Abstract
Context:
Certain medications have higher chances of causing adverse effects in geriatric age group. Evidence is against prescribing these medications to the elderly. A list of such medications is called Beers criteria, which was revised by the American Geriatrics Society in 2015.
Aims:
Using the Beer's list as reference, the researchers intend to find the extent and prevalence of potentially inappropriate medication (PIM) in geriatric population residing in different settings.
Settings and Design:
The researchers analyzed prescription pattern of 200 individuals with age ≥65 years, 100 individuals from old-age homes (OAHs) and 100 individuals from a tertiary care hospital. After collecting data, the researchers tallied each prescription with list of drugs in Beers criteria to find all the possible PIMs in both the groups.
Results:
It was found that the average age of residents of OAHs was significantly higher (P < 0.002) than the corresponding group from a tertiary care hospital. The residents of OAHs were also a receiving significantly higher (P < 0.0001) number of PIM than their counterparts from the tertiary care hospital. The average number of PIMs prescribed to females in OAHs was also significantly higher than those in the other group. About 55% of residents of OAHs received at least one PIM, compared to just 26% in the other group. At least 27% of individuals of OAHs received two or more PIMs, compared to just 2% in a tertiary care hospital. Lorazepam was the most commonly prescribed PIM in OAHs, whereas ranitidine was the most common PIM in a tertiary care hospital. Ibuprofen was the second most common PIM, with 15% of OAHs residents receiving this drug, while none of the patients from a tertiary care hospital received ibuprofen.
Conclusion:
All the results point toward a poor prescription pattern in the residents of OAHs compared to those receiving care from a tertiary care hospital.
Keywords: Beers criteria, elderly, geriatric, old-age homes, potentially inappropriate medication, tertiary care hospital
INTRODUCTION
India has the second largest population in the world, with the country hosting world's second largest geriatric population.[1] At the same time, due to urbanization, the concept of traditional Indian joint family is disintegrating. This has led to increasing number of the elderly shifting to old-age homes (OAHs). With increasing age comes the concern of chronic diseases. It has been found that around 45% of elderly Indians have chronic diseases.[2] The problem is exacerbated by the fact that people living in OAHs are away from family members who can take care of them. This has shown to negatively affect the quality of life and health of the elderly living in OAHs.[3] Hence, it is prudent to compare and contrast numerous aspects of life between the two groups of the elderly: those living in OAHs and those residing in their familial homes. Various studies have been made describing the discrepancies in quality of life between these two populations.[3,4,5] However, not much data are available on the differences in medical care. Hence, the present study was conducted to assess the extent and prevalence of the prescription of potentially inappropriate medications (PIMs). PIM is not a complete measure of medical care; however, it gives an idea of the prescription patterns at both locations, which in turn can be used as one of the many indices to measure the quality of care. The elderly are most vulnerable to polypharmacy as they suffer from several comorbidities.[6] Polypharmacy, in turn, increases the chances of prescription of PIMs. In this project, the researchers use the recently updated list of medications in Beers criteria published in 2015 by the American Geriatrics Society.[7] While several different criteria are present for identification of PIM in the elderly, namely STOPP criteria, Beers criteria is the most popular and comprehensive. A comparative study found Beers criteria to be more stringent than STOPP criteria, causing more drugs to be identified as inappropriate than STOPP criteria.[8] Researchers find it important to use a more comprehensive list as the geriatric population is found to be one that is most vulnerable to the adverse effects of PIM.
Objectives
The objective of the study was to compare the extent and prevalence of prescription of PIM between residents of OAHs and geriatric population receiving care from a tertiary care hospital using Beers criteria.
Study method
After obtaining permission from the Institutional Ethics Committee, a cross-sectional descriptive study was conducted for a total of 3 months, on elderly people from two different settings: (a) OAHs and (b) a tertiary care hospital. A total of 200 adults, 100 from each setting, with age ≥65 years were selected randomly. Twelve OAHs were randomly selected from a list of all OAHs in Ahmedabad using a random number generator. Excluded were those OAHs that scheduled regular visits to a hospital or those that were consulted by a specialist. Furthermore, excluded were those patients in OAHs who were actively taking medications from a specialist outside of the primary care physician visiting the facility. Those who went to a tertiary care hospital for any reason (emergency, for example) but were not actively taking medications prescribed by a specialist at the time of study were included in the study (16 patients). The patients at the tertiary care hospital were also randomly selected and as equally divided as possible from both inpatient and outpatient units of medicine, orthopedic, cardiology, and rheumatology departments. Participants who did not give consent were excluded from the project. Also excluded were adults ≥65 years of age at a tertiary care hospital who did not live with their families. Each participant was interviewed after getting appropriate consent. The researchers collected information regarding the generic name of drug. This was done by physically looking at each drug leaflet and confirming it with the patient's prescription. After obtaining the required information from a total of 200 patients, the data were entered and managed on Microsoft Excel (Office 2018). The researchers later analyzed the data using IBM SPSS, statistical package for social sciences. 23.0, (Armonk, New York, USA). Unpaired t-test is used and values with P < 0.05 were considered statistically significant.
