Abstract
The American Diabetes Association 2020 Standards of Medical Care in Diabetes (Standards of Care) recommends a hemoglobin A1c (A1C) of <7% (53 mmol/mol) for many children with type 1 diabetes (T1D), with an emphasis on target personalization. A higher A1C target of <7.5% may be more suitable for youth who cannot articulate symptoms of hypoglycemia or have hypoglycemia unawareness and for those who do not have access to analog insulins or advanced diabetes technologies or who cannot monitor blood glucose regularly. Even less stringent A1C targets (e.g., <8%) may be warranted for children with a history of severe hypoglycemia, severe morbidities, or short life expectancy. During the “honeymoon” period and in situations where lower mean glycemia is achievable without excessive hypoglycemia or reduced quality of life, an A1C <6.5% may be safe and effective. Here, we provide a historical perspective of A1C targets in pediatrics and highlight evidence demonstrating detrimental effects of hyperglycemia in children and adolescents, including increased likelihood of brain structure and neurocognitive abnormalities, microvascular and macrovascular complications, long-term effects, and increased mortality. We also review data supporting a decrease over time in overall severe hypoglycemia risk for youth with T1D, partly associated with the use of newer insulins and devices, and weakened association between lower A1C and severe hypoglycemia risk. We present common barriers to achieving glycemic targets in pediatric diabetes and discuss some strategies to address them. We aim to raise awareness within the community on Standards of Care updates that impact this crucial goal in pediatric diabetes management.
Introduction
Twenty-seven years ago, the Diabetes Control and Complications Trial (DCCT) first demonstrated in a randomized clinical trial that intensive insulin treatment aiming to lower glucose levels closer to the normal range, beyond that necessary to control symptoms of hyperglycemia, reduced the risk of microvascular (1) and long-term (2) diabetes complications. Increased severe hypoglycemia risk was an adverse effect of intensive therapy. In addition, there was fear that intensive treatment could increase the risk of macrovascular complications due to hyperinsulinemia, and significant real-world impediments to feasibility of and accessibility to the diabetes care required to achieve the study results were noted in the initial report almost three decades ago (3).
Since its 1993 landmark publication, the DCCT and many other studies have progressively provided overwhelming evidence that near-normal glucose control diminishes the risks of retinopathy, nephropathy, neuropathy, and macrovascular complications (4). The development of insulin analogs, more sophisticated insulin delivery systems (e.g., insulin pumps), continuous glucose monitoring (CGM), and, more recently, integrated systems (e.g., sensor-augmented insulin pumps, predictive low-glucose suspend systems, and closed-loop control systems) greatly enhanced the feasibility of maintaining glucose levels within a prespecified target range. These advances have also contributed to lessening hypoglycemia risk and have diminished the relationship of significant or severe hypoglycemia with lower glycemic targets in people with T1D. Consideration of emerging evidence relevant to pediatrics has prompted the American Diabetes Association (ADA) to revise its hemoglobin A1c (A1C) targets in pediatric T1D several times through the years.
The ADA’s Professional Practice Committee updates the Standards of Medical Care in Diabetes (Standards of Care) (5) annually “to ensure that clinicians, health plans, and policy makers can continue to rely on it as the most authoritative source for current guidelines for diabetes care” (6). With the 2020 Standards of Care (5), the ADA issued a new recommendation for children with T1D: “A1C goals must be individualized and reassessed over time. An A1C of <7% (53 mmol/mol) is appropriate for many children” (recommendation 13.21, evidence grade B) (7). The previous version, published in January 2019, had recommended a goal of 7.5% for most children (8).
In this Perspective, we review the history of pediatric A1C targets and the evidence supporting the 2020 revision. Barriers to achieving pediatric A1C targets are discussed, as are proposed strategies to address them. With this article, we aim to raise awareness within the diabetes community of the updated 2020 A1C recommendations to the Standards of Care.
Historical Perspective of A1C Goals in Pediatric T1D
The 2003 Standards of Care established that, while the general A1C goal for individuals with diabetes was <7%, a “less stringent treatment goal may be appropriate for … very young children.” In 2005, the ADA issued a statement with age-specific A1C goals for pediatric T1D. A range of 7.5% to 8.5% was recommended for children <6 years of age, <8% for children 6–12 years old (≤8 stated in the narrative), and <7.5% for adolescents 13–19 years old. The 2011 Standards of Care introduced the concept that lower A1C targets for children with T1D were reasonable if achievable without significant hypoglycemia (see Table 1 for goals). In 2015, the Standards of Care recommended a goal of <7.5% across all pediatric age-groups, <7% if achievable without excessive hypoglycemia, with premeal and bedtime/overnight plasma blood glucose ranges also recommended. The 2020 Standards of Care recommends an A1C goal of <7% for many children with T1D (recommendation 13.21, evidence grade B). A higher target of <7.5% may be more appropriate for youth who cannot articulate symptoms of hypoglycemia or have hypoglycemia unawareness, as well as those who do not have access to analog insulins, cannot monitor their blood glucose regularly, or do not have access to advanced diabetes technologies, including insulin pumps and CGM (recommendation 13.22, evidence grade B). Individuals who have nonglycemic factors that increase A1C, such as higher erythrocyte life span, or are high glycators (i.e., those who, for the same level of glucose, have consistently higher A1C) may also need a higher target such as <7.5% (recommendation 13.22, evidence grade B). Similar to that for adults with diabetes, a target of <8% is recommended for youth with a history of severe hypoglycemia, severe morbidities, or short life expectancy (recommendation 13.23, evidence grade B). A lower A1C target, such as <6.5%, may be appropriate during the partial remission period (or “honeymoon”) or in persons with longer-standing T1D if achievable without excessive hypoglycemia, poor quality of life, or undue burden of care (recommendation 13.24, evidence grade B).
Table 1.
History of ADA guidance for A1C targets for youth with diabetes since 2000. Years when glycemic target changed are illustrated. Specific changes from the previous goal are indicated in boldface type. A more detailed version of this table is provided as Supplementary Table 1.
