Abstract
Most psychiatric disorders develop during adolescence and young adulthood and are preceded by a phase during which attenuated or episodic symptoms and functional decline are apparent. The introduction of the ultra-high risk (UHR) criteria two decades ago created a new framework for identification of risk and for pre-emptive psychiatry, focusing on first episode psychosis as an outcome. Research in this paradigm demonstrated the comorbid, diffuse nature of emerging psychopathology and a high degree of developmental heterotopy, suggesting the need to adopt a broader, more agnostic approach to risk identification. Guided by the principles of clinical staging, we introduce the concept of a pluripotent at-risk mental state. The clinical high at risk mental state (CHARMS) approach broadens identification of risk beyond psychosis, encompassing multiple exit syndromes such as mania, severe depression, and personality disorder. It does not diagnostically differentiate the early stages of psychopathology, but adopts a “pluripotent” approach, allowing for overlapping and heterotypic trajectories and enabling the identification of both transdiagnostic and specific risk factors. As CHARMS is developed within the framework of clinical staging, clinical utility is maximized by acknowledging the dimensional nature of clinical phenotypes, while retaining thresholds for introducing specific interventions. Preliminary data from our ongoing CHARMS cohort study (N = 114) show that 34% of young people who completed the 12-month follow-up assessment (N = 78) transitioned from Stage 1b (attenuated syndrome) to Stage 2 (full disorder). While not without limitations, this broader risk identification approach might ultimately allow reliable, transdiagnostic identification of young people in the early stages of severe mental illness, presenting further opportunities for targeted early intervention and prevention strategies.
Keywords: at-risk (youth), transdiagnostic, pluripotency, clinical staging model, at risk mental state
Introduction
Over the past decade, we have observed increased public awareness of the prevalence and debilitating consequences of severe mental illness. A substantial contributor to the burden of severe mental illness can be the long, progressive illness trajectories that typically become established early in a person's life, generally during adolescence, or late childhood (1, 2). Consequently, there has been a move toward early identification and intervention frameworks, with the aim of reducing the burden by halting the progression of illness or preventing the onset of disorder altogether (3–5).
However, a successful move toward earlier identification and intervention requires a different operationalisation of psychopathology than its current, increasingly criticized, form. Current diagnostic and research systems are less appropriate for these early approaches, as they are based on cross-sectional features observed in entrenched or chronic mental illness, thus embodying the “end-state” of illness trajectories only, failing to represent the progressive and dynamic nature of (emerging) psychopathology (6, 7). Analogically speaking, this corresponds to relying on descriptions of cancer based on final stages of the disease only, ignoring any earlier cell anomalies and their progressive dynamics which might have been present for years. Furthermore, the staggering extent of co-morbidity (8, 9) and phenomena present across disease entities, such as psychomotor slowing, agitation, anhedonia, or delusions, especially early in illness trajectories (10–14), do not support the status quo of separate diagnostic classes. Similarly, a rapidly emerging body of research investigating interacting symptom networks demonstrates widespread and significant interconnections between different diagnostic entities (15–17).
Despite the barriers caused by the current operationalization of mental illness, researchers in Australia initiated a significant move toward pre-emptive psychiatry and early intervention by developing the ultra-high risk (UHR) criteria two decades ago (18). The clinical criteria, identifying young people at risk of developing first episode psychosis (FEP) by a combination of attenuated/short-lived psychotic symptoms and/or trait vulnerability1, did not rely on thresholds provided by current diagnostic systems. The UHR paradigm was developed based on the long-standing understanding that psychotic disorders do not emerge “out of the blue,” but typically have a forerunner phase characterized by milder symptomatology and functional decline (18, 20, 21). This paved the way for a clinical staging model as further outlined below. Three decades later, a multitude of studies have shown that these criteria have a valence for psychosis, as well as for other disorders (mainly anxiety and depression) (22–24), further challenging the siloed approach to diagnostic systems. Similarly, only a small proportion of young people in FEP programs linked to UHR programs go through UHR clinics first (25), implying that there might be alternative early symptom trajectories leading to psychosis, which might be missed by services focusing exclusively on (attenuated) psychotic symptoms (21). These observations, and the modest proportion of UHR young people transitioning to psychosis in research trials [~20% over 2 years (26)] causing statistical challenges for the design of intervention studies (27), highlight the need for the development of a broader, transdiagnostic at-risk approach.
The great challenge lies in developing these wider, transdiagnostic frameworks for early risk identification while maximizing clinical utility. Guided by the principles of the clinical staging framework, we will introduce the concept of a pluripotent at-risk mental state. First, we will provide a theoretical overview of the underpinnings of clinical staging and pluripotency; second, we will present the Clinical High At Risk Mental State (CHARMS) approach and some preliminary data of this ongoing cohort study.
Clinical Staging
“Sub-threshold” versions of mental disorders (i.e., conditions that fall below the threshold of “caseness” as defined by psychiatric diagnostic systems), frequently precede later full syndrome disorders (28), aligning with the increasingly prevailing notion that there is no clear-cut demarcation between absence and presence of mental disorder (29, 30). Dimensional models of mental disorder conceptualize psychopathology on a continuum of severity, ranging from mild liability or expression at one end of the spectrum to fully-fledged, chronic and treatment-resistant disease at the other (31–34). While the view of a continuum of illness and illness progression has gained traction, it poses a challenge for the process of clinical decision making and clinical communication, which inherently requires thresholds (35, 36). Clinical staging, a framework adapted from other areas of medicine, adopts the dimensional approach to mental illness while offering step-wise anchors for phase-specific treatment selection (6, 37, 38). In other words, a person's clinical presentation is mapped onto the spectrum of mental illness, informing intervention plans, and offering a prognosis of potential trajectories of progression and remission (5). In clinical practice, this translates into less aggressive, safer, and more targeted treatment approaches. Rather, a staged care approach recognizes the need for interventions that are tailored according to symptom severity, allowing clinicians to provide low-intensity interventions for patients with milder presentations along the spectrum of illness, prior to reaching a full-threshold disorder.
Stages are defined using symptom severity, specificity, persistence and disability. An early stage is typified by mild symptom severity, a lack of specificity, mild functional impairment; an advanced stage is associated with severe symptom burden, clearer syndromal specificity and stability, significant functional impairment and persistent/recurrent patterns (39, 40). The original clinical staging model spans from stage 0 to stage 4, starting with an at-risk but asymptomatic state (Stage 0) and increases in severity to help seeking, nonspecific symptoms (Stage 1a), attenuated syndrome (stage 1b), full-threshold disorder (Stage 2), recurrence and persistence of illness (Stage 3), and lastly severe and chronic mental health disorders (Stage 4). A revised version of the clinical staging model, currently only focused on psychosis, has been formulated (41). This model further segregates Stage 1 (“high-risk”) into three sub-stages with increasing symptomatic specificity, moving from negative/cognitive symptoms (1a) and attenuated symptoms (1b) to short lived remitting episodes (1c). Stage 3 (“late/incomplete recovery”) is also further subdivided into three stages, moving from single relapse (3a) over multiple relapses (3b) to incomplete recovery from first episode (3c).
