Abstract
Background
Total hip arthroplasty (THA) is one of the most successful procedures in orthopedic surgery. The most frequent THA indications are osteoarthritis and avascular necrosis, whereas symptomatic aseptic loosening is the most common indication to revision surgery. Chondrosarcoma (CS) is the most frequent bone sarcoma in adults, and proximal femur is the most prevalent location. Wide resection is the treatment of choice.We report 3 cases of unrecognized high-grade CS in the setting of primary or revision THA and reviewed the literature on this rare clinical presentation.
Methods
A systematic literature review on CS in the setting of THA, published between 1980 and 2020, was performed on PubMed, Embase, Medline, Ovid SP, and Web of Science, using the guidelines set in the Preferred Reporting Items for Systematic Reviews and Mata-analyses (PRISMA).
Results
Case series: Three patients were referred to our sarcoma center after failure of THA due to unrecognized high-grade CS. All 3 had rapid fatal outcome. Literature review: Fifty-nine articles were identified, of which 8 were included in the study. They confirmed that primary or revision THA failure due to unrecognized CS is extremely rare, with only few cases reported in the literature.
Conclusions
Before proceeding to primary or revision arthroplasty, diagnosis must be ascertained. Atypical presentation of a common pathology, such as osteoarthritis, avascular necrosis, or aseptic loosening of an endoprosthesis, should raise suspicion for another cause to symptoms, and additional workup be performed. As our cases demonstrated, unrecognized or inadequately managed bone sarcoma may lead to poor or even fatal outcome.
Keywords: Chondrosarcoma, Total hip prosthesis, Hip replacement, Unrecognized, Misdiagnosis, Delayed
Introduction
According to the Swedish registry, 125 total hip arthroplasties (THAs) per 100,000 inhabitants per year were performed in the 2000s [1]. With 95% of good or excellent results at 10 years, THA is one of the most successful interventions in orthopedic surgery and was described as the operation of the century in 2007 [2,3].
While benign chondroid tumors are frequent, bone sarcomas have a very low incidence. Altogether, osteosarcoma, Ewing sarcoma, and chondrosarcoma (CS) represent less than 0.2% of all malignancies [4]. CS represents 20% of bone sarcomas and is the most frequent one in adults (sixth to eighth decade) [[5], [6], [7]]. Characterized by the presence of a cartilaginous matrix on plain film, CS is most commonly located in the pelvis and proximal femur [8]. Twice as frequent in men [9], it can occur secondarily to benign lesions, including osteogenic exostoses (osteochondromas), multiple hereditary exostoses, enchondromas, Ollier’s disease, or Maffuci’s syndrome. Nonetheless 85% are primary CS [10].
Altogether, CS has a variable prognosis, with 89% median survival at 5 years for patients with low-grade tumors, and 53% for patients with high-grade tumors [5]. Dedifferentiated CS has a poorer outcome with a survival rate under 20% at 5 years [[11], [12], [13]].
Low-grade CS (atypical cartilaginous tumor) can be treated by curettage, while central low-grade and high-grade CS in all locations should be treated by wide “en bloc” surgical excision [14]. CS is relatively resistant to radiation and chemotherapy, which is hardly ever indicated in this entity. Treatment of CS should be dedicated to sarcoma centers.
Prognosis of CS depends mainly on initial stage, histological subtype, grade, and location. Age, size, and general status at the time of diagnosis are secondary prognostic factors. Finally, initial management in a reference center and surgical resection margins are major prognostic factors that are directly influenced by physicians. In case of inadequate resection of an unrecognized CS, the outcome will be poorer, with a virtual 100% local recurrence rate and a high risk of mutilating salvage procedures [8,12,14,15].
We report on one case of dedifferentiated CS and 2 cases of conventional high-grade CS, misdiagnosed as hip osteoarthritis (OA), osteonecrosis of the femoral head, or aseptic loosening of a THA, with rapid fatal outcome. We also performed a systematic review of the literature on unexpected CS diagnosis in the setting of THA.
