Abstract
OBJECTIVE
We investigated sex and racial differences in insulin sensitivity, β-cell function, and glycated hemoglobin (HbA1c) and the associations with selected phenotypic characteristics.
RESEARCH DESIGN AND METHODS
This is a cross-sectional analysis of baseline data from 3,108 GRADE (Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study) participants. All had type 2 diabetes diagnosed <10 years earlier and were on metformin monotherapy. Insulin sensitivity and β-cell function were evaluated using the HOMA of insulin sensitivity and estimates from oral glucose tolerance tests, including the Matsuda Index, insulinogenic index, C-peptide index, and oral disposition index (DI).
RESULTS
The cohort was 56.6 ± 10 years of age (mean ± SD), 63.8% male, with BMI 34.2 ± 6.7 kg/m2, HbA1c 7.5 ± 0.5%, and type 2 diabetes duration 4.0 ± 2.8 years. Women had higher DI than men but similar insulin sensitivity. DI was the highest in Black/African Americans, followed by American Indians/Alaska Natives, Asians, and Whites in descending order. Compared with Whites, American Indians/Alaska Natives had significantly higher HbA1c, but Black/African Americans and Asians had lower HbA1c. However, when adjusted for glucose levels, Black/African Americans had higher HbA1c than Whites. Insulin sensitivity correlated inversely with BMI, waist-to-hip ratio, triglyceride-to-HDL-cholesterol ratio (TG/HDL-C), and the presence of metabolic syndrome, whereas DI was associated directly with age and inversely with BMI, HbA1c, and TG/HDL-C.
CONCLUSIONS
In the GRADE cohort, β-cell function differed by sex and race and was associated with the concurrent level of HbA1c. HbA1c also differed among the races, but not by sex. Age, BMI, and TG/HDL-C were associated with multiple measures of β-cell function and insulin sensitivity.
Introduction
β-Cell function declines progressively during the transition from normal glucose tolerance to impaired glucose tolerance and ultimately to type 2 diabetes (1). The UK Prospective Diabetes Study (UKPDS) showed that β-cell function, as evaluated by the HOMA2-B index, was already diminished by ≥50% at the time of diagnosis of type 2 diabetes and continued to decline over the 6-year trial despite ongoing glucose-lowering medication (2). Since progressive loss of β-cell function represents one of the most important challenges to maintenance of glycemic control in people with long-term type 2 diabetes (1), identifying factors associated with β-cell function and interventions to delay or prevent its deterioration would be of great value.
Previous studies have reported several potential mechanisms underlying progressive β-cell dysfunction, including metabolic abnormalities such as glucotoxicity and lipotoxicity, local or systemic inflammation, oxidative and endoplasmic reticulum stress, and amyloid deposition (3). The phenotypic characteristics associated with β-cell dysfunction in patients with type 2 diabetes have not been clearly defined. The results vary depending on the method of measuring β-cell function and the cohort studied. Previous cross-sectional studies showed that β-cell function differed by sex and type of glucose-lowering medication (4). Insulin treatment initiation as an indirect measure of more severe β-cell dysfunction was associated with diabetes duration, levels of glycated hemoglobin (HbA1c), triglycerides (TG), and HDL cholesterol (HDL-C) (5).
Other studies have reported racial differences in the relationship between HbA1c and plasma glucose concentration, notably that Black/African Americans have higher HbA1c compared with Whites for similar blood glucose levels (6–8). In studies of patients with diabetes, this difference persisted when adjusted for sociodemographic and lifestyle factors (9) and adherence to glycemic-lowering medications (10). In this study, we studied the racial and ethnic differences in HbA1c in a large and well-characterized cohort of patients with type 2 diabetes and also assessed whether such differences were associated with measures of β-cell function.
Our objective was to describe the sex and racial differences in β-cell function, insulin sensitivity, and glycemia. In addition, we investigated the association of selected participant characteristics with β-cell function, insulin sensitivity, and glycemia in the Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE) cohort comprised of participants with a relatively recent diagnosis of type 2 diabetes (mean duration ∼4 years) using metformin monotherapy.
Research Design and Methods
GRADE is a National Institutes of Health–funded multicenter study designed to compare the effectiveness of four different glucose-lowering medications, each from a different class: glimepiride (sulfonylurea), sitagliptin (dipeptidyl peptidase 4 inhibitor), liraglutide (glucagon-like peptide 1 receptor agonist), or insulin glargine on glycemic control when added to metformin. The study randomly assigned 5,047 adults with type 2 diabetes at 36 clinical centers and 9 additional subsites across the U.S. We present in this study cross-sectional analyses on a subgroup of this cohort with complete baseline data. The rationale and full details of the study design are found elsewhere (11). All participants provided written informed consent, and the study was approved by each center’s institutional review board.
Eligibility
Participants were eligible to participate in the GRADE Study if they had been diagnosed with type 2 diabetes for <10 years at the time of screening and were ≥30 years of age (≥20 years if American Indian) at the time of diagnosis, with HbA1c 6.8–8.5%, and taking at least 1,000 mg of metformin/day at the end of the run-in period. Exclusion criteria included: suspected type 1 diabetes, treatment with glucose-lowering medications other than metformin within the previous 6 months, use of medications that could impact glucose metabolism such as systemic corticosteroids, and significant medical illness or organ failure (11).
Study Procedures
Eligible participants completed a 4–14-week run-in, during which they were provided metformin, and the dose was increased to 2,000 mg/day or a maximal tolerated dose ≥1,000 mg/day. At the end of the run-in, after an 8-h overnight fast, eligible participants (HbA1c between 6.8 and 8.5%) underwent an oral glucose tolerance test (OGTT) with metformin held the morning of the test. The participant consumed a 75-g glucose drink within 5 min, and blood samples were drawn at 0, 15, 30, 60, 90, and 120 min relative to the start of glucose ingestion. Samples were collected on ice, spun and aliquoted promptly, and frozen at −80°C before being shipped on dry ice to the central laboratory (University of Minnesota Advanced Research and Diagnostic Laboratory, Minneapolis, MN), where they were assayed.
Assays
HbA1c was measured in EDTA whole blood on the Automated Glycohemoglobin Analyzer HLC-723G8 (Tosoh Medics, Inc., San Francisco, CA) using an automated high-performance liquid chromatography method. Calibration of this method was evaluated using standard values derived by the NGSP. Glucose was measured in EDTA plasma by a hexokinase method on a Cobas c501 chemistry analyzer (Roche Diagnostics, Indianapolis, IN). Insulin and C-peptide were measured in EDTA plasma on a Cobas e601 immunoassay analyzer using a sandwich immunoassay (Roche Diagnostics). Baseline samples for those randomized to the glargine group (n = 1,263) have not yet been assayed for insulin. These baseline samples are being reserved for potential measurement by mass spectrometry owing to difficulties in measuring insulin with immunoassays in patients treated with glargine.
Measures of Insulin Sensitivity and β-Cell Function
The HOMA of insulin sensitivity (HOMA2-S) was calculated using the HOMA2 Calculator version 2.2.3 (Diabetes Trials Unit, University of Oxford, Oxford, U.K.) (12,13). Mean plasma glucose (Gm) in milligrams per deciliter and mean insulin (Im) in milli-international units per liter were calculated from the values at 0, 30, 60, 90, and 120 min during the OGTT (14). The Matsuda Index of insulin sensitivity was calculated as 104/(I0 × G0 × Im × Gm)1/2, where G0 and I0 are the fasting glucose and insulin.
Early insulin and C-peptide responses to glucose during the OGTT were calculated using the insulinogenic index (IGI) and the C-peptide index, respectively. They were calculated as the increment in insulin or C-peptide values over the first 30 min, respectively, divided by the increment in glucose over 30 min as follows (15): IGI = 100(I30 − I0)/(G30 − G0) and C-peptide index = 100(C30 − C0)/(G30 − G0). The late insulin response to glucose was calculated as the ratio of the area under the curve (AUC) for insulin divided by the AUC of glucose values from 60 to 120 minutes: 100 × (InsulinAUC60–120/60 − I0)/(GlucoseAUC60–120/60 − G0). The oral disposition index (DI), as a measure of β-cell function, was calculated as the ratio of IGI over fasting insulin (DI = IGI/I0) (16).
We used the ratio of fasting C-peptide to fasting insulin (1,000 ∗ C0/I0) as a measure of basal insulin clearance based on the assumption that insulin and C-peptide are secreted into the portal vein in a 1:1 molar ratio, and C-peptide is cleared primarily by the kidney (17).
