 (68.7%); 36.4 (16.18) | physicians (n=233), nurses (n=248) in Hunan; no details on recruitment, cross-sectional; January –March, 2020 | Custom-built: emotions during COVID-19 outbreak, stressors, protective factors, coping and others | 40.6% > 1 (anxious+ nervous) | NR | NR | NR | NR | for stress: concerns about infecting family |
| Huang, JZ. et. al. (2020) (e9) | China; 230; 187 (81.30%); NR [53% age 30-39] | physicians (n=70), nurses (n=160) (all in frontline position); institutional survey, no details on recruitment, cross-sectional; February 7- 14, 2020 | SAS, PTSD-SS | 11.63% of the 43 men, 25.67% of the 187 women SAS>49; (together 23.04 %) |
NR | 18.60% of the 43 men, 29.41% der 187 women PTSD-SS>49; (together 27.39%) | NR | NR | for anxiety: male sex (–); medical profession (–); low professional position (+) for post-traumatic stress: male sex (–) |
| Kang et al. (2020) (e20) | China; 994; 850 (85.5%); NR [63.4% age 30-40] | physicians (n=183), nurses (n=811); interent, recruitment via Wenjuanxing, cross-sectional; January 29 - February 04, 2020 | PHQ-9, GAD-7, ISI, IES-R; K-means-clustering-method for all of the measuring tools > mental health | 22.4% with GAD-7 mean value 8.2; 6.2% with GAD-7-M 15.1 | 22.4% with PHQ-9 mean value 9; 6.2% PHQ-9-M 15.1 | 22.4% with IES-R-mean value 39.9; 6.2% with IES-R mean value 60.0 | 22.4% with ISI mean value 10.4; 6.2% with ISI mean value 15.6 | NR | For mental health: exposure to COVID-19 (+); use of psychoeducational materials (–) |
| Lai et al. (2020) (6) | China; 1,257; 964(76.7%); NR[64.7% age 26 - 40] | subgroups: nurses (n= 764), physicians (n=493), from Wuhan (n=760), direct contact with COVID-19 patients (n=522); no details on recruitment, cross-sectional; January 29 – March 1, 2020 | PHQ-9, GAD-7, ISI, IES | 44.6% GAD-7 > 6 | 50.4% PHQ-9 > 8 | 71.5% IES-R > 25 | 34% ISI > 14 | NR | for depressive symptoms: Nursing staff(+); female sex (+); work at secondary hospital(+); middle professional position(+); direct patient contact(+) for fear: female sex (+); middle professional position (+); work at secondary hospital (+); direct patient contact (+) for sleep-related symptoms: direct patient contact (+) for stress: female sex (+); middle professional position(+); direct patient contact (+); work outside Hubei (–) |
| Mo et al. (2020) (e2) | China; 180; 162 (90%); 129 (71.7%); 32.71 ± 6.52 | nurses from Guangxi in Wuhan; internet, via computer/ smartphone, QR-Code, cross-sectional; end of February, 2020 | SOS, SAS | SAS: M±SD 32.19±7.56 | NR | NR | NR | SOS: stress: 22.22%> 50; (M±SD 39.91±12.92) |
for stress: siblings (–); workload(+) anxiety (+); high professional qualification(+); poor sleep quality (+); severity of the patient's condition (+); lack of adaptation to daily diet (+) |
| Xiao et al. (2020) (e3) | China; 180; 129 (71.7%); 32.31±4.88 | physicians (n=82), nurses (n=98) from Wuhan; no details on recruitment, cross-sectional; January –February, 2020 | SAS, GSES, SASR, PSQI, SSRS | SAS: M±SD 55.256± 14.183 (SAS) |
NR | NR | PSQI: M±SD 8.583±4.567 (higher than norm data2) | stress: M±SD 77.589± 29.525 (SASR) self-efficacy: GSES: M±SD 2.267±0.767 social support: SSRS: M±SD 34.172 ± 10.263 |
for sleep-related symptoms: anxiety (+); stress (+); self-efficacy (–); for anxiety: social support (–); for stress: social support (–); anxiety (+) |
| Mixed Groups | |||||||||
| Huang, Y. et al. (2020) (e6) | China; 7,236; 3,952 (54.6%); 35.3 ± 5.6 | GP, subgroup HCW (n = 2,250); internet, recruitment via WeChat, cross-sectional; February 3 - 17, 2020 | GAD-7, CES-D, PSQI, knowledge about COVID-19 and time spent thinking about COVID-19 | 35.1% GAD-7 > 9 (higher than norm data3); healthcare workers 35.6% (34.9% = mean of the remaining) | 20.1% CES-D > 28 (higher than norm data); HCW 19.8% (GP 20.2% =mean of the remaining) | NR | 18.2% PSQI > 7; HCW 23.8% (GP 15.67% = mean of the remaining) |
NR | for depressive symptoms: age <35 (+); health profession+ >3h/d thinking about COVID-19(+) for sleep related symptoms: health profession(+); health profession+>3h/d thinking about COVID-19(+) |
| Li et al. (2020) (e8) | China; 740; 128 (59.81%); 25 [IQR: 22–38.3] | GP (n=214) + nurses (n= 526), contact with COVID-19 (n=234); App-based, recruitment via WeChat, cross-sectional; February 17 - 21, 2020 | Vicarious Traumatization Questionnaire | NR | NR | Vicarious Traumatization Questionnaire: Median (IQR) GP 75.5 (62–88.3), nurses with contact 64 (52–75), without contact 75.5 (63–92) | NR | NR | for vicarious traumatization: general population or nursing staff without direct contact with COVID-19 (+) |
| Lu et al. (2020) (e21) | China; 2,299; 1,785 (77.6%); NR [78% age <40] | HCW (n=2,042), administrative staff (n=257); internet, no details on recruitment, cross-sectional; February 25 – 26, 2020 | NRS on fear, HAMA, HAMD | HCW: 70.6%>3 in NRS on fear, 25.5% >6 in HAMA; administrative staff: 58.4%> 3 in NRS on fear; 18.7% >6 in HAMA | HCW: 12.1% >6 in HAMD; administrative staff: 8.2% >6 in HAMD |
NR | NR | NR | for fear: health professional (+); high risk contact (+); for depressive symptoms: high-risk contact (+) |
| Yuan et al. (2020) (e22) | China; 939; 582 (61.98%); NR [71.5% age 18-39] | HCW (n=249); students (n=312); internet, no details on recruitment, longitudinal; 2 assessments in February, 2020 | SRQ, PSQI | NR | NR | NR | NR (change in M of the PSQI-items: –0.148) | NR (SRQ: change in M of the emotional state: 0.392; M-change in somatic responses: 0.014) | NR |
| Zhang, W. et al. (2020) (e23) | China; 2,182; 1,401 (64.2%); NR [96.3% age 18-60] | HCW (n=927), GP (n=1,255); internet, recruitment via Wenjuanxing, cross-sectional; February 19 – March 6, 2020 | ISI, SCL-90-R, PHQ-4(GAD-2+PHQ-2) | 10.4% GAD-2>2; HCW 13%; GP 8.5% | 10.6% PHQ-2>2; HCW 12.2%; GP 9.5% | NR | 33.9% ISI>7 (9.5%>14); HCW: 38.4% (10.5%); GP 30.5% (8.8%) | somatization: 0.9% SCL-90-R subscore>2; HCW 1.6%, GP 0.4% Zwang: 3.5% SCL-90-R subscore>2; HCW 5.3%; GP 2.2% phobic anxiety: 2.9% SCL-90-R subscore>2; HCW 3.6%; GP 2.4% |
for anxiety: health profession (+); female sex (+); being married (+); risk of contact with COVID-19 patients in the hospital (+); organic diseases (+); for depressive symptoms: health profession (+); living in rural areas (+); living with family (+); organic diseases (+) for sleep related symptoms: health profession (+); living in rural areas (+); living with family (+); risk of contact with COVID-19 patients in the hospital (+); organic diseases (+) |
Abbreviations:
GP: general population; HCW: healthcare workers; M: mean value; NR: not reported; SD: standard deviation
(+): positive correlation; (-): negative correlation; CES-D: Center for Epidemiologic Studies Depression Scale to assess depressive symptoms; CPDI: COVID-19 Peritraumatic Distress Index; DASS-21: Depression, Anxiety and Stress Scale; GAD-7: Generalized Anxiety Disorder Scale-7 to assess generalized anxiety disorders; GSES: General Self-Efficacy Scale to assess self-efficacy; HAMA: Hamilton Anxiety Scale to assess anxiety symptoms; HAMD: Hamilton Depression Scale to assess depressive symptoms; IES-R: Impact of Event Scale - Revised to assess post-traumatic symptoms; ISI: Insomnia Severity Index to assess sleep disorders; NRS: Numeric Rating Scale; PCL-5: Posttraumatic Stress Disorder Checklist for DSM-5 for post-traumatic stress symptoms; PCL-C: Posttraumatic Stress Disorder Checklist- Civialians for posttraumatic stress symptoms; PHQ-4: Personal Health Questionnaire-4 to assess anxiety and depressive symptoms; PHQ-9: Personal Health Questionnaire 9 to assess depressive symptoms; PSQI: Pittsburgh Sleep Quality Index to assess sleep quality; PTSD: PTSD-SS: PTSD Self-rating Scale to assess post-traumatic stress symptoms; SAS: Self-Rating Anxiety Scale for recording anxiety symptoms; SASR: Stanford Acute Stress Reaction Questionnaire to assess stress reactions; SCL-90-R: Symptom Checklist 90-Revised to assess mental stress; SDS: Self-Rating Depression Scale; SE: Self-developed questionnaire; SOS: Stress Overload Scale to assess stress; SRQ: Stress Response Questionnaire to assess emotional situation, somatic reactions and behavior; SSRS: Social Support Rate Scale to assess social support; Vicarious Traumatization Questionnaire to assess secondary traumatization, based on TSIB (Traumatic Stress Institute Belief Scale), VTS (Vicarious Trauma Scale) and IES
1 prevalence: 7% vs 3.7%
2 M ± SD: 32.19±7.56 vs 29.78±0.46; t=4.27; p<0.001
3 prevalence: 35.1% vs 5.0%
4 prevalence: 20.3% vs 3.6%
eTable 2. Cut-off values or measurement data on the studies included.
| Cut-off values for “abnormal”/reported measurements. scale span | |
| CES-D | Huang et al. (e6): >28 (norm population 3.6%). 0–60 |
| CPDI | Qiu et al. (e4): >27. 0–100 |
| DASS-21: subscale on depression | Wang et al. (16): >12. 0–42 |
| DASS-21: subscale on anxiety | Wang et al. (16): >9. 0–42 |
| DASS-21: Subscale on stress | Wang et al. (16): >18. 0–42 |
| GAD-2 | Zhang et al. (e23): >2; n. a. |
| GAD-7 | Huang et al. (e6): >9 (norm population 5.0%). 0–21; Lai et al. (6): >6. 0–21; Cao et al. (e16): n. a.. 0–21; Kang et al. (e20): M for clusters 0–21 |
| GSES | Xiao et al. (e3): M ± SD 10–40 |
| HAMA | Lu et al. (e21): >6. 0–56* (14 items with scaling 0–4) |
| HAMD | Lu et al. (e21): >6. 0–68* (17 items with scaling 0–4) |
| IES | Zhang et al. (e19): >25 (M ± SD). 0–75* (15 items with scaling 0–5) |
| IES-R | Lai et al. (6): >25. 0–88; Kang et al. (e20): M for clusters. 0–88; Wang. C. (16): >33. 0–23 (normal). 24–32 (mild). 33–36 (moderate). >37 (severe) |
| ISI | Lai et al. (6): >14. 0–28; Kang et al. (e20): M for clusters. 0–28; Zhang et al. (e23): >7. n. a. |
| NRS on fear | Lu et al. (e21): >3. 0–10; |
| PCL-5 | Liu et al. (e7): >1 in 1 criterion-B item each + 1 + criterion-C item + 2 criterion D items + 2 criterion-E items. as well as for single items: >1. 20 items in total with scaling 0–4 |
| PHQ-2 | Zhang et al. (e23): >2. n. a. |
| PHQ-9 | Lai et al. (6): >9. 0–27; Kang et al. (e20): M for clusters. 0–21 |
| PSQI | Huang et al. (e6): >7. 0–21; Liu et al. (e7): only four of the 19 items. each item assessed individually: poor or very poor subjective sleep quality. sleep latency >30 min. sleep disorders: yes. sleep duration >7 h; Xiao et al. (e3): M ± SD (norm data: 7). 0–21; Yuan et al. (e22): three modified items in the test. given as mean change. scaling –3 to 2 |
| PTSD-SS | Huang et al. (e9): >49 (norm data: 25.8%). n. a. |
| SAS | Mo et al. (e2): M ± SD (norm data 29.78 ± 0.46; t = 4.27. p <0.001). n. a..; xiao et al. (e3): m ± sd; wang et al. (e18): >59 (M ± SD). <50 = no symptoms; 50–59 = mild. 60–69 = moderate. >70 = severe; Huang et al. (e9): <50 = normal. 50–60 mild; 61–70 moderate >70 severe |
| SASR | Mo et al. (e2): M ± SD. 0–150 |
| SCL-90-R | Zhang et al. (e23): per subscore >2. scaling 0–4 |
| SDS | Wang et al. (e18): >62 (M ± SD). <53 = no symptoms. 53–62 = mild. 63–72 = moderate. >73 = severe |
| SD | Generally: ≥ moderate; Cai et al. (e1): >1 |
| SOS | Mo et al. (e2): >50 (M ± SD). 22–110 |
| SRQ | Yuan et al. (e22): given as mean change. scaling –3 to 2 |
| SSRS | Xiao et al. (e3): M ± SD. 7–56 |
| VTQ | Li et al. (e8): median (IQR). n. a. |
* Given only indirectly; IQR: interquartile range; M: mean value; n. a.: not available
Measurement tools: CES-D. Center for Epidemiologic Studies Depression Scale to measure depressive symptoms; CPDI. COVID-19 Peritraumatic Distress Index; DASS-21. Depression. Anxiety and Stress Scale; GAD-2. Generalized Anxiety Disorder Scale-2 to measure symptoms of anxiety; GAD-7. Generalized Anxiety Disorder Scale-7 to measure symptoms of anxiety; GSES. General Self-Efficacy Scale to measure self-efficacy; HAMA. Hamilton Anxiety Scale to measure symptoms of anxiety; HAMD. Hamilton Depression Scale to measure depressive symptoms; IES. Impact of Event Scale to measure posttraumatic stress symptoms; IES-R. Impact of Event Scale–Revised to measure posttraumatic stress symptoms; ISI. Insomnia Severity Index to measure sleep disorders; NRS. Numeric Rating Scale; PCL-5. Posttraumatic Stress Disorder Checklist for DSM-5 for posttraumatic stress symptoms; PHQ-2. Personal Health Questionnaire-2 to measure depressive symptoms; PHQ-9. Personal Health Questionnaire 9 to measure depressive symptoms; PSQI. Pittsburgh Sleep Quality Index to measure sleep quality; PTSD-SS. PTSD Self-rating Scale to measure posttraumatic stress symptoms; SAS. Self-Rating Anxiety Scale to measure anxiety symptoms; SASR. Stanford Acute Stress Reaction questionnaire to measure stress reactions; SCL-90-R. symptom checklist 90-Revised to measure psychological distress; SDS. Self-Rating Depression Scale; SD. self-developed questionnaire; SOS. Stress Overload Scale to measure stress; SRQ. Stress Response Questionnaire; SSRS. Social Support Rate Scale to assess social support; VTQ. Vicarious Traumatization Questionnaire to assess secondary traumatization. based. e.g.. on the TSIB (Traumatic Stress Institute Belief Scale). VTS (Vicarious Trauma Scale). and IES
In total, the following publications with 79 664 participants were taken into consideration:
16 nonrepresentative studies from China on psychological burden (data on diagnoses were not available) published between 06.03.2020 (first study: [16]) and 15.04.2020 (e1)
One study from India
A multinational study from China, Hong Kong, Taiwan, and Macao.