Material and methods
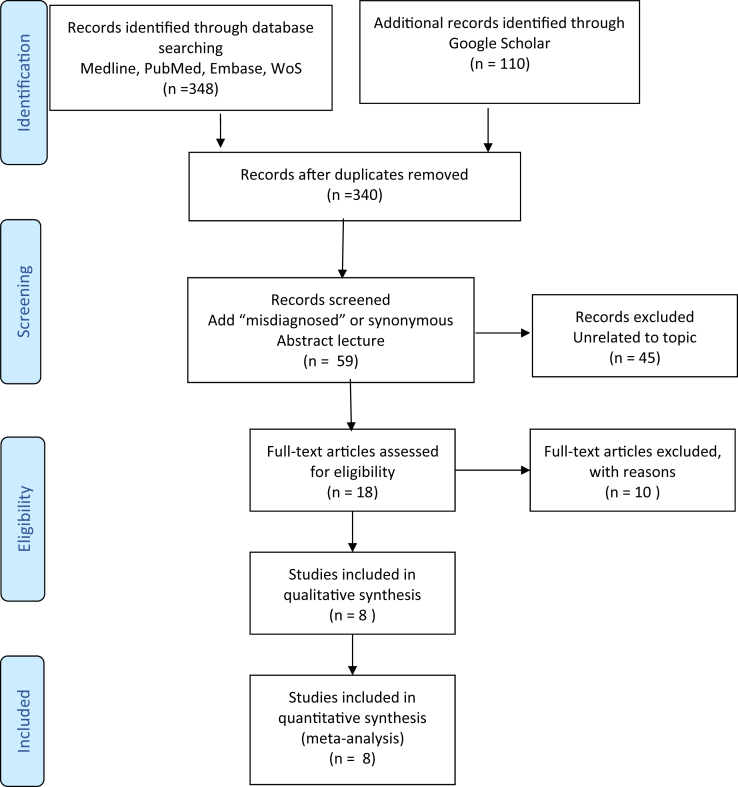
We performed a systematic English literature review, focusing on the relationship between THA and misdiagnosed CS. We followed the guidelines set in the Preferred Reporting Items for Systematic Reviews and Mata-analyses (PRISMA). In February 2020, we searched on PubMed, Embase, Medline, Ovid SP, Web of Science, and Google Scholar. A combination of the terms “chondrosarcoma”, “chondroblastic”, “hip arthroplasty”, “total hip prosthesis”, “hip replacement”, “hip endoprosthesis”, “hip revision”, and “total hip prosthesis” were used. We found 340 publications. We added the criteria “unrecognized”, “misdiagnosis”, “fail”, “delayed”, “diagnostic error”, “mistaken”, “missed diagnosis”, and “diagnostic challenges” and obtained 59 publications. We read all the abstracts and kept 18 articles for full analysis. Eventually, 8 articles on our subject were included in our review (Table 1) [[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26]].
Table 1.
Literature review.
| Authors | Number of cases (including review) | Numbers chondrosarcoma in THR | Subtype chondrosarcoma | Initial diagnosis | Sex/age of the patient (year old) | Delay in diagnosis |
|---|---|---|---|---|---|---|
| Adelani et al., 2009 [16] | 6 | 1 | No information | Nonunion intertrochanter fracture | M/61 | 0 (intraop. diagnosis) |
| Dowdy et al., 1998 [17] | 6 | 3 |
|
|
|
No information |
| Liska et al., 2015 [15] | 1 | 1 | Clear cell chondrosarcoma | Second OA due to hip dysplasia | F/38 | 7 years |
| Sampath Kumar et al., 2013 [26] | 20 | 1 | No information | OA | No information | No information |
| Tay et al., 2014 [19] | 1 | 1 | Clear cell chondrosarcoma | Aneurysmal bone cyst | F/32 | 0 (intraop. diagnosis) |
| Harris et al., 1990 [24] | 1 | 1 | Chondrosarcoma associated to Maffucci’s syndroma | OA | F/70 | 3 years |
| Visuri et al., 2006 [25] | 46 | 1 (cf Harris 1990) | 1 (cf Harris 1990) | 1 (cf Harris 1990) | 1 (cf Harris 1990) | 1 (cf Harris 1990) |
| Soares do Brito et al., 2020 [27] | 1 | 1 | Grade 2 chondrosarcoma | OA | M/60 | 0 (intraop. diagnosis) |
Results
Three patients were referred to our sarcoma center after CS-linked THA failure. The arthroplasties were all performed by senior board-certified surgeons with a general orthopedic practice, working either in a nonacademic (regional) hospital or in private practice. All preoperative radiographs (standard pelvic and hip views) were made in their in-office radiology unit and were therefore not reviewed by a radiologist before initial treatment.