The International Diabetes Federation definition of metabolic syndrome was used to categorize participants in this cohort (18).
Participants
Of a total of 5,047 GRADE participants, a subgroup with complete data on glucose, insulin, and C-peptide values during the baseline OGTT was included in this study. Insulin was not measured in the 1,263 participants randomized to the glargine group, and thus, this group was excluded from the analysis. Also excluded were 321 participants with incomplete glucose data, 350 with incomplete insulin data, and 5 with incomplete C-peptide data. Thus, data from a total of 3,108 were available for this analysis. There was no significant difference in baseline characteristics of participants included in this study compared with those excluded (data not shown).
Among the 3,108 participants, 2,083 participants (67%) were White, including 423 (14%) Hispanic and 1,651 (53%) non-Hispanic, 553 (18%) Black/African American, 119 (4%) Asian, 103 (3%) American Indian/Alaska Native, and 250 (8%) other.
Statistical Analysis
Participant characteristics are presented using means and SDs for quantitative variables and counts and column percentages for qualitative variables. Comparisons between men and women used the χ2 test of independence for qualitative variables and the Student t test with unequal variances using the Welch-Satterthwaite approximation to the df for quantitative variables. Comparisons of the race categories used the χ2 test of independence for qualitative variables and the ANOVA F test for quantitative variables. In Table 1, only racial groups with at least 100 members were considered for analysis.
Table 1.
Participant characteristics for all and stratified by sex and race
| Sex | Race | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Men | Women | P value | American Indian | Asian | African American | White | P value | |
| N | 3,108 | 1,984 | 1,124 | 103 | 119 | 553 | 2,084 | ||
| Age (years) | 56.6 ± 10.0 | 57.7 ± 10.1 | 54.7 ± 9.7 | <0.001 | 45.6 ± 10.4 | 53.9 ±10.3 | 55.6 ± 8.9 | 57.9 ± 9.8 | <0.001 |
| Female | 63 (61.2) | 28 (23.5) | 268 (48.5) | 661 (31.7) | <0.001 | ||||
| Race | <0.001 | ||||||||
| American Indian/Alaska Native | 103 (3.3) | 40 (2.0) | 63 (5.6) | ||||||
| Asian | 119 (3.8) | 91 (4.6) | 28 (2.5) | ||||||
| Hawaiian/Pacific Islander | 20 (0.6) | 15 (0.8) | 5 (0.4) | ||||||
| Black or African American | 553 (17.8) | 285 (14.4) | 268 (23.8) | ||||||
| White | 2,084 (67.1) | 1,423 (71.7) | 661 (58.8) | ||||||
| Other/multiple | 189 (6.1) | 107 (5.4) | 82 (7.3) | ||||||
| Unknown/not reported | 40 (1.3) | 23 (1.2) | 17 (1.5) | ||||||
| BMI (kg/m2) | 34.2 ± 6.7 | 33.6 ± 6.2 | 35.2 ± 7.3 | <0.001 | 36.5 ± 7.4 | 28.9 ± 5.2 | 34.2 ± 6.8 | 34.4 ± 6.5 | <0.001 |
| 100 ∗ WHR | 99.2 ± 8.3 | 102.2 ± 7.2 | 93.8 ± 7.3 | <0.001 | 99.2 ± 8.8 | 96.7 ± 7.9 | 97.0 ± 8.2 | 99.9 ± 8.2 | <0.001 |
| Diabetes duration (years) | 4.0 ± 2.8 | 4.1 ±2.8 | 3.9 ± 2.8 | 0.078 | 2.8 ± 2.6 | 4.3 ± 2.7 | 4.2 ± 2.7 | 4.1 ± 2.8 | <0.001 |
| HbA1c (%) | 7.5 ± 0.5 | 7.5 ± 0.5 | 7.5 ± 0.5 | 0.997 | 7.6 ± 0.5 | 7.4 ± 0.4 | 7.4 ± 0.5 | 7.5 ± 0.5 | 0.004 |
| Fasting glucose (mg/dL) | 151.7 ± 30.9 | 153.1 ± 30.8 | 149.3 ± 30.9 | <0.001 | 144.9 ± 34.6 | 141.2 ± 23.1 | 139.0 ±29.2 | 156.4 ± 30.3 | <0.001 |
| 2-h glucose (mg/dL) | 287.9 ± 55.2 | 283.4 ± 53.8 | 295.9 ± 56.7 | <0.001 | 278.7 ± 62.8 | 285.6 ± 53.3 | 272.7 ± 59.3 | 292.6 ± 53.1 | <0.001 |
| Fasting insulin (mU/L) | 21.5 ± 14.8 | 21.4 ± 15.1 | 21.6 ± 14.4 | 0.847 | 27.0 ± 17.5 | 16.2 ± 10.1 | 18.6 ± 13.1 | 22.5 ± 15.5 | <0.001 |
| Metformin dose at screening (mg/day) | 1,586.6 ± 525.0 | 1,602.5 ± 521.7 | 1,558.3 ± 529.9 | 0.025 | 1,648.1 ± 499.9 | 1,558.0 ± 527.6 | 1,494.9 ± 544.7 | 1,623.9 ± 513.3 | <0.001 |
| Systolic BP (mmHg) | 128.1 ± 14.6 | 128.8 ± 14.6 | 126.9 ± 14.6 | <0.001 | 122.3 ± 11.1 | 126.8 ± 15.2 | 128.6 ± 15.0 | 128.7 ± 14.3 | <0.001 |
| Diastolic BP (mmHg) | 77.2 ± 9.8 | 77.7 ± 9.7 | 76.3 ± 9.8 | <0.001 | 78.2 ± 7.8 | 78.6 ± 10.1 | 78.3 ± 10.4 | 76.9 ± 9.6 | 0.005 |
| Total cholesterol (mg/dL) | 162.8 ± 37.2 | 157.9 ± 37.3 | 171.6 ± 35.3 | <0.001 | 161.0 ± 28.4 | 164.0 ± 35.9 | 166.7 ± 35.8 | 161.7 ± 38.0 | 0.038 |
| HDL (mg/dL) | 43.4 ± 10.6 | 41.0 ± 9.3 | 47.6 ± 11.5 | <0.001 | 41.8 ± 7.5 | 44.9 ± 9.7 | 48.2 ± 12.3 | 42.0 ± 10.0 | <0.001 |
| LDL (mg/dL) | 89.6 ± 31.3 | 86.1 ± 30.8 | 95.7 ± 31.1 | <0.001 | 88.9 ± 24.1 | 92.4 ± 30.2 | 97.6 ± 31.5 | 86.9 ± 31.2 | <0.001 |
| TG (mg/dL) | 154.2 ± 124.1 | 160.1 ± 138.2 | 143.8 ± 93.3 | <0.001 | 153.2 ± 73.3 | 136.2 ± 73.8 | 105.4 ± 69.7 | 169.5 ± 135.7 | <0.001 |
| ACE/ARB | 1,350 (43.4) | 923 (46.5) | 427 (38.0) | <0.001 | 49 (47.6) | 35 (29.4) | 240 (43.4) | 925 (44.4) | 0.012 |
| Diuretics | 722 (23.2) | 464 (23.4) | 258 (23.0) | 0.818 | 3 (2.9) | 21 (17.6) | 157 (28.4) | 497 (23.8) | <0.001 |
| β-Blockers | 560 (18.0) | 396 (20.0) | 164 (14.6) | <0.001 | 8 (7.8) | 16 (13.4) | 95 (17.2) | 415 (19.9) | 0.004 |
| Calcium channel blockers | 428 (13.8) | 292 (14.7) | 136 (12.1) | 0.048 | 4 (3.9) | 15 (12.6) | 125 (22.6) | 263 (12.6) | <0.001 |
| Statins | 1,950 (62.7) | 1,333 (67.2) | 617 (54.9) | <0.001 | 31 (30.1) | 79 (66.4) | 319 (57.7) | 1,383 (66.4) | <0.001 |
| Fibrates | 97 (3.1) | 72 (3.6) | 25 (2.2) | 0.040 | 1 (1.0) | 1 (0.8) | 6 (1.1) | 82 (3.9) | 0.001 |
| Matsuda Index ([µU · mg/dL2]−1) | 2.1 ± 1.4 | 2.2 ± 1.5 | 2.1 ± 1.4 | 0.015 | 1.7 ± 1.1 | 2.5 ± 1.4 | 2.5 ± 1.6 | 2.0 ± 1.4 | <0.001 |
| HOMA2-S | 56.5 ± 40.6 | 57.5 ± 41.7 | 54.8 ± 38.6 | 0.075 | 44.1 ± 31.4 | 69.9 ± 40.9 | 64.3 ± 42.6 | 54.2 ± 39.9 | <0.001 |
| HOMA2-B | 67.7 ± 37.0 | 66.5 ± 37.4 | 69.8 ± 36.1 | 0.015 | 90.7 ± 49.8 | 61.4 ± 29.5 | 71.6 ± 38.6 | 66.0 ± 36.2 | <0.001 |
| IGI (µU/mg) | 33.8 ± 27.9 | 32.6 ± 27.4 | 35.9 ± 28.8 | 0.002 | 52.7 ± 37.3 | 32.3 ± 28.4 | 40.0 ± 32.1 | 31.3 ± 25.0 | <0.001 |
| CPI (nmol/g) | 0.7 ± 0.5 | 0.7 ± 0.5 | 0.8 ± 0.5 | 0.046 | 1.1 ± 0.7 | 0.7 ± 0.5 | 0.9 ± 0.6 | 0.7 ± 0.5 | <0.001 |
| Late insulin response (pmol/mol) | 40.3 ± 35.0 | 39.1 ± 34.3 | 42.4 ± 36.0 | 0.013 | 54.6 ± 47.5 | 42.8 ± 33.6 | 45.8 ± 38.4 | 37.9 ± 33.0 | <0.001 |
| DI (mL/mg) | 1.91 ± 1.55 | 1.85 ± 1.51 | 2.01 ± 1.60 | 0.009 | 2.33 ± 1.82 | 2.20 ± 1.67 | 2.57 ± 1.95 | 1.69 ± 1.32 | <0.001 |
| Insulin clearance (µmol/pmol) | 12.5 ± 4.6 | 12.7 ± 4.6 | 12.2 ± 4.6 | 0.003 | 11.3 ± 4.0 | 12.6 ± 3.4 | 11.6 ± 4.2 | 12.9 ± 4.8 | <0.001 |
Data are mean ± SD or n (%) unless otherwise indicated. The χ2 test of independence was used for qualitative variables. The Student t test with unequal variances was used for quantitative variables comparing men vs. women and the ANOVA F test for quantitative variables in racial groups. Any racial group with <100 members was excluded from this analysis.
