Abstract
Objectives:
To examine whether participants with the most behavioral goals to achieve were more likely to meet more goals than those given fewer goals.
Methods:
Eight hundred ten participants were randomly assigned to advice-only, established guidelines for blood pressure control (reduced sodium, increased physical activity), or established guidelines plus the DASH diet (increased fruits, vegetables, low-fat dairy, reduced fat).
Results:
At 6 months, 11.7% of Advice-Only, 19.3% of Established, and 44.6% of Established plus DASH met at least 3 goals (P<0.0001). At 18 months, 33.5% of Established plus DASH met at least 3 goals.
Conclusions:
Those with the most goals to achieve reached the most goals.
Keywords: health behaviors, physical activity, DASH dietary pattern, blood pressure
National guidelines and professional scientific organizations recommend individuals maintain a normal weight; eat a diet low in saturated fat and sodium and high in fruits, vegetables, and whole grains; and participate in regular physical activity to reduce risk of cardiovascular disease,1,2 hypertension,3,4 diabetes,5 and cancer6 and to maintain health.7 Results from the Diabetes Prevention Program, an intervention trial conducted with persons at high risk for developing diabetes, showed that a lifestyle intervention that targeted multiple behaviors was superior to medication for preventing diabetes.8 Relative to the placebo condition, the lifestyle intervention with goals of a 7% loss in body weight and at least 150 minutes per week of physical activity resulted in a 58% reduction in diabetes incidence – an amount significantly greater than the 31% reduction found from the use of metformin, an antihyperglycemic agent.8 Other multicomponent interventions have resulted in regression of coronary atherosclerotic plaques9,10 and lowered incidence of cardiovascular disease,11 although not all have positively influenced cardiovascular disease outcomes.12,13 Interventions targeting multiple behaviors are thought to be efficacious for disease prevention; the continuing challenge is to promote the adoption and maintenance of these positive health behaviors.
Although the success of multiple lifestyle interventions in preventing disease suggests that individuals are able to make and sustain multiple lifestyle changes, it is unclear how best to design interventions to modify multiple lifestyle behaviors.14 Change in one health behavior may foster additional changes or, conversely, may impede change in other behaviors. For example, a physical activity intervention increased the rate of continuous abstinence from smoking15; but an intervention that combined physical activity, caloric reduction, and behavioral self-management resulted in smoking relapse.16 Given that most middle-aged Americans have at least one major behavioral risk factor17 and only 3% simultaneously meet recommendations for nonsmoking, normal weight, 5+ fruits and vegetable intake per day, and 5+ days per week of 30 minutes of physical activity,18 strategies for promoting multiple behavior change require more attention.
PREMIER was a randomized clinical trial that tested the effects of 2 multicomponent lifestyle interventions on blood pressure control among adults with prehypertension and stage 1 hypertension.19 Individuals with above-optimal blood pressure were randomized to (1) a group to implement established guidelines of weight loss, sodium reduction, increased physical activity, and limited alcohol intake; (2) a group to implement these established guidelines plus the Dietary Approaches to Stop Hypertension (DASH) dietary pattern (ie, diet high in fruits, vegetables, low-fat dairy products, and reduced intake of saturated and total fat); or (3) a group given only advice on nonpharmacologic factors that can affect blood pressure. Previous reports documented that these interventions resulted in improved lifestyle behaviors and, when compared with advice only, improved blood pressure control.20-22 At 6 months relative to Advice-Only, the net reduction in blood pressure was 3.7 mmHg in the Established group and 4.3 mmHg in the Established plus DASH group.20 Blood pressure reductions in both intervention groups were significantly greater than in Advice-Only, but not different from each other.
