Abstract
Objective
The COVID-19 pandemic is demanding for occupational medicine and for public health. As healthcare workers (HCWs) fight impacts of SARS-CoV-2 on front lines, we must create safe work environments through comprehensive risk assessments, evaluation and effective implementation of counter-measures. We ask: ‘What does current literature report on health risks at workplaces regarding COVID-19?’ and ‘What do current studies report on the effectiveness of enacted preventative recommendations?’
Methods
As a snapshot of early HCW research, on 26 April 2020, we conducted a rapid systematic literature search in three databases (PubMed, Web of Science and PsycInfo) for COVID-19-related health outcomes and preventive measures in healthcare-associated workplaces.
Results
27 studies were identified as relevant for exploring the risk of infection, 11 studies evaluated preventive measures. The studies described that SARS-CoV-2 impacts significantly on HCW’s health and well-being, not only through infections (n=6), but also from a mental health perspective (n=16). 4 studies reported indirect risks such as skin injuries, one study described headaches to result from the use of personal protective equipment. Few studies provided information on the effectiveness of prevention strategies. Overall, most studies on health risks as well as on the effectiveness of preventive measures were of a moderate-to-low quality; this was mainly due to limitations in study design, imprecise exposure and outcome assessments.
Conclusions
Due to widespread exposure of HCW to SARS-CoV-2, workplaces in healthcare must be as safe as possible. Information from HCW can provide valuable insights into how infections spread, into direct and indirect health effects and into how effectively counter-measures mitigate adverse health outcomes. However, available research disallows to judge which counter-measure(s) of a current ‘mix’ should be prioritised for HCW. To arrive at evidence-based cost-effective prevention strategies, more well-conceived studies on the effectiveness of counter-measures are needed.
Keywords: public health, epidemiology, occupational & industrial medicine
Strengths and limitations of this study.
Empirical information for timely use and decision-making was assessed in an early phase of the COVID-19 pandemic and synthesised in a ‘real-time’ manner.
The review refers to workplaces of high relevance for individuals and public health.
We developed recommendations for further epidemiological studies that could aid understanding and controlling the pandemic.
The literature focuses on the first phase (until 26 April 2020) of the pandemic.
Introduction
Challenges due to the SARS-CoV-2/COVID-19 pandemic are unprecedented in scope and scale. After massive ‘lockdowns’, numerous countries are choosing careful ways back to former life and work. To support this, occupational medicine can play a pivotal role:
Getting back to work is highly relevant for economic prosperity, individual well-being and wealth. Equally clearly, workplaces with countless human contacts bear the risk for case clusters. Therefore, expertise and insights from occupational medicine should be applied to create workplaces that are as safe as possible and to mitigate adverse health effects caused by a recession.1
Healthcare workers (HCWs)—as important actors of the critical infrastructure—are under considerable risk of infection and other diseases. Within the first months of the pandemic (until early March), 3300 HCWs in China were described as infected, in Italy about 20% of responding HCW.2 Because of the risks for HCW, in our review, we ask ‘What is reported regarding health risks at workplaces concerning COVID-19?’ and ‘What do current studies report on the effectiveness of enacted preventative measures?’. We further ask and discuss ‘What can we recommend from completed COVID-19 research on workplaces for ongoing and future epidemiology?’
Methods
On 26 April 2020, we conducted a rapid systematic literature search using three scientific databases (PubMed, Web of Science and PsycInfo). For PubMed we used the following search term: ((“Workforce”[Mesh] OR worker* OR employee* OR staff OR workforce OR labourer OR “Occupational Medicine”[Mesh] OR “Occupational Health” [Mesh] OR “Occupational Diseases”[Mesh] OR “Workplace”[Mesh] OR “occupational medicine“ OR “occupational health” OR workplace OR “occupational disease” OR “occupation“) AND (“COVID-19” OR “COVID-19” OR “severe acute respiratory syndrome coronavirus 2” OR “novel coronavirus” OR “new coronavirus” OR “COVID-19 pandemic” OR “wuhan coronavirus” OR SARS-CoV-2 OR “2019-nCoV disease”)). This search term was adapted for the other databases.
Inclusion and exclusion criteria
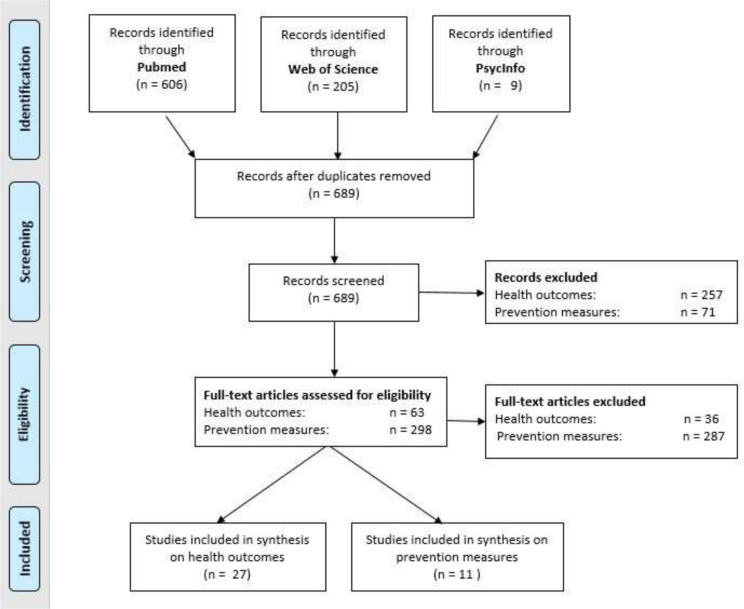
We screened identified relevant studies according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (see figure 1). We included publications focusing on COVID-19-related physical and psychological health outcomes in HCW or studies that investigated prevention measures regarding the risk through COVID-19. Studies focusing on other occupations, not presenting original data, focusing on coronaviruses other than SARS-CoV-2 or on diagnostics, therapies only were excluded. We further excluded articles exploring virus characteristics or transmissibility and those not published in English or German.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart of the included studies.
