Abstract
Background:
Ultrasound has been effective in using low volume of local anesthetics for supraclavicular block. Steroids have been shown to increase the duration of local anesthetics.
Aims and Objectives:
In this study, we compare the efficacy of dexamethasone versus midazolam when added to bupivacaine in supraclavicular brachial plexus block for upper-limb surgeries with regard to the time of onset and duration of sensory and motor blockades, duration of analgesia, sedation, and hemodynamic parameters.
Setting and Design:
This is a prospective, randomized, double-blind study conducted on 60 patients belonging to the American Society of Anesthesiologists physical status classes 1 and 2, undergoing upper-limb surgeries under ultrasound-guided supraclavicular brachial plexus block.
Materials and Methods:
Sixty patients were divided into two groups of 30 each. Group dexamethasone (Group D) received bupivacaine 0.5% 18 mL + dexamethasone 4 mg + 1 mL normal saline. Group midazolam (Group M) received bupivacaine 0.5% 18 mL + 2 mg midazolam. We compared the onset and duration of sensory and motor blocks, hemodynamic variables, pain and sedation scores, and duration of analgesia.
Statistical Analysis:
The statistical software, namely SPSS 18.0 and R environment ver. 3.2.2, were used for the analysis of the data. P < 0.05 was considered statistically significant.
Results:
The onset of sensory and motor blocks was significantly faster in Group D compared to Group M. The duration of sensory and motor blockades and duration of analgesia showed a significant increase in Group D in comparison with Group M.
Conclusion:
Dexamethasone as an adjuvant hastens the onset and prolongs the duration of both sensory and motor blocks and reduces postoperative analgesic requirement when compared to midazolam.
Keywords: Dexamethasone, midazolam, supraclavicular block
INTRODUCTION
Ultrasound has become the cornerstone of peripheral nerve blocks in upper-limb surgeries. The supraclavicular approach provides the easiest and consistent method of anesthesia for below shoulder joint surgeries compared to axillary and infraclavicular approaches.[1] Moreover, a huge volume (30–40 mL) of local anesthetics used in conventional blocks may be associated with complications such as Horner's syndrome, phrenic nerve palsy, and systemic toxicity. The majority of these complications can be overcome using ultrasound-guided technique. The supraclavicular nerve block is ideal for procedures of the upper arm, from the mid-humeral level down to the hand.
The effect of adjuvants has been explored by previous studies, but its role in the context of a lower volume of a local anesthetic agent under ultrasound-guided blocks is still unclear. Adjuncts to local anesthetics for brachial plexus block may enhance the quality and duration of analgesia.[2]
Dexamethasone is a long acting glucocorticoid. When it is administered locally during nerve block, it decreases nociceptive signal transmission and ectopic neuronal discharge. It also exhibits significant anti-inflammatory and antiemetic effects. It prolongs the postoperative analgesia by both central and peripheral mechanisms when administered perineurally.[3]
Midazolam is a water-soluble benzodiazepine which produces an antinociceptive effect and enhances the effect of local anesthetic when it is given epidurally or intrathecally. This effect of midazolam is by its action on gamma-aminobutyric acid-A (GABA-A) receptors present in the peripheral nerves.[4]
In our study, we compared two different groups of drugs as adjuvants to low volume of local anesthetics using ultrasound technique. Since there are not many studies on comparison of a steroid versus benzodiazepine as adjuvants to low volume of bupivacaine in supraclavicular brachial plexus block and also since dexamethasone and midazolam are two commonly available drugs, we undertook this study.
