Abstract
People living in low‐income multi‐problem households may benefit from participation in a community‐based health promotion program. Yet, low participation rates are often a problem. It is important to assess reasons for (not) participating to better tailor programs to the needs of this particular at‐risk group. Back2Balance is a health promotion program for low‐income multi‐problem households from Apeldoorn, the Netherlands. We performed qualitative interviews among participants (n = 16) and non‐participants (n = 12) of the program and asked them for their reasons for (not) participating in the program. Interview transcripts were thematically analysed using the Framework method. Participants indicated that reasons for participating encompassed intrapersonal motivators (e.g. to become healthier), interpersonal motivators (e.g. participating to get to know new people) and program level motivators (e.g. learning about a healthy lifestyle, and free or very low cost). Participants and non‐participants outlined the importance of intrapersonal barriers (e.g. physical health problems), interpersonal barriers (e.g. family circumstances) and program level barriers (e.g. logistic issues, and not understanding or knowing about some part of the program). Concluding, combining health promotion with social interaction motivated participants to participate in the Back2Balance program. Yet, both participants and non‐participants experienced many barriers for participation, some of which were related to their multi‐problem situation.
Keywords: barriers, health behaviour, multi‐problem households, Netherlands, participation, social class, social network
What is known about this topic?
People living in low‐income multi‐problem households often have a less healthy lifestyle and less social contacts than the general population.
Few studies examined motivators and barriers for participation in community‐based health promotion programs among people living in multi‐problem households.
Most studies focused on barriers for participation and did not examine motivators or facilitating factors.
What this paper adds?
Combining health promotion with social interaction motivated participants to participate in our community‐based health promotion program for people living in low‐income multi‐problem households.
Participants and non‐participants experienced many barriers for participation, such as physical health problems, family circumstances, logistic issues, not understanding or knowing about the program, and too little structure in activities.
1. INTRODUCTION
People living in low‐income multi‐problem households do not only have financial and psychosocial problems for which they need professional social care but they also often have a less healthy lifestyle and less social contacts than the general population with, for example, lower levels of physical activity, less healthy nutrition and more loneliness (Nagelhout, Abidi, & De Vries, 2019). It is often difficult for people to start and keep living more healthily on their own, especially for people from vulnerable groups such as people with a low socioeconomic position (Fitzgerald & Spaccarotella, 2009) and people living in multi‐problem households (Nagelhout, Hogeling, Spruijt, Postma, & De Vries, 2017). They may benefit from participation in a community‐based health promotion program that targets physical activity, a healthy dietary intake and increased social contacts. However, low participation rates are an important problem that preclude health promotion programs from having a large impact. It is important to assess reasons for (not) participating in a community‐based health promotion program of people living in low‐income multi‐problem households in order to better tailor programs to the needs of this particular at‐risk group.
Reasons for not participating are often considered barriers and reasons for participating are often considered motivators. Previous studies have mostly focused on barriers for participating in health promotion or parenting programs and not many studies examined motivators. The studies that did examine motivators found the following often mentioned motivators: participating with others, fun activities, social interaction, receiving reminders, health reasons, being motivated, no costs and nice staff (Garcia‐Huidobro et al., 2016; Garmendia et al., 2013; Grow et al., 2013; Kelleher et al., 2017; Smith, Straker, McManus, & Fenner, 2014). Often mentioned barriers are: too little time, no transport, timing of the program, location, family emergencies, stigma, costs, privacy, physical or mental health problems and little motivation (Bolton et al., 2016; Burton, Turrell, & Oldenburg, 2003; Campbell‐Voytal et al., 2017; Chinn, White, Harland, Drinkwater, & Raybould, 1999; Curran, Drust, Murphy, Pringle, & Richardson, 2016; Garcia‐Huidobro et al., 2016; Garmendia et al., 2013; Gatewood et al., 2008; Grow et al., 2013; Heinrichs, Bertram, Kuschel, & Hahlweg, 2005; Kelleher et al., 2017; Smith et al., 2014). However, few of these studies examined motivators and barriers for participation specifically for community‐based health promotion programs among vulnerable groups such as people with a low socioeconomic position or people living in multi‐problem households. It is possible that their vulnerable situation has an impact on which motivators and barriers are important for them.