Quality appraisal
We critically appraised all original studies fulfilling the review’s criteria. To assess quality of quantitative studies, we used the Appraisal Tool for Cross-Sectional Studies (AXIS), the Critical Appraisal Skilss Programm checklist (CASP) for cohort studies, the Joana Briggs Institute (JBI) Critical Appraisal Checklist for case reports and case series and GRADE (Grading of Recommendations, Assessment, Development and Evaluations) for ecological studies. Qualitative studies were appraised by the CASP qualitative checklist. To identify the appropriate checklist, the study designs were evaluated in regards to our study questions. As several studies included various approaches to assess data in addition to investigating staff, our identification process may result in different study designs than stated by the authors. Where possible, overall scores were calculated or categorical scores were presented (see tables 1 and 2).
Table 1.
Studies included for risk of infection, mental health, skin injuries and headaches
| Author and year | Study design | Country | Exposure | Outcome/ evaluation tool | Main findings | Quality assessment |
| Infection | ||||||
| Centers for Disease Control and Prevention, USA, 20203 | Cross-sectional, quantitative | USA | Laboratory confirmed contact with patients with COVID-19, n=9289 (Healthcare personnel) | Infection prevalence among HCW, (assessed through laboratory testing) | As of 9 April, 19% of all infected COVID-19 cases in the USA were HCW, median age was 42 years, death occurred more often among HCW aged >65, hospitalisation rate among HCW 8%–10% | AXIS: 12/20 (some items not applicable due to descriptive census-like study) |
| Chu et al, 20204 | Retrospective case series, quantitative | China | Working in emergency departments versus low-risk departments (non-emergency and technology departments), n=54 | Infection and severity of disease (assessed through laboratory testing and clinical diagnosis) | Much lower incidence of infection among HCW from emergency departments than from other departments (emergency department 3.7% versus other department 72.2%); severe cases were significantly younger than common cases | JBI: 8-9/10 |
| Li et al, 20205 | Report, Editorial (retrospective fatality analysis based on official report data) |
China | No information on exposure assessment, n=24 | Mortality among HCW with COVID-19 | As of 16 March, 13 out of 24 (54.2%) HCW died from COVID-19, other causes for death were traffic injuries and sudden death | N/A |
| McMichael et al, 20206 | Case report, quantitative | USA | Contact to patients with COVID-19 in a long-term care facility, n=167 | Infection and hospitalisation rates among staff members, residents and visitors (assessed through laboratory testing) | As of 18 March, 50 out of 167 confirmed cases were HCW, of whom 6% were hospitalised; indicated lacking PPE adherence and unfamiliarity with infection control measures | JBI: 7/8 |
| Ran et al, 20207 | Retrospective cohort study, quantitative | China | Working in a high-risk department versus low-risk department in one hospital, n=72 | Infection risk (assessed through laboratory testing) | HCW in high-risk departments are at higher risk for COVID-19 than those of low-risk departments due to longer duty hours and suboptimal hand hygiene | CASP: 5/13 |
| Zhan et al 20208 | Report, Editorial | China | – | – | As of 24 February, 4.4% of confirmed COVID-19 cases were HCW. As of 3 April, 23 out of 3387 HCW in China had died from COVID-19 |
N/A |
| Mental health | ||||||
| Cao et al, 20209 | Qualitative study, Editorial | China | Direct exposure to COVID-19 through work in a fever clinic (doctors, nurses, clinical technicians), n=37 | Assessment of physical and psychological burden through interviews | HCW indicated high stress load, overworking, sleep problems and nervousness over own and family members’ infection risk, concerns over shortage of medical supplies, overall mild bodily discomfort such as tiredness, throat pain, back pain headaches | CASP (no: n=7, yes: n=2) |
| Chen et al, 202010 | Cross-sectional, quantitative, Editorial | China | High exposure versus non or low exposure to patients with COVID-19, n=105 | Depression, anxiety (assessed through SDS, SAS) | Symptoms of depression accompanied by anxiety was significantly higher in high-exposure group; no difference when depression or anxiety were considered separately | AXIS: 10/20 |
| Chew et al, 202011 | Cross-sectional, quantitative | Singapore and India | Exposure to SARS-CoV-2 not directly assessed, correlation between physical and psychological symptoms during COVID-19 outbreak, n=906 | Depression, anxiety and distress, PTSD (assessed through DASS-21, IES-R) and physical symptoms | Headache most commonly reported, participants who had experienced physical symptoms in the preceding month were more likely to screen positive for depression, anxiety and stress, PTSD | AXIS: 13/20 |
| Huang and Zhao, 202012 | Cross-sectional, quantitative | China | Comparison between several occupational groups, n=7236 | Depression, anxiety, sleep quality (assessed through CES-D, GAD-7, PSQI) | Compared with other occupational groups, HCW had a higher prevalence of sleep disturbances, no difference in depression and anxiety | AXIS: 14/20 |
| Kang et al, 202013 | Cross-sectional, quantitative | China | High-risk versus low-risk hospital departments, n=994 | Depression, anxiety, insomnia, distress (assessed through PHQ-9, GAD-7, ISI, IES-R) | Staff with fewer contact to patients with COVID-19 showed less severe mental health issues, a higher degree of distress was associated with a more extensive exposure to the virus | AXIS: 13/20 |
| Lai et al, 202014 | Cross-sectional, quantitative | China | Inside versus outside Wuhan and Hubei (high-risk region vs low-risk region), n=1257 | Depression, anxiety, insomnia, distress (assessed through PHQ-9, GAD-7, ISI, IES-R) | Those working in Wuhan reported more severe mental health outcomes than other HCW | AXIS: 15/20 |
| Li et al, 202015 | Cross-sectional, quantitative | China | Front line versus non-front line (high risk vs low risk), n=1266 | Vicarious traumatisation (assessed through vicarious traumatisation scale) | Non-front-line nurses had significantly higher scores in vicarious traumatisation than front-line nurses | AXIS: 11/20 |
| Liu, et al, 202016 | Cross-sectional, quantitative | China | Front-line versus non front-line nurses and doctors (high risk vs low risk), n=4679 | Psychological stress, anxiety, depression (assessed through SRQ-20, SAS, SDS) | Doctors and nurses from high-risk departments, those who live mostly without family members, those who had previous experience in treatment of infectious disease have higher scores for all mental health outcomes; younger age and higher professional degree (doctors) had lower risk of mental health problems | AXIS: 16/20 |
