Abstract
Objective
Sacral neuromodulation (SNM) has been used to treat patients with lower urinary tract dysfunction and bowel dysfunction for many years. Success rates vary between 50% and 80%, indicating that there is much room for improvement. Altering stimulation parameters may result in improved outcome. This paper reports a systematic review of the clinical efficacy of nonconventional stimulation parameters on urinary tract and bowel dysfunction.
Materials and Methods
Three databases were used for the literature search: Ovid (Medline, Embase) and PubMed. Papers were screened by two independent reviewers, who also extracted data from these papers. Clinical papers studying SNM stimulation parameters, that is, intermittent stimulation, frequency, pulse width, and amplitude, in urinary tract and bowel dysfunction were included. Quality of included papers was assessed using standardized guidelines.
Results
Out of 5659 screened papers, 17 papers, studying various stimulation parameters, were included. Overall quality of these papers differed greatly, as some showed no risk of bias, whereas others showed high risk of bias.
Stimulation parameters included intermittent stimulation, frequency, pulse width, amplitude, and unilateral vs. bilateral stimulation. Especially high frequency SNM and either a narrow or wide pulse width seem to improve efficacy in patients with bowel dysfunction. Additionally, implementation of short cycling intervals is promising to improve quality of life for patients with urinary tract or bowel dysfunction.
Conclusion
The results of our systematic review indicate that stimulation parameters may improve efficacy of SNM in treatment of both urinary tract dysfunction and bowel dysfunction.
Keywords: Fecal incontinence, sacral nerve stimulation, stimulation paradigm, voiding dysfunction
INTRODUCTION
Sacral neuromodulation (SNM) is used to treat both urinary and fecal storage and evacuation dysfunctions when conservative treatment options are not sufficient (1). SNM efficacy, defined as >50% reduction in symptoms compared to baseline, varies between 50% and 80% in both urinary tract and bowel dysfunction and depends on interindividual characteristics and indication (2, 3, 4, 5, 6, 7, 8). The fact that not all patients benefit from SNM underlines that there is much room for improvement to increase SNM efficacy. Furthermore, use of implantable pulse generators (IPGs) and SNM has shown to result in unwanted side effects including lead migration and pain surrounding the pocket. Recently, several technical improvements with respect to stimulation hardware have been introduced in SNM, for example, smaller IPGs, which resulted in a decrease of side effects. Additionally, staged implantation, as an alternative to percutaneous nerve evaluation (PNE), increased progression to IPG placement and decrease lead migration significantly (9, 10).
Up until now, SNM is most often applied as a rectangular signal, with a stimulation frequency of 14 Hz and a pulse width of 210 μs, also referred to as standard (conservative) stimulation parameters (11, 12). Additionally, most patients have their IPG switched on 24/7, in contrast to the early years of SNM, when patients had their IPG switched off during the night. There is a continuing debate whether change of SNM stimulation parameters may result in improved outcome. Studies in other clinical fields of neuromodulation, such as spinal cord stimulation in treatment of neuropathic pain or deep brain stimulation in motor disorders, have shown that long‐term efficacy can be improved with use of new stimulation parameters (13, 14). In this context, it is important to review what is known about the efficacy of SNM in patients with urinary tract and bowel dysfunction as related to stimulation parameters, that is, intermittent stimulation, frequency, pulse width, amplitude and unilateral vs. bilateral stimulation. Insights into the underlying mechanism of action related to SNM stimulation parameters in preclinical studies have been reviewed in an accompanying paper (15). However, to our knowledge, no systematic review has been conducted to determine whether these new stimulation parameters can improve the long‐term efficacy of SNM in patients with urinary tract and bowel dysfunction. As such, the aim of this review, and the afore mentioned accompanying paper (15), is to provide clinicians with new programming options regarding stimulation parameters and to provide pointers for future research focusing on SNM stimulation parameters in urinary tract and bowel dysfunction. In doing so, guidelines on trouble shooting, optimizing SNM efficacy and increasing battery life could be formed.
MATERIALS AND METHODS
Search Strategy
Two independent reviewers (PD, RA) performed extensive searches of the literature until January 14, 2020. This search was a shared search for both clinical and the preclinical literature on stimulation parameters for SNM on lower urinary tract and bowel dysfunction, meaning a systematic review on stimulation parameters in preclinical studies was performed in an accompanying paper. This review focuses only on human subjects and clinical outcomes. Due to the clinical heterogeneity across studies concerning study design, indication, outcomes, wash‐out periods, and follow‐up periods, a meta‐analysis was not performed.
Three databases were used to conduct a systematic literature search: Medline (PubMed), Ovid (Embase), and PubMed. Appendix A includes all used search terms. Results of the search were uploaded to EndNote, in which articles were assessed for relevance. Abstracts and full text papers were screened by both reviewers (RA, PD). No language restrictions were used, but no foreign language papers were eligible for inclusion in the review. In case RA and PD were in disagreement on inclusion of a paper, a third author (EAJ) made the final decision.
Study Selection and Inclusion Criteria
After final study inclusion, search results were allocated to either the clinical or the preclinical systematic review. Eligibility for inclusion of search results was evaluated based on the following criteria:
Preclinical or clinical study
Intervention of temporary or permanent SNM
Comparison of various SNM stimulation parameters
The quality of included articles was assessed by two reviewers (PD, RA) using three Risk of Bias (RoB) tools:
RoB 2.0 for randomized controlled trials (RCTs) (16)
RoB 2.0 crossover for randomized controlled crossover trials
The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews‐checklist for case series
If reviewers were in disagreement on RoB related to a certain category, a discussion was started until all issues were resolved. Data were extracted by two independent reviewers (RA and PD), and included first author, year of publication, indication of surgery, number of subjects, type of stimulation parameter, wash‐out period, follow‐up period, and primary outcome measure (Appendix B). A wash‐out period of less than one week was considered very short, and may result in carry‐over effects.
Due to the variety of outcome measures in the included studies, outcomes have been categorized as either objective or subjective. Objective outcomes are urinary voiding diaries, bowel habit diaries, pad changes, and anorectal measurements. Subjective outcomes consist of the following questionnaires: Cleveland Clinic Continence Score (CCCS), Patient Assessment of Constipation Symptoms Questionnaire (PAC‐SYM), Patient Assessment of Constipation Quality of Life questionnaire (PAC‐QOL), Fecal Incontinence Quality of Life Scale (FIQLS), St. Mark's Continence Score (SMCS), Gastrointestinal Symptom Rating Scale for Irritable Bowel Syndrome (GSRS‐IBS), 11‐point VAS scale for overall satisfaction, 101‐point VAS scale for satisfaction, Wexner score.
Studies are discussed, based on the SNM stimulation parameter investigated, in the following order: 1) intermittent stimulation, 2) frequency and pulse width, and 3) unilateral vs. bilateral SNM, amplitude. For each SNM stimulation parameter, first those studies dealing with urinary tract dysfunction are discussed followed by those focused at bowel dysfunction.
RESULTS
A total of 5659 records were identified by the search strategy, of which 1534 were duplicates (Fig. 1). An additional 4042 papers were excluded after title and abstract screening. Screening of the 83 full papers resulted in exclusion of 45 additional papers, resulting in 38 papers that were included, of which 17 were clinical papers (17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33).
Figure 1.
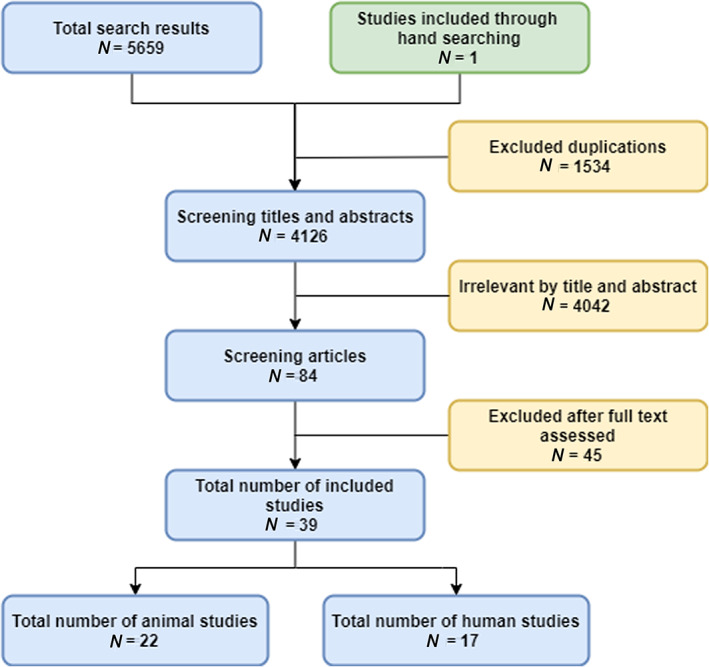
Flowchart of the included studies. [Color figure can be viewed at wileyonlinelibrary.com]
Risk of Bias Assessment
Four papers (23, 25, 26, 33) showed high RoB, mainly due to a very short washout period. Not all RCTs provided a method of randomization, although randomization itself was mentioned. Additionally, one case series showed a high RoB as well. Specifics of the RoB assessment are presented in Appendix C.
Characteristics of Included Studies
The study characteristics are summarized in Appendix B (Table B1). In detail, 11 papers included were RCTs with a crossover design (17, 18, 20, 21, 23, 25, 26, 28, 30, 31, 32). One paper used a RCT design with parallel groups (22) and five papers were based on case series analysis (19, 24, 27, 29, 33), of which four prospectively (19, 27, 29, 33) and one retrospectively (24). Eight papers studied the effect of cycling vs. continuous stimulation on urinary and bowel dysfunction (17, 18, 19, 20, 21, 22, 23, 24). Three papers studied both frequency and pulse width (27, 28, 30). Two papers studied unilateral vs. bilateral SNM (31). Three papers assessed amplitude levels (29, 32, 33) (Appendix B).
Effect of Intermittent Stimulation
Different types of interval stimulation were studied and compared to standard (conservative) stimulation (17, 18, 19, 20, 21, 22, 23, 24). One stimulation interval with both an “on” and “off” component was defined as one cycling interval (Tables 1 and 2). Intermittent stimulation was investigated as a means to improve efficacy and in order to prolong battery life.
Table 1.
Intermittent Stimulation and Outcome in SNM on Urinary Tract Dysfunction.
| Cycling interval | Time on, time off | Objective outcomes | Subjective outcomes | References |
|---|---|---|---|---|
| Short |
16 sec, 8 sec off; 20 sec on, 8 sec off |

