Abstract
Introduction
The API AutosomalDominant AD (ADAD) Colombia Trial is a placebo‐controlled clinical trial of crenezumab in 252 cognitively unimpaired 30 to 60‐year‐old Presenilin 1 (PSEN1) E280A kindred members, including mutation carriers randomized to active treatment or placebo and non‐carriers who receive placebo.
Methods
Of the 252 enrolled, we present data on a total of 242 mutation carriers and non‐carriers matched by age range, excluding data on 10 participants to protect participant confidentiality, genetic status, and trial integrity.
Results
We summarize demographic, clinical, cognitive, and behavioral data from 167 mutation carriers and 75 non‐carriers, 30 to 53 years of age. Carriers were significantly younger than non‐carriers ((mean age ± SD) 37 ± 5 vs 42 ± 6), had significantly lower Mini Mental Status Exam (MMSE) scores (28.8 ± 1.4 vs 29.2 ± 1.0), and had consistently lower memory scores.
Discussion
Although PSEN1 E280A mutation carriers in the Trial are cognitively unimpaired, they have slightly lower MMSE and memory scores than non‐carriers. Their demographic characteristics are representative of the local population.
Keywords: Alzheimer's disease, autosomal‐dominant Alzheimer's disease, baseline data, clinical trial, crenezumab, Alzheimer's Prevention Initiative, preclinical Alzheimer's disease, preclinical, prevention
1. INTRODUCTION
Alzheimer disease (AD) is the most common cause of dementia and poses public health and financial burdens for society. 1 , 2 , 3 Autosomal‐dominant Alzheimer's disease (ADAD) is rare, accounting for up to 1% to 2% of all cases of AD, 4 with symptom onset usually before age 65. 4 , 5 It is caused by mutations in one of three genes: amyloid precursor protein, presenilin 1, or presenilin 2 (APP, PSEN1, or PSEN2). Descriptions of early changes in clinical and cognitive characteristics are limited 6 , 7 , 8 , 9 , 10 , 11 , 12 ; notable are those from the Dominantly Inherited Alzheimer Network (DIAN), which includes persons with mutations in all three genes. 6 , 13 More information about clinical, cognitive, and other characteristics of persons with preclinical ADAD can provide additional knowledge about this condition and inform the design of future preclinical trials. This is important considering the trend toward globalization of clinical trials, 14 given the need to account for ethnic and racial factor differences in education, financial resources, world region, cognitive performance, subjective cognitive decline, and neuropsychiatric symptoms. 15
Since 1984, the Neurosciences Group of Antioquia (GNA) (part of the University of Antioquia) has studied the world's largest known ADAD kindred, with a mutation at codon 280 (PSEN1 E280A), 16 which likely originated from a single founder. 7 , 17 The Colombian API Registry 3 was launched in 2010. Using several outreach and recruitment strategies described elsewhere in association with this trial, 3 , 4 the Registry included neurological and neuropsychological data on over 5800 members of 25 PSEN1 E280A families by 2018, including over 1100 living carriers (Figure 1). 4 Over one third (38.6%) of the carriers and non‐carriers in the Registry were aged 10‐24 years; almost half were younger than 30. Before recruitment for the trial ended, the Registry had 901 persons who did not meet criteria for mild cognitive impairment (MCI) or dementia, 8 with MCI due to AD and 156 with dementia due to AD. 3 Consequently, the pool of preclinical mutation carriers ages 30 to 60 potentially eligible for the trial shrank considerably.
FIGURE 1.
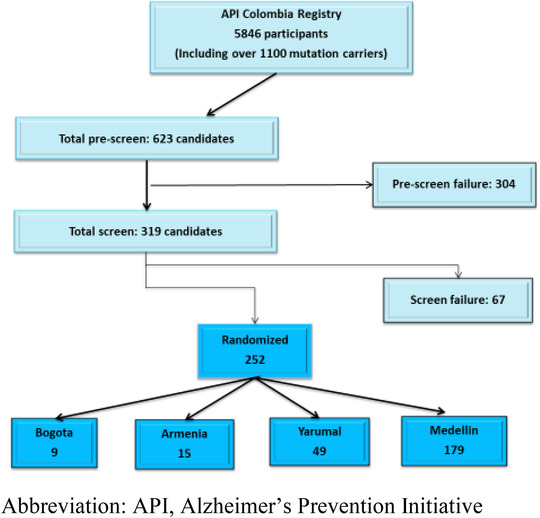
Flow diagram of the Alzheimer's Prevention Initiative (API) Colombia participant recruitment
In 2009, Banner Alzheimer's Institute (BAI) established the Alzheimer's Prevention Initiative (API) to conduct trials in persons at high risk for symptoms of AD; develop new cognitive outcomes; assess biomarker utilities; help establish the regulatory approval pathway needed for “preclinical” AD treatments; provide improved tests of the amyloid hypothesis; create recruitment registries as shared resources; and establish data and sample‐sharing plans. 4 , 18 , 19
In 2012, the collaboration involving BAI, GNA, Roche/Genentech, and the National Institute on Aging (NIA) announced the API ADAD Colombia Trial (NCT01998841) in PSEN1 E280A mutation carriers and non‐carriers was launched in 2013. 4 The trial was designed to evaluate the efficacy, safety, and tolerability of the investigational anti‐amyloid beta (Aβ) drug crenezumab in unimpaired ADAD E280A mutation carriers and the broader API goals above. In 2019, Roche/Genentech announced the termination of crenezumab clinical development in sporadic AD following results from a preplanned interim analysis of the phase III CREAD trial, which found the study was unlikely to meet the primary end point. We are continuing the API ADAD Colombia trial in order to test the efficacy of crenezumab over a much longer period (5 to 8 years) and in a very different population than in phase III: young, genetically predisposed, asymptomatic individuals, roughly 50% of whom lacked elevated brain amyloid at baseline. 37
This article describes baseline selected demographic and clinical and cognitive characteristics of cognitively unimpaired carriers and non‐carriers enrolled in the API ADAD Colombia Trial.
