Abstract
Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH) is a major cause of liver fibrosis and cirrhosis. Accurate assessment of liver fibrosis is important for predicting disease outcomes and assessing therapeutic response in clinical practice and clinical trials. Although noninvasive tests such as transient elastography and magnetic resonance elastography are preferred where possible, histological assessment of liver fibrosis via semiquantitative scoring systems remains the current gold standard. Collagen proportionate area provides more granularity by measuring the percentage of fibrosis on a continuous scale, but is limited by the absence of architectural input. Although not yet used in routine clinical practice, advances in second harmonic generation/two-photon excitation fluorescence (SHG/TPEF) microscopy imaging show great promise in characterising architectural features of fibrosis at the individual collagen fiber level. Quantification and calculation of different detailed variables of collagen fibers can be used to establish algorithm-based quantitative fibrosis scores (e.g., qFibrosis, q-FPs), which have been validated against fibrosis stage in NAFLD. Artificial intelligence is being explored to further refine and develop quantitative fibrosis scoring methods. SHG-microscopy shows promise as the new gold standard for the quantitative measurement of liver fibrosis. This has reaffirmed the pivotal role of the liver biopsy in fibrosis assessment in NAFLD, at least for the near-future. The ability of SHG-derived algorithms to intuitively detect subtle nuances in liver fibrosis changes over a continuous scale should be employed to redress the efficacy endpoint for fibrosis in NASH clinical trials; this approach may improve the outcomes of the trials evaluating therapeutic response to antifibrotic drugs.
Keywords: Nonalcoholic fatty liver disease, Fibrosis, Biopsy
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is a burgeoning global health concern in tandem with metabolic syndrome [1]. NAFLD encompasses steatosis to nonalcoholic steatohepatitis (NASH); the latter may progress to cirrhosis. In the United States, NAFLD is one of the leading indications for liver transplantation [2]. Prevalence of NAFLD in Asia has increased from 25% (1999–2005) to 34% (2012–2017) [3]. The histological diagnosis of NASH is based on four key parameters, viz., steatosis, hepatocellular ballooning, lobular inflammation, and fibrosis. Precise grading of severity and fibrosis staging are crucial for understanding the pathogenesis and development of therapeutic targets to halt, reverse as well as prevent disease.
Accurate quantitative assessment of liver fibrosis in NAFLD is important to predict risk of developing complications and track disease progression, especially as an efficacy endpoint in clinical trials of antifibrotic agents. Fibrosis stage is the most important histological predictor of liver-specific outcome; the risk of cirrhotic decompensation and hepatocellular carcinoma increases with fibrosis stage [4-7].
Noninvasive methods of fibrosis assessment are recommended by international management guidelines for NAFLD [8-12], given that only a minority of patients would eventually develop liver-related complications, and progression to cirrhosis takes decades [13-16]. However, it is increasingly recognised that the liver biopsy, despite its limitations, not only remains the ‘gold standard’ but provides a window into the architectural pattern and nature of fibrosis far beyond the scope of current routine histopathology practice, particularly with recent advances in techniques such as second harmonic generation (SHG)-microscopy and advanced computing systems. Bedossa has reiterated the importance of liver biopsy in the diagnosis and management of NAFLD/NASH in (selected) patients and clinical trials [17]. Wanless in a recent editorial also stated categorically that “quantitative biopsy assessment using SHG-microscopy should be considered the new gold standard for the measurement of liver fibrosis” [18].
There are many unmet needs concerning various aspects of NASH [19]. The current U.S. Food and Drug Administration requirements regarding efficacy endpoints to demonstrate therapeutic response in NASH clinical trials may have to be re-addressed in favour of more precise and granular criteria on a continuous scale with the aid of advancing laser microscopy and machine learning. This review aims to focus on current and developing techniques that assess fibrosis on liver tissue samples.
PATHOGENESIS OF LIVER FIBROSIS IN NAFLD
Hepatocellular injury and inflammation are supposedly the primary drivers of fibrogenesis in NASH patients, finally culminating in cirrhosis. The PIVENS and FLINT clinical trials have demonstrated the strong link between histological resolution of steatohepatitis (NAFLD activity score ≥2) with at least 1-stage decrease or more in fibrosis in NASH [20]. Liver fibrosis is a dynamic wound healing response to chronic liver injury characterized by accumulation of extracellular matrix (ECM) components, including collagen fibers, sulfated proteoglycans and glycoproteins, in excess of matrix degradation by enzymes. Activation of hepatic stellate cells (HSC) during liver injury and inflammation from their quiescent state to proliferative, fibrogenic and contractile myofibroblasts, in conjunction with endothelial cells, Kupffer cell infiltration and activation, and secretion of other inflammatory molecules, is the key event in fibrogenesis [21,22].
The adult NAFLD pattern of fibrosis starts as delicate perisinusoidal deposition of collagen fibers in the space of Disse in the centrilobular zone (zone 3) of the hepatic lobule [23]. Periportal fibrosis then develops with short collagen strands extending into zone 1, and thereafter, bridging with central veins via fibrous septa. Cirrhosis eventually ensues in a small percentage of cases. In comparison, the fibrosis is zone 1-centric in (pre-adolescent) children, beginning around portal regions and progressing to bridging fibrosis.
NONINVASIVE TESTS FOR FIBROSIS ASSESSMENT
Imaging modalities often use liver stiffness as a surrogate measure to assess the amount of liver fibrosis [24]. Vibration-controlled transient elastography (TE) (FibroScan®) is one of the most commonly used techniques [25]. Magnetic resonance elastography (MRE) has been shown to be superior to TE in that it can diagnose earlier stages of fibrosis, evaluate a larger portion of the liver, and provide for fat quantification via MR spectroscopy [26-28]. Other newer techniques include multiparametric magnetic resonance imaging [29,30]. Composite scoring systems based on serum biomarkers, such as fibrosis-4 (FIB-4) index, NAFLD fibrosis score (NFS), and enhanced liver fibrosis (ELF) test, have also been developed as surrogate measures of fibrosis severity in NAFLD [31-36]. Recently, there has been interest in gut microbiome to identify signatures for advanced fibrosis in NAFLD [37,38], as well as proteomic or multiomic studies [39,40]. However, these methods are all indirect measures of fibrosis encumbered by confounders and lack of specificity.
Some of the most pressing issues with noninvasive tests are difficulty in determining the optimum cut-off to differentiate intermediate stages of fibrosis; inability to reflect architectural changes/fibrosis stage that may not correspond with amount of collagen deposition; and the incapability to assess the dynamic nature of fibrosis progression or regression. These data are essential in tracking disease progression, prognostication, identifying patients who are most likely to benefit from any therapeutic intervention, and assessing the efficacy of antifibrotic drugs [13,41,42]. Recent advances in molecular and targeted MR imaging studies of small molecules that bind to fibrillary collagen or other ECM proteins are promising noninvasive approaches in the direct detection and quantification of liver fibrosis that would help overcome some of these limitations [43-45].
HISTOLOGICAL SCORING SYSTEMS BASED ON LIGHT MICROSCOPY
The performance of noninvasive tests is still currently measured against the ‘gold standard’ – histological assessment of liver tissue. The existing histological scoring systems for assessing fibrosis in NAFLD are semiquantitative categorical systems that have been developed to standardize and improve observer variability, especially in clinical trials (Table 1). Masson Trichrome or other connective tissue stains are performed to highlight fibrosis, particularly the delicate perisinusoidal component.
Table 1.