MATERIALS AND METHODS
This is a prospective, randomized, double-blind study conducted at hospitals attached to our institution after obtaining ethical clearance certificate from our hospital ethical committee. The study period was from October 2019 to January 2020. Our study is registered in Clinical Trials Registry – India and CTRI Reg. no. CTRI/2019/10/021555. Sample size was calculated based on the previous study, with the primary outcome measure being the duration of analgesia. Keeping power at 80% and alpha error at 5% and minimum difference of 10%, a minimum of 24 patients would be required. We included 30 patients in each group to compensate for the dropout. The inclusion criteria were patients willing to give written informed consent and aged between 18 and 60 years of either sex, belonging to the American Society of Anesthesiologists (ASA) physical status classes 1 and 2 undergoing elective upper-limb surgeries. Patients with any contraindication to peripheral nerve block and allergy to study drugs were excluded from the study.
Preanesthetic evaluation was done, and the concept of the Visual Analog Scale (VAS) was explained to the patient during recruitment. Patients were premedicated with tablet alprazolam 0.5 mg and tablet ranitidine 150 mg on the night before surgery. After shifting the patient to operating room, standard monitors such as pulse oximetry, noninvasive blood pressure, and electrocardiogram were applied.
Patients were randomly divided into two groups based on random numbers generated by a computer program (www.randomizer.org).
Group dexamethasone (Group D) – Bupivacaine 0.5% 18 mL with 4 mg (1 mL) dexamethasone added to 1 mL normal saline (volume – 20 mL)
Group midazolam (Group M) – Bupivacaine 0.5% 18 mL with 2 mg (2 mL) midazolam (volume – 20 mL).
Allocation concealment was ensured by sequentially numbered opaque sealed envelope method. Block was performed by an experienced anesthesiologist not involved in the study.
A scout scan was performed using a linear high-frequency probe (12 MHz, SonoSite Turbo M5 machine) over the supraclavicular area to rule out anatomical abnormalities including aberrant vasculature. Under all aseptic precautions, ultrasound-guided supraclavicular block was performed using a high-frequency (12 MHz) linear probe using an in-plane approach with a conventional 2.5” long needle with 25G width.
The subclavian artery was taken as a landmark for injection of drugs. The drugs were prepared by an independent consultant, and the person administering the block was unaware of the drug combinations.
The following parameters were noted:
Onset of sensory block: The time taken from the end of the injection to the first dull response to pinprick in the distribution of any of the three sensory nerves in the hand. After injection, patients were assessed for sensory blockade using pinprick
Onset of motor block: From the end of injection until the onset of complete loss of the motor power. Patients with inadequate blockade requiring supplementation were excluded from the study
Hemodynamic parameters: Heart rate, systolic and diastolic blood pressure, and arterial oxygen saturation (SpO2) were measured at 0, 2, 5, 10, 20, and 30 min and thereafter every 15 min till the end of surgery.
Sedation was assessed using the Ramsay Sedation Scale score at 0, 2, 5, 10, 20, and 30 min and repeated every 15 min till surgery was completed.
The duration of sensory block (the time taken between injection of the drug and appearance of sensation) and duration of motor block (the time taken between injection and complete return of motor power) were recorded.
Pain intensity was evaluated using VAS where 0 represents no pain and 10 represents worst possible pain. Rescue analgesia with intramuscular diclofenac injection 75 mg was given if VAS score was ≥4/request for analgesic. VAS score was recorded postoperatively at 0, 1, 2, 6, 12, 20, and 24 h.
The time for the first rescue analgesic was noted.
The duration of analgesia was defined as the time interval between the onset of complete sensory block and the time for request for the first rescue analgesic.
Statistical analysis
Data entered in MS Excel sheet and tabulated. The statistical software, namely SPSS 18.0 and R environment ver. 3.2.2, were used for the analysis of the data. Categorical data were represented as frequencies. Discrete and continuous data were represented as mean (standard deviation) or median (interquartile range). Categorical data – Chi-square (gender and ASA). Quantitative data – Student's t-test (age, body mass index, duration of sensory, motor block, and analgesia). P < 0.05 was considered statistically significant.
RESULTS
In our study, demographic variables were comparable between Group D and Group M [Table 1] [Figures 1-3].
