Abstract
Gastric cancer (GC) is one of the most common cancers with high malignancy. In spite of the great development in diagnostic tools and application of anti-tumor drugs, we have not witnessed a significant increase in the survival time of patients with GC. Multiple studies have revealed that Wnt, Nrf2, MAPK, and PI3K/Akt signaling pathways are involved in GC invasion. Besides, long non-coding RNAs and microRNAs function as upstream mediators in GC malignancy. GC cells have acquired resistance to currently applied anti-tumor drugs. Besides, combination therapy is associated with higher anti-tumor activity. Resveratrol (Res) is a non-flavonoid polyphenol with high anti-tumor activity used in treatment of various cancers. A number of studies have demonstrated the potential of Res in regulation of molecular pathways involved in cancer malignancy. At the present review, we show that Res targets a variety of signaling pathways to induce apoptotic cell death and simultaneously, to inhibit the migration and metastasis of GC cells.
Keywords: Resveratrol, Gastric cancer, Cell signaling, Cancer prevention, Anti‐tumor activity, Molecular pathways
Introduction
Cancer is considered as the most challenging public health issue in both developing and developed countries [1–4]. This life threatening condition burdens high socioeconomic cost. It seems that the incidence rate of cancer is rapidly growing due to the aging of population [5, 6]. Over the past decades, we have witnessed an increase in the incidence rate of Gastric cancer (GC), so that estimates demonstrate that up to 1 million new cases of GC are diagnosed annually and over 700.000 deaths occur [7–11]. This has resulted in much attention towards this cancer. Epidemiological studies demonstrate that GC occurs with high frequency in Asia, Europe, and South America [12]. The World Health Organization (WHO) has divided GC into four characteristic categories including papillary, mucinous, tubular, and signet ring cell [13]. To date, several diagnostic tools have been developed for GC. The most challenging barrier in GC therapy is the diagnosis of this life-threatening condition at advanced stages. Diagnostic tools have enabled us to diagnose GC in its early stages and subsequently, its elimination. Endoscopic ultrasound, computed tomography (CT), magnetic resonance imaging [14], and positron emission tomography are the most common diagnostic tools used in GC diagnosis [15].
Hereditary factors are responsible for about 1–3 % of cancer, while environmental factors are the main reasons of cancer. Smoking, lack of exercise, and poor diet are the major environmental factors of cancer [12, 16]. Much attention has been directed towards cancer therapy and using chemotherapeutic agents is of interest. However, in spite of application of a high amount of chemotherapeutic agents, we have not witnessed a remarkable increase in the survival time of patients with cancer. This has led to the looking at nature as a rich source of anti-tumor drugs. Several studies have revealed the great potential of plant-derived chemicals in inhibition of proliferation and migration of cancer cells, stimulation of apoptotic and autophagic cell death, and enhancing the efficacy of chemotherapy [17–20]. Resveratrol (Res) as a naturally occurring compound, is considered a secondary metabolite exclusively derived from plants and microbial sources [21–23]. The synthesis process of Res is triggered by the action of stilbene synthase (STS) enzyme that incorporates three malonyl coenzyme-A units into 4-hydroxycinnamoyl-CoA (p-coumaroyl-CoA) [24]. This non-flavonoid polyphenol compound is present in a number of plants including grapes, peanuts, and berries [25–27]. A growing body of evidence demonstrates that Res functions as a part of defense system of plants responding to insect and pathogen attacks [28, 29]. Besides, Res is capable of protecting plants against fungal infections and ultra-violet (UV) radiations [30–33]. Overall, Res is available in two forms known as cis and trans due to the central ethylene moiety. It seems that the major form of Res is trans-isomer. However, exposing to the UV is associated with formation of cis-isomer [34–36]. Accumulating data demonstrates that Res has a variety of pharmacological and health-promoting impacts such as antioxidant [37], anti-inflammatory [38], anti-diabetic [39], anti-tumor [40], hepatoprotective [41], and cardioprotective [42].
The great biological and therapeutic activities of Res have led to its application in treatment of various cancers. It is held that Res is able to target different molecular signaling pathways in cancer therapy. One of the difficulties in cancer therapy is the resistance of tumor cells into chemotherapy. This problem has led to the development of novel synthetic anti-tumor drugs. However, application of the high amount of an anti-tumor drug reduces its capability in next treatments. Furthermore, a number of signaling pathways are involved in dynamic progression of tumor cells demanding combination therapy in suppressing cancer cells. It seems that urokinase-type plasminogen activator receptor (uPAR) contributes to the regulation of epidermal growth factor receptor (EGFR) [43]. Overexpression of uPAR is associated with resistance of cancer cells to chemotherapy. Administration of Res sensitizes oral squamous cell carcinoma (OSCC) to chemotherapy by down-regulation of uPAR and its downstream mediator ERK1/2 [44]. Res is able to regulate microRNAs (miRs) in enhancing the efficacy of chemotherapy. Accumulating data demonstrates that Res upregulates oncosuppressor miR to stimulate apoptotic cell death in cancer cells [45, 46]. Exposure to Res improves the chemotherapy potential by enhancing the expression of miR-122-5p leading to the induction of apoptosis and reduced viability of cancer cells [47]. Epithelial-to-mesenchymal transition (EMT) contributes to the increased malignancy and invasion of tumor cells [48]. Inhibition of EMT is of importance in cancer therapy. Administration of Res remarkably diminishes the proliferation and invasion capabilities of breast and lung cancer cells by stimulation of tumor suppressor Rad9 [49]. These studies highlight this fact that Res is capable of regulation of signaling pathways involved in cancer malignancy [50, 51] and its administration can be considered as a promising strategy in tumor therapy. Notably, various molecular signaling pathways are involved in the malignancy of GC cells and there have been efforts to identify these pathways and also their upstream and downstream mediators. Accumulating data demonstrates that abnormal expression of miRs is associated with development of cancer [52–54]. In the case of GC, a similar story occurs. It seems that GC cells down-regulate the expression of miR-27b-3p to ensure their viability and proliferation through enhancing the expression of GSPT1 [55]. It is held that the PI3K/Akt signaling pathway contributes to the progression of GC cells by EMT stimulation [56, 57]. Importantly, UFM1 is associated with decreased migration of GC cells through inhibition of PI3K/Akt molecular signaling [58]. Long non-coding RNAs (lncRNAs) are non-protein coding RNA molecules with the length of 200 nucleotides. It has been reported that lncRNA deregulation leads to cancer generation [59]. LncRNAs are able to dually reduce/enhance the malignancy of cancer cells. A study reveals that lncRNA HOTAIR is capable of elevating the invasion of GC cells by induction of CXCR4 and RhoA signaling pathways, while another study demonstrates that lncRNA GAS5 is related to the inhibited metastasis of GC cells by targeting p53 [60, 61]. Mitogen-activated protein kinase (MAPK), Wnt, and nuclear factor erythroid 2-related factor 2 (Nrf2) are other molecular pathways involved in GC malignancy [62–64].
At the present review, we demonstrate how Res can be beneficial in treatment of gastric cancer (GC).
Current therapeutic strategies, challenges and future prospective for gastric cancer
Currently, surgery and chemotherapy are the most common strategies in treatment of GC [65]. However, the recurrence of GC usually occurs after surgery. Besides, the resistance of GC cells into chemotherapy is another major problem. Notably, there have been efforts to improve the efficacy of chemotherapy. A look at newly published articles demonstrates that naturally occurring compounds are applied to enhance the potential of chemotherapy. Curcumin is one of them with high anti-tumor capability [66–68]. Curcumin is able to improve the anti-tumor activity of 5-fluorouracil (5-FU) against GC cells by inhibition of COX-2 and NF-κB signaling pathways [69]. Berberine is another potential anti-tumor agent [70]. [70]. It seems that administration of berberine is associated with enhanced inhibitory impact of EGFR inhibitors on GC cells [71]. It appears that plant-derived chemicals are extensively used in GC therapy. However, there are some challenges faced in GC therapy. The most important one is the low bioavailability of applied anti-tumor drugs. Furthermore, lack of specific targeting leads to the toxicity of anti-tumor drugs against normal cells. Nanoparticles (NPs) are focused to increase the bioavailability of anit-cancer agents such as Res. NPs are structures with a particle size as low as 100 nm. These nanocarriers are able to remarkably enhance the bioavailability of anti-tumor drugs by protection against degradation and also prevention of drug trapping via phagocytosis system. On the other hand, identification of cell membrane receptors on cancer cells have resulted in the development of receptor-targeted nanocarriers and consequently, high anti-tumor activity [55, 72, 73].
Resveratrol and gastric cancer
Resveratrol effect on tumor cell cycle
Although EMT is suggested to be beneficial in wound healing and other physiological processes, this mechanism remarkably enhances the metastasis of tumor cells [83]. During EMT, an increase occurs in the migratory capability of cells via transformation of epithelial cells into mesenchymal cells [84, 85]. Various signaling pathways are involved in EMT and accumulating data demonstrates that metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) is capable of induction of EMT in a number of cancers leading to their high invasion capability [86–88]. It appears that administration of Res effectively down-regulates MALAT1 to prevent EMT resulting in reduced invasion and metastasis of GC cells [64].