Comparison of histological fibrosis scoring systems
| Fibrosis stage | Brunt system [53] | NASH CRN score [48] | SAF score [57] |
|---|---|---|---|
| 0 | None | None | None |
| 1 | Zone 3 perisinusoidal fibrosis; focally or extensively present | 1a: Mild (delicate) zone 3 perisinusoidal fibrosis | |
| 1b: Moderate (dense) zone 3 perisinusoidal fibrosis | |||
| 1c: Portal fibrosis only | |||
| 2 | Zone 3 perisinusoidal fibrosis with focal or extensive periportal fibrosis | Zone 3 perisinusoidal fibrosis with periportal fibrosis | |
| 3 | Zone 3 perisinusoidal fibrosis and portal fibrosis with focal or extensive bridging fibrosis | Bridging fibrosis | |
| 4 | Cirrhosis | Cirrhosis | |
NASH CRN, Nonalcoholic Steatohepatitis Clinical Research Network; SAF, steatosis activity fibrosis.
Strictly speaking, as categorical labels, histological scoring systems do not quantify the absolute amount of fibrosis across the entire liver, but are rather a reflection of the architectural patterns in the scarred liver. Their accuracy therefore relies not only on a pathologist’s judgment but also on sample adequacy. Besides the sampling variability inherent in a biopsy procedure and disease heterogeneity [46,47], suboptimal samples exacerbate the problem of inter- and intra-observer variability [48]. Both the length and diameter of the cores must be sufficient for adequate assessment of portal tracts and central veins. A core length of 25 mm obtained via a 16-gauge needle is most ideal [49-52].
Brunt system
The Brunt system was the first histological assessment system proposed to categorize the morphologic features of NASH for grading and staging the disease [53]. It was intended to be used only after overall evaluation of the biopsy had established a diagnosis of NASH. Perisinusoidal/pericellular fibrosis was recognised as the earliest stage of fibrosis, with subsequent progression to periportal fibrosis, bridging fibrosis, and cirrhosis.
Nonalcoholic Steatohepatitis Clinical Research
Network (NASH CRN): NAFLD activity score (NAS) The Brunt system was further refined to include the full spectrum of NAFLD and be applicable to adults and children [48]. This new scoring system, developed and validated by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) sponsored NASH CRN Pathology Committee, is currently the most recognised system for scoring NAFLD in clinical trials and experimental studies [23,54]. The score is similarly not meant to supplant the pathologist’s diagnosis of NASH [55]. The NAS is a summative score of three components: steatosis, ballooning and lobular inflammation. Fibrosis is described separately using a 5-stage system (0 to 4), with further subclassification of stage 1 into substages a–c depending on the location of collagen deposition.
The Fatty Liver: Inhibition of Progression (FLIP) consortium: steatosis activity fibrosis (SAF) score
The SAF scoring system, developed by the FLIP European consortium, removes steatosis from the activity score of NAS. It proposes an algorithm to distinguish patients with or without NASH, based on the activity alone (ballooning and lobular inflammation); the three individually scored components of steatosis, activity and fibrosis then comprise the SAF score [56,57]. The fibrosis component is staged similarly as in the NASH CRN system; the inclusion of fibrosis in the SAF score presents a snapshot of the patient’s disease status. This scoring system was recently clinically validated in patients enrolled in a therapeutic trial [58].
Limitations of histological assessment scoring systems
Fibrosis deposition is actually a continuum that may not fall neatly into the designated categories of these semiquantitative staging systems. Distinguishing between the intermediate stages of fibrosis is challenging on liver biopsies [59]. The single numeric value of the staging system does not convey the variability and extent of changes seen within each stage, nor the architectural/vascular alterations present [60]. Moreover, the degree of perisinusoidal fibrosis is not captured in the higher stages of fibrosis. The severity of perisinusoidal fibrosis may contribute to portal hypertension in the absence of advanced fibrosis. Measurement of perisinusoidal fibrosis at all stages might enhance the evaluation of fibrosis outcome in clinical trial endpoints [61].
Fibrosis is a dynamic process with both progression and regression occurring concurrently, together with parenchymal remodeling, even at the ‘final’ cirrhotic stage [62]. In this respect, Sun et al. [63] proposed the Beijing classification based on chronic hepatitis B (CHB) patients to reflect the quality of fibrosis in advanced stage disease, in order to predict patient outcomes. However, this system has yet to be validated in NAFLD; furthermore, it is only applicable for later stage disease after parenchymal extinction and its sequelae have occurred [64].
Fibrosis is also a relatively slow process; current scoring systems may not provide sufficient granularity for assessing subtle changes during follow-up studies [65]. Furthermore, in current practice, the amount of fibrosis assessed based on the few 3 to 4-microns thick sections of the biopsy core examined is assumed to be representative of the entire core, and by extension, the rest of the patient’s liver; truly a ‘sample’ of a ‘sample’. Lastly, traditional light microscopy simply displays the presence of collagen fibers via connective tissue stains; it does not unveil collagen fiber structure nor the status of other cellular players in this fibrogenesis process.
MORPHOMETRIC ANALYSIS
Collagen proportionate area (CPA) measurement is the most validated morphometric approach that quantifies the amount of fibrous tissue present as a proportion of the total biopsy area, after subtracting for structural collagen (e.g., in large vessel walls). This automated process employs digital image analysis on histological sections, most commonly stained with Picro-Sirius red to highlight collagen [66]. CPA has been validated against hepatic venous pressure gradient measurements and clinical outcomes, mainly in patients with chronic hepatitis C (CHC) [67,68]. More recently, Buzzetti et al. [69] demonstrated CPA as an independent predictor of long-term outcome in NAFLD, including early stage disease.
CPA provides a linear quantification of fibrosis that has the sensitivity to detect small variations in the amount of collagen and fibrosis, which is especially useful in clinical trials that are often of relatively short duration. Furthermore, some clinical trials currently use a reduction of fibrosis histological stage by 1 or more as an outcome; however, a reduction in stage from 4 to 3 may have different implications regarding the efficacy of an antifibrotic drug as compared to a reduction from stage 2 to 1, given that CPA increases exponentially by fibrosis stage [70]. As a caveat though, sample adequacy becomes important when dealing with such precise measurements; moreover, adequate sample size differs between etiologies of cirrhosis [71]. CPA measurement is also still subject to technical issues such as variances in staining procedure, operator experience, and imaging software used.
CPA is unable to evaluate architectural changes such as bridging fibrosis and nodularity. Masugi et al. [72] demonstrated a strong but nonlinear relationship between Brunt fibrosis stage and the combined area ratio of collagen and elastin fibers, measured on Elastica van Gieson-stained biopsies from NAFLD patients. There was a marked difference between stages 4 and 3, but much smaller differences among stages 0–3. This was attributed to the relatively limited areas of bridging fibrosis in stage 3; thus, despite the altered architecture, the absolute amount of fibrosis may not differ significantly from earlier stages.
Hence, while CPA is a sensitive linear measurement that directly quantifies fibrosis, it does not provide any information on spatial alterations, the dynamic nature of fibrosis or the other cellular components involved in this process. It is still subject to the same potential sampling error that traditional histology suffers from.
MULTIPLE LASER-BASED MICROSCOPY
SHG/two-photon excitation fluorescence (TPEF) laser microscopy
Recent advancement in ultra-fast lasers have enabled imaging of optical signals, such as autofluorescence, from unstained, paraffin-embedded histological sections of biological samples. The ability to characterize the unique crystalline triple-helix structure and intrinsic optical signals of fibrillar collagen have opened up a whole new realm for quantitative assessment of liver fibrosis, reestablishing the importance of the liver biopsy. SHG microscopy is a nonlinear optical tissue imaging system that enables automated quantification of fibrosis based on the unique architectural features of collagen [73,74]. TPEF permits visualization of the background liver architecture through endogenous tissue signals [75]. SHG/TPEF microscopy therefore allows identification of individual collagen fibers, localization of collagen in 2D and 3D formats, and quantification of their physical attributes, such as number, length, diameter, orientation, contour, and cross-linkages of the collagen fibers with each other [73,74]. Characterization of the collagen fibers and relationship of aggregated thick and dispersed thin fibers within a 3D lattice framework provides insights into the remodeling dynamism and would be of great pathomechanistic and pharmaceutical value.
