Abstract
Few studies have investigated the impact of a change in metabolic syndrome (MetS) components on clinical renal outcomes in the general population. Using nationally representative data from the Korean National Health Insurance System, 13,310,924 subjects who underwent two health examinations over 2 years and were free from end-stage renal disease (ESRD) from 2009 to 2012 were followed to the end of 2016. The subjects were divided into four groups according to the change in MetS components between the two visits over 2 years: no MetS (–/–), post-MetS (–/+), pre-MetS (+/–), and both MetS (+/+). After a median follow up of 5.11 years, 18,582 incident ESRD cases were identified. In the multivariate adjusted model, the hazard ratio (HR) and 95% confidence interval (CI) for the development of ESRD in the both-MetS (+/+) group compared with the no-MetS (–/–) group was 5.65 (95% CI, 5.42–5.89), which was independent of age, sex, and baseline estimated glomerular filtration rate. Additionally, the HR for the pre-MetS (+/–) group versus the no-MetS (–/–) group was 2.28 (2.15–2.42). In subgroup analysis according to renal function, the impact of a change in MetS on the incidence of ESRD was more pronounced in individuals with advanced renal dysfunction. Subjects with resolved MetS components had a decreased risk of ESRD, but not as low as those that never had MetS components. This provides evidence supporting the strategy of modulating MetS in the general population to prevent the development of ESRD.
Subject terms: Endocrinology, Health care
Introduction
Metabolic syndrome (MetS) is defined as the simultaneous occurrence of at least three of the following: abdominal obesity, elevated blood pressure (BP), elevated plasma glucose, and dyslipidaemia1. When these metabolic abnormalities are grouped together, they are associated with an increased risk of both diabetes and cardiovascular disease (CVD). Reports have demonstrated that MetS plays a critical role in the progression of chronic kidney disease (CKD) and CVD2–4. Since CKD is an established risk factor for CVD, it is unsurprising that MetS is a potential risk factor for CKD progression. Furthermore, diabetes and hypertension are the leading causes of the development of both CKD and end-stage renal disease (ESRD)5. Because impaired fasting glucose and elevated BP are included in the definition of MetS, investigations of the independent associations among the other three components of MetS and renal outcome are also important. In a recent cohort study performed in elderly Japanese women, both the presence of MetS and the number of MetS components were associated with a higher prevalence of CKD, and the MetS BP criterion may have enhanced the association6. In addition, Stefansson and collaborators3 confirmed MetS as an independent risk factor for an accelerated age-related glomerular filtration rate (GFR) decline in the general population. They showed that individuals with baseline MetS had a significantly faster mean decline of 0.30 mL/min/year compared with individuals without MetS in a multivariable adjusted linear regression model. However, other studies have reported a non-significant association between MetS and the risk of CKD development and cardiovascular risk7–9. Thus, controversies remain regarding this relationship.
MetS status can change over time through factors such as lifestyle modification or diverse comorbidities. Indeed, previous studies have observed considerable changes in the MetS status of individuals over follow-up periods10–12. Therefore, we investigated the associations between changes in MetS components and the incidence of ESRD in the general Korean population using a nationwide population-based cohort.
Methods
Data source and study population
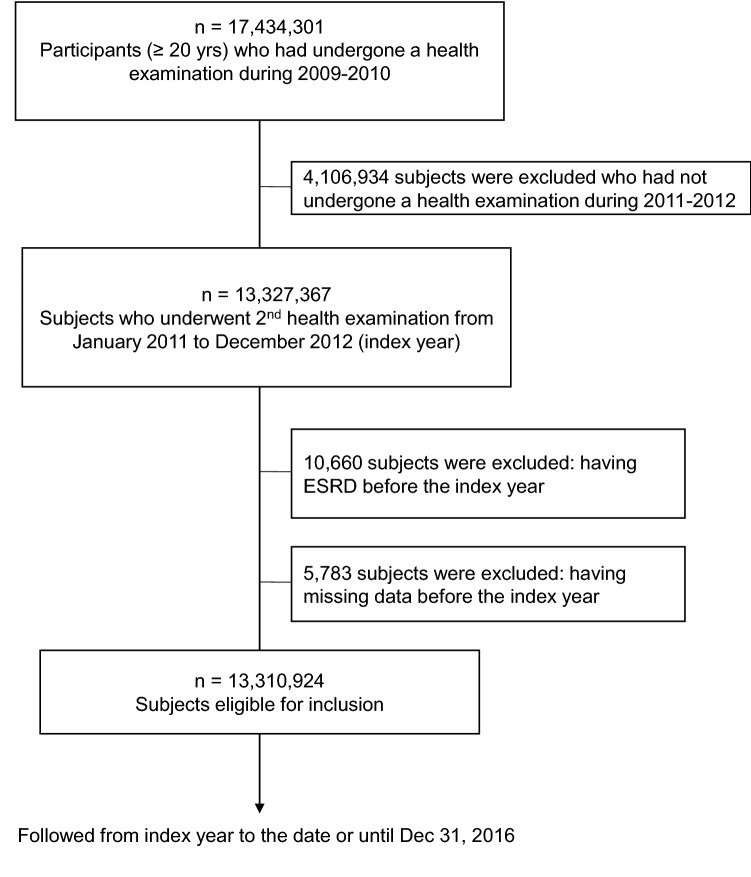
We used the National Health Insurance System (NHIS) database; the NIHS is government-managed and the only insurer providing regular health check-up programs to the public in South Korea. Those enrolled in the health insurance service are recommended to undergo health check-ups at least biennially. In the current study, we included 17,434,301 subjects aged ≥ 20 years who underwent a health examination between 2009 and 2010. Of these, we included 13,327,367 subjects with two visits over 2 years; underwent a second health examination during 2011–2012 (index year). We excluded 10,660 subjects having ESRD and 5,783 subjects having missing data prior to the index year. Finally, the study included 13,310,924 subjects (Fig. 1). All research was performed in accordance with relevant guidelines and regulations.
Figure 1.
Study enrolment flow.
