Abstract
Background
The Risk Assessment Prediction Tool (RAPT) is a validated 6-question survey designed to predict primary total joint arthroplasty (TJA) patients’ discharge disposition. It is scored from 1 to 12 with patients stratified into high-, intermediate-, and low-risk groups. Given recent advancements in rapid-discharge protocols and increasing utilization of home services, the RAPT score may require modified scoring cutoffs.
Methods
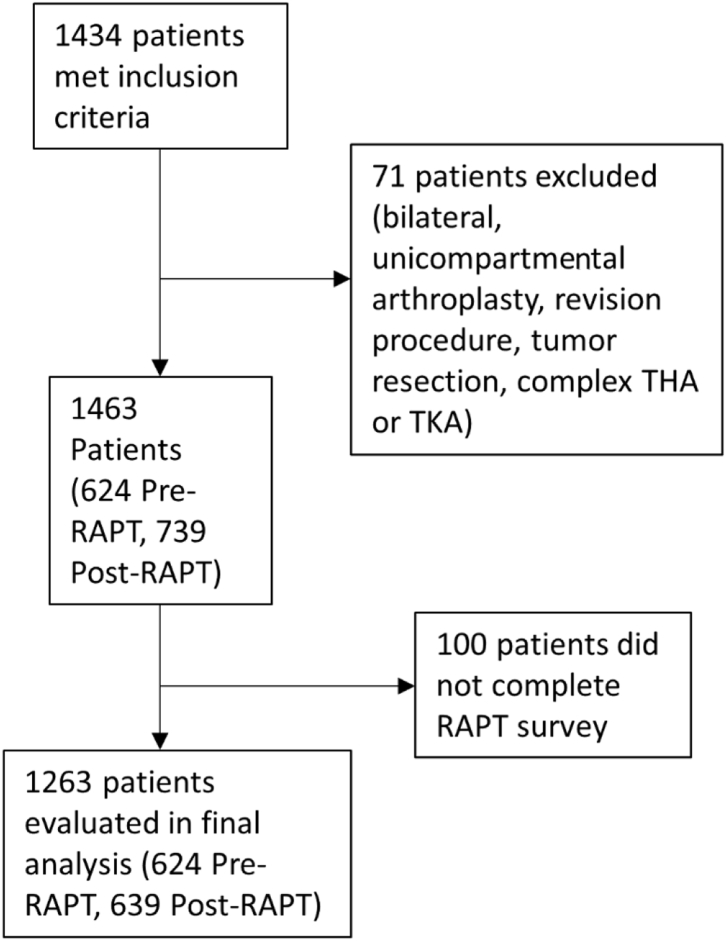
A retrospective chart review of all patients undergoing primary TJA at a single academic center over 14 months was performed. The RAPT score was implemented during the sixth month. Patients undergoing revision TJA, complex TJA, and TJA after resection of malignancy were excluded. Outcomes before and after RAPT implementation were analyzed with additional subanalysis investigating of post-RAPT data.
Results
A total of 1264 patients (624 Pre-RAPT and 640 Post-RAPT) were evaluated. The post-RAPT group (245 total hip arthroplasty and 395 total knee arthroplasty) experienced significant decreases in mean hospital length of stay (2.22 days pre-RAPT to 1.82 days post-RAPT, P < .001) and the proportion of patients discharged to facility (21.8% pre-RAPT to 15.2% post-RAPT, P = .002). The modified system demonstrated the highest overall predictive accuracy at 92% and was found to be predictive of hospital length of stay.
Conclusion
Owing to the recent trends favoring in-home services over rehab facility after discharge, previously published RAPT scoring cutoffs are inaccurate for modern practice. Using mRAPT cutoffs maximizes the number of patients for whom a discharge prediction can be made, while maintaining excellent predictive accuracy.