A key assumption of the clinical staging framework is that a return to previous stages is not possible. For example, a client in Stage 3a can fully remit, i.e., a “Stage 3 in full remission”; however, they cannot return to a “Stage 0” nor to “Stage 1.” In fact, remission and recovery is an integral part of the staging process. Stage 2 is associated with symptomatic and functional early full recovery (remission). Stage 3 is associated with late/incomplete recovery in any symptomatic or functional domain while Stage 4 is severe, persistent, or unremitted illness (41). Recent research has shown that 20% of individuals identified to be at Stage 1b progressed to a more severe stage within 12 months (42). Interrater reliability for the clinical staging model has been found to be adequate, with 90% concordance between independent raters (k = 0.72) (39). Cross et al. (43) identified a range of variables in transdiagnostic samples with attenuated symptoms (Stage 1b) which were associated with progression to a full-threshold disorder (Stage 2) such as not being in education, being unemployed and greater negative symptom severity (43).
The aim is to further develop clinical staging into a clinicopathological framework, linking clinical features with objective pathophysiological measures, improving precision of intervention and prognosis (6). Most importantly, it is a diagnostic framework that increases clinical utility.
A Pluripotential at Risk Mental State: CHARMS
The shortcomings of current diagnostic classification systems, new findings regarding the dynamic and overlapping nature of psychopathology and its heterotypic trajectories, including lessons learned from the UHR paradigm regarding specificity and predictive values, all indicate that we need a new, less siloed, and early risk identification approach. This led to the development of the CHARMS (Clinical High At Risk Mental State) identification strategy, a pluripotential at-risk mental state which broadens both inputs and outputs beyond psychosis and maximizes clinical utility by building on the clinical staging framework (5, 21, 44–47). Currently, we are in the process of conducting a pilot study validating and further refining the “CHARMS criteria.” The CHARMS criteria are a set of clinical criteria that define a pluripotential at risk mental stage as described above and capture risk for a range of different outcomes (see below). Operationally, the CHARMS criteria are a broadening of the existing UHR criteria, extending it from UHR (capturing subthreshold versions/genetic vulnerability for psychotic disorder) to capturing subthreshold versions/genetic vulnerability for affective (unipolar and bipolar depression) and borderline personality disorder (BPD). The decision to also include BPD was informed by evidence that young people with emerging BPD features show non-specific and evolving mixtures of signs and symptoms that substantially overlap with precursors of bipolar and psychotic disorder, recognizing that the early stages of these disorders cannot yet be disentangled adequately to support disorder-specific identification frameworks and preventative interventions (48–50).
CHARMS is an extension of the UHR state and represents the clinical operationalisation of the first stage requiring significant clinical attention in the clinical staging model, that is, Stage 1b. Therefore, recruitment into the CHARMS cohort study is based on presentation to services (i.e., headspace centers in metropolitan Melbourne, Orygen Specialist Clinical Services) rather than based on presence of specific diagnoses.
The Term Pluripotency
The idea of a “pluripotential at risk mental state,” introduced for the first time by Johannessen and McGorry (51) has attracted criticism and misconceptions based on the term used. First, there has been a perception in the literature that the term “pluripotent risk” refers to the existing UHR operationalisation, i.e., the UHR for psychosis state itself is considered pluripotent in that it predicts the onset of disorders other than psychosis (52–55). While UHR is indeed part of CHARMS, the idea of a pluripotential at-risk mental state was always to broaden both input and output points, thus moving beyond UHR for psychosis and considering other mental disorders (44). Second, the term “pluripotential” should be interpreted in light of the clinical staging framework, rather than through the lens of cell biology or oncology as some critics have done (56). Literally, “pluri” refers to several, “potential” refers to capable or possible: It reflects the potential for the picture to evolve into several syndromes or outcomes (51), akin to heterotypy. In other words, we remain agnostic about the future trajectory of the disorder, and simply maintain that a broad range of outcomes are possible. This is not to say that all mental illness is a manifestation of the exact same origin, and the specific trajectory is a result of environmental influences (57). As an example, we do not assert that every young person meeting CHARMS criteria, regardless of clinical presentation and genetic make-up, placed in a certain environment, is capable of developing a particular syndrome. Rather, the CHARMS criteria aim to identify young people who are presenting with unspecified, sub-threshold levels symptoms consistent with stage 1b of the clinical staging model, and therefore considered to be a population with a high risk of transition to a range of full threshold disorders.
Specificity Might Increase Over Time
Among the core principles of CHARMS is the assumption that psychopathology in its earliest stages is protean and non-specific, with greater specificity for certain disorders gained in later stages (58). This is not too dissimilar from the view of a general “liability” psychopathology factor crystallizing into more specific conditions with increasing age (“p-differentiation”) (59–61). While the empirical evidence for p-differentiation has been mixed, these studies have investigated differentiation as a function of age rather than illness severity as suggested by the clinical staging framework.
Another source of support for later, more stable symptom patterns stems from studies investigating the network structure of psychopathology. These studies show that there is increasing connectivity in symptom networks with increasing levels of severity (62–65), pointing toward increasing stability in psychopathology. While a recent study failed to demonstrate increase in global network structure with increasing severity (66), network findings are generally in line with large epidemiological studies. These epidemiological studies have shown how non-specific states in children and adolescents, usually characterized by anxiety and depressive symptoms, develop into more stable adult-type major mood (depression, bipolar) or psychotic disorders (11, 67–69). For this reason, CHARMS proposes a transdiagnostic “lumping” approach (i.e., not differentiating between diagnostic entities as defined by international diagnostic symptoms), representing the most useful approach for providing healthcare to young people with undifferentiated clinical representations. By doing so, it also provides a sampling frame for prospectively researching the evolution of early stages of severe mental disorder, which has been hampered to date by the “diagnostic silo” approach to risk identification. Furthermore, it aligns with studies demonstrating the shared genetic and neurobiological basis of mental illness, as well as the number of shared environmental risk factors (70–73), as further outlined below.
Transdiagnostic
The transdiagnostic approach “involves trying to understand the shared, overarching processes that cut across the classification system” [(74), p. 360]. Although suggested otherwise by some authors (75, 76), the clinical staging framework adopts a transdiagnostic approach. This is in line with the “Research Domain Criteria” (RDoC) introduced by the National Institute of Mental Health (NIMH) (77–79) and the Hierarchical Taxonomy of Psychopathology (HiTOP) (80, 81).