In this secondary analysis of PREMIER, we examined in detail the extent to which participants were able to achieve the multiple behavioral lifestyle goals promoted in the intervention conditions. We were particularly interested in examining whether participants in the treatment condition with the most targeted goals were more likely to meet multiple goals compared with those in the treatment condition with fewer targeted goals, or if the condition associated with high goal expectation was associated with less goal attainment. Previous reports documented that PREMIER participants made behavior changes consistent with their randomized assignment.20,22,23 However, mean changes in nutrients, food groups, and physical activity were reported in the context of documenting adherence to a given treatment condition, and the primary outcome of interest was blood pressure. We have not specifically examined if participants were able to meet the multiple behavioral goals promoted by the interventions. This analysis can provide information regarding whether and how achieving success in one health behavior is associated with success in changing other behaviors.24
METHODS
PREMIER participants were men and women age 25 years or older with prehypertension and stage 1 hypertension at 4 clinical centers (Baltimore, MD, Baton Rouge, LA, Durham, NC, and Portland, OR). Kaiser-Permanente Center for Health Research served as the coordinating center, and the National Heart, Lung, and Blood Institute project office also participated. The study was approved by each site’s human subjects institutional review board, and all participants provided written informed consent. Trial methods and main results are published.20-22
Eligibility Criteria
Blood pressure eligibility was systolic blood pressure between 120 and 159 mmHg and diastolic blood pressure between 80 and 95 mmHg.3 Body mass index (kg/m2) (BMI) criteria were 18.5 to 45. Major exclusion criteria included use of antihypertensive medications, insulin, or oral hypoglycemic drugs; previous cardiovascular event or cancer diagnosis; and congestive heart failure or symptoms of angina or peripheral vascular disease.
Measurements
Physical activity.
Change in physical activity was assessed by self-report. Total daily energy expenditure was assessed with the Stanford 7-Day Physical Activity Recall (PAR).25,26 Participants estimated the number of hours spent over the last 7 days in sleep and in moderate, hard, and very hard activity. Light activity was calculated as the remaining time. The mean intensity value from each category was multiplied by hours spent in the category and summed across categories to estimate energy expenditure as total kilocalories per kilogram body weight per day (kcal/kg/day), For purposes of this manuscript, the number of weekly minutes spent in moderate, hard, and very hard activity was determined and divided by 7 to determine daily minutes in moderate to vigorous physical activity.
Dietary intake.
The Diet Assessment Center of Pennsylvania State University conducted 2 unannounced 24-hour recalls collected by telephone interview, one on a weekday and one on a weekend day. Nutrients and food-group intake were calculated using the Nutrition Data System for Research NDS-R 1998 (University of Minnesota). One 24-hour urine collection was obtained to measure excretion of sodium.
Interventions
After baseline measurements were completed, participants were randomized into one of 2 lifestyle interventions or an advice-only group. The Established intervention included guidelines from the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure VI.27 The Established plus DASH intervention included the same established guidelines plus the DASH dietary pattern.28 The 2 interventions were similar in all respects except for the DASH dietary pattern. In total, the Established intervention targeted 4 behaviors that had specific, standard goals; and the Established plus DASH intervention targeted 6 behaviors.
Participant goals for both interventions are displayed in Table 1. The weight-loss goal was specific to those with a BMI ≥25 kg/m2 and was encouraged by reduced energy intake and increased physical activity. The physical activity goal was 180 minutes per week of moderate-intensity aerobic activity, consistent with national physical activity guidelines29 and was a targeted goal irrespective of a participant’s need to lose weight. Reduced sodium intake to less than or equal to 2400 mg/day was also targeted. In addition to the previous goals, the Established plus DASH intervention included a target of at least 9 servings per day of fruits and vegetables. Both interventions consisted of 18 face-to-face contacts during the first 6 months of the intervention and 12 face-to-face contacts during the remaining 12 months.30 Intervention strategies and materials were identical except for the dietary recommendations. Session content included behavioral skills training, self-monitoring, social support, group accountability, and goal setting. All intervention behaviors were addressed during each intervention contact; thus, multiple behavior changes were simultaneously targeted.
Table 1.