RESEARCH IN CONTEXT
Systematic review: The authors summarized baseline demographic, clinical, cognitive, and behavioral data from 242 cognitively unimpaired age‐matched carriers and non‐carriers of the Alzheimer's Prevention Initiative (API) Autosomal‐Dominant Alzheimer's disease (ADAD) Colombia Trial and reviewed the literature using PubMed regarding relevant publication related to similar data.
Interpretation: We confirmed that although PSEN1 E280A mutation carriers in the API ADAD Colombia Trial are cognitively unimpaired, they have slightly lower MMSE and memory scores than non‐carriers. Their demographic characteristics are representative of the local population.
Future directions: The present results confirm generally lower cognitive performance with numerically larger variance, especially on measures of memory, in this cognitively unimpaired stage of ADAD in the PSE1 E280A population. Later analyses will address the cross‐sectional relationships among age, cognitive performance, and mutation status on multiple baseline measures including transcultural variables. Other data and biological samples will be shared after the trial is completed, and baseline imaging data will be summarized separately.
2. METHODS
2.1. Trial design
The rationale and methods of the API ADAD Colombia Trial have been described previously. 4 It is a 5 to 8 year, randomized, placebo‐controlled preclinical trial of crenezumab in cognitively unimpaired 30 to 60‐year‐old kindred members, including E280A mutation carriers who were randomized to active treatment or placebo and non‐carriers who receive placebo only in order to mask mutation status (Clinicaltrials.gov NCT01998841). For study blinding and ethical reasons, participants are not provided with their mutation test results. This study is conducted at the University of Antioquia in Medellin, Colombia, with satellite sites located in Yarumal, Bogota, and Armenia for drug administration and safety monitoring for participants residing at a distance from Medellin. 4 The trial will compare rates of change in clinical and biomarker outcomes of those carriers on active treatment versus placebo, addressing whether treatment shows a clinical‐biomarker pattern indicative of slowed progression of illness. The primary outcome is change in the API ADAD Composite Cognitive Test Score 4 from baseline to week 260. 22 Secondary outcomes include time to progression to MCI or dementia due to AD; changes in dementia severity, memory, and overall neurocognitive functioning; and changes in amyloid–positron emission tomography (PET), fluorodeoxyglucose (FDG)‐PET, volumetric brain magnetic resonance imaging (MRI), and cerebral spinal fluid levels of Aβ, tau, and p‐tau. All of these clinical, cognitive, imaging, and fluid samples are being collected longitudinally, as described elsewhere, 4 and tau PET imaging was added recently: Results will be presented in the future. Safety and tolerability concerns are assessed twice monthly. 4 The trial's statistical power will be optimized by adoption of a “common close” design, whereby blinded treatment for everyone will be continued until the last person enrolled reaches 5 years. 4 The last participant visit is expected to occur in 2022.
2.2. Clinical and cognitive measures
The trial outcome measures have been published previously. 4 The clinical and cognitive outcome measures were selected primarily based on being used by GNA for over 20 years to characterize the population, data that served as the basis for the trial design. 4 The API Cognitive Composite Test 20 was derived from elements of the following: The Consortium to Establish a Registry for Alzheimer's Disease (CERAD) Word list recall, Multilingual Naming Test, CERAD Constructional Praxis Test, Mini‐Mental State Examination (MMSE) (for Orientation to Time), and Ravens Progressive Matrices. 4 Secondary clinical measures include time to progression to MCI or dementia due to AD 21 and change in Clinical Dementia Rating (CDR) (global score and sum boxes). 4 , 22 Exploratory measures included clinical and cognitive scales and tests: Functional Assessment Staging of Alzheimer's Disease (FAST), Geriatric Depression Scale (GDS), Neuropsychiatric Inventory (NPI), Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), Free and Cued Selective Reminding Test (FCSRT), and subject or partner Subjective Memory Checklist. 4 Some clinical assessments are administered only to the participant, some only to the study partner, and some to both. These assessments are administered by psychometricians or global raters who do not have access to study data other than those related to the specific assessments that they administer.