|

|
(17, 18, 20, 21) |
| Medium |
10 min on, 10 min off; 1 hour on, 2 hours off |

|

|
(18, 21) |
| Long |
8 hours on, 16 hours off; 30 min on, 23.5 hours off; 23 hours on, 1 hour off; On demand |

|

|
(18, 19, 21, 22) |
 = in favor of continuous stimulation;
= in favor of continuous stimulation;  = no difference between conditions;
= no difference between conditions;  = in favor of intermittent stimulation.
= in favor of intermittent stimulation.
Table 2.
Intermittent Stimulation and Outcome in SNM on Bowel Dysfunction.
| Cycling interval | Time on, time off | Objective outcomes | Subjective outcomes | References |
|---|---|---|---|---|
| Short | 20 sec on, 8 sec off |

|
‐ | (24) |
| Long | Day on, night off |

|

|
(23) |
 = in favor of continuous stimulation;
= in favor of continuous stimulation;  = no difference between conditions;
= no difference between conditions;  = in favor of intermittent stimulation.
= in favor of intermittent stimulation.
Intermittent Stimulation and Urinary Tract Dysfunction
In patients with urinary tract dysfunction, objective outcome measures did not differ between standard (conservative) and intermittent stimulation (17, 18, 19, 20, 21, 22) (Table 1). Nevertheless, differences between standard and intermittent stimulation were noted as related to subjective measures, thereby indicating short cycling intervals to be favorable as compared to standard stimulation (17, 18). Conflicting results were reported when comparing long cycling intervals with continuous stimulation: on the one hand a decreased quality of life was found, assessed by IIQ‐7 score (18), on the other hand long cycling intervals seemed to result in less symptom severity for patients, assessed by PFDI‐20 score (19).
Intermittent Stimulation and Bowel Dysfunction
Short cycling SNM stimulation intervals showed noninferiority on objective outcomes (bowel habit diary) when compared with continuous cycling in patients with bowel dysfunction (Table 2). It is concluded that based on objective measures intermittent stimulation is favored (over standard SNM) on every outcome measure (24). It should be noted that this conclusion is based on one study which lacked a statistical analysis. Long cycling SNM stimulation intervals (day on, night off) showed similar effect when compared to continuous stimulation on objective outcomes (bowel habit diary). However, in a study with high risk of bias, they showed inferior efficacy on subjective outcomes (St. Mark's incontinence score, Wexner score) (23).
Effect of Frequency and Pulse Width
Standard, conservative settings for SNM frequency and pulse width are 7–20 Hz and 100–300 μsec, respectively. The effect of low (<7 Hz) and high frequency (>20 Hz), and narrow (<100 μs) and wide (>300 μs) pulse width on SNM efficacy in both urinary tract dysfunction and bowel dysfunction were studied (25, 26, 27, 28, 29).
Frequency and Urinary Tract Dysfunction
In urinary tract dysfunction, both low and high frequency were studied (25, 26) (Table 3). One study found no differences on either objective or subjective outcomes (25). However, the other study found negative objective outcomes (increase in pad changes and number of urinary incontinence episodes) when comparing low frequency with standard settings. It should be noted that both these studies showed high RoB due to a short wash‐out period (one day in both studies).
Table 3.
Frequency and Outcome in SNM on Urinary Tract Dysfunction.
| Frequency | Objective outcomes | Subjective outcomes | References |
|---|---|---|---|
| Low: <7 Hz |

|

|
(25, 26) |
| High: >20 Hz |

|

|
(25, 26) |
 = in favor of conventional frequency;
= in favor of conventional frequency;  = no difference between conditions;
= no difference between conditions;  = in favor of intervention.
= in favor of intervention.
Frequency and Pulse Width and Bowel Dysfunction
Regarding bowel dysfunction, neither objective nor subjective outcomes differed when comparing low frequency with standard frequency settings (Table 4) (27, 28, 30). High frequency did show an improvement in both subjective and objective outcomes when compared to standard settings. Switching to high frequency resulted in a decrease of fecal incontinence (FI) episodes and bowel movements per day and an improved quality of life (27, 28).
Table 4.
Frequency and Outcome in SNM on Bowel Dysfunction.
| Frequency | Objective outcomes | Subjective outcomes | References |
|---|---|---|---|
| Low: <7 Hz |

|

|
(27, 28, 30) |
| High: >20 Hz |

|

|
(27, 28, 30) |
 = in favor of conventional frequency;
= in favor of conventional frequency;  = no difference between conditions;
= no difference between conditions;  = in favor of intervention.
= in favor of intervention.
Narrowing the pulse widths, when compared to standard pulse width, results in improved objective outcomes (number of FI episodes) in one study (27), whereas others did not report this difference (28, 30) (Table 5). Subjective outcomes were contradictory: one study (27) showed improved quality of life, one (28) showed a decrease in quality of life, and one (30) found no differences. A wide pulse width was favorable over conventional pulse width in one study (27) on objective outcomes. No differences on objective and subjective outcomes as related to pulse width were reported in two other studies (28, 30).
Table 5.
Pulse Width and Outcome in SNM on Bowel Dysfunction.
| Pulse width | Objective outcomes | Subjective outcomes | References |
|---|---|---|---|
| Narrow: <100 μsec |