Data collection
Comorbidities were defined mainly by a combination of past history (ICD code and self-reported) and use of medication history for the corresponding disease. The presence of hypertension was defined according to the presence of at least one claim per year under ICD-10 codes I10 or I11 and at least one claim per year for the prescription of an antihypertensive agent or systolic/diastolic BP ≥ 140/90 mmHg13,14. The presence of diabetes mellitus was defined according to the following criteria: (1) at least one claim per year under ICD–10 codes E10–14 and at least one claim per year for the prescription of antidiabetic medication, or (2) fasting glucose level ≥ 126 mg/dL13. Blood samples for the measurement of serum glucose, creatinine (Cr), total cholesterol, triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) levels were drawn after fasting overnight. Estimated GFR was calculated using the four variable modification of diet in renal disease (MDRD) formula: eGFR = 175 × serum Cr (mg/dL) –1.154 × age (y) – 0.203 × (0.742 if female)15,16.
Diagnosis of metabolic syndrome and definition of the change in metabolic syndrome components
Based on the National Cholesterol Education Program’s Adult Treatment Panel III13, we defined MetS as at least three of the five following criteria: (1) abdominal obesity, as defined by a waist circumference (WC) ≥ 90 cm for men and ≥ 85 cm for women; (2) elevated TG levels (≥ 150 mg/dL); (3) decreased HDL-C levels (< 40 mg/dL for men and < 50 mg/ dL for women); (4) elevated BP (systolic BP ≥ 130 mmHg, diastolic BP ≥ 85 mmHg) or treatment for previously diagnosed hypertension; and (5) elevated fasting plasma glucose levels (≥ 100 mg/dL) or previously diagnosed diabetes mellitus type 2.
We divided the individuals into four groups according to the changes in MetS components over the 2-year interval between the first and second health exam: no MetS (–/–), post-MetS (–/+), pre-MetS (+/–), and both MetS (+/+). Individuals in the no-MetS (–/–) group had no diagnosis of MetS at either exam, those in the post-MetS (–/+) group were newly diagnosed with MetS at the second visit, those in the pre-MetS (+/–) group resolved MetS after the first exam, and the both-MetS (+/+) group had MetS that persisted at both exams.
Study outcome and follow-up
The study outcome was newly diagnosed ESRD. We defined incident ESRD using the combination of ICD-10 code (N18-19, Z49, Z94.0, Z99.2) and initiation of renal replacement therapy and/or kidney transplantation (KT) during hospitalisation13. The Korean Health Insurance Review and Assessment Service reimburses all medical care expenses for dialysis. Patients with ESRD are also registered as special medical aid beneficiaries17. Therefore, we could include each ESRD patient in the whole South Korean population and analyse the data for all ESRD patients who started dialysis17,18. The codes for treatment or medical expense claims were O7011-O7020 or V001 for haemodialysis, O7071-O7075 or V003 for peritoneal dialysis, and R3280 for KT14. We excluded individuals without previous CKD who had a transplant or dialysis code on the same date as an acute renal failure code. Subjects on continuous renal replacement therapy or acute peritoneal dialysis were also excluded17,18. The study population was followed from baseline at the index year to the date of ESRD diagnosis or December 31, 2016, whichever came first.
Statistical analysis
Baseline characteristics are presented as means ± standard deviation or n (%). The incidence of primary outcomes was calculated by dividing the number of incident cases by the total follow-up duration (person-years)19. The disease-free probability of primary outcomes according to the change in MetS components was calculated using Kaplan–Meier curves, and a log-rank test was performed to analyse differences among the groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) for ESRD were calculated using a Cox proportional hazards model for each category. Model 1 was adjusted for number of MetS components at 1st visit, age and sex. Model 2 was additionally adjusted for smoking status, alcohol consumption and exercise with variables from model 1. In model 3, we further adjusted for eGFR in addition to variables from model 2. Statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA), and a P value < 0.05 was considered to indicate significance.
Ethics approval and consent to participate
This study was conducted according to the Declaration of Helsinki. Informed consent requirement was waived by the Ethics Committee of The Catholic University of Korea, because personal identifying information was not accessed. The study was approved by the Institutional Review Board of The Catholic University of Korea (No. SC18ZESI0053).
Results
Characteristics of each group according to the change in MetS components
Table 1 shows the demographics of the study population according the change in MetS components. The proportion of subjects in the no-MetS (–/–) group was 61.3%, compared with 10.8%, 8.3%, and 19.5% in the post-MetS (–/+), pre-MetS (+/–), and both-MetS (+/+) groups, respectively. Individuals in the both-MetS (+/+) group were generally older, female, had a higher body mass index (BMI) and a larger WC, exercised less, had a higher prevalence of diabetes and hypertension, increased TG levels, and lower HDL-C and LDL-C levels (Table 1).
Table 1.
Demographics of the study population according the change in MetS components.