There has been a surge in studies utilising SHG to assess liver fibrosis in the past decade (Fig. 1, Table 2) [76-80]. One of the most pivotal developments was the establishment of “qFibrosis” by Xu et al. [80]- a fully-quantitative stain-free method for the automated assessment of liver fibrosis that incorporates spatial architectural features of pathological relevance at the tissue level. In order to achieve this concept of histological staging, the qFibrosis design utilised SHG/TPEF for 1) detection of changes in the respective collagen patterns and 2) quantitative identification of histopathological architectural features. Eighty-seven collagen architectural features were selected and categorized into three groups, namely, portal, septal, and fibrillar collagen, and these features are translated into quantitative parameters to build up the three respective subindices which were then combined into a single index, qFibrosis.
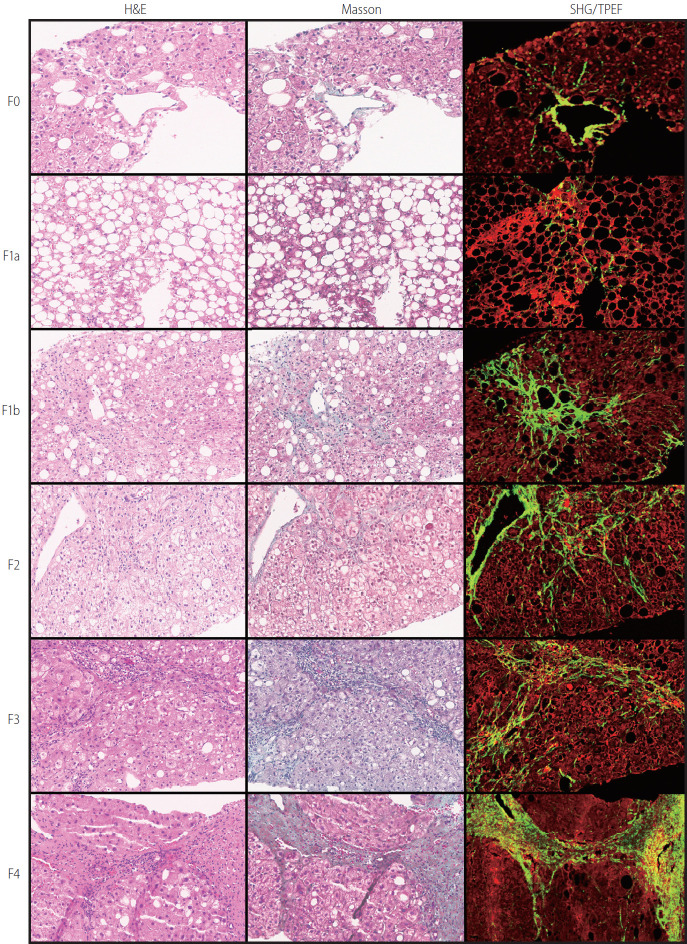
Figure 1.
Comparison of histopathological staining (H&E and Masson trichrome) with SHG/TPEF images of liver biopsy tissue from NAFLD patients. SHG imaging, Masson trichrome, and H&E were performed on serial sections (×200). H&E, haemotoxylin and eosin; SHG, second harmonic generation; TPEF, two-photon excitation fluorescence; NAFLD, nonalcoholic fatty liver disease.
Table 2.
Performance of SHG-based models for quantitative assessment of liver fibrosis in NAFLD
| Study | Model | Methodology | No. of patients | Performance |
|---|---|---|---|---|
| Wang et al. [79] (2017) | q-FP | SHG/TPEF to capture images (of whole biopsy section) | 50 (test cohort) | Principal component analysis model of 16 q-FPs: |
| Images assessed with computerized image-analysis by two independent investigators to output the profile of q-FPs data for each slice in operator-defined segmentation regions of liver tissue, including: | 42 (validation cohort) | - Fibrosis vs. no fibrosis: AUC 0.88 | ||
| (1) General: the liver section in its entirety | - Cirrhosis vs. earlier stages: AUC 0.93 | |||
| (2) Perisinusoidal: hepatocyte-associated collagen in the perisinusoidal space | Linear scale of fibrosis measurement of 4 q-FPs using desirability functions: | |||
| (3) Vessel: collagen fibrils directly connected to veins; and | - Related to fibrosis stage (P<0.0001) | |||
| (4) Vessel bridges: collagen fibrils extending from vein to vein or vein to portal tract. | ||||
| 70 q-FPs had interclass concordance ≥0.8 which were selected for further model development | ||||
| Wang et al. [81] (2020) | q-FP | Compared against NASH CRN staging system (but with substages of stage 1 combined) | 344 (428 biopsies) (larger validation study) | 25 q-FPs with AUC >0.90 for different fibrosis stages; perimeter of collagen fibres and number of long collagen fibres had the best accuracy (88.3–96.2% sensitivity and 78.1–91.1% specificity for different fibrosis stages) |
| Chang et al. [76] (2018) | SHG B-index | SHG/TPEF to capture images (final sampling size of 10 mm2 per biopsy) | 83 adults | Prediction model based on 14 unique SHG-based collagen parameters |
| An image processing algorithm was used to quantify fibrosis features in three specific regions: 1) central vein, 2) portal tract, and 3) perisinusoidal | - Fibrosis vs. no fibrosis: AUC 0.853 | |||
| In total, 100 collagen features were extracted and quantified, of which 28 features including the percentages of different collagen patterns and collagen string features were extracted in each region | - Cirrhosis vs. earlier stages: AUC 0.941 | |||
| - Stage 0/1 vs. 2/3/4: AUC 0.967 | ||||
| - Stage 0/1/2 vs. 3/4: AUC 0.985 | ||||
| Compared against Brunt’s staging system | - High correlation of 0.820 with fibrosis stage (P<0.001) | |||
| Liu et al. [77] (2017) | qFibrosis | SHG/TPEF to capture images (final sampling size of 10 mm2 per biopsy) | 62 adults (30 training, 32 validation); 36 children (18 training, 18 validation) | Prediction model based on six shared parameters for string collagen |
| An image processing algorithm was used to quantify fibrosis features in three specific regions: 1) central vein, 2) portal tract, and 3) perisinusoidal | (Adult) | |||
| - Fibrosis vs. no fibrosis: AUC 0.835 | ||||
| In total, 100 collagen features were extracted and quantified | - Cirrhosis vs. earlier stages: 0.982 | |||
| - Stage 0/1 vs. 2/3/4: AUC 0.892 | ||||
| - Stage 0/1/2 vs. 3/4: AUC 0.87 | ||||
| (Pediatric) | ||||
| - Fibrosis vs. no fibrosis: AUC 0.981 | ||||
| - Stage 0/1 vs. 2/3: AUC 0.931 | ||||
| - Stage 0/1/2 vs. 3: AUC 0.885 | ||||
| Liu et al. [82] (2020) | qFibrosis | Compared against NASH CRN staging system | 219 adults (146 training, 73 validation) (multicenter) | Prediction model based on 17 parameters, with output as a numerical index from 0 and 6.55 |
| - Fibrosis vs. no fibrosis: AUC 0.87 | ||||
| - Cirrhosis vs. earlier stages: 0.951 | ||||
| - Stage 0/1 vs. 2/3/4: AUC 0.881 | ||||
| - Stage 0/1/2 vs. 3/4: AUC 0.945 |
SHG, second harmonic generation; NAFLD, nonalcoholic fatty liver disease; q-FP, quantification of fibrosis-related parameter; TPEF, two-photon excitation fluorescence; AUC, area under curve; NASH CRN, Nonalcoholic Steatohepatitis Clinical Research Network.
qFibrosis, first validated on core biopsies from CHB patients, was shown to reliably stage liver fibrosis with reduced variability of sampling error and inter-/intra-observer bias, as well as differentiate intra-stage cirrhosis changes, an essential step for monitoring progression or regression of cirrhosis and response to antifibrotic drugs. The successful demonstration of qFibrosis as a reproducible and robust tool, outperforming CPA and (hepato)pathologists’ observer variability in CHB and CHC, laid the groundwork for SHG microscopy-based assessment of liver fibrosis in NAFLD.