Intervention Goals and Delivery Approaches for PREMIER Treatment Groups
| Advice-Only | Established | Established + DASH | |
|---|---|---|---|
| Intervention Goals: | |||
| Weight loss | As Needed | ≥15 lba | ≥15 lba |
| Total calories/day | No Target | Individual Targetb | Individual Targetb |
| Physical activity/week | Increase | 180 minutes | 180 minutes |
| Sodium/day | Reduce | ≤2400 mg | ≤2400 mg |
| Alcohol/day | ≤1 oz. Men | ≤1 oz. Men | ≤1 oz. Men |
| ≤.5 oz. Women | ≤.5 oz. Women | ≤.5 oz. Women | |
| Dietary Variables: | Food Guide Pyramid | JNC V | DASH |
| % Kcal Fat | Food Guide Pyramid | ≤30% | ≤25% |
| % Kcal Saturated Fat | Food Guide Pyramid | ≤10% | ≤7% |
| Fruits & Vegetables servings | Food Guide Pyramid | Not emphasized | 9-12 servings |
| Dairy servings | Food Guide Pyramid | Not emphasized | 2-3 servings |
| Self-Monitoring Recommendations: | |||
| Number days per week | None | ≥3 | ≥3 |
| Behavioral targets monitored | None | Sodium, Physical Activity | Sodium, Physical Activity, Fat, Fruits & Vegetables, Dairy |
| Intervention Delivery Approach: | |||
| Number individual sessions | 2 | 7 | 7 |
| Number group sessions | 0 | 26 | 26 |
Note.
Intervention goals specifically targeted indicated in bold.
Weight loss target for those with BMI ≥ 25
Individual target set for caloric intake to achieve weight loss
JNC V The Fifth Report of the Joint National Committee (JNC) on Detection, Evaluation, and Treatment of High Blood Pressure 43
DASH Dietary Approaches to Stop Hypertension (Appel et al, 1997)
Participants assigned to the Advice-Only comparison condition received verbal advice and materials on lifestyle modifications at the time of randomization and after completion of the 6-month data collection. Recommendations included limiting alcohol and dietary sodium intake, engaging in regular physical activity, losing weight if needed, and eating a healthful diet for general cardiovascular health.
Statistical Analyses
For this report, participants from all 3 randomized groups were classified according to whether they did or did not meet predetermined intervention behavioral goals for physical activity and for dietary intake of sodium, fruits and vegetables, dairy products, and total fat. Although total fat and saturated fat were each separate behavioral targets, we report meeting only the goal of saturated fat because of the high correlation (ρ = 0.80, P<0.001) between the 2 variables. Thus, although there was a maximum of 6 goals targeted, for our analyses we used a total of 5 goals. We classified participants based on the Established plus DASH goals because reaching these targets is most efficacious for reducing cardiovascular disease risk.3 Separate classifications were made at each time point (baseline, 6 months, and 18 months). Prevalence of meeting a specific goal and number of goals met were calculated.
Differences between groups in the number of goals met (0, 1, 2, ≥3) at 6 and 18 months were tested using the Pearson chi-square test. Pearson correlations examined the correlations between change in the behavioral targets to determine which behaviors tended to co-occur. Due to the limited range of values for the number of dairy servings, this variable was excluded from the correlation analysis.
Analyses were conducted using SAS version 8.2 (SAS, Cary, NC, USA). All P-values are 2-sided and the term significant is used to describe a P-value less than 0.05.
RESULTS
Eight hundred ten (n=810) participants were enrolled in the trial. The average age was 50 years, 62% of participants were women, 34% were African American, 95% were overweight or obese, and more than 1/3 met the definition for stage 1 hypertension. At study onset, approximately 40% of participants reported they engaged in at least 180 weekly minutes of moderate to vigorous physical activity, and 32% met the dairy goal of at least 2 daily servings. In contrast, only 5% met the fruit and vegetable goal of at least 9 daily servings. Six- and 18-month data were available for approximately 90% of participants.
The data displayed in Table 2 indicate a substantial improvement in the proportion of participants who met intervention goals at 6 and 18 months. The Established and Established plus DASH intervention groups had the highest prevalence of participants meeting goals, although higher prevalence of goal achievement was also noted for the Advice-Only group. Consistent with the intervention-specific behavioral goals, participants in Established plus DASH had greater prevalence of meeting the dairy, fruits and vegetables, and total fat goals than did the other groups. For example, at 6 months, 33.5% of those in the Established plus DASH group met the goal of at least 9 servings of fruits and vegetables compared with 6.0% and 6.6% in the Established and Advice-Only groups, respectively. Recidivism in meeting goals was noted at 18 months in both intervention groups, but not Advice-Only.