The primary aim of the current study was to investigate reasons for (not) participating in the Back2Balance program for low‐income multi‐problem households. A secondary aim was to examine whether these reasons differed among people with different educational levels, ages, gender, overweight versus healthy weight, and the extent to which they participated in the program. When developing the Back2Balance health promotion program, we tried to incorporate elements to make it attractive for the target group to participate and to take away possible barriers for participation (Abidi, Nagelhout, Spruijt, Schutte, & De Vries, 2018). The program was developed in co‐creation with the target group and with involvement of social workers and an expert panel. We used a participatory action research approach (Reason & Bradbury, 2001) in which we assessed reasons for (not) participating in the program early on and changed our program accordingly where needed. Reasons for (not) participating can be found on multiple levels. Ecological models situate factors at the intrapersonal, interpersonal, community/institution and macro/public policy level (Fitzgerald & Spaccarotella, 2009; McLeroy, Bibeau, Steckler, & Glanz, 1988). Knowledge of these reasons on multiple levels can be used to improve health promotion programs and thereby increase participation rates for this particular at‐risk group characterised by a low‐income and multiple life problems. Additionally, knowing which barriers and motivators are relevant for which subgroups can help increase participation for subgroups with lower participation rates.
2. METHODS
2.1. The Back2Balance program
Back2Balance is a health promotion program targeting healthy nutrition, physical activity and social network enhancement for low‐income multi‐problem households from a municipality in the Netherlands (Abidi et al., 2018). It consisted of walking groups, cooking workshops, children's activities, family trips, discounts on existing lifestyle programs, and motivational talks about health behaviour change, social network enhancement, and stress relieve. A quasi‐experimental study was performed to examine the effectiveness of the program, which consisted of a baseline survey and two follow‐up surveys among an intervention and a control group (Abidi et al., 2018). People who participated in the intervention group of this quasi‐experimental study were offered the opportunity to participate in the program for 6 months, but participation was not obligatory. They could take part in all components of the program or chose only one or a few components, making program participation very flexible. In total, 60 people from low‐income multi‐problem households were offered participation in the Back2Balance program and 35 (58%) participated in one or more components of the program. The current paper reports on the results of qualitative interviews performed with a selection of respondents from the intervention group and on their results on the baseline survey.
2.2. Participants
We conducted semi‐structured qualitative interviews with 28 people aged 12–64 years living in low‐income multi‐problem households in the municipality Apeldoorn in the Netherlands. These people were all offered participation in the community‐based health promotion program Back2Balance; 16 of them had already participated in the Back2balance program and 12 had not (yet) participated. Three of the 12 non‐participants started participation in the Back2Balance program sometime after the interview. For the purpose of this study, ‘participation’ is defined as taking part in one or more of the activities of the Back2Balance program. The interviews were conducted between 1 and 6 months after the baseline survey and the offer of participation in Back2Balance (on average 78 days after the baseline survey, SD = 39).
Inclusion criteria were: a disposable household income up to 150% of the minimum wage; problems in more than one of the following areas on which social workers in Apeldoorn work (finances, social networking and social participation, mental health, physical health, addiction, domestic relations, daycare, school, work, housing or delinquent behaviour); 12 years of age or older; and residing in Apeldoorn or in the surrounding villages (Abidi et al., 2018).
2.3. Data collection
Short interviews were administered by telephone or face‐to‐face at respondents' homes by the second author, who is trained in qualitative interviewing, and a research assistant, who was trained by the second author. The interviews lasted on average 10 min (ranging between 4 and 25 min). The shortest interviews were with younger children and with non‐participants, who often mentioned only one reason for (not) participating. Respondents were reimbursed for participation in the quasi‐experimental study but did not receive an extra reimbursement for participation in the interview. Interviews were performed between January and November 2018.
The interviewer asked why the respondent had (not) participated in Back2Balance. We did not use a predefined list of possible reasons so respondents would be encouraged to mention their own reasons. Besides asking for the ‘why’ of (non‐)participation, the interviewer asked ‘whether there were things that made that they did (not) participate in (certain components of) the program’ and ‘whether there would be things that would have made it easier to participate’. This probed respondents to not only mention rationalisations but also mention circumstances and preconditions. The interviewer asked respondents who participated in the program about what went well during the activities of the program and what went less well. Finally, all respondents were asked for tips or areas of improvement for the Back2Balance program.