Pirhonen et al. [78] subsequently performed a proof-of-concept study in NAFLD patients using SHG and coherent anti-Stokes Raman scattering (CARS) microscopy. They focused on patients with no or early stage fibrosis, as early detection of fibrosis is crucial for identifying individuals at risk for advanced liver disease. SHG and CARS imaging could detect fibrillar collagen and fat, respectively, in a label-free manner, allowing for automated and sensitive quantification of early fibrosis with continuous grading in NAFLD.
In 2017, Wang et al. [79] then proposed a validated SHG-based quantification of fibrosis-related parameters (q-FPs) model in NAFLD that offered a more refined assessment of collagen architectural changes along a continuous, quantitative scale. The authors showed that SHG could differentiate subtle differences between fibrosis stages 1a, 1b, and 1c (NASH CRN system) and differences in zonal distribution of fibrosis in patients with cirrhosis. In a 2020 validation study, Wang et al. [81] further showed that q-FP was highly accurate in assessing different stages of fibrosis in NAFLD patients and correlated strongly with histological scoring and liver stiffness measurement.
Similarly, Chang et al. [76] developed a fibrosis index (SHG B-index) comprising 14 unique SHG-based collagen parameters that correlated with severity of NAFLD fibrosis in a continuous fashion, validating the reliability of SHG as an automated method for fibrosis staging. In their cross-validation analysis, the SHG B-index demonstrated high specificity for diagnosis of all grades of fibrosis (Brunt fibrosis stage), although it was less discerning in discriminating between early stages of fibrosis. The advantage of the SHG B-index is that it provides a convenient single composite index that can be easily applied both in routine practice and clinical trials.
Well-defined, accurate, reproducible, and clinically meaningful endpoints are currently lacking to assess efficacy of NASH clinical trials. Besides fibrosis, histological assessment of NASH severity is used as endpoints in clinical trials, despite acknowledged issues with accuracy and reproducibility of these parameters amongst (hepato)pathologists. The qFIBS (Fibrosis, Inflammation, Ballooning, and Steatosis) model, an SHG-based automated quantitative tool developed and validated by Liu et al. [77,82] in a multicenter cohort, shows promise in mitigating these issues. This computational algorithm expands on the initial qFibrosis model developed in CHB patients; it quantifies the four key histopathological features of NASH, namely, fibrosis (qFibrosis), lobular inflammation (qInflammation), hepatocellular ballooning (qBallooning), and steatosis (qSteatosis). In their study, each qFIBS components were strongly correlated with the corresponding NASH CRN components (P<0.001). Validation of qFibrosis showed strong correlation with histological fibrosis stage (r=0.776) and accurate differentiation of fibrosis stages. Of note, however, is that similar to the NASH CRN scoring system, qFIBS is not suited for establishing a de novo diagnosis but is more of an adjunctive tool to quantify disease severity.
All these various models have affirmed SHG microscopy to be an invaluable new platform to study and quantify liver fibrosis, as well as the other key histological parameters of NASH. As current fibrosis staging systems tend to be disease-specific, the strong correlation between the models and traditional histological scoring systems used specifically in NAFLD promises great clinical utility, especially where demonstration of histological fibrosis improvement is an endpoint in drug trials for NAFLD. Similar to CPA measurements, SHG-based microscopy techniques allow for an objective quantitative assessment of fibrosis changes on a continuous scale, thereby providing greater reflection of subtle nuances compared to the stage migration of the traditional simpler semiquantitative scores. However, in addition, combination with techniques such as TPEF or CARS allows for assessment of spatial information of collagen fibres, which are lacking in CPA measurements. In fact, the potential of qFibrosis could be further developed beyond the traditional confines of grouping or staging fibrosis as a single component, and instead be scored separately as the three subindices of perisinusoidal, portal, and septal fibrosis. This more refined fibrosis categorization would potentially be more sensitive and meaningful in monitoring patients’ disease progression. Regardless, it must be remembered that SHG microscopy still requires liver tissue samples to be performed on, and thus is subject to the sampling variances and the risks of an invasive biopsy procedure. The requirement for specialised equipment may also limit its utility in resource-poor areas or countries.
ARTIFICIAL INTELLIGENCE (AI)-ASSISTED SYSTEMS
Current computer-assisted SHG/TPEF image analytics for liver fibrosis scoring is not fully automated as it entails manual pre-processing (segmentation and feature extraction) based on domain knowledge in liver pathology, potentially introducing bias. For example, qFIBS uses an algorithm-derived platform rather than a machine-learning platform, resulting in correlations but not exact correspondence between the pertinent variables [82]. Deep learning-based algorithms can potentially classify these images through learning from a large dataset of images. Yu et al. [83] have shown that deep learning-based algorithms with transfer learning can automatically quantify liver fibrosis progression and score different stages of fibrosis (based on the METAVIR scoring system) with high sensitivity and specificity in a rat model. The level of accuracy by this fully automated algorithm using pre-trained AlexNet-Convolutional Neural Networks is similar to conventional non-deep learning-based algorithms in scoring liver fibrosis stages. However, this approach has yet to be validated in NAFLD patients.
A significant barrier to the widespread adoption of many of the newer technologies is the large computational effort and specialised equipment required. Recognising this difficulty, Forlano et al. [70] developed a high-throughput, machine learning-based and fully automated method of quantification of steatosis, inflammation, ballooning, and collagen in liver biopsies from NAFLD patients that was user-friendly, fast-operating, and accurate. The devised software algorithm analysed biopsy images to compute percentages of each of the three key features of NASH, as well as calculated the CPA, with levels of inter- and intra-observer agreement ranging from 0.95 to 0.99, higher than that of semiquantitative scoring systems. It was also more sensitive in detecting differences in paired liver biopsies compared with the NASH CRN scoring system. The machine learning software is touted to be easily installable on any device and quantification performed within 2 minutes, features that would be attractive, especially in low resource and non-specialist centers.
Most recently, Gawrieh et al. [84] also developed an integrated AIbased automated tool to detect and quantify liver fibrosis in NAFLD liver biopsies via CPA; however, in addition, their method also included assessment of six fibrosis architectural patterns. This added feature helps compensate for the absence of spatial information when using CPA alone for quantitative assessment of liver fibrosis, especially since the authors found considerable overlap in CPA across different stages.
It remains to be seen how well these AI-assisted tools perform alone in large scale validation studies. However, these exciting new developments also have the potential to be integrated with SHG-based microscopy to produce a model for assessing liver fibrosis in NAFLD which is sensitive and accurate, and yet also fully automated, widely accessible, and fast-operating.
LIVER COLLAGEN FRACTIONAL SYNTHESIS RATE (FSR)
Most of the above approaches are static measurements of fibrosis and do not give much information regarding the trajectory of disease progression. Decaris et al. [85] recently proposed a novel method to quantify hepatic fibrogenesis flux rates both within liver tissue and noninvasively in blood, via administration of heavy water and tandem mass spectrometry to measure the liver collagen FSR and plasma lumican FSR. They found that the hepatic collagen FSR in NAFLD increased with advancing disease stage, suggesting that even at advanced stages, fibrosis may be reversible if ongoing collagen deposition rates can be reduced. Patients demonstrating a high FSR may thus benefit most from antifibrotic therapies.