RDoC aims to “implement, for research purposes, a classification system based upon dimensions of observable behavior and neurobiological measures” (78). In other words, the biopsychological basis of fundamental psychological constructs (e.g., reward seeking, memory, and fear) are explored and linked to clinical phenotypes (79). RDoC has primarily been developed as a research tool, not as an aid for practical clinical decision making. It aims to find (biological) explanations for clinical problems and to inform clinical schemes, such as the clinical staging framework. It also does not incorporate the temporal or dynamic aspect and does not facilitate early identification purposes. Thus, RDoC represents a framework complementing CHARMS and clinical staging, rather than representing a competing framework.
Similar to RDoC, HiTOP represents a hierarchical, dimensional approach to psychopathology, with lower-level syndromes based on empirical covariation of signs and symptoms which form higher-level spectra based on covariation of syndromes (80–82). This idea is related to the concept of micro-and macro phenotypes first articulated by van Os (83). In the context of HiTOP, the p-factor can be seen as very broad “super-spectrum,” representing features shared across all mental disorders (81). As stated above, the p-factor and CHARMS approach have the same underlying idea of an underlying vulnerability for psychopathology that is not differentiated by disorder. However, the p-factor describes a transdiagnostic structure (i.e., a factor which is present across disorders). In contrast, the term “transdiagnostic” in CHARMS does not necessarily refer to a common shared factor, but rather to not differentiating or not separating into diagnostic silos according to clinical presentation.
Similar to HiTOP, aiming to integrate the traditionally separate domains of personality and psychopathology (84, 85), the CHARMS approach also aims to bridge the traditional separation between personality and psychopathology. The CHARMS criteria include borderline personality pathology, as this represents a general severity factor in personality pathology (86) and because subthreshold borderline pathology is clinically significant in young people (87).
The transdiagnostic approach in CHARMS has been criticized for pooling together potentially different phenotypes and illness trajectories, thereby interfering with individual risk prediction and specific treatment development (88). However, the CHARMS approach does not prohibit the identification of specific illness trajectories or risk factors for specific phenotypes (see below).
Homotypic vs. Heterotypic Continuity of Psychopathology
There is evidence that young people at UHR for psychosis also have incident or persistent disorders other than psychosis (22–24). Similarly, there is evidence that young people at risk for non-psychotic disorders (such as depression) might develop psychotic disorders (54). Both these trajectories are examples of heterotypic development, i.e., one condition predicting another condition at a later time point (89) There is increasing evidence for heterotypic continuity in children and adolescents (14, 90, 91). For example, a recent study in the ALSPAC cohort (N = 4,815, ages 7.5–14 years) demonstrated widespread heterotypic continuity, even when controlling for homotypic continuities (92). However, heterotypic continuity is also observed in “established” disorder (9, 93). A recent Danish registry study (N = 5,940,778) showed that any given index mental illness is associated with an increased risk of developing any other mental illness, even across diagnostic class (94). Similarly, the Dunedin Study birth cohort (N = 1,037) demonstrated that mental disorder life history traverse across internalizing, externalizing, and thought disorders and all disorders are associated with an increased risk for all other disorders (95). These studies support the idea that mental disorder categories are not a static. Rather, they are highly dynamic process that ought to be considered from a developmental perspective. It also provides support for the idea of pluripotentiality, i.e., it might be useful to not specify the “terminus” of an illness trajectory. The clinical staging/CHARMS approach allows for both (capturing of) homotypic progression (e.g., young person with depressive symptoms without significant comorbidities goes on to develop recurrent depression) and heterotypic progression (e.g., young person with depressive and attenuated psychotic symptoms goes on to develop first episode mania). This will allow one to investigate and specify stable (homotypic, transdiagnostic) continuity, as well as heterotypic, disorder specific continuity (96).
The Power Problem and Prevention Paradox
By widening the outcome target and including high-prevalence disorders such as depression, we not only allow for heterotypic development on a conceptual level, but also allow for greater statistical power at a methodological level. As originally noted by Cuijpers (27), prevention trials rarely investigate whether they are, in fact, able to reduce the incidence of the disorder in question, as the number of participants needed for this is high, especially if the incidence of the target syndrome is low. This is partly explained by the relative non-specificity of known risk factors, as discussed above. By increasing the incidence rate of the target outcome in the population, we drastically reduce the number of participants needed to achieve adequate statistical power. The CHARMS approach increases the incidence rate of new disorders by following all three recommendations by Cuijpers (27): (1) focusing on indicated prevention (symptoms are present without reaching “full threshold”), (2) focusing on high-risk groups with multiple risk factors, and (3) focusing on target groups with multiple disorders. This approach also addresses the “prevention paradox” and “relative blindness” raised in traditional UHR research (45, 97, 98).
The CHARMS Study: Study Details and Preliminary Findings
As mentioned, we are in the process of conducting a pilot study validating and further refining the “CHARMS criteria.” The CHARMS criteria can be sub-divided into four at-risk mental states: high risk for psychosis (UHR), high risk for severe depression (HRD), high risk for mania (HRM), and high risk for borderline personality disorder (HRB), although this division is not the focus of the study. Guided by the UHR criteria, the CHARMS criteria are based on subthreshold symptoms (comprising attenuated psychotic, moderate depressive, subthreshold manic symptoms, and BPD features), trait vulnerability and functional decline. For a detailed description of the criteria, see Hartmann et al. (46). As the focus of this study is on the (broad) early clinical phase of illness, all clients of our clinical services are eligible for the study regardless their presentation, unless full-threshold for illness (the main outcome of the study) has already been reached. That is, inclusion comprises one criterion: Help-seeking at our clinical services. Exclusion criterion comprises ≥ Stage 2 of illness. Important for recruitment, and key to the underlying CHARMS risk identification approach, are our headspace enhanced primary care services. headspace represents a transdiagnostic early intervention service for young people aged 12–25 with a range of subthreshold and threshold presentations and is the main recruitment source for the CHARMS study. Recruitment also takes place at Orygen Specialist programs (a secondary mental health service), however given our exclusion criterion of ≥Stage 2 and the more severe clinical presentation at the specialist programs compared to headspace, this is a minor source.
Consenting participants meeting the CHARMS criteria at baseline are allocated to CHARMS+ (i.e., Stage 1b). Those falling below threshold are allocated to CHARMS– (i.e., Stage 1a, the control group). Participants meeting criteria for Stage 2 (for example, first episode psychosis or mania) are excluded. Participants are re-assessed after 6 and 12 months.