2.3. Referral and pre‐screening process
A team unblinded to genotype referred registrants to the trial to ensure the desired ratio of carriers/non‐carriers. 4 GNA implemented a methodical pre‐screening process starting with generating lists of potentially eligible candidates from the Colombian API Registry 3 to decrease screen failures and identify participants most likely to adhere to trial requirements. 23 We identified 623 (Figure 1) possibly and probably eligible candidates, of whom 48.7% failed pre‐screening. 23 Details of the prescreening process and findings have been published previously. 23
2.4. Ethics approval
Informed consent was obtained from all participants and study partners. An approved companion guide to the informed consent form and infographic about study visits was used. 23 The trial was approved by the Colombian Health Authority (Instituto Nacional de Vigilancia de Medicamento). All consent procedures were conducted in accordance with international and local ethics committee standards and after ethics committee approval. 4
2.5. Statistical analysis of baseline data
The sponsor teams developed a baseline data‐sharing plan intended to benefit the field while also protecting participant confidentiality and trial integrity. Summary statistics were reviewed by sponsor personnel who were independent of the study team to ensure that individual participants could not be identified through tabulated or graphical representations of data. Data from 242 (of 252 randomized) participants (167 E280A mutation carriers and 75 non‐carriers) were analyzed by BAI investigators who are not involved in the API study conduct, analysis, or interpretation of treatment data. Data from 10 participants were excluded from analyses to protect participant confidentiality, genetic status, and trial integrity. Descriptive statistics were calculated. Independent sample T‐test was used for continuous variables and chi‐square test was used for categorical variables, respectively, to test for differences between the E280A mutation carriers and non‐carriers. Statistical tests were not adjusted for multiplicity. All statistical analyses were performed using Systat 13.0 (Systat Software, Inc., San Jose, CA).
3. RESULTS
3.1. Study participants
Enrollment began in December 2013 and ended in February 2017 (Figure 1). More carriers compared to non‐carriers, and more males compared to females, failed pre‐screening. Pre‐screening failure in carriers was mainly due to illiteracy or learning/comprehension difficulties than in non‐carriers. There were more pre‐screen failures in age 50 to 54 and 60 years, presumably because the median age of onset of dementia in PSEN1 E280A is about age 50 and because 60 years was the maximum age for trial eligibility. A total of 319 cognitively unimpaired 30‐ to 60‐year‐old members from the Colombian API Registry consented, 151 females and 101 males were enrolled, including 169 E280A mutation carriers and 83 non‐carriers. The screen failure rate was 21.0% (67/319). The primary reasons for screen failure were expected inability to comply with the protocol (n = 15), chiefly because of work requirements, hypothyroidism or vitamin B12 deficiency (n = 9), low MMSE score (n = 6), and substance abuse and/or positive urine test for drugs of abuse (n = 5).
3.2. Demographics
Participants’ demographic characteristics are summarized in Table 1 (of 252 enrolled, we present data on 242 mutation carriers and non‐carriers matched by age range, excluding data on 10 participants to protect their confidentiality, genetic status, and trial integrity). All participants were born in Colombia. Mutation carriers were significantly younger than non‐carriers (37 ± 5 vs 42 ± 6 years, respectively; P < .001). There were no statistically significant differences between mutation carriers and non‐carriers in terms of sex distribution (P = .36) or years of education (P = .64).
TABLE 1.
Cognitively unimpaired PSEN1 E280A mutation carriers and non‐carriers from the API ADAD Colombia trial: baseline demographic and clinical characteristics a
| Carriers | Non‐carriers | P | |
|---|---|---|---|
| Number | 167 | 75 | — |
| Age (range) | 37 ± 5 (30–53) | 42 ± 6 (30–53) | <.001 |
| Sex (n [%] female) | 101 (60%) | 50 (67%) | .36 |
| Education (years) | 8.8 ± 4.1 | 8.5 ± 4.4 | .64 |
| APOE ε4 carriers (n [%]) | 36 (22%) | 17 (29%) | .85 |
| CDR Global | 0.05 ± 0.2 | 0.03 ± 0.1 | .38 |
| CDR Sum of Boxes | 0.14 ± 0.4 | 0.05 ± 0.2 | .05 |
| FAST | 1.11 ± 0.34 | 1.01 ± 0.12 | .01 |
| NPI | 0.46 ± 1.67 | 0.41 ± 2.05 | .85 |
| GDS | 1.35 ± 1.83 | 1.19 ± 1.81 | .53 |
APOE, apolipoprotein E; CDR, Clinical Dementia Rating Scale; FAST, Functional Assessment Staging Test; GDS, Geriatric Depression Scale; n, number; NPI, Neuropsychiatric Inventory.
Data for continuous variables are presented as mean ± standard deviation. Significant difference, P < .05.
Data from 242 age range–matched mutation carriers and non‐carriers that are available prior to trial completion.
3.3. Clinical characteristics
Participants’ clinical characteristics are summarized in Table 1. There were no statistically significant differences between E280A mutation carriers and non‐carriers in frequency of apolipoprotein ɛ4 (APOE4) carriage (P = .85). Compared to non‐carriers, E280A mutation carriers had slightly higher FAST scores, with numerically larger variance (1.11 ± 0.34 vs 1.01 ± 0.12; P = .01), and higher CDR Sum of Boxes scores (0.14 ± 0.4 vs 0.05 ± 0.2; P = .05). There were no statistically significant differences between E280A mutation carriers and non‐carriers in Global CDR, GDS, or total NPI scores. Per protocol, participants could not be enrolled if they met clinical criteria for major depression or other neuropsychiatric disorders.