| Date and publication | Type 1 diabetes | Type 2 diabetes |
|---|---|---|
| 2000: Type 2 Diabetes in Children and Adolescents (Consensus Statement) (70) | All children: <7% | |
| 2003: Standards of Medical Care for Patients With Diabetes Mellitus (71) | Very young children: less stringent treatment goals than the <7% recommended for other individuals | |
| 2005: Care of Children and Adolescents With Type 1 Diabetes: A Statement of the American Diabetes Association (72) | Children <6 years: between 7.5% and 8.5% | |
| Children 6–12 years: <8% (≤8 in the narrative) | ||
| Adolescents (13–19 years): <7.5% | ||
| 2005: Standards of Medical Care in Diabetes (73) | Plasma blood glucose and A1C goals: | |
| Toddlers and preschoolers (<6 years) | ||
| Before meals: 100–180 mg/dL | ||
| Bedtime/overnight: 110–200 mg/dL A1C: ≤8.5 (but ≥7.5%) | ||
| School age (6–12 years) | ||
| Before meals: 90–180 mg/dL | ||
| Bedtime/overnight: 100–180 mg/dL | ||
| A1C: <8% | ||
| Adolescents and young adults (13–19 years) | ||
| Before meals: 90–130 mg/dL | ||
| Bedtime/overnight: 90–150 mg/dL | ||
| A1C: <7.5% (a lower goal [<7%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2006: Standards of Medical Care in Diabetes (74) | Plasma blood glucose and A1C goals: | |
| Toddlers and preschoolers (0–6 years) | ||
| Before meals: 100–180 mg/dL | ||
| Bedtime/overnight: 110–200 mg/dL | ||
| A1C: <8.5% (but >7.5%) | ||
| School age (6–12 years) | ||
| Before meals: 90–180 mg/dL | ||
| Bedtime/overnight: 100–180 mg/dL | ||
| A1C: <8% | ||
| Adolescents & young adults (13–19 years) | ||
| Before meals: 90–130 mg/dL | ||
| Bedtime/overnight: 90–150 mg/dL | ||
| A1C: <8% (a lower goal [<7.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2007: Standards of Medical Care in Diabetes (75) | Plasma blood glucose and A1C goals: | |
| Toddlers and preschoolers (0–6 years) | ||
| Before meals: 100–180 mg/dL | ||
| Bedtime/overnight: 110–200 mg/dL | ||
| A1C: <8.5% (but >7.5%) | ||
| School age (6–12 years) | ||
| Before meals: 90–180 mg/dL | ||
| Bedtime/overnight: 100–180 mg/dL | ||
| A1C: <8% | ||
| Adolescents & young adults (13–19 years) | ||
| Before meals: 90–130 mg/dL | ||
| Bedtime/overnight: 90–150 mg/dL | ||
| A1C: <7.5% (a lower goal [<7.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2011: Standards of Medical Care in Diabetes (76) | Plasma blood glucose and A1C goals: | |
| Toddlers and preschoolers (0–6 years) | ||
| Before meals: 100–180 mg/dL | ||
| Bedtime/overnight: 110–200 mg/dL | ||
| A1C: <8.5% (a lower goal [<8.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| School age (6–12 years) | ||
| Before meals: 90–180 mg/dL | ||
| Bedtime/overnight: 100–180 mg/dL | ||
| A1C: <8% (a lower goal [<7.5%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| Adolescents and young adults (13–19 years) | ||
| Before meals: 90–130 mg/dL | ||
| Bedtime/overnight: 90–150 mg/dL | ||
| A1C: <7.5% (a lower goal [<7.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2015: Standards of Medical Care in Diabetes (77) | An A1C goal of <7.5% is recommended across all pediatric age-groups. | |
| Plasma blood glucose and A1C goals across all pediatric age-groups: | ||
| Before meals: 90–130 mg/dL (5.0–7.2 mmol/L | ||
| Bedtime/overnight: 90–150 mg/dL (5.0–8.3 mmol/L) | ||
| A1C: <7.5% (a lower goal [<7.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2016: Standards of Medical Care in Diabetes (78) | An A1C goal of <7.5% (58 mmol/mol) is recommended across all pediatric age-groups. | |
| Blood glucose across all pediatric age-groups: | ||
| Before meals: 90–130 mg/dL (5.0–7.2 mmol/L) | ||
| Bedtime/overnight: 90–150 mg/dL (5.0–8.3 mmol/L) | ||
| A1C: <7.5% (58 mmol/mol) (a lower goal [<7.0%] is reasonable if it can be achieved without excessive hypoglycemia) | ||
| 2018: Evaluation and Management of Youth-Onset Type 2 Diabetes: A Position Statement by the American Diabetes Association (79) | <7% (most youth). More stringent A1C goals (such as <6.5%) may be appropriate for selected individual patients if they can be achieved without significant hypoglycemia or other adverse effects of treatment. Appropriate patients might include those with short duration of diabetes and lesser degrees of β-cell dysfunction and patients treated with lifestyle or metformin only who achieve significant weight improvement. E | |
| 2019: Standards of Medical Care in Diabetes (8) | Incorporated the recommendations in the 2018 Position Statement | |
| 2020: Standards of Medical Care in Diabetes (7) | Recommendation 13.21: A1C goals must be individualized and reassessed over time. An A1C of <7% (53 mmol/mol) is appropriate for many children. B | <7% (53 mmol/mol) (most youth); <6.5% (48 mmol/mol] (selected youth as specified in 2019 Standards of Care). Less stringent A1C goals (such as 7.5% [58 mmol/mol]) may be appropriate if there is increased risk of hypoglycemia. |
| Recommendation 13.22: Less stringent A1C goals (such as <7.5% [58 mmol/mol]) may be appropriate for patients who cannot articulate symptoms of hypoglycemia; have hypoglycemia unawareness; lack access to analog insulins, advanced insulin delivery technology, and/or continuous glucose monitors; cannot check blood glucose regularly; or have nonglycemic factors that increase A1C (e.g., high glycators). B | ||
| Recommendation 13.23: Even less stringent A1C goals (such as <8% [64 mmol/mol]) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, or extensive comorbid conditions. B | ||
| Recommendation 13.24: Providers may reasonably suggest more stringent A1C goals (such as <6.5% [48 mmol/mol]) for selected individual patients if they can be achieved without significant hypoglycemia, negative impacts on well-being, or undue burden of care, or in those who have nonglycemic factors that decrease A1C (e.g., lower erythrocyte life span). Lower targets may also be appropriate during the honeymoon phase. B |
The 2020 revision aligns the A1C goals in pediatric T1D and type 2 diabetes (T2D). Table 1 illustrates a summary of the history of ADA’s guidelines for A1C targets in youth with T1D or T2D since 2000. Supplementary Table 1 provides significant narrative information on goals and additional details such as specific changes from year to year, whether guidance was labeled as a recommendation, and level of evidence as graded by the ADA.
The emphasis on glycemic target individualization has been a constant through the years in the ADA clinical guidelines. Age-specific goals were recommended between 2005 and 2015. The 2020 Standards of Care recommends considering a less stringent A1C goal if, based on the individual’s circumstances, the risks (such as increased risk of hypoglycemia, increased burden of care, or decreased feasibility) exceed potential benefits or when A1C is not a reliable indicator of mean glucose concentrations (recommendation 13.22, evidence grade B, and recommendation 13.23, evidence grade B). On the other hand, in selected children, a lower target (e.g., <6.5%) is reasonable (recommendation 13.24, evidence grade B).
Besides A1C goals, the premeal/bedtime/overnight glucose targets have also been adjusted empirically through the years to reflect A1C goal changes. Yet specific evidence on ways to achieve A1C goals is currently sparse, reflecting a need for more data.
Evidence Suggesting Detrimental Effects of Hyperglycemia in Children and Adolescents
Structural and Neurocognitive Effects on the Central Nervous System
The negative effects of hypoglycemia on the brain have long been established, with those of chronic hyperglycemia appreciated more recently. Reported relationships between dysglycemia-associated neurocognitive and brain structure changes have varied by study design and differing clinical populations. Barnea-Goraly et al. (9) studied 127 children aged 4 to <10 years with T1D and 67 age-matched control subjects and found abnormalities in axial diffusivity (a measure that reflects fiber coherence), reduced radial diffusivity (a measure of fiber integrity and myelination), and fractional anisotropy (reflecting the degree of diffusion anisotropy, which is determined by fiber diameter and density, myelination, extracellular diffusion, interaxonal spacing, and fiber tract coherence). These changes correlated with earlier onset of diabetes, longer diabetes duration, and higher A1C. A Diabetes Research in Children Network (DirecNet) longitudinal study (10) in 142 children with T1D and 65 age-matched control subjects (4–10 years of age at study entry) observed slower hippocampal growth in the span of 18 months associated with higher A1C and greater glycemic variability, as assessed by CGM. A separate analysis from this DirecNet study pediatric population (11) incorporated high-resolution structural MRI combined with neurocognitive testing, finding that both hyperglycemia and glucose variability (but not hypoglycemia), were associated with slower growth in specific regions of gray (left precuneus, right temporal, frontal, and parietal lobes and right medial-frontal cortex) and white (splenium of the corpus callosum, bilateral superior-parietal lobe, bilateral anterior forceps, and inferior-frontal fasciculus) matter areas over the 18 months of the study. However, no differences in cognitive and executive function scores between groups were observed. Perantie et al. (12) analyzed a cohort of 108 children 7–17 years old with T1D and 51 healthy sibling control subjects; hyperglycemia was associated with smaller gray matter volume in the right cuneus and precuneus, smaller white matter volume in a right posterior parietal region, and larger gray matter volume in a right prefrontal region, while a history of severe hypoglycemia was associated with smaller gray matter volume in the left superior temporal region. A further study (13) in a subset of the DirecNet cohort of children aged 3 to <10 years with T1D (n = 22) and age- and sex-matched healthy control subjects (n = 14) demonstrated that higher time-weighted A1C values were significantly correlated with lower overall intellectual functioning measured by the full-scale intelligence quotient and, within the diabetes group, there was a significant, positive correlation between time-weighted A1C and radial diffusivity. In a recent study, children with T1D performed worse on visuospatial working memory tasks and showed greater increase in activation with higher working memory load (i.e., compensatory modulation of activation) as measured by functional MRI (14).