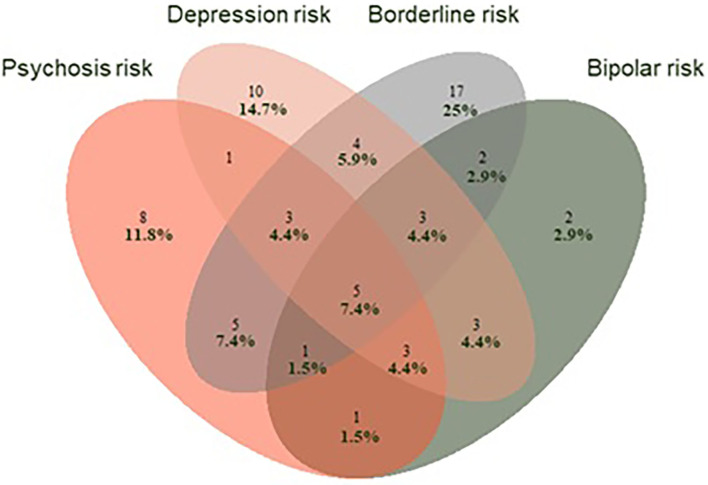
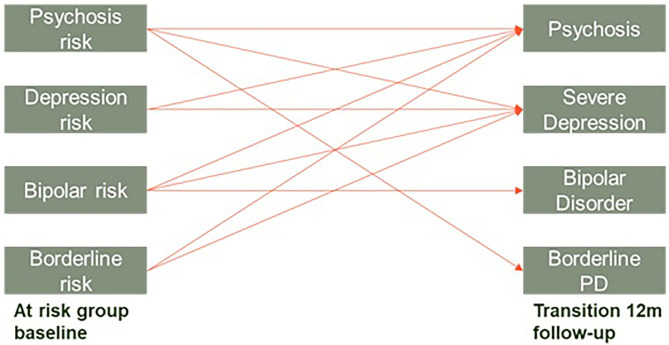
Our preliminary results (sample N = 114, ongoing recruitment) support the CHARMS concept. Sixty-eight percent of participants (68%) met CHARMS criteria at baseline and were allocated to the CHARMS+ group with the remainder allocated to the CHARMS– control group (please see Table 1 for an overview of clinical and demographic variables). Of the CHARMS+ group, almost half (46%) satisfied the criteria for more than one at-risk group. Figure 1 demonstrates the extensive overlap between the four different at-risk mental states. Of those who have completed the month 12 assessment in the CHARMS+ group thus far (N = 78), 34% have transitioned to a Stage 2 disorder (mostly severe depression), compared with 3% in the CHARMS- group. Survival analysis (Kaplan Meier) on these preliminary data show a significant difference in these transition rates between the two groups (p = 0.004). Interestingly, the risk for transition (by 12 months) to Stage 2 in the CHARMS+ group increases to 40% if three or more at risk states are met. When we investigate the patterns of transition, we see homotypic (e.g., a young person meeting high-risk for psychosis transitions to first-episode psychosis) as well as heterotypic development [e.g., a young person meeting high-risk for psychosis transitions to severe depression (Figure 2)], further supporting the CHARMS approach.
Table 1.
Preliminary baseline characteristics.
| Total | CHARMS+ | CHARMS– | P-value* | |
|---|---|---|---|---|
| N | 114 | 68 | 46 | |
| Age (SD) | 19.62 (3.49) | 19.75 (2.89) | 19.43 (4.29) | n.s. |
| Female (%) | 71 (62%) | 41 (60%) | 30 (65%) | n.s. |
| In full or part-time education (%) | 76 (67%) | 40 (59%) | 36 (78%) | 0.03 |
| Full- or part-time employed (%) | 46 (40%) | 26 (38%) | 20 (43%) | n.s. |
| SOFAS (SD) | 63.95 (13.49) | 60.90 (13.29) | 68.72 (12.51) | 0.002 |
| QIDS (SD) | 7.17 (4.38) | 8.75 (4.33) | 4.68 (3.16) | <0.001 |
SD, standard deviation; SOFAS, social and occupational functioning assessment scale; QIDS, quick inventory of depressive symptomatology.
t-test or chi-square.
Figure 1.
Venn Diagram showing the extent of overlap of the four at-risk groups at baseline for those that meet CHARMS criteria (N = 68) at baseline.
Figure 2.
Observed homotypic and heterotypic continuity from baseline to 12-months follow-up in those meeting CHARMS criteria. Young people can meet for multiple at risk groups.
Limitations and Future Directions
The CHARMS can be criticized for still relying on existing categories, criteria sets and diagnostic outcomes, even if in a “merged” form. However, in the absence of any valid alternatives, the CHARMS approach provides a workable solution, and is directly implementable in clinical practice. A future thought to entertain is the possibility that findings born out of HiTOP and RDoC frameworks might help to re-define the CHARMS criteria completely independent of DSM criteria sets and cut-offs.
Furthermore, the CHARMS pilot study has three assessment points only, which contrasts with the discussion earlier regarding the dynamic, fluctuating nature of emerging psychopathology, for which more frequent assessment points would be required in the future. However, studies are underway implementing more dynamic approaches in this cohort, including a combination of intensive longitudinal Ecological Momentary Assessment (EMA) for the duration of 4 months, paired with passive monitoring of sleep-wake cycles, and physical activity. These data-rich, fine-grained time series in this unique CHARMS-cohort will allow for the dynamic modeling of the onset of mental illness (see below).
Dynamic Systems Approach and Joint Modeling
One approach we are taking is to conceptualize mental health as a complex dynamic system (99): A system composed of many elements which interact with each other over time. Other examples of complex systems comprise financial markets, the ecosystem of a lake, or the climate. While these systems are very diverse, they share underlying common (mathematical) principles which are universal to complex systems and describe their behavior. For example, the resilience of a system can be inferred by studying its stability, i.e., how far is a system from a phase transition or “tipping point” (100–102). In our CHARMS identification framework or clinical staging, a tipping point might represent the transition from subthreshold to threshold psychopathology, i.e., from at-risk mental state to full disorder (103, 104). The proximity of such phase transitions can be studied by resilience indicators or “early warning signs” identified in time series (e.g., time series of symptoms obtained using EMA) (105, 106).
Of relevance in the “dynamic” context is also our group's advancement of joint modeling in the mental health field. Joint modeling is a statistical technique that examines the dynamic association between variables assessed repeatedly over time (“longitudinal data”) and time-dependent outcomes (e.g., death, transition to psychosis). It represents a joint approach of combining multilevel models with random effects and a survival model. Our group has investigated the performance of joint modeling and dynamic prediction in the context of transition to psychosis in UHR individuals (107–109). We have shown that, compared to with traditional prediction models that rely exclusively on baseline data, joint modeling offers a superior approach in predicting psychosis in UHR individuals (107–109). Therefore, the joint modeling approach will also be explored in the context of dynamic prediction in our CHARMS cohort.
A further limitation of the CHARMS framework at this stage is the focus on four specific outcomes/at risk groups. Based on the outcomes of our (pilot) CHARMS cohort study, we will investigate the expansion of the framework to encompass other syndromes as well, such as obsessive compulsive disorders and eating disorders. These syndromes are captured and may in the future be incorporated as input and outcomes of interest.