| No-MetS (–/–) | Post-MetS (–/+) | Pre-MetS (+/–) | Both-MetS (+/+) | |
|---|---|---|---|---|
| (n = 8,167,333) | (n = 1,438,425) | (n = 1,105,622) | (n = 2,599,544) | |
| At second visit (index year) | ||||
| Age, years | 46.4 ± 13.1 | 53.7 ± 12.9 | 54.3 ± 12.9 | 59.0 ± 12.0 |
| Male, n (%) | 4,297,945 (52.6) | 820,951 (57.1) | 643,050 (58.2) | 1,288,805 (49.6) |
| BMI, kg/ m2 | 22.8 ± 2.8 | 25.1 ± 3.0 | 24.7 ± 2.9 | 26.0 ± 3.1 |
| Body weight, kg | 61.6 ± 10.6 | 67.3 ± 12.1 | 66.2 ± 11.7 | 68.2 ± 12.5 |
| Height, cm | 164.2 ± 8.9 | 163.2 ± 9.6 | 163.2 ± 9.6 | 161.4 ± 9.7 |
| WC, cm | 77.4 ± 8.0 | 85.0 ± 7.8 | 82.8 ± 7.7 | 87.3 ± 8.1 |
| Current smoker, n (%) | 1,856,325 (22.8) | 342,407 (23.8) | 263,912 (23.9) | 494,569 (19.0) |
| Heavy drinker, n (%) | 429,794 (5.3) | 106,839 (7.5) | 78,270 (7.1) | 170,747 (6.6) |
| Regular exercise, n (%) | 4,579,387 (56.1) | 750,991 (52.2) | 591,503 (53.5) | 1,273,424 (49.0) |
| Income lower 25%, n (%) | 1,754,695 (21.5) | 325,070 (22.6) | 252,501 (22.8) | 603,356 (23.2) |
| Diabetes, n (%) | 113,671 (1.4) | 106,124 (7.4) | 74,375 (6.7) | 681,161 (26.2) |
| Hypertension, n (%) | 601,039 (7.4) | 422,136 (29.4) | 264,618 (23.9) | 1,488,282 (57.3) |
| eGFR, mL/min/1.73 m2 | 91.6 ± 36.6 | 87.8 ± 35.0 | 88.2 ± 36.4 | 84.7 ± 34.4 |
| Fasting glucose, mg/dL | 92.1 ± 14.3 | 104.3 ± 22.8 | 98.56 ± 22.33 | 112.69 ± 31.97 |
| Systolic BP, mmHg | 118.3 ± 13.4 | 129.4 ± 13.8 | 124.75 ± 13.9 | 130.8 ± 14.6 |
| Diastolic BP, mmHg | 74.0 ± 9.3 | 80.3 ± 9.6 | 77.62 ± 9.39 | 80.16 ± 9.92 |
| TC, mg/dL | 192.0 ± 33.2 | 205.1 ± 40.0 | 201.93 ± 36.02 | 197.37 ± 42.12 |
| TG, mg/dL | 93.7 (93.7–93.8) | 158.0 (157.9–158.1) | 122.91 (122.8–123.02) | 163.19 (163.09–163.3) |
| HDL-C, mg/dL | 58.0 ± 14.1 | 50.2 ± 14.1 | 53.1 ± 13.8 | 49.1 ± 13.9 |
| LDL-C, mg/dL | 113.2 ± 35.2 | 120.4 ± 41.9 | 122.0 ± 37.6 | 112.5 ± 44.0 |
| At first visit | ||||
| BMI, kg/ m2 | 22.7 ± 2.7 | 24.73 ± 2.83 | 25.05 ± 2.88 | 26.08 ± 3.07 |
| WC, cm | 77.0 ± 8.0 | 82.74 ± 7.55 | 84.97 ± 7.64 | 87.25 ± 7.94 |
| eGFR, mL/min/1.73 m2 | 89.6 ± 44.2 | 86.39 ± 38.56 | 85.56 ± 37.99 | 83.04 ± 36.12 |
| Fasting glucose, mg/dL | 91.6 ± 14.5 | 97.3 ± 21.66 | 104.33 ± 23.23 | 111.91 ± 32.12 |
| Systolic BP, mmHg | 118.1 ± 13.3 | 124.68 ± 14.11 | 129.76 ± 13.75 | 131.38 ± 14.78 |
| Diastolic BP, mmHg | 73.9 ± 9.2 | 77.79 ± 9.48 | 80.50 ± 9.57 | 80.86 ± 9.98 |
| TC, mg/dL | 190.0 ± 33.0 | 205.33 ± 36.46 | 203.88 ± 38.4 | 203.91 ± 42.2 |
| TG, mg/dL | 92.8 (92.8–92.8) | 125.71 (125.61–125.8) | 162.6 (162.4–162.8) | 170.9 (170.8–171.0) |
Data are expressed as the mean ± SD, median value (interquartile range) or n (%).
MetS metabolic syndrome, BMI body mass index, WC waist circumference, BP blood pressure, TC total cholesterol, TG triglyceride, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, eGFR estimated glomerular filtration rate.
Association between the presence of each MetS component and the risk of ESRD
After a median follow up of 5.11 years, 18,582 incident ESRD cases were identified. We analysed the impact of the presence of each MetS component on the incidence of ESRD (Table 2). Subjects with MetS had a hazard ratio (HR) of 3.51 (95% confidence intervals (CI), 3.40–3.63) for incident ESRD compared with those without MetS after adjusting for age and sex (model 1). After additionally adjusted for smoking status, alcohol consumption and exercise with variables from model 1 (model 2), subjects with MetS had a HR of 4.07 (95% CI, 3.93–4.22); in model 3 with further adjusting for eGFR, those had a HR of 3.57 (95% CI, 3.45–3.70). All MetS criteria increased the risk of ESRD development, among which the BP criterion had the highest HR. That is, subjects with the BP criterion had a 4.57-fold increased risk of ESRD development compared with those without the BP criterion. Among the five MetS, WC had the lowest HR of 1.55 (95% CI, 1.49–1.61) versus those without central obesity after adjusting for all confounding variables (model 3).
Table 2.
Adjusted hazard ratios, 95% confidence intervals, and incidence rates of end-stage renal disease development according to the presence of each MetS component.