A meta-analysis on executive function in T1D, including 17 studies and 1,619 pooled participants, determined that inhibition, working memory, set shifting, and overall executive function were lower in adolescents and young adults with T1D than in control subjects (15). A systematic review of 500 youth concluded that repeated episodes of acute hyperglycemia, e.g., diabetic ketoacidosis (DKA), is detrimental to the brain in children and adolescents (16).
Overall, evidence indicates that both hyperglycemia (chronic and acute) and hypoglycemia are associated with structural brain changes, brain function adaptation, and neurocognitive dysfunction in children. More studies are needed on the underlying pathophysiology that can be leveraged for preventive and treatment purposes as well as on optimal glycemic range/glucose variability targets for brain development and growth.
Microvascular and Macrovascular Complications
The DCCT demonstrated that intensive diabetes treatment diminished the risk and rate of development of diabetic complications in individuals with T1D aged 13 to 39 years (1,2). In a subanalysis of the adolescents between the ages of 13 and 17 years at DCCT study entry (n = 125), who were followed for a mean of 7.4 years (range 4–9 years), those in the intensive treatment group attained a mean A1C of 8.06% (SE 0.13) and had significantly lower risk of microalbuminuria as well as retinopathy appearance or progression compared with participants in the conventional treatment group with a mean A1C of 9.76% (SE 0.12). These results were consistent with the risk reduction observed in adults.
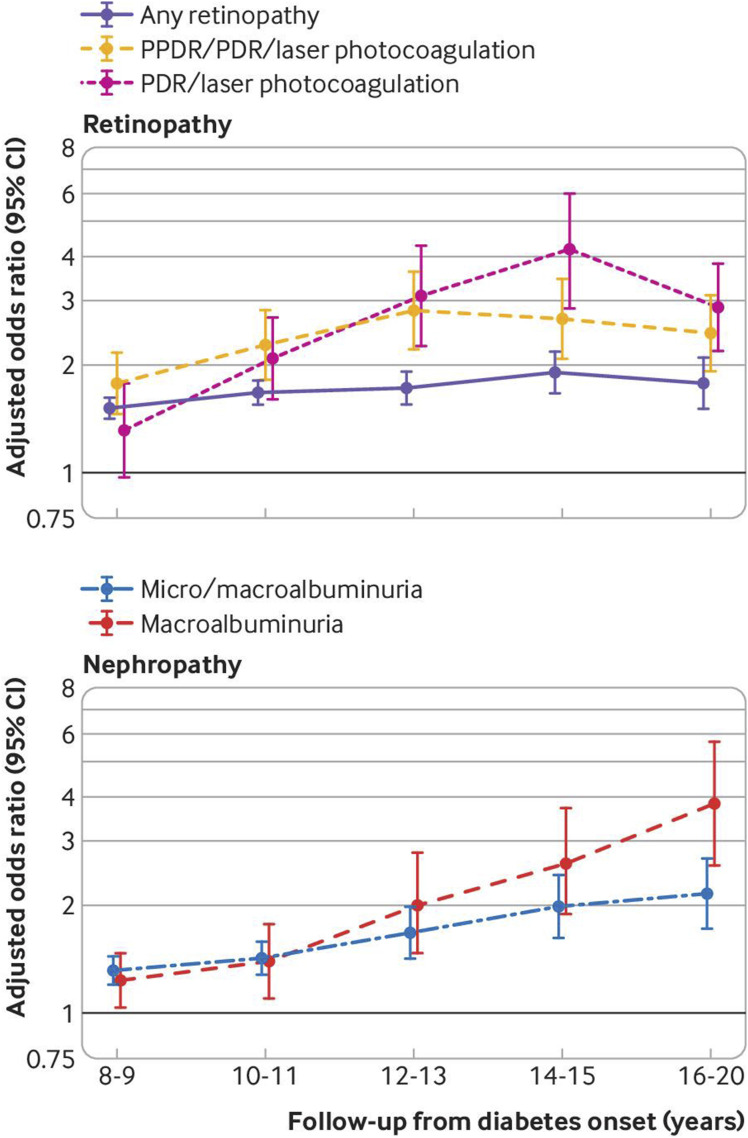
In a longitudinal Australian cohort of adolescents with T1D, a mean decrease in A1C from 9.1% to 8.5% was associated with lower rate of retinopathy (17). The Vascular Diabetic Complications in Southeast Sweden (VISS) study observed 451 individuals diagnosed with T1D before age 35 years and found that no one with long-term weighted mean A1C <7.6% (60 mmol/mol) developed proliferative retinopathy or persistent macroalbuminuria, compared with 51% of individuals with long-term weighted mean A1C >9.5% (60 mmol/mol) (18). A population-based Swedish National Diabetes Registry cohort study of 10,398 children and adults with T1D between 1998 and 2017 observed that, while A1C under 6.5% increased the risk of hypoglycemia, the risk of any retinopathy and nephropathy progressively increased with A1C above 6.5% (19) (Fig. 1).
Figure 1.
Adjusted odds ratios (95% CI) for retinopathy and nephropathy for 10 mmol/mol increase in A1C area under the curve in the Swedish National Diabetes Registry (19), which collected data between 1 January 1998 and 31 December 2017. Whiskers represent 95% CI. PDR, proliferative diabetic retinopathy; PPDR, preproliferative diabetic retinopathy.
Data from the Pittsburgh Epidemiology of Diabetes Complications (EDC) study, including 658 subjects with childhood-onset (<17 years old) T1D diagnosed between 1950 and 1980, evaluated at baseline between 1986 and 1988 and then followed biennially, showed that A1C was an independent risk factor for fatal coronary artery disease (20). Moreover, the longitudinal A1C trajectory was associated with 25-year cardiovascular disease incidence in this cohort; associations were similar across the specific manifestations of cardiovascular disease (21).
Long-term Effects on the Risk of Complications (“Metabolic Memory”)
The Epidemiology of Diabetes Interventions and Complications (EDIC) study was launched to follow adult and pediatric participants after conclusion of the DCCT and evaluate the long-term effects of the DCCT interventions. Over 90% of DCCT participants participated in the EDIC study. After 30 years of diabetes, the cumulative incidences of proliferative retinopathy, nephropathy, and cardiovascular disease were much lower (21%, 9%, and 9%) in the DCCT intensive therapy group compared with 50%, 25%, and 14% in the DCCT in the conventional group (22) despite similar A1C after the DCCT concluded. An analysis restricted to pediatric participants (n = 175) observed that, although the mean A1C trajectories of the intensive and conventional groups converged, the risk of retinopathy progression decreased by 74–78% over the next 4 years in the intensive treatment group compared with the conventional group (23). Longitudinal observation of this cohort of adolescents aged 13–18 years at randomization demonstrated that, although none developed diabetic retinopathy requiring treatment while <18 years of age, there were three cases of proliferative diabetic retinopathy in participants <21 years of age, all females in the conventional therapy arm (24). More long-term DCCT/EDIC outcome studies are needed, especially for the pediatric cohort.