ARB, angiotensin receptor blocker; BP, blood pressure; CPI, C-peptide index.
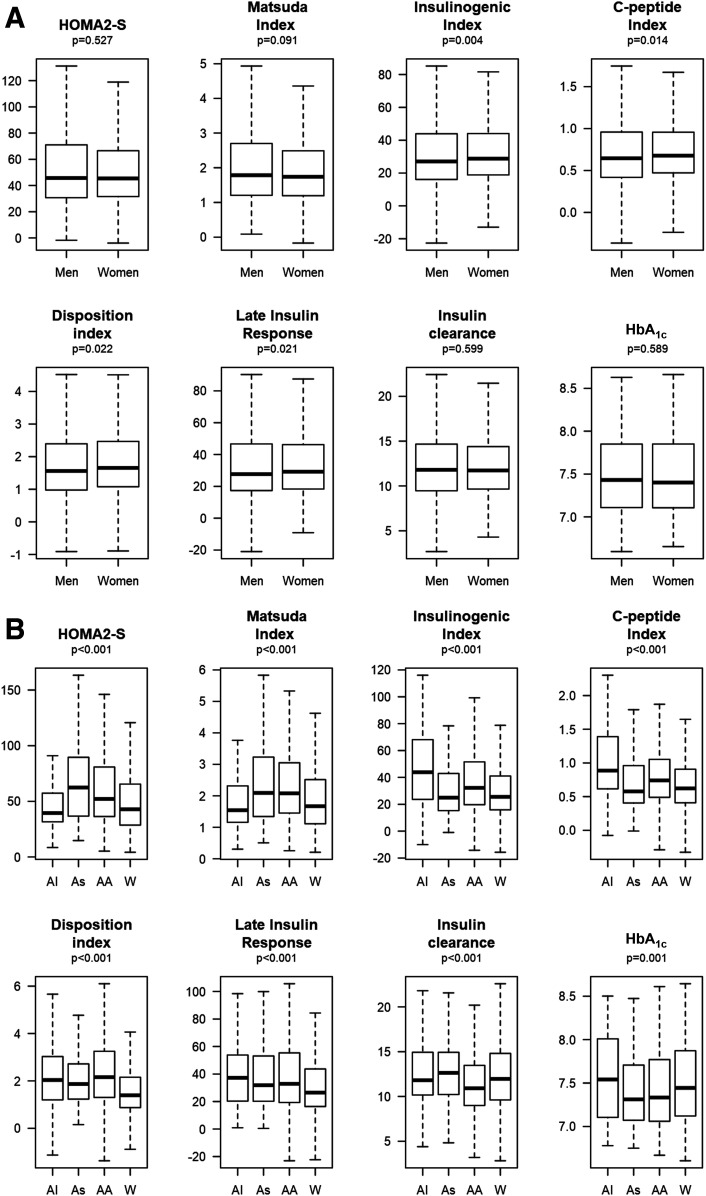
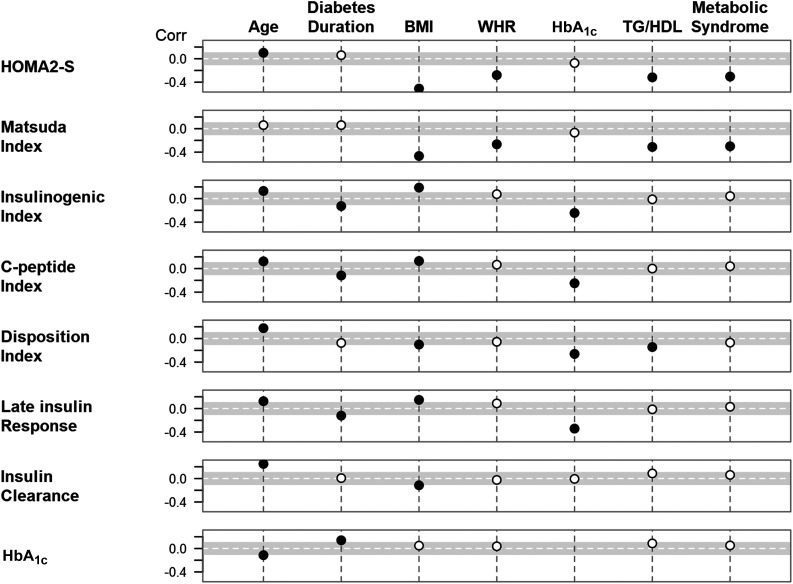
The P values for the sex-based difference in Fig. 1A are from a least-squares regression of the ranks of each of the responses on sex adjusted for age, race, and diabetes duration in the combined cohort. The box plots are based on the residuals from ordinary regression models of each response on age, race, and diabetes duration. The P values in Fig. 1B are from a least-squares regression of the ranks of each of the responses on racial categories adjusted for sex, age, and diabetes duration. The box plots are based on the residuals from ordinary regression models of each response on age, sex, and diabetes duration. In Fig. 2, the Spearman correlation between two responses is computed as the Pearson correlation of the residuals from separate linear regression models of the ranks of each response on age, sex, race, and diabetes duration. Correlations with the IGI, C-peptide index, and late insulin response are adjusted for insulin sensitivity (HOMA2-S). In order to eliminate significant correlations that are not clinically meaningful, any correlations with r < 0.1 in absolute value are considered clinically nonsignificant even if they were statistically significant at the 0.05 level.
Figure 1.
A: Distributions of insulin sensitivity, insulin and C-peptide responses, insulin clearance, and HbA1c for men and women. The box plots are adjusted for age, race, and diabetes duration. The P values are for comparisons between men and women adjusted for covariates including age, race, and diabetes duration. B: Distributions of insulin sensitivity, insulin and C-peptide responses, insulin clearance, and HbA1c by race for American Indian (AI), Asian (As), Black/African American (AA), and White (W). The box plots are adjusted for age, sex, and diabetes duration. The P values are for comparisons among different races adjusted for covariates including age, sex, and diabetes duration.
Figure 2.