Case 1
A 74-year-old male patient presented with recurrent and progressively disabling pain 6 months after uncemented ceramic-on-ceramic THA. Plain films showed extensive osteolysis around the stem, and bone scan confirmed massive uptake around the stem. Blood analysis (C-reactive protein < 1 mg/L) and joint aspiration did not reveal any evidence of periprosthetic joint infection (Fig. 1). Magnetic resonance imaging (MRI) showed a bulky tumoral mass around the proximal femur. Computed tomography (CT)-guided core needle biopsy demonstrated high-grade dedifferentiated CS. Comprehensive workup revealed stage IV disease with multiple lung metastases. After discussion in our sarcoma board, we proposed palliative chemotherapy and radiotherapy. The patient accepted only palliative radiotherapy (39 Gy) and committed medically assisted suicide a few weeks later, as progression of the disease was obvious. At retrospective analysis, initial plain films revealed no classic signs of OA (eg, loss of articular height, sclerosis or osteophytes), in contrast atypical remodeling and lytic changes could be observed in the femoral head.
Figure 1.
Case 1: dedifferentiated chondrosarcoma. (a) Initial plain films displaying no sign of osteoarthritis but remodeling and lytic lesion of the femoral head. (b) CT showing osteolysis of the medial aspect of the femur and loosening of the stem. (c) Plain films with osteolysis around the stem. (d) Single photon emission computed tomography scan (SPECT-CT) with uptake on the stem. (e) MRI revealing a tumoral mass of the proximal femur around the stem.
Case 2
A 66-year-old male patient was referred to our sarcoma center 1 year after anatomic modular uncemented metal-on-metal THA was performed for “OA or aseptic osteonecrosis of the femoral head,” as the orthopedic surgeon mentioned in his operative report. Plain films revealed a lytic tumoral lesion of the iliopubic ramus extending into the acetabulum and surrounding soft tissues (Fig. 2). Comprehensive workup demonstrated localized grade 2 conventional CS. The patient declined extra-articular wide “en bloc” resection of the tumor. The disease progressed locally, lung metastases appeared after a few months, and the patient soon died of the disease. Retrospective analysis of the initial preoperative plain films revealed no signs of OA or aseptic necrosis of the femoral head; however, no additional workup had been performed at this point.
Figure 2.
Case 2: Conventional grade 2 chondrosarcoma. (a) Initial plain film displaying no evidence of OA. (b) One year after THA. (c) MRI revealing a bulky bone and soft tissue mass. (d) Bone scan showing massive uptake of the ramus pubis and soft tissue extension.
Case 3
An 81-year-old male patient complained of progressively debilitating right groin pain 9 years after uncemented anatomic ceramic-on-ceramic THA. Plain films showed radiolucency of the greater trochanter (Fig. 3). Stress shielding or aseptic loosening was initially suspected. Bone scan showed massive uptake around the stem. Infection was excluded by joint aspiration. Despite unclear diagnosis, his orthopedic surgeon performed revision of the stem. Two months later, a second revision was performed for suspicion of delayed acute infection, which was not confirmed. A mass effect then appeared, associated to wound breakdown. MRI and CT scan showed a bulky tumor with compression of the iliac vessels. The patient was finally referred to our sarcoma center. Comprehensive workup demonstrated localized high-grade dedifferentiated CS. The patient declined curative hindquarter amputation and died a few weeks later.
Figure 3.
Case 3: Dedifferentiated chondrosarcoma. (a) Plain film 9 years after right THA displaying osteolysis and remodeling around proximal stem. (b and c) Osteolysis progression after revision of the stem within 3 months. (d) MRI showing a bulky tumor.