No European studies were available at the time of the literature search. Sample sizes ranged from 180 (e2, e3) to 52 730 (e4) participants (table 2). It was not possible to calculate average age or sex distribution due to lacking data in some studies (etable 1). The quality assessment rated nine of the 18 studies as poor, six as fair, and three as good (etable 3).
eTable 3. Quality assessment of the included studies.
| Study | 1. Clear research question | 2. Clearly defined sample? | 3. Participation rate >50%? | 4. Participants from the same or similar population? Prespecified inclusion criteria? | 5. Rationale for sample size. description of the power or variance/effect estimators? | 8. Clear definition of exposure (independent variable)? | 9. Consistency of exposure across all participants? | 11. Clearly defined. valid. reliable. and consistently used outcome measure across all participants? | Quality assessment | Comments |
| General population | ||||||||||
| Cao et al. (e16) |
Y | Y | Y | Y | N | Y | n. r. | Y | ++ | (b). (c) |
| Liu et al. (e7) |
Y | N | n. a. | Y | N | Y | Y | Y | + | (a). (e) |
| Qiu et al. (e4) |
Y | Y | n. a. | n. r. | N | Y | Y | N | + | (a). (d) |
| Roy et al. (e17) |
Y | N | n. a. | Y | N | Y | Y | N | + | (a). (d) |
| Wang C et al. (16) |
Y | Y | n. a. | Y | N | Y | Y | Y | ++ | (a) |
| Wang. Y et al. (e18) |
Y | Y | n. a. | Y | N | Y | Y | Y | ++ | (a). (e) |
| Zhang Y et al. (e19) |
Y | Y | Y | Y | N | Y | Y | Y | ++ | (a) |
| Healthcare workers | ||||||||||
| Cai et al. (e1) |
Y | Y | n. r. | n. r. | N | Y | n. r. | N | + | (a). (b). (d) |
| Huang JZ et al. (e9) |
Y | Y | Y | Y | N | Y | Y | Y | +++ | |
| Kang et al. (e20) |
Y | Y | n. r. | n. r. | N | Y | Y | Y | + | (a). (f) |
| Lai et al. (6) |
Y | Y | Y | Y | Y | Y | Y | Y | +++ | |
| Mo et al. (e2) |
Y | Y | Y | n. r. | N | Y | n. r. | Y | + | (a). (b) |
| Xiao et al. (e3) |
Y | Y | Y | n. r. | N | Y | n. r. | Y | + | (b). (c) |
| Mixed groups | ||||||||||
| Huang Y et al. (e6) |
Y | Y | n. a. | Y | N | Y | Y | Y | ++ | (a) |
| Li et al. (e8) |
Y | N | n .a. | Y | N | Y | Y | N | + | (c). (e) |
| Lu et al. (e21) |
Y | Y | Y | Y | N | Y | Y | Y | +++ | |
| Yuan et al. (e22) |
Y | N | n. r. | n. r. | N | Y | Y | N | + | (b). (c). (e) |
| Zhang W et al. (e23) |
Y | Y | n. a. | Y | N | Y | Y | Y | ++ | (a). (c) |
+: Poor; ++: fair; +++: good; Y. yes; N. no; n. a.. not applicable; n. r.. not reported
(a) Selection bias/possible selection bias due to insufficient description of data collection
(b) No/insufficient details on the survey period
(c) No data on cut-off values and/or scale span to measure outcome(s)
(d) No validated method of measuring outcome(s)
(e) Insufficient description of the sample
(f) Insufficient reasoning given for the summary of outcomes
General population
Of the seven general population-based studies and the five conducted in mixed-population groups, seven studies (n = 16 113) reported data on the point prevalence of anxiety symptoms (1–82% of respondents), while five studies (n = 8308) recorded the prevalence of depressive symptoms (3–20%). Three studies (n = 1758) reported data on the presence of posttraumatic stress symptoms among study participants as percentages (7–54%), while three studies (n = 6903) reported on sleep disorders (13–31% of participants). One study (n = 1210) reported increased symptoms of stress in 8% of respondents. None of the studies recorded suicidal tendency. Prevalence figures were determined using the reported cut-off value for each study and instrument (etable 2).
Only two studies performed comparisons of the frequency of psychopathological symptoms with norm values in the general Chinese population before the outbreak of the SARS-CoV-2 pandemic (i.e., prior to 20.01.2020, since this is the date on which human-to-human transmission became known [e5]) and in the absence of effects from other epidemic events. One of these studies showed increased levels of anxiety (an approximately seven-fold higher prevalence: 35.1 versus 5% [e6]) and increased levels of depression (a more than five-fold higher prevalence: 20.3 versus 3.6% [e6]), while another study showed increased posttraumatic stress symptoms (an almost two-fold higher prevalence: 7% versus 3.7% [e7]).
Healthcare workers
Of the six studies that investigated only healthcare workers and the five that studied the subgroup of healthcare workers as well as mixed population groups, seven studies (n = 8234) reported on the point prevalence of anxiety symptoms (13–70% of healthcare workers) and five studies (n = 7470) on the prevalence of depressive symptoms (12–50%). Three studies (n = 2481) reported data on the presence of posttraumatic stress symptoms among study participants as percentages (27–72 %), while four studies (n = 5428) reported on sleep disorders (24–38% of participants). One study (n = 927) reported symptoms of stress in 22% of respondents. Prevalence figures were determined using the reported cut-off value for each study and instrument (etable 2).
Only two studies compared the frequency of psychopathological symptoms (anxiety and sleep disorders, respectively) with norm values in the general population (comparisons with healthcare workers before the current SARS-CoV-2 pandemic were not available). One study revealed statistically but not clinically relevant levels of anxiety (mean value of the Self-Rating Anxiety Scale (SAS, scale span not given) 32.19 ± 7.56 versus 29.78 ± 0.46; t = 4.27; p ≪0.001 [e2]), while the other showed only a slight increase in sleep-related symptoms (mean value in the Pittsburgh Sleep Quality Index (PSQI, scale span 0–21) 8.583 ± 4.567 versus 7 (standard deviation not reported, [e3]).
Table 3 and eTable 4 provide a summary of the protective factors and risk factors for psychomorbidity due to the COVID-19 pandemic from the 19 studies. Most studies identified the following parameters as risk factors:
Table 3. Risk factors and protective factors for psychomorbidity in the SARS-CoV-2 pandemic.
| Demographic variables | Occupational and workplace-related variables |
Personal variables |
Pandemic-specific variables | Information-/ communicationrelated variables | Disease-related variables | |
| Risk factors | ||||||
| Anxiety | Students (16); female sex (6, 18, e23); age >40 (e18); healthcare profession (e21, e23); married (e23) | Concern about academic disadvantages (e16); working in a secondary care hospital* (6); intermediate professional status (6); direct patient contact (6); high-risk contact (e21) | No confidence in their doctor's ability to diagnose/recognize COVID-19 (16) | Infection of loved ones (e16); concerns about economic effects (e16); concerns about children (16); risk of contact with COVID-19 patients (e23) | n. a. | Physician visits (16); hospital stays (16); poor self-rated health status (16); chronic diseases (16); organic diseases (e23) |
| Depression | Low educational level (16); age <35 (e6); nursing profession (6); female sex (6); healthcare profession (e23); rural areas (e23) | Working in a secondary care hospital* (6); intermediate professional status (6); direct patient contact (6); high-risk contact (e21) | No confidence in their doctor's ability to diagnose/recognize COVID-19 (16); living with family (e23) | Healthcare profession. >3 h/day thinking about COVID-19 (e6) | Dissatisfaction with amount of health information (16) | Poor self-rated health status (16); chronic diseases (16); organic diseases (e23) |
| PTSS | Female sex (e7) | n. a. | Poor sleep quality (e7); sleep latency (e7) | Concerns about children (16); contact with people with suspected COVID-19 (16); general population/nursing staff not in direct contact with COVID-19 (e8) | Dissatisfaction with amount of health information (16) | High-risk population for COVID-19 (e7); respiratory symptoms (16); chronic diseases (16) |
| Sleep disorders | Healthcare profession (e6, e23); rural areas (e23) | Direct patient contact (6) | Living with family (e23) | Healthcare profession + >3 h/day thinking about COVID-19 (e23) | n. a. | Organic diseases (e23) |
| Psychological distress in general | Female sex (e4); participants from Hubei (e4) | Migrant workers (e4) | n. a. | Exposure to COVID-19 (e20) | n. a. | n. a. |
| Stress | Students (16); female sex (6) | Intermediate professional status (6); direct patient contact (6); workload (e9); high professional qualification (e9); severity of patient condition (e9) | No confidence in their doctor's ability to diagnose/recognize COVID-19 (16); poor sleep quality (e2) | Concerns about the family (16, e1) | Dissatisfaction with amount of health information (16) | Poor self-rated health status (16); chronic diseases (16) |
| Protective factors | ||||||
| Factors for fear | Large city (e16); male sex (e9); medical profession (e9) | Social support (e3, e16) | Low professional status (e9) | Stable income (e16); living with parents (e16); precautionary/hygiene measures (16) | Low perceived risk of infection (16) | n. a. |
| Depression | n. a. | n. a. | n. a. | Precautionary/hygiene measures (16) | n. a. | Information on rise in recovery numbers (16) |
| PTSS | Not currently/previously in Wuhan (e7); male sex (16, e9) | n. a. | n. a. | Precautionary/hygiene measures (16); resting (e19) | n. a. | n. a. |
| Sleep disorders | n. a. | Self-efficacy (e3) | n. a. | n. a. | n. a. | n. a. |
| Psychological distress in general | Age <18 (e4) | n. a. | n. a. | n. a. | Use of psychoeducational materials (e20) | n. a. |
| Stress | Working outside Hubei (6); siblings (e2) | Social support (e3) | n. a. | Precautionary/hygiene measures (16) | Low perceived risk of infection (16) | Information on rise in recovery numbers (16) |
*Medium-sized hospital providing interregional care; n. a.: not available; PTSS. posttraumatic stress symptoms
eTable 4. Statistical information on risk factors and protective factors.