Table 2.
Percent of All Participants (n=810) by Treatment Group Meeting Dietary and Physical Activity Goals of Established + DASH at Baseline, 6 Months, and 18 Months
| Behavioral Goal |
Baseline | 6 months | 18 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Advice- Only N=270-273a |
Established N=266-268 |
Established + DASH N=262-268 |
Advice- Only N=219-243 |
Established N=220-233 |
Established + DASH N=222-237 |
Advice- Only N=235-252 |
Established N=225-241 |
Established + DASH N=227-247 |
|
| ≥180 minutes of weekly moderate to vigorous physical activityb | 106c(38.8%)d | 106(39.6%) | 109(40.7%) | 123(51.0%) | 139(59.9%) | 149(62.9%) | 123(50.8%) | 127(54.0%) | 130(54.2%) |
| ≤100 mmol/d of daily sodium intake | 35(13.0%) | 48(18.0%) | 38(14.5%) | 43(19.6%) | 81(36.8%) | 64(28.8%) | 49(20.9%) | 69(30.7%) | 57(25.1%) |
| ≥2 daily servings of dairy intake | 84(31.1%) | 84(31.3%) | 93(34.6%) | 79(32.5%) | 66(28.3%) | 140(59.3%) | 83(32.9%) | 61(25.3%) | 126(51.0%) |
| ≥9 daily servings of fruits and vegetables | 8(3.0%) | 11(4.1%) | 19(7.1%) | 16(6.6%) | 14(6.0%) | 79(33.5%) | 13(5.2%) | 13(5.4%) | 74(30.0%) |
| ≤25% kcal of daily total fat intake | 42(15.6%) | 40(14.9%) | 41(15.2%) | 45(18.5%) | 68(29.2%) | 135(57.2%) | 49(19.4%) | 68(28.2%) | 113(45.7%) |
Note.
Sample size varies depending on variable
Determined from 7-day physical activity recall (Blair et al 1986; Sallis et al 1985)
Number meeting goal
Percent meeting goal
Figure 1 displays the number of behavioral goals met at baseline, 6, and 18 months by intervention condition. Although all groups, including Advice-Only, increased the number of goals that were met at 6 and 18 months, the figure illustrates the gradient in adoption of behavioral goals from the Advice-Only to Established to Established plus DASH. These differences were most evident at 6 months, but still persisted at 18 months. For the Established plus DASH group, 8% and 3% met all 5 behavioral goals at 6 and 18 months, respectively. The number of behavioral goals met (0 vs 1 vs 2 vs 3 or more) significantly differed between the Advice-Only group and each of the 2 active intervention groups at 6 months (P-values < 0.02), and between the Advice-Only and Established plus DASH groups at 18 months (Table 3) (P-values < 0.0001). At 6 months, 44.6% of participants in Established plus DASH met at least 3 behavioral goals, compared with 19.3% of those in Established and 11.7% in Advice-Only. At 18 months, 33.5%, 11.9%, and 11.0% met at least 3 goals in Established plus DASH, Established, and Advice-Only, respectively.
Figure 1.
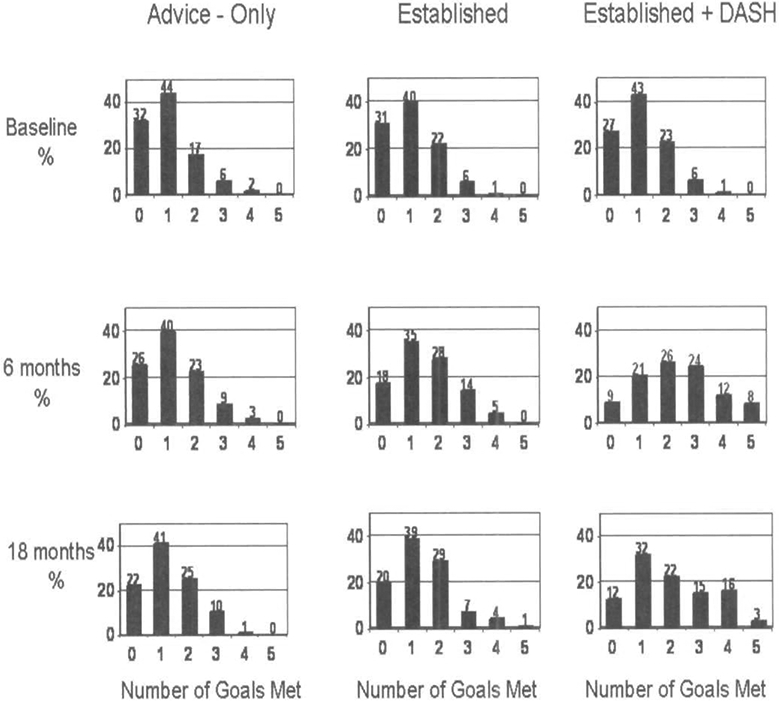
The Percent of Participants by Treatment Group Meeting Behavioral Goals at Baseline, 6 Months, and 18 Months
Table 3.