|

|
(27, 28, 30) |
| Wide: >300 μsec |

|

|
(27, 28, 30) |
 = in favor of conventional pulse width;
= in favor of conventional pulse width;  = no difference between conditions;
= no difference between conditions;  = in favor of intervention.
= in favor of intervention.
Effect of SNM Amplitude
SNM amplitude is normally set at sensory threshold. In the outpatient clinic, amplitude is increased up to a point where the patient feels the tingling sensation of stimulation. However, there is no scientific evidence to back up setting SNM amplitude at this level. The effect of subsensory stimulation, as compared to SNM at sensory threshold, was analyzed in three studies (29, 32, 33).
SNM Amplitude and Bowel Dysfunction
Subsensory stimulation at 50% of sensory threshold did not differ in SNM efficacy on objective and subjective measurements from stimulation at sensory threshold (29, 32). No difference between stimulation at subsensory (75% of sensory threshold) and stimulation at sensory threshold is reported (32). An earlier study (33) looked at amplitudes 0.6, 0.4, and 0.2 V below sensory threshold, but found only stimulation at sensory threshold decreased number of FI episodes significantly. This study only included eight subjects and scored a high RoB.
Effect of Unilateral vs. Bilateral SNM
With standard SNM, the electrode is implanted unilaterally to treat either urinary tract dysfunction or bowel dysfunction. From early studies (34, 35) on SNM in urinary tract dysfunction, it is deduced that bilateral SNM results in better treatment, since the bladder is bilaterally innervated (36, 37). However, at this moment there is no data available to support this.
Unilateral vs. Bilateral SNM and Bowel Dysfunction
No differences in effectiveness of unilateral SNM and bilateral SNM on either objective or subjective outcome measures are reported (31). The study by Duelund‐Jakobsen et al. was stopped after interim analysis of 20 patients showed there was no additional beneficial effect of bilateral stimulation. Moreover, the theoretical possibility of a doubling of infections and device‐related pain or discomfort was ground for an early termination of the study.
DISCUSSION AND CONCLUSION
This systematic review provides an overview of the clinical efficacy of SNM related to its stimulation parameters on lower urinary tract and bowel dysfunction.
Both high frequency and high pulse width showed favorable objective outcomes in patients with bowel dysfunction when compared with standard SNM. In patients with either urinary tract dysfunction or bowel dysfunction, no differences between SNM intermittent stimulation and standard SNM stimulation on objective outcomes were reported. Bilateral SNM efficacy did not differ from unilateral SNM efficacy. The SNM efficacy of subsensory stimulation, at 50% and 75% of subsensory threshold, did not differ from standard stimulation at sensory threshold.
When compared to standard settings, high frequency, but not low frequency, resulted in improved SNM efficacy on bowel dysfunction. As opposed to results in patients with bowel dysfunction, high frequency did not show favorable results in urinary tract dysfunction. It is very easy to alter frequency for patients in the outpatient clinic. Therefore, increasing the frequency to a level that is still comfortable for the patient could be an easy to implement intervention to increase SNM efficacy. In patients with neuropathic pain, high frequency stimulation is a successful alternative to conventional stimulation (38). It would be interesting to study whether such a high frequency would be feasible and effective in SNM patients.
Intermittent stimulation, and in particular short cycling intervals, seems to be a promising form of SNM in urinary tract dysfunction as related to subjective outcomes. On the one hand, short SNM cycling intervals improve quality of life for patients (17, 18). On the other hand, objective outcomes, that is, number of voids or leaks per day, did not improve using short cycling intervals (17, 18). Studies investigating long SNM cycling intervals show conflicting evidence, with one study reporting a decrease in quality of life (18) and another reporting a decrease in symptom severity for patients (19). Since the initial purpose of surgery is to improve quality of life for patients, this is a very interesting finding. In addition to the improved quality of life in patients with urinary tract dysfunction, short cycling intervals show a decrease in FI episodes as well (24), although this study lacked statistical analyses. All scores on intermittent stimulation were better than the scores on continuous stimulation on all domains. However, since no statistical analyses were performed, one can only draw the conclusion that intermittent stimulation is noninferior to continuous stimulation.
Even though the studies included and selected in this review regarding intermittent stimulation show similar results, the low number of studies, combined with different definitions of the duration of the intervals, make it difficult to provide conclusions. For example, short cycling intervals were defined as 16 sec (17, 18, 20, 21) or 20 sec (24) on and 8 sec off. A clear definition on certain cycling intervals, that is, in seconds on and seconds off, could improve homogeneity of studies and allow better comparison of results. Improved homogeneity of cycling intervals would consequently lead to a higher external validity and a stronger advice for clinical practice. Besides improving clinical efficacy, intermittent stimulation is often used as a way to improve battery longevity. Interestingly, Medtronic's manual (39) reports reduced longevity when using a 16 sec on, 8 sec off interval. Improved battery longevity is only 10–15% at a relatively high amplitude of 2.0 V with medium cycling intervals (i.e., 60 sec on, 60 sec off and 10 min on, 10 min off). Only when stimulating at 2.0 V using a long cycling interval (0.5 hour on, 23.5 hours off) a significant improvement in battery longevity of 40% was found. These numbers indicate that using intermittent stimulation is not a good means of prolonging battery life.
Bilateral SNM was studied, but showed no difference between unilateral and bilateral stimulation. One study, not included in this review, compared unilateral and bilateral stimulation using PNE instead of tined lead placement (TLP) (40). No significant differences were found between unilateral and bilateral stimulation and were thus in accordance with the paper included in this review. More studies comparing the unilateral and bilateral SNM in treatment of both urinary tract dysfunction and bowel dysfunction are needed to provide more conclusive results. However, due to the high costs of implanting SNM bilaterally, these studies are scarce.