A final criticism that the CHARMS framework faces is its reliance on clinical interview data only at this stage. Incorporating other (neurocognitive, bio-physiological) modalities will be an important next step, as there is a clear demand to identify markers of illness which directly map onto pathophysiology (110). Clinical staging enables the identification and evaluation of pathophysiology and biomarkers at each stage of illness (110). If we investigate the association between (bio)marker and symptoms in relation to stages in the CHARMS approach, we might be able to identify and differentiate between transdiagnostic markers as well as syndrome-specific markers. Future expansions of the study will include the incorporation of a neurocognitive test battery, blood-based biomarkers, and digital phenotyping.
Conclusion
Emerging mental disorders develop in complex interacting trajectories over time with non-specific symptoms that overlap, intensify and recede, defying diagnostic borders. A new diagnostic approach and case identification framework is needed, with an emphasis on clinical utility. The clinical staging and the transdiagnostic CHARMS risk identification framework is guided by the principle that diagnostic terms or labels only need as much specificity to guide treatment selection (111). One key implication of the pluripotential CHARMS at-risk approach is that if identification and intervention can occur early, progression to later stages might be prevented. The instruments for such preventive treatment approaches, focusing on novel, broader target treatments such as psychosocial and neuroprotective approaches, will be trialed in this broad at-risk population.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Melbourne Health Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JH and BN developed the first draft. LD wrote sections of the manuscript. PM, GA, AC, CD, RG, AP, AR, and HY provided significant input to all sections of the manuscript. All authors approved the final manuscript.
Conflict of Interest
PM reported receiving grant funding from National Alliance for Research on Schizophrenia and Depression and unrestricted research funding from AstraZeneca, Eli Lilly, Janssen-Cilag, Pfizer, and Novartis, as well as honoraria for educational activities with AstraZeneca, Eli Lilly, Janssen-Cilag, Pfizer, Bristol-Myers Squibb, Roche, and the Lundbeck Institute. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1The UHR criteria are assessed using the Comprehensive Assessment of At-Risk Mental States (CAARMS, (19)). Young people at UHR are identified by one or more of the following characteristics: (1) Attenuated Psychotic Symptoms (APS)—young people who have experienced subthreshold, attenuated forms of positive psychotic symptoms during the past year, (2) Brief Limited Intermittent Psychotic Symptoms (BLIPS)—young people who have experienced episodes of frank psychotic symptoms that have not lasted longer than a week and have spontaneously abated, and (3) Trait and State Risk Factor (Trait)—individuals who have a first-degree relative with a psychotic disorder or who have a schizotypal personality disorder in addition to a significant decrease in functioning, or chronic low functioning, during the previous year.
Funding. This work is supported by a grant from the John T. Reid Charitable Trust and the Colonial Foundation. JH is supported by a University of Melbourne McKenzie Postdoctoral Fellowship.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 2.Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry Suppl. (2013) 54:s5–10. 10.1192/bjp.bp.112.119164 [DOI] [PubMed] [Google Scholar]
- 3.McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. (2008) 7:148–56. 10.1002/j.2051-5545.2008.tb00182.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGorry PD. Risk syndromes, clinical staging and DSM V: new diagnostic infrastructure for early intervention in psychiatry. Schizophr Res. (2010) 120:49–53. 10.1016/j.schres.2010.03.016 [DOI] [PubMed] [Google Scholar]
- 5.Mei C, Nelson B, Hartmann J, Spooner R, McGorry PD. Chapter 4 - Transdiagnostic early intervention, prevention, and prediction in psychiatry. In: Baune BT, editor. Personalized Psychiatry. San Diego: Academic Press, 27–37. [Google Scholar]
- 6.McGorry PD, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. (2006) 40:616–22. 10.1080/j.1440-1614.2006.01860.x [DOI] [PubMed] [Google Scholar]
- 7.McGorry P. Transition to adulthood: the critical period for pre-emptive, disease-modifying care for schizophrenia and related disorders. Schizophr Bull. (2011) 37:524–30. 10.1093/schbul/sbr027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kessler RC, Birnbaum H, Demler O, Falloon IR, Gagnon E, Guyer M, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Survey Replication (NCS-R). Biol Psychiatry. (2005) 58:668–76. 10.1016/j.biopsych.2005.04.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2011) 68:90–100. 10.1001/archgenpsychiatry.2010.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merikangas KR, Herrell R, Swendsen J, Rossler W, Ajdacic-Gross V, Angst J. Specificity of bipolar spectrum conditions in the comorbidity of mood and substance use disorders: results from the Zurich cohort study. Arch Gen Psychiatry. (2008) 65:47–52. 10.1001/archgenpsychiatry.2007.18 [DOI] [PubMed] [Google Scholar]
- 11.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. (2010) 49:980–9. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merikangas KR, Cui L, Kattan G, Carlson GA, Youngstrom EA, Angst J. Mania with and without depression in a community sample of US adolescents. Arch Gen Psychiatry. (2012) 69:943–51. 10.1001/archgenpsychiatry.2012.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray GK, Jones PB. Psychotic symptoms in young people without psychotic illness: mechanisms and meaning. Br J Psychiatry. (2012) 201:4–6. 10.1192/bjp.bp.111.107789 [DOI] [PubMed] [Google Scholar]
- 14.Ormel J, Raven D, van Oort F, Hartman CA, Reijneveld SA, Veenstra R, et al. Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol Med. (2015) 45:345–60. 10.1017/S0033291714001469 [DOI] [PubMed] [Google Scholar]
- 15.Cramer AO, Waldorp LJ, van der Maas HL, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. (2010) 33:137–50; discussion 150–93. 10.1017/S0140525X09991567 [DOI] [PubMed] [Google Scholar]
- 16.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 17.Borsboom D. A network theory of mental disorders. World Psychiatry. (2017) 16:5–13. 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. (1996) 22:353–70. 10.1093/schbul/22.2.353 [DOI] [PubMed] [Google Scholar]
- 19.Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. (2005) 39:964–71. 10.1080/j.1440-1614.2005.01714.x [DOI] [PubMed] [Google Scholar]