The Number and Percent of Participants by Treatment Group Meeting 0, 1, 2, or 3 or More Behavioral Goals at Baseline, 6 Months, and 18 Months
| Number of Behavioral Goals Met |
Baseline |
6 months |
18 months |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Advice- Only |
Established | Established + DASH |
Advice- Only |
Established | Established + DASH |
Advice- Only |
Established | Established + DASH |
|
| 0 | 87a(31.9%b) | 83(31.0%) | 73(27.1%) | 64(25.8%) | 42(17.6%) | 21(8.7%) | 57(22.4%) | 49(20.1%) | 31(12.2%) |
| 1 | 120(44.0%) | 106(39.6%) | 115(42.8%) | 99(39.9%) | 84(35.2%) | 50(20.7%) | 105(41.3%) | 95(38.9%) | 81(31.9%) |
| 2 | 47(17.2%) | 59(22.0%) | 61(22.7%) | 56(22.6%) | 67(28.0%) | 63(26.0%) | 64(25.2%) | 71(29.1%) | 57(22.4%) |
| 3 or more | 19(7.0%) | 20(7.5%) | 20(7.4%) | 29(11.7%) | 46(19.3%) | 108(44.6%) | 28(11.0%) | 29(11.9%) | 85(33.5%) |
| Total | 273(100.1%) | 268(100.1%) | 269(100.0%) | 248(100.0%) | 239(100.0%) | 242(100.1%) | 254(100.1%) | 244(100.0%) | 254(100.0%) |
Note.
Number meeting goal
Percent meeting goal
Based on Pearson chi-square test, at 6 and 18 months Established + DASH different from both Advice-Only and from Established (P<0.0001); at 6 months Established different from Advice-Only (P<0.02).
Change in daily total fat intake was negatively correlated with daily number of fruit and vegetable servings (ρ=−0.31, P<0.001) (Table 4). Change in estimated energy expenditure significantly correlated with change in daily sodium intake and change in daily total fat intake, although correlations were low (−0.12 ≤ ρ ≤ 0.12).
Table 4.
Correlations of Baseline to 6 Month Change in PREMIER Intervention Health Behavior Targets
| Baseline to 6-Month Change in: |
|||
|---|---|---|---|
| Baseline to 6-month Change in: |
Daily Sodium Intake (mmol/d) |
Daily Servings of Fruit & Vegetables (number/day) |
Daily Total Fat Intake (% kcal) |
| Estimated Energy Expenditure (kcal/kg/day) | −0.12a n=645 |
0.04 n=694 |
−0.09a n=694 |
| Daily Sodium Intake (mmol/d) | −0.07 n=639 |
0.05 n=639 |
|
| Daily Servings of Fruit & Vegetables (number/day) | −0.31a n=710 |
||
P <0.05
DISCUSSION
All groups were able to increase the number of behavioral goals met at 6 and 18 months, and those who were asked to achieve the most goals (ie, Established plus DASH) succeeded in meeting the most goals. Consistent with concerns raised by Prochaska and Sallis,31 we were unsure if the Established plus DASH group would be able to make the number of behavioral changes required for this treatment arm. Although only a small percentage was able to meet all 5 intervention goals, the Established plus DASH group met more goals than did the Established intervention group. Interventions can successfully target multiple physical activity and dietary goals without negatively impacting goal attainment for those behaviors, at least for the type of patient population targeted in the current trial. Providing concurrent advice about physical activity and dietary changes can be an effective approach to reducing cardiovascular risk.