Partial Spearman correlations (Corr) of measures of insulin sensitivity and insulin/C-peptide response with participant characteristics. Correlations are adjusted for age, sex, race, and diabetes duration (excluding the variable being correlated with insulin response or sensitivity). Insulin and C-peptide responses (IGI, C-peptide index, late insulin response, and insulin clearance) are also adjusted for HOMA2-S. The gray band marks correlations that are smaller than ±0.1, and the dotted line marks the correlation of 0. Partial correlations are shown as a black dot if they are nominally significant at the 0.05 level and at least 0.1 in absolute value and as a white dot otherwise. There were no meaningful correlations with diuretics, β-blockers, calcium channel blockers, statins, or fibrates.
Measures of insulin, HOMA2-S, HOMA2-B, Matsuda Index, insulinogenic and C-peptide indices, late insulin response, and the DI included some extreme outliers. To reduce the influence of outliers on analyses, these variables were winsorized (i.e., values above or below specified cutoffs were replaced by cutoffs) (19). For each variable, the winsorization upper (lower) cutoff was set to the median plus (minus) 8.9 times the distance from the median to the upper (lower) quartiles. For a normally distributed variable, this would result in cutoffs 6 SDs above and below the mean. The number of winsorized values ranged from 5 (0.2%) to 26 (0.8%). Analyses were performed using R version 3.6.0.
Results
Differences in Phenotypic and Metabolic Characteristics by Sex and Race
Table 1 shows characteristics of the cohort stratified by sex and race. Overall, the majority were male, on average middle-aged, obese, and had known diabetes for 4.0 ± 2.8 years. There were no differences between men and women in HbA1c or fasting insulin, but men had significantly higher fasting but lower 2-h glucoses and higher HOMA2-S but lower IGI (Table 1). Adjusting for all of these factors yields mean HbA1c values of 7.55 ± 0.02 (mean ± SE) among men versus 7.54 ± 0.02 among women (P ≤ 0.83). Men had lower BMI but greater waist-to-hip ratio (WHR) compared with women. In addition, men had higher systolic and diastolic blood pressures, despite reporting more prevalent use of blood pressure–lowering medications. They also had higher TG levels but lower cholesterol levels (total, LDL, and HDL) and reported more prevalent use of lipid-lowering medications (Table 1).
There were also racial differences in characteristics (Table 1). American Indians/Alaska Natives were the youngest, reflecting their lower age inclusion criterion, and they had the shortest duration of diabetes. Asians had the lowest BMI, and American Indians/Alaska Natives had the highest BMI. There were also significant differences in the use of blood pressure and lipid medications among races (Table 1).
There were small but significant racial differences in HbA1c (≤0.2%; P = 0.004) (Table 1) and differences in fasting and 2-h glucose, fasting insulin, HOMA2-S, and IGI (Fig. 1B). Unadjusted, the American Indians/Alaska Natives had the highest HbA1c value (7.59%). This was followed by White (7.51%) and Black/African American (7.44%). The pairwise comparisons of Black/African American versus American Indians/Alaska Natives (P = 0.006) and versus White (P = 0.004) were significant. However, when adjusted for the fasting and 2-h glucoses, the Black/African American had higher HbA1c than Whites (7.53% vs. 7.48%; P = 0.009). These results were virtually unchanged with further adjustment for sex, fasting insulin, HOMA2-S, and the IGI.
In additional analyses, the 423 Hispanic White and 1,651 non-Hispanic White groups had mean HbA1c of ∼7.5%, but the estimates differed significantly when adjusted for fasting and 2-h glucose levels (7.46% vs. 7.56%; P < 0.001). Adjusted for glucoses, the mean HbA1c among the Black/African American (7.54%) was not different from that of the Hispanic White (7.56%) but was significantly higher than that of the non-Hispanic White (7.46%; P < 0.001).
Differences in Insulin Sensitivity and β-Cell Function by Sex and Race
After adjustment for age, race, and diabetes duration, DI was higher in women than men (P = 0.022) (Fig. 1A). The IGI (P = 0.004), C-peptide index (P = 0.014), and late insulin responses (P = 0.021) were also higher in women (P = 0.045) (Fig. 1A). There were no differences between men and women in insulin sensitivity quantified as HOMA2-S (P = 0.527) and the Matsuda index (P = 0.091), basal insulin clearance (P = 0.138), or HbA1c (P = 0.460) (Fig. 1A).
After adjustment for age, sex, and diabetes duration, DI was the highest in Black/African Americans followed by American Indians/Alaska Natives, Asians, and Whites in descending order (Fig. 1B). Asians had the highest insulin sensitivity (by HOMA2-S). Black/African Americans and American Indians/Alaska Natives had higher insulin and C-peptide responses than the others (Fig. 1B). Whites had the lowest late insulin response, while Black/African Americans had the lowest insulin clearance (Fig. 1B).
Association of Insulin Sensitivity and β-Cell Function With Selected Phenotypic Characteristics
Figure 2 presents the correlations of participant characteristics with measures of insulin sensitivity and β-cell function. BMI and WHR were inversely correlated with insulin sensitivity (r = −0.51 and r = −0.47 for HOMA2-S and Matsuda with BMI, respectively; r = −0.28 and r = 0.27 for WHR, P < 0.001 for both). The correlation of both BMI and WHR with insulin sensitivity was greater in men than women (r = −0.55 vs. r = −0.44 and r = −0.53 vs. r = −0.36 for HOMA2-S and Matsuda index, respectively, P < 0.001 for both) (Supplementary Tables 1 and 2). Insulin sensitivity also correlated inversely with the triglyceride-to-HDL-cholesterol ratio (TG/HDL-C) (r = −0.32 with HOMA2-S and r = −0.31 with Matsuda, P < 0.001 for both) and presence of metabolic syndrome (r = −0.30 for both HOMA2-S and Matsuda, P < 0.001) (Fig. 2 and Supplementary Tables 1 and 2). Again, the association of insulin sensitivity with either lower TG/HDL-C ratio or the absence of metabolic syndrome was greater in men (Supplementary Tables 1 and 2). The correlations of metabolic syndrome and TG/HDL-C ratio with insulin sensitivity were greater in Black/African Americans than Whites (Supplementary Tables 1 and 2). Age, diabetes duration, and HbA1c were not associated with insulin sensitivity (Fig. 2).
DI was positively associated with age (r = 0.18; P < 0.001) while negatively correlated with BMI, HbA1c, and the TG/HDL-C ratio (r = −0.10, r = −0.26, and r = −0.15 respectively, P < 0.001 for all) (Fig. 2 and Supplementary Table 5). The association of DI with age, BMI, HbA1c, or the TG/HDL-C ratio was stronger in Whites than Black/African Americans (Supplementary Table 5).
Age also had a positive association with markers of β-cell responses, including IGI (r = 0.13), C-peptide index (r = 0.12), late insulin response (r = 0.13), and insulin clearance (r = 0.25, P < 0.001 for all) (Fig. 2 and Supplementary Tables 3–8). The association of age with measures of β-cell response (IGI, C-peptide index, and late insulin response) was stronger in Whites than Black/African Americans (Supplementary Tables 3, 4, and 6). BMI was associated directly with the IGI (r = 0.19), C-peptide index (r = 0.13), and late insulin response (r = 0.15) but inversely with insulin clearance (r = −0.13, P < 0.001 for all) (Fig. 2 and Supplementary Table 3). The association of BMI with measures of β-cell response (IGI, C-peptide index, and late insulin response) was stronger in men than women and not different between Whites and Black/African Americans (Supplementary Tables 3, 4, and 6).
Diabetes duration was inversely correlated with markers of β-cell responses, including IGI (r = −0.13), C-peptide index (r = −0.12), and late insulin response (r = −0.12, P < 0.001 for all) (Fig. 2 and Supplementary Tables 2–6).
HbA1c was not correlated with insulin sensitivity, but was inversely correlated with other measures of β-cell function (r = −0.26 for DI, r = −0.24 for IGI, r = −0.25 for C-peptide index, and r = −0.34 for late insulin response, P < 0.001) (Supplementary Tables 1–7). HbA1c was also negatively correlated with increasing age (r = −0.11) and increasing diabetes duration (r = −0.14, P < 0.001 for both).
Neither treatment for hypertension (ACE/angiotensin receptor blocker, diuretics, β-blockers, or calcium channel blockers) nor dyslipidemia (statins or fibrates) was associated with insulin response or sensitivity (Supplementary Tables 1–7).