Keywords: Arthroplasty, RAPT, Length of stay, Discharge
Introduction
As the number of annual total joint arthroplasty (TJA) procedures continues to rise, so does health-care expenditures on arthroplasty services annually [[1], [2], [3]]. As a result, modern arthroplasty care has focused on controlling costs, improving outcomes, and optimizing the value of care [4]. The development of modern TJA care pathways has resulted in a fundamental shift from prolonged hospital length of stay and discharge to skilled nursing facilities to generally shorter length of stays and discharge home [[5], [6], [7], [8]]. These patient-centered, cost-conscious practices reflect most patients’ preferences. Furthermore, discharge home after surgery has been associated with decreased costs, decreased readmission rates, and more favorable outcomes than discharge to postacute care facilities [[1], [2], [3],9,10].
The ability to accurately predict a TJA patient’s discharge disposition has become imperative for a successful modern rapid recovery total joint pathway. One tool that has been successfully implemented in this endeavor has been the Risk Assessment Prediction Tool (RAPT). The RAPT score was originally validated in Australia by Oldmeadow et al. [11] and was primarily used to predict the need for inpatient rehabilitation after joint arthroplasty. The RAPT score was subsequently validated in the United States by Hansen et al. in 2015 [12] and score modified to reflect their institutional discharge practices. It was once again modified in 2019 by Dibra et al. [1] with significant improvement from prior iterations. The RAPT questionnaire is comprised of 6 questions worth a total of 12 points. It is meant to stratify patients into high-, intermediate-, and low-risk categories to predict whether they will be discharged home or require postacute rehabilitation services. The optimal scoring range for each category continues to be a topic of debate [11,12].
Despite RAPT’s high performance when predicting discharge outcomes for low- and high-risk patients, it has historically not demonstrated the same efficacy with the intermediate-risk groups. Hansen et al. [12] found that 42% of patients were at intermediate risk with a predictive accuracy for discharge disposition of 65.2%, leaving much room for improvement for this tool to be effectively used. Furthermore, the RAPT scoring system was originally developed in 2003 with an average length of stay of over 9 days. The RAPT score was also used by Hansen et al. [12] with approximately 45% of arthroplasty patients requiring discharge to some type of extended care facility. These 2 prior studies are not applicable to most modern enhanced recovery total joint pathways, but more recent investigations suggest that RAPT implementation may be improved with modified scoring criteria [1]. While RAPT scoring has demonstrated the ability to predict discharge disposition for modern day arthroplasty discharge practices in the United States, it still requires further validation in various regions across the country with further investigations aimed at optimizing its predictive ability [1,13].
This study focuses on 3 questions: (1) Does the RAPT score accurately predict discharge disposition in a modern arthroplasty practice at a single academic center in the northeastern United States? (2) Is the utilization of the RAPT score associated with safely decreasing the average length of stay in a modern arthroplasty practice? (3) Can modifications to the RAPT score improve its overall predictive performance?
Materials and methods
After obtaining institutional review board approval, a retrospective chart review of all patients undergoing primary TJA between August 1, 2017, and September 28, 2018, at a single academic center was performed. Procedures from August 1, 2017, to January 31, 2018, occurred before RAPT implementation, whereas procedures from February 1, 2018, to September 28, 2018, had RAPT scores recorded at preadmission testing appointment approximately 3-4 weeks before surgery. RAPT scoring was carried out by office nursing staff, and responses were provided by patients. Surgeons were made aware of scores, and results were discussed in terms of impact on discharge disposition. Case management and physical therapy staff were also granted access to these scores to further optimize discharge planning efforts.
All total knee arthroplastys were performed using a medial parapatellar approach. Surgical approaches for total hip arthroplasty varied according to surgeon preference (anterolateral 34.3%, direct anterior 40.4%, posterior 24.5%). Patients undergoing revision TJA, complex TJA, and TJA after resection of malignancy were excluded. In addition to RAPT scores, demographic, medical, surgical, and outcome-related data were collected on all patients. Student’s t test and chi-square analysis were used for comparison of continuous and categorical variables, respectively. Multiple logistic regression evaluated for association between RAPT implementation and the likelihood of discharge home after controlling for potential confounders.