Discussion
Literature on unrecognized CS in the setting of THA is scarce and limited to case reports and small case series. Moreover, primary bone sarcomas are often mixed with other diagnoses, such as benign tumors, hematologic malignancies, or metastases. To our knowledge, no systematic review on the topic has ever been published. We followed the guidelines set in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (Fig. 4). We could identify 8 relevant articles, which are summarized in Table 1. Altogether, we found 10 cases of misdiagnosed CS after primary or revision of THA. Owing to a low number of cases, we cannot estimate the incidence of misdiagnosed bone malignancies including CS in the setting of THA.
Figure 4.
PRISMA.
In the 1990s, metal implants themselves were suspected to induce bone sarcoma. Jacobs et al. presented a case report on a malignant fibrous histiocytoma (former denomination of unclassified pleomorphic sarcoma) after cementless THA and performed a literature review: They found 17 cases of bone sarcoma (but no CS) and 1 adenocarcinoma associated to THA or total knee arthroplasty. In all cases, cobalt or stainless-steel components were suspected to be associated with sarcomatous degeneration [28]. Ward et al. also described neoplasia associated to metal implants and presented a case of osteosarcoma after nailing of a femoral neck fracture [29]. Brien et al. also described a case of osteogenic sarcoma 8 years after THA [21]. The hypothesis of implant-induced neoplastic degeneration has nowadays been abandoned [30]. These tumors were likely initially misdiagnosed, similar to our cases 1 and 2, or unfortunately developed by chance around an implant, as highlighted in our third case.
Dowdy et al. [17] reported on a series of 6 patients with 3 osteosarcomas and 3 CS accidentally diagnosed in the setting of a THA. The cause for hip prosthesis implantation in CS cases was an enchondroma in a 74-year-old female patient (definitive diagnosis: grade 2 CS), a pathological fracture without diagnosed primary tumor in a 60-year-old male patient (definitive diagnosis: dedifferentiated CS), and a loose cup without suspicion of neoplastic condition in a 61-year-old female patient (definitive diagnosis: grade 2 CS). The patient with the suspected enchondroma needed resection of the proximal femur and reconstruction with a tumor prosthesis. He was still disease-free after 51 months of follow-up. The second patient needed entire femur resection and total femur prosthetic reconstruction; he died of the disease after 21 months. The third one was amputated, 61 months after complex pelvic resection and allograft reconstruction. He was still alive 3 months after amputation [17]. Soares de Brito et al. [27] recently presented a case report on a grade 2 CS of the proximal femur where the tumor was discovered and biopsy performed during THA approach. Wide “en bloc” resection was still feasible and secondarily performed by an orthopedic oncology team, and the femur reconstructed with a tumor prosthesis [27]. Nonetheless, the patient suffered from local recurrence after 2 years and suffered salvage hemipelvectomy. Both studies identified unrecognized CS and therefore contaminated surgical field as predisposing factors for tumor recurrence and poor outcome.
In a retrospective study including 225 patients, Ulrich et al. [2] analyzed the causes for THA revision, looking back at indication to primary hip arthroplasty and causes for revision. Five tumors were identified in the indication for hip replacement, without information either on the primary neoplasia or on whether tumors were initially unrecognized. For the whole series, the cause for revision was aseptic loosening in 51.9%, instability in 16.9%, infection in 15.6%, pain in 8%, periprosthetic fracture in 5.5%, and component failure in 2.1%. The tumor group was revised for aseptic loosening in all cases. There was no description of tumor progression. They performed a literature review, where 9 studies on revision arthroplasty were included, with a total of 1372 revisions: Tumor misdiagnosis or progression was not mentioned as a cause of THA failure [2].
CS is rare and generally presents after the fifth decade [[5], [6], [7],12,13]. In the same time, median age at THA is above 70 years, with indication rising after 50 years of age, as confirmed by the Swedish registry [1,31]. This theoretically should make CS as the most probable misdiagnosed primary bone sarcoma in the setting of a THA: Surprisingly, our systematic review revealed that this hypothesis is not currently supported by the existing literature. Visuri et al. published a review of 46 cases of malignant tumors at the site of a THA: There was only one CS [25]. This case, as described by Harris [24] 16 years earlier, was a 70-year-old woman known for Maffucci’s syndrome. She had received a THA for OA 3 years earlier, and loosening of the femoral implant revealed to be caused by CS [24]. Malignant transformation of benign chondroid tumors, including osteochondroma, multiple hereditary exostoses, enchondroma, Ollier’s disease, or Maffuci’s syndrome is well documented, but not as missed diagnosis in the setting of THA [32].