With standard, conservative SNM, amplitude is set at sensory threshold during programming and is usually between 1 and 2 V. A downside of this way of programming is the fact that patients believe stimulation should always be at sensory threshold, instead of only during programming. As it is suggested in one pilot study (N = 17) and one follow‐up study (N = 75) that stimulation below sensory threshold does not affect efficacy of SNM in bowel dysfunction (29, 32), subsensory stimulation could be used. However, one other study (N = 8) showed no effect of SNM using subsensory stimulation (33). A clinically relevant advantage of SNM at subsensory threshold is the increase of battery life. To further substantiate the suggestion that SNM at subsensory threshold is as effective as SNM at sensory threshold, larger randomized trials are needed. Interestingly, McAlees et al. (41) are studying the effect of SNM in a sham controlled trial. To blind subjects, stimulation at subsensory threshold is used. It will be very interesting to see the results of this study, as this also might give more insight in the effect of stimulation at subsensory threshold.
Unfortunately, some studies were not included in this review due to high risk of bias. In particular, a short wash‐out period led to exclusion of studies. In future studies, a wash‐out period of at least one week is advisable in urinary dysfunction. In bowel dysfunction, a wash‐out period of at least three weeks is advised. Another limitation of this review is the high heterogeneity in subjective measures due to a lot of different questionnaires in both the fields of urology and surgery, which leads to confusion. Consensus on one questionnaire for urinary tract dysfunction and one for bowel dysfunction would make comparison of data a lot easier.
In conclusion, the results of our systematic review indicate that stimulation parameters may improve efficacy of SNM in treatment of both urinary tract dysfunction and bowel dysfunction. Especially implementation of short cycling intervals is promising for treatment of both urinary tract and bowel dysfunction. Additionally, high frequency SNM and either a narrow or wide pulse width seem to improve efficacy in patients with bowel dysfunction. Nevertheless, results should be treated cautiously, since the low number of small‐scale studies and limited quality of studies makes it not possible to provide final conclusions. Hence, large‐scale randomized studies are urgently needed.
Authorship Statement
Roman Assmann, Perla Douven, Gommert A. van Koeveringe, Elbert A. Joosten, Stephanie O. Breukink, and Jarno Melenhorst designed and conceptualized the study. Roman Assmann wrote the manuscript. Perla Douven, Roman Assmann, and Jos Kleijnen determined the systematic literature search strategy and performed the search. Perla Douven and Roman Assmann critically filtered the manuscripts and performed quality assessments. All authors have approved the final version of the manuscript.
COMMENT
This is a systematic review of all literature regarding stimulation parameters for patients with implanted sacral neurostimulation for bladder and bowel dysfunction. This is an interesting exploration that highlights the heterogeneity of evidence and lack of high quality evidence on the settings of stimulation parameters in sacral neuromodulation.
Kate Meriwether, MD
Rio Rancho, NM USA
All search strategies are based on work published in:
Riemsma R, Hagen S, Kirschner‐Hermanns R, Norton C, Wijk H, Andersson KE, Chapple C, Spinks J, Wagg A, Hutt E, Misso K, Deshpande S, Kleijnen J, Milsom I. Can incontinence be cured? A systematic review of cure rates [Internet]. BMC Med. 2017 [accessed 12.3.18];15(1):63. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5364653/
Embase (ovid): 1974–2020/01/13
Searched 14.1.2020
1. incontinence/
2. continence/
3. (incontinen$ or continen$ or obstipat$).ti,ab,ot.
4. urine incontinence/ or mixed incontinence/ or stress incontinence/ or urge incontinence/
5. ((Urine$ or urinary or urinat$ or micturat$ or bladder$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “lack of control” or “no control” or “out of control” or “not voluntary” or involuntary or wetting or leaked or seeped or retention$ or retain$ or dysfunct$ or malfunct$ or obstruct$ or block$ or overactiv$ or over‐activ$)).ti,ab,ot.
6. (bladder$ adj3 control$).ti,ab,ot.
7. (SUI or OAB or BPS).ti,ab,ot.
8. “giggle enuresis”.ti,ab,ot.
9. “enuresis risoria”.ti,ab,ot.
10. (incontinentia urinae or enuresis ureterica or ureter enuresis or enuresis diurnal).ti,ab,ot.
11. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (urine$ or urinat$ or urinary or micturat$)).ti,ab,ot.
12. neurogenic bladder/
13. ((neurogenic$ or neurologic$ or spinal or spastic$) adj4 bladder$).ti,ab,ot.
14. neurogenic vesical dysfunct$.ti,ab,ot.
15. (Bladder sphincter dys?ynergia or detrusor sphincter dys?ynergia or neurogenic detrusor overactiv$).ti,ab,ot.
16. feces incontinence/
17. (Encopresis or incontinentia alvi).ti,ab,ot.
18. ((bowel$ or rectum or rectal$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or uncontrolled or trickl$ or “lack of control” or “no control” or “out of control” or “not voluntary” or involuntary or control$)).ti,ab,ot.
19. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (faeces or faecal$ or feces or fecal$ or stool$ or rectum or rectal$ or bowel$ or bladder$ or anal$ or anus or urine or urinary or diarrh$ or soiling)).ti,ab,ot.
20. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
21. ((diarrh$ or Pseudodiarrh$ or Pseudo‐diarrh$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
22. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (diarrh$ or Pseudodiarrh$ or Pseudo‐diarrh$)).ti,ab,ot.
23. ((bowel$ or rectum or rectal$ or defecat$) adj4 (disorder$ or malfunction$ or dysfunction$ or evacuat$ or obstruct$ or block$)).ti,ab,ot.
24. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
25. (urinary tract adj3 (dysfunct$ or disorder$ of syndrome$)).ti,ab,ot.
26. (LUTD or LUTS).ti,ab,ot.
27. (pelvic floor adj3 (dysfunct$ or disorder$ of syndrome$)).ti,ab,ot.
28. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj2 (store or stored or storag$) adj2 (disorder$ or dysfunct$ or malfunct$ or syndrome$)).ti,ab,ot.
29. ((disorder$ or difficult$ or syndrome$) adj4 (urine$ or urinat$ or urinary or micturat$ or bladder$)).ti,ab,ot.
30. overactive bladder/
31. (detrusor adj2 (overactiv$ or over‐activ$)).ti,ab,ot.
32. cystitis/ or interstitial cystitis/
33. ((pain$ or discomfort$ or inflamm$ or infect$) adj4 (urine$ or urinat$ or urinary or micturat$ or bladder$ or pelvis or pelvic)).ti,ab,ot.
34. (megacystitis or cystitis or pericystitis).ti,ab,ot.
35. (detrusor adj2 (overactiv$ or over‐activ$)).ti,ab,ot.
36. ((bladder$ or hunner or hunneri or submucos$ or sub‐mucos$) adj2 (ulcus or ulcer$)).ti,ab,ot.
37. or/1‐36
38. sacral nerve stimulation/
39. InterStim.ti,ab,ot.
40. (SNS or SNM).ti,ab,ot.