Accumulating data demonstrates that the hedgehog (Hh) signaling pathway is vital for physiological conditions such as hematopoiesis and is also involved in tumorigenesis [89, 90]. It has been reported that aberration in Hh signaling pathway occurs in a number of cancers such as lung cancer, prostate cancer and so on [91–95]. Notably, the Hh pathway stimulates EMT in GC [96]. Hence, modulation of this signaling pathway is of importance in inhibition of migration and metastasis of cancer cells. It appears that Gli-1 is a biomarker of abnormal expression of Hh pathway [97]. Administration of Res significantly deactivates Hh pathway by down-regulation of Gli-1. As a result, the expressions of factors involved in EMT such as Snail and N-cadherin undergo down-regulation, while an increase occurs in the expression of E-cadherin to suppress EMT resulting in reduced invasion and migration of GC cells [98].
Accumulating data reveals that Res is able to affect various signaling pathway in treatment of disorders [99, 100]. Down-regulation of protein kinase C (PKC) by Res is related to the reduced viability and growth of cells. It seems that PKC α has high sensitivity to Res administration [101]. It has been demonstrated that PKC σ exerts anti-proliferative and pro-apoptotic impacts [102–104]. Res follows a same strategy in treatment of GC. Administration of Res enhances the expression of cytosolic PKC α and reduces membrane-associated PKC σ protein. These impacts lead to the induction of tumor suppressor p21 and p53. Besides, Res treatment elevates the levels of Fas and Fas-L protein. These effects altogether result in stimulation of cell cycle arrest at G2/M phase and trigger apoptotic cell death to suppress GC malignancy [105]. Chemotherapeutic activity of Res mainly depends on its impact on PKC. A growing body of evidence demonstrates that PKC participates in tumor progression, tumor proliferation, tumor viability and tumor migration [106–108]. Res exerts a negligible impact on cell lysis, while it considerably induces G0/G1 cell cycle arrest and apoptosis by down-regulation of PKC [109] demonstrating the potential role of this signaling pathway in progression and malignancy of GC cells.
Importantly, Res has shown great potential in suppressing the proliferation of tumor cells through targeting cell cycle [110–112]. Res applies various signaling pathways to target cell cycle. It has been demonstrated that Res is capable of affecting the expression of sirtuin 1 (Sirt1) [113, 114]. A same story occurs in GC therapy. Administration of Res stimulates the activation of Sirt1 leading to the cell cycle arrest and induction of senescence in tumor cell of nude mice [115].
Resveratrol effect on apoptosis
The stimulation of apoptotic cell death is still one of the most common strategies in the field of cancer therapy. Notably, various molecular signaling pathways contribute to the regulation of apoptosis in cancer cells and identification of these pathways is of importance in cancer therapy [38]. Nuclear factor-κB (NF-κB) is responsible for regulation of immunological responses [116]. A variety of studies have shed some light on the involvement of NF-κB signaling pathway in cancer progression and it seems that NF-κB overexpression is related to the generation of cancer [117–120]. Administration of Res sensitizes cancer cells to apoptosis via NF-κB down-regulation leading to a decrease in the level of anti-apoptotic factor Bcl-2 and an increase in apoptotic factors caspase-3 and caspase-8 [121]. Mitochondria play a significant role in apoptosis induction. As a central gateway, mitochondrial pathway modulates both anti- and pro-apoptotic factors [122–125]. Compounds targeting mitochondria are of interest in cancer therapy by induction of apoptotic cell death [126, 127]. Res uses same strategy in combating GC. Administration of Res is associated with disruption of mitochondrial membrane potential. This leads to the induction of apoptotic cell death through upregulation of caspase-3 and caspase-9, and down-regulation of Bcl-2. Finally, a remarkable decrease occurs in the viability and proliferation of GC cells [128]. Exposing GC cells into Res increases the cells having morphological features of apoptosis such as chromatin condensation, chromatin crescent formation and nucleus fragmentation. Upregulation of BAX and down-regulation of Bcl-2 by Res are involved in these anti-tumor impacts in implanted human primary gastric carcinoma cells in nude mice [129]. Resveratrol plus curcumin could regulate p53 post-translational alterations in rat model of gastric cancer [130].
It is held that various GC cell lines respond differently to the Res administration. A study conducted by Riles and colleagues obviously clarifies this statement. They applied three distinct types of GC cells including AGS, SNU-1 and KATO-III cells. In SUN-1 cells treated with Res, there was no trace of alteration in the expression of mitochondrial-mediated apoptotic proteins such as Bcl-2, BAX, Bid and Smad/Diablo. It seems that survivin inhibition by Res contributes to the reduced viability and proliferation of SUN-1 cells. However, the story is a little different for AGS and KATO-III cells. It appears that mitochondrial dysfunction induced by Res is involved in the stimulation of apoptotic cell death in these cells since an increase occurs in the level of cytochrome C [131]. Regardless of the apoptotic pathway, Res administration is a promising strategy in reducing the migration and malignancy of GC cells [132].
Resveratrol effect on inflammation
A growing body of evidence demonstrates that pro-inflammatory cytokines such as interleukin-6 (IL-6) are present with high levels in cancer cells. It seems that enhanced concentration of IL-6 significantly promotes the viability and proliferation of tumor cells [133, 134]. Investigation of molecular signaling pathways shows that IL-6 elevates the progression of cancer cells through induction of Raf-MAPK signaling pathway [135, 136]. Similarly, administration of Res suppresses IL-6-mediated GC invasion through inhibition of Raf-MAPK signaling pathway [137]. The cytokines and peptide growth factors force cells to produce ROS [138, 139]. The ROS generation is a vital step in enhancing the proliferation of cells by acting as intracellular messenger and interacting with molecular pathways such as Ras pathway [140–142]. In respect to the carcinogenesis impact of ROS, using naturally occurring antioxidants such as Res is of interest in cancer therapy. After Res supplementation, an increase occurs in nitric oxide (NO) production by nitric oxide synthase (NOS) induction that interacts with ROS leading to the reduced viability, proliferation and migration of GC cells [143].
Resveratrol effect on oxidative stress
As it was mentioned, ROS are considered as potential targets in cancer therapy. It has been demonstrated that enhanced concentration of ROS is associated with a number of pathological conditions [144, 145]. This is due to the adverse impact of Res on the cell membrane and more importantly, genetic material that sensitizes cells to high proliferation and generation of cancer [146]. Although much emphasis was put on the negative role of ROS, it seems that ROS are important elements of homeostasis since they function as second messengers of molecular signaling pathways [147]. Hence, regulation of ROS synthesis is of importance in treatment of pathological conditions and preserving homeostasis. In the case of GC therapy, Res remarkably reduces the concentrations of ROS via its great antioxidant activity. Investigation of molecular pathways demonstrates that inhibition of ROS-mediated GC progression is induced by down-regulation of c-Jun and ERK1/2 phosphorylation through MEK1/2 [148].
Resveratrol effect on autophagy
Over the past decades, we have witnessed an attention into autophagy mechanism due to its dual role between life and death [149]. This has resulted in targeting autophagy in cancer therapy [150]. This lysosome-mediated mechanism ensures homeostasis and survival during physiological condition by degradation of aged and damaged organelles and components [70]. Notably, autophagy is involved in caspase-independent programmed cell death [151]. So, autophagic cell death is considered as one of the most promising strategies in cancer therapy [152]. There are a number of pathways and macromolecules that are able to regulate autophagy [73, 153, 154]. Dihydroceramide is a ceramide metabolic precursor involved in sphingolipid synthesis. Dihydroceramide desaturases (Des1 and Des2) convert the dihydroceramide into ceramide. Accumulating data demonstrates that dihydroceramide is capable of induction of autophagy [155, 156]. Res administration significantly enhances the intracellular level of dihydroceramide to trigger autophagy leading to the reduced viability and proliferation of GC cells and sensitizing these malignant cells into apoptosis [157].
Table 1 indicates the potential therapeutic effects of resveratrol against gastric cancer.
Table 1.