For post-RAPT patients specifically, repeated binary logistic regression modeling was performed to determine the score cutoffs resulting in the highest overall predictive accuracy. The resulting values were termed “modified RAPT” (mRAPT) cutoffs. The “mRAPT” cutoffs were then defined as follows: modified high-risk (mHR) score 1-3, modified intermediate-risk (mIR) 4-7, and modified low-risk (mLR) 8-12. In contrast, the traditional RAPT scoring cutoffs were defined as high risk (HR) 1-5, intermediate risk (IR) 6-9, and low risk (LR) 10-12. Student’s t test and chi-square analysis were used for direct comparison of continuous and categorical variables, respectively. Microsoft Excel version 16.11.1 (Microsoft Corporation, 2017, Redmond, Washington) was used for data collection and visualization. All statistical analyses were performed using Stata 15.0 (StataCorp., 2017, College Station, TX). Statistical significance was defined as P < .05 a priori.
Results
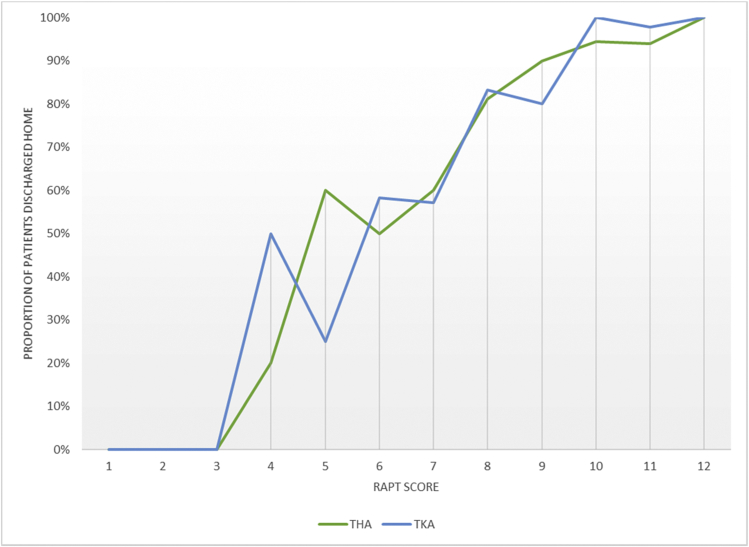
A total of 1264 patients (624 pre-RAPT and 640 post-RAPT) were evaluated (Fig. 1). Higher RAPT scores were associated with increased probability home discharge with no patients scoring RAPT of 3 or less being discharged home than over 80% of patients scoring 8 or higher (Fig. 2). Using the original Oldmeadow et al. [11] scoring system, 45.8% of patients were deemed to be at intermediate risk (IR scored 6-9) for which an accurate discharge disposition prediction was unable to be determined (Table 1). Furthermore, while the predictive accuracy of the LR group was excellent at 96.8%, the predictive accuracy of the HR group was poor at 66.7%. Similarly, the newer Hansen et al. [12] scoring system resulted in 64.8% of patients being deemed IR (score 7-10) with no disposition prediction determined (Table 1). The predictive accuracy among LR groups in this system was again excellent at 97.0%; however, the predictive accuracy for HR groups was even poorer, at 57.6%.
Figure 1.
Flow chart of study sample.
Figure 2.
Proportion of patients discharged to facility, pre-RAPT vs post-RAPT.
Table 1.
Predictive accuracy of various Risk Assessment Prediction tool (RAPT) scoring cutoffs.