Early good glycemic control may also beget long-term improved control. Glucose control tracking has been demonstrated in a longitudinal study (25) of 1,146 children and adolescents in Austria and Germany where prepubertal A1C predicted metabolic control in young adulthood after adjustment for confounders. Similarly, the Swedish pediatric diabetes quality registry and the Swedish National Diabetes Register analyzed data from 1,543 youth and found that higher A1C close to diagnosis was associated with higher A1C in adult life as well as risk of microalbuminuria and retinopathy (26). Although more research is needed in this area, it is clear that achieving the best glucose control possible as early as feasible after diagnosis is an important pediatric goal.
Mortality
Mortality is increased for persons diagnosed with T1D during childhood and is associated with glycemic control. The Swedish National Diabetes Register studied 27,195 individuals with T1D registered between 1998 and 2012 and 135,178 matched general population control subjects. This study found the highest excess risks compared with the control subjects of both all-cause mortality and cardiovascular disease in individuals who were diagnosed with T1D at <10 years of age, adjusting for diabetes duration, with risk over fourfold for all-cause mortality, over sevenfold for cardiovascular mortality, and over elevenfold for cardiovascular disease. In comparison, the corresponding hazard ratios in individuals diagnosed with T1D between 26 and 30 years of age were 2.83, 3.64, and 3.85 (27). Therefore, earlier age at T1D diagnosis is associated with higher risk of mortality and cardiovascular disease, suggesting the importance of early risk factor control. These findings are in direct contradiction to the historical wisdom that the clock determining risk of complications does not start until puberty. An analysis of 12,652 individuals in the Swedish pediatric diabetes quality registry from 2006 to 2014 showed that higher mortality in young people (<30 years of age) was associated with higher A1C during childhood (28).
Evidence of Decrease in Hypoglycemia Risk—An Evolution Since DCCT
Historically, the increased risk of hypoglycemia associated with lower A1C led to establishing guidelines with higher glycemic targets for youth. At the individual level, fear of hypoglycemia leads persons with T1D, caregivers of children with T1D, and diabetes care providers to adopt strategies to maintain hyperglycemia to mitigate this risk (29). While increased risk of hypoglycemia was a major adverse effect in the intensive treatment group in the DCCT study, this study started recruitment in 1983 and concluded follow-up of participants in 1993. The incidence of hypoglycemia has been declining over the almost three decades since then.
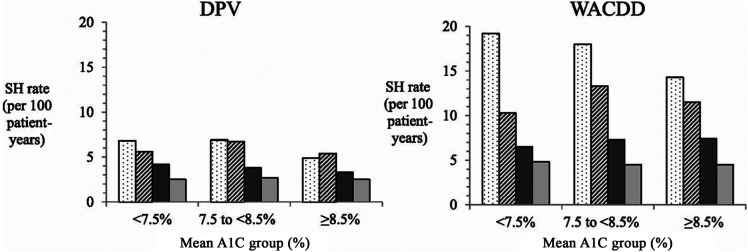
The Danish Adult Diabetes Database (DADD) documented an annual decrease of 8.4% in the incidence rate of severe hypoglycemia (30). An analysis of temporal trends in children diagnosed with T1D <15 years of age from 1995 to 2016 from the longitudinal, prospective, population-based German/Austrian Diabetes Patient History Documentation (Diabetes Patienten Verlaufsdokumenation, DPV) (N = 59,883) and Western Australian Children's Diabetes Database (WACDD) (N = 2,595) diabetes registries demonstrated concurrent improvements in A1C and decreasing severe hypoglycemia rates (31) between 1995 and 2016. The relationship of A1C and severe hypoglycemia has also changed in the 27 years that have elapsed since the DCCT report. In children and adolescent participants in the U.S. T1D Exchange (N = 7,102), German/Austrian DPV (N = 18,887), or WACDD (N = 865) diabetes registries between 2011 and 2012, rates of severe hypoglycemia per 100 patient-years were not associated with lower A1C overall or with source registry, treatment regimen, or age-group (32). These results are consistent with a previous analysis of 37,539 participants aged 1 to 20 years old with T1D in the DPV study in Germany and Austria that observed a weakening of the association between lower A1C and severe hypoglycemia (33). A more recently analysis of the DPV and WACDD cohorts confirmed the decreases in A1C and severe hypoglycemia rate and found similarly low severe hypoglycemia rates in all A1C categories (Fig. 2) (31). Similarly, in a study (34) of 1,770 children (<16 years of age) followed between 2000 and 2011, those with A1C <7% did not have higher rates of hypoglycemia compared with children with A1C 8–9%. A study of 8,806 children <15 years of age (n = 8,806) in Nordic countries Denmark, Iceland, Norway, and Sweden between 2008 and 2012 showed that the risk of severe hypoglycemia was not different between the children with A1C ≤6.7% and those with higher A1C after adjusting for confounders (35). In the DADD cohort, the risk of severe hypoglycemia associated with a lower A1C decreased between the time periods of 1995–2003 and 2004–2012 (36). A further analysis of data from 17,230 older teenagers (>16 years old) and adults with T1D in the DADD between 2006 and 2012 found that the association between hypoglycemia and A1C was nonlinear, with a much more marked increase for hypoglycemia risk with A1C above 7.6% (60 mmol/mol) than below that level (30).
Figure 2.
A1C and rates of severe hypoglycemia, adjusted for sex, age at diagnosis, and diabetes duration, observed in the longitudinal, prospective DPV (German-Austrian) and WACDD (Austrialian) cohorts since 1991 (31). The rates of severe hypoglycemia (SH) decreased since 1991 and were similar across A1C groups (i.e., <7.5%, 7.5 to <8.5%, and ≥8.5%), particularly in the last time period (2012–2016). Severe hypoglycemia was defined as a hypoglycemic episode resulting in loss of consciousness and/or seizure. White bar with dots represent 1991–2001; striped bar, 2002–2006; dark gray bar, 2007–2011; and light gray bar, 2012–2016.
Newer Treatment Modalities and Hypoglycemic Risk
A plausible explanation for the observed decline in hypoglycemia rates is the increased use of insulin analogs and diabetes technology. The rapid succession of newer and better insulins that started with the approval of the first rapid-acting insulin analog, lispro, in 1996 has been followed by dramatic falls in the rates of hypoglycemia at night and after meals (37).
Advances in technology to administer insulin and monitor glucose have been shown to improve glucose control in T1D. In the study by Cooper et al. (34) with 1,770 children (<16 years of age) followed between 2000 and 2011, children utilizing insulin pumps had lower risk of severe hypoglycemia than children using insulin injections. The study of 8,806 children <15 years of age in the four Nordic countries between 2008 and 2012 showed that pump use was associated with lower risk of severe hypoglycemia (35). In a case-controlled, nonrandomized study, Johnson et al. (38) observed that use of insulin pumps reduced A1C by 0.6% and lowered the risk of severe hypoglycemia by 50%. In the DPV population-based cohort study with over 30,000 pediatric participants with T1D between 2011 and 2015 in Germany, Austria, and Luxembourg, pump therapy was associated with lower A1C and lower rates of severe hypoglycemia and DKA (39).
The recent CGM Intervention in Teens and Young Adults with T1D (CITY) study randomized 153 adolescents and young adults (ages 14–24 years old) with T1D to CGM or blood glucose monitoring (usual care) and demonstrated a significant improvement in glucose control (A1C, time in range) and mean time in hypoglycemia and higher glucose monitoring satisfaction over the 26 weeks of the study (40). This is in contrast with a 2008 study where an early-generation CGM system improved A1C in adult patients (>25 years of age) but not in younger participants, who also had lower device wear times (41). This difference reflects that later-generation devices are better tolerated and have improved in ease of placement and accuracy, leading to greater wear time.