The potential therapeutic effects of Res in GC therapy
| Cell line/Animal mod-el | Dose | Duration | Outcomes | Refs. |
|---|---|---|---|---|
| Human gastric cancer cell lines SGC7901 and BGC823 | 0, 5, 10, 25, 50, 100, 200 and 400 µM | 24, 48 and 72 h | Inhibition of MALAT1-induced EMT | [63] |
| Human gastric cancer SGC-7901 cell line | 0, 100, 200, 300 and 400 µmol/L | 48 h | Suppressing Hh signaling pathway is associated with EMT inhibition | [93] |
| SGC7901 cells | 35.69 µM | 72 h | Administration of Res stimulates apoptotic cell death and cell cycle arrest in GC cells | [99] |
| Human gastric cancer SNU-1 cells | 0, 10, 50 and 100 µM | 24 h | Induction of apoptosis and reduced viability of cancer cells | [100] |
| Human gastric adenocarcinoma SGC7901 cells | 0, 25, 50, 100 and 200 µmol/L | 48 h | Stimulation of apoptotic cell death and DNA damage through enhancing the ROS production | [101] |
|
Human GC cell lines AGS Nude mice xenograft model |
0, 5, 10, 25, 50, 100 and 200 µM 40 mg/kg |
24 h 4 weeks |
Induction of cell cycle arrest and senescence | [110] |
|
Balb/c-nu/nu mice BGC823 cells |
0.1, 1, 5, 10, 20, 50 and 100 µg/ml 10 mg/kg |
24 h 3 days |
A significant reduction in tumor burden and an increase in apoptosis | [111] |
| Human gastric cancer SGC-7901 cell line | 0, 100, 200, 300 and 400 µmol/L | 48 h | Suppressing Hh signaling pathway is associated with EMT inhibition | [93] |
| SGC7901 cells | 35.69 µM | 72 h | Administration of Res stimulates apoptotic cell death and cell cycle arrest in GC cells | [99] |
| SGC-7901 cells | 50, 200 and 400 µM | 24 h | Induction of apoptosis by down-regulation of NF-κB | [112] |
| Human gastric cancer cell lines | 0, 10, 20, 30, 40, 50 and 100 µM | 48 h | Inhibition of IL-6-induced Raf-MAPK | [113] |
| Human gastric cancer cell lines that were either sensitive or resistant to cytostatic drugs | 30 and 50 µM | 72 h | Inhibition of MDR by down-regulation of ABCB1, P-gp, ANXA1 and TXN | [114] |
|
Human gastric carcinoma SGC-7901 cells Nude mice |
25 and 50 µM 50 mg/kg |
24 h 21 days |
Stimulation of apoptotic cell death in GC cells through mitochondrial pathway | [115] |
|
Human gastric cancer cells SGC7901 and MGC803 Nude mice inoculated subcutaneously with SGC7901/DOX cells |
50 mg/L 50 mg/kg |
48 h 4 weeks |
Res activates PTEN to down-regulate Akt resulting in EMT-mediated drug resistance | [168] |
| Human gastric adenocarcinoma cell line MGC803 | 0, 50, 100 and 200 µM | 24 h | Inhibition of PI3K/Akt signaling pathway through PTEN down-regulation significantly induces cell cycle arrest | [167] |
Resveratrol effect on multidrug resistance in chemotherapy
One of the most important difficulties faced in cancer therapy is multidrug resistance (MDR) [158–160]. MDR remarkably reduces the efficacy of chemotherapy [161, 162]. ATP binding cassette subfamily B member 1 (ABCB1) is one of the genes involved in MDR that by encoding P-glycoprotein (P-gp) inhibits the entering of anti-tumor drugs into cells [163–166]. Annexin A1 (ANXA1) and thioredoxin (TXN) are other possible mechanisms involved in MDR and consequently, cancer progression [167–169]. Administration of Res effectively diminishes the expression of ABCB1, P-gp, ANXA1 and TXN to suppress MDR [170]. [171]. Doxorubicin (DOX) is one of the potential chemotherapeutic agents with high capability in reducing the viability of cancer cells [172]. However, resistance to DOX treatment is a common phenomenon. It has been shown that PTEN is involved in EMT-mediated drug resistance [82]. Res is able to inhibit DOX resistance by stimulation of PTEN. The activated PTEN significantly diminishes Akt signaling pathway resulting in suppressing EMT-mediated drug resistance [173].
Resveratrol‐loaded drug delivery systems
There are a number of properties associated with mesoporous silica NPs (SLNs) making them suitable for delivery of genes and drugs [174]. These features include low particle size, sustained-release manner and large surface area [175]. This has led to the development of anti-miR-21- and Res-loaded SLNs for GC therapy. MiR-21 is an oncogenesis miR that significantly enhances the malignancy and invasion of cancer cells [176]. It seems that loading a combination of Res and anti-miR-21 on SLNs remarkably induces apoptotic cell death in GC cells. Besides, the synergistic impact of anti-miR-21 and Res reduces tumor burden [177], showing their efficacy in GC therapy.
Conclusion and remarks
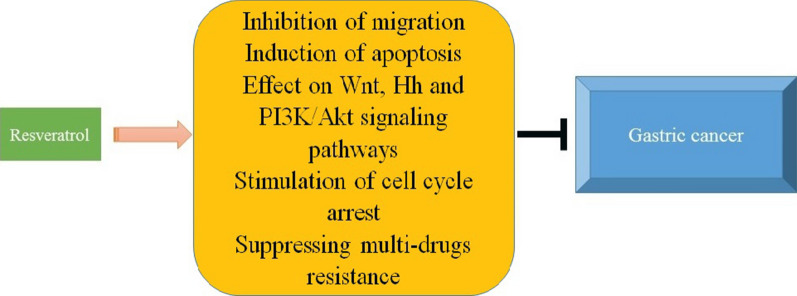
Taking everything into account, it seems that GC is still one of the most challenging disorders and there have been much effort to treat it. It is worth mentioning that cancer cells are able to obtain resistance to anti-tumor drugs. This urges scientists to develop novel anti-tumor drugs. However, it appears that synthetic anti-tumor drugs have high cost with a number of adverse effects against normal cells. Hence, plant-derived chemicals are of interest in cancer therapy. Res is a non-flavonoid polyphenol with several effects including apoptosis, cell proliferation inhibition, anti-inflammatory aspects. Several research has shown the therapeutic effects of Res for the amelioration of CRC and GC. Res has the potential preventive importance in gastric cancer. Res with several potential effects, is comparatively safe as well as able to target several cell signaling pathways. On the other hand, the bioavailability of Res seems to be very low in humans and due to the metabolic characteristics of res, even a high dose may not reach a sufficient concentration of treatment. Res may be of benefit for treatment of gasteric cancer. However, different techniques have been originated to increase the bioavailability of Res, more research are needed to differ the efficacy of Res in gastric cancer. Res is a non-flavonoid polyphenol with great anti-tumor activity. In the present review, we discussed the latest studies about the efficacy of Res in GC therapy. First off, it is noteworthy that nanocarriers are promising candidates in cancer therapy and due to the low bioavailability of Res, loading this compound on nanocarriers improves its anti-tumor activity. The metastasis of GC cells is a challenge and using Res is associated with reduced migration of GC cells through EMT inhibition. Chemotherapeutic agents are able to diminish the viability and proliferation of cancer cells through induction of apoptotic cell death. Res applies same strategy in GC therapy. Targeting Wnt signaling pathway is another capability of Res. By inhibition of Wnt, Res remarkably reduces the invasion of GC cells. Besides, Res is capable of targeting PI3K/Akt and Hh signaling pathways in GC therapy. More importantly, administration of Res enhances the potential of chemotherapy by sensitizing tumor cells (Fig. 1). These significant anti-tumor effects of Res make it an appropriate choice for treatment of GC. Importantly, urging scientists to investigate the potential anti-tumor activity of Res against GC in clinical trials in of interest. A look into clinicaltrials.gov demonstrates that Res is able to prevent cancer progression and recurrence. Unfortunately, there is no study regarding the anti-tumor activity of Res against GC in clinical trial. This should be considered at the next studies.
Fig. 1.
Application of Res in GC therapy. Hh hedgehog, GC gastric cancer, PI3K phosphatidylinositide 3-kinase
Acknowledgements
Not-applicable.
Abbreviations
- Res
Resveratrol
- STS
Stilbene synthase
- UV
Ultra-violet
- uPAR
Urokinase-type plasminogen activator receptor
- EGFR
Epidermal growth factor receptor
- OSCC
Oral squamous cell carcinoma
- miR
MicroRNA
- EMT
Epithelial-to-mesenchymal transition
- WHO
World Health Organization
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- GC
Gastric cancer
- lncRNA
Long non-coding RNA
- MAPK
Mitogen-activated protein kinase
- Nrf2
Nuclear factor erythroid 2-related factor 2
- 5-FU
5-fluorouracil
- NPs
Nanoparticles
- SLNs
Mesoporous silica NPs
- MALAT1
Metastasis-associated lung adenocarcinoma transcript 1
- NF-KB
Nuclear factor-KB
- IL-6
Interleukin-6
- MDR
Multidrug resistance
- ABCB1
ATP binding cassette subfamily B member 1
- P-gp
P-glycoprotein
- ANXA1
Annexin A1
- TXN
Thioredoxin
- DOX
Doxorubicin
- GSK-3β
Glycogen synthase kinase-3β
- Hh
Hedgehog
- Sirt1
Sirtuin 1
- PKC
Protein kinase C
- NO
Nitric oxide
- NOS
Nitric oxide synthase
Authors’ contributions
Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data: MA., HR, RM. TF and SS. Drafting the article or revising it critically for important intellectual content: MA, HR and RM. Final approval of the version to be published: All authors read and approved the final manuscript.
Funding
Not-applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not-applicable.
Consent for publication
Not-applicable.