| Lu et al, 202017 | Cross-sectional, quantitative | China | Medical workers versus administrative staff and subgroup analysis of clinical staff (high-risk vs low-risk clinical staff), n=2299 | Fear, anxiety, depression (assessed through NRS, HAMA, HAMD) | No significant difference in depression in medical staff compared with administrative staff, subgroup analysis: staff in high-risk department showed significantly greater fear, depressive symptoms, and anxiety compared with low-risk groups | AXIS: 14/20 |
| Mo et al, 202018 | Cross-sectional, quantitative | China | Exposure to SARS-CoV-2 not directly assessed, correlation between stress and anxiety, n=180 | Stress and anxiety (assessed through SOS, SAS) | The higher the stress load, the higher the anxiety among nurses; working long hours, being an only child, anxiety were main factors affecting nurse stress | AXIS: 10/20 |
| Sun et al, 202019 | Qualitative study | China | Direct exposure to COVID-19 through work on a negative pressure ward, n=20 | Interview about emotions, coping styles, personal growth, positive emotions during the pandemic | At the beginning of the outbreak, the participants were mainly concerned over unknown conditions of patients, severe emergencies and patients’ psychological state, a few developed symptoms of depression and isolated themselves. Over time, the nurses developed coping strategies to deal with stress and indicated a feeling of personal growth under pressure. After 1 week positive emotions prevailed in 70% of nurses. | CASP (no: n=2, yes: n=8) |
| Tan et al, 202020 | Cross-sectional, quantitative | Singapore | Medical versus non-medical staff (high risk vs low risk), n=470 | Depression, anxiety, stress (assessed through DASS-21, IES-R) | Anxiety and stress were higher in non-medical staff | AXIS:12/20 |
| Wu et al, 202021 | Cross-sectional, quantitative | China | Medical staff versus non-medical staff (college students); inside versus outside Wuhan (high risk vs low risk), n=4268 |
Psychological stress (assessed via piloted questionnaire) | Positive exposure effect: in all provinces of China, medical staff scored higher in psychological stress than college students; medical staff in Wuhan scored higher than staff outside Wuhan | AXIS: 9/20 |
| Xiao et al, 202022 | Cross-sectional, quantitative | China | Exposure to SARS-CoV-2 not directly assessed, n=180 | Anxiety, Self-efficacy, Stress, Sleep (assessed through SAS, GSES, SASR, PSQI) | During the COVID-19 pandemic, social support reduced stress and anxiety and increased self-efficacy in medical staff, no significant effect on sleep quality | AXIS: 10/20 |
| Xu 202023 | Cross-sectional, quantitative, Editorial | China | Outbreak versus non-outbreak period (high vs low exposure), n=120 | Depression, anxiety, anxiety dreams (assessed via scoring system and SF-36) | All endpoints were significantly higher in outbreak period compared with non-outbreak period | AXIS: 5-6/20 |
| Zhang et al, 202024 | Cross-sectional, quantitative | China | Medical versus non-medical staff (high risk vs low risk), n=2182 | Insomnia, somatisation, obsessive compulsive disorder, anxiety, anxiety and depression (assessed through ISI, SCL-90R, PHQ-4) | Medical workers had a higher prevalence for all mental health disorders except for phobic anxiety, having an organic disease was independently associated with mental health outcomes | AXIS: 11/20 |
| Headaches | ||||||
| Ong et al, 202029 | Cross-sectional, quantitative | Singapore | Frequent use of PPE due to SARS-CoV-2 exposure, n=158 | PPE-related headaches (assessed through self-administered questionnaire) | 81.0% of respondents developed de novo PPE-associated headaches. A pre-existing primary headache diagnosis and combined PPE usage for >4 hour per day were independently associated with de novo PPE-associated headaches. | AXIS: 15/20 |
| Skin injuries | ||||||
| Gheisari et al, 202025 | Report, Editorial | Iran | Frequent use of PPE due to SARS-CoV-2 exposure | PPE-related skin injuries | Respirator masks were found to provoke occupational dermatoses, acne, skin irritation, contact dermatitis, allergies, pigmentation, pressure damage; goggles were associated with frictional erosions, pressure damage, xerosis, skin reactions on nasal bridge including; gowns were linked to contact dermatitis, itching | N/A |
| Jiang et al, 202026 | Cross-sectional, quantitative | China | Frequent use of PPE due to SARS-CoV-2 exposure, n=4308 | PPE-related skin injuries (assessed through self-administered questionnaire) | Overall prevalence of skin injuries 42.8% (mostly device-related pressure injuries, moist associated skin damage and skin tear). Daily wearing time of >4 hour, high-grade PPE (PPE 3), sweating and male sex were associated with skin injuries | AXIS: 14-15/20 |
| Lan et al, 202027 | Cross-sectional, quantitative, Editorial | China | Frequent use of PPE due to SARS-CoV-2 exposure, n=542 | PPE-related skin injuries (self-administered questionnaire) | Prevalence of skin injuries among first-line HCW was 97%, most affected areas were nasal bridge, cheeks, hands and forehead, wearing time of N95 respirators>6 hour was positively correlated with skin damages, frequent hand hygiene (>10 times) was associated with hand skin damage | AXIS: 6/20 |
| Lin et al, 202028 | Cross-sectional, quantitative, Editorial | China | Frequent use of PPE due to SARS-CoV-2 exposure, n=376 | PPE-related skin injuries (assessed through self-administered questionnaire) | Skin on hands, cheeks, nasal bridge and auricular areas most affected by dryness, maceration, erythema; duration of wearing PPE, frequency of hand washing significantly associated with adverse skin reactions | AXIS: 8-9/20 |
AXIS, The Appraisal Tool for Cross-Sectional Studies; CASP, Critical Appraisal Skills Programme; CES-D, Centre for Epidemiology Scale for Depression; DASS-21, Depression Anxiety and Stress Scale; GAD-7, Generalized Anxiety Disorder-7; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; GSES, General Self-Efficacy Scale; HAMA, Hamilton Anxiety Rating Scale; HAMD, Hamilton Rating Scale for Depression; HCW, healthcare worker; IES-R, Impact of Event Scale; ISI, Insomnia severity Index; JBI, Joana Briggs Institute; N/A, not applicable (N/A in quality assessment was used for articles with no clear study design such as reports or editorials); NRS, Numeric rating scale; PHQ, Patient Health Questionnaire; PSQI, Pittsburgh Sleep Quality Index; PTSD, Post-traumatic stress disorder; SAS, Self-rating anxiety scale; SASR, Stanford Acute Stress Reaction Questionnaire; SCL-90-R, Symptom Checklist 90- Standard; SDS, Self-rating depression scale; SF-36, Short Form Health 36; SOS, Stress Overload Scale; SRQ-20, Self Reporting Questionnaire 20-Item.