As part of the quasi‐experimental study, respondents filled in a survey at baseline with questions about sociodemographic characteristics, health and health behaviours, and social network questions. Sociodemographic characteristics that were measured were: gender, age, children in their household (yes or no), educational level (low, moderate or high) and paid employment (yes or no). Educational level was categorised as low (primary education or lower pre‐vocational secondary education), moderate (middle pre‐vocational and secondary vocational education) and high (senior general secondary education, higher professional education and university). Self‐perceived health was measured with one question: ‘How is your health condition generally?’ (5‐point response scale from ‘very bad’ to ‘very good’) (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006; RIVM, 2017a). Smiley faces were added above the scale to facilitate interpretation. Mental health was measured using the five‐item Mental Health Inventory in which three questions assess depressive symptoms and psychological well‐being, and two questions measure symptoms of anxiety (Cuijpers, Smits, Donker, Ten Have, & de Graaf, 2009). The Body Mass Index (BMI) was calculated after asking respondents their height and weight. Social contacts were measured with a three‐item index from the Dutch Public Health Monitor (RIVM, 2017b) and loneliness was measured with a six‐item validated scale for overall, emotional and social loneliness (De Jong Gierveld & Van Tilburg, 2006). Respondents aged 12–15 years old answered a shortened version of the questionnaire and therefore not all questions were answered by all interviewed respondents.
2.4. Analysis
The interviews were audio recorded and transcribed verbatim. Analyses were performed manually using Microsoft Excel. After conducting 15 interviews, a first analysis was performed by a research assistant with the aim of finding urgent things that needed to be changed to the program early on. Based on this analysis, we simplified the ‘discount’ component of the program (participants could get discounts on existing lifestyle programs), because the analysis showed that many participants did not understand this component of the program. No other changes were made to the program based on this first analysis of the interviews, although changes were made (e.g. doing activities from another location, at other times of the day, and creating more structure in the activities) based on conversations by the program staff member with participants and non‐participants.
We performed thematic analyses using the Framework method (Ritchie & Spencer, 1994). The first author read through the first 23 transcripts and made notes about recurring themes. Based on these notes, a list of codes was made that was shared with the second author. Codes were subdivided between motivators and barriers for participation the Back2Balance program. In line with ecological models, we further subdivided codes into intrapersonal, interpersonal and program level (ecological models also make the distinction between community/institution and macro/public policy level, but this was not supported by our data). The first and second author independently coded all transcripts and added some new codes that emerged from the data. Disagreements between coders were discussed until consensus was reached.
A matrix was made with all respondents and all codes to facilitate comparisons between codes within participants and comparisons between participants within codes. Only codes that were mentioned by at least three respondents were further analysed and reported in the paper, the other codes are reported in Table S1. This was done to keep the paper concise and the reported reasons for (not) participating relevant, as reasons that were reported by only one or two respondents may have been very specific to those respondents. Differences in answering patterns between respondents with certain characteristics (educational level, age, gender, overweight versus healthy weight, and the extent to which they participated in the program) were explored. We mention these subgroup differences in the results section only where we found differences.
Saturation was reached for the motivators after 16 interviews and for the barriers after 23 interviews (see Figure 1). We kept interviewing until we had 28 respondents to ensure enough variation in age distribution and because we wanted to interview respondents who participated at the start of the Back2Balance program and respondents who participated when the Back2Balance program was already running for several months.
Figure 1.
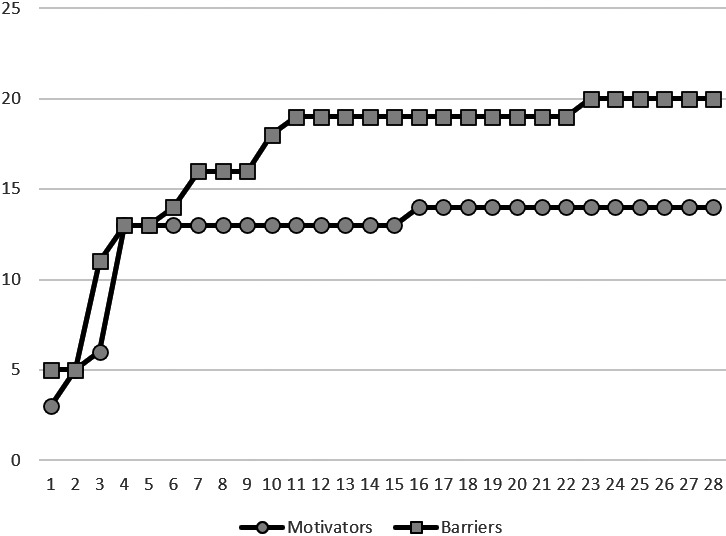
Total number of motivators and barriers (y axis) mentioned during the 28 interviews (x axis)
2.5. Ethical approval and trial registration
The study protocol was approved by the Medical Ethics Committee of Zuyderland and Zuyd Hogeschool (METC number: 17‐N‐80) and the study was registered at the Dutch Trial Register (NTR6512). Respondents signed an informed consent form before taking part in the study. Additionally, oral informed consent was given for participation in the interview.