Competing Interests
The authors declare no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F, et al., Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 2018. 68(6): p. 394–424. [DOI] [PubMed]
- 2.Ma J, et al. The American Cancer Society 2035 challenge goal on cancer mortality reduction. CA Cancer J Clin. 2019;69(5):351–62. doi: 10.3322/caac.21564. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA: A Cancer Journal for Clinicians, 2013. 63(1): p. 11–30. [DOI] [PubMed]
- 4.Ashrafizadeh MA, Kotla Z, Afshar NG, Samarghandian EG, Mandegary S, Pardakhty A, Mohammadinejad A, Sethi R. Nanoparticles Targeting STATs in Cancer Therapy Cells. 2019;8(10):1158. doi: 10.3390/cells8101158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel R, et al., Cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 2014. 64(1): p. 9–29. [DOI] [PubMed]
- 6.DeSantis C, Naishadham D, Jemal A, Cancer statistics for African Americans, 2013. CA: A Cancer Journal for Clinicians, 2013. 63(3): p. 151–166. [DOI] [PubMed]
- 7.Abuderman AA. Gastric cancer and prospectsof cancer in Saudi Arabia peninsula. Saudi Journal of Biological Sciences. 2019;26(6):1095–100. doi: 10.1016/j.sjbs.2018.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salati M, et al. Gastric cancer: Translating novels concepts into clinical practice. Cancer Treatment Rev. 2019;79:101889. doi: 10.1016/j.ctrv.2019.101889. [DOI] [PubMed] [Google Scholar]
- 9.Slavin TP, et al., Genetics of gastric cancer: what do we know about the genetic risks? Translational Gastroenterology and Hepatology, 2019. [DOI] [PMC free article] [PubMed]
- 10.Tang L, et al. Gastric cancer and image-derived quantitative parameters: Part 2—a critical review of DCE-MRI and 18F-FDG PET/CT findings. Eur Radiol. 2020;30(1):247–60. doi: 10.1007/s00330-019-06370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinasco K, et al., Microbial carcinogenesis: Lactic acid bacteria in gastric cancer. Biochimica et Biophysica Acta (BBA) - Reviews on Cancer, 2019. 1872(2): p. 188309. [DOI] [PubMed]
- 12.Torre LA, et al., Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians, 2015. 65(2): p. 87–108. [DOI] [PubMed]
- 13.Bosman FT, et al. WHO classification of tumours of the digestive system. Geneva: World Health Organization; 2010. p. 417. [Google Scholar]
- 14.Bahri S, et al. Protective role of vitamin E against cadmium induced oxidative stress into the rat liver. La Tunisie medicale. 2019;97(1):100–5. [PubMed] [Google Scholar]
- 15.Brenkman HJF, et al. Evaluation of PET and laparoscopy in STagIng advanced gastric cancer: a multicenter prospective study (PLASTIC-study) BMC Cancer. 2018;18(1):450. doi: 10.1186/s12885-018-4367-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lydiatt WM, et al. Head and neck cancers—major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122–37. doi: 10.3322/caac.21389. [DOI] [PubMed] [Google Scholar]
- 17.Ahmadi Z, Ashrafizadeh M. Melatonin as a potential modulator of Nrf2. Fundam Clin Pharmacol. 2020;34(1):11–9. doi: 10.1111/fcp.12498. [DOI] [PubMed] [Google Scholar]
- 18.Ashrafizadeh M, et al. MicroRNAs mediate the anti-tumor and protective effects of ginsenosides. Nutr Cancer. 2020;72(8):1264–75. doi: 10.1080/01635581.2019.1675722. [DOI] [PubMed] [Google Scholar]
- 19.Ashrafizadeh M, et al. Therapeutic and biological activities of berberine: The involvement of Nrf2 signaling pathway. J Cell Biochem. 2020;121(2):1575–85. doi: 10.1002/jcb.29392. [DOI] [PubMed] [Google Scholar]
- 20.Ashrafizadeh M, Ahmadi Z. Effects of Statins on Gut Microbiota (Microbiome) Rev Clinical Med. 2019;6(2):55–9. [Google Scholar]
- 21.Boo YC. Human Skin Lightening Efficacy of Resveratrol and Its Analogs: From in Vitro Studies to Cosmetic Applications. Antioxidants. 2019;8(9):332. doi: 10.3390/antiox8090332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Intagliata SM, Maria N, Santagati LM, Montenegro L. Strategies to Improve Resveratrol Systemic and Topical Bioavailability: An Update. Antioxidants. 2019;8(8):244. doi: 10.3390/antiox8080244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MenezesC.J.M.D.S. J, Diederich MF. Natural dimers of coumarin, chalcones, and resveratrol and the link between structure and pharmacology. Eur J Med Chem. 2019;182:111637. doi: 10.1016/j.ejmech.2019.111637. [DOI] [PubMed] [Google Scholar]
- 24.Dewick PM. The acetate pathway: fatty acids and polyketides. Medicinal Natural Products: A Biosynthetic Approach: Second Edition, 2001: p. 35–120.
- 25.Farkhondeh T, et al. The Neuroprotective Effects of Thymoquinone: A Review. Dose-Response. 2018;16(2):1559325818761455. doi: 10.1177/1559325818761455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koushki M, et al. Resveratrol: A miraculous natural compound for diseases treatment. Food Science Nutrition. 2018;6(8):2473–90. doi: 10.1002/fsn3.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmadi Z, Mohammadinejad R, Ashrafizadeh M. Drug delivery systems for resveratrol, a non-flavonoid polyphenol: Emerging evidence in last decades. Journal of Drug Delivery Science Technology. 2019;51:591–604. doi: 10.1016/j.jddst.2019.03.017. [DOI] [Google Scholar]
- 28.Gu J, Hu W, Zhang D-d. Resveratrol, a polyphenol phytoalexin, protects against doxorubicin-induced cardiotoxicity. J Cell Mol Med. 2015;19(10):2324–8. doi: 10.1111/jcmm.12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pervaiz S. Chemotherapeutic potential of the chemopreventive phytoalexin resveratrol. 2004. [DOI] [PubMed]
- 30.Hosseini S, et al., Hairy root culture optimization and resveratrol production from Vitis vinifera subsp. sylvesteris. World Journal of Microbiology and Biotechnology, 2017. 33. [DOI] [PubMed]
- 31.Chripkova MZ, Mojzis F. Antiproliferative Effect of Indole Phytoalexins Molecules. 2016;21(12):1626. doi: 10.3390/molecules21121626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeandet P, et al. Biosynthesis, metabolism, molecular engineering, and biological functions of stilbene phytoalexins in plants. BioFactors. 2010;36(5):331–41. doi: 10.1002/biof.108. [DOI] [PubMed] [Google Scholar]
- 33.Adrian M, et al. Stilbene Content of Mature Vitis vinifera Berries in Response to UV-C Elicitation. J Agric Food Chem. 2000;48(12):6103–5. doi: 10.1021/jf0009910. [DOI] [PubMed] [Google Scholar]
- 34.Stervbo U, Vang O, Bonnesen C. A review of the content of the putative chemopreventive phytoalexin resveratrol in red wine. Food Chem. 2007;101:449–57. doi: 10.1016/j.foodchem.2006.01.047. [DOI] [Google Scholar]
- 35.Lamuela-Raventos RM, et al. Direct HPLC Analysis of cis- and trans-Resveratrol and Piceid Isomers in Spanish Red Vitis vinifera Wines. J Agric Food Chem. 1995;43(2):281–3. doi: 10.1021/jf00050a003. [DOI] [Google Scholar]
- 36.Yang I, et al. Photochemical generation of a new, highly fluorescent compound from non-fluorescent resveratrol. Chem Commun. 2012;48(32):3839–41. doi: 10.1039/c2cc30940h. [DOI] [PubMed] [Google Scholar]
- 37.Duca AS, Moacă A, Negrea EA, Lalescu M, Lungeanu V-D, Dehelean D, Muntean C-A, Alexa DM, Ersilia., Identification of Resveratrol as Bioactive Compound of Propolis from Western Romania and Characterization of Phenolic Profile and Antioxidant Activity of Ethanolic Extracts. Molecules 2019. 24(18): p. 3368. [DOI] [PMC free article] [PubMed]
- 38.Rodriguez-Ruiz ME, et al. Apoptotic caspases inhibit abscopal responses to radiation and identify a new prognostic biomarker for breast cancer patients. OncoImmunology. 2019;8(11):e1655964. doi: 10.1080/2162402X.2019.1655964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang DK, Kang H-S, Anti-Diabetic Effect of Cotreatment with Quercetin and Resveratrol in Streptozotocin-Induced Diabetic Rats. Biomolecules & Therapeutics, 2018. 26(2): p. 130–138. [DOI] [PMC free article] [PubMed]