Although the expectations for the 3 treatment groups were different (no specific physical activity and dietary goals for the Advice-Only group and no formal goals for fruit, vegetable, or dairy intake for the Established group), we applied the most stringent goals (ie, Established plus DASH goals) for our analyses. Given that participants were motivated to enter the trial and were told about the health behavior changes they may have been asked to make, it is understandable that some participants from all 3 assignment groups were able to make the changes needed to meet the goals of the Established plus DASH intervention.
Previous studies have not been consistent regarding the relationship among physical activity and dietary behaviors. Cross-sectional analyses suggest that physical activity and a healthful dietary intake are correlated.32-35 However, comparing a physical activity-only intervention and a physical activity-plus-nutrition intervention in adolescents, Prochaska and Sallis31 found that both interventions resulted in increased physical activity for boys, with only minimal change in fruit and vegetable intake. Others also found that changes in physical activity were not associated with naturally occurring dietary changes among middle-aged and older adults.36
In contrast, our data indicate that making dietary changes was related to improvement in physical activity. We found significant correlations in the hypothesized direction between change in physical activity and change in daily sodium and total fat intake. Because the PREMIER participants had either prehypertension or stage 1 hypertension, they may have had greater motivation to make multiple lifestyle behavior changes than would otherwise healthy individuals. Such motivation may enhance the ability to make multiple behavior changes. When self-efficacy is low and there are numerous barriers to change, changing one behavior at a time may be more successful.37 Multiple behavior change may also be easier with intensive counseling for extended periods of time, as was the case in PREMIER.
There were significant correlations in the hypothesized direction among change in daily intake of total fat and daily fruit and vegetable intake. Some participants may have replaced high-fat foods with additional fruits and vegetables, providing a partial explanation for the high prevalence of meeting 2 or more goals in all treatment groups at 6 and 18 months. However, because the correlations were only of moderate magnitude, other behaviors were combined to meet multiple goals.
We intentionally structured goal setting so the issue of sequence and combinations of targeted goals was determined by the participant. Although the intervention targeted multiple behaviors simultaneously, participants may have chosen to sequentially adopt behaviors. There is an emerging literature on adherence to multiple lifestyle behaviors. Although evidence is building that tailoring interventions to meet individual preferences is preferable to not tailoring intervention strategies,15,38-40 it has not been established if it is more effective for individuals to make multiple health behavior changes simultaneously or sequentially.41 Hyman and colleagues42 reported that intervening simultaneously to address smoking cessation, reduced dietary sodium, and increased physical activity was more effective than addressing each behavior sequentially.
Study Limitations and Strengths
There are several limitations to this study. Some participants were already meeting goals at baseline. Given that baseline goal attainment was comparable across treatment groups, this does not compromise our results. Additionally, participants had to continue these behaviors to meet 6- and 18-month goals. The PREMIER interventions only promoted the health behaviors of physical activity and dietary intake. Estimated daily energy expenditure, daily servings of fruits, vegetables, and dairy, along with percent daily calories from fat were assessed by self-report, which is subject to recall bias. However, previous analyses from this trial indicate that biomarkers of dietary intake patterns from urine collection were consistent with the self-report increases in fruit, vegetable, dairy, and protein intake.20 The dietary and self-reported physical activity measurements are imprecise. Additional measurements at each time point would have enhanced our power to detect associations.
Another limitation is we conducted a secondary analysis using PREMIER, a trial with blood pressure as its primary outcome — not behavioral goal attainment. Prochaska and Sallis31 randomized adolescents to a multifactor (physical activity and nutrition) or single-factor (physical activity) intervention and found no dietary change. Their trial differed in a number of respects, however, including age of participants, intervention delivery mode (computer based), contact frequency (one-time exposure). In contrast, we intervened in adults using multiple face-to-face contacts in group and individual settings. A study design that directly tests the ability of participants to meet few versus many behavior goals would provide important information that our analysis cannot provide.