3.4. Cognitive performance
Selected cognitive characteristics are summarized in Table 2. Compared to non‐carriers, E280A mutation carriers had significantly lower scores on MMSE (28.8 ± 1.4 vs 29.2 ± 1.0; P = .01), CERAD Word List delayed Recall (6.9 ± 2.2 vs 7.7 ± 1.9; P = .01), RBANS Total Scale (68.1 ± 12.7 vs 74.9 ± 11.8, P < .001), RBANS Immediate Memory (87.7 ± 13.5 vs 96.9 ± 13.9; P < .001), RBANS Delayed Memory (77.4 ± 17.0 vs 87.3 ± 12.9, P < .001), FCSRT Total (42.4 ± 6.5 vs 44.6 ± 3.2, P < .001), and FCSRT Delayed Recall (14.2 ± 2.8 vs 15.2 ± 1.3, P < .001). There were no statistically significant differences, but slightly worse performance in E280A mutation carriers compared to non‐carriers, in CERAD Word List Total Recall (P = .07), RBANS Attention (P = .09), and RBANS language (P = .08). There were no statistically significant differences in RBANS Visuospatial/Constructional, or subject or partner Subjective Memory Checklist scores between E280A mutation carriers and non‐carriers. Because the carriers were younger than non‐carriers, we also adjusted for age. Adjusting for age resulted in lower P values across all cognitive measures (data not shown).
TABLE 2.
Cognitively unimpaired PSEN1 E280A mutation carriers and non‐carriers from the API ADAD Colombia trial: baseline cognitive characteristics a
| Carriers | Non‐carriers | P | |
|---|---|---|---|
| MMSE | 28.8 ± 1.4 | 29.2 ± 1.0 | .01 |
| CERAD Word List Total Recall | 20.1 ± 4.2 | 21.13 ± 4.0 | .07 |
| CERAD Word List Delayed Recall | 6.9 ± 2.2 | 7.7 ± 1.9 | .01 |
| RBANS Total Scale | 68.1 ± 12.7 | 74.9 ± 11.8 | <.001 |
| RBANS Immediate Memory | 87.7 ± 13.5 | 96.9 ± 13.9 | <.001 |
| RBANS Delayed Memory | 77.4 ± 17.0 | 87.3 ± 12.9 | <.001 |
| RBANS Attention | 60.5 ± 15.7 | 64.2 ± 14.3 | .09 |
| RBANS Visuospatial/Constructional | 70.9 ± 12.7 | 73.1 ± 12.8 | .22 |
| RBANS Language | 75.8 ± 18.1 | 80.1 ± 17.2 | .08 |
| FCSRT Total | 42.4 ± 6.5 | 44.6 ± 3.2 | <.001 |
| FCSRT Delayed Recall | 14.2 ± 2.8 | 15.2 ± 1.3 | <.001 |
| Subjective Memory Checklist—Participant | 9.8 ± 6.3 | 9.2 ± 6.2 | .51 |
| Subjective Memory Checklist—Study Partner | 6.2 ± 5.5 | 5.6 ± 4.6 | .46 |
MMSE, Mini‐Mental Status Examination; CERAD, Consortium to Establish a Registry for Alzheimer's disease; RBANS, Repeatable Battery for the Assessment of Neuropsychological Status; FCSRT, Free and Cued Selective Reminding Task
Data for continuous variables are presented as mean ± standard deviation. Significant difference, P < .05.
Data from 242 age range–matched mutation carriers & non‐carriers that are available prior to trial completion.
4. DISCUSSION
Compared to cognitively unimpaired non‐carriers in the trial, these cognitively unimpaired E280A mutation carriers were younger; had similar educational attainment; reported no difference in subjective concerns regarding cognition; showed generally lower cognitive performance with numerically larger variance, especially on measures of memory; and had small or no differences in FAST and CDR scores, with numerically larger variance. There were no statistically significant differences between groups in neuropsychiatric symptoms based on caregiver‐reported NPI total scores.
E280A mutation carriers were likely younger than non‐carriers because carriers were more likely to meet criteria for MCI or dementia due to AD as they age. Previous studies in this population 8 showed a median age of onset of 44 years (95% confidence interval [CI] 43–45) for MCI and of 49 years (95% CI 49–50) for dementia, and carriers died at a median age of 59 years (58 to 61). Consequently, older E280A mutation carriers were more likely to screen fail due to cognitive impairment. There was a prospective and blinded effort to match carriers and non‐carriers by age when they were referred to the trial from the Registry, but full matching was not possible. 4
Educational attainment of participants was similar to that reported previously for this population 12 but lower compared with what DIAN reported in 2014 from its observational cohort, where carriers with CDR 0 had 14.4 (±2.5) while E280A non‐mutation carriers had 14.7 (±2.6) years of education, respectively. 6
More than 60% of participants are women, even though ADAD affects both sexes equally. This female predominance was reported in other studies in similar populations with ADAD. 6 It might be explained partly because males failed pre‐screening more than females and most candidates who failed pre‐screening due to substance dependence were male 22/25 (88%). 23 Another major factor for screen failure was expected inability to comply with the protocol 15/67 (22.3%), chiefly due to work requirements: Men were more likely to be in the work force and faced absences from work for trial procedures. Trial duration was a deciding factor for some who could entertain the possibility of periodic but not sustained absence from work. Women were more likely to work at home and, anecdotally at least, were more willing than men were to participate in studies. It is unknown whether this gender difference, and the possible reasons for it, impact retention or treatment response in the trial.