- 40.Yuan L, et al., Resveratrol inhibits the invasion and metastasis of colon cancer through reversal of epithelial– mesenchymal transition via the AKT/GSK–3β/Snail signaling pathway. Molecular Medicine Reports, 2019. 20. [DOI] [PMC free article] [PubMed]
- 41.Bingul I, et al., The protective effect of resveratrol against cyclosporine A-induced oxidative stress and hepatotoxicity. Archives of Physiology and Biochemistry, 2019: p. 1–6. [DOI] [PubMed]
- 42.Zhu L, Li CW, Chen G, Liao H, Zhang W, Xiao L. Upregulated RACK1 attenuates gastric cancer cell growth and epithelial–mesenchymal transition via suppressing Wnt/β-catenin signaling. Onco Targets Ther. 2019;12:4795–805. doi: 10.2147/OTT.S205869. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Uzawa K, et al. EGF receptor transactivation by urokinase receptor stimulus through a mechanism involving Src and matrix metalloproteinases. Exp Cell Res. 2004;292(1):201–208. doi: 10.1016/j.yexcr.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 44.Uzawa K, et al. Resveratrol Targets Urokinase-Type Plasminogen Activator Receptor Expression to Overcome Cetuximab-Resistance in Oral Squamous Cell Carcinoma. Sci Rep. 2019;9(1):12179. doi: 10.1038/s41598-019-48717-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Venkatadri R, et al. Role of apoptosis-related miRNAs in resveratrol-induced breast cancer cell death. Cell Death Dis. 2016;7(2):e2104–4. doi: 10.1038/cddis.2016.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dhar S, Hicks C, Levenson AS. Resveratrol and prostate cancer: Promising role for microRNAs. Mol Nutr Food Res. 2011;55(8):1219–29. doi: 10.1002/mnfr.201100141. [DOI] [PubMed] [Google Scholar]
- 47.Zhang W, et al. Resveratrol chemosensitizes adriamycin-resistant breast cancer cells by modulating miR-122-5. J Cell Biochem. 2019;120(9):16283–92. doi: 10.1002/jcb.28910. [DOI] [PubMed] [Google Scholar]
- 48.Thiery JP. Epithelial–mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2(6):442–54. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 49.Chen K-Y, et al., Resveratrol induced premature senescence and inhibited epithelial-mesenchymal transition of cancer cells via induction of tumor suppressor Rad9. PLOS ONE, 2019. 14: p. e0219317. [DOI] [PMC free article] [PubMed]
- 50.Jang Y-G, et al. Resveratrol inhibits DHT-induced progression of prostate cancer cell line through interfering with the AR and CXCR4 pathway. The Journal of Steroid Biochemistry Molecular Biology. 2019;192:105406. doi: 10.1016/j.jsbmb.2019.105406. [DOI] [PubMed] [Google Scholar]
- 51.Izquierdo-Torres E, et al. Resveratrol up-regulates ATP2A3 gene expression in breast cancer cell lines through epigenetic mechanisms. The International Journal of Biochemistry Cell Biology. 2019;113:37–47. doi: 10.1016/j.biocel.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 52.Soleimani A, et al. Role of TGF-β signaling regulatory microRNAs in the pathogenesis of colorectal cancer. J Cell Physiol. 2019;234(9):14574–80. doi: 10.1002/jcp.28169. [DOI] [PubMed] [Google Scholar]
- 53.Soleimani A, et al. Role of Regulatory Oncogenic or Tumor Suppressor miRNAs of PI3K/AKT Signaling Axis in the Pathogenesis of Colorectal Cancer. Curr Pharm Des. 2018;24(39):4605–10. doi: 10.2174/1381612825666190110151957. [DOI] [PubMed] [Google Scholar]
- 54.Soleimani A, et al. The potential role of regulatory microRNAs of RAS/MAPK signaling pathway in the pathogenesis of colorectal cancer. J Cell Biochem. 2019;120(12):19245–53. doi: 10.1002/jcb.29268. [DOI] [PubMed] [Google Scholar]
- 55.Wu D, et al. Synergistically Enhanced Inhibitory Effects of Pullulan Nanoparticle-Mediated Co-Delivery of Lovastatin and Doxorubicin to Triple-Negative Breast Cancer Cells. Nanoscale Res Lett. 2019;14(1):314. doi: 10.1186/s11671-019-3146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial–mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saunders LR, McClay DR. Sub-circuits of a gene regulatory network control a developmental epithelial-mesenchymal transition. Development. 2014;141(7):1503–13. doi: 10.1242/dev.101436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lin J-X, et al. UFM1 suppresses invasive activities of gastric cancer cells by attenuating the expression of PDK1 through PI3K/AKT signaling. Journal of Experimental Clinical Cancer Research. 2019;38(1):410. doi: 10.1186/s13046-019-1416-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prensner JR, Chinnaiyan AM. The Emergence of lncRNAs in Cancer Biology. Cancer Discov. 2011;1(5):391–407. doi: 10.1158/2159-8290.CD-11-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xiao J, et al. lncRNA HOTAIR promotes gastric cancer proliferation and metastasis via targeting miR-126 to active CXCR4 and RhoA signaling pathway. Cancer Med. 2019;8(15):6768–79. doi: 10.1002/cam4.1302. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 61.Liu Y, et al. Long non-coding RNA GAS5 inhibits migration and invasion in gastric cancer via interacting with p53 protein. Digestive Liver Disease. 2020;52(3):331–8. doi: 10.1016/j.dld.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 62.Kim SH, et al. Silymarin induces inhibition of growth and apoptosis through modulation of the MAPK signaling pathway in AGS human gastric cancer cells. Oncol Rep. 2019;42(5):1904–14. doi: 10.3892/or.2019.7295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang B, et al. TCF7L1 indicates prognosis and promotes proliferation through activation of Keap1/NRF2 in gastric cancer. Acta Biochim Biophys Sin. 2019;51(4):375–85. doi: 10.1093/abbs/gmz015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang Z, et al. Resveratrol suppresses the invasion and migration of human gastric cancer cells via inhibition of MALAT1–mediated epithelial–to–mesenchymal transition. Exp Ther Med. 2019;17(3):1569–78. doi: 10.3892/etm.2018.7142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fisher BW, et al. Urgent Surgery for Gastric Adenocarcinoma: A Study of the National Cancer Database. J Surg Res. 2020;245:619–28. doi: 10.1016/j.jss.2019.07.073. [DOI] [PubMed] [Google Scholar]
- 66.Mortezaee K, et al. Mechanisms of apoptosis modulation by curcumin: Implications for cancer therapy. J Cell Physiol. 2019;234(8):12537–50. doi: 10.1002/jcp.28122. [DOI] [PubMed] [Google Scholar]
- 67.Barati N, et al. Potential therapeutic effects of curcumin in gastric cancer. J Cell Physiol. 2019;234(3):2317–28. doi: 10.1002/jcp.27229. [DOI] [PubMed] [Google Scholar]
- 68.Kouhpeikar H, et al. Curcumin as a therapeutic agent in leukemia. J Cell Physiol. 2019;234(8):12404–14. doi: 10.1002/jcp.28072. [DOI] [PubMed] [Google Scholar]
- 69.Yang H, et al. Curcumin Enhances the Anticancer Effect Of 5-fluorouracil against Gastric Cancer through Down-Regulation of COX-2 and NF- κB Signaling Pathways. J Cancer. 2017;8:3697–706. doi: 10.7150/jca.20196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mohammadinejad R, et al. Berberine as a potential autophagy modulator. J Cell Physiol. 2019;234(9):14914–26. doi: 10.1002/jcp.28325. [DOI] [PubMed] [Google Scholar]
- 71.Wang J, et al., Berberine inhibits EGFR signaling and enhances the antitumor effects of EGFR inhibitors in gastric cancer. Oncotarget, 2016. 7(46). [DOI] [PMC free article] [PubMed]
- 72.Mohammadinejad R, et al. Shedding light on gene therapy: Carbon dots for the minimally invasive image-guided delivery of plasmids and noncoding RNAs - A review. J Adv Res. 2019;18:81–93. doi: 10.1016/j.jare.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ahmadi ZaR, Sahar, Bemani N, Ashrafizadeh, Milad The Targeting of Autophagy and Endoplasmic Reticulum Stress Mechanisms by Honokiol Therapy. Reviews in Clinical Medicine. 2019;6(2):66–73. [Google Scholar]
- 74.Miyoshi K, Hennighausen L. Beta-catenin: a transforming actor on many stages. Breast Cancer Res. 2003;5(2):63–8. doi: 10.1186/bcr566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Maruyama K, et al. Cytoplasmic Beta-Catenin Accumulation as a Predictor of Hematogenous Metastasis in Human Colorectal Cancer. Oncology. 2000;59(4):302–9. doi: 10.1159/000012187. [DOI] [PubMed] [Google Scholar]