Table 1.
Demographic parameters (n=30)
| Parameters | Group D (n=30) | Group M (n=30) |
|---|---|---|
| Age | 38.67±10.85 | 38.53±10.18 |
| Gender distribution (male:female) | 17:13 | 13:17 |
| Body mass index | 24.08±1.69 | 23.41±1.95 |
| Duration of surgery | 101.67±21.55 | 100.50±25.13 |
Figure 1.
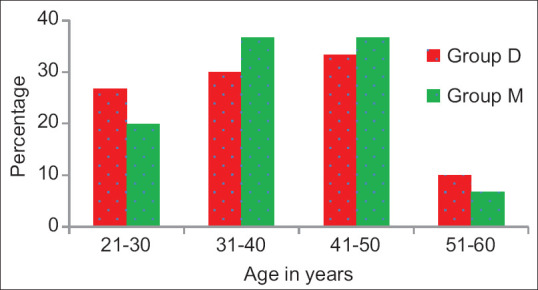
Graph showing distribution of age groups in two groups
Figure 3.
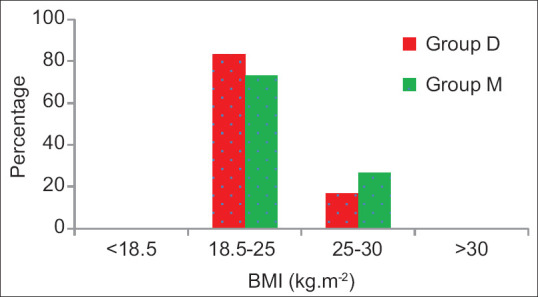
Graph of body mass index in two groups
Figure 2.
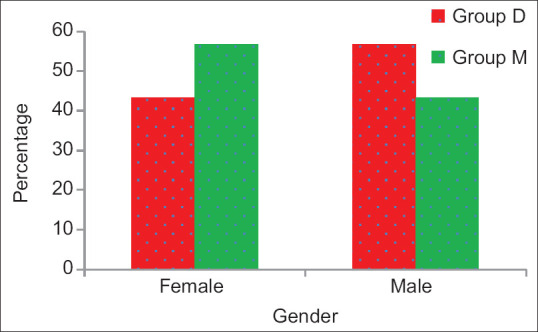
Graph showing gender distribution in two groups
The time of onset of sensory block in Group D was 9.38 ± 1.04 min. The time of onset of sensory block in Group M was 11.23 ± 1.29 min. P value is 0.001 between both the groups with respect to the onset of sensory block, which was statistically significant [Figure 4].
Figure 4.
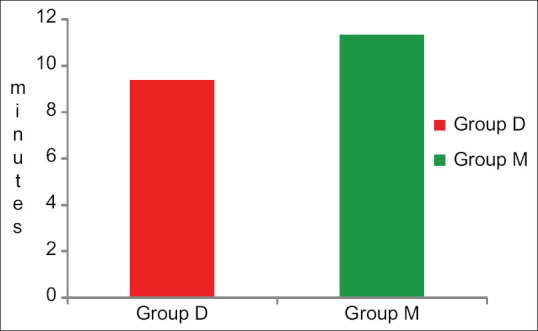
Onset of sensory block comparison between two groups
The onset of motor block in Group D was10.86 ± 1.11 min. The onset of motor block in Group M was 12.25 ± 1.45 min. P value (0.001) was statistically significant between the two groups [Figure 5].
Figure 5.
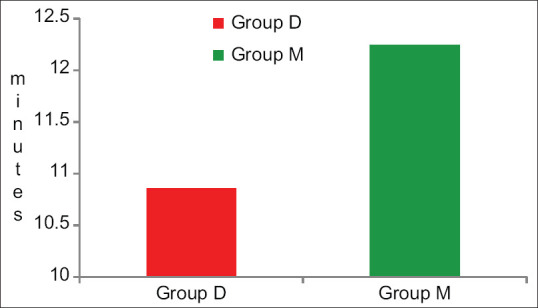
Onset of motor block comparison between two groups
The duration of sensory block was 8.83 ± 1.01 h in Group D and 7.41 ± 0.84 h in Group M. The duration of sensory block was prolonged in Group D when compared to Group M. P value (0.001) was statistically significant between both the groups [Figure 6].