Sensor-augmented insulin pump therapy with the threshold-suspend feature (i.e., predictive low-glucose suspend system) reduced nocturnal hypoglycemia in a randomized trial with 247 participants (42). In a pediatric randomized clinical trial, Ly et al. (43) demonstrated that the predictive low-glucose suspend system significantly reduced time in hypoglycemia although, as expected since the system does not address hyperglycemia, A1C did not decrease.
Closed-loop control systems have been developed to address both hypo- and hyperglycemia. A randomized clinical trial with a total of 168 participants between 14 and 71 years old found 11% significantly higher mean adjusted time in range in participants on the closed-loop system than in those on sensor-augmented pump therapy (control group) (44). A recent study demonstrated that switching to a predictive low-glucose suspend system reduced time in range and increased A1C compared with participants who stayed on a closed-loop system, while time in hypoglycemia did not change (45).
A systematic review and meta-analysis conducted with data up to January 2017 that included 27 comparisons from 24 studies and a total of 585 participants (219 in adult studies, 265 in pediatric studies, and 101 in combined studies) concluded that time in target was 12.59% higher with artificial pancreas systems (95% CI 9.02–16.16; P < 0.0001) (46). Similar conclusions were reached by others (47).
Overall, these results support the concept that in the future hypoglycemia rates will continue to decline and time in range will continue to increase. Diabetes technology has consistently demonstrated that it has the potential to improve glucose control in pediatric and adult individuals with T1D. This evidence supports the ADA Standards of Care statement that CGM should be considered for all children and adolescents with T1D (recommendation 7.12, evidence grade B) (5). Studies are needed to translate the interventions proven efficacious in research trials into real-world settings.
A1C and Continuous Glucose Monitoring as Measures of Glycemic Control
Utilization of A1C as an indicator of glycemic control must acknowledge potential nonglycemic confounders. These include factors that lower the measured A1C, e.g., lower erythrocyte life span, and those that increase it, e.g., untreated iron deficiency anemia (48). High or low “glycator” individuals will have, respectively, higher or lower A1C levels than expected based on their glucose levels. In addition, there are significant racial differences in the relationship between glucose levels and A1C, with Black individuals having A1C that is on average 0.4 percentage points (95% CI 0.2–0.6) higher than that in White individuals for a given mean glucose concentration. Of note, this phenomenon was not observed with glycated albumin or fructosamine (49). To overcome the potential risk of error when estimating average glucose from measured A1C, when feasible clinicians can use recent CGM data to document time above and below target range prior to lowering an individual’s A1C target. In addition, CGM allows estimation of time in range and, in particular within close-loop systems, minimization of hypoglycemia and hyperglycemic excursions (50). A1C and CGM-derived measures provide complementary assessments of glucose control. Besides widespread accessibility and acceptability of CGM across all population subsets, studies are needed comparing the ability of A1C and CGM-derived measures of glucose control to predict long-term outcomes in individuals with diabetes.
International A1C Target Recommendations
The International Society for Pediatric and Adolescent Diabetes (ISPAD) Clinical Practice Consensus Guidelines in 2018 (51) recommended a target of <7% for children and youth >5 years old. However, aiming for <7.5% was endorsed for those who cannot articulate symptoms of hypoglycemia or have hypoglycemia unawareness, have a history of severe hypoglycemia, lack access to analogs, are unable to monitor blood glucose regularly, or lack access to advanced insulin delivery technology or CGMs and in high glycators. A target of <6.5% was deemed optimal in situations where this target is attainable without excessive hypoglycemia, poor quality of life, or undue burden of care, and lower targets may be appropriate during the honeymoon period.
The National Institute for Health Care and Excellence (NICE) in the U.K. recommended in 2015 that providers explain to children and young people with T1D and their family members or caregivers (as appropriate) that an A1C target level of 48 mmol/mol (6.5%) or lower is ideal to minimize the risk of long-term complications (52).
The Swedish National Diabetes Register 2018 report revised A1C targets from <57 mmol/mol (<7.4%) to <48 mmol/mol (<6.5%) in May 2017, based on the results from the population-based cohort analysis between 1998 and 2017 (19). Of note, this decrease in A1C target was followed by a sharp decline in average A1C in children to 54.7 mmol/mol (7.2%).
Common Barriers to Achieving A1C Targets in T1D in Youth and Strategies to Address Them
Although near-normalization of A1C in children is associated with better diabetes outcomes during childhood and beyond, there are numerous barriers to achieving this goal. A major one is the fear of hypoglycemia on the part of persons with diabetes, their caregivers, and their clinical care providers (53). However, as detailed in the previous sections, the previously reported correlation between hypoglycemia and A1C is not observed with contemporary therapies and technology. The use of insulin analogs and diabetes technologies has increased the feasibility of achieving near-normal glycemia and demonstrably lowered the risk of severe hypoglycemia for children with T1D. It is expected that ongoing studies on the impact of the newest devices and systems on hypoglycemia and other diabetes-relevant outcomes including or focusing on pediatric participants (e.g., NCT04084171 in preschoolers, NCT02129868 in children and adolescents, NCT02302963, NCT02844517, and others; ClinicalTrials.gov) will demonstrate further risk reductions. Weight gain is another potential concern with intensive control, as the DCCT reports showed greater weight gain in persons in the intensive group (54). However, a subsequent pediatric study of children in four cohorts (1999, 2002, 2006, and 2009) found that, although use of intensive therapy increased, prevalence of overweight or obesity remained stable over time (55). In addition, in this study there was no relationship between A1C and BMI z-score after adjusting for potential confounders. Working with children and their parents to prevent weight gain is crucial in this population.
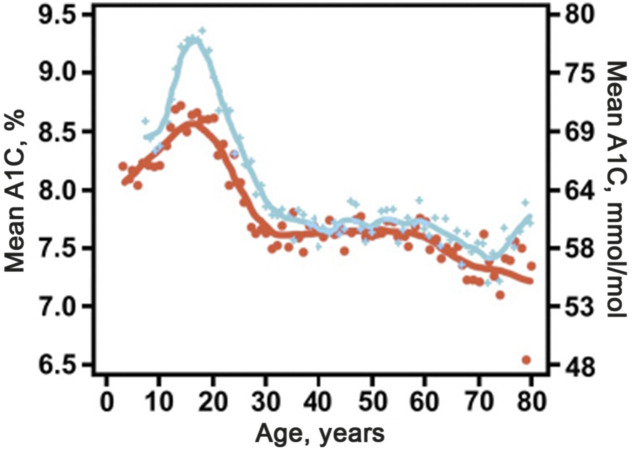
There are multiple levels where barriers to optimal glucose control may exist: biological (e.g., lack of residual β-cell function), behavioral (e.g., burnout), familial (e.g., burden of care), societal (e.g., lack of health insurance), as well as at the health care provider level (e.g., therapeutic inertia). An interplay of influences may result in marked worsening in glucose control, such as during adolescence, when puberty and growth hormones that promote gluconeogenesis and insulin resistance compound with the normal psychological process of striving for independence. Therefore, overcoming hurdles to optimal glucose control will require combinations of strategies. While diabetes technology has been demonstrated to lower A1C, the recent rise in A1C in the pediatric cohort of the T1D Exchange (56) (Fig. 3), despite increased technology adoption, emphasizes the need for multilayer approaches, including strategies that preserve β-cell function after T1D onset (57), improve quality of life, promote adherence to evidence-based recommendations and ongoing treatment plans, provide education to caregivers, advocate for policy changes, and combat therapeutic inertia, among others. The long-term tracking of glucose control from the time of onset (25,26) supports efforts to optimize modifiable factors as close to diagnosis as possible.
Figure 3.