Conclusions
In the GRADE cohort, there were modest differences between men and women in insulin sensitivity, insulin clearance, and β-cell function in unadjusted models (Table 1). However, with the exception of β-cell function, sex differences in insulin sensitivity and clearance attenuated when adjusted for age, race, and diabetes duration (Fig. 1A). There was also no sex difference in HbA1c even though men had a higher fasting glucose and lower 2-h glucose.
In unadjusted analyses, we observed small racial differences in HbA1c, with higher levels among Whites. However, after adjusting for fasting and 2-h glucose levels, the Black/African Americans had a slightly higher mean HbA1c than Whites (7.53% vs. 7.48%). In an analysis of Hispanic and non-Hispanic White separately, adjusted for glucoses, the difference between Black/African American and non-Hispanic White was equivalent to that in the full cohort (7.54% vs. 7.46%). Others have also reported interracial and interethnic differences in the relationship of average glycemia and HbA1c (7,9,10,20,21). Most studies, with rare exceptions (22,23), have not collected reliable measures of average glycemia and have not evaluated differences in red blood cell turnover or genetic variation in hemoglobin glycation as plausible mechanisms (24,25). To further investigate the relationship of average glucose and HbA1c among different racial/ethnic groups, continuous glucose monitoring and evaluation of red blood cell age and turnover studies will be completed in a subgroup of the GRADE cohort, which should help to distinguish the contribution of abnormalities in red blood cell turnover from differences in glycation (26).
There were also significant racial differences in insulin sensitivity and β-cell function as well as the early insulin and C-peptide responses, late insulin response, and insulin clearance in the fasting state. Black/African Americans were more insulin sensitive than Whites, but Black/African Americans had higher insulin and C-peptide responses compared with others, resulting in the highest DI among different races. These racial differences in β-cell function, as well as HbA1c, persisted when adjusted for basic factors.
Racial differences in β-cell function have been previously reported (20,27–30). The ADOPT study (20) enrolled 4,360 participants with type 2 diabetes aged 30–75 years (mean 57 years) of <3 years’ duration on diet therapy alone with plasma glucose 7–10 mmol/L. In the subset of patients from North America, compared with the 1,815 Caucasians, Blacks had a higher HbA1c (8.0% vs. 7.3%) and lower fasting insulin and higher insulin secretory index despite no difference in fasting glucose.
In a systematic review, Kodama et al. (27) analyzed data from 74 study cohorts comprising 3,800 individuals, the majority being without diabetes, and reported that Black/African Americans without diabetes had robust insulin responses to reduced insulin sensitivity, while East Asians were insulin sensitive and thus required less robust insulin responses. However, racial differences in insulin sensitivity and β-cell responses were less prominent in individuals with type 2 diabetes, but the study was limited to relatively small number of individuals with type 2 diabetes (11 cohorts, n = 255).
The etiology for these racial differences remains unknown. Decreased insulin clearance in Black/African Americans, as seen in our cohort, has been proposed as one of the mechanisms for the higher insulin response (31). This study suggested that the racial differences in insulin clearance were due to decreased hepatic extraction of insulin during the first pass and not the extrahepatic component of insulin clearance (31). Proposed mechanisms for this racial difference include decreased expression/activity of insulin-degrading enzyme and/or carcinoembryonic antigen-related cell adhesion molecule-1, which enhances the rate of uptake of the insulin receptor complex, and reduced hepatic insulin receptor number or activity (31,32). The higher C-peptide responses in Black/African Americans suggests that other mechanisms are also likely involved because C-peptide is not degraded by the liver (33,34). Racial differences in body size (height, weight, and BMI), body composition, and fat distribution have been proposed as potential contributors to racial differences in insulin sensitivity or insulin response (35). Whether the difference in DI in Black/African Americans represents an adaptation to a reduction in glucose uptake or other mechanisms independent of insulin, such as genetic variation, cannot be discerned from these data. However, genome-wide association studies have reported that racial differences exist in the association between genetic variation and T2D risk (36,37).
In the GRADE cohort, age (positively) and BMI, TG/HDL-C ratio, and HbA1c (inversely) were correlated with β-cell function. Among baseline characteristics, HbA1c had the strongest correlation with DI, consistent with the long-held belief that β-cell function plays an important role in determining glycemic control. This observation is in keeping with other studies, including a cross-sectional analysis comprising four ethnic groups in the U.S. with varying glucose tolerance in whom DI was most strongly associated with the 2-h glucose (28). It is also consistent with a study involving a large group of people with newly diagnosed, drug-naive type 2 diabetes in whom more severe β-cell dysfunction was associated with a higher baseline HbA1c and a greater risk of glycemic progression (38). Older individuals with type 2 diabetes in the GRADE cohort had a higher insulin response and DI. Our finding of the direct association of age with β-cell function is not supported by epidemiologic studies that have shown a higher prevalence of diabetes with increasing age (39). This is likely the result of a decreased ability of the β-cells to maintain adequate insulin responses for metabolic demand over time (40). The most likely explanation is that older individuals in the GRADE Study had less severe disease, which is supported by the negative correlation between age and HbA1c, and thus may have better β-cell function at the time of the study. There is also the possibility that the inclusion criteria imposed by the study design excluded older individuals who had worse β-cell function and failed metformin earlier (39).
Although BMI correlated with DI inversely, there was direct association of BMI with IGI and C-peptide response. The association remained significant after adjusting for age, sex, race, diabetes duration, and HOMA2-S, suggesting that obesity might be associated with higher β-cell response beyond what was expected for decreased insulin sensitivity. The inverse association of BMI with DI was likely driven by the stronger reverse association of insulin sensitivity with BMI dominating the direct association of BMI with β-cell response.
Similar to our findings, Ferrannini et al. (41) reported higher fasting insulin in obese compared with lean individuals without diabetes and the difference remained significant after adjusting for insulin sensitivity. They also reported significantly lower insulin clearance in obesity independent of insulin sensitivity (41), suggesting that peripheral hyperinsulinemia in obese subjects may reflect both insulin hypersecretion and reduced insulin clearance.
Although diabetes duration correlated inversely with insulin and C-peptide responses in this cohort, it did not correlate significantly with DI. This could be related to the relatively short duration of diabetes and narrow range of diabetes duration dictated by the GRADE Study inclusion criteria.
Similar to the previous studies (42,43), we confirm the inverse association between TG/HDL-C ratio and insulin sensitivity. Additionally, we report an inverse association of TG/HDL-C ratio with β-cell function. This association was previously reported only in a small study limited to Black/African American women (44). However, this information should be considered with some caution, as the majority of participants were treated with statins (63%) or other lipid-lowering medications such as fibrates (3%). Our study also investigated sex and racial differences in the correlation between baseline characteristics with insulin sensitivity and β-cell function. We reported that the association between insulin sensitivity and traditional clinical markers including BMI, presence of metabolic syndrome, and TG/HDL-C ratio is stronger in men than women.
In addition, correlation of BMI with β-cell function and insulin and C-peptide responses were stronger in men, suggesting that there might be a need for different BMI cutoffs for risk evaluation based on sex. Epidemiologic studies have also reported a sex-related disparity in the prevalence of metabolic syndrome and type 2 diabetes (45). Women are diagnosed with type 2 diabetes at a higher BMI than men (46), suggesting that obesity could be defined differently according to sex, similar to the different cutoff values of waist circumference for men and women. We also reported racial differences in the correlation of β-cell function with baseline characteristics. The association of DI with HbA1c and TG/HDL-C ratio was stronger in Whites compared with Black/African Americans, which could be the result of racial variation in glycation (6) and racial differences in lipid metabolism (47). Furthermore, BMI and age correlated with DI in the entire cohort and in Whites, but were not associated with DI in Black/African Americans, suggesting racial differences in the regulation of β-cell function.
Our study has several strengths, including the large and racially diverse cohort of adults early in the course of diabetes with a relatively short duration of type 2 diabetes of <10 years and HbA1c of 6.8–8.5% while using metformin monotherapy. This cohort provided the opportunity to investigate the association of several characteristics with β-cell function, which was evaluated using both fasting and post–glucose load β-cell responses at several time points during an OGTT. Insulin and C-peptide assays were performed at a central laboratory, which minimized interassay variabilities. The study cohort also includes both men and women and adequate representation from a range of ethnic and racial groups. Further, the cohort represents a sample of subjects with early type 2 diabetes treated with metformin alone that is comparable to the general U.S. population selected to include individuals who meet the principal GRADE eligibility criteria (48).