| N | Events (n) | Follow-up duration (person-years) | Incidence rate (per 1000 person-years) | Adjusted hazard ratios ( 95% confidence intervals) | |||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||
| WC criterion | |||||||
| No | 10,544,298 | 12,275 | 52,652,426 | 0.23 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 2,766,626 | 6,307 | 13,733,667 | 0.46 | 1.45 (1.41, 1.49) | 1.51 (1.45, 1.57) | 1.55 (1.49, 1.61) |
| BP criterion | |||||||
| No | 7,181,413 | 2,252 | 35,937,081 | 0.06 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 6,129,511 | 16,330 | 30,449,013 | 0.54 | 4.85 (4.63, 5.07) | 5.23 (5.00, 5.48) | 4.57 (4.36, 4.78) |
| Glucose criterion | |||||||
| No | 8,904,300 | 6,473 | 44,579,195 | 0.15 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 4,406,624 | 12,109 | 21,806,898 | 0.56 | 2.53 (2.46, 2.61) | 2.59 (2.51, 2.67) | 2.26(2.19, 2.33) |
| TG criterion | |||||||
| No | 8,303,071 | 6,610 | 41,430,791 | 0.16 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 5,007,853 | 11,972 | 24,955,302 | 0.48 | 2.25 (2.19, 2.32) | 2.29 (2.22, 2.36) | 2.1 (2.03,2.16) |
| HDL-C criterion | |||||||
| No | 9,204,479 | 6662 | 46,048,303 | 0.15 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 4,106,445 | 11,920 | 20,337,791 | 0.59 | 3.11 (3.01, 3.20) | 2.99 (2.90, 3.09) | 2.66 (2.58, 2.75) |
| MetS | |||||||
| No | 9,272,955 | 5498 | 46,399,629 | 0.12 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Yes | 4,037,969 | 13,084 | 19,986,465 | 0.65 | 3.51 (3.40, 3.63) | 4.07 (3.93, 4.22) | 3.57 (3.45, 3.70) |
Model 1, adjusted for No. of MetS components at 1st visit, age and sex; Model 2, Model 1 plus adjusted for smoking, drinking and exercise; Model 3, Model 2 plus adjusted for estimated GFR.
WC waist circumference, BP blood pressure, TG triglyceride, HDL-C high-density lipoprotein cholesterol; MetS, metabolic syndrome.
Consistent with previous reports, the risk of ESRD development increased progressively as the number of components of MetS increased from one to five criteria; subjects with five criteria of MetS had an ~ 24-fold increased risk of developing ESRD compared with subjects with no criteria. These results showed a similar pattern as the data from the first visit (Supplementary Table S1).
Risk of ESRD according to the change in each MetS component
We assessed the associations between the change in each MetS component and the risk of ESRD development (Table 3). The HR and 95% CI comparing the both-MetS (+/+) group with the no-MetS (–/–) group was 5.09 (95% CI, 4.90–5.28) for ESRD development in model 1, and 6.69 (95% CI, 6.42–6.97) in model 2 and 5.65 (95% CI, 5.42–5.89) in model 3, respectively. In terms of WC, the HR for ESRD in the both-WC (+/+) group was 1.95 (95% CI, 1.86–2.05), compared with 1.53 (1.45–1.61) in the pre-WC (+/–) group after adjusting for all confounding variables including baseline eGFR (model 3). The HR of individuals in the both-BP (+/+) group was 7.02 (95% CI, 6.62–7.44), whereas that of individuals in the resolved-BP (+/–) group was 1.94 (1.78–2.11) in model 3. Also, the results with other MetS criteria—including glucose, TG and HDL-C showed the similar pattern (Table 3). However, the change in obesity, which was defined as a BMI > 25 kg/m2, had a particularly interesting effect. Unlike other MetS criteria, subjects in the resolved-obesity (+/–) group had a higher risk of ESRD development than persistently obese subjects when the no-obesity (–/–) group was used as the reference.
Table 3.
Adjusted hazard ratios, 95% confidence intervals, and incidence rates of end-stage renal disease development according to the change of each MetS component.
| N | Events (n) | Follow-up duration (person-years) | Incidence rate (per 1000 person-years) | Adjusted hazard ratios ( 95% confidence intervals) | ||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||
| WC criterion | No (–/–) | 9,652,099 | 10,380 | 48,230,672 | 0.22 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 1,010,018 | 1705 | 5,015,280 | 0.34 | 1.23 (1.17,1.30) | 1.36 (1.29, 1.44) | 1.44 (1.36,1.52) | |
| Pre (+/–) | 892,199 | 1895 | 4,421,754 | 0.43 | 1.38 (1.32,1.45) | 1.49 (1.42, 1.57) | 1.53 (1.45,1.61) | |
| Both (+/+) | 1,756,608 | 4602 | 8,718,387 | 0.53 | 1.66 (1.60,1.72) | 1.93 (1.84, 2.02) | 1.95 (1.86, 2.05) | |
| BP criterion | No (–/–) | 5,746,514 | 1374 | 28,742,096 | 0.05 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 1,685,406 | 1314 | 8,424,416 | 0.16 | 2.32 (2.15, 2.50) | 2.50 (2.32, 2.70) | 2.4 (2.22, 2.59) | |
| Pre (+/–) | 1,434,899 | 878 | 7,194,985 | 0.12 | 1.84 (1.69, 2.00) | 1.95 (1.79, 2.13) | 1.94 (1.78, 2.11) | |
| Both (+/+) | 4,444,105 | 15,016 | 22,024,597 | 0.68 | 7.21 (6.81, 7.63) | 8.25 (7.78, 8.74) | 7.02 (6.62, 7.44) | |
| Glucose criterion | No (–/–) | 7,347,391 | 4918 | 36,791,423 | 0.13 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 1,760,736 | 1742 | 8,761,835 | 0.20 | 1.13 (1.07,1.20) | 1.17 (1.10, 1.23) | 1.06 (1.01, 1.12) | |