INVESTIGATING OTHER CONTRIBUTORS TO FIBROSIS
Elastin
Fibrosis is a mixture of various ECM proteins and glycoproteins, of which collagen is among the most abundant but not the sole component. Elastin is actively synthesized by portal fibroblasts and possibly HSC in the diseased liver, and is biochemically stable compared with collagen [86]. Nakayama et al. [87] found that the presence of perivenular elastic fibers was associated with at least stage 3 fibrosis, and suggested that this may be a useful marker to determine advanced fibrosis in NAFLD; similarly, Masugi et al. [72] detected higher elastin area ratios in advanced stages of NAFLD. Future studies may further clarify the clinical significance of elastin deposition with respect to disease reversibility as well as clinical outcomes.
Activated hepatic stellate cells
Activated HSC can be detected with antibodies against α-smooth muscle cells (ASMA) [88]. The degree of HSC activation correlates with the degree of fibrosis in NAFLD patients [89]. Feldstein et al. [90] devised an HSC activation score using a semiquantitative 12-point scoring system based on ASMA immunohistochemistry, and tested it in a cohort of 39 untreated NAFLD patients with paired liver biopsies. In their study, the HSC score was accurate in predicting fibrosis progression, suggesting that this score may be a useful adjunct to existing staging systems in predicting patients’ fibrosis progression rate, and in patient stratification in antifibrotic clinical trials [91].
Liver sinusoidal endothelial cells (LSEC)
LSEC are now known to be major effectors of inflammation in NASH and thereby contributors to fibrosis. Capillarization of LSECs and LSEC dysfunction appear to precede as well as promote liver fibrosis [92]. Baiocchini et al. [93] recently found that capillarization was only observed at initial stages of liver fibrosis in CHC patients. There are as yet no studies focused on correlating LSEC changes with different stages of fibrosis in NAFLD.
Molecular pathways
In situ mass spectrometry has been performed on liver biopsies, allowing direct characterization of the spatial distribution of various lipid species on tissue sections and providing insights into the pathogenesis of NASH and its progression [94,95]. Urasaki et al. [96] also used hyperspectral simulated Raman scattering microscopy and nanofluidic proteomics to quantitatively measure the liver composition of protein, DNA, and lipids and identify affected cellular signalling and metabolic pathways. However, these techniques have yet to be applied in investigating fibrosis stage in NAFLD.
FUTURE DIRECTIONS
There are many unmet needs in NAFLD. The pathogenesis of the disease and mechanisms responsible for liver fibrosis and remodeling in cirrhosis are still unchartered. The significance of the histological features required for the diagnosis of NASH, and the presently used efficacy endpoints in NASH clinical trials including the absence of ballooning and at least 1-point decrease in fibrosis stage based on current histological scoring systems, may not be adequate and are being questioned [97].
There have been many exciting recent developments and research pathways to address the issue of liver fibrosis. So far, despite its shortcomings, none of the noninvasive tools can currently replace liver biopsy as the reference standard in evaluating the various histological patterns of disease and their severity in NAFLD. The recent application of SHG microscopy on liver tissue samples promises to further refine the accuracy of this ‘gold’ standard, thereby changing the landscape of the role of the liver biopsy (Fig. 2).
Figure 2.
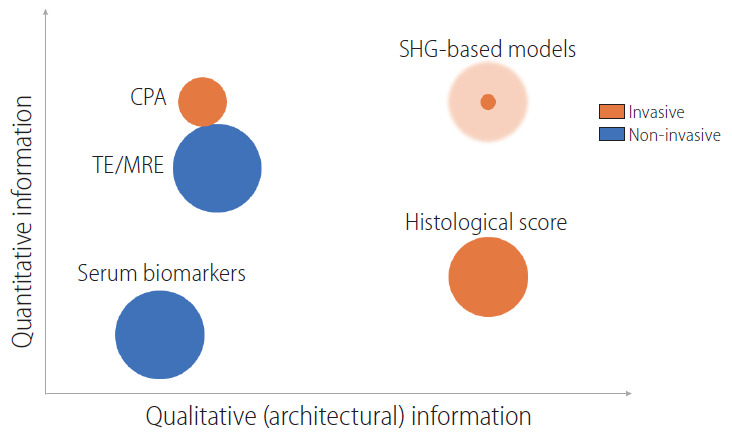
Comparison of the various noninvasive and invasive methods for fibrosis assessment in terms of the quantitative and qualitative information yielded. The size of the circle represents current utility in clinical practice/trials (shaded area represents potential growth). CPA, collagen proportionate area; TE, transient elastography; MRE, magnetic resonance elastography; SHG, second harmonic generation.
SHG-based tools can provide a more standardized, accurate, and precise approach to staging NASH by incorporating a quantitative assessment of changes on a continuous scale across the stages of fibrosis, detecting subtle nuances and characteristics of the deposited collagen fibers, as well as characterizing spatial and architectural changes. SHG microscopy therefore outperforms current staging systems in capturing the full spectrum of fibrosis in NASH, and provides a more reproducible, tractable, and sensitive reference to analyse progression or regression of fibrosis in NASH. Current models can be further refined to assess the severity of perisinusoidal fibrosis at all stages of fibrosis. Integrating the use of AI-assisted systems to achieve a fully-automated and fast-operating system may also facilitate wider adoption of these models.
Much more work needs to be done before these proposed systems and models are used routinely in clinical practice and therapeutic trials. One thing, however, is certain: the liver tissue biopsy still has much to contribute to deepening our understanding and assessment of liver fibrosis in NAFLD.
Acknowledgments
The authors would like to thank Dr. Pang Yin Huei for critical review of the draft manuscript, and Dr. Dean Tai of HistoIndex for contributing the microscopy images.
Abbreviations
- AI
artificial intelligence
- ASMA
antibodies against α-smooth muscle cells
- CARS
coherent anti-Stokes Raman scattering
- CHB
chronic Hepatitis B
- CHC
chronic hepatitis C
- CPA
collagen proportionate area
- ECM
extracellular matrix
- ELF
enhanced liver fibrosis
- FIB-4
fibrosis-4
- FLIP
Fatty Liver: Inhibition of Progression
- FSR
fractional synthesis rate
- HSC
hepatic stellate cells
- LSEC
liver sinusoidal endothelial cells
- MRE
magnetic resonance elastography
- NAFLD
nonalcoholic fatty liver disease
- NAS
nonalcoholic fatty liver disease activity score
- NASH CRN
Nonalcoholic Steatohepatitis Clinical Research Network
- NASH
nonalcoholic steatohepatitis
- NFS
nonalcoholic fatty liver disease fibrosis score
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- q-FPs
quantification of fibrosis-related parameters
- SAF
steatosis activity fibrosis
- SHG
second harmonic generation
- TE
transient elastography
- TPEF
two-photon excitation fluorescence
Footnotes
Authors’ contribution
Gwyneth Soon and Aileen Wee contributed to the literature review and manuscript preparation.
Conflicts of Interest: The authors have no conflicts of interests to disclose.