However, a limitation is that the selective nature of the cohort may limit generalizability to the general population of those with longer diabetes duration who have already been treated with multiple glycemic-lowering medications. Another limitation is that β-cell function and insulin sensitivity were not evaluated using more precise methods such as the euglycemic/hyperglycemic clamp or the frequently sampled intravenous glucose tolerance test. However, measures of insulin sensitivity and β-cell function derived from the OGTT are reported to agree well with those from the euglycemic insulin clamp (14,49). The higher variability in β-cell function measures using an OGTT was likely mitigated by the large sample size in this study. We were unable to calculate hepatic insulin extraction using more sophisticated methods and estimated only fasting hepatic clearance. In addition, information regarding menopausal status was unavailable, but the analysis was adjusted for age.
In conclusion, in a large cohort of participants with type 2 diabetes, insulin response measures were differentially correlated with age, BMI, and HbA1c. There were racial differences in these responses as well as insulin sensitivity and insulin clearance that jointly may explain previously observed racial differences in the level of HbA1c. The underlying mechanisms regulating the racial differences in insulin sensitivity, β-cell function, and insulin clearance are not totally clear. As such, more studies are needed addressing the mechanisms responsible for these differences. Understanding potential differences in these mechanisms could in time lead to more personalized approaches to diabetes care.
Article Information
Funding. The GRADE Study is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number U01-DK-098246. The planning of GRADE was supported by a U34 planning grant from the National Institute of Diabetes and Digestive and Kidney Diseases (U34-DK-088043). The American Diabetes Association supported the initial planning meeting for the U34 proposal. The National Heart, Lung, and Blood Institute and the Centers for Disease Control and Prevention also provided funding support. The Department of Veterans Affairs provided resources and facilities. Additional support was provided by grants P30 DK017047, P30 DK020541-44, P30 DK020572, P30 DK072476, P30 DK079626, P30 DK092926, U54 GM104940, UL1 TR000439, UL1 TR000445, UL1 TR001108, UL1 TR001409, UL1 TR001449, UL1 TR002243, UL1 TR002345, UL1 TR002378, UL1 TR002489, UL1 TR002489, UL1 TR002529, UL1 TR002535, UL1 TR002537, and UL1 TR002548. Educational materials have been provided by the National Diabetes Education Program. Material support in the form of donated medications and supplies has been provided by Becton, Dickinson and Company, Bristol-Myers Squibb, Merck, Novo Nordisk, Roche Diagnostics, and Sanofi.
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Duality of Interest. N.R. reports grants and other support from Novo Nordisk, outside the submitted work. K.M.U. reports other support from Medtronic and personal fees from Novo Nordisk, outside the submitted work. S.E.I. reports personal fees from Merck; personal fees and nonfinancial support from Boehringer Ingelheim, AstraZeneca, and Novo Nordisk; and personal fees from Sanofi/Lexicon Pharmaceuticals, Abbott/Alere, and vTv Therapeutics, outside the submitted work. R.M.C. reports grants from the National Institutes of Health, during the conduct of the study, other support from Bristol-Myers Squibb, and other support from Pfizer, outside the submitted work. S.E.K. reports grants from the National Institutes of Health, during the conduct of the study, and personal fees from Boehringer Ingelheim, Eli Lilly and Company, Intarcia Therapeutics, Janssen, Merck, Novo Nordisk, and Pfizer, outside the submitted work. No other potential conflicts of interest were reported.
Author Contributions. N.R. contributed to the conception and design of the research, acquisition of data, interpretation of data and results, supervision and management of research, and drafting of the manuscript. N.Y. contributed to the conception and design of the research, statistical analysis of data, interpretation of data and results, and drafting of the statistical sections of the manuscript. K.M.U. contributed to the acquisition of data, interpretation of data and results, supervision and management of research, and critical revision of the manuscript. S.E.I., A.L.C., F.I.-B., and D.E.O. contributed to the interpretation of data and results and the critical revision of the manuscript. A.B. contributed to the conception and design of the research, interpretation of data and results, and critical revision of the manuscript. R.M.C. and R.A.D. contributed to the interpretation of data and results, drafting of the manuscript, and critical revision of the manuscript. W.H.H. contributed to the acquisition of data, interpretation of data and results, acquisition of funding, supervision and management of research, and the critical revision of the manuscript. J.M.L. contributed to the conception and design of the research, statistical analysis of data, interpretation of data and results, acquisition of funding, supervision and management of research, and the critical revision of the manuscript. S.E.K. contributed to the conception and design of the research, statistical analysis of data and results, interpretation of data and results, and drafting of parts of the manuscript. All authors affirm that authorship is merited based on the International Committee of Medical Journal Editors authorship criteria. N.R. and N.Y. are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. This study was presented in abstract form at the 78th Scientific Sessions of the American Diabetes Association, Orlando, FL, 22–26 June 2018.
Footnotes
A complete list of GRADE Research Group members is included in the supplementary material online.
Clinical trial reg. no. NCT01794143, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.13247033.
Contributor Information
Collaborators: GRADE Research Group, Jill P. Crandall, Melissa Diane McKee, Janet Brown-Friday, Entila Xhori, Keisha Ballentine-Cargill, Sally Duran, Jennifer Lukin, Stephanie Beringher, Susana Gonzalez de la torre, Lawrence Phillips, Elizabeth Burgess, Darin Olson, Mary Rhee, Peter Wilson, Tasha Stephanie Raines, Julie Costello, Chona Gullett, Maxine Maher-Albertelli, Folayan Morehead, Radhika Mungara, Saranjit Person, Louise Savoye, Mabil Sibymon, Sridhar Tanukonda, Carol Ann White, Leah Holloway, Cynthia Adams, April Ross, Ashok Balasubramanyam, Erica Gonzalez, Charlyne Wright, Priscilla Hollander, Erin Roe, Analyn Uy, Polly Burt, Lorie Estrada, Kris Chionh, Faramarz Ismail-Beigi, Corinna Falck-Ytter, Laure Sayyed Kassem, Ajay Sood, Margaret Tiktin, Bethany Cramer, Jacalyn Iacoboni, Maria V. Kononets, Tanya Kulow, Cynthia Newman, Katherine A. Stancil, Cristina Sanders, Lisa Tucker, Amanda Werner, Adrienne Krol, Gloria McPhee, Christine Patel, Linda Colosimo, Robin Goland, James Pring, Patricia Kringas, Jessica Tejada, Camille Hausheer, Harvey Schneier, Kelly Gumpel, Amanda Kirpitch, Jennifer B. Green, Hiba AbouAssi, Ranee Chatterjee, Mark N. Feinglos, Jennifer English Jones, Shubi A. Khan, Jeanne B. Kimpel, Ronna P. Zimmer, Mary Furst, Barbara M. Satterwhite, Connie R. Thacker, Kathryn Evans Kreider, Kieren J. Mather, Amale Lteif, Tonya Hamilton, Nick Patel, Gabriela Riera, Marcia Jackson, Vivian Pirics, Devin Howard, Danielle Aguillar, Sloan Hurt, Richard Bergenstal, Anders Carlson, Thomas Martens, Mary Johnson, Renae Hill, Jamie Hyatt, Connie Jensen, Marcia Madden, Dianna Martin, Holly Willis, Wanda Konerza, Rebecca Passi, Kathleen Kleeberger, Stephen Fortmann, Michael Herson, Karen Mularski, Harry Glauber, James Prihoda, Britt Ash, Christina Carlson, Phyllis Anne Ramey, Emily Schield, Britta Torgrimson-Ojerio, Kathy Arnold, Bryan Kauffman, Elease Panos, Samantha Sahnow, Kristi Bays, Jennifer Cook, Jennifer Gluth, Debra Sasaki, Katrina Schell, Jennifer