| Pre (+/–) | 1,556,909 | 1555 | 7,787,772 | 0.20 | 1.16 (1.094,1.23) | 1.191 (1.12, 1.26) | 1.15 (1.09, 1.22) | |
| Both (+/+) | 2,645,888 | 10,367 | 13,045,063 | 0.79 | 3.42 (3.30, 3.54) | 3.55 (3.43, 3.68) | 3.02 (2.91, 3.13) | |
| TG criterion | No (–/–) | 6,899,908 | 4699 | 34,438,940 | 0.14 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 1,678,415 | 2332 | 8,385,458 | 0.28 | 1.61 (1.53, 1.69) | 1.64 (1.56, 1.73) | 1.59 (1.51, 1.67) | |
| Pre (+/–) | 1,403,163 | 1911 | 6,991,851 | 0.27 | 1.49 (1.41, 1.57) | 1.52 (1.44, 1.61) | 1.50 (1.42,1.58) | |
| Both (+/+) | 3,329,438 | 9640 | 16,569,844 | 0.58 | 2.88 (2.78, 2.98) | 2.99(2.89, 3.10) | 2.67 (2.57, 2.77) | |
| HDL-C criterion | No (–/–) | 7,854,976 | 4845 | 39,324,738 | 0.12 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 1,620,717 | 3076 | 8,041,271 | 0.38 | 2.53 (2.42, 2.65) | 2.45 (2.34, 2.57) | 2.36 (2.25,2.47) | |
| Pre (+/–) | 1,349,503 | 1817 | 6,723,565 | 0.27 | 1.92 (1.82, 2.02) | 1.86 (1.77,1.97) | 1.84 (1.74, 1.94) | |
| Both (+/+) | 2,485,728 | 8844 | 12,296,520 | 0.72 | 4.31 (4.15, 4.47) | 4.17 (4.02, 4.33) | 3.55 (3.41, 3.68) | |
| Met S | No (–/–) | 8,167,333 | 3930 | 40,896,957 | 0.10 | 1 (ref.) | 1(ref.) | 1 (ref.) |
| Post (–/+) | 1,438,425 | 2210 | 7,147,323 | 0.31 | 2.23 (2.12, 2.36) | 2.68 (2.54, 2.82) | 2.54 (2.40, 2.68) | |
| Pre (+/–) | 1,105,622 | 1568 | 5,502,672 | 0.28 | 1.98 (1.87, 2.10) | 2.32 (2.19, 2.46) | 2.28 (2.15, 2.42) | |
| Both (+/+) | 2,599,544 | 10,874 | 12,839,141 | 0.85 | 5.09 (4.90, 5.28) | 6.69 (6.42, 6.97) | 5.65 (5.42, 5.89) | |
| Obesity | No (–/–) | 8,251,129 | 10,223 | 41,158,447 | 0.25 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Post (–/+) | 753,917 | 1065 | 3,760,971 | 0.28 | 1.13 (1.06, 1.20) | 1.06 (0.99, 1.14) | 1.06 (0.99, 1.14) | |
| Pre (+/–) | 650,083 | 1391 | 3,223,253 | 0.43 | 1.38 (1.31, 1.46) | 1.34 (1.26, 1.42) | 1.32 (1.25, 1.40) | |
| Both (+/+) | 3,655,795 | 5903 | 18,243,423 | 0.32 | 1.20 (1.16, 1.23) | 1.10 (1.04, 1.16) | 1.14 (1.08, 1.20) | |
Model 1, adjusted for No. of MetS components at 1st visit, age and sex; Model 2, Model 1 plus adjusted for smoking, drinking and exercise; Model 3, Model 2 plus adjusted for estimated GFR.
WC waist circumference, BP blood pressure, TG triglyceride, HDL-C high-density lipoprotein cholesterol, MetS metabolic syndrome.
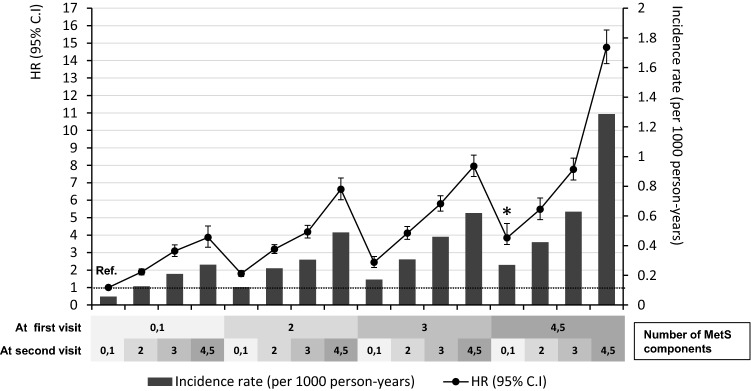
Risk of ESRD according to the change in number of MetS components
Figure 2 shows the risk of incident ESRD according to the change in number of MetS components when compared with subjects with 0–1 MetS components at both exams over two years. As the number of MetS components increase at second visit (index year), the risk of incident ESRD increase regardless of the number of MetS components at first visit. As the number of MetS components decreased from 4–5 to 3, 2, and 0–1 over two years, the HR for incident ESRD decreased sequentially from 14.76 (95% CI, 13.83–15.75) to 7.76 (7.16–8.41), 5.48 (4.90–6.13), and 3.84 (3.17–4.67), respectively. However, it did not show absolute recovery to the same degree of risk observed in individuals with 0–1 MetS components at both visits. Thus, the subject whose the number of MetS components decreased from 4–5 even to 0–1 (expressed with asterisk in Fig. 2), the HR for the risk of incident ESRD remained 3.84 (95% CI, 3.17–4.67) compared with subjects who persistently had 0–1 MetS components over two years (reference).
Figure 2.
Adjusted hazard ratios, 95% confidence intervals, and incidence rates of end-stage renal disease according to changes in the number of metabolic syndrome components as reference with the subjects with 0–1 MetS components at both exams over two years. The model was adjusted for metabolic syndrome components at first visit, age, sex, smoking, alcohol consumption, exercise, and estimated glomerular filtration rate. *The subjects whose the number of MetS components decreased from 4–5 even to 0–1, the HR for the risk of ESRD remained 3.84 (95% CI, 3.17–4.67) compared with subjects who persistently had 0–1 MetS components over two years.
Stratified analysis for risk of ESRD in different renal function subgroups
We conducted subgroup analyses in each group with different renal functions. When we divided subjects into three subgroups (eGFR < 60 mL/min/1.73 m2, 60 mL/min/1.73 m2 < eGFR < 90 mL/min/1.73 m2, and > 90 mL/min/1.73 m2) the risk of ESRD was higher in groups with more advanced renal dysfunction (Supplementary Table S2). That is, individuals meeting all five MetS criteria exhibited an ~ 85-fold increased risk of ESRD in subgroups with an eGFR < 60 mL/min 1.73 m2 compared to those without any MetS criteria. By contrast, in the eGFR 60–90 mL/min/1.73 m2 and eGFR > 90 mL/min 1.73 m2 subgroups, subjects with all five MetS criteria had HRs of 9.30 (95% CI, 7.84–11.03) and 5.01 (3.95–6.36), respectively.
