Summary
Background
Many causes of vision impairment can be prevented or treated. With an ageing global population, the demands for eye health services are increasing. We estimated the prevalence and relative contribution of avoidable causes of blindness and vision impairment globally from 1990 to 2020. We aimed to compare the results with the World Health Assembly Global Action Plan (WHA GAP) target of a 25% global reduction from 2010 to 2019 in avoidable vision impairment, defined as cataract and undercorrected refractive error.
Methods
We did a systematic review and meta-analysis of population-based surveys of eye disease from January, 1980, to October, 2018. We fitted hierarchical models to estimate prevalence (with 95% uncertainty intervals [UIs]) of moderate and severe vision impairment (MSVI; presenting visual acuity from <6/18 to 3/60) and blindness (<3/60 or less than 10° visual field around central fixation) by cause, age, region, and year. Because of data sparsity at younger ages, our analysis focused on adults aged 50 years and older.
Findings
Global crude prevalence of avoidable vision impairment and blindness in adults aged 50 years and older did not change between 2010 and 2019 (percentage change −0·2% [95% UI −1·5 to 1·0]; 2019 prevalence 9·58 cases per 1000 people [95% IU 8·51 to 10·8], 2010 prevalence 96·0 cases per 1000 people [86·0 to 107·0]). Age-standardised prevalence of avoidable blindness decreased by −15·4% [–16·8 to −14·3], while avoidable MSVI showed no change (0·5% [–0·8 to 1·6]). However, the number of cases increased for both avoidable blindness (10·8% [8·9 to 12·4]) and MSVI (31·5% [30·0 to 33·1]). The leading global causes of blindness in those aged 50 years and older in 2020 were cataract (15·2 million cases [9% IU 12·7–18·0]), followed by glaucoma (3·6 million cases [2·8–4·4]), undercorrected refractive error (2·3 million cases [1·8–2·8]), age-related macular degeneration (1·8 million cases [1·3–2·4]), and diabetic retinopathy (0·86 million cases [0·59–1·23]). Leading causes of MSVI were undercorrected refractive error (86·1 million cases [74·2–101·0]) and cataract (78·8 million cases [67·2–91·4]).
Interpretation
Results suggest eye care services contributed to the observed reduction of age-standardised rates of avoidable blindness but not of MSVI, and that the target in an ageing global population was not reached.
Funding
Brien Holden Vision Institute, Fondation Théa, The Fred Hollows Foundation, Bill & Melinda Gates Foundation, Lions Clubs International Foundation, Sightsavers International, and University of Heidelberg.
Introduction
With rising sociodemographic status and life expectancy, many countries around the world are seeing more people live into adulthood, increases in the average age of the population, and a shift in the disease burden towards non-communicable diseases and disabilities. Most of the principal causes of vision impairment, including cataract and undercorrected refractive error,1 are subject to this epidemiological transition2 and carry significant individual and societal costs.3, 4 Cataract surgery and the dispensing of spectacles are among the most cost-effective health-care interventions currently available.5, 6, 7 Addressing these reversible conditions by scaling up existing health-care systems to provide access to cataract surgery and spectacles is an important opportunity. To highlight this need, the WHO and the International Agency for Prevention of Blindness created an initiative in 1999 called “Vision 2020: The Right to Sight”. In 2013, the World Health Asssembly (WHA) launched a new plan, Towards universal eye health: a global action plan 2014–2019 (GAP).8 It set a global target: to achieve by 2019 a 25% reduction from the baseline of 2010 in prevalence of “avoidable”8 visual impairment, defined as the aggregated crude prevalence of cataract and undercorrected refractive error (presenting visual acuity <6/18).
Previously, the Vision Loss Expert Group (VLEG) reported the results of a systematic review of population-based studies that reported the prevalence of blindness and vision impairment dating from 1980. These studies were compiled in a continuously updated database called the Global Vision Database.1, 9 WHO used these estimates as the basis for their 2019 world report on vision, which focused on people-centred eye care as a means for health system strengthening,10 and cause-specific data by region for 2015 were made available online.
Research in context.
Evidence before this study
The growing and ageing of populations have led to increasing numbers of individuals with moderate or worse vision impairment globally. These trends triggered WHO and the International Agency for the Prevention of Blindness to create an initiative in 1999 called “Vision 2020: The Right to Sight”. This initiative set a goal to eliminate avoidable blindness. Previous publications by the Vision Loss Expert Group, and by the Global Burden of Diseases, Injuries, and Risk Factors Study demonstrated that, in 2015, cataract and undercorrected refractive error were responsible for the majority of moderate or worse vision impairment, and case numbers continued to rise over time.