RESULTS
Age distribution
The patients included in the study were all above the age of 65 years. Table 1 shows the distribution of age among the patients of two population.
Table 1.
Average number of potentially inappropriate medications
| Number of PIMs | Tertiary care hospital | OAHs | t | P |
|---|---|---|---|---|
| Mean (SD) | 0.28 (0.496) | 0.86 (0.892) | 5.6829 | <0.0001 |
PIM=Potentially inappropriate medication, SD=Standard deviation, OAHs=Old-age homes
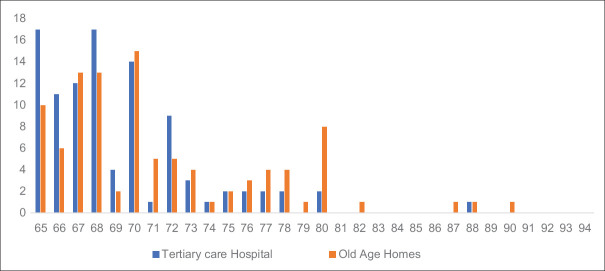
The mean age of the elderly receiving care from a tertiary care hospital was 69.19 years with standard deviation (SD) of 4.10 years while that of those living in OAHs was 71.34 years with SD of 5.562. The difference between mean age of the two groups was statistically significant (P < 0.002).
Average number of drugs prescribed to each population
The average number of drugs prescribed to patients of a tertiary care hospital was 4.8 with a SD of 1.99. The average for residents of OAHs was 4.29 with a SD of 2.39. While the number was higher for patients of a tertiary care hospital, the difference was not statistically significant (P < 0.10).
Average number of potentially inappropriate medications prescribed to each population
There was a significant difference in the average number of PIMs between the two groups.
This difference in prescription pattern can be highlighted further by looking at the number of people in each group receiving at least one PIM [Table 2]. In patients receiving medications from a tertiary care hospital, only 26 out of 100 (26%) received a PIM (1 or more PIMs), whereas 55 out of 100 people (55%) living in OAHs received a PIM (one or more PIMs). In addition, adults living in OAHs had more instances where they were prescribed two or three PIMs.
Table 2.
Frequency distribution of the number of potentially inappropriate medication
| Number of PIMs | Tertiary care hospital | OAHs |
|---|---|---|
| 0 | 74 | 45 |
| 1 | 24 | 28 |
| 2 | 2 | 24 |
| 3 | 0 | 3 |
PIM=Potentially inappropriate medication, OAHs=Old-age homes
List of potentially inappropriate medication according to Beers criteria
In Beers criteria, drugs are categorized according to the quality of evidence (QE) and strength of recommendation (SR). The use of drugs with QE = high is strongly discouraged because of evidence from several well-conducted studies. The use of drugs with QE = moderate is also discouraged as evidence is sufficient to determine the risk of adverse events, but the number, size, consistency, and quality of supporting studies are not up to the standard of QE = high.
As seen in Table 3, drugs prescribed to residents of OAHs carry, on an average, a higher QE.. In those receiving care from a tertiary care hospital, only 1 out of 9 (11%) drugs carried a QE = high, whereas 5 out of 20 (25%) PIMs prescribed to residents of OAHs carried a QE = high.
Table 3.