In terms of changes in MetS components, the impact of MetS over two years was stronger in the more advanced renal dysfunction subgroups (Table 4). The HR of individuals in the both-MetS (+/+) group was 2.49 (95% CI, 2.20–2.82) versus the no-MetS (–/–) group in the subgroup of patients with an eGFR > 90 mL/min/1.73 m2. The HRs of subjects in the both-MetS (+/+) group versus the no-MetS (–/–) group were 3.12 (2.88–3.39) and 7.95 (7.50–8.42) in the subgroups with an eGFR of 60–90 mL/min/1.73 m2 and < 60 mL/min/1.73 m2, respectively. In addition, the difference in the risk of ESRD between the both-MetS (+/+) and pre-MetS (+/–) groups was larger in the advanced renal dysfunction subgroups.
Table 4.
Adjusted hazard ratios, 95% confidence intervals, and incidence rates of end-stage renal disease development according to the change of MetS component in different renal function groups.
| eGFR (ml/min 1.73 m2) | Met S | N | Events (n) | Follow-up duration (person-years) | Incidence rate (per 1000 person-years) | Adjusted hazard ratios ( 95% confidence intervals) | ||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||
| ≥ 90 | ||||||||
| No (–/–) | 3,860,370 | 743 | 19,327,628 | 0.04 | 1 (ref.) | 1 (ref.) | 1 (ref.) | |
| Post (–/+) | 569,066 | 238 | 2,827,416 | 0.08 | 1.53 (1.32, 1.77) | 1.70 (1.46, 1.98) | 1.70 (1.46, 1.98) | |
| Pre (+/–) | 443,490 | 165 | 2,207,881 | 0.07 | 1.29 (1.09, 1.53) | 1.42 (1.19, 1.68) | 1.42 (1.19,1.68) | |
| Both (+/+) | 886,095 | 604 | 4,386,917 | 0.14 | 2.10 (1.88, 2.35) | 2.49 (2.20, 2.82) | 2.49 (2.20, 2.82) | |
| 60–90 | ||||||||
| No (–/–) | 4,033,388 | 1287 | 20,186,181 | 0.06 | 1 (ref.) | 1 (ref.) | 1 (ref.) | |
| Post (–/+) | 782,638 | 578 | 3,892,718 | 0.15 | 1.70 (1.54, 1.88) | 1.92 (1.73, 2.12) | 1.88 (1.70, 2.08) | |
| Pre (+/–) | 598,265 | 392 | 2,981,306 | 0.13 | 1.45 (1.29,1.62) | 1.61 (1.43, 1.80) | 1.59 (1.41, 1.78) | |
| Both (+/+) | 1,438,726 | 1935 | 7,125,683 | 0.27 | 2.66 (2.47, 2.86) | 3.21 (2.96, 3.48) | 3.12 (2.88, 3.39) | |
| < 60 | ||||||||
| No (–/–) | 273,575 | 1900 | 1,383,148 | 1.37 | 1 (ref.) | 1 (ref.) | 1 (ref.) | |
| Post (–/+) | 86,721 | 1394 | 427,189 | 3.26 | 2.30 (2.14, 2.46) | 2.85 (2.65, 3.06) | 3.32 (3.09,3.57) | |
| Pre (+/–) | 63,867 | 1011 | 3,134,865 | 3.23 | 2.29 (2.12, 2.47) | 2.75 (2.55, 2.98) | 3.12(2.89, 3.38) | |
| Both (+/+) | 274,723 | 8335 | 1,326,542 | 6.28 | 4.70 (4.45, 4.95) | 6.47 (6.11, 6.85) | 7.95 (7.50, 8.42) | |
Model 1, adjusted for No. of MetS components at 1st visit, age and sex; Model 2, Model 1 plus adjusted for smoking, drinking and exercise; Model 3, Model 2 plus adjusted for estimated GFR.
Discussion
The present study demonstrated the impact of a change in MetS status over 2 years on the incidence of ESRD as well as per se MetS in the nationwide 13.3 million study population, which is about 26% of total 50 million South Koreans. A total of 19.1% of individuals experienced changes in MetS status (i.e. the post-MetS (+/–) and pre-MetS (–/+) groups). Compared with the no-MetS (–/–) group, subjects in the post-MetS (–/+) group had an ~ 2.5-fold increased risk of ESRD at the second visit after a median follow up of 5.11 years from the index year. Of particular interest, the present study included a comparison of the risk between subjects in the pre-MetS (+/–) and both-MetS (+/+) groups. Although the pre-MetS group had a reduced risk of ESRD compared with subjects with the both-MetS (+/+) group, the risk did not decline to the degree observed in subjects with no MetS (–/–). Furthermore, the HR for the development of ESRD remained 2.28 (95% CI, 2.15–2.42). Even when the number of MetS components declined from 2 to 0–1, the HR for ESRD remained 1.80 (1.63–1.97) compared with individuals without MetS components. Thus, an initial metabolic change over 2 years had a distinct impact on renal outcomes for a median follow-up period of 5.11 years. This legacy effect could be associated with the concept of “metabolic memory”, where transient intensive metabolic controls create a “memory” for the improvement of microvascular outcomes20–22. Metabolic controls include the regulation of glucose, BP, and dyslipidaemia, as well as reduced WC21. The findings imply that early successful management of MetS can attenuate renal damage, and suggest that intensive interventions should be initiated as early as possible to prevent ESRD23.
Data published in the last decade have revealed that MetS also affects the risk of CKD progression4,24–28. The current study confirmed that the risk of ESRD increased progressively as the number of MetS components increased from 1 to 5, with HRs that were increased by 2.8-, 4.8-, 8.2-, 14.5-, and 24.8-fold compared with individuals with no-MetS components. Thus, multiple metabolic components had synergistic rather than additive effects of the risk of ESRD. The exact mechanism explaining the link between MetS and kidney disease has not been completely elucidated, although proposed pathophysiological factors include hyperfiltration, insulin resistance, adipokines, endothelial dysfunction, renin–angiotensin–aldosterone-system activation, and oxidative stress1,11.