Figure 6.
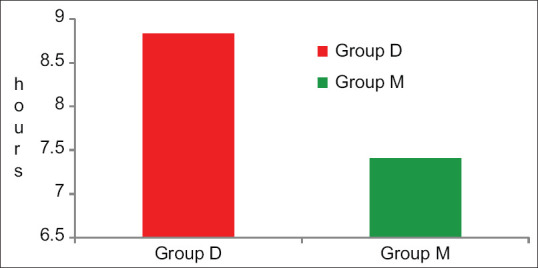
Duration of sensory block comparison between two groups
The duration of motor block was 7.83 ± 0.81 h in Group D and 6.55 ± 0.48 h in Group M. P value (0.001) was statistically significant between both the groups. The duration of motor block was more in Group D when compared to Group M [Figure 7].
Figure 7.
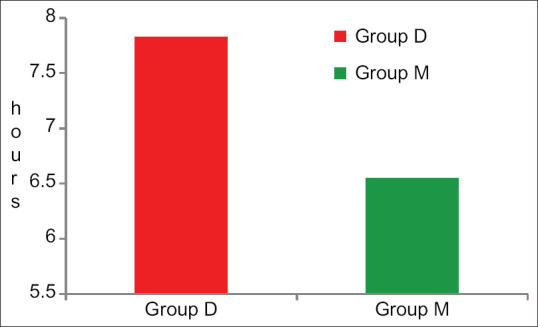
Graph showing duration of motor block comparison between two groups
The duration of analgesia was more in Group D when compared to Group M. The duration of analgesia was 9.68 ± 0.77 h in Group D, whereas in Group M, it was 6.82 ± 1.10. P value is <0.001 between both the groups, which was statistically significant. [Figure 8].
Figure 8.
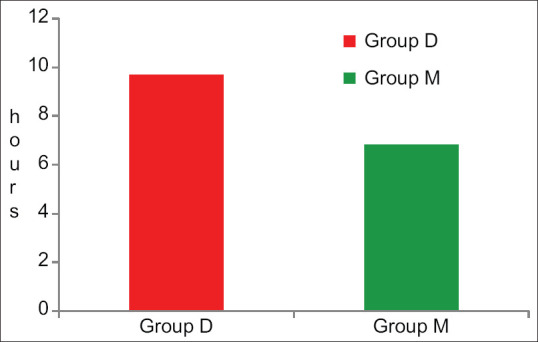
Graph showing comparison of duration of analgesia between two groups
Ramsay Sedation scale Score was comparable between the two groups [Table 2] [Figure 9].
Table 2.
Ramsay Sedation Score
| Ramsey sedation score (min) | Group D | Group M | P |
|---|---|---|---|
| 2 | 2 | 2 | 0.791 |
| 5 | 2 | 2 | 1.000 |
| 10 | 2 | 2 | 1.000 |
| 20 | 2 | 2 | 1.000 |
| 30 | 2 | 2 | 0.009 |
| 45 | 2 | 2 | 0.155 |
| 60 | 2 | 2 | 0.039 |
| 75 | 2 | 2 | 0.155 |
| 90 | 2 | 2 | 0.398 |
| 105 | 2 | 2 | 0.475 |
| 120 | 2 | 2 | 0.484 |
| 135 | 2 | 2 | 0.321 |
| 150 | 2 | 2 | 0.321 |
| 165 | 2 | 2 | 0.321 |
| 180 | 2 | 2 | 0.009 |
Figure 9.