| Oldmeadow et al. [11] | Number of patients | Proportion of patients | Proportion discharged home | Predictive accuracy | Mean hospital LOS (d) |
|---|---|---|---|---|---|
| High risk (RAPT score 1-5) | 33 | 5.16% | 33.33% | 66.67% | 2.6 |
| Intermediate risk (RAPT score 6-9) | 293 | 45.78% | 77.82% | – | 2.0 |
| Low risk (RAPT score 10-12) | 314 | 49.06% | 96.82% | 96.82% | 1.6 |
| Hansen et al. [12] | |||||
| High risk (RAPT score 1-6) | 59 | 9.22% | 42.37% | 57.63% | 2.4 |
| Intermediate risk (RAPT score 7-10) | 415 | 64.84% | 86.02% | – | 1.9 |
| Low risk (RAPT score 11-12) | 166 | 49.06% | 96.99% | 96.99% | 1.6 |
| mRAPT | |||||
| High risk (RAPT score 1-3) | 6 | 0.94% | 0.00% | 100.00% | 2.7 |
| Intermediate risk (RAPT score 4-7) | 102 | 15.94% | 52.94% | – | 1.9 |
| Low risk (RAPT score 8-12) | 532 | 83.13% | 91.92% | 91.92% | 1.7 |
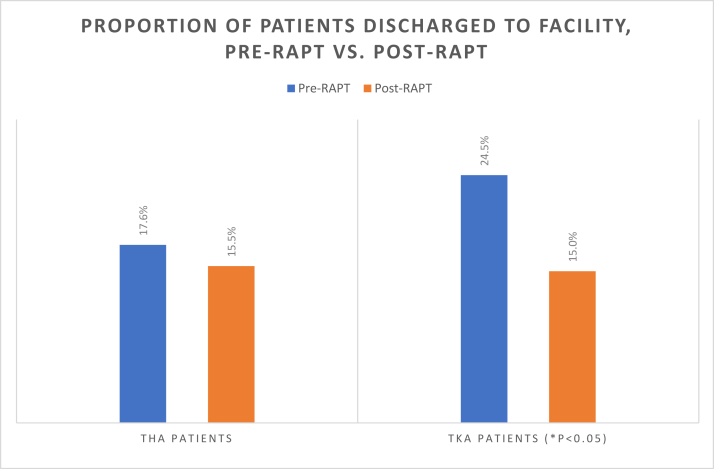
The post-RAPT group had a higher proportion of females (65.9% vs 60%, P = .029); otherwise, there were no significant demographic differences between cohorts (Table 2). The post-RAPT group experiences significant decreases in mean hospital length of stay (2.22 days pre-RAPT to 1.82 days post-RAPT, P < .001) and the proportion of patients discharged to facility (21.8% pre-RAPT to 15.2% post-RAPT, P = .002) (Table 3, Fig. 3). There was no difference in adverse events or unplanned readmission between cohorts (Table 4). After implementation of RAPT, 96.8% of low-risk patients (RAPT scores 10-12) were discharged home, vs 33.3% of high-risk patients (RAPT scores 1-5) (Table 1).
Table 2.
Patient demographics.
| Pre-RAPT | Post-RAPT | P value | |
|---|---|---|---|
| Number of patients | 624 | 639 | – |
| Age, mean ± SD | 66.9 | 66.5 | .546 |
| Gender, n (%) | |||
| Female | 374 (60.0%) | 421 (65.9%) | .029 |
| Male | 250 (40.1%) | 218 (34.1%) | |
| Primary language, n (%) | |||
| English | 592 (94.9%) | 599 (93.9%) | .591 |
| Spanish | 12 (1.9%) | 23 (3.6%) | |
| Portuguese | 11 (1.8%) | 12 (1.9%) | |
| Other | 9 (1.4%) | 4 (0.6%) | |
| Insurance, n (%) | |||
| Medicaid | 52 (8.5%) | 46 (7.2%) | .187 |
| Medicare | 290 (47.2%) | 338 (52.0%) | |
| Private | 268 (43.6%) | 247 (38.7%) | |
| Worker's compensation | 5 (0.8%) | 7 (1.1%) | |
| BMI, n (%) | |||
| Nonobese (<35) | 277 (44.4%) | 268 (42.0%) | .221 |
| Class I obesity (30-34.9) | 175 (28.0%) | 207 (32.4%) | |
| Class II obesity (35-39.9) | 114 (18.3%) | 119 (18.6%) | |
| Class III obesity (≥40) | 58 (9.3%) | 45 (7.0%) | |
| Season of surgery, n (%) | |||
| Fall | 343 (55.0%) | 12 (1.9%) | <.001 |
| Winter | 0 (0.0%) | 228 (35.7%) | |
| Spring | 165 (26.4%) | 228 (35.7%) | |
| Summer | 165 (26.4%) | 291 (45.5%) | |
| Surgical start time, n (%) | |||
| Early (before 10:30 AM) | 350 (56.1%) | 330 (51.6%) | .113 |
| Late (10:30 AM or later) | 274 (43.9%) | 309 (48.4%) |
LOS, length of stay; RAPT, Risk Assessment Prediction tool.