- 20.Malla AK, Norman RM. Prodromal symptoms in schizophrenia. Br J Psychiatry. (1994) 164:487–93. 10.1192/bjp.164.4.487 [DOI] [PubMed] [Google Scholar]
- 21.McGorry PD, Mei C. Ultra-high-risk paradigm: lessons learnt and new directions. Evid Based Ment Health. (2018) 21:131–3. 10.1136/ebmental-2018-300061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR. Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry. (2015) 172:249–58. 10.1176/appi.ajp.2014.13030418 [DOI] [PubMed] [Google Scholar]
- 23.Rutigliano G, Valmaggia L, Landi P, Frascarelli M, Cappucciati M, Sear V, et al. Persistence or recurrence of non-psychotic comorbid mental disorders associated with 6-year poor functional outcomes in patients at ultra high risk for psychosis. J Affect Disord. (2016) 203:101–10. 10.1016/j.jad.2016.05.053 [DOI] [PubMed] [Google Scholar]
- 24.Beck K, Andreou C, Studerus E, Heitz U, Ittig S, Leanza L, et al. Clinical and functional long-term outcome of patients at clinical high risk (CHR) for psychosis without transition to psychosis: a systematic review. Schizophr Res. (2019) 210:39–47. 10.1016/j.schres.2018.12.047 [DOI] [PubMed] [Google Scholar]
- 25.Ajnakina O, Morgan C, Gayer-Anderson C, Oduola S, Bourque F, Bramley S, et al. Only a small proportion of patients with first episode psychosis come via prodromal services: a retrospective survey of a large UK mental health programme. BMC Psychiatry. (2017) 17:308. 10.1186/s12888-017-1468-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. (2012) 69:220–9. 10.1001/archgenpsychiatry.2011.1472 [DOI] [PubMed] [Google Scholar]
- 27.Cuijpers P. Examining the effects of prevention programs on the incidence of new cases of mental disorders: the lack of statistical power. Am J Psychiatry. (2003) 160:1385–91. 10.1176/appi.ajp.160.8.1385 [DOI] [PubMed] [Google Scholar]
- 28.Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry. (2009) 50:1485–94. 10.1111/j.1469-7610.2009.02117.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krueger RF, Piasecki TM. Toward a dimensional and psychometrically-informed approach to conceptualizing psychopathology. Behav Res Ther. (2002) 40:485–99. 10.1016/S0005-7967(02)00016-5 [DOI] [PubMed] [Google Scholar]
- 30.Krueger RF, Markon KE. A dimensional-spectrum model of psychopathology: progress and opportunities. Arch Gen Psychiatry. (2011) 68:10–1. 10.1001/archgenpsychiatry.2010.188 [DOI] [PubMed] [Google Scholar]
- 31.Johns LC, van Os J. The continuity of psychotic experiences in the general population. Clin Psychol Rev. (2001) 21:1125–41. 10.1016/S0272-7358(01)00103-9 [DOI] [PubMed] [Google Scholar]
- 32.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. (2009) 39:179–95. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- 33.Fleming S, Shevlin M, Murphy J, Joseph S. Psychosis within dimensional and categorical models of mental illness. Psychosis. (2013) 6:4–15. 10.1080/17522439.2012.752027 [DOI] [Google Scholar]
- 34.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. (2013) 43:1133–49. 10.1017/S0033291712001626 [DOI] [PubMed] [Google Scholar]
- 35.Pickles A, Angold A. Natural categories or fundamental dimensions: on carving nature at the joints and the rearticulation of psychopathology. Dev Psychopathol. (2003) 15:529–51. 10.1017/S0954579403000282 [DOI] [PubMed] [Google Scholar]
- 36.Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the Diagnostic And Statistical Manual Of Mental Disorders–fifth edition J Abnorm Psychol. (2005) 114:494–504. 10.1037/0021-843X.114.4.494 [DOI] [PubMed] [Google Scholar]
- 37.McGorry PD. Issues for DSM-V: clinical staging: a heuristic pathway to valid nosology and safer, more effective treatment in psychiatry. Am J Psychiatry. (2007) 164:859–60. 10.1176/ajp.2007.164.6.859 [DOI] [PubMed] [Google Scholar]
- 38.Scott J, Leboyer M, Hickie I, Berk M, Kapczinski F, Frank E, et al. Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry. (2013) 202:243–5. 10.1192/bjp.bp.112.110858 [DOI] [PubMed] [Google Scholar]
- 39.Hickie IB, Scott EM, Hermens DF, Naismith SL, Guastella AJ, Kaur M, et al. Applying clinical staging to young people who present for mental health care. Early Interv Psychiatry. (2013) 7:31–43. 10.1111/j.1751-7893.2012.00366.x [DOI] [PubMed] [Google Scholar]
- 40.Cross SP, Hermens DF, Scott EM, Ottavio A, McGorry PD, Hickie IB. A clinical staging model for early intervention youth mental health services. Psychiatr Serv. (2014) 65:939–43. 10.1176/appi.ps.201300221 [DOI] [PubMed] [Google Scholar]
- 41.Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry. (2017) 16:251–65. 10.1002/wps.20446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iorfino F, Scott EM, Carpenter JS, Cross SP, Hermens DF, Killedar M, et al. Clinical stage transitions in persons aged 12 to 25 years presenting to early intervention mental health services with anxiety, mood, and psychotic disorders. JAMA Psychiatry. (2019) 76:1167–75. 10.1001/jamapsychiatry.2019.2360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cross SPM, Scott J, Hickie IB. Predicting early transition from sub-syndromal presentations to major mental disorders. BJPsych Open. (2017) 3:223–7. 10.1192/bjpo.bp.117.004721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McGorry P, Nelson B. Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry. (2016) 73:191–2. 10.1001/jamapsychiatry.2015.2868 [DOI] [PubMed] [Google Scholar]
- 45.McGorry PD, Hartmann JA, Spooner R, Nelson B. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry. (2018) 17:133–42. 10.1002/wps.20514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hartmann JA, Nelson B, Spooner R, Paul Amminger G, Chanen A, Davey CG, et al. Broad clinical high-risk mental state (CHARMS): Methodology of a cohort study validating criteria for pluripotent risk. Early Interv Psychiatry. (2019) 13:379–86. 10.1111/eip.12483 [DOI] [PubMed] [Google Scholar]
- 47.Spooner R, Hartmann JA, McGorry PD, Nelson B. Chapter 21 - New paradigms to study psychosis risk: clinical staging, pluripotency, and dynamic prediction. In: Thompson AD, Broome MR, editors. Risk Factors for Psychosis. Academic Press, 399–416. [Google Scholar]
- 48.Chanen AM, Berk M, Thompson KJH. Integrating early intervention for borderline personality disorder and mood disorders. Harv Rev Psychiatry. (2016) 24:330–41. 10.1097/HRP.0000000000000105 [DOI] [PubMed] [Google Scholar]
- 49.Mazer AK, Cleare AJ, Young AH, Juruena MF. Bipolar affective disorder and borderline personality disorder: differentiation based on the history of early life stress and psychoneuroendocrine measures. Behav Brain Res. (2019) 357:48–56. 10.1016/j.bbr.2018.04.015 [DOI] [PubMed] [Google Scholar]