| Moderating factors | ||
| Significant | Non-significant | |
| General Population | ||
| Cao et al. (2020) (e16) |
For anxiety: (+) infection in loved ones (logistic regression; OR = 3.007; 95%-CI = 2.377 - 3.804; p<0.001) (+) concerns about economic impact of the epidemic (correlation analysis; r= 0.327; p < 0.001); (+) concerns about academic delays (correlation analysis; r = 0.315; p < 0.001); (+) influence of the epidemic on daily life (correlation analysis; r = 0.316; p < 0.001); (–) stability of family income (logistic regression; OR = 0.726; 95% CI = 0.645 - 0.817; p < 0.001); (–) living in a large city (logistic regression; OR = 0.810; 95% CI = 0.709 - 0.925; p=0.002); (–) living with parents (logistic regression; OR = 0.752; 95% CI = 0.596 - 0.950; p=0.017); (–) social support (correlation analysis; r = –0.151; p < 0.001) |
For anxiety: (0) region (Hubei/ north/south; univariate analysis; Kruskal-Wallis test: H=0.292; p= 0.864) (0) sex (univariate analysis; M comparison (Mann-Whitney U test): U=–0.805; p=0.421); (0) rural-urban residence (logistic regression: OR = 0.928; 95%-CI 0.803- 1.073; p= 0.310) |
| Liu et al. (2020) (e7) |
For posttraumatic stress symptoms: (+) female sex (f vs. m; hierarchical regression, step 2: β = 0.192; p< 0.001); (–) male sex (f. criterion B symptoms; m vs. w; Mann-Whitney U-test: U= –4.209; p<0.001); (–) male sex (f. Criterion D symptoms; m vs. w; Mann-Whitney U-test: U=–1.994; p<0.05); (–) male sex (f. Criterion E symptoms; m vs. w; Mann-Whitney U-test: U=–2.273; p<0.05) (–) no current stay in Wuhan (t-test: t= –2.210 p=0.028); (–) no previous stay in Wuhan (t-test: t= –2.077 p=0.039); (+) risk groups (general population/ HCW/near contact/ confirmed or suspected COVID-19 cases; hierarchical regression: β =0.153; P < 0.01); (+) poor subjective sleep quality (hierarchical regression; β= 0.312; p < 0.001); (+) sleep latency (hierarchical regression: β = 0.172; p < 0,01); |
For posttraumatic stress symptoms: (0) age (t-test: F/t =–0,924; p=0,356); (0) education level (t-test: F/t= 1.553; p=0.213) (0) sex (f. Criterion C symptoms; m vs. w; Mann-Whitney U test: U= –1.488; =0.112) |
| Qiu et al. (2020) (e4) |
For PCDI: (+) female sex (vs. male; Whitney-Mann test (M ±SD comparison): 24.87± 15.03 vs. 21.41±15.97; p<0.001); (–) age < 18 (m ±sd: 14.83±13.41 vs. 18-30 years 27.76±15.69 vs. >60 years 27.49±24.22); (0) education (n/a); (+) Migrant workers (PCDI-M±SD=31.89±23.51; F=1602.501; p<0.001); (+) participants from Hubei (PCDI-M ±SD: 30.94 (19.22), F=929.306; p<0.001); (0) Availability of local medical resources(NR); (0) Efficiency of the regional public health system (NR); (0) Prevention and control measures (NR) |
NR |
| Roy et al. (2020) (e17) | NR | NR |
| Wang, C. et al. (2020) (16) |
For posttraumatic stress symptoms: -regarding IES-R: (–) male sex (logistic regression: β =–0.20; 95%-CI –0.35 - –0.05; p<0.05); (+) students (logistic regression: β =0.20; 95%-CI 0.05-0.35; p<0.05); (–) highest education level: primary school (vs. doctorate; logistic; logistic regression: β =–1.07; 95%-CI –2.09- –0.06; p<0.05) (+) respiratory symptoms (e.g. rhinitis; logistic regression: β = 0.39; 0.20-0.58; p<0.001) (+) chronic diseases (logistic regression: β =0.29; 95%-CI 0.01-0.58; p<0.05); (+) discontent with the information available on COVID-19 (logistic regression: β =0.63; 95%-CI: 0.11-1.14; p<0.05); (+) concerns about children (logistic regression: β =0.25; 95%-CI 0.05-0.44; p<0.05); (–) hygiene behavior (e.g. washing hands after coughing; β = –0.47; 95%-CI: –0.77- –0.17; p<0.05); (–) feeling that too many unnecessary worries about COVID-19 are being worried about (always vs. never; logistic regression: β =–0.47; 95%-CI –0.69-0.25; p>0.05); (+) need for information on COVID-19 (e.g. recommendations for prevention; β =0.52; 95%-CI 0.23-0.81; p<0.001); for stress: -regarding DASS-21 stress subscale: (+) male sex (logistic regression: β = 0.10; 95%-CI: 0.02-0.19); (+) students (logistic regression: β = 0.11; 95%-CI: 0.02-0.19); (+) respiratory symptoms; (+) reduced perceived health (logistic regression: β = 0.45; 95%-CI: 0.02-0.88; p<0.05); (+) chronic diseases (logistic regression: β = 0.24; 95%-CI 0.07-0.41; p<0.01); (+) discontent with information on COVID-19 (logistic regression: β = 0.32; 95%-CI: 0.02-0.62; p<0.05) (-) Information on the increase in the number of people cured (logistic regression: β=–0.24; 95%-CI: –0.40-0.07; p<0.01) (+) no confidence in the doctor (logistic regression: β =1.18; 95%-CI 0.61-1.75; p<0.001); (–) low perceived risk of infection (logistic regression: β = –0.18; 95%-CI: –0.35- –0.01; p<0.05) (+) high perceived risk of death in case of infection (probable/very probable; logistic regression: β (95%-CI) =0.18 (0.02-0.34)/0.34 (0.01-0.68); p<0.05); (+) worries about family (logistic regression: β =0.50; 95%-CI 0.04- 0.96); (–) hygiene behavior (e.g. washing hands after coughing; logistic regression: β =–0.31; 95%-CI –0.49 - –0.13; p<0.05), for anxiety: (+) male sex (logistic regression: β = 0.19; 95%-CI: 0.05-0.33); (+) students (logistic regression: β = 0.16; 95%-CI: 0.02-0.30) (+) respiratory symptoms (e.g. rhinitis symptoms; logistic regression: β =0.46; 95%-CI 0.28-0.63; p<0.001); (+) visits to a doctor (in a hospital in the last 14d; logistic regression: β =0.38; 95%-CI: 0.02- 0.73); (+) hospital stays (in a hospital in the last 14d; logistic regression: β = 1.23; 95%-CI: 0.09-2.36) (+) reduced perceived health (logistic regression: β =0.90; 95%-CI:0.2-1.58) (+) chronic diseases (logistic regression: β =0.48; 95%-CI 0.22-0.75; p<0.001) (+) contact to person with mainly COVID-19 or infected materials (logistic regression: β=0.98; 95%-CI: 0.32-1.64; p<0.01); (+) Information source radio (logistic regression: β =2.67; 95%-CI 0.22-5.11; p<0.05); (+) no confidence in the doctor (logistic regression: β=1.86; 95%-CI 0.96-2.76; p<0.001); (–) low perceived risk of infection (logistic regression: β=–0.36; 95%-CI –0.63-–0.09; p<0.05) (+) worries about children (logistic regression: β=0.24; 95%-CI 0.07- 0.42; p<0.01); (–) hygiene behaviour (e.g. washing hands after coughing; logistic regression: β =–0.63; 95%-CI –0.91- –0.35; p<0.001); (–) need for regular updates on the current situation regarding COVID-19 (logistic regression: β =–0.62; 95%-CI –1.00-–0.24; p<0.01); (–) need for information on the availability and effectiveness of drugs and vaccinations against COVID-19 (logistic regression: β =–0.63; 95%-CI –0.99-–0.26; p<0.01); (–) need for up-to-date information on the number of infected persons and their stay (logistic regression: β =–0.30; 95%-CI –0.57-–0.02; p<0.01); (–) need for updates on transmission routes of COVID-19 (logistic regression: β =–0.39; 95%-CI –0.77-–0.02); p<0.05) for depressive symptoms: (+) male sex (logistic regression: β = 0.12; 95%-CI 0.01-0.23); (+) low education level (no degree vs. doctorate; logistic regression: β = 1.81; 95%-CI: 0.46-3.16; p<0.001); (+) respiratory symptoms (e.g. persistent fever: β = 0.98; 95%-CI 0.23-1.72; p<0.05) (+) reduced perceived health (poor or very poor/ average vs. good or very good; logistic regression: β (95%-CI)=0.65 (0.10-1.20); p<0.05/ 0.26 (0.15-0.38); p<0.001); (+) chronic diseases (logistic regression: β =0.38; 0.17-0.59; p<0.001) (+) close contact with confirmed COVID-19 patient (logistic regression: β =0.97; 95%-CI 0.06-1.88; p>0.05); (+) close contact with person with mainly COVID-19 or infected materials (logistic regression: β =0.81; 95%-CI 0.29-1.34; p<0.01) (+) discontent with information about COVID-19 (logistic regression: β = 0.43; 95%-CI 0.04-0.81; p<0.05); (-) information about increase in number of cured patients (logistic regression: β =-0.24; 95%-CI -0.45 --0.03; p<0.05); (+) information source radio (logistic regression: β = 2.67; 95%-CI 0.70-4.63; p<0.01); (+) no confidence in the doctor (logistic regression: β = 1.66; 95%-CI 0.94-2.38; p<0.001); (+) high perceived risk of death (vs. I don't know; logistic regression: β = 0.49; 95%-CI 0.07-0.92; p>0.05); (-) hygiene behavior (e.g. avoidance of sharing chopsticks; logistic regression: β =-0.31; 95%-CI -0.46--0.15; p<0.001); (+) feeling that too many unnecessary worries are being made about COVID-19 (mostly vs. never; logistic regression: β =0.20; 95%-CI 0.003-0.39; p<0.05); (-) need for information on availability and effectiveness of drugs and vaccinations against COVID-19 (logistic regression: β =-0.35; 95%-CI -0.65--0.06; p>0.05); |
For posttraumatic stress symptoms: -regarding IES-R: (0) age (12-21.4/ 21.4-30.8/30.8-40.2/40.2-49.6 vs. 49.6-59 years; logistic regression: β (95%-CI)= 0.21 (–0.20 -0.62)/ 0.09 (–0.31-0.50)/ -0.17 (–0.64-0.29)/ –0.16 (–0.63- 0.30); p>0.05); (0) parenthood (child <17/ >17 years vs. no child; logistic regression: β (95%-CI) =0.04(–0.16-0.25)/ –0.06(–0.22-0.10); p>0.05); (0) marital status (single/ married/ divorced or separated vs. widowed; logistic regression: β (95%-CI)= –0.04 (–1.46-1.38)/ 0.09(–1.33-1.50)/ 0.11 (–1.52-1.74); p=0.05); (0) household size (>5/ 3-5/ 2 vs. 1 person; logistic regression: β (95%-CI)= 0.38 (–0.39-1.14)/ 0.25 (–0.49-0.99)/ 0.41 (–0.40-1.22); p>0.05); (0) employment (unemployed/farmers/retired vs. employed; logistic regression: β (95%-CI)=0.13 (–0.19-0.45)/ –0.08 (–0.59-0.43)/ –0.76 (–1.69-0.17); p>0.05); (0) highest education level (none / lower secondary school/ upper secondary school/ bachelor/master vs. doctorate; logistic regression: β (95%-CI)= –0.07 (-1.88-1.74)/ 0.21 (–0.42-0.84)/ 0.01 (–0.59-0.61)/ 0.19 (–0.35-0.73)/ 0.14 (–0.42-0.69); p>0.05); (0) persistent fever (>38°C≥1d; logistic regression: β =–0.23; 95%-CI –1.23-0.78; p>0.05); (0) respiratory symptoms (logistic regression: β =0.88; –0.22-1.97; p>0.05); (0) fever + cough or breathing problems (logistic regression: β =–0.23; 95%-CI –1.45-1.00; p>0.05); (0) visit to a hospital during the last 14d (logistic regression: β =–0.06 95%-CI –0.44-0.32; p>0.05) (0) hospitalization in the last 14d (logistic regression: β =0.78; –0.45-2.00; p>0.05); (0) SARS-CoV-2 test in the last 14d (logistic regression: β =–0.18; 95%-CI –0.92-0.56; p>0.05) (0) quarantine in the last 14d (logistic regression: β =0.32; 95%-CI –0.16-0.81; p>0.05); (0) health insurance coverage (logistic regression: β =0.09; 95%-CI –0.18-0.36; p>0.05); (0) close contact with confirmed COVID-19 patient (logistic regression: β =0.53; 95%-CI –0.70-1.75; p>0.05) (0) indirect contact with confirmed COVID-19 patient (logistic regression: β =–0.06; 95%-CI –1.06-0.94) (0) contact with suspected SARS-CoV-2 infected or infected materials (logistic regression: β =0.36; 95%-CI –0.35-1.07; p>0.05); (0) knowledge about COVID-19 (e.g. on transmission path; logistic regression: β = 0.21; 95%-CI –0.07-0.49; p>0.05); (0) source of information (internet/ television/ radio/ family vs. others; logistic regression: β (95%-CI)= –0.46(–1.46-0.54)/ –0.22 (–1.26-0.83)/ 0.83 (–1.81-3.47)/ –0.47 (–1.73-0.80); p>0.05); (0) satisfaction with the information situation on COVID-19 (very satisfied vs. I don't know; logistic regression: β =0.02; 95%-CI –0.34-0.37; p>0.05); (0) trust in the doctor (very satisfied/ somewhat satisfied/ not very satisfied/ not at all satisfied vs. I don't know; logistic regression: β (95%-CI)= –0.2 (–0.66-0.27)/ 0.19 (–0.28-0.66)/ 0.19 (–0.39-0.76)/ 0.66 (–0.31-1.63); p>0.05); (0) low perceived risk of infection (logistic regression: β =–0.23; 95%-CI (–0.52-0.06); p>0.05) (0) perceived risk of death in case of infection (not at all probable/ not very probable/ somewhat probable/ very probable vs. I don't know; logistic regression: β (95%-CI)=-0.19 (–0.41-0.03)/ 0.12 (–0.07-0.31)/ 0.23 (–0.04-0.50)/ 0.42 (–0.15-0.99); p>0.05); (0) worries about family (very worried/ somewhat worried/ not very worried/ not worried at all vs. no families; logistic regression: β (95%-CI)= 0.75 (–0.03-1.53)/ 0.67 (–0.10-1.45)/ 0.44 (–0.34-1.23)/ 0.19 (–0.64-1.01); p>0.05); (0) no worries about children (logistic regression: β =–0.02; 95%-CI –0.30-0.26; p>0.05); (0) covering mouth when coughing and sneezing (always vs. never; logistic regression: β =0.02; 95%-CI –0.34-0.37; p>0.05); (0) washing hands with soap and water (always/ most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.42 (–0.85-0.01)/ –0.12 (–0.56-0.33)/ 0.07 (–0.40-0.54)/ 0.13 (–0.35-0.62); p>0.05); (0) mask wearing independently of symptoms (always/mostly/ sometimes vs. never; logistic regression: β (95%-CI)= –0.19 (–0.59-0.21)/ 0.12 (–0.30-0.53)/ 0.16 (–0.29-0.61); p>0.05); (0) washing hands after touching contaminated objects (always/ most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI) =–0.11 (–0.69-0.47)/ 0.19 (–0.40-0.78)/ 0.40 (–0.25-1.04)/ 0.31 (–0.39-1.00); p>0.05); (0) feeling that too many unnecessary worries about COVID-19 are being made (sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.19 (–0.44-0.07)/ -0.03 (–0.21-0.16)/ 0.13 (–0.09-0.34); p>0.05) (0) time spent at home to avoid COVID-19 (0-9/ 10-19 vs. 20-24; logistic regression: β (95%-CI)= –0.15 (–0.55-0.25)/ 0.11 (–0.10-0.33); p>0.05); (0) need for regular updates on the current situation regarding COVID-19 (logistic regression: β =–0.11; 95%-CI -0.35-0.13); (0) need for up-to-date information on local COVID 19 outbreaks (logistic regression: β =0.06; 95%-CI –0.21-0.33; p>0.05); (0) need for recommendations for special groups, e.g. pre-existing conditions (logistic regression: β =0.19; 95%-CI –0.21-0.59; p>0.05); (0) need for information on the availability and effectiveness of drugs Vaccinations for COVID-19 (logistic regression: β =0.16>; 95%-CI –0.40-0.07; p>0.05) (0) need for up-to-date information on the number of infected persons and their stay (logistic regression: β =–0.09; 95%-CI –0.27-0.08; p>0.05); (0) need for travel recommendations (logistic regression: β =0.07; 95%-CI –0.29-0.42; p>0.05); (0) need for updates on transmission paths (logistic regression: β =0.15; 95%-CI –0.25-0.55; p>0.005); (0) need for updates on the approach of other countries to the COVID 19 outbreak (logistic regression: β =0.25; 95%-CI –0.06-0.56; p>0.05) for stress: -regarding DASS-21 stress subscale: (0) age (12-21.4/ 21.4-30.8/30.8-40.2/40.2-49.6 vs. 49.6-59 years; logistic regression: β (95%-CI)=0.08 (–0.16-0.32)/ 0.12 (–0.12-0.36)/ –0.07 (–0.35-0.20)/ –0.12 (–0.39-0.16); p>0.05); (0) parenthood (child <17/ >17 years vs. no child; logistic regression: β (95%-CI)= –0.02 (–0.14-0.10)/ –0.07 (–0.17-0.02); p>0.05); (0) marital status (single/ married/ divorced or separated vs. widowed; logistic regression: β (95%-CI)=0.02 (–0.81-0.86)/ 0.12 (–0.71-0.96)/ <0.001 (–0.96-0.96); p>0.05); (0) household size (>5/ 3-5/ 2 vs. 1 person; logistic regression: β (95%-CI)= –0.23 (–0.68-0.22)/ –0.20 (–0.63-0.24)/ –0.33 (–0.81-0.15); p>0.05); (0) employment (unemployed/farmers/retired vs. employed; logistic regression: β (95%-CI)=0.12 (–0.07-0.31)/ 0.003 (–0.30-0.30)/ –0.37 (–0.92-0.18); p>0.05); (0) highest educational level (none / primary school / lower secondary school / upper secondary school / bachelor / master vs. PhD; logistic regression: β (95%-CI)= 0.76 (–0.30-1.83)/ –0.11 (–0.71-0.49)/ 0.20 (–0.17-0.57)/ 0.16 (–0.20-0.51)/ 0.21 (–0.11-0.53); 0.18 (–0.15-0.51); p>0.05); (0) persistent fever (>38°C≥1d; logistic regression: β=0.40; 95%-CI –0.19-0.99; p>0.05); (0) headache (logistic regression: β=0.12; 95%-CI –0.02-0.26; p>0.05); (0) breathing problems (logistic regression: β=0.57; 95%-CI –0.07-1.22; p>0.05); (0) fever + cough or breathing problems (logistic regression: β=0.32; 95%-CI –0.40-1.04; p>0.05); (0) visit to a hospital in the last 14d (logistic regression: β=0.17; 95%-CI –0.06-0.40; p>0.05); (0) hospitalization in the last 14d (logistic regression: β=0.32; 95%-CI –0.40-1.04; p>0.05); (0) SARS-CoV-2 test in the last 14d (logistic regression: β=–0.07; 95%-CI –0.51-0.37; p>0.05) (0) quarantine in the last 14d (logistic regression: β=–0.01; 95%-CI –0.30-0.28 p>0.05); (0) health insurance coverage (logistic regression: β=–0.003; 95%-CI –0.16-0.15; p>0.05); (0) close contact with confirmed COVID-19 patient (logistic regression: β=0.32; 95%-CI –0.40-1.04; p>0.05) (0) indirect contact with confirmed COVID-19 patients (logistic regression: β=–0.27; 95%-CI –0.86-0.32; p>0.05); (0) contact with suspected SARS-CoV-2 infected or infected materials (logistic regression: β=0.41; 95%-CI –0.01-0.82; p>0.05); (0) knowledge of COVID-19 (e.g. on transmission path; logistic regression: β=0.15; 95%-CI –0.01-0.32; p>0.05); (0) source of information (Internet/ television/ radio/ family vs. others; logistic regression: β(95%-CI)= –0.25 (–0.83-0.34)/ –0.07 (–0.68-0.54)/ 1.33 (–0.22-2.89)/ –0.27 (–1.01-0.48); p>0.05); (0) satisfaction with the information situation about COVID-19 (very satisfied vs. I don't know; logistic regression: β=–0.09; 95%-CI –0.30-0.13; p>0.05); (0) trust in the doctor (very satisfied/ somewhat satisfied/ not very satisfied vs. I don't know; logistic regression: β (95%-CI)=0.05 (–0.23-0.32)/ 0.16 (–0.12-0.44)/ 0.18 (–0.16-0.52); p>0.05); (0) high perceived risk of infection (logistic regression: β=0.05; 95%-CI –0.11-0.22; p>0.05); (0) perceived risk of death in case of infection (not probable/ not very probable vs. I don't know; logistic regression: β (95%-CI)= –0.02 (–0.15-0.11)/ 0.01 (–0.10-0.13); p>0.05); (0) medium-low worries about family (somewhat worried/ not very worried/ not worried at all vs. no families; logistic regression: β (95%-CI)= 0.40 (–0.05-0.86)/ 0.43 (–0.04-0.89)/ 0.33 (–0.16-0.81); p>0.05); (0) worries about children (very worried/ somewhat worried/ not very worried/ not worried at all vs. no children; logistic regression: β (95%-CI)=0.05 (–0.07-0.16)/ 0.03 (–0.09-0.14)/ 0.04 (–0.10-0.18)/ 0.004 (–0.16-0.17); p>0.05); (0) covering mouth when coughing and sneezing (always/mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)=0.02 (–0.19-0.23)/ 0.09 (–0.13-0.31)/ 0.12 (–0.13-0.36); –0.03 (–0.29-0.23); p>0.05); (0) washing hands with soap and water (sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.22 (–0.50-0.07)/ –0.17 (–0.46-0.12); p>0.05) (0) washing hands directly after coughing, sneezing (mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.17 (–0.36-0.02)/ –0.12 (–0.32-0.07)/ –0.08 (–0.28-0.12); p>0.05); (0) mask wearing independently of symptoms (always/mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.21 (–0.45-0.02)/ –0.09 (–0.34-0.16)/ –0.08 (–0.35-0.19)/ –0.04 (–0.33-0.24); p>0.05); (0) washing hands after touching contaminated objects (always/ mostly/ sometimes/ occasionally vs. never; logistic regression: β=–0.21 (–0.56-0.13)/ –0.15 (–0.49-0.21)/ –0.01 (–0.39-0.38)/ –0.07 (–0.48-0.34); p>0.05); (0) feeling that too many unnecessary worries about COVID-19 are being made (always/ mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.08 (–0.21-0.05)/ –0.05 (–0.20-0.11)/ –0.01 (–0.12-0.10)/ 0.03 (–0.10-0.16); p>0.05); (0) time spent at home to avoid COVID-19 (0-9/ 10-19 vs. 20-24; logistic regression: β (95%-CI)= –0.16 (-0.39-0.08)/ -0.03 (-0.16-0.10); p>0.05); (0) need for details on COVID-19 symptoms (logistic regression: β=-0.02; 95%-CI -0.17-0.13; p>0.05); (0) need for recommendations on prevention (logistic regression: β=0.11; 95%-CI -0.06-0.28; p>0.05); (0) need for recommendations on treatment of COVID-19 (logistic regression: B=0.03; 95%-CI -0.08-0.14; p>0.05) (0) need for regular updates on the current situation regarding COVID-19 (logistic regression: β=–0.11; 95%-CI –0.35-0.13; p>0.05); (0) need for up-to-date information on local COVID-19 outbreaks (logistic regression: β=0.01; 95%-CI –0.15-0.17; p>0.05); (0) need for recommendations for special groups, e.g. pre-existing conditions (logistic regression: β=0.004; 95%-CI –0.17-0.17; p>0.05) (0) need for information on the availability and effectiveness of drugs Vaccinations for COVID-19 (logistic regression: β=–0.16; 95%-CI –0.40-0.07; p>0.05) (0) need for up-to-date information on the number of infected persons and their stay (logistic regression: β=–0.09; 95%-CI –0.27-0.08; p>0.05); (0) need for travel recommendations (logistic regression: β=–0.07; 95%-CI –0.28-0.14; p>0.05) (0) need for updates on transmission paths (logistic regression: β=–0.10; 95%-CI –0.33-0.14; p>0.05); (0) need for updates on other countries' approach to the COVID 19 outbreak (logistic regression: β=–0.008; 95%-CI –0.19-0.18; p>0.05); for anxiety: (0) age (12-21.4/ 21.4-30.8/30.8-40.2/40.2-49.6 vs. 49.6-59 years; logistic regression: β (95%-CI)=0.10 (–0.28-0.48)/ 0.07 (–0.31-0.44)/ –0.16 (–0.59-0.27)/ –0.23 (–0.67-0.20); p>0.05); (0) parenthood (child <17/ >17 years vs. no child; logistic regression: β (95%-CI)= 0.08 (–0.11-0.27); p>0.05); (0) marital status (single/ married/ divorced or separated vs. widowed; logistic regression: β (95%-CI)=0.71 (–0.61-2.03)/ 0.80 (–0.51-2.12)/ 0.44 (–1.07-1.96); p>0.05); (0) household size (>5/ 3-5/ 2 vs. 1 person; logistic regression: β (95%-CI)= –0.17 (–0.87-0.54)/ –0.12 (–0.81-0.57)/ –0.18 (–0.93-0.58); p>0.05); (0) employment (unemployed /farmers/retired vs. employed; logistic regression: β (95%-CI)=0.21 (–0.09-0.51)/0.07 (–0.41-0.54)/ –0.54 (–1.41-0.32); p>0.05); (0) highest educational level (none / primary school / lower secondary school / upper secondary school / bachelor / master vs. PhD; logistic regression: β (95%-CI)= 1.02 (–0.66-2.71)/ –0.10 (–1.05-0.84)/ 0.38 (–0.21-0.96)/ 0.36 (–0.19-0.92)/ 0.32 (–0.18-0.82)/ 0.24 (–0.28-0.76); p>0.05); (0) fever + cough or breathing problems (logistic regression: β=0.98; 95%-CI –0.16-2.11; p>0.05); (0) SARS-CoV-2 test in the last 14d (logistic regression: β=0.22; 95%-CI –0.47- 0.91; p>0.05) (0) quarantine in the last 14d (logistic regression: β=0.03; 95%-CI –0.42-0.48; p>0.05); (0) health insurance coverage (logistic regression: β=–0.04; 95%-CI –0.29-0.21; p>0.05); (0) close contact with confirmed COVID-19 patient (logistic regression: β=0.98; 95%-CI –0.16-2.11; p>0.05) (0) indirect contact with confirmed COVID-19 patient (logistic regression: β= –0.28; 95%-CI –1.21-0.65; p>0.05) (0) knowledge of COVID-19 (e.g. on transmission path; logistic regression: β=0,17 (–0.09-0.43); p>0.05); (0) information on increase in number of cured people (logistic regression: β= –0.25; 95%-CI –0.51-0.01; p>0.05); (0) information source (Internet/TV/family vs. others; logistic regression: β(95%-CI)= –0.57 (–1.50-0.35/ –0.35 (–1.32-0.62)/ –0.33 (–1.50-0.84); p>0.05); (0) satisfaction with the information situation about COVID-19 (very satisfied/ somewhat satisfied/ not very satisfied/ not at all satisfied vs. I don't know; logistic regression: β (95%-CI)= –0.20 (–0.53-0.14)/ –0.02 (–0.36-0.31)/ 0.05 (–0.31-0.40)/ 0.41 (–0.07-0.88); p>0.05) (0) trust in the doctor (very satisfied/ somewhat satisfied/ not very satisfied vs. I don't know; logistic regression: β (95%-CI)=0.02 (–0.42-0.45)/ 0.22 (–0.22-0.65)/ 0.38 (–0.15-0.91); p>0.05); (0) high perceived risk of infection (very high/ high/ not very high; logistic regression: β=0.07 (–0.20-0.33)/ –0.02 (–0.23-0.20)/ –0.05 (–0.26-0.16); p>0.05); (0) perceived risk of death in case of infection (not at all probable/ not very probable/ somewhat probable/ very probable vs. I don't know; logistic regression: β (95%-CI)= –0.06 (–0.27-0.14)/ –0.03 (–0.21-0.15)/ 0.18 (–0.08-0.43)/ 0.42 (–0.11-0.95); p>0.05); (0) worries about family (very worried/ somewhat worried/ not very worried/ not worried at all vs. no family; logistic regression: β (95%-CI)= 0.59 (–0.13-1.32)/ 0.43 (–0.30-1.15)/ 0.44 (–0.30-1.15)/ 0.36 (–0.41-1.13); p>0.05); (0) few concerns about children (not very concerned/ not concerned at all vs. no children; logistic regression: β (95%-CI)=0.21 (–0.01-0.43)/0.14 (–0.12-0.40); p>0.05); (0) covering mouth when coughing and sneezing (always/mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.19 (–0.52-0.14)/ –0.09 (–0.43-0.26)/ 0.09 (–0.30-0.47)/ –0.32 (–0.73-0.09); p>0.05); (0) avoid sharing chopsticks (mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.03 (–0.26-0.19)/ –0.13 (–0.37-0.11)/ –0.14 (–0.38-0.11); p>0.05); (0) washing hands with soap and water (mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.40 (–0.81-0.02)/ –0.23 (–0.67-0.21)/ –0.21 (–0.67-0.21)/ –0.21 (–0.67-0.24); p>0.05); (0) occasional hand washing directly after coughing, sneezing, sniffing (vs. never; logistic regression: β=–0.29; 95%-CI –0.60-0.02; p>0.05); (0) mask wearing independently of symptoms (most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.27 (–0.66-0.12)/ –0.25 (–0.67-0.17)/ –0.14 (–0.60-0.31); p>0.05); (0) washing hands after touching contaminated objects (always/ mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.52 (–1.06-0.02)/ –0.37 (–0.92-0.18)/ –0.03 (–0.63-0.58)/ –0.22 (–0.87-0.43); p>0.05); (0) feeling that too many unnecessary worries about COVID-19 are being made (always/ mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= 0.12 (–0.09-0.33)/ 0.20 (–0.04-0.44)/ 0.07 (–0.10-0.25)/ 0.12 (–0.08-0.33); p>0.05); (0) time spent at home to avoid COVID-19 (0-9/ 10-19 vs. 20-24; logistic regression: β (95%-CI)= –0.15 (–0.52-0.22)/ –0.06 (–0.26-0.14); p>0.05); (0) need for further health information on COVID-19 (logistic regression: β=0.16; 95%-CI –0.03-0.35; p>0.05) (0) need for details on COVID-19 symptoms (logistic regression: β=–0.12; 95%-CI –0.36-0.11; p>0.05); (0) need for recommendations on prevention (logistic regression: β=0.13; 95%-CI –0.14-0.40; p>0.05); (0) need for recommendations on treatment of COVID-19 (logistic regression: β=0.03; 95%-CI –0.14-0.20; p>0.05); (0) need for up-to-date information on local COVID-19 outbreaks (logistic regression: β=–0.10; 95%-CI –0.36-0.15; p>0.05); (0) need for recommendations for special groups, e.g. pre-existing conditions (logistic regression: β=–0.14; 95%-CI –0.41-0.13; p>0.05); (0) need for travel recommendations (logistic regression: β=–0.19; 95%-CI –0.52-0.14; p>0.05); (0) need for updates on other countries' approach to the COVID 19 outbreak (logistic regression: β=–0.14; 95%-CI –0.43-0.15; p>0.05); for depressive symptoms: (0) age (12-21.4/ 21.4-30.8/30.8-40.2/40.2-49.6 vs. 49.6-59 years; logistic regression: β (95%-CI)=0.06 (–0.25-0.37)/ 0.18 (–0.12-0.47)/ –0.06 (–0.41-0.28)/ –0.16 (–0.51-0.19); p>0.05); (0) Parenthood (child <17/ >17 years vs. no child; logistic regression: β (95%-CI)=0.05 (–0.10-0.20)/ –0.06 (–0.18-0.06); p>0.05); (0) marital status (single/ married/ divorced or separated vs. widowed; logistic regression: β (95%-CI)= 0.45 (–0.60-1.51)/ 0.56 (–0.50-1.61)/ 0.44 (–0.77-1.66); p>0.05); (0) household size (>5/ 3-5/ 2 vs. 1 person; logistic regression: β (95%-CI)= –0.19 (–0.76-0.38)/ –0.09 (–0.64-0.47)/ –0.21 (–0.82-0.39); p>0.05); (0) employment (unemployed/farmers/retired vs. employed; logistic regression: β (95%-CI)=0.16 (–0.08-0.40)/ –0.07 (–0.45-0.31)/ –0.48 (–1.18-0.21); p>0.05); (0) highest educational level (primary school/ lower secondary school/ upper secondary school/ bachelor/master vs. doctorate; logistic regression: β (95%-CI)= –0.07 (–0.82-0.69)/ 0.41 (–0.06-0.88)/ 0.34 (–0.11-0.79)/ 0.35 (–0.05-0.75)/ 0.33 (–0.09-0.74); p>0.05); (0) fever + cough or breathing problems (logistic regression: β= 0.22; 95%-CI –0.69-1.13; p>0.05); (0) visit to a doctor in a hospital in the last 14d (logistic regression: β=0.22; 95%-CI –0.07-0.50; p>0.05); (0) hospitalization in the last 14d (logistic regression: β=–0.28; 95%-CI –1.19-0.63; p>0.05); (0) SARS-CoV-2 test in the last 14d (logistic regression: β=0.02; 95%-CI –0.54-0.57; p>0.05); (0) quarantine in the last 14d (logistic regression: β=–0.11; 95%-CI –0.47-0.25; p>0.05); (0) health insurance coverage (logistic regression: β=0.02; 95%-CI –0.18-0.22; p>0.05); (0) indirect contact with confirmed COVID-19 patient (logistic regression: β=–0.37; 95%-CI –1.11-0.38; p>0.05) (0) knowledge of COVID-19 (e.g. for transmission via contaminated objects; logistic regression: β=0.02; 95%-CI –0.12-0.15; p>0.05); (0) source of information (Internet/TV/family vs. others; logistic regression: β(95%-CI)= 0.19 (–0.55-0.94)/ 0.31 (–0.47-1.09)/ –0.03 (–0.97-0.91); p>0.05); (0) satisfaction with the information situation about COVID-19 (very satisfied/ somewhat satisfied/ not very satisfied vs. I don't know; logistic regression: β(95%-CI)= –0.12 (–0.38-0.15)/ –0.001 (–0.27-0.27)/ 0.08 (–0.21-0.36); p>0.05); (0) trust in the doctor (very satisfied/ somewhat satisfied/ not very satisfied vs. I don't know; logistic regression: β(95%-CI)=0.02 (–0.33-0.37)/ 0.09 (–0.26-0.44)/ 0.10 (–0.33-0.52); p>0.05); (0) perceived risk of infection (very high/ high/ not very high/ not likely at all vs. I don't know; logistic regression: β=0.15 (–0.06-0.36)/ 0.04 (–0.14-0.21)/ 0.03 (–0.14-0.20)/ –0.19 (–0.41-0.03); p>0.05); (0) perceived risk of death in case of infection (not at all probable/ not very probable/ something probable vs. I don't know; logistic regression: β (95%-CI)= 0.01 (–0.15-0.17)/ –0.01 (–0.15-0.14)/ 0.15 (–0.06-0.35); p>0.05); (0) worries about family (very worried / somewhat worried / not very worried / not worried at all vs. no family; logistic regression β (95%-CI)=0.29 (–0.05-0.24)/ 0.08 (–0.06-0.23)/ 0.04 (–0.57-0.66); p>0.05); (0) worries about children (very worried/ somewhat worried/ not very worried/ not worried at all vs. no children; logistic regression: β (95%-CI)=0.09 (–0.05-0.24)/ 0.08 (–0.06-0.23)/ 0.08 (–0.09-0.26)/ 0.03 (–0.18-0.23); p>0.05); (0) covering mouth when coughing and sneezing (always/ most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= -0.09 (-0.35-0.18)/ -0.04 (-0.32-0.24)/ 0.02 (-0.30-0.33)/ -0.02 (-0.35-0.31); p>0.05); (0) avoid sharing chopsticks (most/ occasionally vs. never; logistic regression: β (95%-CI)= –0.27 (–0.60-0.07)/ –0.25 (–0.61-0.10)/ –0.15 (–0.51-0.22); p>0.05) (0) washing hands with soap and water (most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.27 (–0.60-0.07)/ –0.25 (–0.61-0.10)/ –0.15 (–0.51-0.22); p>0.05) (0) washing hands directly after coughing, sneezing (sometimes/ occasionally vs. never; logistic regression: β= –0.18 (–0.42-0.06)/ –0.04 (–0.29-0.20); p>0.05); (0) wearing mask independently of symptoms (most/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.21 (–0.52-0.10)/ –0.25 (–0.59-0.08)/ 0.006 (–0.36-0.37); p>0.05); (0) washing hands after touching contaminated objects (mostly/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= –0.41 (–0.85-0.03)/ –0.27 (–0.76-0.21)/ 0.24 (–0.76-0.28); p>0.05) (0) Feeling that too many unnecessary worries about COVID-19 are being worried about (always/ sometimes/ occasionally vs. never; logistic regression: β (95%-CI)= 0.12 (–0.04-0.29)/ 0.01 (–0.13-0.15)/ 0.10 (–0.07-0.26); p>0.05) (0) time spent at home to avoid COVID-19 (0-9/ 10-19 vs. 20-24; logistic regression: β (95%-CI)= –0.21 (–0.51-0.08)/ –0.08 (–0.24-0.08); p>0.05); (0) need for further health information on COVID-19 (logistic regression: β=0.1; 95%-CI –0.06-0.25; p>0.05); (0) need for details on COVID-19 symptoms (logistic regression: β=–0.11; 95%-CI –0.30-0.08; p>0.05); (0) need for recommendations on prevention (logistic regression: β=0.05; 95%-CI –0.17-0.26; p>0.05); (0) need for recommendations on treatment of COVID-19 (logistic regression: β=–0.05; 95%-CI –0.18-0.09; p>0.05); (0) need for regular updates on the current situation regarding COVID-19 (logistic regression: β=–0.29; 95%-CI –0.59-0.01; p>0.05); (0) need for up-to-date information on local COVID-19 outbreaks (logistic regression: β=0.09; 95%-CI –0.11-0.30; p>0.05); (0) need for recommendations for special groups, e.g. pre-existing conditions (logistic regression: β=–0.02; 95%-CI –0.23-0.20; p>0.05); (0) need for up-to-date information on the number of infected persons and their stay (logistic regression: β=–0.13; 95%-CI –0.35-0.10; p>0.05); (0) need for travel recommendations (logistic regression: β=–0.07; 95%-CI –0.34-0.19; p>0.05); (0) need for updates on transmission paths (logistic regression; β=–0.21; 95%-CI –0.51-0.09; p>0.05); (0) need for updates on other countries' approach to the COVID 19 outbreak (logistic regression: β=–0.08; 95%-CI -0.31-0.15; p>0.05) |
| Wang, Y et al. (2020) (e18) | correlation of anxiety and depressive symtpoms (logistic regression; r = 0.696; p < 0.001) for anxiety: (+) female sex (χ² test: χ² = 7.118, p = 0.011; logistic regression: OR=3.01; 95%-CI 1.39-6.52; p=0.005); (+) age > 40 (logistic regression: OR= 0.40; 95%-CI 0.16-0.99; p=0.046); for depressive symptoms: (–) lower education level (bachelor vs. master; logistic regression: OR= 0.39; 95%-CI 0.17-0.87; p=0.021) (–) occupation: industrial worker (logistic regression: OR=0.31; 95%-CI 0.15-0.65; p=0.002) (–) other professions (logistic regression: OR= 0.38; 95%-CI 0.15-0.93; p=0.035 |
for anxiety: (0) Educational level (χ² test: χ²= 3.046; p=0.386); (0) Occupation (χ²-Test: χ²= 1.765; p=0.633); (0) Region (χ²-test: χ²= 0,136; p=0,738) for depressive symptoms: (0) college degree (vs. master; logistic regression: OR=0.54; 95%-CI 0.24-1.21; p=0.133) (0) highschool degree or lower (vs. master; logistic regression: OR=0.95; 95%-CI 0.40-2.29; p=0.916) (0) being employed (logistic regression: OR=0.86; 95%-CI 0.47-1.59; 0.862); |
| Zhang, Y. et al. (2020) (e19) |
for posttraumatic stress symptoms: (–) time to rest (no details on; p= 0.028); |
for posttraumatic stress symptoms: (0) sex (unpaired test; p=0.478); (0) age (linear regression: t=0.706; p=0.481); (0) BMI (linear regression: t=1.175; p=0.241); (0) education level (linear regression: t=1.013; p=0.312); |
| Healthcare workers | ||
| Cai et al. (2020) (e1) | NR | NR |
| Huang, JZ. et. al. (2020) (e9) |
for anxiety: (–) male sex (t-test: t=–2.548; p=0.012); (–) medical profession (vs. nursing profession; t-test: t=-4.207; p<0.001); (+) low occupational position (junior/ middle/senior; ANOVA: F=3.275; p=0.040); for posttraumatic stress symptoms: (-) male sex (t-Test: t=-2.472; p=0.014); |
for anxiety: (0) age (ANOVA: F=1.447; p=0.237); (0) marital status (single/married; t-test: t=0.232; p=0.817); (0) professional field (surgery/conservative medicine/infectiology; ANOVA: F=0.397; p=0.673); (0) education (education vs. bachelor or higher; t-test: t=-0.876; p=0.382); (0) current work situation (active vs. quarantined; t-test: t=0.00; p=1); for posttraumatic stress symptoms: (0) age (ANOVA: F=0.531; p=0.589); (0) marital status (single/married; t-test: t=0.881; p=0.379); (0) physician (vs. nursing profession; T-test: t=-0.811; p=0.418); (0) professional field (surgery/conservative medicine/infectiology; ANOVA: F=1.191; p=0.827); (0) education (education vs. bachelor or higher; t-test: t=-0.982; p=0.326); (0) current working situation (active vs. quarantined; t-test: t=0.165; p=0.869); |
| Kang et al. (2020) (e20) |
for mental health: (+) exposure to COVID-19 (own infection/ in loved ones/ co-residents with symptoms; structural equation model: Estimate=5.347; 95%-CI 3.831-8.184; p<0001); (-) use of non-personal psychological support (structural equation model; Estimate=-0.868; 95%-CI: -1.385 - -0.289; p=0.001); |
for mental health: (0) age (χ² test; χ² NR; p=0.101); (0) sex (χ² test; χ² NR; p=0.133); (0) marital status (married/unmarried; χ² test; χ² NR; p=0.127); (0) educational level (postgraduate/lower; χ² test; χ² NR; p=0.322); (0) occupation (doctor/nurse; χ² test; χ² NR; p=0.409); (0) work area (high risk/ normal; χ² test; χ² NR; p=0.092); (0) professional position (junior/ intermediate/ senior; χ² test; χ² NR; p=0.307); (0) counseling or psychotherapy (χ² test; χ² NR; p=0.216) |
| Lai et al. (2020) (6) |
for depressive symptoms (+) female sex (logistic regression; OR 1.94; 95%-CI 1.26-2.98; p = 0.003); (+) female sex (PHQ-9 median [IQR] men vs. women: 3.0 [0-7.0] vs. 5.0 [2.0-8.0]; p<0.001); (+) nursing staff (PHQ-9 median [IQR]) Doctors vs. nurses: 4.0 [1.0-7.0] vs 5.0 [2.0-8.0]; p = 0.007); (+) working at secondary care provider (vs. tertiary care providers, OR 1.65; 95%-CI 1.17-2.34; p = 0.004); (+) working at secondary care provider (PHQ-9 median [IQR] tertiary vs. secondary care provider: 4.0 [1.0-7.0] vs. 5.0 [2.0-9.0];p <0.001); (+) middle professional position (OR 1.77 95%-CI 1.25-2.49; p= 0.001); (+) direct patient contact (logistic regression; OR 1.52; 95%CI, 1.11-2.09; p =0.01); (+) direct patient contact (PHQ-9 Median [IQR] Frontline vs. 2nd-line: 6.0 [2.0-9.0] vs. 4.0 [1.0-7.0]; p<0.001); (+) working in Wuhan (PHQ-9-Median [IQR] Wuhan vs. Hubei outside of Wuhan vs. outside of Hubei: 5.0 [2.0-8.0] vs. 4.0 [1.0-7.0] vs. 3.0 [0-7.0]; p<0.001); for anxiety: (+) female sex (logistic regression; OR 1.69; 95%-CI 1.23-2.33; p= 0.001); (+) female sex (GAD-7 median [IQR] men vs. women: 2.0 [0-6.0] vs. 4.0 [1.0-7.0]; p<0.001); (+) middle professional position: (OR 1.82; 95%-CI 1.38-2.39; p < 0.001); (+) working at secondary care provider (compare with tertiary care provider, OR 1.43; 95%-CI 1.08-1.90; p= 0.01); (+) working at secondary care provider (GAD-7 median [IQR] tertiary vs. secondary care provider: 3.0 [0-7.0] vs. 4.0 [1.0-7.0]; p=0.005); (+) direct patient contact (logistic regression; OR 1.57; 95%-CI 1.22-2.02; p < 0.001); (+) direct patient contact (GAD-7 Median [IQR] Frontline vs. 2nd-line 5.0 [1.0-7.0] vs. 3.0 [0.0-6.5]; p<0.001); (+) nursing staff (GAD-7 median [IQR] doctors vs. nurses: 3.0 [0-7.0] vs. 4.0 [1.0-7.0]; p= 0.008); (+) working in Wuhan (GAD-7 median [IQR] Wuhan vs. Hubei outside of Wuhan vs. outside of Hubei: 4.0 [1.0-7.0] vs. 3.0 [0-6.0] vs. 2.0 [0-6.0]; p<0.001) for sleep related symptoms: (+) direct patient contact (logistic regression; OR 2.97; 95%CI, 1.92-4.60; p < 0.001); (+) nursing profession (ISI median [IQR] doctors vs. nurses: 4.0 [1.0-8.0] vs. 5.0 [2.0-10.0]; p < 0.001); (+) female sex (ISI median [IQR] men vs. women: 3.0 [1.0-8.0] vs. 5.0 [2.0-9.0]; p<0.001); (+) direct patient contact (ISI median [IQR] frontline vs. 2nd line: 6.0 [2.0-11.0] vs. 4.0 [1.0-8.0]; p<0.001); (+) working at secondary care provider (ISI median [IQR] tertiary vs. secondary care provider: 4.0 [2.0-9.0] vs. 6.0 [2.0-10.0]; p=0.008); (+) working in Wuhan (ISI median [IQR] Wuhan vs. Hubei outside Wuhan vs. outside Hubei: 5.0 [2.0-10.0] vs. 4.0 [1.0-8.0] vs. 3.0 [1.0-8.0]; p<0.001); for stress: (+) female sex (logistic regression; OR 10.45; 95%-CI 1.08-1.96; p= 0.01); (+) female sex (IES median [IQR] men vs. women 14.0 [3.0-28.0] vs. 21.0 [9.0-32.0]; p<0.001); (+) mean occupational position (logistic regression; OR 1.94 95%-CI 1.48-2.55; p < 0.001); (+) direct patient contact (logistic regression; OR 1.60; 95%-CI 1.25-2.04; p < 0.001); (+) nursing profession (IES-R median [IQR] physicians vs. nurses: 18.0 [5.0-30.0] vs. 20.5 [8.0-32.0]; p= 0.009); (+) direct patient contact (IES-R median [IQR] frontline vs. 2nd line: 22.5 [9.0-35.0] vs. 17.0 [5.5-28.5]; p<0.001); (+) working in Wuhan (IES-R-Median [IQR] Wuhan vs. Hubei outside Wuhan vs. outside Hubei: 21.0 [8.5-34.5] vs. 18.0 [6.0-28.0] vs. 15.0 [4.0-26.0]; p<0.001); (-) working outside Hubei (logistic regression; OR 0.62; 95%-CI 0.43-0.88; p = 0.008) |
for depressive symptoms: (+) high professional position (compared to low position: OR 1.21; 95%-CI 0.72-2.03; p=0.47) for anxiety: (+) high professional position (compared to low position: OR 1.01; 95%-CI 0.67-1.51; p=0.97); for sleep related symptoms: NR for stress: (0) working at secondary care provider (IES-R median [IQR] tertiary vs. secondary care provider: 19.0 [7.0-32.0] vs. 20.0 [6.0-31.0]; p=0.46); (0) high occupational position (IES-R vs. low position: OR 1.03; 95%-CI 0.69-1.55; p=0.87) (0) working in Hubei outside ofWuhan (ISI, see Wuhan; logistic regression; OR 0.77; 95%-CI 0.57-1.06; p=0.10) |
| Mo et al. (2020) (e2) |
for stress: (+) Siblings (logistic regression for being only child: r=-0.241; p<0.001); (+) workload (logistic regression: r=0.106 p= 0.048) (+) anxiety (correlation analysis according to Pearson: r=0.676; p<0.001) (+) high professional qualification (primary nurse/ senior nurse/ supervisor/ deputy chief nurse; M±SD comparison (ANOVA): 26.57±4.721/ 40.34±12.70/ 41.07±14.08/ 38.25±7.24; F=2.833; p=0.04) (+) poor sleep quality (great/ good/ normal/ not good/ bad; M±SD comparison (ANOVA): 32.65±12.44/ 35.83±10.43/ 41.80±12.37/ 44.50±12.74/ 48.38±20.01; F=4.818; p=0.01) (+) Severity of the patient's condition (suspicious/moderate/ moderate/ severe/ critical; M±SD comparison (ANOVA): 37.38±7.82/ 41.02±13.27/ 36.05±11.16/ 39.83±12.33/ 49.30±17.27; F=2.638; p=0.036) (+) Adaptation to daily diet (adapted/ not adapted; M comparison 38.72±11.79/ 43.68±15.57; T-test: t=-2.216; p=0.028) |
NR |
| Xiao et al. (2020) (e3) |