REFERENCES
- 1.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Younossi Z, Stepanova M, Ong JP, Jacobson IM, Bugianesi E, Duseja A, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates. Clin Gastroenterol Hepatol. 2019;17:748–755. doi: 10.1016/j.cgh.2018.05.057. e3. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999-2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–398. doi: 10.1016/S2468-1253(19)30039-1. [DOI] [PubMed] [Google Scholar]
- 4.Hagström H, Nasr P, Ekstedt M, Hammar U, Stål P, Hultcrantz R, et al. Fibrosis stage but not NASH predicts mortality and time to development of severe liver disease in biopsy-proven NAFLD. J Hepatol. 2017;67:1265–1273. doi: 10.1016/j.jhep.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 5.Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397. doi: 10.1053/j.gastro.2015.04.043. e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65:1557–1565. doi: 10.1002/hep.29085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554. doi: 10.1002/hep.27368. [DOI] [PubMed] [Google Scholar]
- 8.Castera L. Non-invasive tests for liver fibrosis in NAFLD: creating pathways between primary healthcare and liver clinics. Liver Int. 2020;40 Suppl 1:77–81. doi: 10.1111/liv.14347. [DOI] [PubMed] [Google Scholar]
- 9.Tapper EB, Loomba R. Noninvasive imaging biomarker assessment of liver fibrosis by elastography in NAFLD. Nat Rev Gastroenterol Hepatol. 2018;15:274–282. doi: 10.1038/nrgastro.2018.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Shiha G, Ibrahim A, Helmy A, Sarin SK, Omata M, Kumar A, et al. Asian-Pacific Association for the Study of the Liver (APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: a 2016 update. Hepatol Int. 2017;11:1–30. doi: 10.1007/s12072-016-9760-3. [DOI] [PubMed] [Google Scholar]
- 12.Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology. 2019;156:1264–1281. doi: 10.1053/j.gastro.2018.12.036. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanyal AJ, Friedman SL, McCullough AJ, Dimick-Santos L, American Association for the Study of Liver Diseases. United States Food and Drug Administration Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration joint workshop. Hepatology. 2015;61:1392–1405. doi: 10.1002/hep.27678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liou I, Kowdley KV. Natural history of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40 Suppl 1:S11–S16. doi: 10.1097/01.mcg.0000168644.23697.31. [DOI] [PubMed] [Google Scholar]
- 15.Fassio E, Alvarez E, Domínguez N, Landeira G, Longo C. Natural history of nonalcoholic steatohepatitis: a longitudinal study of repeat liver biopsies. Hepatology. 2004;40:820–826. doi: 10.1002/hep.20410. [DOI] [PubMed] [Google Scholar]
- 16.Chávez-Tapia NC, Méndez-Sánchez N, Uribe M. Role of nonalcoholic fatty liver disease in hepatocellular carcinoma. Ann Hepatol. 2009;8 Suppl 1:S34–S39. [PubMed] [Google Scholar]
- 17.Bedossa P. Diagnosis of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: why liver biopsy is essential. Liver Int. 2018;38 Suppl 1:64–66. doi: 10.1111/liv.13653. [DOI] [PubMed] [Google Scholar]
- 18.Wanless IR. Quantitative SHG-microscopy: unraveling the nanoarchitecture of the cirrhotic liver. Clin Res Hepatol Gastroenterol. 2020;44:1–3. doi: 10.1016/j.clinre.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Ratziu V, Friedman SL. Why do so many NASH trials fail? Gastroenterology. 2020 May 18; doi: 10.1053/j.gastro.2020.05.046. doi: 10.1053/j.gastro.2020.05.046. [DOI] [PubMed] [Google Scholar]
- 20.Brunt EM, Kleiner DE, Wilson LA, Sanyal AJ, Neuschwander-Tetri BA, Nonalcoholic Steatohepatitis Clinical Research Network Improvements in histologic features and diagnosis associated with improvement in fibrosis in nonalcoholic steatohepatitis: results from the nonalcoholic steatohepatitis clinical research network treatment trials. Hepatology. 2019;70:522–531. doi: 10.1002/hep.30418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Friedman SL. Liver fibrosis -- from bench to bedside. J Hepatol. 2003;38 Suppl 1:S38–S53. doi: 10.1016/s0168-8278(02)00429-4. [DOI] [PubMed] [Google Scholar]
- 22.Schwabe RF, Tabas I, Pajvani UB. Mechanisms of fibrosis development in nonalcoholic steatohepatitis. Gastroenterology. 2020;158:1913–1928. doi: 10.1053/j.gastro.2019.11.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleiner DE, Makhlouf HR. Histology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis in adults and children. Clin Liver Dis. 2016;20:293–312. doi: 10.1016/j.cld.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Younossi ZM, Loomba R, Anstee QM, Rinella ME, Bugianesi E, Marchesini G, et al. Diagnostic modalities for nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, and associated fibrosis. Hepatology. 2018;68:349–360. doi: 10.1002/hep.29721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang X, Wong GL, Wong VW. Application of transient elastography in nonalcoholic fatty liver disease. Clin Mol Hepatol. 2020;26:128–141. doi: 10.3350/cmh.2019.0001n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park CC, Nguyen P, Hernandez C, Bettencourt R, Ramirez K, Fortney L, et al. Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease. Gastroenterology. 2017;152:598–607. doi: 10.1053/j.gastro.2016.10.026. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaswala DH, Lai M, Afdhal NH. Fibrosis assessment in nonalcoholic fatty liver disease (NAFLD) in 2016. Dig Dis Sci. 2016;61:1356–1364. doi: 10.1007/s10620-016-4079-4. [DOI] [PubMed] [Google Scholar]
- 28.Loomba R. Role of imaging-based biomarkers in NAFLD: recent advances in clinical application and future research directions. J Hepatol. 2018;68:296–304. doi: 10.1016/j.jhep.2017.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Banerjee R, Pavlides M, Tunnicliffe EM, Piechnik SK, Sarania N, Philips R, et al. Multiparametric magnetic resonance for the non-invasive diagnosis of liver disease. J Hepatol. 2014;60:69–77. doi: 10.1016/j.jhep.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDonald N, Eddowes PJ, Hodson J, Semple SIK, Davies NP, Kelly CJ, et al. Multiparametric magnetic resonance imaging for quantitation of liver disease: a two-centre cross-sectional observational study. Sci Rep. 2018;8:9189. doi: 10.1038/s41598-018-27560-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 32.Guha IN, Parkes J, Roderick P, Chattopadhyay D, Cross R, Harris S, et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: validating the European liver fibrosis panel and exploring simple markers. Hepatology. 2008;47:455–460. doi: 10.1002/hep.21984. [DOI] [PubMed] [Google Scholar]
- 33.Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1104–1112. doi: 10.1016/j.cgh.2009.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology. 2017;66:1486–1501. doi: 10.1002/hep.29302. [DOI] [PubMed] [Google Scholar]
- 35.Ampuero J, Pais R, Aller R, Gallego-Durán R, Crespo J, García-Monzón C, et al. Development and validation of hepamet fibrosis scoring system-a simple, noninvasive test to identify patients with nonalcoholic fatty liver disease with advanced fibrosis. Clin Gastroenterol Hepatol. 2020;18:216–225. doi: 10.1016/j.cgh.2019.05.051. e5. [DOI] [PubMed] [Google Scholar]
- 36.Lin B, Ma Y, Wu S, Liu Y, Liu L, Wu L. Novel serum biomarkers for noninvasive diagnosis and screening of nonalcoholic fatty liver disease-related hepatic fibrosis. OMICS. 2019;23:181–189. doi: 10.1089/omi.2019.0035. [DOI] [PubMed] [Google Scholar]