Compared to E280A mutation non‐carriers in the trial, carriers showed generally lower cognitive performance, with numerically larger variance, especially on measures of memory, results like those from prior studies in this and other ADAD populations. 6 In prior studies of PSEN1 E280A mutation carriers, cognitive decline could be detected by neuropsychological tests more than a decade before the onset of clinical symptoms. 12 This likely account for differences in cognitive scores in the carrier group compared with the non‐carrier group.
The RBANS total score and subscores (particularly attention) were lower compared to another clinical study of patients with MCI due to probable sporadic AD. 24 This might be explained by the relatively lower educational attainment of participants in our trial. 24 In addition, early onset AD (EOAD) differs significantly from late‐onset AD (LOAD), particularly in the substantial percentage of patients with early onset AD, who have phenotypic variants as well as the larger percentage of those with a familial form of the disease, 25 factors that may contribute to differences in cognitive tests results.
The frequency of apolipoprotein (APOE) ɛ4 variant (APOE4) carriage, the strongest genetic risk factor for late onset AD, 26 was higher in our study population (22% of E280A mutation carriers and 29% of non‐carriers) compared with other studies done in different regions of Colombia, including Bogota (8.9%), 27 and in the Amerindians communities (up to 18%). 28 However, our result was like what DIAN has reported (22% in E280A mutation carriers and 28% in non‐carriers). 6 However, APOE4 carriage does not modify the onset of ADAD in this population. 29 ADAD mutations are enough to cause symptomatic onset of AD with virtual certainty at a much younger age compared to persons with LOAD, and this is apparently not affected by this genetic risk factor for LOAD.
Some (five) E280A mutation non‐carriers had CDR Global scores that were greater than zero, something that might not be expected for healthy individuals. This might be due to several factors, including “stereotype threat,” worse‐than‐expected scores due to fear and anxiety about normal forgetfulness in everyday life. This phenomenon may have been magnified by perceived genetic risk, as well as fear among those who care(d) for family members with symptomatic ADAD and experience(d) reminders of their own possible future with this disease, something seen in a previous study published about this population. 30 All participants in this trial are members of 25 families with PSEN1 E280A mutation; all had at least one family member with the disease, and some are or were caregivers of other symptomatic family members. Prior studies have shown that people who had prior experience dealing with genetically influenced AD seemed vulnerable to the effects of negative stereotype beliefs about perceived threat of AD and showed an inverse relationship between their cognitive performance and their perception of personal AD threat. 38 In addition, individuals who learned that they were at increased susceptibility for AD dementia by virtue of carrying the APOE4 allele had poorer perceptions of their memory abilities and performed worse on objective memory tests compared to individuals who did not know their APOE results. 39
As a related matter, compared to non‐carriers, E280A mutation carriers enrolled in the trial showed no statistically significant difference in subjective memory concerns measured by self or study partner report. This may also be a manifestation of stereotype threat. Compared to non‐carriers, E280A mutation carriers had significantly higher FAST results and borderline higher CDR Sum of Boxes (with numerically larger variance) without significant differences in Global CDR. This subtle baseline finding is not likely to be clinically significant, but it is possible that carriers close to the age of the clinical onset of AD may have been in a “pre‐MCI,” stage of illness, 8 with some study partners detecting subtle changes not fully evident on clinical assessment or objective testing. The Global CDR is less sensitive to subtle changes in cognitive and/or functional state and usually shows differences only when MCI or dementia symptoms are imminent. 8 , 31
E280A mutation carriers showed no statistically significant differences in measures of neuropsychiatric features, as expected. DIAN investigators have also not reported increased prevalence of such features in ADAD mutation carriers versus non‐carriers during the pre‐symptomatic stage of illness, suggesting that these symptoms may develop as the threshold of neurodegeneration is near instead of being life‐long attributes. 32 We will learn whether there are differences between E280A mutation carriers and non‐carriers in emergent neuropsychiatric features over time in the trial and whether this affects retention or treatment response. For example, emergent depressive features might constitute a prodromal manifestation of the disease in PSEN1 E280A mutation carriers, 33 and prior work in LOAD 34 , 35 showed that persons with AD can manifest behavioral features prior to dementia onset.