Bold values are significance of P ≤ .05.
Table 3.
Mean hospital length of stay and proportion of patients discharged to facility, pre-RAPT vs post-RAPT.
| Pre-RAPT | Post-RAPT | P value | |
|---|---|---|---|
| Mean hospital LOS (d), mean (SD) | |||
| All patients | 2.22 | 1.82 | <.001 |
| THA patients | 2.24 | 1.81 | <.001 |
| TKA patients | 2.21 | 1.84 | <.001 |
| Proportion discharged to facility, n (%) | |||
| All patients | 136 (21.8%) | 97 (15.2%) | .002 |
| THA patients | 43 (17.6%) | 38 (15.5%) | .543 |
| TKA patients | 93 (24.5%) | 59 (15.0%) | .001 |
LOS, length of stay; RAPT, Risk Assessment Prediction tool; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Bold values are significance of P ≤ .05.
Figure 3.
Proportion of patients discharged home according to RAPT score.
Table 4.
Outcome variables, pre-RAPT vs post-RAPT.
| Outcome variable | Pre-RAPT | Post-RAPT | P value |
|---|---|---|---|
| Adverse in-hospital event, n (%) | 24 (3.9%) | 35 (5.5%) | .170 |
| Postoperative transfusion, n (%) | 6 (0.96%) | 7 (1.10%) | .807 |
| Unplanned readmission, n (%) | 25 (4.01%) | 29 (4.54%) | .640 |
RAPT, Risk Assessment Prediction tool.
The mRAPT had only 15.94% of patients score mIR (score 4-7) for which no accurate discharge disposition prediction could be achieved. Among the 84.06% of patients with a discharge predicted by the mRAPT, the overall predictive accuracy was 92.01%, with a 100% predictive accuracy for those deemed mHR (score 1-3) and 91.92% for those deemed mLR (score 8-12). The mRAPT scoring system was also found to be predictive of hospital length of stay: mHR 2.8 days, mIR 2.2 days, and mLR 1.7 days (P < .001) (Table 3).
Discussion
The demand for TJA is expected to increase as the United States population ages [14]. With an increase in TJA, there has been a push to improve quality of care while lowering associated health-care costs. Postarthroplasty care is one area of focus in the effort to lower costs through decreased hospital length of stay as well and appropriate discharge home of patients. In response to the increased costs associated with discharge to skilled care facilities, many institutions have implemented clinical care pathways with tremendous success through reductions in length of hospital stay, usage of postacute care services, and rates of readmission [[1], [2], [3],9,10,15]. Appropriate identification and risk stratification of each patient is imperative as unexpected deviations may lead to increased financial expenditures, unnecessary medical waste, and poor patient satisfaction [15]. Originally developed by Oldmeadow et al. [11] in 2003, the Risk Assessment Prediction Tool (RAPT) was designed to predict the need for extended inpatient rehabilitation after TJA. The RAPT score was then validated in the United States by Hansen et al. in 2015 [12] at which time approximately 45% of arthroplasty patients required discharge to some type of extended care facility. More recently, however, there has been growing evidence for RAPT’s efficacy with modern discharge practices. A recent meta-analysis from Sconza et al. [13] highlighted the ability of the RAPT system to effectively stratify patients and capacity to influence a patient’s length of stay after TJA, and a retrospective study from Dibra et al. [1] proposed modified scoring criteria for improved prediction accuracy.