- 76.Polakis P. Wnt signaling and cancer. Genes Dev. 2000;14(15):1837–51. [PubMed] [Google Scholar]
- 77.Dai H, et al. Resveratrol inhibits the growth of gastric cancer via the Wnt/β-catenin pathway. Oncol Lett. 2018;16(2):1579–83. doi: 10.3892/ol.2018.8772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kim J-E, et al. Sequential treatment of HPV E6 and E7-expressing TC-1 cells with bortezomib and celecoxib promotes apoptosis through p-p38 MAPK-mediated downregulation of cyclin D1 and CDK2. Oncol Rep. 2014;31(5):2429–37. doi: 10.3892/or.2014.3082. [DOI] [PubMed] [Google Scholar]
- 79.Zhang J, et al. Overexpression of Rab25 contributes to metastasis of bladder cancer through induction of epithelial–mesenchymal transition and activation of Akt/GSK-3β/Snail signaling. Carcinogenesis. 2013;34(10):2401–8. doi: 10.1093/carcin/bgt187. [DOI] [PubMed] [Google Scholar]
- 80.Olga K, Mirzoeva BH, Yun K, Hom J, Debnath D, Aftab K, Shokat WM, Korn Autophagy suppression promotes apoptotic cell death in response to inhibition of the PI3K—mTOR pathway in pancreatic adenocarcinoma. J Mol Med. 2011;89:877–89. doi: 10.1007/s00109-011-0774-y. [DOI] [PubMed] [Google Scholar]
- 81.Yan-nan B, et al. MicroRNA-21 accelerates hepatocyte proliferation in vitro via PI3K/Akt signaling by targeting PTEN. Biochem Biophys Res Commun. 2014;443(3):802–7. doi: 10.1016/j.bbrc.2013.12.047. [DOI] [PubMed] [Google Scholar]
- 82.Jing X, et al. Resveratrol induces cell cycle arrest in human gastric cancer MGC803 cells via the PTEN–regulated PI3K/Akt signaling pathway. Oncol Rep. 2016;35(1):472–8. doi: 10.3892/or.2015.4384. [DOI] [PubMed] [Google Scholar]
- 83.Radisky DC. Epithelial-mesenchymal transition. J Cell Sci. 2005;118(19):4325–6. doi: 10.1242/jcs.02552. [DOI] [PubMed] [Google Scholar]
- 84.Acloque H, et al. Epithelial-mesenchymal transitions: the importance of changing cell state in development and disease. J Clin Investig. 2009;119(6):1438–49. doi: 10.1172/JCI38019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thiery JP, et al. Epithelial-Mesenchymal Transitions in Development and Disease. Cell. 2009;139(5):871–90. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 86.Liang J, et al. MALAT1 induces tongue cancer cells’ EMT and inhibits apoptosis through Wnt/β-catenin signaling pathway. Journal of Oral Pathology Medicine. 2017;46(2):98–105. doi: 10.1111/jop.12466. [DOI] [PubMed] [Google Scholar]
- 87.Li J, et al. LncRNA MALAT1 exerts oncogenic functions in lung adenocarcinoma by targeting miR-204. American journal of cancer research. 2016;6(5):1099–107. [PMC free article] [PubMed] [Google Scholar]
- 88.Zhou X, et al. Long Non Coding RNA MALAT1 Promotes Tumor Growth and Metastasis by inducing Epithelial-Mesenchymal Transition in Oral Squamous Cell Carcinoma. Sci Rep. 2015;5(1):15972. doi: 10.1038/srep15972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McMahon AP, Ingham PW, Tabin CJ, 1 Developmental roles and clinical significance of Hedgehog signaling, in Current Topics in Developmental Biology. 2003, Academic Press. p. 1-114. [DOI] [PubMed]
- 90.Lee J, et al. Gli1 is a target of Sonic hedgehog that induces ventral neural tube development. Development. 1997;124(13):2537–52. doi: 10.1242/dev.124.13.2537. [DOI] [PubMed] [Google Scholar]
- 91.Watkins DN, et al. Hedgehog signalling within airway epithelial progenitors and in small-cell lung cancer. Nature. 2003;422(6929):313–7. doi: 10.1038/nature01493. [DOI] [PubMed] [Google Scholar]
- 92.Kubo M, et al. Hedgehog Signaling Pathway is a New Therapeutic Target for Patients with Breast Cancer. Can Res. 2004;64(17):6071–4. doi: 10.1158/0008-5472.CAN-04-0416. [DOI] [PubMed] [Google Scholar]
- 93.Mimeault M, et al. Cytotoxic effects induced by a combination of cyclopamine and gefitinib, the selective hedgehog and epidermal growth factor receptor signaling inhibitors, in prostate cancer cells. Int J Cancer. 2006;118(4):1022–31. doi: 10.1002/ijc.21440. [DOI] [PubMed] [Google Scholar]
- 94.Qualtrough D, et al. Hedgehog signalling in colorectal tumour cells: Induction of apoptosis with cyclopamine treatment. Int J Cancer. 2004;110(6):831–7. doi: 10.1002/ijc.20227. [DOI] [PubMed] [Google Scholar]
- 95.Thayer SP, et al. Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature. 2003;425(6960):851–6. doi: 10.1038/nature02009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yoo YA, et al. Sonic Hedgehog Pathway Promotes Metastasis and Lymphangiogenesis via Activation of Akt, EMT, and MMP-9 Pathway in Gastric Cancer. Can Res. 2011;71(22):7061–70. doi: 10.1158/0008-5472.CAN-11-1338. [DOI] [PubMed] [Google Scholar]
- 97.Ohta M, et al. p53-Independent Negative Regulation of p21/Cyclin-Dependent Kinase–Interacting Protein 1 by the Sonic Hedgehog-Glioma-Associated Oncogene 1 Pathway in Gastric Carcinoma Cells. Can Res. 2005;65(23):10822–9. doi: 10.1158/0008-5472.CAN-05-0777. [DOI] [PubMed] [Google Scholar]
- 98.Gao Q, et al. Resveratrol inhibits the hedgehog signaling pathway and epithelial-mesenchymal transition and suppresses gastric cancer invasion and metastasis. Oncol Lett. 2015;9(5):2381–7. doi: 10.3892/ol.2015.2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kim J, et al. Grape Peel Extract and Resveratrol Inhibit Wrinkle Formation in Mice Model Through Activation of Nrf2/HO-1 Signaling Pathway. J Food Sci. 2019;84(6):1600–8. doi: 10.1111/1750-3841.14643. [DOI] [PubMed] [Google Scholar]
- 100.Zhao XE, Zhang YZ, Yao H, Liu G, Wei J, Ma Q. Resveratrol Promotes Osteogenic Differentiation of Canine Bone Marrow Mesenchymal Stem Cells Through Wnt/Beta-Catenin Signaling Pathway. Cellular Reprogramming. 2018;20(6):371–81. doi: 10.1089/cell.2018.0032. [DOI] [PubMed] [Google Scholar]
- 101.Slater SJ, et al., Inhibition of protein kinase C by resveratrol. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, 2003. 1637(1): p. 59–69. [DOI] [PubMed]
- 102.Sawai H, et al. Ceramide-induced translocation of protein kinase C-δ and -ε to the cytosol. Implications in apoptosis. J Biol Chem. 1997;272:2452–8. doi: 10.1074/jbc.272.4.2452. [DOI] [PubMed] [Google Scholar]
- 103.Emoto Y, et al. Proteolytic activation of protein kinase C delta by an ICE-like protease in apoptotic cells. The EMBO Journal. 1995;14(24):6148–56. doi: 10.1002/j.1460-2075.1995.tb00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Teruhiko Fujii MaLGa-B, Bernabo´ JL, Caaman˜o J, Ohbai M, Kurokii T, Li L, Yuspa SH, Kazanietz MG. Involvement of Protein Kinase C d (PKCd) in Phorbol Ester-induced Apoptosis in LNCaP Prostate Cancer Cells LACK OF PROTEOLYTIC CLEAVAGE OF PKCd. J Biol Chem. 2000;276(11):7574–82. doi: 10.1074/jbc.275.11.7574. [DOI] [PubMed] [Google Scholar]
- 105.Atten MJ, et al. Resveratrol regulates cellular PKC α and δ to inhibit growth and induce apoptosis in gastric cancer cells. Invest New Drugs. 2005;23(2):111–9. doi: 10.1007/s10637-005-5855-8. [DOI] [PubMed] [Google Scholar]
- 106.Lu P, et al. Belinostat suppresses cell proliferation by inactivating Wnt/β-catenin pathway and promotes apoptosis through regulating PKC pathway in breast cancer. Artificial Cells Nanomedicine Biotechnology. 2019;47(1):3955–60. doi: 10.1080/21691401.2019.1671855. [DOI] [PubMed] [Google Scholar]
- 107.Tang T, et al. Protease Nexin I is a feedback regulator of EGF/PKC/MAPK/EGR1 signaling in breast cancer cells metastasis and stemness. Cell Death Dis. 2019;10(9):649. doi: 10.1038/s41419-019-1882-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hamshaw I, Ajdarirad M, Mueller A. The role of PKC and PKD in CXCL12 directed prostate cancer migration. Biochem Biophys Res Commun. 2019;519(1):86–92. doi: 10.1016/j.bbrc.2019.08.134. [DOI] [PubMed] [Google Scholar]