Criscola, Camille Friason, Suzi Jones, Sergey Nazarov, Joshua Barzilay, Negah Rassouli, Rachel Puttnam, Michelle Curtis, Kia Stokes, Bonita Hollis, Cynthia Sanders-Jones, Roslin Nelson, Zakiah El-Haqq, Abby Kolli, Tu Tran, Deborah Wexler, Mary Larkin, James Meigs, Amy Dushkin, Gianna Rocchio, Brittany Chambers, Mike Yepes, Barbara Steiner, Hilary Dulin, Melody Cayford, Andrea DeManbey, Lindsey Gurry, Mallory Hillard, Kimberly Martin, Christine Stevens, Nopporn Thangthaeng, Raquel Kochis, Elyse Raymond, Valerie Ripley, Jean Park, Vanita Aroda, Adline Ghazi, Amy Loveland, Maria Hurtado, Alexander Kuhn, Florence Mofor, Hermes J. Florez, Willy Marcos Valencia, Jennifer Marks, Lisset Oropesa-Gonzalez, Ana K. Riccio Veliz, Ramfis Nieto-Martinez, Miriam Gutt, Andrew Ahmann, Diana Aby-Daniel, Farahnaz Joarder, Victoria Morimoto, Carol Sprague, Daisuke Yamashita, Nancy Cady, Patricia Kirchhoff, Nadia Rivera-Eschright, Joseph Adducci, Brianna Morales Gomez, Alina Goncharova, Sophia H. Hox, Helen Petrovitch, Michael Matwichyna, Victoria Jenkins, Nina O. Bermudez, Renée R. Ishii, Daniel S. Hsia, William T. Cefalu, Frank L. Greenway, Celeste Waguespack, Erin King, Natalie Haynes, Amy Thomassie, Brandi Bourgeois, Claire Hazlett, Robert Henry, Sunder Mudaliar, Schafer Boeder, Jeremy Pettus, Elsa Diaz, Catherine DeLue, Erick Castro, Sylvia Hernandez, Jonathan Krakoff, Jeffrey M. Curtis, Tina Killean, Erica Joshevama, Enrique Diaz, Denelle Martin, Tracey Karshner, Jeanine Albu, F. Xavier Pi-Sunyer, Sylvaine Frances, Carol Maggio, Emily Ellis, Joseph Bastawrose, Xiuqun Gong, Mary Ann Banerji, Phyllis August, Daniel Lorber, Necole M. Brown, Debra H. Josephson, Lorraine L. Thomas, Mari Tsovian, Ajini Cherian, Marlo H. Jacobson, Motria M. Mishko, M. Sue Kirkman, Katherine Bergamo, John B. Buse, Jean Dostou, Laura Young, April Goley, Jeffrey Kerr, Joseph F. Largay, Sonia Guarda, Juanita Cuffee, Dawn Culmer, Rachael Fraser, Hope Almeida, Samantha Coffer, Elizabeth Debnam, Lauren Kiker, Sarah Morton, Kim Garvey, Gai Fuller, W. Timothy Garvey, Andrea Cherrington, Dana Golson, Olivia Griffith, Mary Robertson Catherine, April Agne, Steve McCullars, Robert M. Cohen, Jacqueline Craig, Kimberly Kersey, M. Colleen Rogge, Carla Wilson, Kathryn Burton, Sonia Lipp, Vonder Meulen Mary Beth, Neda Rasouli, Emily Schroeder, Stephanie Steiner, Chelsea Baker, Chantal Underkofler, Sara Douglass, William Sivitz, Erin Cline, Laura Knosp, Jennifer McConnell, Tamara Lowe, William H. Herman, Rodica Pop-Busui, Meng H. Tan, Catherine Martin, Andrea Waltje, Lynn Goodhall, Rebecca Eggleston, Shihchen Kuo, Stephanie Bule, Nancy Kessler, Elizabeth LaSalle, Elizabeth R. Seaquist, Anne Bantle, Anjali Kumar, Bruce Redmon, John Bantle, Tasma Harindhanavudhi, Mary Coe, Michael Mech, Abdisa Taddese, Lesia Lesne, Shannon Smitha, Cyrus Desouz, Lisa Kuechenmeister, Vijay Shivaswamy, Ana Laura Morales, Maria Grace Rodriguez, Kris Seipel, Alissa Alfred, Jenna Eggert, Grace Lord, William Taylor, Renee Tillson, David S. Schade, Allen Adolphe, Mark Burge, Elizabeth Duran-Valdez, Janae Martinez, Doris Hernandez McGinnis, Benjamin Pucchetti, Elizabeth Scripsick, Ralph A. DeFronzo, Eugenio Cersosimo, Muhammad Abdul-Ghani, Curtis Triplitt, Hector Verastiqui, Rosa Irene Garza, Kathryn Wright, Curtiss Puckett, Philip Raskin, Chanhaeng Rhee, Soma Abraham, Lin Fan Jordan, Serey Sao, Luisa Morton, Oralenda Smith, Laura Osornio Walker, Laura Schnurr-Breen, Rosa Ayala, Robert Brian Kraymer, Daytheon Sturgess, Kristina M. Utzschneider, Steven E. Kahn, Lorena Alarcon-Casas Wright, Edward J. Boyko, Elaine C. Tsai, Dace L. Trence, Basma N. Fattaleh, Brenda K. Montgomery, Karen M. Atkinson, Tessa Concepcion, Alexandra Kozedub, Cameron Moak, Samantha Rhothisen, Tom A. Elasy, Stephanie Martin, Laura Shackelford, Rita Goidel, Nina Hinkle, Janie Lipps Hogan, Cynthia Lovell, Janet Myers, Janet B. McGill, Maamoun Salam, Sarah Kissel, Toni Schweiger, Carol Recklein, William Tamborlane, Patricia Gatcomb, Anne Camp, Barbara Gulanski, Silvio Inzucchi, Kim Pham, Michele Alguard, Katarzyna Lessard, Magalys Perez, Elizabeth Magenheimer, Abmaridel Montoza, David M. Nathan, David M. Nathan, John Lachin, John B. Buse, Steven E. Kahn, Heidi Krause-Steinrauf, Mary Larkin, Margaret Tiktin, Deborah Wexler, Henry B. Burch, Barbara Linder, Andrew Bremer, John Lachin, Heidi Krause-Steinrauf, Naji Younes, Michael Backman, Ionut Bebu, C.J. Buys, Anna Fagan Murphy, Yuping Gao, Michaela Gramzinski, Stephanie Hall, Elizabeth Legowski, Alyssa Arey, Joel Bethepu, Claire Lund, Pam Mangat Dhaliwal, Paula McGee, Emily Mesimer, Lisa Ngo, Michael Steffes, Jesse Seegmiller, Amy Saenger, Valerie Arends, Deanna Gabrielson, Todd Conner, Stuart Warren, Jolene Day, Alexandra Scrymgeour, Elsayed Z. Soliman, Zhu-Ming Zhang, Charles Campbell, Julie Hu, Lisa Keasler, Susan Hensley, Yabing Li, William Herman, Catherine Martin, Andrea Waltje, Shihchen Kuo, Rada Mihalcea, Veronica Perez-Rosas, Lisa Prosser, Kenneth Resnicow, Wen Ye, Hui Shao, Ping Zhang, Jose Luchsinger, Danurys Sanchez, Henry B. Burch, Andrew Bremer, Barbara Linder, Judith Fradkin, Erik Groessl, Helen Chong, Naomi Hillery, Ivan Abdouch, Paula Brantley, Frances E. Broyles, Gay Canaris, Paul Copeland, Jeri J. Craine, Warren L. Fein, Melissa S. Lee, Rebecca Meiners, Vaughn Meiners, Hollis O’Neal, James E. Park, Edward Sledge, Jr., Jeanne Steppel-Resnick, Alexander Turchin, Barbara Brooks-Worrell, Christiane S. Hampe, Christopher B. Newgard, Jerry P. Palmer, Ali Shojaie, John Higgins, Lawrence Fischer, Sherita Golden, Jeffery Gonzalez, Aanand Naik, Elizabeth Walker, Lynne Doner Lotenberg, Joanne M. Gallivan, Joanne Lim, Diane M. Tuncer, and Stephanie Behringer-Massera
References
- 1.Wajchenberg BL β-Cell failure in diabetes and preservation by clinical treatment. Endocr Rev 2007;28:187–218 [DOI] [PubMed] [Google Scholar]
- 2.Holman RR Assessing the potential for α-glucosidase inhibitors in prediabetic states. Diabetes Res Clin Pract 1998;40(Suppl.):S21–S25 [DOI] [PubMed] [Google Scholar]
- 3.Halban PA, Polonsky KS, Bowden DW, et al. β-Cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. Diabetes Care 2014;37:1751–1758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Russo GT, Giorda CB, Cercone S, Nicolucci A, Cucinotta D; BetaDecline Study Group . Factors associated with beta-cell dysfunction in type 2 diabetes: the BETADECLINE study. PLoS One 2014;9:e109702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gentile S, Strollo F, Viazzi F, et al.; The Amd-Annals Study Group . Five-year predictors of insulin initiation in people with type 2 diabetes under real-life conditions. J Diabetes Res 2018;2018:7153087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsia DS, Rasouli N, Pittas AG, et al.; D2d Research Group . Implications of the hemoglobin glycation index on the diagnosis of prediabetes and diabetes. J Clin Endocrinol Metab 2020;105:e130–e138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirk JK, D’Agostino RB Jr., Bell RA, et al. Disparities in HbA1c levels between African-American and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2006;29:2130–2136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Selvin E, Sacks DB. Variability in the relationship of hemoglobin A1c and average glucose concentrations: how much does race matter? Ann Intern Med 2017;167:131–132 [DOI] [PubMed] [Google Scholar]
- 9.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med 2007;167:1853–1860 [DOI] [PubMed] [Google Scholar]
- 10.Adams AS, Trinacty CM, Zhang F, et al. Medication adherence and racial differences in A1C control. Diabetes Care 2008;31:916–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nathan DM, Buse JB, Kahn SE, et al.; GRADE Study Research Group . Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care 2013;36:2254–2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419 [DOI] [PubMed] [Google Scholar]
- 13.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care 2004;27:1487–1495 [DOI] [PubMed] [Google Scholar]