Higher A1C in the 2016–2018 period compared with 2010–2012 across all ages, with particular elevation in adolescents and young adults (56) in the T1D Exchange Clinical Registry, which collected data from multiple clinical centers across the U.S.
Wide disparities exist in A1C and other health outcomes among youth with T1D. Socioeconomically disadvantaged children and those from racial/ethnic minority backgrounds have worse glycemic control, more frequent comorbidities (58–60), more frequent diabetes complications (61), and higher diabetes-associated costs (62). Strategies are needed that address the potentially modifiable factors that underlie disparities at multiple levels, including less access to care and technology, lower health education, and higher frequency of comorbidities (e.g., obesity, hypertension, dyslipidemia) (63). Racial and ethnic disparities in health outcomes are apparent from stage 3 diabetes onset, when African Americans are more likely to present in DKA and less likely to experience a partial remission period, and continue during the first years after diagnosis, with higher A1Cs and more frequent severe hypoglycemia and cardiovascular risk factors (64). Therefore, intervention approaches that are delivered early in the disease course among socioeconomically disadvantaged youth are needed to promote optimal T1D management and prevent costly complications.
Unfortunately, not every child worldwide has access to modern insulins, diabetes supplies, and even food. Similarly, diabetes technologies are not equally accessible to everyone. Studies demonstrate disparities in their use based on factors related to socioeconomics, health insurance type, age, access to care, race/ethnicity, education, and geography, among others (59). Trials to translate efficacious interventions into real-world settings, cost analyses, and advocacy are needed to help close the gaps in access to diabetes technology.
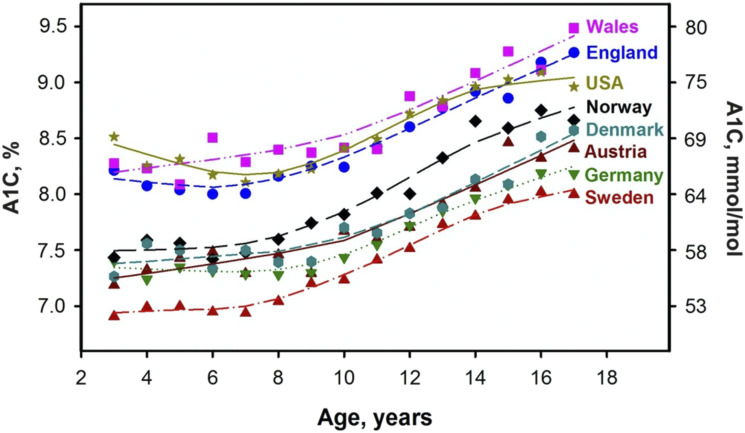
Mean A1C is higher in the U.S. than in some European countries. A comparison of eight high-income countries for glucose control in youth with T1D, with adjustment for sex, age, diabetes duration, and racial/ethnic minority status, found the lowest A1C in Sweden, where variation within centers was also lowest (65) (Fig. 4). Although all registries in this study reported International Federation of Clinical Chemistry and Laboratory Medicine (IFCC)-aligned values, differences in methodology across the different laboratories could have contributed to the variation observed. However, supporting international differences in A1C, a decline in A1C levels was observed in Sweden after lowering the target, unlike in the U.S., where a 2014 decrease in A1C target did not modify the upward temporal trend of A1C in youth with T1D. Participation in a quality improvement collaborative was a significantly differential factor between centers that experienced a decrease in A1C and others that did not between 2010 and 2014 in Sweden (66). In the U.S., the T1D Exchange Quality Improvement Collaborative (T1DX-QI) was established in 2016, initially with 10 U.S. participating diabetes clinics, and has since expanded with the goal to share data and best practices to improve care delivery in T1D (67).
Figure 4.
Comparison of mean A1C by age across eight high-income countries (69) in the Pediatric Diabetes Quality Registry, which collected data from Austria, Denmark, England, Germany, Norway, Sweden, the U.S., and Wales between 2013 and 2014.
Conclusions and Future Directions
The 2020 Standards of Care recommends adopting an A1C goal of <7% (53 mmol/mol) for many children with T1D, with an emphasis on individualized targets based on the individual risk-benefit ratio (recommendation 13.21, evidence grade B). This recommendation is driven by the overwhelming evidence of the deleterious influences of both chronic and acute hypoglycemia and hyperglycemia (e.g., brain structure changes, neurocognitive defects, long-lasting effects on the risk of microvascular and macrovascular complications), the decrease in overall incidence of severe hypoglycemia, the waning association between lower A1C target and hypoglycemia, and newer insulins and technological advances that have increased the feasibility of minimizing out-of-range glucose levels. The recent adaptation of a lower target for children by the ADA reflects similar guidance from other societies worldwide. Specifically, ISPAD proposed <7% in 2018 (51), NICE in the U.K. <6.5% in 2015 (52), and the Swedish National Diabetes Register 6.5% in 2018 (68).
Current gaps in knowledge include the risk factors for poor diabetes outcomes and hypoglycemia that allow identification of high-risk individuals for targeted interventions. Additionally, it will be important to understand the pathophysiology of the deleterious consequences of hypo- and hyperglycemia (e.g., effects on the brain, relative contribution of the degree and duration of hyperglycemia) that can be leveraged for prevention and treatment. A key gap area is socioeconomic and racial/ethnic disparities in diabetes outcomes and inequality in access to diabetes care and technology; this recognized need is fueling multiple initiatives at the research level, including trials to translate efficacious interventions to real-world settings, advocacy, and public policy. Furthermore, the implementation of strategies proven effective to optimize diabetes outcomes will be facilitated by ongoing behavioral research to address lack of adherence to treatment plans, concerns about quality of life, undue burden of care, and therapeutic inertia. International data indicate that lower A1C can be achieved safely in pediatrics, and there are ongoing efforts to utilize quality improvement methodology to implement proven efficacious strategies to optimize A1C in the U.S.
Article Information
Funding. D.M.M. was supported by National Institute of Diabetes and Digestive and Kidney Diseases grant P30DK116074.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.J.R. wrote the first draft of the manuscript. I.L., D.M.M., S.K.L., M.S., J.R., H.R., and L.A.D. contributed to the discussion and manuscript review and edits.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.13235495.