Added value of this study
This study updates global and regional estimates of causes of moderate and severe vision impairment and blindness through 2020. We examined age-adjusted and sex-adjusted differences in the contribution of these causes to vision impairment, with a focus on older age groups. We incorporated studies from an updated systematic review for a total of 376 cause-specific sources. Rapid Assessment of Avoidable Blindness studies—key sources of vision loss data from low-income and middle-income settings—were disaggregated from prevalence for ages 50–99 years into 5-year age groups, providing more accurate data on age patterns. This update also allowed us to assess the World Health Assembly 2013 Global Action Plan (WHA GAP) target to reduce avoidable vision impairment, which was specifically defined as a reduction in moderate or worse vision impairment from undercorrected refractive error and cataract by 25% between 2010 and 2019.
Implications of all the available evidence
We found that in adults aged 50 years and older there was no change in the crude prevalence of avoidable vision impairment between 2010 and 2019, and case numbers increased. Cataract remained the largest contributor to global blindness in adults aged 50 years and older in 2020, with over 15 million individuals, approximately 45% of the 33·6 million cases of global blindness. Undercorrected refractive error remains the largest contributor to global moderate and severe vision impairment (MSVI) in adults aged 50 years and older, with over 86 million individuals, approximately 42% of the 206 million cases of global MSVI. Although less easily treatable, glaucoma, diabetic retinopathy, and age-related macular degeneration collectively led to more than 19 million cases of moderate or worse vision impairment in adults aged 50 years and older in 2020, making these diseases important targets for prevention and treatment. Age-standardised prevalence was higher in women than in men for all modelled causes of moderate or worse vision impairment, with the exception of glaucoma for which age-standardised prevalence was higher in men. Although the number of affected individuals increased for blindness due to all modelled causes, age-standardised prevalence for all modelled causes of vision except diabetic retinopathy has decreased over the past three decades. This suggests that eye care services did successfully reduce age-standardised prevalence, but they did not meet the growing need due to ageing and growth of the populations.
Since then, the VLEG has conducted a major update of the Global Vision Database in collaboration with researchers from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD study). Updated estimates are of particular interest because of recent rapid socioeconomic development, for example in China and south Asia. Additionally, the progressive emergence of causes of vision impairment such as myopic macular degeneration (particularly in China11, 12) and diabetic retinopathy as significant contributors to the vision impairment burden warrants a global update. With ageing populations, it was anticipated that two other conditions, glaucoma13 and age-related macular degeneration,14 would continue to be major causes of vision impairment. We now have more detailed and representative data sources from surveys of eye disease, bolstering our ability to track changes over time in cataract, undercorrected refractive error, macular degeneration, diabetic retinopathy, and glaucoma.
We report global and regional estimates of the burden of moderate and severe vision impairment (MSVI) and blindness due to cataract, undercorrected refractive error, glaucoma, age-related macular degeneration, and diabetic retinopathy. We examined temporal, sex, and age trends, with a focus on older age groups. We also assessed progress against the WHA GAP target of 25% reduction in avoidable vision impairment between 2010 and 2019.
Methods
Estimates described here were produced in compliance with the Guidelines for Accurate and Transparent Health Estimates Reporting.15
Input data
Preparation of data included first a systematic review of published population-based studies of vision impairment and blindness by the VLEG, that also included grey literature sources. Eligible studies from this review were then combined with data from Rapid Assessment of Avoidable Blindness (RAAB) studies by VLEG and finally data from the US National Health and Nutrition Examination survey and the WHO Study on Global Ageing and Adult Health were contributed by the GBD team. These stages are explained in more detail as follows. We included population-representative studies as data sources for cause-specific vision impairment modelling, primarily national and subnational cross-sectional surveys. RAAB surveys, which sample individuals aged 50 years and older, were major sources of data for low-income and middle-income settings.
The VLEG has systematically reviewed scientific literature published between 1980 and 2018 by commissioning the York Health Economics Consortium, UK, to search Embase, SciELO, MEDLINE, WHOLIS, and Open Grey, and additional grey literature sources. After title and abstract screening, abstracts were sent to regional committees of VLEG members to assess quality and make final inclusion decisions on whether to admit data to VLEG's Global Vision Database. Additionally, the VLEG commissioned the preparation of 5-year age-disaggregated RAAB data from the RAAB repository.
To meet inclusion criteria, visual acuity data had to be measured using a vision chart that could be mapped to the Snellen scale; studies based on self-report of vision impairment were excluded. We included studies that measured either presenting vision impairment (where visual acuity was measured using the usual corrective lenses a person arrived wearing), or best-corrected vision impairment (where a pinhole or lenses with power based on refraction were used to address any refractive error), or both. We applied WHO criteria for vision impairment severity, categorising people according to vision in the better-seeing eye on presentation. The categories were moderate vision impairment (defined as visual acuity of ≥6/60 and <6/18), severe vision impairment (visual acuity of ≥3/60 and <6/60), and blindness (visual acuity of <3/60 or <10° visual field around central fixation, although the visual field definition is rarely utilised in population-based eye surveys). We report a composite term of MSVI that comprises people meeting either moderate or severe visual acuity definitions. We also report a composite term of moderate or worse vision impairment that comprises people meeting moderate, severe, or blind visual acuity definitions.