Another interesting observation was that a change in obesity, defined as a BMI > 25 kg/ m2, exhibited a different pattern from the changes in other MetS criteria. Compared with the no-obesity (–/–) group, subjects in the pre-obesity (+/–) group had a higher risk of developing ESRD than those in the both-obesity (+/+) group. These trends were inconsistent with the change in the WC criterion; the HRs for developing ESRD in the both-WC (+/+) and pre-WC (+/–) groups were 1.95 and 1.53, respectively. Therefore, subjects who reduced their WC over 2 years had a lower risk of ESRD compared with those with sustained central obesity. However, subjects who reduced their BMI to < 25 kg/ m2 over 2 years had a higher risk of ESRD compared with those with a sustained BMI ≥ 25 kg/ m2. These results were consistent with previous studies demonstrating that a lower BMI resulted in poor outcomes in patients with CKD or ESRD26–29. BMI correlates well with adiposity, but it does not reflect the fat distribution pattern and can be affected by muscle mass30. Therefore, the opposing impact of a change in BMI and WC on ESRD could be explained by the poor prognosis of patients with both extreme malnutrition and excessive adiposity, with U-curve or J-curve patterns in CKD patients31–36.
A previous study demonstrated that early intervention in MetS could slow CKD progression in patients with early-stage CKD11, and established the risk of MetS change on renal function in individuals with early-stage CKD. However, in the subgroup analysis according to renal function in the present study, the impact of a change in MetS components on the incidence of ESRD was stronger in more advanced CKD groups. In the subgroup of patients with an eGFR < 60 mL/min/1.73 m2, individuals in the both-MetS (+/+) and pre-MetS (+/–) groups had HRs for ESRD development of 7.95 and 3.12, respectively, compared with the no-MetS (–/–) group. These findings support the hypothesis that the impact of MetS on ESRD differs according to the degree of renal function and that interventions to achieve active control of MetS may result in better renal outcomes, even in subjects with advanced CKD28,37.
Several findings from the present study warrant further consideration. First, the study followed an observational design; therefore, inferences of causality should not be made regarding individual changes in MetS components and declining renal function. Second, the assessment of renal function was limited, and no information on proteinuria was available. Calculating estimated GFR using a serum Cr-based MDRD formula is less accurate for subjects with a higher GFR than for those with a lower GFR. Also, the formula may not be suitable for use outside of American white and black populations. Despite these limitations, this is the first nationally representative, population-based study to evaluate changes in MetS components as risk factors for ESRD, and the results verify the possibility of a potential protective effect of combining individual MetS improvements using either medications or lifestyle modifications to slow the progression of CKD. A future intervention study could help isolate the impact of changes in MetS components as a risk factor for renal outcome. It is noteworthy to emphasise the need to regulate these metabolic risk factors with active interventions, particularly lifestyle modifications, to prevent the development of ESRD.
Supplementary information
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2018R1D1A1B07049079 and 2017R1D1A1B03031133). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. This study was performed using the database from the National Health Insurance System (NHIS-2018-1-259), and the results do not necessarily represent the opinion of the National Health Insurance Corporation.
Author contributions
E.S.K., K.D.H., and H.S.K. conceived and designed the study. K.D.H. performed a statistical analysis and E.S.K. wrote the manuscript. M.K.K., E.S.K., M.K.L., G.E.N., and O.K.H. contributed to discussion. H.S.K. is the guarantor of this work and had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed the manuscript.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2018R1D1A1B07049079; 2017R1D1A1B03031133). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41598-021-81396-0.
References
- 1.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 2.Isomaa B, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 3.Stefansson VTN, et al. Metabolic syndrome but not obesity measures are risk factors for accelerated age-related glomerular filtration rate decline in the general population. Kidney Int. 2018;93:1183–1190. doi: 10.1016/j.kint.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 4.Jin DC, et al. Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res. Clin. Pract. 2018;37:20–29. doi: 10.23876/j.krcp.2018.37.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurata M, Tsuboi A, Takeuchi M, Fukuo K, Kazumi T. Association of metabolic syndrome with chronic kidney disease in elderly Japanese women: comparison by estimation of glomerular filtration rate from creatinine, Cystatin c, and both. Metab. Syndr. Relat. Disord. 2016;14:40–45. doi: 10.1089/met.2015.0085. [DOI] [PubMed] [Google Scholar]
- 6.Cai Q, et al. Metabolic syndrome does not always play a critical role in decreased GFR. Ren. Fail. 2016;38:383–389. doi: 10.3109/0886022X.2015.1136873. [DOI] [PubMed] [Google Scholar]
- 7.Cheong KC, et al. The discriminative ability of waist circumference, body mass index and waist-to-hip ratio in identifying metabolic syndrome: Variations by age, sex and race. Diabetes Metab. Syndr. 2015;9:74–78. doi: 10.1016/j.dsx.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DW, et al. Metabolic syndrome in severe chronic kidney disease: prevalence, predictors, prognostic significance and effects of risk factor modification. Nephrology (Carlton). 2007;12:391–398. doi: 10.1111/j.1440-1797.2007.00804.x. [DOI] [PubMed] [Google Scholar]
- 9.Ryu S, et al. Time-dependent association between metabolic syndrome and risk of CKD in Korean men without hypertension or diabetes. Am. J. Kidney Dis. 2009;53:59–69. doi: 10.1053/j.ajkd.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Lin JH, et al. Association between management of metabolic syndrome and progression of early-stage chronic kidney disease: an observational cohort study. Ren. Fail. 2015;37:29–36. doi: 10.3109/0886022X.2014.964140. [DOI] [PubMed] [Google Scholar]