Table 2.
Studies included for preventive measures
| Author and year | Study design | Country | Exposure/ prevention measure | Outcome/ evaluation tool |
Main findings | Quality assessment |
| Cao et al, 20209 | Qualitative interviews | China | HCW (n=37)/ Coping strategies as video chats or telephone calls with family and friends |
Interview | Psychological support may help buffer negative impact on stress. | CASP (No: n=7, Yes: n=2) |
| Chen et al, 202039 | Qualitative interviews | China | HCW (n=13), stress, influence on mental health/ psychological intervention medical team, hotline | Interview | Not scared to get infected, help for resting, skills to cope with patients’ anxiety and PPE shortage needed | CASP (No: n=5, Yes: n=2, can’t tell: n=2) |
| Chen et al, 202034 | Ecological study | China | Caesarean delivery (n=17)/ appropriate PPE (N95 masks, goggles, protective suits, disposable caps, rubber gloves), if endotracheal intubation air-purifying respirator; negative operating room, | RT-PCR | No medical staff involved in operation were infected | GRADE: very low |
| Htun et al, 202036 | Cross-sectional study | Singapore | Hospital overall (staff n=10 583)/ Fever and sickness surveillance for staff; risk-based PPE; enhanced surveillance for unwell staff |
Mixed (clinical assessment, swabs for PCR) | No infection with COVID-19 | AXIS: positive aspect n=10, negative n=4, don’t know n=6 |
| Huang et al, 202035 | Ecological study | China | Nurses, 35 confirmed, 260 suspected cases/ PPE (hat, respirator, inner gloves, eye mask, protective clothing. Shoe covers, isolation gowns, outer gloves, face shield), hand hygiene, ward disinfection, medical waste management, sterilisation of patient care devices, management of occupational exposure. Teaching. Shift schedule evaluated; psychological counselling |
Not specified | Zero infection rate in nurses | GRADE: very low |
| Huang et al, 202030 | Ecological study | China | Radiology department, 3083 suspected or confirmed COVID-19 patients/ Reconfiguring of the department, PPE (protective clothing, surgical cap, N95 mask, gloves, face shields, goggles), training, donning and doffing under supervision, strategic planning of examination procedures | Clinical symptoms | None of the staff became infected. | GRADE: very low |
| Kabesch et al, 202038 | Ecological study | Germany | Outbreak scenario, midwife → colleagues / Face masks, social distancing in cafeteria and break rooms, on site visits hygiene experts, staff training, transparent, timely and direct communication, testing all symptomatic employees |
Laboratory test for symptomatic staff | Successful containment of the outbreak within 3 weeks, 36 staff members tested positive | GRADE: very low |
| Malik 202033 | Ecological study | Pakistan | Admission of a COVID-19 positive patient to the ICU/ HCW with N95 or surgical masks |
PCR | All HCW (n=34) tested negative for COVID-19 | GRADE: low |
| Ng et al, 202032 | Ecological study | Singapore | one patient with pneumonia/ HCW (n=41) exposed during aerosol-generating procedures |
Clinical monitoring and PCR | No HCW infected | GRADE: low |
| Wee et al, 202031 | Ecological study | Singapore | Emergency department, PCR tests for all patients with respiratory syndromes, n=70 patients tested positive/ PPE risk stratified |
PCR testing, extensive surveillance | No nosocomial transmission | GRADE: low |
| Zhu et al et al, 202037 | Ecological study | China | one patient with endonasal adenoma resection, general care and operation/ no prevention measures initially before confirmed infection | Diagnosis of infection not specified. | four nurses without prevention measures (and 10 persons without contact to the patient) got infected, none of the persons in the operation room or under specific prevention got infected. | GRADE: very low |
AXIS, Appraisal Tool for Cross-Sectional Studies; CASP, Critical Appraisal Skills Programme; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; HCW, healthcare worker.
Patient and public involvement
No patient involved.
Results
Our literature search identified 820 publications; after removing duplicates, 689 were screened for title and abstract. According to our research questions, JM reviewed studies on workplace-associated health outcomes associated with SARS-CoV-2. JVG reviewed studies on implemented prevention measures in healthcare settings and their implications for HCW’s health (see PRISMA flowchart, figure 1).
Health risks at healthcare workplaces
Of 27 included studies, 6 provided information on the risk of infection,3–8 16 on mental health,9–24 4 on skin injuries associated with PPE25–28 and 1 on resulting headaches29 (see tables 1 and 2).
Infection
Due to frequent contact with infected people, HCW’s own infection and the virus transmission to others is an important concern. Six3–8 out of twenty-seven included studies on health outcomes reported on the prevalence of SARS-CoV-2 infection as well as on COVID-19-related morbidity and mortality among HCW. In all six studies, exposure was assessed based on known contact with patients with SARS-CoV-2 positive and infection was diagnosed through laboratory tests (reverse transcription PCR).