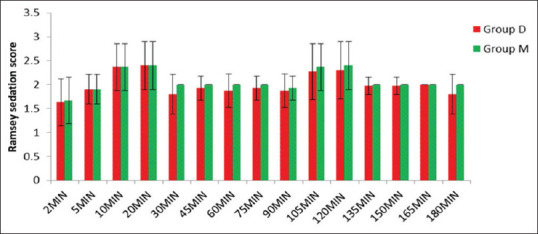
Ramsay Sedation Score
VAS score was significantly more in the midazolam group when compared to the dexamethasone group (P < 0.001) [Table 3] [Figure 10].
Table 3.
Visual Analog Scale score comparison between two groups
| VAS score | Group D | Group M | P |
|---|---|---|---|
| Immediate postoperative | 0 | 0 | - |
| 1 h | 0 | 0 | - |
| 2 h | 0 | 0 | - |
| 6 h | 0 | 3 | <0.001 |
| 12 h | 4 | 7 | <0.001 |
| 24 h | 7 | 7 | 1.000 |
VAS=Visual Analog Scale
Figure 10.
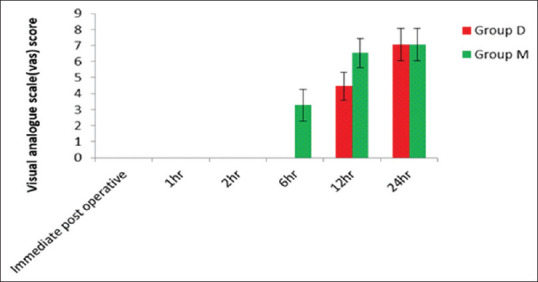
Visual Analog Scale score
Hemodynamic variables such as heart rate and blood pressure were within the normal limits in both the groups [Tables 4 and 5] [Figures 11 and 12].
Table 4.
Hemodynamic variables such as heart rate and mean arterial pressure were comparable between both the groups
| Pulse rate (bpm) | Group D | Group M | P |
|---|---|---|---|
| Baseline | 92.47±13.25 | 88.23±12.89 | 0.215 |
| 2 min | 84.57±7.56 | 82.40±6.58 | 0.241 |
| 5 min | 80.10±7.33 | 79.13±7.06 | 0.605 |
| 10 min | 77.70±7.95 | 76.97±7.22 | 0.710 |
| 20 min | 74.37±7.05 | 74.23±7.32 | 0.943 |
| 30 min | 71.43±6.66 | 71.67±6.71 | 0.893 |
| 45 min | 68.33±6.37 | 69.63±5.44 | 0.399 |
| 60 min | 68.67±7.66 | 68.57±5.18 | 0.953 |
| 75 min | 68.00±7.35 | 66.86±4.34 | 0.480 |
| 90 min | 66.88±6.62 | 65.46±3.41 | 0.353 |
| 105 min | 69.53±6.08 | 65.38±3.52 | 0.040 |
| 120 min | 68.38±5.34 | 65.36±4.43 | 0.197 |
| 135 min | 69.00±4.36 | 65.33±5.43 | 0.347 |
| 150 min | 74.00±0.00 | 65.25±6.08 | 0.288 |
| Immediate postoperative | 66.37±2.57 | 68.33±2.32 | 0.003 |
| 1 h | 67.30±2.42 | 70.30±2.77 | <0.001 |
| 2 h | 72.27±1.72 | 72.37±3.34 | 0.885 |
| 3 h | 72.07±2.70 | 74.07±3.41 | 0.015 |
| 4 h | 75.80±2.58 | 76.83±3.21 | 0.174 |
| 8 h | 81.33±1.99 | 79.37±4.72 | 0.040 |
| 12 h | 77.50±5.71 | 81.57±6.06 | 0.010 |
| 16 h | 82.10±2.43 | 83.53±7.15 | 0.303 |
| 20 h | 83.30±3.04 | 84.73±7.70 | 0.347 |
| 24 h | 83.73±4.23 | 86.00±7.94 | 0.173 |
Table 5.