The study has limitations. Although the Colombian API registry includes many people, with over 1100 E280A mutation carriers, those enrolled in this trial may not be representative of the broader PSEN1 E280A population at risk for symptoms of AD. We excluded registrants who did not meet pre‐screening criteria. 23 We do not have the same extent of data on persons who screen failed as for those enrolled. It is possible that some E280A mutation carriers who met protocol criteria were in a “pre‐MCI” stage, that is, overtly unimpaired but showing lower performance on objective testing because they were closer to symptom onset. 8 We did not assess stereotype threat directly, although based on our prior work, we hypothesize that this might be one reason that PSEN1 E280A mutation carriers performed worse than non‐carriers. 30 We did not collect occupational attainment information, which might have helped address possible “cognitive reserve,” 36 a factor that may protect certain individuals from early clinical manifestations of AD. Randomization should minimize the effect of transcultural variables on the primary outcome. On the other hand, the study has strengths including extensive phenotyping (cognitive, clinical, and fluid and imaging biomarkers) selected because of decades of study of this homogenous population with ADAD risk resulting from a single E280A mutation. These factors led to an efficient study design that we hope will address our aims.
5. CONCLUSION/SUMMARY
We describe baseline demographic, clinical, and cognitive characteristics of participants in the first precedent‐setting study in a series of API trials. Selected baseline data from 242 trial participants are now available on the GAAIN website (http://gaain.org/) and interested investigators can contact us if they are interested in pursuing additional analyses of baseline data (APIData@bannerhealth.com). Other data and biological samples will be shared after the trial is completed, and baseline imaging data will be summarized separately. The present results confirm generally lower cognitive performance with numerically larger variance, especially on measures of memory, in this cognitively unimpaired stage of ADAD in the PSE1 E280A population. Later analyses will address the cross‐sectional relationships among age, cognitive performance and E280A mutation status on multiple baseline measures including transcultural variables such as the impact of occupational attainment, marital status, study partner status, and residential status.
ACKNOWLEDGEMENTS/CONFLICTS/FUNDING SOURCES
This work is supported by the NIA (RF1 AG041705‐01A1, R01 AG055444, P30 AG19610); Roche/Genentech, Banner Alzheimer's Foundation; anonymous international foundation; Flinn Foundation; Forget Me Not Initiative; Nomis Foundation; Colciencias and University of Antioquia (1115‐545‐31651, 1115‐657‐4185); and the State of Arizona (Arizona Alzheimer's Consortium). BAI, Roche/Genentech, and GNA led the creation of the study design and the analysis and interpretation of the data, as well as the writing of this article. Funding for Open Access was provided by Roche/Genentech. Avid/Eli Lilly contributed a radiotracer. The NIA served in an advisory capacity in the design of the trial and in oversight of the Data Monitoring Committee (DMC). No other sponsor was involved.
The authors gratefully acknowledge former contributors Laureano Mestra, MD, and Madelyn Gutierrez, the entire GNA team, and most of all the families with PSEN1 E280A mutation from Colombia. The authors acknowledge the contribution of former contributors Carole Ho, MD; Shehnaaz Suliman, MD; Robert Paul, MD, PhD, as well as the following additional API contributors: Independent Data Monitoring Committee: Karl Kieburtz, MD, MPH (Chair); Charles Davis, PhD; Serge Gauthier, CM, MD, FRCPC; William Jagust, MD; Facundo Manes, MD; Ethics and Cultural Sensitivities Committee: Jason Karlawish, MD, Scott Kim, MD, PhD; Kenneth Kosik, MD; Progression Adjudication Committee: Howard Feldman, MD, FRCP; Ronald Petersen, MD, PhD; Treatment Selection Advisory Committee: Paul Aisen, MD, Steven DeKosky, MD, David Holtzman, MD, Kenneth Kosik, MD; Frank La Ferla, PhD, Lon S. Schneider, MD; Banner Alzheimer's Institute: Constance Boker, Vivek Devadas, Laura Jakimovich, and Don Saner.
Silvia Rios‐Romenets, Francisco Lopera, Margarita Giraldo‐Chica, Carlos Tobon, Natalia Acosta‐Baena, Claudia Muñoz, Paula Ospina, Victoria Tirado, Eliana Henao, Yamile Bocanegra report participation in other projects financed by the National Institutes of Health, Comite para el Desarrollo de la Investigacion (CODI‐ UdeA) and COLCIENCIAS. Kaycee Sink, Heather Guthrie, Nan Hu, Qinshu Lian, William Cho, and Howard Mackey are full‐time employees of Genentech, a member of the Roche group, and hold stock in Roche. Pierre N. Tariot reports receiving: grants from National Institute of Aging (RF1 AG041705‐01A1, UF1 AG046150, R01 AG055444, 1R01AG058468), and Genentech/Roche; other research support from Arizona Department of Health Services, Alzheimer's Association, Banner Alzheimer's Foundation, FBRI, GHR, Nomis Foundation, and the Flinn Foundation; consultant fees from Acadia, Abbott Laboratories, AbbVie, AC Immune, Auspex, Boehringer‐Ingelheim, Brain Test Inc., California Pacific Medical Center, Chase Pharmaceuticals, CME Inc., GliaCure, Insys Therapeutics, Pfizer, and T3D; consulting fees and research support from AstraZeneca, Avanir, Lilly, Lundbeck, Merck & Co., Roche, and Takeda; research support only from Amgen, Avid, Biogen, Elan, Functional Neuromodulation [f(nm)], GE, Genentech, Novartis, and Targacept; and stock options in Adamas Pharmaceuticals. Eric M. Reiman has received consulting fees from Alkahest, Alzheon, Aural Analytics, Biogen, Denali, Green Valley, Pfizer, Roche (Expenses Only), United Neuroscience, and Zinfandel Pharma. He received research support from Avid/Lilly, Genentech/Roche, and Novartis/Amgen, the National Institute on Aging, the National Institute of Neurologic Disorders, Banner Alzheimer's Foundation, Alzheimer's Association, GHR Foundation, FBRI, NOMIS Foundation, Flinn Foundation, and the State of Arizona.