41. (sacral adj3 (neuromodulat$ or neuro‐modulat$ or deafferent$ or de‐afferent$ or neurostimulat$ or neuro‐stimulat$)).ti,ab,ot.
42. medical electrical stimulation therap$.ti,ab,ot.
43. ((bladder$ or sacral$) adj2 (Autoaugment$ or Auto‐augment$)).ti,ab,ot.
44. (sacral nerve$ adj3 (modulat$ or stimulat$)).ti,ab,ot.
45. or/38‐44
46. 37 and 45
Medline (Ovid): 1946–2020/01/13
Searched 14.1.2020
1. Fecal Incontinence/
2. exp Urinary Incontinence/
3. Urinary Bladder, Neurogenic/
4. Urinary Bladder, Overactive/
5. cystitis/ or cystitis, interstitial/
6. urination disorders/ or urinary retention/
7. (incontinen$ or continen$ or obstipat$).ti,ab,ot.
8. ((Urine$ or urinary or urinat$ or micturat$ or bladder$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “lack of control” or “no control” or “out of control” or “not voluntary” or involuntary or wetting or leaked or seeped or retention$ or retain$ or dysfunct$ or malfunct$ or obstruct$ or block$ or overactiv$ or over‐activ$)).ti,ab,ot.
9. (bladder$ adj3 control$).ti,ab,ot.
10. (SUI or OAB or BPS).ti,ab,ot.
11. “giggle enuresis”.ti,ab,ot.
12. “enuresis risoria”.ti,ab,ot.
13. (incontinentia urinae or enuresis ureterica or ureter enuresis or enuresis diurnal).ti,ab,ot.
14. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (urine$ or urinat$ or urinary or micturat$)).ti,ab,ot.
15. ((neurogenic$ or neurologic$ or spinal or spastic$) adj4 bladder$).ti,ab,ot.
16. neurogenic vesical dysfunct$.ti,ab,ot.
17. (Bladder sphincter dys?ynergia or detrusor sphincter dys?ynergia or neurogenic detrusor overactiv$).ti,ab,ot.
18. (Encopresis or incontinentia alvi).ti,ab,ot.
19. ((bowel$ or rectum or rectal$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or uncontrolled or trickl$ or “lack of control” or “no control” or “out of control” or “not voluntary” or involuntary or control$)).ti,ab,ot.
20. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (faeces or faecal$ or feces or fecal$ or stool$ or rectum or rectal$ or bowel$ or bladder$ or anal$ or anus or urine or urinary or diarrh$ or soiling)).ti,ab,ot.
21. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
22. ((diarrh$ or Pseudodiarrh$ or Pseudo‐diarrh$) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
23. ((Unable or inabilit$ or abilit$ or able) adj3 control$ adj3 (diarrh$ or Pseudodiarrh$ or Pseudo‐diarrh$)).ti,ab,ot.
24. ((bowel$ or rectum or rectal$ or defecat$) adj4 (disorder$ or malfunction$ or dysfunction$ or evacuat$ or obstruct$ or block$)).ti,ab,ot.
25. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj4 (leak or leakage or leaks or leaking or seep or seepage or seeps or seeping or accident$ or escap$ or escaping or uncontrolled or trickl$ or “not voluntary” or involuntary or control$)).ti,ab,ot.
26. (urinary tract adj3 (dysfunct$ or disorder$ of syndrome$)).ti,ab,ot.
27. (LUTD or LUTS).ti,ab,ot.
28. (pelvic floor adj3 (dysfunct$ or disorder$ of syndrome$)).ti,ab,ot.
29. ((feces or faeces or fecal$ or faecal$ or stool or stools or defecat$ or soiling) adj2 (store or stored or storag$) adj2 (disorder$ or dysfunct$ or malfunct$ or syndrome$)).ti,ab,ot.
30. ((disorder$ or difficult$ or syndrome$) adj4 (urine$ or urinat$ or urinary or micturat$ or bladder$)).ti,ab,ot.
31. (detrusor adj2 (overactiv$ or over‐activ$)).ti,ab,ot.
32. ((pain$ or discomfort$ or inflamm$ or infect$) adj4 (urine$ or urinat$ or urinary or micturat$ or bladder$ or pelvis or pelvic)).ti,ab,ot.
33. (megacystitis or cystitis or pericystitis).ti,ab,ot.
34. (detrusor adj2 (overactiv$ or over‐activ$)).ti,ab,ot.
35. ((bladder$ or hunner or hunneri or submucos$ or sub‐mucos$) adj2 (ulcus or ulcer$)).ti,ab,ot.
36. or/1‐35
37. InterStim.ti,ab,ot.
38. (SNS or SNM).ti,ab,ot.
39. (sacral adj3 (neuromodulat$ or neuro‐modulat$ or deafferent$ or de‐afferent$ or neurostimulat$ or neuro‐stimulat$)).ti,ab,ot.
40. medical electrical stimulation therap$.ti,ab,ot.
41. ((bladder$ or sacral$) adj2 (Autoaugment$ or Auto‐augment$)).ti,ab,ot.
42. (sacral nerve$ adj3 (modulat$ or stimulat$)).ti,ab,ot.
43. or/37‐42
44. 36 and 43
PubMed (NLM): 1947–2020/01/13
Searched 14.1.2020
#52 Search (#41 AND #46 AND #51)
#51 Search (#50 OR #49)
#50 Search (((pubstatusaheadofprint OR publisher[sb])))
#49 Search (#47 OR (#47 AND #48))
#48 Search human*[tiab]
#47 Search (((rat[tiab] or rats[tiab] or mouse[tiab] or mice[tiab] or murine[tiab] or rodent[tiab] or rodents[tiab] or hamster[tiab] or hamsters[tiab] or pig[tiab] or pigs[tiab] or porcine[tiab] or rabbit[tiab] or rabbits[tiab] or animal[tiab] or animals[tiab] or dogs[tiab] or dog[tiab] or cats[tiab] or cow[tiab] or bovine[tiab] or sheep[tiab] or ovine[tiab] or monkey[tiab] or monkeys[tiab])))
#46 Search (#42 OR #43 OR #44 OR #45 OR)
#45 Search (“sacral nerve”[Title/Abstract]) AND (modulat*[Title/Abstract] OR stimulat*[Title/Abstract])
#44 Search ((sacral[Title/Abstract] OR Bladder*[Title/Abstract])) AND (neuromodulat*[Title/Abstract] OR neuro‐modulat*[Title/Abstract] OR deafferent*[Title/Abstract] OR de‐afferent*[Title/Abstract] OR neurostimulat*[Title/Abstract] OR neuro‐stimulat*[Title/Abstract] OR Autoaugment*[Title/Abstract] OR Auto‐augment*[Title/Abstract])
#43 Search (medical electrical stimulation[Title/Abstract]) AND therap*[Title/Abstract]
#42 Search (InterStim[Title/Abstract] OR SNS[Title/Abstract] OR SNM[Title/Abstract] OR PTNS[Title/Abstract])
#41 Search (#21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40)
#40 Search (#11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20)
#39 Search ((bladder*[Title/Abstract] OR hunner[Title/Abstract] OR hunneri[Title/Abstract] OR submucos*[Title/Abstract] OR sub‐mucos*[Title/Abstract])) AND (ulcus[Title/Abstract] OR ulcer*[Title/Abstract])
#38 Search ((pain*[Title/Abstract] OR discomfort*[Title/Abstract] OR inflamm*[Title/Abstract] OR infect*[Title/Abstract])) AND (urine*[Title/Abstract] OR urinat*[Title/Abstract] OR urinary[Title/Abstract] OR micturat*[Title/Abstract] OR bladder*[Title/Abstract] OR pelvis[Title/Abstract] OR pelvic[Title/Abstract])
#37 Search ((disorder*[Title/Abstract] OR difficult*[Title/Abstract] OR syndrome*[Title/Abstract])) AND (urine* or urinat* or urinary or micturat* or bladder*)
#36 Search (((feces[Title/Abstract] OR faeces[Title/Abstract] OR fecal*[Title/Abstract] OR faecal*[Title/Abstract] OR stool[Title/Abstract] OR stools[Title/Abstract] OR defecat*[Title/Abstract] OR soiling[Title/Abstract])) AND (store[Title/Abstract] OR stored[Title/Abstract] OR storag*[Title/Abstract])) AND (disorder*[Title/Abstract] OR dysfunct*[Title/Abstract] OR malfunct*[Title/Abstract] OR syndrome*[Title/Abstract])
#35 Search ((“urinary tract”[Title/Abstract] OR “pelvic floor”[Title/Abstract])) AND (dysfunct*[Title/Abstract] OR disorder*[Title/Abstract] OR syndrome*[Title/Abstract])
#34 Search (OAB[Title/Abstract] OR BPS[Title/Abstract] OR LUTD[Title/Abstract] OR LUTS[Title/Abstract])