- 14.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999;22:1462–1470 [DOI] [PubMed] [Google Scholar]
- 15.Seltzer HS, Allen EW, Herron AL Jr., Brennan MT. Insulin secretion in response to glycemic stimulus: relation of delayed initial release to carbohydrate intolerance in mild diabetes mellitus. J Clin Invest 1967;46:323–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Utzschneider KM, Prigeon RL, Faulenbach MV, et al. Oral disposition index predicts the development of future diabetes above and beyond fasting and 2-h glucose levels. Diabetes Care 2009;32:335–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Polonsky KS, Rubenstein AH. C-peptide as a measure of the secretion and hepatic extraction of insulin. Pitfalls and limitations. Diabetes 1984;33:486–494 [DOI] [PubMed] [Google Scholar]
- 18.International Diabetes Federation IDF Consensus Worldwide Definition of the Metabolic Syndrome. Accessed 8 December 2020. Available from https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html
- 19.Dixon WJ, Tukey JW. Approximate behavior of the distribution of winsorized t (trimming/winsorization 2). Technometrics 1968;10:83–98 [Google Scholar]
- 20.Viberti G, Lachin J, Holman R, et al.; ADOPT Study Group . A Diabetes Outcome Progression Trial (ADOPT): baseline characteristics of type 2 diabetic patients in North America and Europe. Diabet Med 2006;23:1289–1294 [DOI] [PubMed] [Google Scholar]
- 21.Herman WH, Ma Y, Uwaifo G, et al.; Diabetes Prevention Program Research Group . Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care 2007;30:2453–2457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergenstal RM, Gal RL, Connor CG, et al.; T1D Exchange Racial Differences Study Group . Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med 2017;167:95–102 [DOI] [PubMed] [Google Scholar]
- 23.Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ; A1c-Derived Average Glucose Study Group . Translating the A1C assay into estimated average glucose values. Diabetes Care 2008;31:1473–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen RM, Franco RS, Khera PK, et al. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood 2008;112:4284–4291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soranzo N, Sanna S, Wheeler E, et al.; WTCCC . Common variants at 10 genomic loci influence hemoglobin A1(C) levels via glycemic and nonglycemic pathways [published correction appears in Diabetes 2011;60:1050–1051]. Diabetes 2010;59:3229–3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Larkin ME, Nathan DM, Bebu I, et al.; GRADE Research Group . Rationale and design for a GRADE substudy of continuous glucose monitoring. Diabetes Technol Ther 2019;21:682–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kodama K, Tojjar D, Yamada S, Toda K, Patel CJ, Butte AJ. Ethnic differences in the relationship between insulin sensitivity and insulin response: a systematic review and meta-analysis. Diabetes Care 2013;36:1789–1796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jensen CC, Cnop M, Hull RL, Fujimoto WY, Kahn SE; American Diabetes Association GENNID Study Group . β-Cell function is a major contributor to oral glucose tolerance in high-risk relatives of four ethnic groups in the U.S. Diabetes 2002;51:2170–2178 [DOI] [PubMed] [Google Scholar]
- 29.Rasouli N, Spencer HJ, Rashidi AA, Elbein SC. Impact of family history of diabetes and ethnicity on β-cell function in obese, glucose-tolerant individuals. J Clin Endocrinol Metab 2007;92:4656–4663 [DOI] [PubMed] [Google Scholar]
- 30.Michaliszyn SF, Lee S, Bacha F, et al. Differences in β-cell function and insulin secretion in Black vs. White obese adolescents: do incretin hormones play a role? Pediatr Diabetes 2017;18:143–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piccinini F, Polidori DC, Gower BA, Bergman RN. Hepatic but not extrahepatic insulin clearance is lower in African American than in European American women. Diabetes 2017;66:2564–2570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fosam A, Sikder S, Abel BS, et al. Reduced insulin clearance and insulin-degrading enzyme activity contribute to hyperinsulinemia in African Americans. J Clin Endocrinol Metab 2020;105:e1835–e1846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kühl C, Faber OK, Hornnes P, Jensen SL. C-peptide metabolism and the liver. Diabetes 1978;27(Suppl. 1):197–200 [DOI] [PubMed] [Google Scholar]
- 34.Polonsky K, Jaspan J, Pugh W, et al. Metabolism of C-peptide in the dog. In vivo demonstration of the absence of hepatic extraction. J Clin Invest 1983;72:1114–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rahman M, Temple JR, Breitkopf CR, Berenson AB. Racial differences in body fat distribution among reproductive-aged women. Metabolism 2009;58:1329–1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen G, Bentley A, Adeyemo A, et al. Genome-wide association study identifies novel loci association with fasting insulin and insulin resistance in African Americans. Hum Mol Genet 2012;21:4530–4536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palmer ND, Hester JM, An SS, et al. Resequencing and analysis of variation in the TCF7L2 gene in African Americans suggests that SNP rs7903146 is the causal diabetes susceptibility variant. Diabetes 2011;60:662–668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kahn SE, Lachin JM, Zinman B, et al.; ADOPT Study Group . Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes 2011;60:1552–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benoit SR, Hora I, Albright AL, Gregg EW. New directions in incidence and prevalence of diagnosed diabetes in the USA. BMJ Open Diabetes Res Care 2019;7:e000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Tata V Age-related impairment of pancreatic Beta-cell function: pathophysiological and cellular mechanisms. Front Endocrinol (Lausanne) 2014;5:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferrannini E, Camastra S, Gastaldelli A, et al. β-cell function in obesity: effects of weight loss. Diabetes 2004;53(Suppl. 3):S26–S33 [DOI] [PubMed] [Google Scholar]
- 42.McLaughlin T, Deng A, Gonzales O, et al. Insulin resistance is associated with a modest increase in inflammation in subcutaneous adipose tissue of moderately obese women. Diabetologia 2008;51:2303–2308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Young KA, Maturu A, Lorenzo C, et al. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance, β-cell function, and diabetes in Hispanics and African Americans. J Diabetes Complications 2019;33:118–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maturu A, DeWitt P, Kern PA, Rasouli N. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of β-cell function in African American women. Metabolism 2015;64:561–565 [DOI] [PubMed] [Google Scholar]
- 45.Yang Y-M, Shin B-C, Son C, Ha I-H. An analysis of the associations between gender and metabolic syndrome components in Korean adults: a national cross-sectional study. BMC Endocr Disord 2019;19:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kwon SK Women are diagnosed with type 2 diabetes at higher body mass indices and older ages than men: Korea National Health and Nutrition Examination Survey 2007-2010. Diabetes Metab J 2014;38:74–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Racette SB, Horowitz JF, Mittendorfer B, Klein S. Racial differences in lipid metabolism in women with abdominal obesity. Am J Physiol Regul Integr Comp Physiol 2000;279:R944–R950 [DOI] [PubMed] [Google Scholar]
- 48.Wexler DJ, Krause-Steinrauf H, Crandall JP, et al.; GRADE Research Group . Baseline characteristics of randomized participants in the Glycemia Reduction Approaches in Diabetes: A Comparative Effectiveness Study (GRADE). Diabetes Care 2019;42:2098–2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Uwaifo GI, Fallon EM, Chin J, Elberg J, Parikh SJ, Yanovski JA. Indices of insulin action, disposal, and secretion derived from fasting samples and clamps in normal glucose-tolerant black and white children. Diabetes Care 2002;25:2081–2087 [DOI] [PubMed] [Google Scholar]