Mean arterial pressure
| MAP (mm Hg) | Group D | Group M | P |
|---|---|---|---|
| Baseline | 96.23±8.72 | 96.50±8.79 | 0.906 |
| 2 min | 88.47±5.25 | 90.70±5.67 | 0.119 |
| 5 min | 87.10±7.11 | 87.13±6.38 | 0.985 |
| 10 min | 84.83±6.76 | 87.07±6.99 | 0.213 |
| 20 min | 86.90±5.89 | 86.87±6.90 | 0.984 |
| 30 min | 85.43±5.73 | 86.50±7.49 | 0.538 |
| 45 min | 85.90±6.87 | 87.90±8.00 | 0.303 |
| 60 min | 84.53±7.66 | 87.03±7.34 | 0.202 |
| 75 min | 85.66±5.42 | 88.07±7.38 | 0.163 |
| 90 min | 84.36±7.56 | 88.83±7.95 | 0.049 |
| 105 min | 83.80±8.61 | 86.46±7.20 | 0.387 |
| 120 min | 86.56±6.37 | 86.82±7.35 | 0.934 |
| 135 min | 92.33±1.15 | 88.00±5.97 | 0.267 |
| 150 min | 95.00±0.00 | 86.00±4.24 | 0.154 |
| Immediate postoperative | 88.00±6.12 | 75.20±3.65 | <0.001 |
| 1 h | 87.27±5.82 | 81.37±3.85 | <0.001 |
| 2 h | 86.37±5.47 | 84.07±4.03 | 0.069+ |
| 3 h | 85.90±5.25 | 83.93±4.84 | 0.137 |
| 4 h | 84.73±4.66 | 83.93±5.26 | 0.536 |
| 8 h | 84.33±4.73 | 86.13±5.52 | 0.180 |
| 12 h | 84.60±5.24 | 86.37±4.67 | 0.173 |
| 16 h | 84.67±4.91 | 88.47±5.98 | 0.009 |
| 20 h | 85.53±4.26 | 92.43±6.85 | <0.001 |
| 24 h | 86.53±3.40 | 99.67±7.02 | <0.001 |
MAP=Mean arterial pressure
Figure 11.
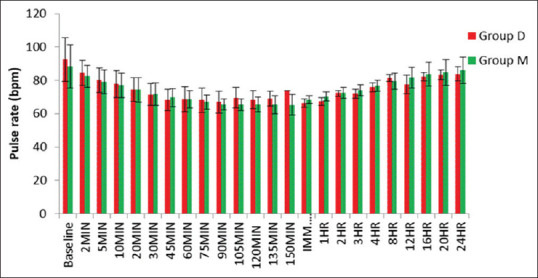
Pulse rate
Figure 12.
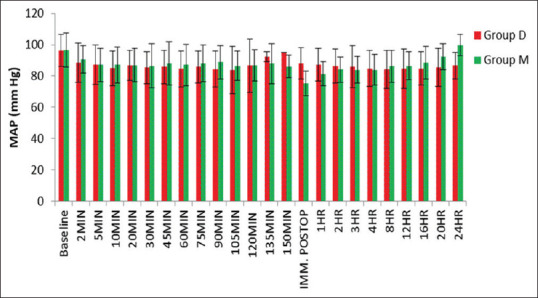
Mean arterial pressure
DISCUSSION
Brachial plexus block is one of the safest and most commonly performed peripheral nerve blocks for upper-limb surgeries. The advantages of brachial plexus block over general anesthesia are effective analgesia, extended postoperative analgesia, avoiding polypharmacy, and early mobilization.[5] Ultrasound-guided block is a safe and reliable technique of regional anesthesia in patients undergoing upper-limb surgeries.[6]
In this study, we compared the effectiveness of dexamethasone and midazolam when used as adjuvants to 0.5% bupivacaine in ultrasound-guided supraclavicular brachial plexus block for upper-limb surgeries.