References
- 1.Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med 1993;329:304–309 [DOI] [PubMed] [Google Scholar]
- 2.Diabetes Control and Complications Trial Research Group; Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 3.Lasker RD The Diabetes Control and Complications Trial. Implications for policy and practice. N Engl J Med 1993;329:1035–1036 [DOI] [PubMed] [Google Scholar]
- 4.Nathan DM, Cleary PA, Backlund J-YC, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group . Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association Standards of Medical Care in Diabetes—2020 Diabetes Care 2020;43(Suppl. 1):S1–S212 [DOI] [PubMed]
- 6.American Diabetes Association Introduction: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S1–S2 [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association 13. Children and adolescents: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S163–S182 [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association 13. Children and adolescents: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S148–S164 [DOI] [PubMed] [Google Scholar]
- 9.Barnea-Goraly N, Raman M, Mazaika P, et al.; Diabetes Research in Children Network (DirecNet) . Alterations in white matter structure in young children with type 1 diabetes. Diabetes Care 2014;37:332–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foland-Ross LC, Buckingam B, Mauras N, et al.; Diabetes Research in Children Network (DirecNet) . Executive task-based brain function in children with type 1 diabetes: An observational study. PLoS Med 2019;16:e1002979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mauras N, Mazaika P, Buckingham B, et al.; Diabetes Research in Children Network (DirecNet) . Longitudinal assessment of neuroanatomical and cognitive differences in young children with type 1 diabetes: association with hyperglycemia. Diabetes 2015;64:1770–1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perantie DC, Wu J, Koller JM, et al. Regional brain volume differences associated with hyperglycemia and severe hypoglycemia in youth with type 1 diabetes. Diabetes Care 2007;30:2331–2337 [DOI] [PubMed] [Google Scholar]
- 13.Aye T, Barnea-Goraly N, Ambler C, et al. White matter structural differences in young children with type 1 diabetes: a diffusion tensor imaging study. Diabetes Care 2012;35:2167–2173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foland-Ross LC, Tong G, Mauras N, et al.; Diabetes Research in Children Network (DirecNet) . Brain function differences in children with type 1 diabetes: a functional MRI study of working memory. Diabetes 2020;69:1770–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Broadley MM, White MJ, Andrew B. A systematic review and meta-analysis of executive function performance in type 1 diabetes mellitus. Psychosom Med 2017;79:684–696 [DOI] [PubMed] [Google Scholar]
- 16.Pourabbasi A, Tehrani-Doost M, Qavam SE, Arzaghi SM, Larijani B. Association of diabetes mellitus and structural changes in the central nervous system in children and adolescents: a systematic review. J Diabetes Metab Disord 2017;16:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Downie E, Craig ME, Hing S, Cusumano J, Chan AKF, Donaghue KC. Continued reduction in the prevalence of retinopathy in adolescents with type 1 diabetes: role of insulin therapy and glycemic control. Diabetes Care 2011;34:2368–2373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nordwall M, Abrahamsson M, Dhir M, Fredrikson M, Ludvigsson J, Arnqvist HJ. Impact of HbA1c, followed from onset of type 1 diabetes, on the development of severe retinopathy and nephropathy: the VISS Study (Vascular Diabetic Complications in Southeast Sweden). Diabetes Care 2015;38:308–315 [DOI] [PubMed] [Google Scholar]
- 19.Lind M, Pivodic A, Svensson A-M, Ólafsdóttir AF, Wedel H, Ludvigsson J. HbA1c level as a risk factor for retinopathy and nephropathy in children and adults with type 1 diabetes: Swedish population based cohort study. BMJ 2019;366:l4894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conway B, Costacou T, Orchard T. Is glycaemia or insulin dose the stronger risk factor for coronary artery disease in type 1 diabetes? Diab Vasc Dis Res 2009;6:223–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller RG, Anderson SJ, Costacou T, Sekikawa A, Orchard TJ. Hemoglobin A1c level and cardiovascular disease incidence in persons with type 1 diabetes: an application of joint modeling of longitudinal and time-to-event data in the Pittsburgh Epidemiology of Diabetes Complications Study. Am J Epidemiol 2018;187:1520–1529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group; Nathan DM, Zinman B, Cleary PA, et al. Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983-2005). Arch Intern Med 2009;169:1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White NH, Cleary PA, Dahms W, Goldstein D, Malone J, Tamborlane WV; Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group . Beneficial effects of intensive therapy of diabetes during adolescence: outcomes after the conclusion of the Diabetes Control and Complications Trial (DCCT). J Pediatr 2001;139:804–812 [DOI] [PubMed] [Google Scholar]
- 24.Gubitosi-Klug RA, Bebu I, White NH, et al.; Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group . Screening eye exams in youth with type 1 diabetes under 18 years of age: Once may be enough? Pediatr Diabetes 2019;20:743–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hofer SE, Raile K, Fröhlich-Reiterer E, et al.; Austrian/German Diabetes Patienten Verlaufsdokumentation DPV Initiative; German Competence Network for Diabetes Mellitus . Tracking of metabolic control from childhood to young adulthood in type 1 diabetes. J Pediatr 2014;165:956–961.e1–2 [DOI] [PubMed] [Google Scholar]
- 26.Samuelsson U, Steineck I, Gubbjornsdottir S. A high mean-HbA1c value 3-15 months after diagnosis of type 1 diabetes in childhood is related to metabolic control, macroalbuminuria, and retinopathy in early adulthood—a pilot study using two nation-wide population based quality registries. Pediatr Diabetes 2014;15:229–235 [DOI] [PubMed] [Google Scholar]
- 27.Rawshani A, Sattar N, Franzén S,, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 2018;392:477–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Samuelsson J, Samuelsson U, Hanberger L, Bladh M, Åkesson K. Poor metabolic control in childhood strongly correlates to diabetes-related premature death in persons <30 years of age—a population-based cohort study. Pediatr Diabetes 2020;21:479–485 [DOI] [PubMed] [Google Scholar]
- 29.Van Name MA, Hilliard ME, Boyle CT, et al. Nighttime is the worst time: parental fear of hypoglycemia in young children with type 1 diabetes. Pediatr Diabetes 2018;19:114–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ishtiak-Ahmed K, Carstensen B, Pedersen-Bjergaard U, Jørgensen ME. Incidence trends and predictors of hospitalization for hypoglycemia in 17,230 adult patients with type 1 diabetes: a Danish register linkage cohort study. Diabetes Care 2017;40:226–232 [DOI] [PubMed] [Google Scholar]
- 31.Haynes A, Hermann JM, Clapin H, et al.; WACDD and DPV registries . Decreasing trends in mean HbA1c are not associated with increasing rates of severe hypoglycemia in children: a longitudinal analysis of two contemporary population-based pediatric type 1 diabetes registries from Australia and Germany/Austria between 1995 and 2016. Diabetes Care 2019;42:1630–1636 [DOI] [PubMed] [Google Scholar]
- 32.Haynes A, Hermann JM, Miller KM, et al.; T1D Exchange; WACDD and DPV registries . Severe hypoglycemia rates are not associated with HbA1c: a cross-sectional analysis of 3 contemporary pediatric diabetes registry databases. Pediatr Diabetes 2017;18:643–650 [DOI] [PMC free article] [PubMed]
- 33.Karges B, Rosenbauer J, Kapellen T, et al. Hemoglobin A1c Levels and risk of severe hypoglycemia in children and young adults with type 1 diabetes from Germany and Austria: a trend analysis in a cohort of 37,539 patients between 1995 and 2012. PLoS Med 2014;11:e1001742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cooper MN, O’Connell SM, Davis EA, Jones TW. A population-based study of risk factors for severe hypoglycaemia in a contemporary cohort of childhood-onset type 1 diabetes. Diabetologia 2013;56:2164–2170 [DOI] [PubMed] [Google Scholar]
- 35.Birkebaek NH, Drivvoll AK, Aakeson K, et al. Incidence of severe hypoglycemia in children with type 1 diabetes in the Nordic countries in the period 2008-2012: association with hemoglobin A1c and treatment modality. BMJ Open Diabetes Res Care 2017;5:e000377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karges B, Kapellen T, Wagner VM, et al.; DPV Initiative . Glycated hemoglobin A1c as a risk factor for severe hypoglycemia in pediatric type 1 diabetes. Pediatr Diabetes 2017;18:51–58 [DOI] [PubMed] [Google Scholar]