The RAPT score is presently used at our institution preoperatively to predict TJA patients’ discharge disposition in an effort to appropriately allocate resources, streamline discharge planning, and prepare patients for their planned discharge disposition before surgery. As anticipated, collection and utilization of RAPT scores was associated with significantly decreased hospital length of stay (pre-RAPT 2.22 days vs post-RAPT 1.82 days, P < .001) and proportion of patients discharged to a facility (pre-RAPT 21.8% vs post-RAPT 15.2%, P = .002) without an increased rate of readmission or adverse events.
However, given recent advancements in rapid-discharge protocols, we analyzed our RAPT scores and discharge data and modified the RAPT score cutoffs to provide more accurate discharge predictions for our modern arthroplasty practice.
The Oldmeadow et al. [11] and Hansen et al [12] RAPT scoring cutoffs both had poor predictive accuracy for high- and intermediate-risk groups when used in our modern arthroplasty population. This resulted in large percentage of patients for whom discharge planning could not be predicted as well as poor predictive accuracy for patients defined as high risk. Previous RAPT studies have reported poor predictive accuracy for intermediate risk patients; however, poor predictive accuracy among high-risk cohorts has not yet been reported [1,9,10]. Failure of prior published scoring cutoffs is likely secondary to a general shift toward home discharge among patients overall. Only 15.2% of patients in our modern cohort required discharge to skilled care facilities compared with over 40% in the Oldmeadow et al. [11] and Hansen et al. [12] cohorts. By developing and applying our mRAPT group cutoffs, we were able to improve our discharge predictive accuracy and better reflect modern arthroplasty discharge practices. The “mRAPT” cutoffs developed defined the mHR score as 1-3, mIR as 4-7, and mLR as 8-12. Compared to the Oldmeadow et al. [11] and Hansen et al. [12] RAPT cutoff values, mRAPT was able to accurately predict a higher percentage of patients’ discharges (84.1%, compared with 54.2% for Oldmeadow et al. [11] and 35.2% for Hansen et al. [12]) and had a better predictive accuracy for the high-risk patients (100.0%, compared with 66.7% for Oldmeadow et al. [11] and 57.6% for Hansen et al. [12]). In addition to discharge disposition, the mRAPT groups were also predictive of length of stay.
A study from 2019 published by Dibra et al. [1] at the University of Florida applied the RAPT score to their institution’s modern total joint program. Interestingly, the authors ultimately concluded that the same modified RAPT cutoff values the present study proposes improved the predictive accuracy to their modern arthroplasty practice [1]. Similar to our study, Dibra et al. [1] had only 14% of patients discharged to skilled care facilities. The concordance between the 2 studies suggests that the mRAPT score may be broadly applicable to institutions in various regions throughout the country assuming access to similar care pathways and modern rapid recovery arthroplasty programs. Of note, Dibra et al. [1] further evaluated other factors that may influence discharge disposition and found the only other patient factor was patient-reported discharge expectations. Similarly, Halawi et al. [3] also found that age, care-giver support, and patient discharge expectations were significant predictors of discharge disposition. Given that the RAPT score includes a question on age and care-giver support but does not include a question on patient discharge expectations, this may be a potential area for improvement and further investigation in the future.
There are several limitations of the study including the retrospective design which is subject to inherent bias associated with data collection. This study was conducted at a single academic institution, and therefore results may be influenced by unique patient demographics and characteristics as well as institutional protocols, which highlights the need for additional validation studies in various regions throughout the country. This study only evaluated primary TJA patients, and therefore, results may not be applicable for conversion or revision arthroplasty patients as well as outpatient TJA. Further studies should evaluate the RAPT score and the applicability of these procedures.