CONCLUSIONS
Participants were able to meet multiple behavioral goals. Participants in the intervention group who had the most goals to achieve were more likely to meet more goals than were those with fewer behavioral targets. Rather than being overwhelmed by targeting multiple health behaviors, participants were able to meet dietary and physical activity goals. Interventions can promote multiple health behavior change, particularly among motivated individuals at high risk for cardiovascular disease.
Acknowledgments
This work was supported by NIH grants UOl HL60570, UOl HL60571, UOl 60573, UOl HL60574, UOl HL62828.
Contributor Information
Deborah Rohm Young, Department of Epidemiology and Biostatistics, University of Maryland School of Public Health, College Park, MD..
William M. Vollmer, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Abby C. King, Health Research & Policy and Medicine, Stanford Prevention Research Center, Stanford University School of Medicine, Stanford, CA..
Ann J. Brown, Duke Academic Program in Women’s Health, Department of Medicine/Endocrinology, Duke University School of Medicine, Duke University Medical Center, Durham, NC..
Victor J. Stevens, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Patricia J. Elmer, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Shirley Craddick, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
Dana L. Sturtevant, Center for Health Research, Kaiser Permanente Northwest, Portland, OR..
David W. Harsha, Pennington Biomédical Research Center, Baton Rouge, LA..
Lawrence J. Appel, Medicine, Epidemiology and International Health, Johns Hopkins Medical Institutions, Baltimore, MD..
REFERENCES
- 1.Lichtenstein AH, Appel LJ, Brands M, et al. Summary of American Heart Association Diet and Lifestyle Recommendations revision 2006. Arterioscler Thromb Vasc Biol. 2006;26:2186–2191. [DOI] [PubMed] [Google Scholar]
- 2.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 4.Klein S, Sheard NF, Pi-Sunyer X, et al. Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Diabetes Care. 2004;27:2067–2073. [DOI] [PubMed] [Google Scholar]
- 5.Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003;26(Suppl 1):S51–S61. [DOI] [PubMed] [Google Scholar]
- 6.Kushi LH, Byers T, Doyle C, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006;56:254–281. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Service, US Department of Agriculture. Dietary Guidelines for Americans. 6th Edition ed. Washington, DC: US Government Printing Office; 2005. [Google Scholar]
- 8.Diabetes Prevention Program Research Group. Intensive lifestyle intervention or Metformin on inflammation and coagulation in participants with impaired glucose tolerance. Diabetes. 2005;54:1566–1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haskell WL, Alderman EL. Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP). Circulation. 1994;89:975–990. [DOI] [PubMed] [Google Scholar]
- 10.Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–2007. [DOI] [PubMed] [Google Scholar]
- 11.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–393. [DOI] [PubMed] [Google Scholar]
- 12.Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA. 1982;248:1465–1477. [PubMed] [Google Scholar]
- 13.Howard BV, Van HL, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–666. [DOI] [PubMed] [Google Scholar]
- 14.Wing RR, Goldstein MG, Acton KJ, et al. Behavioral science research in diabetes: lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care. 2001;24:117–123. [DOI] [PubMed] [Google Scholar]
- 15.Marcus BH, Albrecht AE, King TK, et al. The efficacy of exercise as an aid for smoking cessation in women: a randomized controlled trial. Arch Intern Med. 1999;159:1229–1234. [DOI] [PubMed] [Google Scholar]
- 16.Hall SM, Tunstall CD, Vila KL, Duffy J. Weight gain prevention and smoking cessation: cautionary findings. Am J Public Health. 1992;82:799–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fine LJ, Philogene GS, Gramling R, et al. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. Am J Prev Med. 2004;27:18–24. [DOI] [PubMed] [Google Scholar]
- 18.Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med. 2005; 165:854–857. [DOI] [PubMed] [Google Scholar]