Name and frequency of potentially inappropriate medication in each group
| PIM | Tertiary care hospital | OAHs | Evidence |
|---|---|---|---|
| Lorazepam | 4 | 17 | QE=High, SR=Strong |
| Ibuprofen | 0 | 15 | QE=Moderate, SR=Strong |
| Diclofenac | 2 | 12 | QE=Moderate, SR=Strong |
| Famotidine | 0 | 7 | QE=Moderate, SR=Strong |
| Alprazolam | 0 | 3 | QE=High, SR=Strong |
| Amitriptyline | 0 | 3 | QE=High, SR=Strong |
| Digoxin >0.125 mg | 3 | 3 | QE=Moderate, SR=Strong |
| Ranitidine | 8 | 3 | QE=Moderate, SR=Strong |
| Spironolactone >25 mg | 4 | 3 | QE=Moderate, SR=Strong |
| Theophylline | 0 | 3 | QE=Moderate, SR=Strong |
| Clonazepam | 0 | 2 | QE=High, SR=Strong |
| Diphenhydramine | 0 | 2 | QE=Moderate, SR=Strong |
| Nicorandil | 1 | 2 | QE=Moderate, SR=Weak |
| Risperidone | 0 | 2 | QE=Moderate, SR=Strong |
| Trifluoperazine | 0 | 2 | QE=Moderate, SR=Strong |
| Chlorpheniramine | 0 | 1 | QE=Moderate, SR=Strong |
| Clonidine | 0 | 1 | QE=Low, SR=Strong |
| Pioglitazone | 0 | 1 | QE=High, SR=Strong |
| Tramadol | 0 | 1 | QE=Moderate, SR=Strong |
| Trihexyphenidyl | 0 | 1 | QE=Moderate, SR=Strong |
| Duloxetine | 1 | 0 | QE=Moderate, SR=Strong |
| Prasugrel | 1 | 0 | QE=Moderate, SR=Weak |
| Sertraline | 4 | 0 | QE=Moderate, SR=Strong |
PIM=Potentially inappropriate medication, QE=Quality of evidence, SR=Strength of recommendation, OAHs=Old-age homes
The most commonly prescribed PIM in residents of OAHs were ibuprofen and diclofenac, while lorazepam was most commonly prescribed PIM in both OAHs and tertiary care hospitals. As seen in Table 4, the number of PIM prescribed to females of OAHs (0.714) was significantly higher (P<0.0038) than that of the other group (0.22). Patients in tertiary care hospitals were mostly prescribed aceclofenac, a comparatively safer nonsteroidal anti-inflammatory drug that is not listed on Beers criteria. Interestingly enough, ranitidine was prescribed in much higher frequency in patients of tertiary care hospitals. Residents of OAHs were prescribed first-generation antihistamines and antipsychotics, which can cause falls and delirium. As seen in Figure 1, the residents of OAHs were significantly older than their counterparts from tertiary care hospital. None of the 100 patients of tertiary care hospitals were prescribed first-generation drugs indicating a higher prevalence of knowledge in physicians of tertiary care hospitals, a trend seen throughout the prescription pattern.
Table 4.
Average number of potentially inappropriate medications prescribed to females in each group
| Number of PIMs | Tertiary care hospital | Old-age homes | t | P |
|---|---|---|---|---|
| Mean (SD) | 0.22 (0.49) | 0.714 (0.88) | 2.98 | <0.0038 |
| Number of females | 37 | 43 |
PIM=Potentially inappropriate medication, SD=Standard deviation, OAHs=Old-age homes
Figure 1.
Age distribution
Females and potentially inappropriate medication
There were 43 females in OAHs and 37 in tertiary care hospitals. The number of PIMs prescribed to females of OAHs (0.714) was significantly higher (P < 0.0038) than that the other group (0.22).
DISCUSSION
The residents of OAHs were significantly older than their counterparts from a tertiary care hospital, which is concerning as older population is more likely affected by the adverse effects of drugs, especially those living in OAHs who have limited access to health-care facilities.[6] Even more alarming is that the average number of PIMs prescribed to females in OAHs was significantly higher (P < 0.0038) than those in a tertiary care hospital. Females are more likely to experience adverse effects from drugs than males and also report a higher number of adverse drug reaction per capita than males.[9,10] The reason for this has been thought to be due to differences in pharmacokinetics of drugs.[10]
Lorazepam is a sedative/hypnotic whose use is strongly discouraged among geriatric population (QE: High, SR: Strong). In addition to memory impairment, the use of benzodiazepines has been linked to falls, fractures, and motor vehicle accidents.[11,12,13,14] The fact that it was the most commonly prescribed PIM among the residents of OAHs adds to the evidence of negligence of care. The number of prescriptions of sertraline, amitriptyline, and first-generation antipsychotics was higher in OAHs. These drugs carry a very high QE against their use in geriatric population.[15]
Lack of specialty care seems to be a plausible factor in differences of prescription patterns in the two settings, since majority of OAH residents received medications from a visiting primary care physician. This is further seen in the fact that majority of residents of OAHs received diclofenac for joint pain, while majority of patients from a tertiary care hospital received aceclofenac, a drug not mentioned in the Beers criteria. Various studies have noted the superiority of aceclofenac over diclofenac in terms of safety and efficacy.[16,17] One of the main reasons for the recommendation of usage of aceclofenac over diclofenac is the reduced number and severity of gastrointestinal adverse effects. The superiority of prescription patterns in patients of a tertiary care hospital is also evident by the fact that while the average number of drugs prescribed to them was higher, though not significantly higher, the average number of PIMs prescribed to them was significantly lower than those in OAHs. A study done by Pakistani authors[18] concludes that prescription patterns of general practitioners in Peshawar consist of over-prescription of analgesics and multivitamins among other drugs. This finding is similar to the finding of the current research in which diclofenac was one of the most commonly prescribed PIMs in residents of OAHs. Such discrepancies in prescription patterns could be caused by various reasons, one of which might be the lack of specialty training of primary care physicians providing care in OAHs.