Conclusion
The RAPT score identifies a patient’s potential discharge disposition preoperatively allowing appropriate allocation of resources resulting in decreased length of stay and decreased discharge to rehab facility in patients residing in the northeast region of the United States. However, owing to the recent postarthroplasty care trends favoring discharge home over inpatient rehabilitation, historically published RAPT scoring cutoffs are inaccurate for modern arthroplasty practice. Using modified RAPT cutoffs, similar to those used by Dibra et al. [1], (mHR 1-3, mIR 4-7, mLR 8-12) maximizes the number of patients for whom an accurate discharge prediction can be made. This knowledge allows for early postoperative discharge planning and accurate identification of high-risk patients who may require further hospital resources and rehabilitation as well as identification of low-risk patients who may be fast-tracked for discharge home.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
References
- 1.Dibra F.F., Silverberg A.J., Vasilopoulos T., Gray C.F., Parvataneni H.K., Prieto H.A. Arthroplasty care redesign impacts the predictive accuracy of the risk assessment and prediction tool. J Arthroplasty. 2019;34:2549. doi: 10.1016/j.arth.2019.06.035. [DOI] [PubMed] [Google Scholar]
- 2.Ponnusamy K.E., Naseer Z., Dafrawy M.H.E. Post-discharge care duration, charges, and outcomes among medicare patients after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2017;99:e55. doi: 10.2106/JBJS.16.00166. [DOI] [PubMed] [Google Scholar]
- 3.Halawi M.J., Vovos T.J., Green C.L., Wellman S.S., Attarian D.E., Bolognesi M.P. Patient expectation is the most important predictor of discharge destination after primary total joint arthroplasty. J Arthroplasty. 2015;30:539. doi: 10.1016/j.arth.2014.10.031. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz A.J., Bozic K.J., Etzioni D.A. Value-based total hip and knee arthroplasty: a framework for understanding the literature. J Am Acad Orthop Surg. 2019;27:1. doi: 10.5435/JAAOS-D-17-00709. [DOI] [PubMed] [Google Scholar]
- 5.Featherall J., Brigati D.P., Faour M., Messner W., Higuera C.A. Implementation of a total hip arthroplasty care pathway at a high-volume health system: effect on length of stay, discharge disposition, and 90-day complications. J Arthroplasty. 2018;33:1675. doi: 10.1016/j.arth.2018.01.038. [DOI] [PubMed] [Google Scholar]
- 6.London D.A., Vilensky S., O’Rourke C., Schill M., Woicehovich L., Froimson M.I. Discharge disposition after joint replacement and the potential for cost savings: effect of hospital policies and surgeons. J Arthroplasty. 2016;31:743. doi: 10.1016/j.arth.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Molloy I.B., Martin B.I., Moschetti W.E., Jevsevar D.S. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99:402. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarpong N.O., Boddapati V., Herndon C.L., Shah R.P., Cooper H.J., Geller J.A. Trends in length of stay and 30-day complications after total knee arthroplasty: an analysis from 2006 to 2016. J Arthroplasty. 2019;34:1575. doi: 10.1016/j.arth.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 9.Slover J., Mullaly K., Karia R. The use of the risk assessment and prediction tool in surgical patients in a bundled payment program. Int J Surg. 2017;38:119. doi: 10.1016/j.ijsu.2016.12.038. [DOI] [PubMed] [Google Scholar]
- 10.Cizmic Z., Feng J.E., Anoushiravani A.A., Borzio R.W., Schwarzkopf R., Slover J.D. The risk assessment and prediction tool is less accurate in extended length of stay patients following total joint arthroplasty. J Arthroplasty. 2019;34:418. doi: 10.1016/j.arth.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Oldmeadow L.B., McBurney H., Robertson V.J. Predicting risk of extended inpatient rehabilitation after hip or knee arthroplasty. J Arthroplasty. 2003;18:775. doi: 10.1016/s0883-5403(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 12.Hansen V.J., Gromov K., Lebrun L.M., Rubash H.E., Malchau H., Freiberg A.A. Does the risk assessment and prediction tool predict discharge disposition after joint replacement? Clin Orthop Relat Res. 2015;473:597. doi: 10.1007/s11999-014-3851-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sconza C., Respizzi S., Grappiolo G., Monticone M. The risk assessment and prediction tool (Rapt) after hip and knee replacement: a systematic review. Joints. 2019;7:41. doi: 10.1055/s-0039-1693459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz A.J., Bozic K.J., Etzioni D.A. Value-based total hip and knee arthroplasty. J Am Acad Orthop Surg. 2019;27:1. doi: 10.5435/JAAOS-D-17-00709. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.