According to Zhan et al who refers to statistics of the National Health Commission of People’s Republic of China, as of 24 February, 4.4% of the infected people in China (3387 of 77,262 patients with COVID-19) were HCW.8 A cross-sectional study conducted by the US Centers for Disease Control and Prevention (CDC) revealed that as of 9 April, HCW accounted for 11% of all reported cases in the USA.3
Two studies provided information on hospitalisation rates.3 6 For instance, in a long-term care facility in the USA, McMichael et al observed that 6% of 50 infected nursing staff were hospitalised,6 which is similar to a prevalence of 8% stated by the CDC.3 More specifically, in a case series Chu et al observed more cases of severe and critical illness among younger HCW than in older colleagues who were hospitalised due to COVID-19.4
Two studies provided information on HCW’s mortality.5 8 According to Zhan et al as of 3 April, 23 out of 3387 (~0.7%) COVID-19-positive HCW in China had died from the infection.8 Additionally, in their retrospective fatality analysis Li et al reported that as of 16 March, 13 out of 24 fatalities among HCW (54.2 %) were attributable to COVID-19 and most cases were recorded in Hubei province or Wuhan.5
Among the reasons for HCW’s infection, shortage of PPE and insufficient knowledge and training in infection control measures were reported to be most relevant.4 6 Chu et al pointed out that normal wards evinced a disproportionally high number of infected HCW compared with first-line departments (3.7% from first-line departments vs 72.2% from non-first-line departments) that were prioritised over second-line departments in terms of PPE allocation.4 Moreover, McMichael et al reported on disease spreading in a US-American long-term care facility, where staff worked while being symptomatic and moved between several facilities indicating lacking knowledge about infection control and containment measures.6
The high importance of protective measures was also emphasised in a retrospective cohort study by Ran et al who found that unqualified hand washing, suboptimal hand hygiene before and after patient contact and improper PPE increased the risk of infection by 2.64 (95% CI: 1.04 to 6.71), 3.10 (95% CI: 1.43 to 6.73), 2.43 (95% CI: 1.34 to 4.39) and 2.82 (95% CI: 1.11 to 7.18), respectively.7 The study also found that longer working hours, that is, longer exposure to SARS-CoV-2, was positively correlated with a higher proportion of infection.7
Mental health
Sixteen9–24 out of the twenty-seven included studies reported on mental health problems, four investigated PPE-related skin injuries25–28 and one reported on headaches associated with frequent PPE use.29
Most studies found that the exposure to SARS-CoV-2 was positively correlated with mental health problems.10 12–14 16 17 21 23 24 Depression, anxiety and stress were the most commonly assessed disorders showing a significantly higher prevalence in HCW in high-risk departments or high-risk regions (Wuhan, Hubei province) compared with medical staff in low-risk departments, non-clinical staff or staff in low-risk regions.10 11 13 14 16 17 19 23 24
Factors contributing to psychical exhaustion and development of mental illness were concerns over self-infection and infection of relatives due to insufficient protection, worry about patients, helplessness, unfamiliarity with infection control measures, overworking and traumatising events at work, to name but a few.9 15 17 19
More specifically, Kang et al indicated that the severity of psychological disturbances increased with the frequency of contacts to patients with COVID-19.13 A study by Huang et al compared different occupational groups during the pandemic and revealed that HCWs were more likely to develop sleep disturbances than other workers whereas no difference in prevalence of depression or anxiety was found.12
In contrast, Tan et al reported higher scores of anxiety and stress among non-medical workers (allied HCW, technicians etc) compared with medical workers.20 Moreover, a similar direction of effect was found by Li et al indicating that non-front-line nurses without any patient contact had significantly higher vicarious traumatisation scores than front-line nurses.15
Furthermore, a qualitative interview study by Sun et al showed that attitudes and feelings changed over time.19 They observed that front-line nurses experienced a high degree of helplessness and anxiety at the beginning of the pandemic, but could transform their negative emotions into feelings of higher professional identity and responsibility and personal growth. They further indicated that they felt grateful for the support from colleagues and family members.19
The importance of social support was demonstrated by Xiao et al.22 The authors highlighted a potentially mitigating effect on anxiety and stress and showed that social support improved HCW’s self-efficacy.22 Likewise, nurses in Sun et al.’s study emphasised the importance of support by their families and colleagues.19 Moreover, Mo et al identified that social characteristics such as being the only child could have a predisposing effect for the development of stress.18
Furthermore, underlying organic diseases were associated with developing mental health disorders including insomnia, anxiety, depression, obsessive–compulsive disorder, somatisation, stress and post-traumatic stress disorder (PTSD).11 24
Health effects through prevention measures
In a cross-sectional study, Ong et al explored the prevalence of de novo PPE-related headaches among medical workers from different high-risk areas of a tertiary health centre in Singapore.29 Data from a self-administered questionnaire revealed that 81% of the 158 respondents suffered from de-novo headaches when wearing N95 respirators or eye protection. The chance of developing PPE-related headaches increased significantly for those with pre-existing headaches (OR 4.20; 95% CI: 1.48 to 15.4) and for those who used PPE for more than 4 hours per day (OR 3.91; 95% CI: 1.35 to 11.31).29
Moreover, PPE-related skin damages were evaluated in four studies.25–28 Lin et al showed a positive correlation between self-perceived adverse skin reactions (such as dryness, erythema, maceration mostly on hands, cheeks and the nasal bridge) and the duration of wearing PPE (>6 hour).28 The prevalence of skin irritation was reported to be 74.5%.28 Furthermore, Gheisari et al pointed out the most common adverse skin effects (dermatoses, acne, skin irritation, frictional and pressure erosions) associated with goggles and respirator masks.25 Lan et al found that 97% of HCW suffered from some sort of skin damages, especially dryness and desquamation on the forehead and nasal bridge as a result of enhanced hygienic and infection control measures.27 Wearing N95 respirators for a period longer than 6 hour doubled the risk for facial skin lesions (OR 2.02; 95% CI: 1.35 to 3.01). The authors further observed that frequent hand hygiene (>10 times per day) may increase the risk of skin damage twofold, (OR 2.17; 95% CI: 1.38 to 3.43).27 Similarly, a large multicentre cross-sectional study performed by Jiang et al found an overall prevalence of skin injuries of 42.8%, involving pressure-related and moisture-related skin issues as well as skin tear. The prevalence of skin injuries was found to be higher when daily wearing time exceeded 4 hours and when high-grade PPE (ie, PPE3) was used.26
Effectiveness of enacted preventive measures
Only nine studies30–38 focused on evaluating the effectiveness of implemented preventive strategies regarding risk of infection, all of which were case reports or case series (see table 2). The studies observed operative procedures34 37 as well as general care and diagnostics.30–33 Infection was assessed by laboratory testing or clinical diagnosis of COVID-19.30 The number of investigated patients ranged from 132 33 37 to 308.30
Most of the studies reported zero staff infections,30–36 in one study four nurses who contacted a patient without protection (before quarantine) became infected while there was no transmission for staff members using PPE (after the patient’s confirmed infection).37 Malik et al suggested that surgical masks may be as effective as N95 masks, but further studies were needed to confirm this.33 However, in most studies the enacted preventive measures were complex and do not allow deducing the effectiveness of single measures.