- 109.Atten MJ, et al. Resveratrol-induced inactivation of human gastric adenocarcinoma cells through a protein kinase C-mediated mechanism. Biochem Pharmacol. 2001;62(10):1423–32. doi: 10.1016/S0006-2952(01)00788-2. [DOI] [PubMed] [Google Scholar]
- 110.Frazzi R, et al. Resveratrol-mediated apoptosis of hodgkin lymphoma cells involves SIRT1 inhibition and FOXO3a hyperacetylation. Int J Cancer. 2013;132(5):1013–21. doi: 10.1002/ijc.27748. [DOI] [PubMed] [Google Scholar]
- 111.Bai Y, et al. Resveratrol induces apoptosis and cell cycle arrest of human T24 bladder cancer cells in vitro and inhibits tumor growth in vivo. Cancer Sci. 2010;101(2):488–93. doi: 10.1111/j.1349-7006.2009.01415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Casanova F, et al. Resveratrol chemosensitizes breast cancer cells to melphalan by cell cycle arrest. J Cell Biochem. 2012;113(8):2586–96. doi: 10.1002/jcb.24134. [DOI] [PubMed] [Google Scholar]
- 113.Jill C, Milne PDL, Schenk S, Carney DP, Smith JJ, Gagne DJ, Jin L, Boss O, Perni RB, Vu CB, Bemis JE, Xie R, Disch JS, Pui Yee Ng, Joseph J, Nunes AV, Lynch H, Yang H, Galonek K, Israelian W, Choy A, Iffland S, Lavu O, Medvedik DA, Sinclair JM, Olefsky MR, Jirousek PJ, Elliott, Christoph H, Westphal, Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature 2017. 450(7170): p. 712–716. [DOI] [PMC free article] [PubMed]
- 114.Knight CM, et al. Mediobasal Hypothalamic SIRT1 Is Essential for Resveratrol’s Effects on Insulin Action in Rats. Diabetes. 2011;60(11):2691–700. doi: 10.2337/db10-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yang Q, et al. Resveratrol Inhibits the Growth of Gastric Cancer by Inducing G1 Phase Arrest and Senescence in a Sirt1-Dependent Manner. PloS one. 2013;8:e70627. doi: 10.1371/journal.pone.0070627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Karin M, Greten FR. NF-κB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5(10):749–59. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- 117.Gasparini C, et al. NF-κB pathways in hematological malignancies. Cell Mol Life Sci. 2014;71(11):2083–102. doi: 10.1007/s00018-013-1545-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Karin M. Nuclear factor-κB in cancer development and progression. Nature. 2006;441(7092):431–6. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 119.Liu B, et al. A Cytoplasmic NF-κB Interacting Long Noncoding RNA Blocks IκB Phosphorylation and Suppresses Breast Cancer Metastasis. Cancer Cell. 2015;27(3):370–81. doi: 10.1016/j.ccell.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 120.Pacifico F, Leonardi A. NF-κB in solid tumors. Biochem Pharmacol. 2006;72(9):1142–52. doi: 10.1016/j.bcp.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 121.Wu X, et al. Resveratrol induces apoptosis in SGC–7901 gastric cancer cells. Oncol Lett. 2018;16(3):2949–56. doi: 10.3892/ol.2018.9045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Green DR, Reed JC. Mitochondria Apoptosis Science. 1998;281(5381):1309–12. doi: 10.1126/science.281.5381.1309. [DOI] [PubMed] [Google Scholar]
- 123.Hengartner MO. The biochemistry of apoptosis. Nature. 2000;407(6805):770–6. doi: 10.1038/35037710. [DOI] [PubMed] [Google Scholar]
- 124.Reed JC. Double identity for proteins of the Bcl-2 family. Nature. 1997;387(6635):773–6. doi: 10.1038/42867. [DOI] [PubMed] [Google Scholar]
- 125.Youle RJ, Strasser A. The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol. 2008;9(1):47–59. doi: 10.1038/nrm2308. [DOI] [PubMed] [Google Scholar]
- 126.Anderson G. Breast cancer: Occluded role of mitochondria N-acetylserotonin/melatonin ratio in co-ordinating pathophysiology. Biochem Pharmacol. 2019;168:259–68. doi: 10.1016/j.bcp.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 127.Tao f-f, Zhang Y, Zhang Z. The Role of Herbal Bioactive Components in Mitochondria Function and Cancer Therapy. Evidence-Based Complementary and Alternative Medicine, 2019. 2019: p. 1–12. [DOI] [PMC free article] [PubMed]
- 128.Yang Y, et al. Resveratrol induced apoptosis in human gastric carcinoma SGC-7901 cells via activation of mitochondrial pathway. Asia-Pacific Journal of Clinical Oncology. 2018;14(5):e317–24. doi: 10.1111/ajco.12841. [DOI] [PubMed] [Google Scholar]
- 129.Zhou H-B, et al. Anticancer activity of resveratrol on implanted human primary gastric carcinoma cells in nude mice. World journal of gastroenterology. 2005;11(2):280–4. doi: 10.3748/wjg.v11.i2.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Xu H, et al., Modulatory Potential of Curcumin and Resveratrol on p53 Post-Translational Modifications during Gastric Cancer. 2018. 37(2): p. 93–101. [DOI] [PubMed]
- 131.Riles WL, et al. Resveratrol engages selective apoptotic signals in gastric adenocarcinoma cells. World journal of gastroenterology. 2006;12(35):5628–34. doi: 10.3748/wjg.v12.i35.5628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zheng GH, Li HQ, [Effects of garlic oil combined with resveratrol on inducting of apoptosis and expression of Fas, bcl-2 and bax in human gastric cancer cell line]. Zhonghua Yu Fang Yi Xue Za Zhi, 2008. 42(1): p. 39–42. [PubMed]
- 133.Eltweri AM, et al. PWE-169 Treatment of oesophageal cell lines with docosahexaenoic fatty acid (DHA) and oxaliplatin: effects on proliferation, expression of vascular endothelial growth factor and IL-6. Gut. 2015;64(Suppl 1):A286. doi: 10.1136/gutjnl-2015-309861.616. [DOI] [Google Scholar]
- 134.Lin M-T, et al. IL-6 induces AGS gastric cancer cell invasion via activation of the c-Src/RhoA/ROCK signaling pathway. Int J Cancer. 2007;120(12):2600–8. doi: 10.1002/ijc.22599. [DOI] [PubMed] [Google Scholar]
- 135.Costa-Pereira AP. Regulation of IL-6-type cytokine responses by MAPKs. Biochem Soc Trans. 2014;42(1):59–62. doi: 10.1042/BST20130267. [DOI] [PubMed] [Google Scholar]
- 136.Sano M, et al. ERK and p38 MAPK, but not NF-κB, Are Critically Involved in Reactive Oxygen Species–Mediated Induction of IL-6 by Angiotensin II in Cardiac Fibroblasts. Circulation research. 2001;89:661–9. doi: 10.1161/hh2001.098873. [DOI] [PubMed] [Google Scholar]
- 137.Yang T, et al. Resveratrol inhibits Interleukin-6 induced invasion of human gastric cancer cells. Biomed Pharmacother. 2018;99:766–73. doi: 10.1016/j.biopha.2018.01.153. [DOI] [PubMed] [Google Scholar]
- 138.Finkel T. Signal transduction by reactive oxygen species. J Cell Biol. 2011;194(1):7–15. doi: 10.1083/jcb.201102095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Singh SV, et al. Mechanism of inhibition of benzo[a]pyrene-induced forestomach cancer in mice by dietary curcumin. Carcinogenesis. 1998;19(8):1357–60. doi: 10.1093/carcin/19.8.1357. [DOI] [PubMed] [Google Scholar]
- 140.Irani K, Goldschmidt-Clermont PJ. Ras, superoxide and signal transduction. Biochem Pharmacol. 1998;55(9):1339–46. doi: 10.1016/S0006-2952(97)00616-3. [DOI] [PubMed] [Google Scholar]
- 141.Irani K, et al. Mitogenic Signaling Mediated by Oxidants in Ras-Transformed Fibroblasts. Science. 1997;275(5306):1649–52. doi: 10.1126/science.275.5306.1649. [DOI] [PubMed] [Google Scholar]
- 142.Burdon RH. Superoxide and hydrogen peroxide in relation to mammalian cell proliferation. Free Radic Biol Med. 1995;18(4):775–94. doi: 10.1016/0891-5849(94)00198-S. [DOI] [PubMed] [Google Scholar]
- 143.Holian O, et al. Inhibition of gastric cancer cell proliferation by resveratrol: role of nitric oxide. American Journal of Physiology-Gastrointestinal Liver Physiology. 2002;282(5):G809–16. doi: 10.1152/ajpgi.00193.2001. [DOI] [PubMed] [Google Scholar]
- 144.Samarghandian S, Samini F, Azimi-Nezhad M, Farkhondeh T. Anti-oxidative effects of safranal on immobilization-induced oxidative damage in rat brain. Neurosci lett. 2017;659:26–32. doi: 10.1016/j.neulet.2017.08.065. [DOI] [PubMed] [Google Scholar]