The WHO has recommended an ideal average upper limit of 2.0 drugs per prescription.[19] Findings of the current research project of an average of 4.8 drugs in a tertiary care hospital and 4.29 in OAHs suggest polypharmacy. The side effects of polypharmacy are unnecessary adverse effects, and interactions amongst different drugs themselves.[20] The fact that the average number of drugs per prescriptions in both the settings is more than twice the recommended ideal average by the WHO raises the possibility of the presence of drug interactions and multiple undocumented adverse effects.
Merits
The researchers successfully documented all the drugs of all the patients in the study. They used the most updated list of drugs in Beers criteria. The present study is unique in that our main objective was to compare the existence of PIM between the OAHs and patients of a tertiary care hospital. No other studies are present that could compare the two groups. The current research project produced unique results in showing exactly which drug was prescribed in abundance in which group (lorazepam and diclofenac in OAHs and ranitidine in tertiary care hospitals). In addition, the research produced results on the existence of significantly higher proportion of PIM prescribed to females, who are more likely to experience adverse effects of drugs. No other studies have produced results specific to females with regard to PIM.
Demerits
The researchers could not tally the dosage of individual drugs and the duration of treatment. They also could not verify the compliance of medications for the patients. Researchers suspect lack of compliance in residents of OAHs due to financial constraints. There is a significant difference in age of both the groups. In older patients with chronic diseases, it is inevitable to prescribe certain medications that might be categorized as PIM since it is very difficult to find an alternative medication for certain diseases (insomnia and palliative care for example). Since data from the psychiatry department of a tertiary care hospital were not included in our study, the difference between the number lorazepam, sertraline, amitriptyline, and first-generation antipsychotic prescription in the two settings might be affected.
Future work
To add on to this comprehensive study, future work can be focused on:
Collecting data on compliance and dosage and duration of each medication
Comorbidities suffered by patients of both the groups and the effect they have on prescription pattern
Tallying the drugs in each group with several other lists of PIM, one of which is the STOPP criteria.
CONCLUSION
Optimal drug therapy is essential in caring for the geriatric population. The changes in metabolism that come with age severely limit the type and dosage of drugs that can be prescribed to elderly. Residents of OAHs are significantly older than their counterparts receiving care at tertiary care hospitals and living with their families. At the same time, residents of OAHs receive significantly higher number of PIM per capita with higher QE than their counterparts. These data point toward a significantly poor prescription pattern in OAHs, which might ultimately add to the morbidity and poor quality of life experienced by its residents.
Financial support and sponsorship
This study was financially supported by the Department of Pharmacology, Smt. NHL Municipal Medical College.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge Dr. Supriya Malhotra from the Department of Pharmacology, Smt. NHL Municipal Medical College for her guidance and encouragement.