- 50.Cavelti M, Thompson K, Chanen A, Kaess M. Psychotic symptoms in borderline personality disorder: developmental aspects. Curr Opin Psychol. (2020) 37:26–31. 10.1016/j.copsyc.2020.07.003 [DOI] [PubMed] [Google Scholar]
- 51.Johannessen JO, McGorry P. DSM-5 and the ‘Psychosis Risk Syndrome’: the need for a broader perspective. Psychosis. (2010) 2:93–6. 10.1080/17522431003759974 [DOI] [Google Scholar]
- 52.Fusar-Poli P, Carpenter WT, Woods SW, McGlashan TH. Attenuated psychosis syndrome: ready for DSM-5.1? Annu Rev Clin Psychol. (2014) 10:155–92. 10.1146/annurev-clinpsy-032813-153645 [DOI] [PubMed] [Google Scholar]
- 53.Fusar-Poli P. The hype cycle of the clinical high risk state for psychosis: the need of a refined approach. Schizophr Bull. (2018) 44:250–3. 10.1093/schbul/sbx181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee TY, Lee J, Kim M, Choe E, Kwon JS. Can we predict psychosis outside the clinical high-risk state? A systematic review of non-psychotic risk syndromes for mental disorders. Schizophr Bull. (2018) 44:276–85. 10.1093/schbul/sbx173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Woods SW, Powers AR, 3rd, Taylor JH, Davidson CA, Johannesen JK, Addington J, et al. Lack of diagnostic pluripotentiality in patients at clinical high risk for psychosis: specificity of comorbidity persistence and search for pluripotential subgroups. Schizophr Bull. (2018) 44:254–63. 10.1093/schbul/sbx138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Amos AJ. A review of spin and bias use in the early intervention in psychosis literature. Prim Care Companion CNS Disord. (2014) 16:P 10.4088/PCC.13r01586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goodday SM, Duffy A. Shedding light on the onset of psychiatric illness: looking through a developmental lens. Evid Based Ment Health. (2019) 22:134–6. 10.1136/ebmental-2018-300076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McGorry P, van Os J. Redeeming diagnosis in psychiatry: timing versus specificity. Lancet. (2013) 381:343–5. 10.1016/S0140-6736(12)61268-9 [DOI] [PubMed] [Google Scholar]
- 59.Patalay P, Fonagy P, Deighton J, Belsky J, Vostanis P, Wolpert M. A general psychopathology factor in early adolescence. Br J Psychiatry. (2015) 207:15–22. 10.1192/bjp.bp.114.149591 [DOI] [PubMed] [Google Scholar]
- 60.Murray AL, Eisner M, Ribeaud D. The development of the general factor of psychopathology 'p factor' through childhood and adolescence. J Abnorm Child Psychol. (2016) 44:1573–86. 10.1007/s10802-016-0132-1 [DOI] [PubMed] [Google Scholar]
- 61.McElroy E, Belsky J, Carragher N, Fearon P, Patalay P. Developmental stability of general and specific factors of psychopathology from early childhood to adolescence: dynamic mutualism or p-differentiation? J Child Psychol Psychiatry. (2018) 59:667–75. 10.1111/jcpp.12849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wigman JT, van Os J, Thiery E, Derom C, Collip D, Jacobs N, et al. Psychiatric diagnosis revisited: towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS One. (2013) 8:e59559. 10.1371/journal.pone.0059559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One. (2015) 10:e0137621. 10.1371/journal.pone.0137621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pe ML, Kircanski K, Thompson RJ, Bringmann LF, Tuerlinckx F, Mestdagh M, et al. Emotion-network density in major depressive disorder. Clin Psychol Sci. (2015) 3:292–300. 10.1177/2167702614540645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boschloo L, Schoevers RA, van Borkulo CD, Borsboom D, Oldehinkel AJ. The network structure of psychopathology in a community sample of preadolescents. J Abnorm Psychol. (2016) 125:599–606. 10.1037/abn0000150 [DOI] [PubMed] [Google Scholar]
- 66.Groen RN, Wichers M, Wigman JTW, Hartman CA. Specificity of psychopathology across levels of severity: a transdiagnostic network analysis. Sci Rep. (2019) 9:18298. 10.1038/s41598-019-54801-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. (2003) 60:709–17. 10.1001/archpsyc.60.7.709 [DOI] [PubMed] [Google Scholar]
- 68.Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet. (2014) 383:1404–11. 10.1016/S0140-6736(13)62116-9 [DOI] [PubMed] [Google Scholar]
- 69.Hartmann JA, Nelson B, Ratheesh A, Treen D, McGorry PD. At-risk studies and clinical antecedents of psychosis, bipolar disorder and depression: a scoping review in the context of clinical staging. Psychol Med. (2019) 49:177–89. 10.1017/S0033291718001435 [DOI] [PubMed] [Google Scholar]
- 70.Tsuang MT, Bar JL, Stone WS, Faraone SV. Gene-environment interactions in mental disorders. World Psychiatry. (2004) 3:73–83. [PMC free article] [PubMed] [Google Scholar]
- 71.Lichtenstein P, Yip BH, Bjork C, Pawitan Y, Cannon TD, Sullivan PF, et al. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet. (2009) 373:234–9. 10.1016/S0140-6736(09)60072-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Agius M, Goh C, Ulhaq S, McGorry P. The staging model in schizophrenia, and its clinical implications. Psychiatr Danub. (2010) 22:211–20. [PubMed] [Google Scholar]
- 73.Anttila V., Bulik-Sullivan B., Finucane H. K., Walters R. K., Bras J., Duncan L., et al. (2018). Analysis of shared heritability in common disorders of the brain. Science 360:eaap8757. 10.1126/science.aap8757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mansell W. Transdiagnostic psychiatry goes above and beyond classification. World Psychiatry. (2019) 18:360–1. 10.1002/wps.20680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Duffy A, Malhi GS. Mapping the developmental trajectory of bipolar disorder: Importance of prerequisite groundwork. Aust N Z J Psychiatry. (2017) 51:761–3. 10.1177/0004867417720035 [DOI] [PubMed] [Google Scholar]
- 76.Scott J, Henry C. Clinical staging models: from general medicine to mental disorders. BJPsych Adv. (2017) 23:292–9. 10.1192/apt.bp.116.016436 [DOI] [Google Scholar]
- 77.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. (2010) 167:748–51. 10.1176/appi.ajp.2010.09091379 [DOI] [PubMed] [Google Scholar]
- 78.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. (2013) 11:126. 10.1186/1741-7015-11-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kozak MJ, Cuthbert BN. The NIMH research domain criteria initiative: background, issues, and pragmatics. Psychophysiology. (2016) 53:286–97. 10.1111/psyp.12518 [DOI] [PubMed] [Google Scholar]
- 80.Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. (2017) 126:454–77. 10.31234/osf.io/zaadn [DOI] [PubMed] [Google Scholar]