Steroids are very potent immunosuppressive and anti-inflammatory agents. Dexamethasone is a synthetic glucocorticoid, which prolongs the duration of block through local action mediated through glucocorticoid receptors. Dexamethasone is also known to reduce postoperative nausea and vomiting through its anti-inflammatory effect.[7] Midazolam produces antinociception effect and prolongs the duration of local anesthetics.[8] This effect of midazolam is due to the action of midazolam on GABA-A receptors present in the peripheral nerves.
A meta-analysis concluded that smaller doses of dexamethasone (4–5 mg) were as equally effective as higher doses of dexamethasone (8–10 mg).[9] Hence, we chose a dose of 4 mg of dexamethasone for our study. To make the total volume equal, we chose midazolam dose as 2 mg.
The major finding of this study is that the onset of sensory and motor blocks was significantly faster (P = 0.001) in Group D when compared to Group M. The duration of sensory and motor blocks was significantly more (P = 0.001) in Group D when compared to Group M. The duration of analgesia is more in Group D than in Group M (P < 0.001). Ramsay Sedation Score was comparable between both the groups. VAS score was significantly more in the midazolam group when compared to the dexamethasone group.
Our findings were in accordance with the study conducted by El-Baradey and Elshmaa[10] which showed faster onset of sensory block in the dexamethasone group when compared to the midazolam group and increased duration of sensory block, motor block, and analgesia in the dexamethasone group compared to the midazolam group.
In our study, the duration of sensory block was more than the duration of motor block. This is because the minimal effective concentration of local anesthetics for motor fibers which are larger is greater than for the sensory fibers which are smaller. Hence, the motor function returns before sensory function.[11]
Akkenapalli et al.[11] in their study conducted showed that the addition of midazolam to bupivacaine increased the duration of sensory block and motor block and faster onset of sensory and motor blocks in the midazolam bupivacaine group. The duration of sensory was 13.65 ± 2.01 h in this study which is more than the duration of sensory block in our study. This may be due to the use of higher volume (30 ml) of local anesthetic and dose of midazolam according to body weight in their study.
Engineer et al.[12] found that dexamethasone, when added to bupivacaine, increased the duration of sensory and motor blocks and duration of effective analgesia. The duration of analgesia was more in this study compared to our study, probably due to the use of higher volume of bupivacaine.
Arish et al.[13] in their study found that dexamethasone increases the duration of both sensory and motor blocks when added to bupivacaine, which is similar to our study. Singh et al.[14] conducted a study on addition of midazolam to lignocaine and compared different doses of midazolam and found that addition of midazolam to local anesthetics increases the duration of analgesia. Moharam et al.[15] also concluded that addition of midazolam to local anesthetics increases the duration of effective analgesia which supports our study.
Mathew et al.[16] compared intravenous dexamethasone and perineural dexamethasone in supraclavicular block and found that the perineural dexamethasone group had a faster onset of sensory and motor blocks.
In our study, hemodynamic variables such as heart rate and blood pressure were within the normal limits in both the groups, which is in agreement with the other studies.
There were no significant side effects observed in our study.