- 19.Svetkey LP, Harsha DW, Volimer WM, et al. Premier: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics. Ann Epidemiol. 2003;13:462–471. [DOI] [PubMed] [Google Scholar]
- 20.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. [DOI] [PubMed] [Google Scholar]
- 21.Svetkey LP, Erlinger TP, Vollmer WM, et al. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. J Hum Hypertens. 2005;19:21–31. [DOI] [PubMed] [Google Scholar]
- 22.Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485–495. [DOI] [PubMed] [Google Scholar]
- 23.Obarzanek E, Vollmer WM, Lin PH, et al. Effects of individual components of multiple behavior changes: the PREMIER trial. Am J Health Behav. 2007;31:545–560. [DOI] [PubMed] [Google Scholar]
- 24.Eccles JS, Wigfietd A, Motivational beliefs, values, and goals, Annu Rev Psychol. 2002;53:109–132. [DOI] [PubMed] [Google Scholar]
- 25.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985; 122:794–804. [DOI] [PubMed] [Google Scholar]
- 26.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project, Am J Epidemiol. 1985; 121:91–106. [DOI] [PubMed] [Google Scholar]
- 27.The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 28.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 29.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. [DOI] [PubMed] [Google Scholar]
- 30.Funk KL, Elmer PJ, Stevens VJ, et al. PREMIER—A Trial of Lifestyle Interventions for Blood Pressure Control: Intervention Design and Rationale. Health Promot Pract. 2006. [DOI] [PubMed] [Google Scholar]
- 31.Prochaska JJ, Sailis JF. A randomized controlled trial of single versus multiple health behavior change: promoting physical activity and nutrition among adolescents. Health Psychol. 2004;23:314–318. [DOI] [PubMed] [Google Scholar]
- 32.Gillman MW, Pinto BM, Tennstedt S, et al. Relationships of physical activity with dietary behaviors among adults. Prev Med. 2001;32:295–301. [DOI] [PubMed] [Google Scholar]
- 33.Eaton CB, McPhillips JB, Gans KM, et al. Cross-sectional relationship between diet and physical activity in two southeastern New England communities. Am J Prev Med. 1995; 11:238–244. [PubMed] [Google Scholar]
- 34.Emmons KM, Marcus BH, Linnan L, et al. Mechanisms in multiple risk factor interventions: smoking, physical activity, and dietary fat intake among manufacturing workers, Working Well Research Group. Prev Med. 1994;23:481–489. [DOI] [PubMed] [Google Scholar]
- 35.French SA, Hennrikus DJ, Jeffery RW. Smoking status, dietary intake, and physical activity in a sample of working adults. Health Psychol. 1996;15:448–454. [DOI] [PubMed] [Google Scholar]
- 36.Wilcox S, King AC, Castro C, Bortz W. Do changes in physical activity lead to dietary changes in middle and old age? Am J Prev Med. 2000;18:276–283. [DOI] [PubMed] [Google Scholar]
- 37.Glasgow RE, Goldstein MG, Ockene JK, Pronk NP. Translating what we have learned into practice. Principles and hypotheses for interventions addressing multiple behaviors in primary care. Am J Prev Med. 2004;27:88–101. [DOI] [PubMed] [Google Scholar]
- 38.Steptoe A, Doherty S, Rink E, et al. Behavioural counselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease: randomised trial. BMJ. 1999;319:943–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevens VJ, Glasgow RE, Toobert DJ, et al. One-year results from a brief, computer-assisted intervention to decrease consumption of fat and increase consumption of fruits and vegetables. Prev Med. 2003;36:594–600. [DOI] [PubMed] [Google Scholar]
- 40.Strecher V, Wang C, Derry H, et al. Tailored interventions for multiple risk behaviors. Health Educ Res. 2002;17:619–626. [DOI] [PubMed] [Google Scholar]
- 41.Vandelanotte C, De Bourdeaudhuij I, Sailis JF, et al. Efficacy of sequential or simultaneous interactive computer-tailored interventions for increasing physical activity and decreasing fat intake. Ann Behav Med. 2005;29:138–146. [DOI] [PubMed] [Google Scholar]
- 42.Hyman DJ, Pavlik VN, Taylor WC, et al. Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med. 2007;167:1152–1158. [DOI] [PubMed] [Google Scholar]
- 43.The Fifth Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153:154–183. [PubMed] [Google Scholar]