3. FINDINGS
3.1. Sample characteristics
Sample characteristics are shown in Table 1. We interviewed 12 men and 16 women, with a mean age of 45.7 years (SD = 15.7). More than half lived with children in their household. Most respondents were low educated and did not have paid employment. Compared to interviewed non‐participants, interviewed participants had significantly fewer social contacts at baseline (t = 2.22, df = 24, p = .036).
Table 1.
Sample characteristics from participants and non‐participants
| Participants (n = 16) | Non‐participants (n = 12) | |
|---|---|---|
| Gender | ||
| Male (n, %) | 6 (37.5) | 6 (50.0) |
| Female (n, %) | 10 (62.5) | 6 (50.0) |
| Age | ||
| Mean (SD) | 45.4 (15.4) | 46.0 (16.8) |
| Children in household | ||
| Yes (n, %) | 11 (68.8) | 6 (50.0) |
| No (n, %) | 5 (31.3) | 6 (50.0) |
| Educational level | ||
| Low (n, %) | 7 (46.7) | 5 (45.5) |
| Moderate (n, %) | 5 (33.3) | 5 (45.5) |
| High (n, %) | 3 (20.0) | 1 (9.1) |
| Paid employment | ||
| Yes (n, %) | 2 (15.4) | 2 (20.0) |
| No (n, %) | 11 (84.6) | 8 (80.0) |
| Self‐perceived health (1–5) a | ||
| Mean (SD) | 2.9 (0.7) | 3.2 (0.9) |
| BMI | ||
| Mean (SD) | 30.5 (8.1) | 26.3 (5.1) |
| Mental health (0–100) a | ||
| Mean (SD) | 58.4 (21.1) | 72.7 (20.2) |
| Social contacts (1–5) a | ||
| Mean (SD) | 3.8 (1.4) | 5.0 (1.3) |
| Loneliness (1–5) a | ||
| Mean (SD) | 2.4 (1.1) | 2.6 (0.9) |
Higher scores means better self‐perceived health, better mental health, more social contacts and more loneliness.
3.2. Motivators
Aspects that motivated people to participate in the Back2Balance program were mentioned only by participants and not by non‐participants. A larger number of motivators was mentioned by participants who participated more often in the program than by participants who participated less often in the program. Motivators could be categorised into intrapersonal motivators, interpersonal motivators and program level motivators that motivated participation (Table 2).
Table 2.
Summary of main results
| Motivators | Barriers | |
|---|---|---|
| Intrapersonal level |
|
|
| Interpersonal level |
|
|
| Program level |
|
|
3.2.1. Intrapersonal motivators
An often mentioned intrapersonal motivator was participating to become healthier (11/16). Respondents mentioned for example that the program fitted with their goal to lose weight, to reduce blood pressure or simply to become healthier. This motivator was more often mentioned by respondents who were overweight than respondents with a healthy weight. I read the folder and think that you should, despite all the problems that you have, should still watch your health. That's why it appealed to me (respondent #22, woman, 40 years).
Another mentioned intrapersonal motivator was to have something to do (3/16). This was only mentioned by lower educated respondents, women and participants who participated eight times or more often in the program. Also because, like I said: to get out of the house. Because you tend to stay inside all too often (respondent #4, woman, 48 years).
Finally, an intrapersonal motivator was doing it for the children (3/16), which was only mentioned by women. I found it very nice for the children because they could participate in the activities (respondent #27, woman, 41 years).
3.2.2. Interpersonal motivators
Many respondents who participated in Back2Balance mentioned that they participated because it was a social program in which they got to know new people (12/16). And also to get some new social contacts.. so that was important for me too (respondent #3, woman, 45 years). This was more often mentioned by participants who participated more often in the program than by participants who participated less often in the program.