Epiphyseal or apophyseal primary tumors are extremely rare, with clear cell CS as the theoretically exclusive malignant representative. Its benign, although locally aggressive, counterpart is chondroblastoma. Clear cell CS represents 2-5% of all CS and usually develops in younger patients [8,19]. Consequently, the femoral head and both trochanters should be at risk of misdiagnosed clear cell CS in the setting of THA. Liska et al. described the case of a 38-year-old woman who had a THA implanted for OA secondary to dysplasia, which actually turned out to be an undiagnosed clear cell CS [15]. We retrieved similar cases in our literature review (Table 1) [19].
Some of the typical radiological signs of hip OA, that is, joint space narrowing, marginal osteophytes, subchondral sclerosis, and periarticular bone cysts, should be present on plain films to support diagnosis and surgical indication to THA [33]. Likewise, signs of avascular necrosis of the femoral head must be present on plain films or on MRI. In most cases, the combination of the symptoms and typical plain films is sufficient to confirm the indication to THA. If not, Karachalios et al. proposed to proceed with further diagnostic workup (CT scan or MRI) to exclude other causes for hip pain [33,34]. Plain films of case 1 demonstrated some signs of OA, but essentially atypical remodeling of the femoral head, with loss of sphericity and some osteolysis in the inferior and medial aspect of the head, which are typical neither for OA nor for avascular necrosis. Even more, in case 2, there was no joint space, bone or soft tissue anomaly to be detected on initial plain films. Retrospective analysis reveals unspecific osteolysis of the iliopubic ramus. Indication to THA cannot be supported by these findings, and MRI would have been indicated to complete the workup. Preoperative plain films (standard pelvic and hip views) of all 3 cases were made in an in-office radiology unit and were therefore not reviewed by a board-certified radiologist before initial treatment. It is likely that abnormal findings would otherwise have been identified and prompted further workup before undergoing THA. In our institution, we recommend careful review of radiologic reports regarding unexpected findings on plain films. Furthermore, whenever the clinical signs are not in accordance to the radiologic findings, the threshold for additional imaging (MRI > CT) is low. On plain films, aseptic loosening is suspected if radiolucent areas and cystic changes are present around the implant or cement, in case of cement fracture or secondary displacement of implants [35]. Additional workup with bone scan or metal artifact reduction sequence MRI and joint aspiration are indicated to rule out infection, the second most common cause for revision [36]. In case 3, progressive radiolucency around the stem was highly atypical for a classical loosening, and, in the absence of infection, another cause for painful THA should have been actively sought.
Diagnosis of benign chondroid tumors (osteochondroma and enchondroma) is generally obvious on plain film. On the other hand, CS may be difficult to differentiate from benign chondroid tumors and should be evoked in bigger lesions, when cortical erosion (endosteal scalloping >50%) or destruction is apparent in the presence of chondroid matrix, sometimes accompanied by a bulky soft tissue component. CT scan and MRI are used to confirm the presence of cartilaginous matrix and appreciate bone extension and soft tissue involvement [37,38]. Johan et al. reviewed 6000 patients in the databank of the Netherlands Committee of Bone Tumors and concluded that there should be a low threshold to perform complementary CT or MRI in doubtful cases [10].