Kabesch et al described how rigorous testing for SARS-CoV-2 and targeted self-isolating of HCWs in addition to improved hygienic measures and consequent use of surgical face masks could stop a COVID-19 outbreak in a large maternity and perinatal centre in Germany. While maintaining the clinical services, the virus was stopped within 3 weeks38.
Measures concerning mental health were evaluated in two studies.9 39 Concerning the effectiveness of supporting mental health, in qualitative interviews (n=13) in a tertiary general hospital in Beijing, communication with colleagues, family members or psychologists was described as being most helpful for most workers.9 Monitoring HCW in a Chinese hospital who received psychological support revealed that they would particularly appreciate designated resting areas and sufficient protection supply as well as the acquisition of necessary skills to manage patients’ anxiety.39
Quality assessment
Overall, most studies on health risks as well as on the effectiveness of preventive measures were of a moderate-to-low quality mainly due to limitations in study design, imprecise exposure and outcome assessments. Hence, selection, misclassification and information bias need to be taken into account when interpreting the findings (see tables 1 and 2 for the studies’ quality scores).
Discussion
Currently, and presumably in the near future, we will have to cope with enormous challenges due to COVID-19. HCW at the front lines are under particular risk. In times when numerous preventative measures are taken for HCW, our review asks two questions, deliberately confining our evidence search to publications until 26 April 2020: ‘What is reported regarding health risks at workplaces concerning COVID-19?’ and ‘What do current studies report on the effectiveness of enacted preventative recommendations?’ We focus on a limited time period to identify effective evidence-based responses, on the one hand, or lack of studies into the effects of measures to protect HCW, on the other at an early stage of the pandemic. Answering our study question in ‘real time’ is important as we need to know—and apply—‘what’ does protect ‘whom’ effectively or otherwise instigate much-needed studies seeking such evidence.
Safety at healthcare workplaces
Among workplace-associated risks through SARS-CoV-2, virus transmission seems to be the biggest concern. However, robust data on incidence and prevalence are difficult to obtain due to uncertainty around infection pathways, inconsistent testing modalities within and between countries and varying disease manifestations including the unknown proportions of asymptomatic cases.
In most studies, exposure assessment referred to HCWs’ contact to patients with COVID-19 without specifying the exact contact time and duration. Yet, this is important to consider, as we know that viral shedding and infectivity differ over the course of disease.40 Moreover, a considerable proportion of included studies did not perform a thorough exposure assessment risking biased study findings on infection-related health consequences.
Another aspect to consider is virus transmission through HCW from outside healthcare facilities, which makes containment measures difficult and increases the risk for nosocomial infection.41 Of note, as protective equipment is usually prioritised to high-risk areas (fever clinics, emergency departments), undersupplied second-line departments could become breeding grounds for new infections.4
Beyond infections, the pandemic’s impact on mental health can be significant. Apart from the fear of self-infection and infecting others, high work pressure, changing relationships between HCW and patients, and possible stigmatisation in society42 43 may have detrimental effects on HCW’s psychological stability. While front-line HCW seem to be at highest risk, impacts on second line and non-clinical staff should not be underestimated. Since front-line HCW generally have better access to mental health support and protective and infection control measures, their psychological resilience is assumed to be higher than in second-line staff.15 20
To understand determinants of mental health disorders, qualitative studies can bring valuable insights. Since recent evidence is predominantly built on cross-sectional studies, it seems to be difficult to quantify the true effect of the ‘SARS-CoV-2 challenge’ on mental health, particularly with respect to pre-existing psychological and physical issues. For this review, we found great heterogeneity in self-administered outcome assessment (tables 1 and 2), which likely introduces information bias and complicates comparison of studies. Given both complexity and durability of mental health problems, longitudinal studies are warranted to explore HCWs’ mental and psychological health over time. Moreover, in future studies, mental health disorders such as PTSD may come on the study radar.
Our observations of COVID-19-related mental health outcomes were consistent with a recent systematic review and meta-analysis on the prevalence of depression, anxiety and insomnia by Pappa et al.44 Our work complements their findings as our broader scope of outcomes and study types adds valuable insight for occupational health research of HCWs in challenging times.
Overall, it becomes clear that healthcare workplaces pose multifaceted challenges to HCWs’ health, which require diligent investigations and a swift implementation of effective precautionary and supportive measures.
Effectiveness of enacted preventive measures
Since the COVID-19 pandemic could last for long(er) and effective medications, improving and developing appropriate protective measures are a must. While many publications describe preventive measures for general and specific healthcare settings, the imbalance regarding—or scarcity of 11—studies into the very effectiveness of a ‘mix’ of enacted measures is striking and needs to be corrected.
Indeed, the dynamic pandemic necessitates flexible adaptation of precautionary measures to take note of rapidly changing recommendations.45 With so many people under risk worldwide, one main objective must be to protect as many of those most under risk as possible. This does certainly not imply to use a maximum prevention in a ‘mix’ of available counter-measures. To the contrary, recommending highest standards of protection can be(come) overuse which has been described as a form of misuse.46 To exemplify, during the last months we all experienced that shortage of prevention measures, especially for PPE47 or laboratory tests,48 can occur. Therefore, when creating effective prevention measures, we also have to consider whether or how long they are available.
Given the obvious need of studies into which counter-measure(s)—alone or in combination—is/are effective, it is unfortunate that only very few studies focus on measuring effectiveness. Moreover, since most studies describe complex prevention concepts, effects of individual measures could hardly be investigated. Finally, the identified case and cross-sectional studies clearly complicate a generalisation of results. Moreover, as the virus is not specific for workplaces, studies should assess the risk of infection in private life, too. Unfortunately, non-workplace associated risks were not explicitly considered.
Cost–Benefit ratio
When discussing prevention measures, possible negative effects have to be considered and investigated. As described above, the PPE’s use can have negative impact on health and well-being. Additionally, the inappropriate use of preventive measures could be a danger49 resulting from a false sense of security due to unawareness which can have a negative impact on workers’ actions and the protective effect of instigated measures. Preferably, before implementing preventive strategies, the effectiveness of the specific measure (the benefit) has to be weighed up against possible risks and inconveniences (the costs).