Of the people who mentioned this interpersonal motivator, some also mentioned that they liked that they could come together with someone else (e.g. their children) (4/16) and that it was pleasant that it was with people who were in the same multi‐problem situation as they were (3/16). Because my mother also participated ánd to make new contacts (respondent #23, man, 16 years). The nice thing is indeed to get to know people who are perhaps not entirely in the same situation but do have similar, who are participating in the program for the same reasons. It creates a bond (respondent #16, woman, 30 years).
Interpersonal motivators were more often mentioned by women than men.
3.2.3. Program level motivators
A program characteristic that respondents who participated in the program liked and motivated them to come was that they could learn about a healthy lifestyle at Back2Balance, for example, learn new recipes (7/16). Some respondents also mentioned learning things about a healthy lifestyle from other participants. Well, I just wanted to get to know people, but also other people's ideas about food. Because food can also get monotonous. You actually always make the same things (respondent #1, man, 59 years). This motivator was more often mentioned by participants who participated more often in the program than by participants who participated less often in the program.
The fact that activities in the program were free or very low cost was important to people (5/16). The fact that it is cheap and accessible. Because you then have a free social outing, so to speak (respondent #2, woman, 59 years).
The open and flexible character of the program was also mentioned as a motivator (4/16). People liked that they could decide together with the program staff member what activities they would do and would sometimes even decide the time and place together.
A final program level motivator was the program staff member whom participants thought was very nice and who stimulated them to come to activities (4/16). She motivates people and I really have the feeling that she is interested and, yes she also asks about things and so tries to understand us and she takes it into account (respondent #11, woman, 50 years). This motivator was only mentioned by women and not by men.
3.3. Barriers
Barriers were mentioned as often by participants as non‐participants of the Back2Balance program. Barriers could be categorised into intrapersonal barriers, interpersonal barriers and program level barriers that were barriers to participation (Table 2).
3.3.1. Intrapersonal barriers
Physical health problems were often mentioned as barrier to participate in the program (11/28), mostly by older respondents. I could go with the walking group, but with me they would not get to their destination until next year and my husband has COPD and always gets wheezy, that will not work (respondent #17, woman, 62 years).
Another intrapersonal barrier (mostly mentioned by different people than the ones who mention physical health problems) is a lack of time to participate in the activities (10/28), due to work or other appointments. Because a lot of the activities are on the Thursday or Friday. I just cannot come then because I have a volunteer job (respondent #7, woman, 54 years).
Finally, some people already participated in similar group activities (such as cooking and walking together) from another program of the municipality or from their school (6/28). This made participation in Back2Balance less attractive and not needed for these people.
3.3.2. Interpersonal barriers
Family circumstances were a common interpersonal barrier to participate in the program (6/28). Well, I'm a single mum of two children and my youngest has an intellectual disability so really has to eat at fixed times and too many stimulants are not good for him (respondent #26, woman, 39 years).
An interpersonal barrier that was only mentioned by some non‐participants was that they could not handle or did not want to be in groups of people (3/28). Because I cannot handle large groups of people. Then I get a little panicky and I start to shake, then I need to get out (respondent #9, man, 61 years).
3.3.3. Program level barriers
The two program characteristics that were most often mentioned as barriers to participation were logistic issues (e.g. a location that was too far, lack of transportation, and a time that they could not come) (8/28) and not understanding or not knowing about a certain component of the program (8/28). Both problems were handled by making changes to the program as soon as these barriers came to light. After making these changes, these barriers were less often mentioned. Not understanding or not knowing about a certain component of the program was most often mentioned by lower educated respondents and by some of the moderate educated respondents, but not by higher educated respondents. Well uh because I don't know what is going on, I did not get any message about this. I only filled in the surveys (respondent #8, man, 62 years).
In the winter period, respondents mentioned that they did not like the walking groups because of bad weather and darkness in the evenings (5/28). Seven at night… That's no time for a walk in winter (respondent #1, man, 59 years).
Some people also mentioned that they did not like the activities at all (5/28) and that they would rather do something different, such as a creative activity. Based on comments by participants and non‐participants to the program staff member, a creative activity was organised, but this was done only once, and the focus of the program stayed on healthy and social activities. She talked about walking groups and cooking workshops and it didn't seem too much fun to me (respondent #27, woman, 41 years).