Whatever be the stage and general status of the patient, treatment of CS should be dedicated to specialized sarcoma centers. Bone sarcoma management is beyond the goal of the present article [39]. Overall, except in central locations (typically in the pelvis), intralesional excision may be acceptable for low-grade (atypical cartilaginous tumors, or grade 1 CS) tumors, when imaging is in accordance with the diagnosis. On contrary, for high-grade and central tumors, wide “en bloc” resection is the generally recommended option [8,14,40,41]. Bone defect reconstruction after “en bloc” resection remains challenging and is also beyond the scope of our review [[40], [41], [42]]. In our series, the first patient was not to be operated anymore because of his advanced disease (multiple lung metastases), the second would have been a candidate for wide “en bloc” extra-articular resection of pelvic zones 2 and 3, and the third would have theoretically been a candidate for hindquarter amputation. In all 3 cases, initial mismanagement of an unrecognized CS led to potentially extreme salvage procedures at best, palliative treatment at worst, while all 3 might have been treated with curative intent if initially recognized by their hip surgeon.
Conclusion
Unrecognized CS is an extremely rare cause of THA failure, with only a few cases described in the literature. In our series, preoperative diagnostic workup was constantly insufficient. Atypical presentation of a common pathology, such as OA, avascular necrosis of the femoral head, or aseptic loosening of a hip prosthesis, should raise suspicion for another underlying pathology, and additional workup is indicated. In native hips, an MRI is the favored imaging modality in the absence of a contraindication. A metal artifact reduction sequence MRI is favored in the presence of THA. In any unclear case, a second opinion should be asked in a multidisciplinary reference center.
Conflict of interests
The authors declare there are no conflicts of interest.
Acknowledgment
Cécile Jacques, Medical Library, Research and Education Department, Lausanne university Hospital—CHUV assisted with bibliography and references.
Supplementary data
References
- 1.Malchau H., Herberts P., Eisler T., Garellick G., Soderman P. The Swedish total hip replacement register. J Bone Joint Surg Am. 2002;84-A(Suppl 2):2. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 2.Ulrich S.D., Seyler T.M., Bennett D. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32(5):597. doi: 10.1007/s00264-007-0364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 4.SEER Surveillance, Epidemiology, and end results program (SEER) 2018. www.seer.cancer.gov
- 5.Fletcher C.D., Unni K.K., Mertens F. IARC Press; Lyon: 2002. World Health Organization Classification of Tumors. Pathology and genetics of tumours of soft tissue and bone WHO classification of tumours; p. 241. [Google Scholar]
- 6.Damron T.A., Ward W.G., Stewart A. Osteosarcoma, chondrosarcoma, and ewing's sarcoma: national cancer data base report. Clin Orthop Relat Res. 2007;459:40. doi: 10.1097/BLO.0b013e318059b8c9. [DOI] [PubMed] [Google Scholar]
- 7.Thorkildsen J., Taksdal I., Bjerkehagen B. Chondrosarcoma in Norway 1990-2013; an epidemiological and prognostic observational study of a complete national cohort. Acta Oncol. 2019;58(3):273. doi: 10.1080/0284186X.2018.1554260. [DOI] [PubMed] [Google Scholar]
- 8.Riedel R.F., Larrier N., Dodd L., Kirsch D., Martinez S., Brigman B.E. The clinical management of chondrosarcoma. Curr Treat Options Oncol. 2009;10(1-2):94. doi: 10.1007/s11864-009-0088-2. [DOI] [PubMed] [Google Scholar]
- 9.Sisu A.M., Tatu F.R., Stana L.G., Petrescu C.I., Tatu C., Motoc A. Chondrosarcoma of the upper end of the femur. Rom J Morphol Embryol. 2011;52(2):709. [PubMed] [Google Scholar]