for sleep related symptoms: (+) anxiety (SEM*: β=0.257; p<0.001); (+) stress (SEM*: β=0.255; p<0.001) (-) self-efficacy (SEM*: β=-0.308; p<0.001); for anxiety: (–) social support (SEM*: β=–0.565; p<0.0001) for stress: (–) social support (SEM*: β=–0.245; P=0.003) (+) anxiety (SEM*: β=0.259; p=0.001) for self-efficacy: (+) social support (SEM*: β=0.304; p<0.001) (–) anxiety (SEM*: β=–0.179; p=0.029) |
for sleep related symptoms: (0) social support (SEM*: β=–0.046; p=0.538) for anxiety NR for stress: NR for self-efficacy: NR |
| Mixed Groups | ||
| Huang, Y. et al. (2020) (e6) |
for depressive symptoms: (+) age <35 years (χ² test; χ²=13.91; p<0.001); (+) health profession+ >3h/d Thinking of COVID-19 (χ²-Test; χ²= 18.03; p<0.001) for anxiety: (+) <35 years (χ² test; χ²=20.6; p<0.001); (+) health profession+>3h/d COVID thoughts (χ²-Test; χ² =78.17; p <0.001); (+) <35 years+>3h/d COVID-thoughts (χ²-Test; χ²= 68.55; p<0.001) for sleep related symptoms: (+) health profession (χ² test; χ²=98.82; p<0.001); (+) health profession+>3h/d Thinking about COVID-19 (χ²-Test; χ²= 7.36; p< 0.025) |
for depressive symptoms: (0) sex (χ²-Test; χ²=3,67; p=0,055); (0) occupation (health workers/employees in companies/ teacher or pupils/ other occupations; χ² test; χ²=2.71; p=0.439); (0) <35 years old + time of reflection on covid-19 (χ²-test; χ²=6,11; p=0,047) for anxiety: (0) sex (χ² test; χ²=2.19; p=0.089); (0) occupation (healthcare workers/employees in companies/ teacher or pupils/ other occupations; χ²-Test; χ²=2.36; p=0.501) for sleep related symptoms: (0) sex (χ² test; χ²=2.59; p=0.108); (0) age (χ² test; χ²=0.58; p=0.446); (0) healthcare profession + time spent thinking about COVID-19 (χ²-Test; χ²=7.36; p=0.025); (0) <35 years old + time spent thinking about covid-19 (χ² test; χ²=6.11; p=0.047) |
| Li et al. (2020) (e8) |
for vicarious traumatization: (+) general population or nursing staff without direct contact to COVID-19 (vs. nursing staff with direct contact to COVID-19; Z-value=57.258; p<0.001) |
NR |
| Lu et al. (2020) (e21) |
for depressive symptoms: -regarding HAMD: (+) healthcare workers (vs. administrative staff; Mann-Whitney U-test (M ±SD comparison): 2.41 ± 3.979 vs. 1.86 ± 3.277; p= 0.029) (+) high risk contact (vs. non-clinical work; logistic regression; HR=2.016; 95%-CI 1.102- 3.685; p= 0.023) for anxiety: -regarding NRS on fear: (+) healthcare workers (vs. administrative staff; χ²-test; χ²=16.953; p< 0.001); (+) Health workers (vs. administrative staff; Mann-Whitney-U-Test (M ±SD comparison): 4.89 ± 2.389 vs. 4.19 ± 2.384; p < 0.001) (+) High risk contact (vs. non-clinical work; logistic regression; HR=1.408; 95%-CI 1.025-1.933; p= 0.034) -regarding HAMA: (+) healthcare workers (vs. administrative personnel; χ²- test; χ²=6.040; p=0.049); (+) healthcare workers (vs. administrative staff; for HAMA; Mann-Whitney-U-Test (M ±SD comparison): 4.73 ± 6.291 vs. 3.67 ± 5.072; p=0.015) (+) high risk contact (vs. non-clinical work; logistic regression; HR=2.062; 95%-CI 1.349 -3.153; p= 0.001) |
for depressive symptoms: -regarding HAMD: (0) healthcare workers (vs. administrative personnel; χ²-test=3.137; p=0.191); (0) low risk contact (vs. non-clinical work; logistic regression; HR=1.394; 95%-CI 0.798-2.433; p= 0.243); for anxiety: -regarding NRS on fear: (0) low risk contact (vs. non-clinical work; logistic regression; HR=1.301; 95%-CI 0.986 -1.716; p= 0.063); -regarding HAMA: (0) low risk contact (vs. non-clinical work; logistic regression; HR= 1.306; 95%-CI 0.888-1.922; p= 0.175) |
| Yuan et al. (2020) (e22) | NR | NR |
| Zhang, W. et al. (2020) (e23) |
for sleep related symptoms: -whole sample: (+) health profession (logistic regression: OR =1.24; 95%-CI 1.02- 1.50; p=0.03); (+) living in rural areas (logistic regression: OR= 1.38; 95%-CI 1.08-1.77; p=0.01) (+) living with family (logistic regression: OR= 0.68; 95%-CI 0.52- 0.89; p=0.01); (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR= 2.45; 95%-CI 1.68-3.56; p<0.01); (+) organic diseases (logistic regression: OR=2.69; 95%-CI 2.05-3.55; p<0.01); - healthcare workers: (+) living in rural areas (logistic regression: OR=2.18; 95%-CI 1.42-3.35; p<0.01) (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR=2.53; 95%-CI 1.74-3.68; <0.01) (+) organic diseases (logistic regression: OR=3.39; 95%-CI 2.20-5.22; p<0.01); -other professions: (+) organic diseases (logistic regression: OR=2.23; 95%-CI 1.55-3.20; p<0.01) for anxiety: - whole sample: (+) health profession (vs. other profession; Mann-Whitney test (GAD-2-M±SD comparison): 1.51±1.28 vs. 1.25±1.23; p <0.01); (+) female sex (logistic regression: OR=1.69; 95%-CI 1.24-2.32; p<0.01) (+) marital status (married/old; logistic regression: OR=1.56; 95%-CI 1.03-2.35; p=0.04); (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR=2.47; 95%-CI 1.59-3.83; p=0.05); (+) organic diseases (logistic regression: OR=2.09; 95%-CI 1.45-3.00; p<0.01); - healthcare workers: (+) female sex (logistic regression: OR=1.80; 95%-CI 1.10-2.95; p = 0.02); (+) rural housing (logistic regression: OR=1.88; 95%-CI; 1.09-3.21; p = 0.02); (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR=2.06; 95%-CI; 1.28-3.32; p < 0.01); (+) organic diseases (logistic regression: OR=2.85; 95%-CI, 1.73-4.68; p < 0.01); for depressive symptoms: - whole sample: (+) health profession (vs. other profession; Mann-Whitney test (PHQ-2-M±SD comparison): 1.35±1.37 vs. 1.18±1.28; p =0.01); (+) living in rural areas(logistic regression: OR=1.46; 95%-CI 1.03-2.07; p=0.04) (+) living with family (logistic regression: OR=0.52; 95%-CI 0.36-0.74; p<0.01) (+) organic diseases (logistic regression: OR=2.17; 95%-CI 1.51-3.12; p<0.01); - healthcare workers: (+) female sex (logistic regression: OR=1.85; 95%-CI 1.11-3.08; p = 0.02); (+) organic diseases (logistic regression: OR=2.51; 95%-C 1.51-4.18; p < 0.01); -other professions: (+) organic diseases (logistic regression: OR=1.90; 95%-CI; 1.13-3.20; p <0.01); (+) living with family (logistic regression: OR=0.36; 95%-CI; 0.21-0.59; p < 0.01) for somatization: - whole sample: (+) health profession (logistic regression: OR=4.70; 95%CI 1.67- 13.22; p<0.01); (+) living in rural areas (logistic regression: OR=3.30; 1.22-8.93; p=0.02); (+) organic diseases (logistic regression: OR=7.14; 95%-CI 2.90-17.60; p<0.01) - healthcare workers: (+) living in rural areas (logistic regression: OR=4.78; 95%-CI; 1.55-14.76; p = 0.01); (+) organic diseases (OR=7.89; 95%-CI; 2.75-22.62; p < 0.01) for obsessive-compulsive symptoms: -whole sample: (+) health profession (logistic regression; OR: 1.85; 95%-CI 1.10- 3.10; p=0.02); (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR=3.38; 95%-CI 1.81-6.29; p<0.01) (+) organic diseases (logistic regression: OR=2.43; 95%-CI 1.38-4.28; p<0.01); -healthcare workers: (+) living in rural areas (logistic regression: OR=2.49; 95%-CI 1.21-5.11; p = 0.01); (+) risk of contact with COVID-19 patients in hospital (logistic regression: OR=3.27; 95%-CI; 1.75-6.11; p < 0.01); (+) organic diseases (logistic regression: OR=2.24; 95%-CI; 1.07-4.71; p = 0.03); -other professions: (+) organic diseases (logistic regression: OR=2.84; 95%-CI; 1.18-6.80; p = 0.02) for phobic anxiety: (+) female sex (logistic regression: OR=2.19; 95% CI 1.18- 4.05; p=0.01) |
for sleep related symptoms: NR for anxiety: NR for depressive symptoms: NR for somatization: NR for obsessive-compulsive symptoms: NR for phobic anxiety: (0) health profession (vs. other profession; Mann-Whitney test (SCL-90-R subscore M±SD comparison): 3.78±4.18 vs. 3.68±3.96; p= 0.87); |
Abbreviations:
HR: hazard ratio; M: mean value; NR: not reported; OR=odds ratio; p: level of significance; r: correlation coefficient; SD = standard deviation; β: regression coefficient
(+) = positive correlation; (–) = negative correlation; (0) = no correlation; CES-D: Center for Epidemiologic Studies Depression Scale to assess depressive symptoms; CPDI: COVID-19 Peritraumatic Distress Index; DASS-21: Depression, Anxiety and Stress Scale; GAD-7: Generalized Anxiety Disorder Scale-7 to assess generalized anxiety disorders; GSES: General Self-Efficacy Scale to assess self-efficacy; HAMA: Hamilton Anxiety Scale to assess anxiety symptoms; HAMD: Hamilton Depression Scale to assess depressive symptoms; IES-R: Impact of Event Scale -Revised to assess post-traumatic symptoms; ISI: Insomnia Severity Index to assess sleep disorders; NRS: Numeric Rating Scale; PCL-5: Posttraumatic Stress Disorder Checklist for DSM-5 for posttraumatic stress symptoms; PCL-C: Posttraumatic Stress Disorder Checklist- Civilians for posttraumatic stress symptoms; PHQ-4: Personal Health Questionnaire-4 to assess anxiety and depressive symptoms; PHQ-9: Personal Health Questionnaire 9 to assess depressive symptoms; PSQI: Pittsburgh Sleep Quality Index to assess sleep quality; PTBS: Post-traumatic stress symptoms; PTSD-SS: PTSD Self-rating Scale to assess post-traumatic stress symptoms; SAS: Self-Rating Anxiety Scale to assess anxiety symptoms; SASR: Stanford Acute Stress Reaction Questionnaire to assess stress reactions; SCL-90-R: Symptom Checklist 90-Revised for recording psychological stress; SDS: Self-Rating Depression Scale; SE: Self-developed questionnaire; SEM: Structural equation model; SOS: Stress Overload Scale to assess stress; SRQ: Stress Response Questionnaire to assess emotional situation, somatic reactions and behavior; SSRS: Social Support Rate Scale to assess social support; Vicarious Traumatization Questionnaire to assess secondary traumatization, based on TSIB (Traumatic Stress Institute Belief Scale), VTS (Vicarious Trauma Scale) and IES, among others
*for SEM (Xiao et al.): GFI=0.995, CFI=0.995, TLI=0.953, IFI=0.996, NFI=0.991, AGFI=0.931, RMSEA=0.077, χ²/df=2.073
Contact with SARS-CoV-2 patients (n = 5 studies)
Female sex (n = 5)
Healthcare professions (n = 4)
Low (perceived) health status (n = 3)
Concern for loved ones (n = 2)
Poor sleep quality (n = 2).
In contrast to this, one study (e8) found an increased risk in healthcare workers not in contact with SARS-CoV-2 patients and another (e9) an increased risk in men. Professional qualification also had varying effects in the different studies (6, e2, e9). Protective factors were identified in 10 studies, with a broad spectrum of factors emerging.
Exploratory analyses of psychomorbidity and resilience in Germany
At the three measurement points (wave 4, 5, and 8) in the COSMO study (9, 10), 1114, 1030, and 1012 different individuals in the German population were anonymously surveyed, respectively. Since the samples did not differ significantly with regard to sex and level of education and only slightly with regard to age (F [2, 3153] = 22.38, p = <0.001, η² = 0.014), one can compare the samples with one another (etable 5). In a comparison of the ADS and the GAD-7 items (11, 12) with the values for the German population before the pandemic, the COSMO sample shows small effects for increased psychological distress (d = 0.15 to d = 0.28) (table 4). The mean subjective assessment among respondents of their resilience (the ability to recover from stressful events) remains unchanged compared to a German norm sample (14) (p = 0.073, d = 0.05, Table 4).
eTable 5. Sociodemographics of the COSMO study.
| COSMO study | |||||||
| 24.03.2020 | 31.03.2020 | 21.04.2020 | F | p | η² | ||
| N | 1114 | 1030 | 1012 | ||||
| Age M (SD) | 50.54 (18.42) | 45.84 (15.95) | 46.84 (15.34) | 22,38 | <0.001 | 0,014 | |
| Sex | Male | 572 (51%) | 507 (49%) | 491 (49%) | 0,394 | ||
| Female | 542 (49%) | 523 (51%) | 521 (51%) | ||||
| Educational level | <10 years | 123 (11%) | 104 (10%) | 114 (33%) | 0,895 | ||
| ≥ 10 Years with no UEQ | 379 (34%) | 360 (35%) | 329 (56%) | ||||
| ≥ 10 Years with UEQ | 612 (55%) | 566 (55%) | 569 (56%) | ||||
Group differences calculated using one-way ANOVA (age) and the Kruskal–Wallis test (remaining variables)
UEQ. university entrance qualification; η². effect size of the ANOVA; p. significance of the group differences
Table 4. Comparisons of the items to measure psychomorbidity. resilience. and anxiety over the survey period. as well as comparisons of the items with values before the SARS-CoV-2 pandemic.
| COSMO survey | COSMO | Norm | |||||||
| 24.03.2020 | 31.03.2020 | 21.04.2020 | |||||||
| N | 1114 | 1030 | 1012 | 3156 | *1 | ||||
| M (SD) |
M (SD) |
M (SD) |
p | η2 | M (SD) |
M (SD) |
p | d | |
| GAD-7: Item 1 (“anxious”) |
0.77 (0.94) |
0.75 (0.91) |
0.60 (0.83) |
<0.001 | 0,007 | 0.71 (0.90) |
0.50 (0.64) |
<0.001 | 0,27 |
| ADS: Item 6 (“depressed”) |
0.68 (0.89) |
0.68 (0.89) |
0.63 (0.85) |
0,29 | <0.001 | 0.66 (0.88) |
0.43 (0.70) |
<0.001 | 0,28 |
| ADS: Item 14 (“lonely”) |
0.55 (0.90) |
0.64 (0.93) |
0.59 (0.89) |
0,08 | 0,002 | 0.59 (0.90) |
0.46 (0.75) |
<0.001 | 0,15 |
| ADS: Item 8 (“hopeful”)*2 |
1.63 (1.06) |
1.65 (1.07) |
1.65 (1.08) |
0,89 | <0.001 | 1.64 (1.07) |
1.47 (0.97) |
<0.001 | 0,16 |
| IES-R: Item 19 (“physical symptoms of anxiety”) |
0.32 (0.71) |
0.25 (0.60) |
0.19 (0.55) |
<0.001 | 0,007 | ||||
| Psychological distress Overall |
0.79 (0.60) |
0.79 (0.57) |
0.73 (0.55) |
0,028 | 0,002 | ||||
| Resilience (BRS) | 3.47 (0.84) |
3.41 (0.85) |
3.47 (0.49) |
0,258 | 0,002 | 3.45 (0.85) |
3.49 (0.84) |
0,073 | 0,05 |
| Fear of COVID-19 | 4.08 (0.98) |
4.14 (0.94) |
3.76 (0.88) |
<0.001 | 0,03 | ||||
Since there were no significant differences with regard to the ADS items and resilience between the three time points. the groups were pooled to create an overall value for comparison with the norm values (norm values: GAD-7 [11]. ADS [11]. BRS [14]). Norm values are not available for the IES-R items.