Finally, some of the first participants in the program (3/28) mentioned that the activities were too chaotic and unstructured for them. This was only mentioned by low educated respondents. After remarks about this, the program staff member ensured that activities were more structured. The first time we went to an Escape Room and that is a lot of fun, but if you are a little bit chaotic then it is hard. And the second time we went to a Christmas market, but the whole afternoon was just very messy. And for me it then is not structured enough and that makes it very hard for me (respondent #3, woman, 45 years).
4. DISCUSSION
The aim of our study was to identify reasons for (not) participating in the Back2Balance community‐based health promotion program for low‐income multi‐problem households. Reasons for participating encompassed intrapersonal motivators: people wanted to become healthier, to have something else on their mind, and were sometimes participating for their children. Interpersonal motivators were also mentioned: people participated to get to know new people, they appreciated that they could come together with someone they already knew, and that other participants were in the same multi‐problem situation. Program level motivators were: learning about a healthy lifestyle, free or very low cost, the open and flexible character of the program, and that the program staff member was very nice and stimulating. Participants and non‐participants outlined the importance of intrapersonal barriers: they had physical health problems, a lack of time, or were already participating in similar activities. Interpersonal barriers were, for example, family circumstances and not able or wanting to be in groups of people. Certain program level characteristics were also mentioned as barriers: logistic issues (e.g. a location that was too far, lack of transportation, and a time that they could not come), not understanding or knowing about the program, outside activities in bad weather and dark winter evenings, not liking the activities, and too little structure. In short, combining health promotion with social interaction motivated participants to participate in the Back2Balance program, which was also found in previous studies (Garcia‐Huidobro et al., 2016; Garmendia et al., 2013; Grow et al., 2013; Kelleher et al., 2017; Smith et al., 2014). Both participants and non‐participants experienced many barriers for participation, some of which were related to their multi‐problem situation.
Some of the reasons for not participating in the program pointed to the fact that the program or some elements of it were unclear, too complex or not structured enough. These reasons were mainly mentioned by low educated respondents. Simplifying the information and better structuring the activities worked, as demonstrated by a reduction in respondents mentioning these reasons over time. Therefore, an important recommendation for similar programs with a low socioeconomic target group is to provide highly structured activities and make the program elements very easy to understand. This will also accommodate participants with low literacy, a mild intellectual disability, or, for example, autism spectrum disorder.
Our findings are in line with other studies that found similar motivators and barriers (Bolton et al., 2016; Burton et al., 2003; Campbell‐Voytal et al., 2017; Chinn et al., 1999; Curran et al., 2016; Garcia‐Huidobro et al., 2016; Garmendia et al., 2013; Gatewood et al., 2008; Grow et al., 2013; Heinrichs et al., 2005; Kelleher et al., 2017; Smith et al., 2014). Motivators and barriers that we found and were not mentioned in previous studies were: to have something else on their minds, other participants who are in the same multi‐problem situation, not able or wanting to be in groups of people, not understanding or knowing about the program, and too little structure. These motivators and barriers may be specific to the needs of our particular at‐risk group and should be taken into account when running a program for low‐income multi‐problem households.
Our findings also suggest that low‐income multi‐problem households are a heterogenous group with different backgrounds, different (mental) problems, barriers and needs. Health promotion programs could take this diversity into account by tailoring the program to the specific needs of individuals or families. This requires program staff with relatively much time for the program and well‐developed social skills, and also a program with more choice in activities. Such a tailored program is more expensive but could potentially tackle many of the barriers for participation that were mentioned by the participants and non‐participants of our program.
Strengths of our study are that we examined both motivators and barriers and that we interviewed both participants and non‐participants. Our study group was relatively large for a qualitative study, we ensured enough variation in gender and age distribution of respondents, and we interviewed both respondents who participated at the start of the program and respondents who participated when the program was already running for several months. A limitation is that the interviews were very short, simply asking respondents why they did or did not participate in the program. Although some follow‐up questions were asked about whether there would be things that would have made it easier to participate, what went well and what went less well, and what would be tips or areas of improvement for the program, respondents could answer the questions on a shallow level without revealing underlying reasons. For example, many respondents mentioned a lack of time as reason, but were not prompted to explain why they prioritised other things over the program. Additionally, recall bias may have played a role when asking non‐participants about their reasons for non‐participating 1–6 months after being invited. Finally, we cannot be sure that our results are generalisable to low‐income multi‐problem households living in other cities in the Netherlands or living in other countries.