- 37.Loomba R, Seguritan V, Li W, Long T, Klitgord N, Bhatt A, et al. Gut microbiome-based metagenomic signature for non-invasive detection of advanced fibrosis in human nonalcoholic fatty liver disease. Cell Metab. 2017;25:1054–1062. doi: 10.1016/j.cmet.2017.04.001. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caussy C, Tripathi A, Humphrey G, Bassirian S, Singh S, Faulkner C, et al. A gut microbiome signature for cirrhosis due to nonalcoholic fatty liver disease. Nat Commun. 2019;10:1406. doi: 10.1038/s41467-019-09455-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Younossi ZM, Karrar A, Pierobon M, Birerdinc A, Stepanova M, Abdelatif D, et al. An exploratory study examining how nano-liquid chromatography-mass spectrometry and phosphoproteomics can differentiate patients with advanced fibrosis and higher percentage collagen in non-alcoholic fatty liver disease. BMC Med. 2018;16:170. doi: 10.1186/s12916-018-1136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pirola CJ, Sookoian S. Multiomics biomarkers for the prediction of nonalcoholic fatty liver disease severity. World J Gastroenterol. 2018;24:1601–1615. doi: 10.3748/wjg.v24.i15.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hardy T, McPherson S. Imaging-based assessment of steatosis, inflammation and fibrosis in NAFLD. Curr Hepatology Rep. 2017;16:298–307. [Google Scholar]
- 42.Karsdal MA, Krarup H, Sand JM, Christensen PB, Gerstoft J, Leeming DJ, et al. Review article: the efficacy of biomarkers in chronic fibroproliferative diseases - early diagnosis and prognosis, with liver fibrosis as an exemplar. Aliment Pharmacol Ther. 2014;40:233–249. doi: 10.1111/apt.12820. [DOI] [PubMed] [Google Scholar]
- 43.Salarian M, Turaga RC, Xue S, Nezafati M, Hekmatyar K, Qiao J, et al. Early detection and staging of chronic liver diseases with a protein MRI contrast agent. Nat Commun. 2019;10:4777. doi: 10.1038/s41467-019-11984-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fuchs BC, Wang H, Yang Y, Wei L, Polasek M, Schühle DT, et al. Molecular MRI of collagen to diagnose and stage liver fibrosis. J Hepatol. 2013;59:992–998. doi: 10.1016/j.jhep.2013.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li S, Sun X, Chen M, Ying Z, Wan Y, Pi L, et al. Liver fibrosis conventional and molecular imaging diagnosis update. J Liver. 2019;8:236. [PMC free article] [PubMed] [Google Scholar]
- 46.Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 47.Ooi GJ, Clouston A, Johari Y, Kemp WW, Roberts SK, Brown WA, et al. Evaluation of the histological variability of core and wedge biopsies in nonalcoholic fatty liver disease in bariatric surgical patients. Surg Endosc. 2020 Mar 13; doi: 10.1007/s00464-020-07490-y. doi: 10.1007/s00464-020-07490-y. [DOI] [PubMed] [Google Scholar]
- 48.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 49.Vuppalanchi R, Unalp A, Van Natta ML, Cummings OW, Sandrasegaran KE, Hameed T, et al. Effects of liver biopsy sample length and number of readings on sampling variability in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:481–486. doi: 10.1016/j.cgh.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bedossa P, Dargère D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449–1457. doi: 10.1016/j.hep.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 51.Goldstein NS, Hastah F, Galan MV, Gordon SC. Fibrosis heterogeneity in nonalcoholic steatohepatitis and hepatitis C virus needle core biopsy specimens. Am J Clin Pathol. 2005;123:382–387. doi: 10.1309/EY72-F1EN-9XCB-1KXX. [DOI] [PubMed] [Google Scholar]
- 52.Colloredo G, Guido M, Sonzogni A, Leandro G. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol. 2003;39:239–244. doi: 10.1016/s0168-8278(03)00191-0. [DOI] [PubMed] [Google Scholar]
- 53.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 54.Sanyal AJ, Brunt EM, Kleiner DE, Kowdley KV, Chalasani N, Lavine JE, et al. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54:344–353. doi: 10.1002/hep.24376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA, NASH Clinical Research Network (CRN) Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–820. doi: 10.1002/hep.24127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bedossa P, FLIP Pathology Consortium Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60:565–575. doi: 10.1002/hep.27173. [DOI] [PubMed] [Google Scholar]
- 57.Bedossa P, Poitou C, Veyrie N, Bouillot JL, Basdevant A, Paradis V, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–1759. doi: 10.1002/hep.25889. [DOI] [PubMed] [Google Scholar]
- 58.Nascimbeni F, Bedossa P, Fedchuk L, Pais R, Charlotte F, Lebray P, et al. Clinical validation of the FLIP algorithm and the SAF score in patients with non-alcoholic fatty liver disease. J Hepatol. 2020;72:828–838. doi: 10.1016/j.jhep.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 59.Poynard T, Lenaour G, Vaillant JC, Capron F, Munteanu M, Eyraud D, et al. Liver biopsy analysis has a low level of performance for diagnosis of intermediate stages of fibrosis. Clin Gastroenterol Hepatol. 2012;10:657–663. doi: 10.1016/j.cgh.2012.01.023. e7. [DOI] [PubMed] [Google Scholar]
- 60.Brunt EM. Nonalcoholic fatty liver disease and the ongoing role of liver biopsy evaluation. Hepatol Commun. 2017;1:370–378. doi: 10.1002/hep4.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pai RK, Kleiner DE, Hart J, Adeyi OA, Clouston AD, Behling CA, et al. Standardising the interpretation of liver biopsies in non-alcoholic fatty liver disease clinical trials. Aliment Pharmacol Ther. 2019;50:1100–1111. doi: 10.1111/apt.15503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–654. doi: 10.1016/j.cgh.2014.04.014. e1-e9; quiz e39-e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sun Y, Zhou J, Wang L, Wu X, Chen Y, Piao H, et al. New classification of liver biopsy assessment for fibrosis in chronic hepatitis B patients before and after treatment. Hepatology. 2017;65:1438–1450. doi: 10.1002/hep.29009. [DOI] [PubMed] [Google Scholar]
- 64.Theise ND, Jia J, Sun Y, Wee A, You H. Progression and regression of fibrosis in viral hepatitis in the treatment era: the Beijing classification. Mod Pathol. 2018;31:1191–1200. doi: 10.1038/s41379-018-0048-0. [DOI] [PubMed] [Google Scholar]
- 65.Bedossa P, Patel K. Biopsy and noninvasive methods to assess progression of nonalcoholic fatty liver disease. Gastroenterology. 2016;150:1811–1822. doi: 10.1053/j.gastro.2016.03.008. e4. [DOI] [PubMed] [Google Scholar]
- 66.Standish RA, Cholongitas E, Dhillon A, Burroughs AK, Dhillon AP. An appraisal of the histopathological assessment of liver fibrosis. Gut. 2006;55:569–578. doi: 10.1136/gut.2005.084475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Calvaruso V, Burroughs AK, Standish R, Manousou P, Grillo F, Leandro G, et al. Computer-assisted image analysis of liver collagen: relationship to Ishak scoring and hepatic venous pressure gradient. Hepatology. 2009;49:1236–1244. doi: 10.1002/hep.22745. [DOI] [PubMed] [Google Scholar]
- 68.Tsochatzis E, Bruno S, Isgro G, Hall A, Theocharidou E, Manousou P, et al. Collagen proportionate area is superior to other histological methods for sub-classifying cirrhosis and determining prognosis. J Hepatol. 2014;60:948–954. doi: 10.1016/j.jhep.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 69.Buzzetti E, Hall A, Ekstedt M, Manuguerra R, Guerrero Misas M, Covelli C, et al. Collagen proportionate area is an independent predictor of long-term outcome in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2019;49:1214–1222. doi: 10.1111/apt.15219. [DOI] [PubMed] [Google Scholar]