#33 Search (((cystitis[Title/Abstract]) OR “overactive bladder”[Title/Abstract]) OR (“over‐active detrusor”[Title/Abstract] OR “overactive detrusor”[Title/Abstract])) OR (megacystitis[Title/Abstract] OR pericystitis[Title/Abstract])
#32 Search ((((Unable[Title/Abstract] OR inabilit*[Title/Abstract] OR abilit*[Title/Abstract] OR able[Title/Abstract])) AND control*[Title/Abstract]) AND (diarrh*[Title/Abstract] OR Pseudodiarrh*[Title/Abstract] OR Pseudo‐diarrh*[Title/Abstract]))
#31 Search (((diarrh*[Title/Abstract] OR Pseudodiarrh*[Title/Abstract] OR Pseudo‐diarrh*[Title/Abstract])) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR control*[Title/Abstract]))
#30 Search (((feces[Title/Abstract] OR faeces[Title/Abstract] OR fecal*[Title/Abstract] OR faecal*[Title/Abstract] OR stool[Title/Abstract] OR stools[Title/Abstract] OR defecat*[Title/Abstract] OR soiling[Title/Abstract])) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR control*[Title/Abstract]))
#29 Search ((((Unable[Title/Abstract] OR inabilit*[Title/Abstract] OR abilit*[Title/Abstract] OR able[Title/Abstract])) AND control*[Title/Abstract]) AND (faeces[Title/Abstract] OR faecal*[Title/Abstract] OR feces[Title/Abstract] OR fecal*[Title/Abstract] OR stool*[Title/Abstract] OR rectum[Title/Abstract] OR rectal*[Title/Abstract] OR bowel*[Title/Abstract] OR bladder*[Title/Abstract] OR anal*[Title/Abstract] OR anus[Title/Abstract] OR urine[Title/Abstract] OR urinary[Title/Abstract] OR diarrh*[Title/Abstract] OR soiling[Title/Abstract]))
#28 Search ((rectal[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR control*[Title/Abstract]))
#27 Search ((rectum[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR control*[Title/Abstract]))
#26 Search ((bowel*[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR control*[Title/Abstract]))
#25 Search ((Encopresis[Title/Abstract] OR “incontinentia alvi”[Title/Abstract]))
#24 Search ((“Bladder sphincter dyssynergia”[Title/Abstract] OR “detrusor sphincter dysynergia”[Title/Abstract] OR “Bladder sphincter dysynergia”[Title/Abstract] OR “detrusor sphincter dyssynergia”[Title/Abstract] OR “neurogenic detrusor overactivity”[Title/Abstract]))
#23 Search ((SUI[Title/Abstract] OR “giggle enuresis”[Title/Abstract] OR “enuresis risoria”[Title/Abstract] OR “incontinentia urinae”[Title/Abstract] OR “enuresis ureterica”[Title/Abstract] OR “ureter enuresis”[Title/Abstract] OR “enuresis diurnal”[Title/Abstract]))
#22 Search ((bladder*[Title/Abstract]) AND control*[Title/Abstract])
#21 Search “neurogenic vesical dysfunction”[Title/Abstract]
#20 Search ((bladder*[Title/Abstract]) AND (neurogenic*[Title/Abstract] OR neurologic*[Title/Abstract] OR spinal[Title/Abstract] OR spastic*[Title/Abstract]))
#19 Search ((((Unable[Title/Abstract] OR inabilit*[Title/Abstract] OR abilit*[Title/Abstract] OR able[Title/Abstract])) AND control*[Title/Abstract]) AND (urine*[Title/Abstract] OR urinat*[Title/Abstract] OR urinary[Title/Abstract] OR micturat*[Title/Abstract]))
#18 Search ((bladder*[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR wetting[Title/Abstract] OR leaked[Title/Abstract] OR seeped[Title/Abstract]))
#17 Search ((micturat*[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR wetting[Title/Abstract] OR leaked[Title/Abstract] OR seeped[Title/Abstract]))
#16 Search ((urinat*[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR wetting[Title/Abstract] OR leaked[Title/Abstract] OR seeped[Title/Abstract]))
#15 Search ((urinary[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR wetting[Title/Abstract] OR leaked[Title/Abstract] OR seeped[Title/Abstract]))
#14 Search ((Urine*[Title/Abstract]) AND (leak[Title/Abstract] OR leakage[Title/Abstract] OR leaks[Title/Abstract] OR leaking[Title/Abstract] OR seep[Title/Abstract] OR seepage[Title/Abstract] OR seeps[Title/Abstract] OR seeping[Title/Abstract] OR accident*[Title/Abstract] OR escap*[Title/Abstract] OR escaping[Title/Abstract] OR uncontrolled[Title/Abstract] OR trickl*[Title/Abstract] OR “lack of control”[Title/Abstract] OR “no control”[Title/Abstract] OR “out of control”[Title/Abstract] OR “not voluntary”[Title/Abstract] OR involuntary[Title/Abstract] OR wetting[Title/Abstract] OR leaked[Title/Abstract] OR seeped[Title/Abstract]))
#13 Search (“bladder* control*”[Title/Abstract] OR SUI[Title/Abstract] OR “giggle enuresis”[Title/Abstract] OR “enuresis risoria”[Title/Abstract] OR “incontinentia urinae”[Title/Abstract] OR “enuresis ureterica”[Title/Abstract] OR “ureter enuresis”[Title/Abstract])
#12 Search (incontinen*[Title/Abstract]) OR continen*[Title/Abstract]
#11 Search ((((((((“Urinary Incontinence”[Mesh]) OR “Fecal Incontinence”[Mesh:NoExp]) OR “Urinary Bladder, Neurogenic”[Mesh:NoExp]) OR “Urinary Bladder, Overactive”[Mesh]) OR “Cystitis”[Mesh:NoExp]) OR “Cystitis, Interstitial”[Mesh:NoExp]) OR “Urination Disorders”[Mesh:NoExp]) OR “Urinary Retention”[Mesh])
Table B1.
Characteristics of Included Articles.
| Study | Year | Indication | No. of subjects | Stimulation parameter | Cycling: on vs. off | Frequency | Pulse width | Amplitude | Primary outcome | Wash‐out period | Follow‐up period |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beer et al. (17) | 2016 | OAB | 23 | Intermittent stimulation | 16 sec on, 8 sec off | ‐ | ‐ | ‐ | OABq SF scores | 3 months | 3 days |
| Cadish et al. (18) | 2016 | OAB | 23 | Intermittent stimulation |
16 sec on, 8 sec off;23 hours on, 1 hour off; 1 hour on, 2 hours off |
‐ | ‐ | ‐ |
IIQ‐7 score and Likert score; Number of voids/day and number of leaks/day |
13 days | 1 day |
| Hoen et al. (19) | 2007 | OAB | 19 | Intermittent stimulation | 8 hours on, 16 hours off | 14 Hz | 210 μsec | 1.1–2.9 V |
UDI‐6, IIQ‐7, PFDI‐20, PFIQ‐7, PISQ‐12, FIQLS, and FISI; Voiding diary |
2 weeks | 12 weeks |
| Markle Price and Noblett (20) | 2015 | OAB | 32 | Intermittent stimulation | 16 sec on, 8 sec off | 14 Hz | 210 μsec | ST | UIIQ and UDI; Voiding diary | 4 weeks | 3 days |
| Siegel et al. (21) | 2017 | OAB | 28 | Intermittent stimulation |
16 sec on, 8 sec off 10 min on, 10 min off 30 min on, 23.5 hours off |
‐ | ‐ | ‐ |
GRA scores; Incontinence episodes per day |
3 weeks | 1 week |
| Oerlemans et al. (22) | 2011 | OAB | 21 | Intermittent stimulation | On demand vs. continuous (min. 4 hours off) | ‐ | ‐ | ‐ |
UMQ; Voiding diary |
‐ | Not mentioned |
| Michelsen et al. (23) | 2008 | FI | 19 | Intermittent stimulation | Day on, night off | ‐ | ‐ | ‐ |
Wexner score, St. Mark's continence score; Bowel habit diary |
No wash‐out | 3 weeks |
| Norderval et al. (24) | 2013 | FI | 29 | Intermittent stimulation | 20 sec on, 8 sec off | ‐ | ‐ | ‐ | Bowel habit diary | ‐ | 3–34 months |
| Marcelissen et al. (25) | 2011 | OAB | 50 | Frequency | ‐ | 5.2, 10, 21, 40 Hz | 210 μsec | ST |
Questionnaire; Voiding diary |
1 day | 6 days |
| Peters et al. (26) | 2013 | OAB | 12 | Frequency | ‐ | 5.2, 14, 25 Hz | ‐ | ‐ |
11‐point VAS scale on pelvic pain; Voiding and bowel habit diaries |
1 day | 6 days |
| Dudding et al. (27) | 2009 | FI | 12 | Frequency + pulse width | ‐ |