Concluding, our study revealed several motivators and barriers for participating in the Back2Balance community‐based health promotion program for low‐income multi‐problem households. Based on these motivators and barriers, we deduce that health promotion programs for this group should be social, together with others who are in a similar multi‐problem situation, with program staff who show a genuine interest in the participants, with free or very low cost activities, flexible, accessible, and very easy to understand. Due to the multitude and complexity of the problems they encounter, health promotion programs may also have to be more tailored to the specific needs of individuals or families.
CONFLICTS OF INTEREST
None.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
We are grateful to all participants who have participated in the interviews and the social workers who helped with participant recruitment. We thank Ninouk Kaptein and Joerie van der Wel for transcribing the interviews and Lieke Goijaarts for performing and transcribing some of the interviews. Several employees of Stimenz Apeldoorn, the municipality Apeldoorn and the social neighbourhood team Apeldoorn have helped with the development and execution of the Back2Balance program which we gratefully acknowledge. In particular, we thank Renate Spruijt, Tamar Jansen and Natalie Spaans for the development and execution of the program. We thank Tamar Jansen also for checking our manuscript. We also thank the advisory committee (Janneke Harting, Silvia Evers, Carry Renders, Patricia van Assema, Marjolijn van Leeuwen, Monique L'hoir, Annet Roose, Sharida Imamdi and Judith Neter) of Back2Balance for their guidance.
Nagelhout GE, Abidi L, de Vries H. Reasons for (not) participating in a community-based health promotion program for low-income multi-problem households in the Netherlands: A qualitative study. Health Soc Care Community. 2021;29:241–249. 10.1111/hsc.13087
Funding information
This study was supported by a grant from Fonds NutsOhra (#101.230).
REFERENCES
- Abidi, L. , Nagelhout, G. E. , Spruijt, R. , Schutte, H. , & De Vries, H. (2018). Quasi‐experimental study evaluating a health promotion program targeting health nutrition, physical activity and social network enhancement for low‐income multi‐problem households: Study protocol. International Journal of Clinical Trials, 5, 132–141. [Google Scholar]
- Bolton, K. A. , Kremer, P. , Gibbs, L. , Swinburn, B. , Waters, E. , & de Silva, A. (2016). Expanding a successful community‐based obesity prevention approach into new communities: Challenges and achievements. Obesity Research & Clinical Practice, 10(2), 197–206. 10.1016/j.orcp.2015.05.017 [DOI] [PubMed] [Google Scholar]
- Burton, N. W. , Turrell, G. , & Oldenburg, B. (2003). Participation in recreational physical activity: Why do socioeconomic groups differ? Health Education & Behavior, 30(2), 225–244. 10.1177/1090198102251036 [DOI] [PubMed] [Google Scholar]
- Campbell‐Voytal, K. , Hartlieb, K. B. , Cunningham, P. B. , Jacques‐Tiura, A. J. , Ellis, D. A. , Jen, K. L. , & Naar, S. (2017). Evaluation of an evidence‐based weight loss trial for urban African American adolescents and caregivers. Journal of Nutrition & Health (Northborough), 3(2), 6. [PMC free article] [PubMed] [Google Scholar]
- Chinn, D. J. , White, M. , Harland, J. , Drinkwater, C. , & Raybould, S. (1999). Barriers to physical activity and socioeconomic position: Implications for health promotion. Journal of Epidemiology and Community Health, 53(3), 191 10.1136/jech.53.3.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P. , Smits, N. , Donker, T. , Ten Have, M. , & de Graaf, R. (2009). Screening for mood and anxiety disorders with the five‐item, the three‐item, and the two‐item Mental Health Inventory. Psychiatry Research, 168(3), 250–255. 10.1016/j.psychres.2008.05.012 [DOI] [PubMed] [Google Scholar]
- Curran, K. , Drust, B. , Murphy, R. , Pringle, A. , & Richardson, D. (2016). The challenge and impact of engaging hard‐to‐reach populations in regular physical activity and health behaviours: An examination of an English Premier League ‘Football in the Community’men's health programme. Public Health, 135, 14–22. 10.1016/j.puhe.2016.02.008 [DOI] [PubMed] [Google Scholar]
- De Jong Gierveld, G. J., & Van Tilburg, T. (2006). A 6‐item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28(5), 582–598. 10.1177/0164027506289723 [DOI] [Google Scholar]