- 70.Forlano R, Mullish BH, Giannakeas N, Maurice JB, Angkathunyakul N, Lloyd J, et al. High-throughput, machine learning-based quantification of steatosis, inflammation, ballooning, and fibrosis in biopsies from patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2020;18:2081–2090. doi: 10.1016/j.cgh.2019.12.025. e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hall AR, Tsochatzis E, Morris R, Burroughs AK, Dhillon AP. Sample size requirement for digital image analysis of collagen proportionate area in cirrhotic livers. Histopathology. 2013;62:421–430. doi: 10.1111/his.12010. [DOI] [PubMed] [Google Scholar]
- 72.Masugi Y, Abe T, Tsujikawa H, Effendi K, Hashiguchi A, Abe M, et al. Quantitative assessment of liver fibrosis reveals a nonlinear association with fibrosis stage in nonalcoholic fatty liver disease. Hepatol Commun. 2017;2:58–68. doi: 10.1002/hep4.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gailhouste L, Le Grand Y, Odin C, Guyader D, Turlin B, Ezan F, et al. Fibrillar collagen scoring by second harmonic microscopy: a new tool in the assessment of liver fibrosis. J Hepatol. 2010;52:398–406. doi: 10.1016/j.jhep.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 74.Guilbert T, Odin C, Le Grand Y, Gailhouste L, Turlin B, Ezan F, et al. A robust collagen scoring method for human liver fibrosis by second harmonic microscopy. Opt Express. 2010;18:25794–25807. doi: 10.1364/OE.18.025794. [DOI] [PubMed] [Google Scholar]
- 75.Sun W, Chang S, Tai DC, Tan N, Xiao G, Tang H, et al. Nonlinear optical microscopy: use of second harmonic generation and two-photon microscopy for automated quantitative liver fibrosis studies. J Biomed Opt. 2008;13:064010. doi: 10.1117/1.3041159. [DOI] [PubMed] [Google Scholar]
- 76.Chang PE, Goh GBB, Leow WQ, Shen L, Lim KH, Tan CK. Second harmonic generation microscopy provides accurate automated staging of liver fibrosis in patients with non-alcoholic fatty liver disease. PLoS One. 2018;13:e0199166. doi: 10.1371/journal.pone.0199166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu F, Zhao JM, Rao HY, Yu WM, Zhang W, Theise ND, et al. Second harmonic generation reveals subtle fibrosis differences in adult and pediatric nonalcoholic fatty liver disease. Am J Clin Pathol. 2017;148:502–512. doi: 10.1093/ajcp/aqx104. [DOI] [PubMed] [Google Scholar]
- 78.Pirhonen J, Arola J, Sädevirta S, Luukkonen P, Karppinen SM, Pihlajaniemi T, et al. Continuous grading of early fibrosis in nafld using label-free imaging: a proof-of-concept study. PLoS One. 2016;11:e0147804. doi: 10.1371/journal.pone.0147804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang Y, Vincent R, Yang J, Asgharpour A, Liang X, Idowu MO, et al. Dual-photon microscopy-based quantitation of fibrosis-related parameters (q-FP) to model disease progression in steatohepatitis. Hepatology. 2017;65:1891–1903. doi: 10.1002/hep.29090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xu S, Wang Y, Tai DCS, Wang S, Cheng CL, Peng Q, et al. qFibrosis: a fully-quantitative innovative method incorporating histological features to facilitate accurate fibrosis scoring in animal model and chronic hepatitis B patients. J Hepatol. 2014;61:260–269. doi: 10.1016/j.jhep.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang Y, Wong GL, He FP, Sun J, Chan AW, Yang J, et al. Quantifying and monitoring fibrosis in non-alcoholic fatty liver disease using dual-photon microscopy. Gut. 2020;69:1116–1126. doi: 10.1136/gutjnl-2019-318841. [DOI] [PubMed] [Google Scholar]
- 82.Liu F, Goh GB, Tiniakos D, Wee A, Leow WQ, Zhao JM, et al. qFIBS: an automated technique for quantitative evaluation of fibrosis, inflammation, ballooning, and steatosis in patients with nonalcoholic steatohepatitis. Hepatology. 2020;71:1953–1966. doi: 10.1002/hep.30986. [DOI] [PubMed] [Google Scholar]
- 83.Yu Y, Wang J, Ng CW, Ma Y, Mo S, Fong ELS, et al. Deep learning enables automated scoring of liver fibrosis stages. Sci Rep. 2018;8:16016. doi: 10.1038/s41598-018-34300-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gawrieh S, Sethunath D, Cummings OW, Kleiner DE, Vuppalanchi R, Chalasani N, et al. Automated quantification and architectural pattern detection of hepatic fibrosis in NAFLD. Ann Diagn Pathol. 2020;47:151518. doi: 10.1016/j.anndiagpath.2020.151518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Decaris ML, Li KW, Emson CL, Gatmaitan M, Liu S, Wang Y, et al. Identifying nonalcoholic fatty liver disease patients with active fibrosis by measuring extracellular matrix remodeling rates in tissue and blood. Hepatology. 2017;65:78–88. doi: 10.1002/hep.28860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kanta J. Elastin in the liver. Front Physiol. 2016;7:491. doi: 10.3389/fphys.2016.00491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nakayama H, Itoh H, Kunita S, Kuroda N, Hiroi M, Matsuura H, et al. Presence of perivenular elastic fibers in nonalcoholic steatohepatitis fibrosis stage III. Histol Histopathol. 2008;23:407–409. doi: 10.14670/HH-23.407. [DOI] [PubMed] [Google Scholar]
- 88.Mann DA, Smart DE. Transcriptional regulation of hepatic stellate cell activation. Gut. 2002;50:891–896. doi: 10.1136/gut.50.6.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Washington K, Wright K, Shyr Y, Hunter EB, Olson S, Raiford DS. Hepatic stellate cell activation in nonalcoholic steatohepatitis and fatty liver. Hum Pathol. 2000;31:822–828. doi: 10.1053/hupa.2000.8440. [DOI] [PubMed] [Google Scholar]
- 90.Feldstein AE, Papouchado BG, Angulo P, Sanderson S, Adams L, Gores GJ. Hepatic stellate cells and fibrosis progression in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2005;3:384–389. doi: 10.1016/s1542-3565(04)00616-0. [DOI] [PubMed] [Google Scholar]
- 91.Trautwein C, Friedman SL, Schuppan D, Pinzani M. Hepatic fibrosis: concept to treatment. J Hepatol. 2015;62(1 Suppl):S15–S24. doi: 10.1016/j.jhep.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 92.Hammoutene A, Rautou PE. Role of liver sinusoidal endothelial cells in non-alcoholic fatty liver disease. J Hepatol. 2019;70:1278–1291. doi: 10.1016/j.jhep.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 93.Baiocchini A, Del Nonno F, Taibi C, Visco-Comandini U, D’Offizi G, Piacentini M, et al. Liver sinusoidal endothelial cells (LSECs) modifications in patients with chronic hepatitis C. Sci Rep. 2019;9:8760. doi: 10.1038/s41598-019-45114-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wattacheril J, Seeley EH, Angel P, Chen H, Bowen BP, Lanciault C, et al. Differential intrahepatic phospholipid zonation in simple steatosis and nonalcoholic steatohepatitis. PLoS One. 2013;8:e57165. doi: 10.1371/journal.pone.0057165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hall Z, Bond NJ, Ashmore T, Sanders F, Ament Z, Wang X, et al. Lipid zonation and phospholipid remodeling in nonalcoholic fatty liver disease. Hepatology. 2017;65:1165–1180. doi: 10.1002/hep.28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Urasaki Y, Zhang C, Cheng JX, Le TT. Quantitative assessment of liver steatosis and affected pathways with molecular imaging and proteomic profiling. Sci Rep. 2018;8:3606. doi: 10.1038/s41598-018-22082-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yoo JJ, Kim W, Kim MY, Jun DW, Kim SG, Yeon JE, et al. Recent research trends and updates on nonalcoholic fatty liver disease. Clin Mol Hepatol. 2019;25:1–11. doi: 10.3350/cmh.2018.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]