- 11.Lee SJ, et al. Metabolic syndrome status over 2 years predicts incident chronic kidney disease in mid-life adults: a 10-year prospective cohort study. Sci. Rep. 2018;8:12237. doi: 10.1038/s41598-018-29958-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh ES, et al. Intra-individual variability in high density lipoprotein cholesterol and risk of end-stage renal disease: a nationwide population-based study. Atherosclerosis. 2019;286:135–141. doi: 10.1016/j.atherosclerosis.2019.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Lamb EJ, Tomson CR, Roderick PJ. Estimating kidney function in adults using formulae. Ann. Clin. Biochem. 2005;42:321–345. doi: 10.1258/0004563054889936. [DOI] [PubMed] [Google Scholar]
- 14.Ko SH, et al. Past and current status of adult type 2 diabetes mellitus management in Korea: a national health insurance service database analysis. Diabetes Metab J. 2018;42:93–100. doi: 10.4093/dmj.2018.42.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grundy SM, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 16.Levey AS, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 17.Kim MK, et al. Weight change and mortality and cardiovascular outcomes in patients with new-onset diabetes mellitus: a nationwide cohort study. Cardiovasc. Diabetol. 2019;18:36. doi: 10.1186/s12933-019-0838-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim MK, et al. Variability in total cholesterol is associated with the risk of end-stage renal disease: a nationwide population-based study. Arteriosclero. Thromb. Vasc. Biol. 2017;37:1963–1970. doi: 10.1161/ATVBAHA.117.309803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tonna S, El-Osta A, Cooper ME, Tikellis C. Metabolic memory and diabetic nephropathy: potential role for epigenetic mechanisms. Nat. Rev. Nephrol. 2010;6:332–341. doi: 10.1038/nrneph.2010.55. [DOI] [PubMed] [Google Scholar]
- 20.Ceriello A, Ihnat MA, Thorpe JE. Clinical review 2: the "metabolic memory": is more than just tight glucose control necessary to prevent diabetic complications? J. Clin. Endocrinol. Metab. 2009;94:410–415. doi: 10.1210/jc.2008-1824. [DOI] [PubMed] [Google Scholar]
- 21.Testa R, et al. The "metabolic memory" theory and the early treatment of hyperglycemia in prevention of diabetic complications. Nutrients. 2017;9:437. doi: 10.3390/nu9050437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ihnat MA, Thorpe JE, Ceriello A. Hypothesis: the 'metabolic memory', the new challenge of diabetes. Diabet. Med. 2007;24:582–586. doi: 10.1111/j.1464-5491.2007.02138.x. [DOI] [PubMed] [Google Scholar]
- 23.Saito T, Mochizuki T, Uchida K, Tsuchiya K, Nitta K. Metabolic syndrome and risk of progression of chronic kidney disease: a single-center cohort study in Japan. Heart Vessels. 2013;28:323–329. doi: 10.1007/s00380-012-0254-5. [DOI] [PubMed] [Google Scholar]
- 24.Martins D, Ani C, Pan D, Ogunyemi O, Norris K. Renal dysfunction, metabolic syndrome and cardiovascular disease mortality. J. Nutr. Metab. 2010;2010:167162. doi: 10.1155/2010/167162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song YM, Sung J, Lee K. Longitudinal relationships of metabolic syndrome and obesity with kidney function: Healthy Twin Study. Clin. Exp. Nephrol. 2015;19:887–894. doi: 10.1007/s10157-015-1083-5. [DOI] [PubMed] [Google Scholar]
- 26.Sun F, Tao Q, Zhan S. Metabolic syndrome and the development of chronic kidney disease among 118 924 non-diabetic Taiwanese in a retrospective cohort. Nephrology (Carlton) 2010;15:84–92. doi: 10.1111/j.1440-1797.2009.01150.x. [DOI] [PubMed] [Google Scholar]
- 27.Thomas G, et al. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin. J. Am. Soc. Nephrol. 2011;6:2364–73. doi: 10.2215/CJN.02180311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang T, et al. Impact of metabolic syndrome on the incidence of chronic kidney disease: a Chinese cohort study. Nephrology (Carlton). 2012;17:532–538. doi: 10.1111/j.1440-1797.2012.01607.x. [DOI] [PubMed] [Google Scholar]
- 29.Chang TI, et al. Association of body weight changes with mortality in incident hemodialysis patients. Nephrol. Dial. Transpl. 2017;32:1549–1558. doi: 10.1093/ndt/gfx289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalantar-Zadeh K, et al. The obesity paradox in kidney disease: how to reconcile it with obesity management. Kidney Int. Rep. 2017;2:271–281. doi: 10.1016/j.ekir.2017.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Su CT, et al. Changes in anthropometry and mortality in maintenance hemodialysis patients in the HEMO Study. Am. J. Kidney Dis. 2013;62:1141–1150. doi: 10.1053/j.ajkd.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 32.Ryu S, et al. Changes in body weight predict CKD in healthy men. J. Am. Soc. Nephrol. 2008;19:1798–1805. doi: 10.1681/ASN.2007121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oh H, et al. Waist circumference, not body mass index, is associated with renal function decline in korean population: hallym aging study. PLoS ONE. 2013;8:e59071. doi: 10.1371/journal.pone.0059071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lodebo BT, Shah A, Kopple JD. Is it important to prevent and treat protein-energy wasting in chronic kidney disease and chronic dialysis patients? J. Ren. Nutr. 2018;28:369–379. doi: 10.1053/j.jrn.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Vashistha T, et al. Effect of age and dialysis vintage on obesity paradox in long-term hemodialysis patients. Am. J. Kidney Dis. 2014;63:612–622. doi: 10.1053/j.ajkd.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoogeveen EK, et al. Obesity and mortality risk among younger dialysis patients. Clin. J. Am. Soc. Nephrol. 2012;7:280–288. doi: 10.2215/CJN.05700611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zammit AR, Katz MJ, Derby C, Bitzer M, Lipton RB. Metabolic syndrome and smoking are associated with future development of advanced chronic kidney disease in older adults. Cardiorenal. Med. 2016;6:108–115. doi: 10.1159/000441624. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.