CONCLUSION
Dexamethasone as an adjuvant hastens the onset and prolongs the duration of both sensory and motor blocks and reduces postoperative analgesic requirement when compared to midazolam.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alarasan AK, Agrawal J, Choudhary B, Melhotra A, Uike S, Mukherji A. Effect of dexamethasone in low volume supraclavicular brachial plexus block: A double-blinded randomized clinical study. J Anaesthesiol Clin Pharmacol. 2016;32:234–9. doi: 10.4103/0970-9185.182108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vadhanan P, Ganesh N, Ahmed MI. Comparison of dexamethasone and buprenorphine as adjuvant in ultrasound-guided brachial plexus blocks: A randomized controlled trial. Anesth Essays Res. 2018;12:176–9. doi: 10.4103/aer.AER_129_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huynh TM, Marret E, Bonnet F. Combination of dexamethasone and local anaesthetic solution in peripheral nerve blocks: A meta-analysis of randomised controlled trials. Eur J Anaesthesiol. 2015;32:751–8. doi: 10.1097/EJA.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes S, Deshmukh V. Prospective randomised study to evaluate the efficacy of midazolam as an adjuvant to local anaesthetics in brachial plexus block. Int J Contemp Med Res. 2016;3:1542–6. [Google Scholar]
- 5.Kaur M, Kaur R, Kaur S, Baghla N, Bansal A, Kalia A, et al. A study to compare the analgesic efficacy of dexmedetomidine and fentanyl as adjuvants to levobupivacaine in ultrasound-guided supraclavicular brachial plexus block. Anesth Essays Res. 2018;12:669–73. doi: 10.4103/aer.AER_64_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parveen S, Jan M, Taj A, Bhat AA. Effect of dexamethasone as an adjuvant with bupivacaine in ultrasound guided single shot supraclavicular brachial plexus block in upper extremity surgeries-a prospective randomized study. Int J Res Med Sci. 2017;5:2139–43. [Google Scholar]
- 7.Kaur M, Lakhani A, Hashia AM. Comparative study between dexamethasone and dexmedetomidine in supraclavicular block. Int J Adv Med. 2018;5:57–61. [Google Scholar]
- 8.Mishra JC, Maharana PK. A clinical comparison between bupivacaine midazolam combination and bupivacaine plain in brachial plexus block by supraclavicular approach. IAIM. 2017;4:106–14. [Google Scholar]
- 9.Knezevic NN, Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia for brachial plexus block improves pain but delays block onset and motor blockade recovery. Pain Physician. 2015;18:1–4. [PubMed] [Google Scholar]
- 10.El-Baradey GF, Elshmaa NS. The efficacy of adding dexamethasone, midazolam, or epinephrine to 0.5% bupivacaine in supraclavicular brachial plexus block. Saudi J Anaesth. 2014;8:S78–83. doi: 10.4103/1658-354X.144083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akkenapalli AK, Sasidhar GV. A comparative study of brachial plexus block using bupivacaine with midazolam and bupivacaine alone in upper limb surgeries. IAIM. 2016;3:69–77. [Google Scholar]
- 12.Engineer SR, Patel R, Bishnoi A, Umrigar CM. Dexamethasone as an adjuvant to bupivacaine in brachial plexus block in upper limb surgery. Int J Sci Rep. 2017;3:265–70. [Google Scholar]
- 13.Arish BT, Babu DD, Lazarus SP, Chandar DD, Balasubramanian S, Kumar KS. Effect of dexamethasone as an adjuvant to local anesthetic in supraclavicular brachial plexus block. Int J Sci Stud. 2016;3:147–53. [Google Scholar]
- 14.Singh J, Verma V, Sood P, Thakur A, Rana S, Thakur L. Midazolam as an adjunct to lignocaine at two different doses in ultrasound-guided supraclavicular brachial plexus block: A randomized controlled trial. Ain-Shams J Anaesthesiol. 2016;9:549–57. [Google Scholar]
- 15.Moharam SA, Basuoni AS, Abd-elhafez AA, Ibrahim AS. Evaluation of midazolam as an adjuvant to bupivacaine in supraclavicular brachial plexus block. Tanta Med J. 2017;45:99–03. [Google Scholar]
- 16.Mathew R, Radha KR, Hema VR. Effect of perineural and intravenous dexamethasone on duration of analgesia in supraclavicular brachial plexus block with bupivacaine: A comparative study. Anesth Essays Res. 2019;13:280–3. doi: 10.4103/aer.AER_15_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