REFERENCES
- 1.Ministry of Planning. Eleventh Five Year Plan Document 2007-2012. New Delhi: Government of India; 2008. [Last accessed on 2019 Jan 19]. Available from: http://www.planningcommission.nic.in\plan\planer\fiveyr\11th\11\v1 . [Google Scholar]
- 2.Laxmi Devi S, Roopa KS. Quality of life elderly men and women in institutional and non-institutional settings in urban Bangalore district. Res J Fam Community Consum Sci. 2013;1:7–13. [Google Scholar]
- 3.Amonkar P, Mankar MJ, Thatkar P, Sawardekar P, Goel R, Anjenaya S, et al. A comparative study of health status and quality of life of elderly people living in old age homes and within family setup in Raigad district, Maharashtra. Indian J Community Med. 2018;43:10–3. doi: 10.4103/ijcm.IJCM_301_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A, Mohan U, Singh SK, Manar MK, Tiwari SC, Singh VK, et al. Screening depression among elderly in a city of Southeast Asia. J Clin Diagn Res. 2015;9:LC01–5. doi: 10.7860/JCDR/2015/14100.6426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zalavadiya DD, Banerjee A, Sheth AM, Rangoonwala M, Mitra A, Kadri AM, et al. A comparative study of depression and associated risk factors among elderly inmates of old age homes and community of Rajkot: A Gujarati version of the geriatric depression scale-short form (GDS-G) Indian J Community Med. 2017;42:204–8. doi: 10.4103/ijcm.IJCM_181_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salwe KJ, Kalyansundaram D, Bahurupi Y. A study on polypharmacy and potential drug-drug interactions among elderly patients admitted in department of medicine of a tertiary care hospital in Puducherry. J Clin Diagn Res. 2016;10:FC06–10. doi: 10.7860/JCDR/2016/16284.7273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–46. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 8.Oliveira MG, Amorim WW, de Jesus SR, Heine JM, Coqueiro HL, Passos LC, et al. A comparison of the beers and STOPP criteria for identifying the use of potentially inappropriate medications among elderly patients in primary care. J Eval Clin Pract. 2015;21:320–5. doi: 10.1111/jep.12319. [DOI] [PubMed] [Google Scholar]
- 9.Miller MA. Gender-based differences in the toxicity of pharmaceuticals – The food and drug administration's perspective. Int J Toxicol. 2001;20:149–52. doi: 10.1080/109158101317097728. [DOI] [PubMed] [Google Scholar]
- 10.Ekhart C, van Hunsel F, Scholl J, de Vries S, van Puijenbroek E. Sex differences in reported adverse drug reactions of selective serotonin reuptake inhibitors. Drug Saf. 2018;41:677–83. doi: 10.1007/s40264-018-0646-2. [DOI] [PubMed] [Google Scholar]
- 11.Dassanayake T, Michie P, Carter G, Jones A. Effects of benzodiazepines, antidepressants and opioids on driving: A systematic review and meta-analysis of epidemiological and experimental evidence. Drug Saf. 2011;34:125–56. doi: 10.2165/11539050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Tannenbaum C, Paquette A, Hilmer S, Holroyd-Leduc J, Carnahan R. A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs. Drugs Aging. 2012;29:639–58. doi: 10.1007/BF03262280. [DOI] [PubMed] [Google Scholar]
- 13.Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–60. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 14.Zint K, Haefeli WE, Glynn RJ, Mogun H, Avorn J, Stürmer T, et al. Impact of drug interactions, dosage, and duration of therapy on the risk of hip fracture associated with benzodiazepine use in older adults. Pharmacoepidemiol Drug Saf. 2010;19:1248–55. doi: 10.1002/pds.2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexopoulos GS, Streim J, Carpenter D, Docherty JP. Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(Suppl 2):5–99. [PubMed] [Google Scholar]
- 16.Ward DE, Veys EM, Bowdler JM, Roma J. Comparison of aceclofenac with diclofenac in the treatment of osteoarthritis. Clin Rheumatol. 1995;14:656–62. doi: 10.1007/BF02207932. [DOI] [PubMed] [Google Scholar]
- 17.Pareek A, Chandurkar N. Comparison of gastrointestinal safety and tolerability of aceclofenac with diclofenac: A multicenter, randomized, double-blind study in patients with knee osteoarthritis. Curr Med Res Opin. 2013;29:849–59. doi: 10.1185/03007995.2013.795139. [DOI] [PubMed] [Google Scholar]
- 18.Raza UA, Khursheed T, Irfan M, Abbas M, Irfan UM. Prescription patterns of general practitioners in Peshawar, Pakistan. Pak J Med Sci. 2014;30:462–5. doi: 10.12669/pjms.303.4931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO Action Programme on Essential Drugs. Comparative Analysis of National Drug Policies in 12 Countries: second Workshop. Geneva: World Health Organization; 1997. [Last accessed on 2019 Jan 19]. Available from: http://www.who.int/iris/handle/10665/63513 . [Google Scholar]
- 20.Nguyen JK, Fouts MM, Kotabe SE, Lo E. Polypharmacy as a risk factor for adverse drug reactions in geriatric nursing home residents. Am J Geriatr Pharmacother. 2006;4:36–41. doi: 10.1016/j.amjopharm.2006.03.002. [DOI] [PubMed] [Google Scholar]