The GAD-7 item. ADS items. and IES-R item were each assessed with a four-level scale. resilience with a five-level scale. and fear of COVID-19 with a seven-level scale.
*1 Size of norm samples: GAD-7 = 5030; ADS = 1156; BRS = 2609. *2Higher values here indicate a less hopeful look ahead to the future. ADS. German General Depression Scale (Allgemeine Depressionsskala); BRS. Brief Resilience Scale; COSMO. COVID-19 Snapshot Monitoring study; d. Cohen’s d; GAD-7. Generalized Anxiety Disorder Scale-7; IES-R. Impact of Event Scale—Revised Version; M. mean value; Norm. values in norm samples; η2. effect size of the ANOVA; p. statistical probability of group parity; SD. standard deviation
The reported psychological burden due to depressive symptoms (ADS) remained at a slightly increased level consistently over the three waves of the survey, whereas anxiety due to SARS-CoV-2, physical symptoms when thinking about the SARS-CoV-2 pandemic, and overall psychological distress declined over time (table 4). No differences were seen over time in the subjective assessment of resilience. Men assessed their resilience higher than did women (p ≪0.001, d = 026). Older individuals assessed their resilience higher (r = 0.169, [95% confidence interval: 0.152; 0.186], p = ≪0.001) and their psychological burden lower than did younger individuals (r = –0.228, [-0.245; -0.211], p = ≪0.001). Fear of SARS-CoV-2 was independent of age (r = 0.013; [0.005; 0.031], p = 0.482) (etable 6).
eTable 6. Risk factors for psychomorbidity*1 with and without resilience as a covariate.
| r | p | r(Cov) | p(Cov) | ||||||
| Age | -0.228 | <0.001 | -0.166 | <0.001 | |||||
| N | M | SD | F | p | η² | p(Cov) | η²(Cov) | ||
| Sex | Male | 1570 | 0,73 | 0,55 | 20,211 | <0.001 | 0,006 | ||
| Female | 1586 | 0,82 | 0,6 | ||||||
| Own children | Yes | 799 | 0,84 | 0,57 | 12,849 | <0.001 | 0,004 | ||
| No | 2357 | 0,75 | 0,58 | ||||||
| Single parent | Yes | 103 | 1,02 | 0,6 | 13,135 | <0.001 | 0,016 | <0.001 | 0,013 |
| No | 696 | 0,81 | 0,56 | ||||||
| Migration background | Yes | 464 | 0,87 | 0,61 | 7,716 | <0.001 | 0,005 | 0,006 | 0,003 |
| No | 2682 | 0,76 | 0,57 | ||||||
| Healthcare profession | Yes | 233 | 0,79 | 0,57 | 0,235 | 0,628 | <0.001 | 0,366 | <0.001 |
| No | 2923 | 0,77 | 0,58 | ||||||
| Education | <10 years | 341 | 0,76 | 0,55 | 0,864 | 0,422 | 0,001 | 0,07 | 0,002 |
| >10 Years (without UEQ) | 1068 | 0,76 | 0,58 | ||||||
| >10 Years (with UEQ) | 1747 | 0,78 | 0,58 | ||||||
| People in the household | Only me | 858 | 0,83 | 0,61 | 16,308 | <0.001*2 | 0,015 | ||
| 2 People | 1272 | 0,69 | 0,54 | ||||||
| 3–4 People | 886 | 0,82 | 0,57 | ||||||
| More than 4 people | 140 | 0,86 | 0,57 | ||||||
*1 Since the differences between samples in the survey waves were negligible with regard to psychological distress (assessed using GAD-7: item 1; ADS: items 6. 14. 8; IES-R: item 19). these were summarized for an exploratory analysis of the risk factors. Higher values signify greater psychological distress.
*2 Post hoc Games–Howell tests show that two people in a household is associated with lower psychological distress compared to only one person or more than two people in a household.
p(Cov) and η²(Cov) only reported if ANCOVA requirements fulfilled.
ADS. Allgemeine Depressionsskala (German General Depression Scale); d. Cohen’s d; GAD-7. Generalized Anxiety Disorder Scale-7 to measure anxiety symptoms; IES-R. Impact of Event Scale–Revised to measure posttraumatic stress symptoms; M. mean of distress; η². effect size of the ANOVA; η²(Cov). for resilience as a covariate of controlled effect size; p. significance of the r. t-. or F-value; p(Cov). significance of the F-value of the ANCOVA with resilience as a covariate; r. Pearson product-moment correlation; SD. standard deviation of distress; r(Cov). correlation value of the partial correlation controlled for resilience; UEQ. university entrance qualification
Also when checking for self-assessed resilience as a possible confounding variable, evidence of various risk factors for psychomorbidity were seen (young age, female sex, own children, single parenthood, migrant background, living alone, or more than two people in a household). Practicing a healthcare profession was not identified as a risk factor (etable 6).
Discussion
The systematic literature analysis of the primarily Chinese studies provides evidence of an increase in anxious, depressive, and posttraumatic stress symptoms. More pronounced symptoms of depression, anxiety, and sleep disorders can be seen in healthcare workers (table 3). In accordance with this, the results of the COSMO study suggest that the investigated samples show slightly higher levels of psychological distress (anxiety, depression, hopelessness) compared to the general German population prior to the outbreak of the SARS-CoV-2 pandemic. At the same time, one sees that symptoms of anxiety abate again over time, consistent with a functional psychological adjustment to a stressful event (3, 17– 19). The absence of change in self-assessed resilience as recorded using the BRS (14) compared to before and during the SARS-CoV-2 pandemic can possibly be explained by the fact that the time period from onset of the stressor (the pandemic) was too short for self-assessed resilience to be revised. The age effects reported in the validation studies (14, 15), according to which younger people report a higher subjective ability to recover from stressful events, are in complete contrast to the results of our study, while the gender effects are in agreement (14). The finding that older individuals assessed their resilience as higher compared to younger people may suggest that they are able to deal with the pandemic in a more functional manner, possibly by drawing on cognitive, emotional, and behavior-based experiential contexts in which crises have played a role. Women and younger people report a higher psychological burden compared to high-risk groups (men and older people, [e10]). One possible explanation for this could be that younger people are more restricted in their everyday lives and that women generally report higher levels of psychological distress (e11).
The studies included in the systematic literature analysis identify numerous risk factors. Those particularly worthy of note include female sex, working in the health sector, and pandemic-specific factors (for example, contact with infected individuals) (e7). Awareness of these vulnerable groups opens up the potential of targeted prevention and low-threshold support (e.g., online services). In China, some hospitals developed and successfully implemented multimodal strategies for psychological interventions, which integrate measures not requiring personal contact, such as telephone hotlines and online platforms (20, 21). The results of the COSMO study also suggest that young age, female sex, having children, being a single parent, having a migrant background, as well as living alone or in a household with more than two people represent possible risk factors for psychomorbidity. We found it surprising that healthcare professionals did not report significantly higher psychological distress, in contrast to our analysis of the studies from China. However, this result should be evaluated with caution, since the type of healthcare occupation and whether these people were in contact with COVID-19 patients is unclear.
It becomes clear from some of the studies that social support, self-efficacy, psychoeducational measures, and providing up-to-date, positive and situation-specific information can protect against psychological distress. In line with this, interventional concepts that take into account these protective and resilience factors could be developed (Kunzler et al.: Mental health and psychosocial support strategies in highly contagious emerging disease outbreaks of substantial public concern: a systematic scoping review. PLOS ONE [submitted], [22]). However, there is still insufficient evidence from interventional studies in either the current pandemic or earlier pandemics.
This systematic literature analysis is based on the state of publications up to 16.04.2020. Since then, a number of European studies have been conducted that also reveal a picture of increased psychomorbidity. In a survey of German neurologists and psychiatrists conducted in early April 2020, approximately a third reported deep concern, high own risk of infection, and financial threat (e12). A nationwide survey of the Italian population in March 2020 found increased psychological distress compared to before the pandemic, with almost a fifth of respondents reporting pronounced symptoms of anxiety and around a third reporting pronounced symptoms of depression (e13).
To make a valid assessment of the psychological sequelae of the pandemic, it is necessary to conduct in particular population-representative studies, comparisons with data from before the SARS-CoV-2 pandemic, and longitudinal studies (Kunzler et al.: Mental health and psychosocial support strategies in highly contagious emerging disease outbreaks of substantial public concern: a systematic scoping review. PLOS ONE [submitted]).
On the basis of previous research on potentially traumatic life events, greater attention should be focused on resilience in the sense of positive individual trajectories (23, 24). Taking the findings presented in this article as a starting point, one could deploy psychological interventions, aimed in particular at self-efficacy, information strategies and their evaluation, opportunities for social support, and psychoeducational initiatives in the media, in order to minimize the negative effects of the SARS-CoV-2 pandemic and learn for future pandemics.
Limitations
The present study has limitations that narrow down the conclusions that can be drawn. For the COSMO study, these include:
The early timing of the survey in the course of the SARS-CoV-2 pandemic
The short survey period
The assessment of mental health by means of a combination of items from different questionnaires, for some of which norm values for the general population are lacking
The fact that the sensitivity of BRS has not yet been validated with respect to changes in self-assessed resilience at different points in time
The low response rate of under 20%, which limits the generalizability of the results to the German population.
Limitations of the systematic literature analysis include:
The limited quality and lack of representativeness of the studies
Lack of comparisons with norm data
The questionable extent to which the results can be extrapolated to Germany
Inconsistencies in the use of measurement tools and their cut-off values
A potential publication bias
The problematic use of the term “posttraumatic stress symptoms,” which leaves unclear the relationship to the concept of trauma and the diagnosis of a posttraumatic stress disorder according to ICD-10 (e14, e15).
Supplementary Material
eMETHODS
Literature search
To identify relevant studies, a literature search was conducted in the electronic databases PubMed, PsycINFO, and Web of Science (Core Collection) for the period 01.01.1990 to 16.04.2020. The search in Web of Science was restricted in the database itself to the period 01.01.1990 to 16.04.2020. The search in PubMed and PsycINFO was later manually restricted to the same period. The strategy for the electronic database search is documented in the eBox. The search strategy comprised three key sets of search terms:
For the three term clusters mentioned above, different search terms were used as appropriate for each database (for example, MeSH terms, title, abstract, keywords). To create the possibility for further systematic literature analyses at a later point in time, additional search terms relating in particular to “pandemic” and “populations” were used (e.g. “ebola,” “patients”); however, these are not relevant for the current literature analysis. In addition, due to the focus of the present systematic literature analysis on the current SARS-CoV-2 pandemic, search results from the three databases were restricted to the period 01.01.2019 to 16.04.2020. This restriction was made in view of the fact that first SARS-CoV-2 infections were reported from December 2019 onwards and that studies investigating the associated psychological distress and potential protective factors were only conducted in the period thereafter. Since there are no systematic reviews or meta-analyses available as yet on psychological distress, protective factors, and resilience in the context of the current SARS-CoV-2 pandemic, it was not possible to review pertinent reference lists for this review article.
Study selection
Once duplicates had been excluded, the titles and abstracts of the identified publications were reviewed for relevance in a first step by two independent reviewers (NR, MB) using the previously specified inclusion criteria. Articles that were clearly not relevant were excluded before the full texts of relevant papers were then re-screened by two independent reviewers (NR, MB) with regard to the inclusion criteria. Since no areas of uncertainty arose, there was no need to contact the authors of any of these studies. One study needed to be translated from Chinese into English. Any disagreement was resolved through discussion or by involving a third assessor (KL).
Extraction of relevant data
The following data were extracted from the included studies on the basis of a data extraction table developed and pre-tested (five studies) for systematic literature analysis by two reviewers (NR, MB):
In addition, the investigated moderating factors, i.e., risk and protective factors, for psychological distress were extracted from the included studies, together with the reported statistical parameters (e.g., odds ratio from regression analyses, correlation coefficients). Any disagreements in the extracted data were also resolved by consensus discussions. A detailed data extraction table can be requested from the corresponding author.
Effect sizes and data synthesis
The included studies were highly heterogeneous with regard to several characteristics (for example, population, endpoints surveyed, scales and cut-offs used), including the statistical analysis used (for example, logistic regression analysis, correlation analysis, χ2 test) and the presentation of continuous and dichotomous endpoints. For this reason, only the reported statistical results were extracted in each case, and no effect sizes were calculated or quantitative synthesis performed of the study data in meta-analyses.
Quality assessment
To assess the quality of the studies included, a risk-of-bias assessment based on the quality assessment tool for cross-sectional and cohort studies of the National Heart, Lung, and Blood Institute was used (8). The assessment was carried out by two independent reviewers (NR, JSW). The presence of the stress factor “SARS-CoV-2 pandemic” was considered exposure (independent variable) in all studies. This was defined as the time following the announcement of the first COVID-19 patient nationwide and—in the case of China, after 20.01.2020—the day on which human-to-human transmission was officially confirmed (e5).
For some questions in the quality assessment tool (etable 3), adjustments were made due to these particular independent variables in order to account for the studies included. Questions that were not applicable to the included studies are not listed for the sake of clarity. If “no” or “not reported” were given for two or more questions, the study was overall deemed to be “poor.” A guide to the use of the modified instrument is available on request from the authors.
Modifications were made to the following points:
The following questions are not included in eTable 3:
Terms relating to mental health, psychological distress, and resilience (for example, “mental health,” “burden,” “resilien*”
Terms associated with pandemics, including the current SARS-CoV-2 pandemic (for example “COVID-19,” “coronavirus”)
Terms related to various populations of interest, such as the general population and healthcare workers (for example, “health* personnel,” “community”).