- 10.Bloem J.L., Reidsma Bone and soft tissue tumors of hip and pelvis. Eur J Radiol. 2012;81(12):3793. doi: 10.1016/j.ejrad.2011.03.101. [DOI] [PubMed] [Google Scholar]
- 11.Strotman P.K., Reif T.J., Kliethermes S.A., Sandhu J.K., Nystrom L.M. Dedifferentiated chondrosarcoma: a survival analysis of 159 cases from the SEER database (2001-2011) J Surg Oncol. 2017;116(2):252. doi: 10.1002/jso.24650. [DOI] [PubMed] [Google Scholar]
- 12.Liu C., Xi Y., Li M. Dedifferentiated chondrosarcoma: radiological features, prognostic factors and survival statistics in 23 patients. PLoS One. 2017;12(3):e0173665. doi: 10.1371/journal.pone.0173665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Staals E.L., Bacchini P., Bertoni F. Dedifferentiated central chondrosarcoma. Cancer. 2006;106(12):2682. doi: 10.1002/cncr.21936. [DOI] [PubMed] [Google Scholar]
- 14.Pring M.E., Weber K.L., Unni K.K., Sim F.H. Chondrosarcoma of the pelvis. A review of sixty-four cases. J Bone Joint Surg Am. 2001;83-A(11):1630. [PubMed] [Google Scholar]
- 15.Liska F., Toepfer A., Straub M., Rechl H., von Eisenhart-Rothe R. Delayed diagnosis of clear cell chondrosarcoma after total hip replacement. A case report of a rare entity encountered in common surgery. Hip Int. 2015;25(1):98. doi: 10.5301/hipint.5000181. [DOI] [PubMed] [Google Scholar]
- 16.Adelani M.A., Stover D.G., Halpern J.L., Schwartz H.S., Holt G.E. Caveat arthroplasty. J Arthroplasty. 2009;24(5):728. doi: 10.1016/j.arth.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 17.Dowdy P.A., Griffin A.M., White L.M., Wunder J.S., Bell R.S. Bone sarcoma diagnosed at the time of reconstructive hip surgery. Can J Surg. 1998;41(4):273. [PMC free article] [PubMed] [Google Scholar]
- 18.Hermann G., Klein M.J., Abdelwahab I.F., Kenan S. Synovial chondrosarcoma arising in synovial chondromatosis of the right hip. Skeletal Radiol. 1997;26(6):366. doi: 10.1007/s002560050249. [DOI] [PubMed] [Google Scholar]
- 19.Tay T., Wong S.B., Sittampalam K., Lie D.T. Clear cell chondrosarcoma with secondary aneurysmal bone cyst changes. Singapore Med J. 2014;55(3):e49. doi: 10.11622/smedj.2014038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moura D.L., Fonseca R., Freitas J., Figueiredo A., Casanova J. Reconstruction with iliac pedestal cup and proximal femur tumor prosthesis after wide resection of chondrosarcoma - 10-year follow-up results. Rev Bras Orthop. 2017;52(6):748. doi: 10.1016/j.rboe.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brien W.W., Salvati E.A., Healey J.H., Bansal M., Ghelman B., Betts F. Osteogenic sarcoma arising in the area of a total hip replacement. A case report. J Bone Joint Surg Am. 1990;72(7):1097. [PubMed] [Google Scholar]
- 22.Ward J.J., Thornbury D.D., Lemons J.E., Dunham W.K. Metal-induced sarcoma. A case report and literature review. Clin Orthop Relat Res. 1990;(252):299. [PubMed] [Google Scholar]
- 23.Wakeshima Y., Ellen M.I. Atypical hip pain origin in a young athletic woman: a case report of giant cell carcinoma. Arch Phys Med Rehabil. 2001;82(10):1472. doi: 10.1053/apmr.2001.25994. [DOI] [PubMed] [Google Scholar]
- 24.Harris W.R. Chondrosarcoma complicating total hip arthroplasty in Maffucci's syndrome. Clin Orthop Relat Res. 1990;260:212. [PubMed] [Google Scholar]
- 25.Visuri T., Pulkkinen P., Paavolainen P. Malignant tumors at the site of total hip prosthesis. Analytic review of 46 cases. J Arthroplasty. 2006;21(3):311. doi: 10.1016/j.arth.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 26.Sampath Kumar V., Tyrrell P.N., Singh J., Gregory J., Cribb G.L., Cool P. Surveillance of intramedullary cartilage tumours in long bones. Bone Joint J. 2016;98-b(11):1542. doi: 10.1302/0301-620X.98B11.37864. [DOI] [PubMed] [Google Scholar]