6.9, 14, 31 Hz |
90, 210, 450 μsec | ST |
St. Mark's continence score, FIQLS; Bowel habit diary |
‐ | 2 weeks |
| Duelund‐Jakobsen et al. (28) | 2012 | FI | 15 | Frequency + pulse width | ‐ | 6.9, 14, 31 Hz | 90, 210, 330 μsec | ST |
FIQLS, CCCS, SMCS, GSRS‐IBS, 11‐point VAS scale for overall satisfaction; Bowel habit diary, anorectal measurements |
1 week | 3 weeks |
| Duelund‐Jakobsen et al. (29) | 2019 | FI | 17 | Frequency | ‐ | 14, 31 Hz | 90, 210 μsec | ‐ | FIQoL, CCCS, VAS scale for satisfaction; Bowel habit diary | 2 months | 12 months |
| Thomas et al. (30) | 2015 | Constipation | 11 | Frequency + pulse width | ‐ | 6.9, 14, 31 Hz | 90, 210, 450 μsec | ST |
CCCS, PAC‐SYM, PAC‐QOL, 101‐point VAS scale for satisfaction; Bowel habit diary |
2 weeks | 3 weeks |
| Duelund‐Jakobsen et al. (31) | 2015 | FI | 27 | Bilateral vs. unilateral SNM | ‐ | 14 Hz | 210 μsec | ST |
Wexner score, SMCS, GSRS‐IBS, FIQLS; Bowel habit diary, anorectal measurements |
1 week | 3 weeks |
| Duelund‐Jakobsen et al. (32) | 2013 | FI | 17 | Amplitude | ‐ | ‐ | ‐ |
50% ST; 75% ST; ST |
Wexner score, SMCS, GSRS‐IBS, FIQLS, 11‐point VAS score on satisfaction; Bowel habit diary, anorectal measurements |
1 week | 3 weeks |
| Duelund‐Jakobsen et al. (29) | 2019 | FI | 75 | Amplitude | ‐ | 14, 31 Hz | 90, 210 μsec |
50% ST; ST |
FIQoL, CCCS, VAS scale for satisfaction; Bowel habit diary | 2 months | 12 months |
| Koch et al. (33) | 2005 | FI | 8 | Amplitude | ‐ | ‐ | ‐ |
0.6 V < ST; 0.4 V < ST; 0.2 V < ST; ST |
Bowel habit diary | ‐ | 4 weeks |
Randomized Controlled Trials [Color table can be viewed at wileyonlinelibrary.com]
| Article | Bias from randomization process | Bias due to deviations from intended interventions | Bias due to missing outcome data | Bias in measurement of outcome | Bias in selection of reported result | Overall bias |
|---|---|---|---|---|---|---|
| Oerlemans et al. (22) | SOME RISK | SOME RISK | LOW RISK | LOW RISK | LOW RISK | MODERATE RISK |
RCT With Cross‐Over Design [Color table can be viewed at wileyonlinelibrary.com]
| Article | Bias from randomization process | Bias due to deviations from intended interventions | Bias due to missing outcome data | Bias in measurement of outcome | Bias in selection of reported result | Overall bias |
|---|---|---|---|---|---|---|
| Beer et al. (17) | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK |
| Cadish et al. (18) | SOME RISK | LOW RISK | LOW RISK | LOW RISK | SOME RISK | MODERATE RISK |
| Duelund‐Jakobsen et al. (28) | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK |
| Duelund‐Jakobsen et al. (32) | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK |
| Duelund‐Jakobsen et al. (31) | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK |
| Marcelissen et al. (25) | SOME RISK | HIGH RISK | LOW RISK | LOW RISK | SOME RISK | HIGH RISK |
| Michelsen et al. (23) | LOW RISK | HIGH RISK | LOW RISK | LOW RISK | LOW RISK | HIGH RISK |
| Peters et al. (26) | SOME RISK | HIGH RISK | LOW RISK | LOW RISK | LOW RISK | HIGH RISK |
| Price et al. (20) | LOW RISK | LOW RISK | SOME RISK | LOW RISK | LOW RISK | MODERATE RISK |
| Thomas et al. (30) | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK |
| Siegel et al. (21) | SOME RISK | LOW RISK | LOW RISK | LOW RISK | LOW RISK | MODERATE RISK |
Case Series [Color table can be viewed at wileyonlinelibrary.com]
| Article | Clear criteria for inclusion in case series | Condition measured in standard, reliable way | Valid methods used for identification of the condition | Consecutive inclusion of participants | Complete inclusion of participants | Clear reporting of demographics | Clear reporting of clinical information | Outcomes clearly reported | Clear reporting of presenting sites | Statistical analysis appropriate | Wash‐out period sufficient | Overall bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dudding, et al., 2009 (27) | YES | YES | YES | UNCLEAR | UNCLEAR | YES | YES | YES | YES | YES | N/A | MODERATE RISK |
| Duelund‐Jakobsen, et al., 2019 (29) | YES | YES | YES | UNCLEAR | YES | NO | YES | YES | YES | YES | YES | LOW RISK |
| Hoen, et al., 2017 (19) | YES | YES | YES | UNCLEAR | UNCLEAR | YES | YES | YES | UNCLEAR | YES | YES | MODERATE RISK |
| Koch, et al., 2005 (33) | YES | YES | YES | UNCLEAR | UNCLEAR | YES | YES | YES | UNCLEAR | YES | NO | HIGH RISK |
| Norderval, et al., 2013 (24) | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | N/A | LOW RISK |
For more information on author guidelines, an explanation of our peer review process, and conflict of interest informed consent policies, please go to http://www.wiley.com/WileyCDA/Section/id-301854.html
Source(s) of financial support: There were no sources of financial support.
Conflict of Interest: Gommert A. van Koeveringe declares to have a conflict of interest for Medtronic and Axonics. All other authors declare that they have no conflicts of interest.
REFERENCES
- 1. Moore CK, Rueb JJ, Derisavifard S. What is new in neuromodulation? Curr Urol Rep 2019;20:55. [DOI] [PubMed] [Google Scholar]
- 2. Janssen PTJ, Kuiper SZ, Stassen LPS, Bouvy ND, Breukink SO, Melenhorst J. Fecal incontinence treated by sacral neuromodulation: long‐term follow‐up of 325 patients. Surgery 2017;161:1040–1048. [DOI] [PubMed] [Google Scholar]
- 3. Peeters K, Sahai A, De Ridder D, Van Der Aa F. Long‐term follow‐up of sacral neuromodulation for lower urinary tract dysfunction. BJU Int 2014;113:789–794. [DOI] [PubMed] [Google Scholar]
- 4. Marcelissen TAT, Leong RK, de Bie RA, van Kerrebroeck PEV, de Wachter SGG. Long‐term results of sacral neuromodulation with the tined lead procedure. J Urol 2010;184:1997–2000. [DOI] [PubMed] [Google Scholar]
- 5. Siegel S, Noblett K, Mangel J et al. Results of a prospective, randomized, multicenter study evaluating sacral neuromodulation with InterStim therapy compared to standard medical therapy at 6‐months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn 2015;34:224–230. [DOI] [PubMed] [Google Scholar]
- 6. Thin NN, Horrocks EJ, Hotouras A et al. Systematic review of the clinical effectiveness of neuromodulation in the treatment of faecal incontinence. Br J Surg 2013;100:1430–1447. [DOI] [PubMed] [Google Scholar]
- 7. van Kerrebroeck PEV, van Voskuilen AC, Heesakkers JPFA et al. Results of sacral neuromodulation therapy for urinary voiding dysfunction: outcomes of a prospective, worldwide clinical study. J Urol 2007;178:2029–2034. [DOI] [PubMed] [Google Scholar]
- 8. Jarrett MED, Mowatt G, Glazener CMA et al. Systematic review of sacral nerve stimulation for faecal incontinence and constipation. Br J Surg 2004;91:1559–1569. [DOI] [PubMed] [Google Scholar]