- 37.Bulsara MK, Holman CDJ, Davis EA, Jones TW. The impact of a decade of changing treatment on rates of severe hypoglycemia in a population-based cohort of children with type 1 diabetes. Diabetes Care 2004;27:2293–2298 [DOI] [PubMed] [Google Scholar]
- 38.Johnson SR, Cooper MN, Jones TW, Davis EA. Long-term outcome of insulin pump therapy in children with type 1 diabetes assessed in a large population-based case-control study. Diabetologia 2013;56:2392–2400 [DOI] [PubMed] [Google Scholar]
- 39.Karges B, Schwandt A, Heidtmann B, et al. Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis, and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA 2017;318:1358–1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laffel LM, Kanapka LG, Beck RW, et al.; CGM Intervention in Teens and Young Adults with T1D (CITY) Study Group . Effect of continuous glucose monitoring on glycemic control in adolescents and young adults with type 1 diabetes: a randomized clinical trial. JAMA 2020;323:2388–2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group; Tamborlane WV, Beck RW, Bode BW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 42.Bergenstal RM, Klonoff DC, Garg SK, et al.; ASPIRE In-Home Study Group . Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med 2013;369:224–232 [DOI] [PubMed] [Google Scholar]
- 43.Ly TT, Nicholas JA, Retterath A, Lim EM, Davis EA, Jones TW. Effect of sensor-augmented insulin pump therapy and automated insulin suspension vs standard insulin pump therapy on hypoglycemia in patients with type 1 diabetes: a randomized clinical trial. JAMA 2013;310:1240–1247 [DOI] [PubMed] [Google Scholar]
- 44.Brown SA, Kovatchev BP, Raghinaru D, et al.; iDCL Trial Research Group . Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med 2019;381:1707–1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown SA, Beck RW, Raghinaru D, et al.; iDCL Trial Research Group . Glycemic outcomes of use of CLC versus PLGS in type 1 diabetes: a randomized controlled trial. Diabetes Care 2020;43:1822–1828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weisman A, Bai J-W, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol 2017;5:501–512 [DOI] [PubMed] [Google Scholar]
- 47.Steineck I, Ranjan A, Nørgaard K, Schmidt S. Sensor-augmented insulin pumps and hypoglycemia prevention in type 1 diabetes. J Diabetes Sci Technol 2017;11:50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wright LA-C, Hirsch IB. Metrics beyond hemoglobin A1C in diabetes management: time in range, hypoglycemia, and other parameters. Diabetes Technol Ther 2017;19(S2):S16–S26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bergenstal RM, Gal RL, Connor CG, et al.; T1D Exchange Racial Differences Study Group . Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med 2017;167:95–102 [DOI] [PubMed] [Google Scholar]
- 50.Pease A, Lo C, Earnest A, Kiriakova V, Liew D, Zoungas S. Time in range for multiple technologies in type 1 diabetes: a systematic review and network meta-analysis. Diabetes Care 2020;43:1967–1975 [DOI] [PubMed] [Google Scholar]
- 51.DiMeglio LA, Acerini CL, Codner E, et al. ISPAD Clinical Practice Consensus Guidelines 2018: Glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diabetes 2018;19(Suppl. 27):105–114 [DOI] [PubMed] [Google Scholar]
- 52.National Institute for Health and Care Excellence (NICE). Diabetes (type 1 and type 2) in children and young people: diagnosis and management. NICE guideline [NG18], 2015. Accessed 30 October 2020. Available from https://www.nice.org.uk/guidance/ng18 [PubMed]
- 53.Haugstvedt A, Wentzel-Larsen T, Graue M, Søvik O, Rokne B. Fear of hypoglycaemia in mothers and fathers of children with Type 1 diabetes is associated with poor glycaemic control and parental emotional distress: a population-based study. Diabet Med 2010;27:72–78 [DOI] [PubMed] [Google Scholar]
- 54.Fullerton B, Jeitler K, Seitz M, Horvath K, Berghold A, Siebenhofer A. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev 2014;2:CD009122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baskaran C, Volkening LK, Diaz M, Laffel LM. A decade of temporal trends in overweight/obesity in youth with type 1 diabetes after the Diabetes Control and Complications Trial. Pediatr Diabetes 2015;16:263–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D Exchange in 2016-2018. Diabetes Technol Ther 2019;21:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haller MJ, Long SA, Blanchfield JL, et al.; Type 1 Diabetes TrialNet ATG-GCSF Study Group . Low-dose anti-thymocyte globulin preserves C-Peptide, reduces HbA1c, and increases regulatory to conventional T-cell ratios in new-onset type 1 diabetes: two-year clinical trial data. Diabetes 2019;68:1267–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hamman RF, Bell RA, Dabelea D, et al.; SEARCH for Diabetes in Youth Study Group . The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Willi SM, Miller KM, DiMeglio LA, et al.; T1D Exchange Clinic Network . Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mayer-Davis EJ, Beyer J, Bell RA, et al.; SEARCH for Diabetes in Youth Study Group . Diabetes in African American youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care 2009;32(Suppl. 2):S112–S122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lado JJ, Lipman TH. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am 2016;45:453–461 [DOI] [PubMed] [Google Scholar]
- 62.Glantz NM, Duncan I, Ahmed T, et al. Racial and ethnic disparities in the burden and cost of diabetes for US Medicare beneficiaries. Health Equity 2019;3:211–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Agarwal S, Kanapka LG, Raymond JK, et al. Racial-ethnic inequity in young adults with type 1 diabetes. J Clin Endocrinol Metab 2020;105:dgaa236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Redondo MJ, Libman I, Cheng P, et al.; Pediatric Diabetes Consortium . Racial/ethnic minority youth with recent-onset type 1 diabetes have poor prognostic factors. Diabetes Care 2018;41:1017–1024 [DOI] [PubMed] [Google Scholar]
- 65.Charalampopoulos D, Hermann JM, Svensson J, et al. Exploring variation in glycemic control across and within eight high-income countries: a cross-sectional analysis of 64,666 children and adolescents with type 1 diabetes. Diabetes Care 2018;41:1180–1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Samuelsson U, Åkesson K, Peterson A, Hanas R, Hanberger L. Continued improvement of metabolic control in Swedish pediatric diabetes care. Pediatr Diabetes 2018;19:150–157 [DOI] [PubMed] [Google Scholar]
- 67.Alonso GT, Corathers S, Shah A, et al. Establishment of the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Clin Diabetes 2020;38:141–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Åkesson K, Eriksson E, Samuelsson U, et al. Swediabkids - Swedish national quality registry for diabetes in children and adolescents, annual report 2018. Accessed 30 October 2020. Available from https://www.ndr.nu/pdfs/Yearreport_Swediabkids_2018_Eng.pdf
- 69.Anderzén J, Hermann JM, Samuelsson U, et al. International benchmarking in type 1 diabetes: large difference in childhood HbA1c between eight high-income countries but similar rise during adolescence-A quality registry study. Pediatr Diabetes 2020;21:621–627 [DOI] [PubMed] [Google Scholar]
- 70.American Diabetes Association Type 2 diabetes in children and adolescents. Diabetes Care 2000;23:381–389 [DOI] [PubMed] [Google Scholar]
- 71.American Diabetes Association Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003;26(Suppl. 1):S33–S50 [DOI] [PubMed] [Google Scholar]
- 72.Silverstein J, Klingensmith G, Copeland K, et al.; American Diabetes Association . Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care 2005;28:186–212 [DOI] [PubMed] [Google Scholar]
- 73.American Diabetes Association Standards of medical care in diabetes. Diabetes Care 2005;28(Suppl. 1):S4–S36 [PubMed] [Google Scholar]
- 74.American Diabetes Association Standards of medical care in diabetes—2006. Diabetes Care 2006;29(Suppl. 1):S4–S42 [PubMed] [Google Scholar]
- 75.American Diabetes Association Standards of medical care in diabetes—2007. Diabetes Care 2007;30(Suppl. 1):S4–S41 [DOI] [PubMed] [Google Scholar]
- 76.American Diabetes Association Standards of medical care in diabetes—2011. Diabetes Care 2011;34(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed]
- 77.American Diabetes Association Standards of Medical Care in Diabetes—2015 Diabetes Care 2015;38(Suppl. 1):S1–S93 [PubMed]
- 78.American Diabetes Association 11. Children and adolescents. Diabetes Care 2016;39(Suppl. 1):S86–S93 [DOI] [PubMed] [Google Scholar]
- 79.Arslanian S, Bacha F, Grey M, Marcus MD, White NH, Zeitler P. Evaluation and management of youth-onset type 2 diabetes: a position statement by the American Diabetes Association. Diabetes Care 2018;41:2648–2668 [DOI] [PMC free article] [PubMed] [Google Scholar]