- 27.Brito JSd, Spranger A., Almeida P., Presa D., Fernandes I., Protela J. Proximal femur chondrosarcoma misdiagnosed as hip arthritis. J Bone Joint Surg Case Connect. 2020;10:e0324. doi: 10.2106/JBJS.CC.19.00324. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs J.J., Rosenbaum D.H., Hay R.M., Gitelis S., Black J. Early sarcomatous degeneration near a cementless hip replacement. A case report and review. J Bone Joint Surg Br. 1992;74(5):740. doi: 10.1302/0301-620X.74B5.1326562. [DOI] [PubMed] [Google Scholar]
- 29.Ward J.J., Thornbury D.D., Lemons J.E., Dunham W.K. Metal-Induced Sarcoma - a case report and literature review. Clin Orthop Relat Res. 1990;252:299. [PubMed] [Google Scholar]
- 30.Signorello L.B., Ye W., Fryzek J.P. Nationwide study of cancer risk among hip replacement patients in Sweden. J Natl Cancer Inst. 2001;93(18):1405. doi: 10.1093/jnci/93.18.1405. [DOI] [PubMed] [Google Scholar]
- 31.Christofilopoulos P., Lubbeke A., Peter R., Hoffmeyer P. [Update on total hip arthroplasty] Rev Med Suisse. 2010;6(276):2454. [PubMed] [Google Scholar]
- 32.Verdegaal S.H., Bovee J.V., Pansuriya T.C. Incidence, predictive factors, and prognosis of chondrosarcoma in patients with Ollier disease and Maffucci syndrome: an international multicenter study of 161 patients. Oncologist. 2011;16(12):1771. doi: 10.1634/theoncologist.2011-0200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hayashi D., Roemer F.W., Guermazi A. Imaging for osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):161. doi: 10.1016/j.rehab.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 34.Karachalios T., Karantanas A.H., Malizos K. Hip osteoarthritis: what the radiologist wants to know. Eur J Radiol. 2007;63(1):36. doi: 10.1016/j.ejrad.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 35.Kobayashi A., Donnelly W.J., Scott G., Freeman M.A. Early radiological observations may predict the long-term survival of femoral hip prostheses. J Bone Joint Surg Br. 1997;79(4):583. doi: 10.1302/0301-620x.79b4.7210. [DOI] [PubMed] [Google Scholar]
- 36.Koutalos A.A., Toms A.P., Cahir J.G., Smith E.J. Correlation of MARS MRI findings with cup position, metal ion levels and function in metal-on-metal total hip arthroplasty. Hip Int. 2020;30(1):64. doi: 10.1177/1120700019868162. [DOI] [PubMed] [Google Scholar]
- 37.Littrell L.A., Wenger D.E., Wold L.E. Radiographic, CT, and MR imaging features of dedifferentiated chondrosarcomas: a retrospective review of 174 de novo cases. Radiographics. 2004;24(5):1397. doi: 10.1148/rg.245045009. [DOI] [PubMed] [Google Scholar]
- 38.Bernard S.A., Murphey M.D., Flemming D.J., Kransdorf M.J. Improved differentiation of benign osteochondromas from secondary chondrosarcomas with standardized measurement of cartilage cap at CT and MR imaging. Radiology. 2010;255(3):857. doi: 10.1148/radiol.10082120. [DOI] [PubMed] [Google Scholar]
- 39.Song K., Shi X., Liang X. Risk factors for metastasis at presentation with conventional chondrosarcoma: a population-based study. Int Orthop. 2018;42:2941. doi: 10.1007/s00264-018-3942-7. [DOI] [PubMed] [Google Scholar]
- 40.Abdel M.P., von Roth P., Perry K.I., Rose P.S., Lewallen D.G., Sim F.H. Early results of acetabular reconstruction after wide periacetabular oncologic resection. J Bone Joint Surg Am. 2017;99(3):e9. doi: 10.2106/JBJS.16.00803. [DOI] [PubMed] [Google Scholar]
- 41.Chan L.W., Imanishi J., Ngan S.Y. Extracorporeal irradiation and reimplantation with total hip arthroplasty for periacetabular pelvic resections: a review of 9 cases. Sarcoma. 2016;2016:2549616. doi: 10.1155/2016/2549616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bus M.P., Szafranski A., Sellevold S. LUMiC((R)) endoprosthetic reconstruction after periacetabular tumor resection: short-term results. Clin Orthop Relat Res. 2017;475(3):686. doi: 10.1007/s11999-016-4805-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.