- 9. Baxter C, Kim J‐H. Contrasting the percutaneous nerve evaluation versus staged implantation in sacral neuromodulation. Curr Urol Rep 2010;11:310–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bannowsky A, Wefer B, Braun PM, Jünemann K‐P. Urodynamic changes and response rates in patients treated with permanent electrodes compared to conventional wire electrodes in the peripheral nerve evaluation test. World J Urol 2008;26:623–626. [DOI] [PubMed] [Google Scholar]
- 11. Matzel KE, Stadelmaier U, Hohenfellner M, Gall FP. Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Lancet 1995;346:1124–1127. [DOI] [PubMed] [Google Scholar]
- 12. Thon WF, Baskin LS, Jonas U, Tanagho EA, Schmidt RA. Neuromodulation of voiding dysfunction and pelvic pain. World J Urol 1991;9:138–141. [Google Scholar]
- 13. Miller JP, Eldabe S, Buchser E, Johanek LM, Guan Y, Linderoth B. Parameters of spinal cord stimulation and their role in electrical charge delivery: a review. Neuromodulation 2016;19:373–384. [DOI] [PubMed] [Google Scholar]
- 14. Dayal V, Limousin P, Foltynie T. Subthalamic nucleus deep brain stimulation in Parkinson's disease: the effect of varying stimulation parameters. J Parkinsons Dis 2017;7:235–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Douven PAR, Breukink SO, Melenhorst J et al. Sacral neuromodulation for lower urinary tract and bowel dysfunction in animal models: a systematic review with focus on stimulation parameter selection MUMC+, 2020:21. [DOI] [PMC free article] [PubMed]
- 16. Sterne JAC, Savović J, Page MJ et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 17. Beer GM, Gurule MM, Komesu YM, Qualls CR, Rogers RG. Cycling versus continuous mode in neuromodulator programming: a crossover, randomized, controlled trial. Urol Nurs 2016;36:123–132. [PMC free article] [PubMed] [Google Scholar]
- 18. Cadish LA, Osann KE, Noblett KL. Stimulation latency and comparison of cycling regimens in women using sacral neuromodulation. Neurourol Urodyn 2017;36:486–489. [DOI] [PubMed] [Google Scholar]
- 19. Hoen LA, Groen J, Scheepe JR, Blok BF. Intermittent sacral neuromodulation for idiopathic urgency urinary incontinence in women. Neurourol Urodyn 2017;36:385–389. [DOI] [PubMed] [Google Scholar]
- 20. Markle Price D, Noblett K. Prospective randomized crossover trial comparing continuous and cyclic stimulation in InterStim therapy. Female Pelvic Med Reconstr Surg 2015;21:355–358. [DOI] [PubMed] [Google Scholar]
- 21. Siegel S, Kreder K, Takacs E, McNamara R, Kan F. Prospective randomized feasibility study assessing the effect of cyclic sacral neuromodulation on urinary urge incontinence in women. Female Pelvic Med Reconstr Surg 2018;24:267–271. [DOI] [PubMed] [Google Scholar]
- 22. Oerlemans DJAJ, Van Voskuilen AC, Marcelissen T, Weil EHJ, De Bie RA, Van Kerrebroeck PEV. Is on‐demand sacral neuromodulation in patients with OAB syndrome a feasible therapy regime? Neurourol Urodyn 2011;30:1493–1496. [DOI] [PubMed] [Google Scholar]
- 23. Michelsen HB, Krogh K, Buntzen S, Laurberg S. A prospective, randomized study: switch off the sacral nerve stimulator during the night? Dis Colon Rectum 2008;51:538–540. [DOI] [PubMed] [Google Scholar]
- 24. Norderval S, Behrenbruch C, Brouwer R, Keck JO. Efficacy of cyclic sacral nerve stimulation for faecal incontinence. Tech Coloproctol 2013;17:511–516. [DOI] [PubMed] [Google Scholar]
- 25. Marcelissen TA, Leong RK, Nieman FH, de Bie RA, van Kerrebroeck PE, de Wachter SG. The effect of pulse rate changes on the clinical outcome of sacral neuromodulation. J Urol 2011;185:1781–1785. [DOI] [PubMed] [Google Scholar]
- 26. Peters KM, Shen L, McGuire M. Effect of sacral neuromodulation rate on overactive bladder symptoms: a randomized crossover feasibility study. Low Urin Tract Symptoms 2013;5:129–133. [DOI] [PubMed] [Google Scholar]
- 27. Dudding TC, Vaizey CJ, Gibbs A, Kamm MA. Improving the efficacy of sacral nerve stimulation for faecal incontinence by alteration of stimulation parameters. Br J Surg 2009;96:778–784. [DOI] [PubMed] [Google Scholar]
- 28. Duelund‐Jakobsen J, Dudding T, Bradshaw E et al. Randomized double‐blind crossover study of alternative stimulator settings in sacral nerve stimulation for faecal incontinence. Br J Surg 2012;99:1445–1452. [DOI] [PubMed] [Google Scholar]
- 29. Duelund‐Jakobsen J, Buntzen S, Laurberg S, Lundby L. Improved longevity and efficacy of sacral nerve stimulation by simple adjustments at follow‐up. Colorectal Dis 2020;22:310–318. [DOI] [PubMed] [Google Scholar]
- 30. Thomas GP, Duelund‐Jakobsen J, Dudding TC et al. A double‐blinded randomized multicentre study to investigate the effect of changes in stimulation parameters on sacral nerve stimulation for constipation. Colorectal Dis 2015;17:990–995. [DOI] [PubMed] [Google Scholar]
- 31. Duelund‐Jakobsen J, Buntzen S, Lundby L, Sorensen M, Laurberg S. Bilateral compared with unilateral sacral nerve stimulation for faecal incontinence: results of a randomized, single‐blinded crossover study. Colorectal Dis 2015;17:1085–1093. [DOI] [PubMed] [Google Scholar]
- 32. Duelund‐Jakobsen J, Buntzen S, Lundby L, Laurberg S. Sacral nerve stimulation at subsensory threshold does not compromise treatment efficacy: results from a randomized, blinded crossover study. Ann Surg 2013;257:219–223. [DOI] [PubMed] [Google Scholar]
- 33. Koch SMP, van Gemert WG, Baeten CGMI. Determination of therapeutic threshold in sacral nerve modulation for faecal incontinence. Br J Surg 2005;92:83–87. [DOI] [PubMed] [Google Scholar]
- 34. Hohenfellner M, Schultz‐Lampel D, Dahms S, Matzel K, Thuroff JW. Bilateral chronic sacral neuromodulation for treatment for lower urinary tract dysfunction. J Urol 1998;160:821–824. [DOI] [PubMed] [Google Scholar]
- 35. Sauerwein D, Kutzenberger B, Domurath B. Bilateraler sakraler Zugang nach Laminektomie zur permanenten Neuromodulation durch veränderte Operationstechnik und modifizierte Elektroden. Urologe A 1997;36:57. [Google Scholar]
- 36. Ingersoll EH, Jones LL, Hegre ES. Effect on urinary bladder of unilateral stimulation of pelvic nerves in the dog. Am J Physiol 1957;189:167–172. [DOI] [PubMed] [Google Scholar]
- 37. Diokno A, Davis R, Lapides J. The effect of pelvic nerve stimulation on detrusor contraction. Invest Urol 1973;11:178–181. [PubMed] [Google Scholar]
- 38. Russo M, Van Buyten J‐P. 10‐kHz high‐frequency SCS therapy: a clinical summary. Pain Med 2015;16:934–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Medtronic . System Eligibility, Battery Longevity, Specifications InterStim Systems 2020. http://manuals.medtronic.com/content/dam/emanuals/neuro/M988757A003A_view.pdf
- 40. Scheepens WA, De Bie RA, Weil EHJ, Van Kerrebroeck EV. Unilateral versus bilateral sacral neuromodulation in patients with chronic voiding dysfunction. J Urol 2002;168:2046–2050. [DOI] [PubMed] [Google Scholar]
- 41. McAlees E, Vollebregt PF, Stevens N et al. Efficacy and mechanism of sub‐sensory sacral (optimised) neuromodulation in adults with faecal incontinence: study protocol for a randomised controlled trial. Trials 2018;19:336. [DOI] [PMC free article] [PubMed] [Google Scholar]