- 81.Kotov R, Krueger RF, Watson D. A paradigm shift in psychiatric classification: the Hierarchical Taxonomy Of Psychopathology (HiTOP). World Psychiatry. (2018) 17:24–5. 10.1002/wps.20478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kotov R, Jonas KG, Carpenter WT, Dretsch MN, Eaton NR, Forbes MK, et al. Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): I. Psychosis superspectrum. World Psychiatry. (2020) 19:151–72. 10.1002/wps.20730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.van Os J, Linscott RJ. Introduction: the extended psychosis phenotype–relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr Bull. (2012) 38:227–30. 10.1093/schbul/sbr188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Widiger TA, Sellbom M, Chmielewski M, Clark LA, DeYoung CG, Kotov R, et al. Personality in a Hierarchical model of psychopathology. Clin Psychol Sci. (2019) 7:77–92. 10.1177/2167702618797105 [DOI] [Google Scholar]
- 85.Krueger RF, Watson D, Widiger TA. The vibrant intersection of personality and psychopathology research: a special issue of the Journal of Research in Personality. J. Res Pers. (2020) 84:103890 10.1016/j.jrp.2019.103890 [DOI] [Google Scholar]
- 86.Sharp C, Wright AG, Fowler JC, Frueh BC, Allen JG, Oldham J, et al. The structure of personality pathology: Both general ('g') and specific ('s') factors? J Abnorm Psychol. (2015) 124:387–98. 10.1037/abn0000033 [DOI] [PubMed] [Google Scholar]
- 87.Thompson KN, Jackson H, Cavelti M, Betts J, McCutcheon L, Jovev M, et al. The clinical significance of subthreshold borderline personality disorder features in outpatient youth. J Pers Disord. (2019) 33:71–81. 10.1521/pedi_2018_32_330 [DOI] [PubMed] [Google Scholar]
- 88.Duffy A, Goodday S, Passos IC, Kapczinski F. Changing the bipolar illness trajectory. Lancet Psychiatry. (2017) 4:11–3. 10.1016/S2215-0366(16)30352-2 [DOI] [PubMed] [Google Scholar]
- 89.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. (1999) 40:57–87. 10.1111/1469-7610.00424 [DOI] [PubMed] [Google Scholar]
- 90.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry. (2005) 46:1200–10. 10.1111/j.1469-7610.2005.00422.x [DOI] [PubMed] [Google Scholar]
- 91.Kessler RC, Avenevoli S, McLaughlin KA, Green JG, Lakoma MD, Petukhova M, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Psychol Med. (2012) 42:1997–2010. 10.1017/S0033291712000025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shevlin M, McElroy E, Murphy J. Homotypic and heterotypic psychopathological continuity: a child cohort study. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1135–45. 10.1007/s00127-017-1396-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lahey BB, Zald DH, Hakes JK, Krueger RF, Rathouz PJ. Patterns of heterotypic continuity associated with the cross-sectional correlational structure of prevalent mental disorders in adults. JAMA Psychiatry. (2014) 71:989–96. 10.1001/jamapsychiatry.2014.359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Plana-Ripoll O, Pedersen CB, Holtz Y, Benros ME, Dalsgaard S, de Jonge P, et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiatry. (2019) 76:259–70. 10.1001/jamapsychiatry.2018.3658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Caspi A, Houts RM, Ambler A, Danese A, Elliott ML, Hariri A, et al. Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the Dunedin birth cohort Study. JAMA Netw Open. (2020) 3:e203221 10.1001/jamanetworkopen.2020.3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Krueger RF, Eaton NR. Transdiagnostic factors of mental disorders. World Psychiatry. (2015) 14:27–9. 10.1002/wps.20175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.van Os J, Guloksuz S. A critique of the “ultra-high risk” and “transition” paradigm. World Psychiatry. (2017) 16:200–6. 10.1002/wps.20423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Guloksuz S, van Os J. Need for evidence-based early intervention programmes: a public health perspective. Evid Based Ment Health. (2018) 21:128–30. 10.1136/ebmental-2018-300030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nelson B, McGorry PD, Wichers M, Wigman JTW, Hartmann JA. Moving from static to dynamic models of the onset of mental disorder: a review. JAMA Psychiatry. (2017) 74:528–34. 10.1001/jamapsychiatry.2017.0001 [DOI] [PubMed] [Google Scholar]
- 100.Scheffer M. Critical Transitions in Nature and Society. Princeton: Princeton University Press; (2009). [Google Scholar]
- 101.Scheffer M, Bascompte J, Brock WA, Brovkin V, Carpenter SR, Dakos V, et al. Early-warning signals for critical transitions. Nature. (2009) 461:53–9. 10.1038/nature08227 [DOI] [PubMed] [Google Scholar]
- 102.Scheffer M, Carpenter SR, Lenton TM, Bascompte J, Brock W, Dakos V, et al. Anticipating critical transitions. Science. (2012) 338:344–8. 10.1126/science.1225244 [DOI] [PubMed] [Google Scholar]
- 103.Hartmann J, Wichers M, McGorry P, Nelson B. Tipping points:-predicting transitions to mental illness and remission in at-risk young people. Early Interv Psychiatry. (2018) 12:12–12. [Google Scholar]
- 104.Hartmann JA, McGorry PD, Wichers M, Nelson B. T30. Tipping POINTS-PREDICTING TRANSITIONS TO PSYCHOSIS IN AT-RISK YOUNG PEOPLE Schizophr Bull. (2018) 44:S124–S5. 10.1093/schbul/sby016.306 [DOI] [Google Scholar]
- 105.van de Leemput IA, Wichers M, Cramer AO, Borsboom D, Tuerlinckx F, Kuppens P, et al. Critical slowing down as early warning for the onset and termination of depression. Proc Natl Acad Sci U S A. (2014) 111:87–92. 10.1073/pnas.1312114110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wichers M, Groot PC, Psychosystems ESMGEWSG. Critical slowing down as a personalized early warning signal for depression. Psychother Psychosom. (2016) 85:114–6. 10.1159/000441458 [DOI] [PubMed] [Google Scholar]
- 107.Yuen HP, Mackinnon A, Hartmann J, Amminger GP, Markulev C, Lavoie S, et al. Dynamic prediction of transition to psychosis using joint modelling. Schizophr Res. (2018) 202:333–40. 10.1016/j.schres.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 108.Yuen HP, Mackinnon A, Nelson B. A new method for analysing transition to psychosis: Joint modelling of time-to-event outcome with time-dependent predictors. Int J Methods Psychiatr Res (2018) 27:e1588. 10.1002/mpr.1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yuen HP, Mackinnon A, Nelson B. Dynamic prediction systems of transition to psychosis using joint modelling: extensions to the base system. Schizophr Res. (2020) 216:207–12. 10.1016/j.schres.2019.11.059 [DOI] [PubMed] [Google Scholar]
- 110.McGorry P, Keshavan M, Goldstone S, Amminger P, Allott K, Berk M, et al. Biomarkers and clinical staging in psychiatry. World Psychiatry. (2014) 13:211–23. 10.1002/wps.20144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.McGorry PD. Diagnosis without borders: a pluripotential approach to preventive intervention in emerging mental disorders. In Clinical Staging in Psychiatry: Making Diagnosis Work for Research and Treatment. McGorry PD, Hickie IB, editors. Cambridge: Cambridge University Press; (2019), p. 1–11. 10.1017/9781139839518.001 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.