- DeSalvo, K. B. , Bloser, N. , Reynolds, K. , He, J. , & Muntner, P. (2006). Mortality prediction with a single general self‐rated health question. Journal of General Internal Medicine, 21(3), 267–275. 10.1111/j.1525-1497.2005.00291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald, N. , & Spaccarotella, K. (2009). Barriers to a healthy lifestyle: From individuals to public policy—an ecological perspective. Journal of Extension, 47(1), 1–8. [Google Scholar]
- Garcia‐Huidobro, D. , Allen, M. , Rosas‐Lee, M. , Maldonado, F. , Gutierrez, L. , Svetaz, M. V. , & Wieling, E. (2016). Understanding attendance in a community‐based parenting intervention for immigrant Latino families. Health Promotion Practice, 17(1), 57–69. 10.1177/1524839915582155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmendia, M. L. , Dangour, A. D. , Albala, C. , Eguiguren, P. , Allen, E. , & Uauy, R. (2013). Adherence to a physical activity intervention among older adults in a post‐transitional middle income country: A quantitative and qualitative analysis. The Journal of Nutrition, Health & Aging, 17(5), 466–471. 10.1007/s12603-012-0417-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatewood, J. G. , Litchfield, R. E. , Ryan, S. J. , Geadelmann, J. D. M. , Pendergast, J. F. , & Ullom, K. K. (2008). Perceived barriers to community‐based health promotion program participation. American Journal of Health Behavior, 32(3), 260–271. 10.5993/AJHB.32.3.4 [DOI] [PubMed] [Google Scholar]
- Grow, H. M. G. , Hsu, C. , Liu, L. L. , Briner, L. , Jessen‐Fiddick, T. , Lozano, P. , & Saelens, B. E. (2013). Understanding family motivations and barriers to participation in community‐based programs for overweight youth: One program model does not fit all. Journal of Public Health Management and Practice, 19(4), E1–E10. 10.1097/PHH.0b013e31825ceaf9 [DOI] [PubMed] [Google Scholar]
- Heinrichs, N. , Bertram, H. , Kuschel, A. , & Hahlweg, K. (2005). Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: Barriers to research and program participation. Prevention Science, 6(4), 275–286. 10.1007/s11121-005-0006-1 [DOI] [PubMed] [Google Scholar]
- Kelleher, E. , Davoren, M. P. , Harrington, J. M. , Shiely, F. , Perry, I. J. , & McHugh, S. M. (2017). Barriers and facilitators to initial and continued attendance at community‐based lifestyle programmes among families of overweight and obese children: A systematic review. Obesity Reviews, 18(2), 183–194. 10.1111/obr.12478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy, K. R. , Bibeau, D. , Steckler, A. , & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. [DOI] [PubMed] [Google Scholar]
- Nagelhout, G. E. , Abidi, L. , & De Vries, H. (2019). How do health and social networks compare between low‐income multi‐problem households and the general population? International Journal of Environmental Research and Public Health, 16, 4967 10.3390/ijerph16244967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagelhout, G. E. , Hogeling, L. , Spruijt, R. , Postma, N. , & De Vries, H. (2017). Barriers and facilitators for health behavior change among adults from multi‐problem households: A qualitative study. International Journal of Environmental Research and Public Health, 14, 1229 10.3390/ijerph14101229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reason, P. , & Bradbury, H. (2001). Handbook of action research: Participative inquiry and practice. London: Sage Publications. [Google Scholar]
- Ritchie, J. , & Spencer, L. (1994). Qualitative data analysis for applied policy research In Bryman A., & Burgess R. G. (Eds.), Analyzing qualitative data (pp. 173–194). London, UK: Routledge. [Google Scholar]
- RIVM (2017a). Ervaren gezondheid. Retrieved from http://www.toolkitvtv.nl/inhoud/indicatoren‐en‐bronnen/gezondheidstoestand/ervaren‐gezondheid/ [Google Scholar]
- RIVM . (2017b). Indicatoren voor de Monitor Volksgezondheid. Retrieved from https://www.monitorgezondheid.nl/volksindicatoren.aspx
- Smith, K. L. , Straker, L. M. , McManus, A. , & Fenner, A. A. (2014). Barriers and enablers for participation in healthy lifestyle programs by adolescents who are overweight: A qualitative study of the opinions of adolescents, their parents and community stakeholders. BMC Pediatrics, 14(1), 53 10.1186/1471-2431-14-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