Rios‐Romenets S, Lopera F, Sink KM, et al. Baseline demographic, clinical, and cognitive characteristics of the Alzheimer's Prevention Initiative (API) autosomal‐dominant Alzheimer's Disease Colombia trial. Alzheimer's Dement. 2020;16:1023–1030. 10.1002/alz.12109
Silvia Rios‐Romenets and Francisco Lopera are co‐first authors.
Eric M. Reiman and Pierre N. Tariot are co‐last authors.
REFERENCES
- 1. Reiman EM, Langbaum JB, Tariot PN, et al. CAP—advancing the evaluation of preclinical Alzheimer disease treatments. Nat Rev Neurol. 2016;12(1):56‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saunders KT, Langbaum JB, Holt CJ, et al. Arizona Alzheimer's registry: strategy and outcomes of a statewide research recruitment registry.J Prev Alzheimers Dis. 2014;1(2):74‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rios‐Romenets S, Lopez H, Lopez L, et al. The Colombian Alzheimer's Prevention Initiative (API) registry. Alzheimers Dement. 2017;13:602‐605. [Google Scholar]
- 4. Tariot PN, Lopera F, Langbaum JB, et al. The Alzheimer's Prevention Initiative Autosomal‐Dominant Alzheimer's Disease Trial: A study of crenezumab versus placebo in preclinical PSEN1 E280A mutation carriers to evaluate efficacy and safety in the treatment of autosomal‐dominant Alzheimer's disease, including a placebo‐treated noncarrier cohort. Alzheimers Dement (N Y). 2018;4:150‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kosik KS, Munoz C, Lopez L, et al. Homozygosity of the autosomal dominant Alzheimer disease presenilin 1 E280A mutation. Neurology. 2015;84(2):206‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Storandt M, Balota DA, Aschenbrenner AJ, Morris JC. Clinical and psychological characteristics of the initial cohort of the Dominantly Inherited Alzheimer Network (DIAN). Neuropsychology. 2014;28(1):19‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lopera F, Ardilla A, Martinez A, et al. Clinical features of early‐onset Alzheimer disease in a large kindred with an E280A presenilin‐1 mutation. JAMA. 1997;277(10):793‐799. [PubMed] [Google Scholar]
- 8. Acosta‐Baena N, Sepulveda‐Falla D, Lopera‐Gomez CM, et al. Pre‐dementia clinical stages in presenilin 1 E280A familial early‐onset Alzheimer's disease: a retrospective cohort study. Lancet Neurol. 2011;10(3):213‐220. [DOI] [PubMed] [Google Scholar]
- 9. Fox NC, Warrington EK, Seiffer AL, Agnew SK, Rossor MN. Presymptomatic cognitive deficits in individuals at risk of familial Alzheimer's disease. A longitudinal prospective study. Brain. 1998;121(pt 9):1631‐1639. [DOI] [PubMed] [Google Scholar]
- 10. Ringman JM, Diaz‐Olavarrieta C, Rodriguez Y, et al. Neuropsychological function in nondemented carriers of presenilin‐1 mutations. Neurology. 2005;65(4):552‐558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mondadori CR, Buchmann A, Mustovic H, et al. Enhanced brain activity may precede the diagnosis of Alzheimer's disease by 30 years. Brain. 2006;129(pt 11):2908‐2922. [DOI] [PubMed] [Google Scholar]
- 12. Aguirre‐Acevedo DC, Lopera F, Henao E, et al. Cognitive decline in a Colombian kindred with autosomal dominant Alzheimer disease: a retrospective cohort study. JAMA Neurol. 2016;73(4):431‐438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tang M, Ryman DC, McDade E, et al. Neurological manifestations of autosomal dominant familial Alzheimer's disease: a comparison of the published literature with the Dominantly Inherited Alzheimer Network observational study (DIAN‐OBS). Lancet Neurol. 2016;15(13):1317‐1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cummings JL, Atri A, Ballard C, et al. Insights into globalization: comparison of patient characteristics and disease progression among geographic regions in a multinational Alzheimer's disease clinical program. Alzheimers Res Ther. 2018;10(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Babulal GM, Quiroz YT, Albensi BC, et al. Perspectives on ethnic and racial disparities in Alzheimer's disease and related dementias: update and areas of immediate need. Alzheimers Dement. 2019;15(2):292‐321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lendon CL, Martinez A, Behrens IM, et al. E280A PS‐1 mutation causes Alzheimer's disease but age of onset is not modified by ApoE alleles. Hum Mutat. 1997;10(3):186‐195. [DOI] [PubMed] [Google Scholar]