Acceptance and appropriate use
When interpreting the epidemiological studies, it seems misleading to assume the effectivity of PPE tested under laboratory conditions to be equal to real workplace situations as the PPE’s effectivity depends on the acceptance and actual use by the individual worker. For instance, in a Chinese hospital the use of PPE was investigated, revealing that 100% of the staff used masks, with an accuracy rate of 73.79% only, but the compliance rate of hand hygiene of all staff was limited to 40.78%.50 Reasons for HCWs’ ability and willingness to follow guidelines regarding respiratory infections were investigated in a Cochrane review51: Insecurity on how to handle guidelines, frequently changing guidelines, the resulting additional workload and fatigue, little support, uncomfortable PPE and unwanted effects on the patients (for instance through covering parts of the face by a mask) were described as negative factors. On the other hand, a clear communication, training on how to use PPE and seeing the value of the recommended measures were deemed positive.
It is astonishing that even in hospital settings, PPE is often used inappropriately: In 2019, Herron et al found that only 18% of theatre staff (n=1034) used face masks according to the CDC standard.52 During the current pandemic, Wennmann et al described that HCW in an emergency department of a German University hospital required more PPE training than expected.53
Overall, ignoring the acceptance and appropriate use of preventive measures in epidemiological studies can result in severe information and misclassification bias. As inadequate knowledge is a risk for inappropriate PPE use,54 information and transparent communication is important to improve the acceptance and correct use of prevention measures. Moreover, exaggerated and untargeted measures might decrease workers’ acceptance and willingness to wear PPE as intended with far-reaching consequences for individual and public health.
Suggestions for ongoing research
What could be viewed as a limitation of this review, viz that we are still at an early stage of the pandemic and that our review covers a short period of time only, can be judged as a strength as well: Empirically, we identified lack of evidence for which counter-measure(s) of a current ‘mix’ provides the necessary protection of HCW and should be prioritised in what setting. Material regarding our review questions may now be considered to shape much-needed studies seeking such evidence. Clearly, (some) data for currently missing ‘effect studies’ may be collected now or never.55
Indeed, this review about HCW allows a first ‘real-time’ insight into current research and highlights challenges we face when investigating COVID-19. Due to high exposure to SARS-CoV-2, healthcare workplaces provide ideal conditions to study virus transmission, the effectiveness of prevention measures and findings may be transferred, at least partially, to other workplaces. Against the background of emerging disease clusters in other essential services, as recently observed in military service or in slaughterhouses, lessons learnt in the healthcare sector can be critical for occupational research to prevent further disruptions of everyday life.
However, as demonstrated in this review, high-quality studies from different parts of the world are lacking. Therefore, we do agree with Glasziou that the current phase of the pandemic has generated replicative studies of low methodological quality highlighting the need for well-defined study questions and robust study designs in order to reduce waste in COVID-19 research.56 Moreover, studies from different countries and economical settings are needed to avoid ‘geographical bias’. To achieve this end, multifaceted studies investigating the risk through COVID-19 at healthcare—and other—workplaces should include and consider:
The risk of infection.
The effectiveness of prevention measures.
The availability of prevention measures.
The risks of prevention measures.
The cost–benefit ratio of prevention measures.
The acceptance and appropriate use of prevention measures among workers.
Conclusion
COVID-19 poses severe risks for HCWs’ physical and mental health. While a plethora of prevention measures is currently enacted, we lack informative evaluations of their effectiveness and possible negative consequences. Taken together, available research disallows to judge which counter-measure(s) of a current ‘mix’ should be prioritised at healthcare workplaces. After reviewing hitherto scarce COVID-19-HCW-associated literature, recommendations for effect-based epidemiology to arrive at evidence-based cost-effective counter-measures should be considered when shaping ongoing and future research.
Supplementary Material
Footnotes
Contributors: JVG was involved in creating and conducting the literature search and provided the first draft of this paper. JM was involved in creating and conducting the literature search and drafting the paper. TCE was involved in drafting the paper and supervision of this review.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article. Studies included in this review are presented in tables 1 and 2.
References
- 1.Godderis L, Luyten J. Challenges and opportunities for occupational health and safety after the COVID-19 lockdowns. Occup Environ Med 2020;77:511–2. 10.1136/oemed-2020-106645 [DOI] [PubMed] [Google Scholar]
- 2.The Lancet COVID-19: protecting health-care workers. The Lancet 2020;395:922 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC COVID-19 Response Team Characteristics of Health Care Personnel with COVID-19 - United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:477–81. 10.15585/mmwr.mm6915e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chu J, Yang N, Wei Y, et al. . Clinical characteristics of 54 medical staff with COVID-19: a retrospective study in a single center in Wuhan, China. J Med Virol 2020;92:807–13. 10.1002/jmv.25793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li W, Zhang J, Xiao S. Characteristics of health worker fatality in China during the outbreak of COVID-19 infection. J Infect 2020;81 10.1016/j.jinf.2020.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMichael TM, Currie DW, Clark S, et al. . Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med 2020;382:2005–11. 10.1056/NEJMoa2005412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ran L, Chen X, Wang Y, et al. . Risk factors of healthcare workers with coronavirus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis 2020;71:2218–21. 10.1093/cid/ciaa287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhan M, Qin Y, Xue X, et al. . Death from Covid-19 of 23 health care workers in China. N Engl J Med 2020;382:2267–8. 10.1056/NEJMc2005696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao J, Wei J, Zhu H, et al. . A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary General Hospital in Beijing during the COVID-19 outbreak. Psychother Psychosom 2020;89:252–4. 10.1159/000507453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Zhou H, Zhou Y, et al. . Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res 2020;288:113005. 10.1016/j.psychres.2020.113005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chew NWS, Lee GKH, Tan BYQ, et al. . A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020;88:559–65. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang L, Ma S, Chen M, et al. . Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun 2020;87:11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai J, Ma S, Wang Y, et al. . Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Z, Ge J, Yang M, et al. . Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun 2020;88:916–9. 10.1016/j.bbi.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.ZaH L, Jiang R, et al. . Mental health status of doctors and nurses during COVID-19 epidemic in China, 2020. [Google Scholar]