- 145.Samarghandian S, Azimi-Nezhad M, Farkhondeh T. Catechin Treatment Ameliorates Diabetes and Its Complications in Streptozotocin-Induced Diabetic Rats. Dose-Response. 2017;15(1):1559325817691158. doi: 10.1177/1559325817691158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jackson AL, Loeb LA. The contribution of endogenous sources of DNA damage to the multiple mutations in cancer. Mutation Research/Fundamental Molecular Mechanisms of Mutagenesis. 2001;477(1):7–21. doi: 10.1016/S0027-5107(01)00091-4. [DOI] [PubMed] [Google Scholar]
- 147.Samarghandian S, Borji A, Afshari R, Delkhosh MB, Gholami A. The effect of lead acetate on oxidative stress and antioxidant status in rat bronchoalveolar lavage fluid and lung tissue. Toxicol mech methods. 2013;23(6):432–6. doi: 10.3109/15376516.2013.777136. [DOI] [PubMed] [Google Scholar]
- 148.Aquilano K, et al. trans-Resveratrol inhibits H2O2-induced adenocarcinoma gastric cells proliferation via inactivation of MEK1/2-ERK1/2-c-Jun signalling axis. Biochem Pharmacol. 2009;77(3):337–47. doi: 10.1016/j.bcp.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 149.Ashrafizadeh M, et al. Monoterpenes modulating autophagy: A review study. Basic Clin Pharmacol Toxicol. 2020;126(1):9–20. doi: 10.1111/bcpt.13282. [DOI] [PubMed] [Google Scholar]
- 150.Ashrafizadeh M, et al. Modulatory effects of statins on the autophagy: A therapeutic perspective. J Cell Physiol. 2020;235(4):3157–68. doi: 10.1002/jcp.29227. [DOI] [PubMed] [Google Scholar]
- 151.Tavakol SA, Deng M, Azarian S, Abdoli M, Motavaf A, Poormoghadam M, Khanbabaei D, Afshar HG, Mandegary E, Pardakhty A, Yap A, Mohammadinejad CT, Kumar R, Alan P, Autophagy Modulators: Mechanistic Aspects and Drug Delivery Systems. Biomolecules & Therapeutics, 2019. 9(10): p. 530. [DOI] [PMC free article] [PubMed]
- 152.Ashrafizadeh M, et al., Autophagy as a molecular target of quercetin underlying its protective effects in human diseases. Archives of Physiology and Biochemistry, 2019: p. 1–9. [DOI] [PubMed]
- 153.Ashrafizadeh M, et al. Effects of newly introduced antidiabetic drugs on autophagy. Diabetes & Metabolic Syndrome: Clinical Research & Reviews; 2019. pp. 2445–9. [DOI] [PubMed] [Google Scholar]
- 154.Ashrafizadeh M, et al. Autophagy, anoikis, ferroptosis, necroptosis, and endoplasmic reticulum stress: Potential applications in melanoma therapy. J Cell Physiol. 2019;234(11):19471–9. doi: 10.1002/jcp.28740. [DOI] [PubMed] [Google Scholar]
- 155.Zheng W, et al. Ceramides and other bioactive sphingolipid backbones in health and disease: Lipidomic analysis, metabolism and roles in membrane structure, dynamics, signaling and autophagy. Biochimica et Biophysica Acta (BBA) - Biomembranes. 2006;1758(12):1864–84. doi: 10.1016/j.bbamem.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 156.Ordóñez-Gutiérrez L, et al. Dihydroceramide Desaturase 1 Inhibitors Reduce Amyloid-β Levels in Primary Neurons from an Alzheimer’s Disease Transgenic Model. Pharm Res. 2018;35(3):49. doi: 10.1007/s11095-017-2312-2. [DOI] [PubMed] [Google Scholar]
- 157.Signorelli P, et al. Dihydroceramide intracellular increase in response to resveratrol treatment mediates autophagy in gastric cancer cells. Cancer Lett. 2009;282(2):238–43. doi: 10.1016/j.canlet.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 158.Gilmore TD, Herscovitch M. Inhibitors of NF-κB signaling: 785 and counting. Oncogene. 2006;25(51):6887–99. doi: 10.1038/sj.onc.1209982. [DOI] [PubMed] [Google Scholar]
- 159.Liu Y, Li Q, Zhou L, Xie N, Nice EC, Zhang H, Huang C, Lei Y. Cancer drug resistance: Redox resetting renders a way. Oncotarget. 2016;7(27):42740–61. doi: 10.18632/oncotarget.8600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kartal-Yandim M, Adan-Gokbulut A, Baran Y. Molecular mechanisms of drug resistance and its reversal in cancer. Crit Rev Biotechnol. 2016;36(4):716–26. doi: 10.3109/07388551.2015.1015957. [DOI] [PubMed] [Google Scholar]
- 161.Abdallah HM, et al. P-glycoprotein inhibitors of natural origin as potential tumor chemo-sensitizers: A review. J Adv Res. 2015;6(1):45–62. doi: 10.1016/j.jare.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Nieth C, et al. Modulation of the classical multidrug resistance (MDR) phenotype by RNA interference (RNAi) FEBS Lett. 2003;545(2):144–50. doi: 10.1016/S0014-5793(03)00523-4. [DOI] [PubMed] [Google Scholar]
- 163.Wu C-P, Ambudkar SV. The pharmacological impact of ATP-binding cassette drug transporters on vemurafenib-based therapy. Acta Pharmaceutica Sinica B. 2014;4(2):105–11. doi: 10.1016/j.apsb.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kapse-Mistry S, et al., Nanodrug delivery in reversing multidrug resistance in cancer cells. Frontiers in Pharmacology, 2014. 5(159). [DOI] [PMC free article] [PubMed]
- 165.Borska S, et al. In vitro effect of quercetin on human gastric carcinoma: Targeting cancer cells death and MDR. Food Chem Toxicol. 2012;50(9):3375–83. doi: 10.1016/j.fct.2012.06.035. [DOI] [PubMed] [Google Scholar]
- 166.Subburayan K, Hoti S. Resveratrol Modulates Expression of ABC Transporters in Non-Small Lung Cancer Cells: Molecular Docking and Gene Expression Studies. Journal of Cancer Science and Therapy, 2014. 6.
- 167.Belvedere R, et al. Annexin A1 contributes to pancreatic cancer cell phenotype, behaviour and metastatic potential independently of Formyl Peptide Receptor pathway. Sci Rep. 2016;6(1):29660. doi: 10.1038/srep29660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Gao Y, et al. Differential expression of ANXA1 in benign human gastrointestinal tissues and cancers. BMC Cancer. 2014;14(1):520. doi: 10.1186/1471-2407-14-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Biran H, Sulkes A, Biran S, 5-Fluorouracil, Doxorubicin (Adriamycin) and Mitomycin-C (FAM) in Advanced Gastric Cancer: Observations on Response, Patient Characteristics, Myelosuppression and Delivered Dosage. Oncology, 1989. 46(2): p. 83–87. [DOI] [PubMed]
- 170.Mieszala K, et al. Expression of genes and proteins of multidrug resistance in gastric cancer cells treated with resveratrol. Oncol Lett. 2018;15(4):5825–32. doi: 10.3892/ol.2018.8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Mieszala K, et al. Expression of genes and proteins of multidrug resistance in gastric cancer cells treated with resveratrol. Oncology letters. 2018;15(4):5825–32. doi: 10.3892/ol.2018.8022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.MacDonald JS, Woolley SP, Smythe PV, Ueno T, Hoth W, Smith D, Boiron F, Gisselbrecht M, Brunet C, Lagarde R C, 5-Fluorouracil, Doxorubicin, and Mitomycin (FAM) Combination Chemotherapy for Advanced Gastric Cancer. Annals of Internal Medicine, 1980. 93(4): p. 533–536. [DOI] [PubMed]
- 173.Xu J, et al. Resveratrol reverses Doxorubicin resistance by inhibiting epithelial-mesenchymal transition (EMT) through modulating PTEN/Akt signaling pathway in gastric cancer. Journal of Experimental Clinical Cancer Research. 2017;36(1):19. doi: 10.1186/s13046-016-0487-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Choi JY, et al. PEGylated lipid bilayer-supported mesoporous silica nanoparticle composite for synergistic co-delivery of axitinib and celastrol in multi-targeted cancer therapy. Acta Biomater. 2016;39:94–105. doi: 10.1016/j.actbio.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 175.Choi JY, et al. PEGylated polyaminoacid-capped mesoporous silica nanoparticles for mitochondria-targeted delivery of celastrol in solid tumors. Colloids Surf B. 2018;165:56–66. doi: 10.1016/j.colsurfb.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 176.Kasinski AL, Slack FJ. MicroRNAs en route to the clinic: progress in validating and targeting microRNAs for cancer therapy. Nat Rev Cancer. 2011;11(12):849–64. doi: 10.1038/nrc3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hu Y, et al. Anti-miRNA21 and resveratrol-loaded polysaccharide-based mesoporous silica nanoparticle for synergistic activity in gastric carcinoma. J Drug Target. 2019;27(10):1135–43. doi: 10.1080/1061186X.2019.1610766. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.