Country
Survey period and methods
-
Population group investigated:
General population
Healthcare workers
Number of participants, including average age and percentage of female subjects
Subgroups, if any
Representativeness of the sample and any reported comparison with norm data
Psychological distress (survey instruments used and, where appropriate, the proportion of subjects above the cut-off value for the respective measurement tools) in the areas anxiety and worry
Depression
Posttraumatic stress
Sleep and stress (supplemented by additional areas of stress where appropriate).
Question 8 (8) (“For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome [e.g., categories of exposure, or exposure measured as continuous variable]?”): This question was modified since a linear relationship is assumed between exposure and effect. Normally, a study is more positively assessed if it records several time points or exposure levels, since this makes the relationship more readily apparent. However, since in our case a linear relationship cannot be assumed, the item was modified to “Was the exposure (independent variable) clearly specified?”
Question 9 (8) (“Were the exposure measures [independent variables] clearly defined, valid, reliable, and implemented consistently across all study participants?”): This question was modified in such as way that the heterogeneity of exposure is assessed, since exposure in the case of the COVID-19 pandemic could show significant differences over a longer period of observation, e.g., in the event of a relaxation or tightening of initial containment measures or an increase or decrease in the number of infections. As such, a shorter survey period is desirable in terms of a more homogeneous sample. Thus, the question was modified to: “Was the exposure consistent across all study participants?”
Question 6 (8) (“For the analyses in this paper, were the exposure[s] of interest measured prior to the outcome[s] being measured?”): Since exposure was not predictable, this question is not applicable.
Question 7 (8) (“Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?”): This question was also not applicable since the psychological burden is likely to vary over time (for example, due to rising or falling infection numbers, tightening or relaxing of containment measures, etc.). In any event, it is not known whether longer exposure leads to a greater burden, which the question assumes. Furthermore, this item applies only to studies with repeated measurements, but not to other comparisons, such as those of exposed groups with norm samples.
Question 10 (8) (“Was the exposure(s) assessed more than once over time?”): The use of this question for the studies considered here would require that the existence of the SARS-CoV-2 pandemic has been verified several times. It does not appear possible to make meaningful use of this assessment item.
Question 12 (8) (“Were the outcome assessors blinded to the exposure status of participants?”: Since it is not possible to blind studies in which the SARS-CoV-2 pandemic is exposure, this question is not applicable.
Question 13 (8) (“Was loss to follow-up after baseline 20% or less?”: Since no follow-up surveys were conducted in any of the studies, this question is not applicable.
Question 14 (8) (“Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure[s] and outcome[s]?”): Since none of the studies considered here made a direct comparison between exposed and non-exposed participants, it is not meaningful to measure confounding variables and, therefore, the question is not applicable.
Key messages.
Studies, primarily from China, point to an increase in depressive, anxious, and posttraumatic stress symptoms as well as sleep disorders in association with the SARS-CoV-2 pandemic compared to norm values.
Despite the rise in self-reported psychological distress, the German sample rates its own resilience as unchanged.
High-risk groups such as women, healthcare workers, single parents, and people with a migrant background should be taken into particular consideration in the development of measures to strengthen mental health.
Psychological interventions should promote in particular opportunities for social support and self-efficacy, as well as psychoeducational initiatives in the media, in order to minimize the negative effects of the SARS-CoV-2 on mental health.
When investigating potential long-term effects of the SARS-CoV-2 pandemic on mental health, investigators should focus greater attention on resilience in the sense of positive individual trajectories of development.
Acknowledgments
Translated from the original German by Christine Rye.
Acknowledgments
Footnotes
Conflicts of interest statement
The authors state that no conflicts of interest exist.
References
- 1.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus (COVID-19) Dashboard. https://who.sprinklr.com/ (last accessed on 10 July 2020) 2020 [Google Scholar]
- 3.Veer IM, Riepenhausen A, Zerban M, et al. Psycho-social factors associated with mental resilience in the corona lockdown. PsyArXiv Preprints. 2020 doi: 10.1038/s41398-020-01150-4. Doi:10.31234/osf.io/4z62t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robertson E, Hershenfield K, Grace SL, Stewart DE. The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can J Psychiatry. 2004;49:403–407. doi: 10.1177/070674370404900612. [DOI] [PubMed] [Google Scholar]
- 6.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 e1000097. [PMC free article] [PubMed] [Google Scholar]
- 8.National Heart, Lung, and Blood Institute. Study Quality Assessment Tools. www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (last accessed on 23 June 2020) [Google Scholar]
- 9.Betsch C, Wieler LH, Habersaat K, COSMO group Monitoring behavioural insights related to COVID-19. Lancet. 2020;395:1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Betsch C, Wieler, L, Bosnjak, M, et al. 2020 Germany COVID-19 Snapshot Monitoring (COSMO Germany): Monitoring knowledge, risk perceptions, preventive behaviours, and public trust in the current coronavirus outbreak in Germany. https://hdl.handle.net/20.500.12034/2386 (last accessed on 7 May 2020) [Google Scholar]
- 11.Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 12.Hautzinger M, Bailer M, Hofmeister D, Keller F. Allgemeine Depressionsskala (ADS), 2nd edition. Göttingen: Hogrefe; 2012 [Google Scholar]
- 13.Maercker A, Schützwohl M. Erfassung von psychischen Belastungsfolgen: Die Impact of Event Skala - Revidierte Version. Diagnostica. 1998;44:130–141. [Google Scholar]
- 14.Chmitorz A, Wenzel M, Stieglitz RD, et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS One. 2018;13 doi: 10.1371/journal.pone.0192761. e0192761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunzler AM, Chmitorz A, Bagusat C, et al. Construct validity and population-based norms of the German Brief Resilience Scale (BRS) Eur J Health Psychol. 2018;25:107–117. doi: 10.1027/2512-8442/a000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalisch R, Cramer AOJ, Binder H, et al. Deconstructing and reconstructing resilience: a dynamic network approach. Perspect Psychol Sci. 2019;14:765–777. doi: 10.1177/1745691619855637. [DOI] [PubMed] [Google Scholar]
- 18.Kalisch R, Baker DG, Basten U, et al. The resilience framework as a strategy to combat stress-related disorders. Nat Hum Behav. 2017;1:784–790. doi: 10.1038/s41562-017-0200-8. [DOI] [PubMed] [Google Scholar]
- 19.Kalisch R, Müller MB, Tüscher O. A conceptual framework for the neurobiological study of resilience. Behav Brain Sci. 2015;38 doi: 10.1017/S0140525X1400082X. e92. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precis Clin Med. 2020 doi: 10.1093/pcmedi/pbaa006. pbaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7 doi: 10.1016/S2215-0366(20)30047-X. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petzold MB, Plag J, Ströhle A. Psychische Belastungen können reduziert werden. Dtsch Arztebl. 2020;117:A 648–A 654. [Google Scholar]
- 23.Bonanno GA, Diminich ED. Annual research review: Positive adjustment to adversity-trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry. 2013;54:378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kunzler AM, Gilan DA, Kalisch R, Tüscher O, Lieb K. Aktuelle Konzepte der Resilienzforschung. Nervenarzt. 2018;89:747–753. doi: 10.1007/s00115-018-0529-x. [DOI] [PubMed] [Google Scholar]
- E1.Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei, China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.924171. e924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020;28:1002–1009. doi: 10.1111/jonm.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E3.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923549. e923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E4.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.dpa/aerzteblatt.de. Virus in China verbreitet sich von Mensch zu Mensch. www.aerzteblatt.de/nachrichten/108769 (last accessed on 27 April 2020) [Google Scholar]
- E6.Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol Health Med. 2020:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- E7.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. 112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- E10.Dreher M, Kersten A, Bickenbach J, et al. The characteristics of 50 hospitalized COVID-19 patients with and without ARDS. Dtsch Arztebl Int. 2020;117:271–278. doi: 10.3238/arztebl.2020.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Bohlken J, Schömig F, Seehagen T, et al. Experience of practice-based psychiatrists and neurologists during the COVID-19 pandemic. Psychiatr Prax. 2020;47:214–217. doi: 10.1055/a-1159-5575. [DOI] [PubMed] [Google Scholar]
- E13.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.ICD-10-Code. Posttraumatische Belastungsstörung. ICD-10-GM-2020 F43.1. https://www.icd-code.de/icd/code/F43.1.html (last accessed on 13 August 2020) [Google Scholar]
- E15.Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102083. 102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020:1–10. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- E19.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17072381. 2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E20.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel Coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E21.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. 112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E22.Yuan S, Liao Z, Huang H, et al. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the Coronavirus Disease 2019 (COVID-19) outbreak in February 2020. Med Sci Monit. 2020;26 doi: 10.12659/MSM.923767. e923767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E23.Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020:;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Literature search
To identify relevant studies, a literature search was conducted in the electronic databases PubMed, PsycINFO, and Web of Science (Core Collection) for the period 01.01.1990 to 16.04.2020. The search in Web of Science was restricted in the database itself to the period 01.01.1990 to 16.04.2020. The search in PubMed and PsycINFO was later manually restricted to the same period. The strategy for the electronic database search is documented in the eBox. The search strategy comprised three key sets of search terms:
For the three term clusters mentioned above, different search terms were used as appropriate for each database (for example, MeSH terms, title, abstract, keywords). To create the possibility for further systematic literature analyses at a later point in time, additional search terms relating in particular to “pandemic” and “populations” were used (e.g. “ebola,” “patients”); however, these are not relevant for the current literature analysis. In addition, due to the focus of the present systematic literature analysis on the current SARS-CoV-2 pandemic, search results from the three databases were restricted to the period 01.01.2019 to 16.04.2020. This restriction was made in view of the fact that first SARS-CoV-2 infections were reported from December 2019 onwards and that studies investigating the associated psychological distress and potential protective factors were only conducted in the period thereafter. Since there are no systematic reviews or meta-analyses available as yet on psychological distress, protective factors, and resilience in the context of the current SARS-CoV-2 pandemic, it was not possible to review pertinent reference lists for this review article.
Study selection
Once duplicates had been excluded, the titles and abstracts of the identified publications were reviewed for relevance in a first step by two independent reviewers (NR, MB) using the previously specified inclusion criteria. Articles that were clearly not relevant were excluded before the full texts of relevant papers were then re-screened by two independent reviewers (NR, MB) with regard to the inclusion criteria. Since no areas of uncertainty arose, there was no need to contact the authors of any of these studies. One study needed to be translated from Chinese into English. Any disagreement was resolved through discussion or by involving a third assessor (KL).
Extraction of relevant data
The following data were extracted from the included studies on the basis of a data extraction table developed and pre-tested (five studies) for systematic literature analysis by two reviewers (NR, MB):
In addition, the investigated moderating factors, i.e., risk and protective factors, for psychological distress were extracted from the included studies, together with the reported statistical parameters (e.g., odds ratio from regression analyses, correlation coefficients). Any disagreements in the extracted data were also resolved by consensus discussions. A detailed data extraction table can be requested from the corresponding author.
Effect sizes and data synthesis
The included studies were highly heterogeneous with regard to several characteristics (for example, population, endpoints surveyed, scales and cut-offs used), including the statistical analysis used (for example, logistic regression analysis, correlation analysis, χ2 test) and the presentation of continuous and dichotomous endpoints. For this reason, only the reported statistical results were extracted in each case, and no effect sizes were calculated or quantitative synthesis performed of the study data in meta-analyses.
Quality assessment
To assess the quality of the studies included, a risk-of-bias assessment based on the quality assessment tool for cross-sectional and cohort studies of the National Heart, Lung, and Blood Institute was used (8). The assessment was carried out by two independent reviewers (NR, JSW). The presence of the stress factor “SARS-CoV-2 pandemic” was considered exposure (independent variable) in all studies. This was defined as the time following the announcement of the first COVID-19 patient nationwide and—in the case of China, after 20.01.2020—the day on which human-to-human transmission was officially confirmed (e5).
For some questions in the quality assessment tool (etable 3), adjustments were made due to these particular independent variables in order to account for the studies included. Questions that were not applicable to the included studies are not listed for the sake of clarity. If “no” or “not reported” were given for two or more questions, the study was overall deemed to be “poor.” A guide to the use of the modified instrument is available on request from the authors.
Modifications were made to the following points:
The following questions are not included in eTable 3:
Terms relating to mental health, psychological distress, and resilience (for example, “mental health,” “burden,” “resilien*”
Terms associated with pandemics, including the current SARS-CoV-2 pandemic (for example “COVID-19,” “coronavirus”)
Terms related to various populations of interest, such as the general population and healthcare workers (for example, “health* personnel,” “community”).
Country
Survey period and methods
-
Population group investigated:
General population
Healthcare workers
Number of participants, including average age and percentage of female subjects
Subgroups, if any
Representativeness of the sample and any reported comparison with norm data
Psychological distress (survey instruments used and, where appropriate, the proportion of subjects above the cut-off value for the respective measurement tools) in the areas anxiety and worry
Depression
Posttraumatic stress
Sleep and stress (supplemented by additional areas of stress where appropriate).
Question 8 (8) (“For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome [e.g., categories of exposure, or exposure measured as continuous variable]?”): This question was modified since a linear relationship is assumed between exposure and effect. Normally, a study is more positively assessed if it records several time points or exposure levels, since this makes the relationship more readily apparent. However, since in our case a linear relationship cannot be assumed, the item was modified to “Was the exposure (independent variable) clearly specified?”
Question 9 (8) (“Were the exposure measures [independent variables] clearly defined, valid, reliable, and implemented consistently across all study participants?”): This question was modified in such as way that the heterogeneity of exposure is assessed, since exposure in the case of the COVID-19 pandemic could show significant differences over a longer period of observation, e.g., in the event of a relaxation or tightening of initial containment measures or an increase or decrease in the number of infections. As such, a shorter survey period is desirable in terms of a more homogeneous sample. Thus, the question was modified to: “Was the exposure consistent across all study participants?”
Question 6 (8) (“For the analyses in this paper, were the exposure[s] of interest measured prior to the outcome[s] being measured?”): Since exposure was not predictable, this question is not applicable.
Question 7 (8) (“Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?”): This question was also not applicable since the psychological burden is likely to vary over time (for example, due to rising or falling infection numbers, tightening or relaxing of containment measures, etc.). In any event, it is not known whether longer exposure leads to a greater burden, which the question assumes. Furthermore, this item applies only to studies with repeated measurements, but not to other comparisons, such as those of exposed groups with norm samples.
Question 10 (8) (“Was the exposure(s) assessed more than once over time?”): The use of this question for the studies considered here would require that the existence of the SARS-CoV-2 pandemic has been verified several times. It does not appear possible to make meaningful use of this assessment item.
Question 12 (8) (“Were the outcome assessors blinded to the exposure status of participants?”: Since it is not possible to blind studies in which the SARS-CoV-2 pandemic is exposure, this question is not applicable.
Question 13 (8) (“Was loss to follow-up after baseline 20% or less?”: Since no follow-up surveys were conducted in any of the studies, this question is not applicable.
Question 14 (8) (“Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure[s] and outcome[s]?”): Since none of the studies considered here made a direct comparison between exposed and non-exposed participants, it is not meaningful to measure confounding variables and, therefore, the question is not applicable.