- 17.Lu W, Wang H, Lin Y, et al. . Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res 2020;288:112936. 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mo Y, Deng L, Zhang L, et al. . Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag 2020;28:1002–9. 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun N, Wei L, Shi S, et al. . A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control 2020;48:592–8. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.BYQ T, Chew NWS, GKH L. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med 2020. 10.7326/M20-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu W, Zhang Y, Wang P, et al. . Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol 2020;92:1962–70. 10.1002/jmv.25914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiao H, Zhang Y, Kong D, et al. . The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 2020;26:e923549. 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu J, Xu Q-H, Wang C-M, et al. . Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res 2020;288:112955. 10.1016/j.psychres.2020.112955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang W-R, Wang K, Yin L, et al. . Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 2020;89:242–50. 10.1159/000507639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gheisari M, Araghi F, Moravvej H, et al. . Skin reactions to non-glove personal protective equipment: an emerging issue in the COVID-19 pandemic. J Eur Acad Dermatol Venereol 2020;34:e297–8. 10.1111/jdv.16492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang Q, Song S, Zhou J, et al. . The prevalence, characteristics, and prevention status of skin injury caused by personal protective equipment among medical staff in fighting COVID-19: a multicenter, cross-sectional study. Advances in Wound Care 2020;9:357–64. 10.1089/wound.2020.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lan J, Song Z, Miao X, et al. . Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol 2020;82:1215–6. 10.1016/j.jaad.2020.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin P, Zhu S, Huang Y, et al. . Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak: a survey in Wuhan and its surrounding regions. Br J Dermatol 2020;183:190–2. 10.1111/bjd.19089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ong JJY, Bharatendu C, Goh Y, et al. . Headaches Associated With Personal Protective Equipment - A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache 2020;60:864–77. 10.1111/head.13811 [DOI] [PubMed] [Google Scholar]
- 30.Huang Z, Zhao S, Li Z, et al. . The battle against coronavirus disease 2019 (COVID-19): emergency management and infection control in a radiology department. J Am Coll Radiol 2020;17:710–6. 10.1016/j.jacr.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wee LE, Fua T-P, Chua YY, et al. . Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med 2020;27:379–87. 10.1111/acem.13984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ng K, Poon BH, Kiat Puar TH, et al. . COVID-19 and the risk to health care workers: a case report. Ann Intern Med 2020;172:766–7. 10.7326/L20-0175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malik T. COVID-19 and the efficacy of different types of respiratory protective equipment used by health care providers in a health care setting. Cureus 2020;12 10.7759/cureus.7621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen R, Zhang Y, Huang L, et al. . Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing cesarean delivery: a case series of 17 patients. Can J Anaesth 2020;67:655–63. 10.1007/s12630-020-01630-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang L, Lin G, Tang L, et al. . Special attention to nurses' protection during the COVID-19 epidemic. Crit Care 2020;24:120. 10.1186/s13054-020-2841-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Htun HL, Lim DW, Kyaw WM, et al. . Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis 2020;71:1947–52. 10.1093/cid/ciaa468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu W, Huang X, Zhao H, et al. . A COVID-19 patient who underwent endonasal endoscopic pituitary adenoma resection: a case report. Neurosurgery 2020;87:E140–6. 10.1093/neuros/nyaa147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kabesch M, Roth S, Brandstetter S, et al. . Successful containment of Covid‐19 outbreak in a large maternity and perinatal center while continuing clinical service. Pediatr Allergy Immunol 2020;31:560–4. 10.1111/pai.13265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen Q, Liang M, Li Y, et al. . Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e15–16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He X, Lau EHY, Wu P, et al. . Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 2020;26:672–5. 10.1038/s41591-020-0869-5 [DOI] [PubMed] [Google Scholar]
- 41.Reusken CB, Buiting A, Bleeker-Rovers C, et al. . Rapid assessment of regional SARS-CoV-2 community transmission through a convenience sample of healthcare workers, the Netherlands, March 2020. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.12.2000334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson AN, Ravaldi C, Scoullar MJL, et al. . Caring for the carers: ensuring the provision of quality maternity care during a global pandemic. Women Birth 2020. 10.1016/j.wombi.2020.03.011. [Epub ahead of print: 08 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr 2020;51:102080. 10.1016/j.ajp.2020.102080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pappa S, Ntella V, Giannakas T, et al. . Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:S0889-1591(20)30845-X. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lancaster EM, Sosa JA, Sammann A, et al. . Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg 2020;230:1064–73. 10.1016/j.jamcollsurg.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cook TM. Personal protective equipment during the COVID-19 pandemic - a narrative review. Anaesthesia 2020;75 10.1111/anae.15071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Delgado D, Wyss Quintana F, Perez G, et al. . Personal safety during the COVID-19 pandemic: realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17082798. [Epub ahead of print: 18 Apr 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coffey S, Moynagh A, Green B, et al. . Changes to management of a non-pandemic illness during the COVID-19 pandemic: case study of invasive management of acute coronary syndrome. N Z Med J 2020;133:101–6. [PubMed] [Google Scholar]
- 49.Bhadelia N. Coronavirus: hospitals must learn from past pandemics. Nature 2020;578:193. 10.1038/d41586-020-00354-4 [DOI] [PubMed] [Google Scholar]
- 50.Xu C, Jin J, Song J, et al. . Application of refined management in prevention and control of the coronavirus disease 2019 epidemic in non-isolated areas of a general Hospital. Int J Nurs Sci 2020;7:143–7. 10.1016/j.ijnss.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Houghton C, Meskell P, Delaney H, et al. . Barriers and facilitators to healthcare workers' adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev 2020;4:Cd013582. 10.1002/14651858.CD013582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Herron JBT, Kuht JA, Hussain AZ, et al. . Do theatre staff use face masks in accordance with the manufacturers' guidelines of use? J Infect Prev 2019;20:99–106. 10.1177/1757177418815551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wennmann DO, Dlugos CP, Hofschröer A, et al. . [Handling of COVID-19 in the emergency department : Field report of the emergency ward of the University Hospital Münster]. Med Klin Intensivmed Notfmed 2020;115:380-387. 10.1007/s00063-020-00693-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang M, Zhou M, Tang F, Wang Y, et al. . Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect 2020;105:183-187. 10.1016/j.jhin.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Erren TC, Lewis P, Shaw DM. The COVID-19 Pandemic: Ethical and Scientific Imperatives for "Natural" Experiments. Circulation 2020;142:309–11. 10.1161/CIRCULATIONAHA.120.048671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Glasziou PP, Sanders S, Hoffmann T. Waste in covid-19 research. BMJ 2020;369:m1847. 10.1136/bmj.m1847 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.