- 17. Lalli MA, Cox HC, Arcila ML, et al. Origin of the PSEN1 E280A mutation causing early‐onset Alzheimer's disease. Alzheimers Dement. 2014;10(5 suppl):S277‐S83 e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reiman EM, Langbaum JB, Tariot PN. Alzheimer's prevention initiative: a proposal to evaluate presymptomatic treatments as quickly as possible. Biomark Med. 2010;4(1):3‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reiman EM, Langbaum JB, Fleisher AS, et al. Alzheimer's Prevention Initiative: a plan to accelerate the evaluation of presymptomatic treatments. J Alzheimers Dis. 2011;26(suppl 3):321‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ayutyanont N, Langbaum JB, Hendrix SB, et al. The Alzheimer's prevention initiative composite cognitive test score: sample size estimates for the evaluation of preclinical Alzheimer's disease treatments in presenilin 1 E280A mutation carriers. J Clin Psychiatry. 2014;75(6):652‐660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging‐Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):270‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412‐2414. [DOI] [PubMed] [Google Scholar]
- 23. Rios‐Romenets S, Giraldo‐Chica M, Lopez H, et al. The Value of Pre‐Screening in the Alzheimer's Prevention Initiative (API) autosomal dominant Alzheimer's disease trial. J Prev Alzheimers Dis. 2018;5(1):49‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Karantzoulis S, Novitski J, Gold M, Randolph C. The Repeatable battery for the assessment of neuropsychological status (rbans): utility in detection and characterization of mild cognitive impairment due to Alzheimer's disease. Arch Clin Neuropsychol. 2013;28(8):837‐844. [DOI] [PubMed] [Google Scholar]
- 25. Mendez MF. Early‐onset Alzheimer Disease and its variants. Continuum (Minneap Minn). 2019;25(1):34‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bu G. Apolipoprotein E and its receptors in Alzheimer's disease: pathways, pathogenesis and therapy. Nat Rev Neurosci. 2009;10(5):333‐344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Forero DA, Pinzon J, Arboleda GH, et al. Analysis of common polymorphisms in angiotensin‐converting enzyme and apolipoprotein e genes and human longevity in Colombia. Arch Med Res. 2006;37(7):890‐894. [DOI] [PubMed] [Google Scholar]
- 28. Jaramillo‐Correa JP, Keyeux G, Ruiz‐Garcia M, Rodas C, Bernal J. Population genetic analysis of the genes APOE, APOB(3'VNTR) and ACE in some black and Amerindian communities from Colombia. Hum Hered. 2001;52(1):14‐33. [DOI] [PubMed] [Google Scholar]
- 29. Velez JI, Lopera F, Sepulveda‐Falla D, et al. APOE*E2 allele delays age of onset in PSEN1 E280A Alzheimer's disease. Mol Psychiatry. 2016;21(7):916‐924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Garcia‐Toro M, Sanchez‐Gomez MC, Madrigal Zapata L, Lopera FJ. “In the flesh”: narratives of family caregivers at risk of Early‐onset Familial Alzheimer's disease. Dementia (London). 2018:1471301218801501. [DOI] [PubMed] [Google Scholar]
- 31. Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303‐308. [DOI] [PubMed] [Google Scholar]
- 32. Ringman JM, Liang LJ, Zhou Y, et al. Early behavioural changes in familial Alzheimer's disease in the Dominantly Inherited Alzheimer Network. Brain. 2015;138(pt 4):1036‐1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mejia S, Giraldo M, Pineda D, Ardila A, Lopera F. Nongenetic factors as modifiers of the age of onset of familial Alzheimer's disease. Int Psychogeriatr. 2003;15(4):337‐349. [DOI] [PubMed] [Google Scholar]
- 34. Canevelli M, Adali N, Voisin T, et al. Behavioral and psychological subsyndromes in Alzheimer's disease using the Neuropsychiatric Inventory. Int J Geriatr Psychiatry. 2013;28(8):795‐803. [DOI] [PubMed] [Google Scholar]
- 35. Pocnet C, Rossier J, Antonietti JP, von Gunten A. Personality traits and behavioral and psychological symptoms in patients at an early stage of Alzheimer's disease. Int J Geriatr Psychiatry. 2013;28(3):276‐283. [DOI] [PubMed] [Google Scholar]
- 36. Stern Y, Albert S, Tang MX, Tsai WY. Rate of memory decline in AD is related to education and occupation: cognitive reserve? Neurology. 1999;53(9):1942‐1947. [DOI] [PubMed] [Google Scholar]
- 37. Reiman EM, Sink KM, Hu N, et al. A public resource of baseline data from the API autosomal dominant Alzheimer's disease Colombia trial (abstract P4‐209). Alzheimer's and Dementia: The Journal of the Alzheimer's Association. 2018;14(7 suppl):1521. [Google Scholar]
- 38. Suhr JA, Kinkela JH. Perceived threat of Alzheimer disease (AD): the role of personal experience with AD. Alzheimer Dis Assoc Disord. 2007;21(3):225‐231. [DOI] [PubMed] [Google Scholar]
- 39. Lineweaver TT, Bondi MW, Galasko D, Salmon DP. Effect of knowledge of APOE genotype on subjective and objective memory performance in healthy older adults. Am J Psychiatry. 2014;171(2):201‐208. [DOI] [PMC free article] [PubMed] [Google Scholar]