Data preparation
The separation of raw data into datasets, including total all-cause moderate vision impairment, severe vision impairment, and blindness, has been explained in detail elsewhere, in addition to a full list of the data sources.16 Cause-specific analyses are described below.
Presenting vision impairment was the reference definition for each level of severity. Undercorrected refractive error data were extracted directly from data sources where available, and otherwise calculated by subtracting best-corrected vision impairment from presenting vision impairment prevalence for each level of severity in studies that reported both measures for a given location, sex, age group, and year. All other causes were quantified as part of the best-corrected estimates of vision impairment at each level of severity.
We modelled distance vision impairment and blindness due to the following causes: cataract, undercorrected refractive error, age-related macular degeneration, myopic macular degeneration, glaucoma, diabetic retinopathy, and other causes of vision impairment (in aggregate). Minimum age for inclusion of data for these causes was set at 20 years for cataract and diabetic retinopathy; and 45 years for glaucoma and age-related macular degeneration. Other vision impairment estimates were combined with less prevalent causes of vision impairment to create a residual category (eg, retinopathy of prematurity, vitamin A deficiency, trachoma). Trachoma data were extracted as a proportion, in which the numerator was total cases of trachoma, and the denominator was total cases of vision impairment at a given severity level. Geographic restrictions were applied so that zero prevalence was imputed for non-endemic locations.
Data collected using RAAB methodology were adjusted to comprehensive surveys (reference definition) using the same adjustment factors as for all-cause MSVI and blindness (described in a sister paper on all-cause vision loss).16 This approach was used because there were many more data available for all-cause moderate vision impairment, severe vision impairment, and blindness than for each specific cause, allowing for more data-rich models.
Disease modelling meta-regression 2.1 modelling
We produced location, year, age, and sex-specific estimates of MSVI and blindness using Disease Modelling Meta-Regression (Dismod-MR) 2.1, which is described in detail elsewhere.16, 17, 18 Global estimates are first produced with a mixed effects non-linear model using all available data to produce a global model fit as well as fixed and random effects. These outputs are passed to the GBD super-region level (seven super-regions) as a prior, and super-region fits are generated using super-region input data and the global prior. The super-region outputs are passed to the region level (21 regions), then to the country level, and finally the subnational level for 21 countries. Final estimates were generated by aggregation, for which the region final was the sum of country estimates, etc. To location aggregate (eg, super-regions or global estimates), we aggregated the most granular estimates using straightforward summation of cases, which were then used to compute all-age and age-standardised rates. For location estimates, we used draw-level regional estimates of regional case numbers (“draws” from the 1000 posterior runs of the model) and summed these to obtain super-region and global case numbers. We then summarised the draw level estimates by taking the mean across values. No weighting was used in the global or regional aggregations. For avoidable vision loss we took draw-level regional estimates of case numbers for uncorrected refractive error and cataract and summed these together.
During data processing, we applied data adjustments if we knew there were potential measurement errors using a meta-regression tool developed at Institute for Health Metrics and Evaluation (IHME) called MR-BRT.17 For example, our reference definition for all-cause vision loss was presenting visual acuity systematically on the basis of the results of a regression analysis comparing the prevalence of the two methods. We similarly adjusted for studies that used RAAB methodology or non-standard severity definitions. Our estimation tool (Dismod) made quantification of between-study heterogeneity—the part of variance not ascribed to fixed effects or geographical random effects–and added uncertainty based on that finding.
Modelling and post-processing steps
Dismod-MR 2.1 models were run for all vision impairment by severity (moderate, severe, blindness) regardless of cause and, separately, for MSVI and blindness due to each modelled cause of vision impairment (eg, MSVI due to cataract and blindness due to cataract). Then, models of MSVI due to specific causes were split into moderate and severe estimates using the ratio of overall prevalence in the all-cause moderate presenting vision impairment and severe presenting vision impairment models. Next, prevalence estimates for all causes by severity were scaled to the models of all-cause prevalence by severity. This produced final estimates by age, sex, year, and location for each individual cause of vision impairment by severity. Models were iterated until reaching convergence, and estimates were calculated with the final 1000 model runs, or draws. These draws were used to produce mean estimates and 95% uncertainty intervals (UIs), bounded by the 25th and 975th values of the ordered 1000 draws.
To assess whether targets of the WHA GAP were reached in the 2010–19 period, we aggregated estimates for cataract and undercorrected refractive error to create the “avoidable vision impairment” category used as a metric for assessing whether the GAP target was met.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had access to all estimates presented in the paper, and the corresponding author had final responsibility for the decision to submit for publication.
Results
We used 512 data sources to calculate the prevalence of categories of distance vision impairment. 376 data sources reported cause-specific data disaggregated to include at least one of the following: undercorrected refractive error, cataract, glaucoma, age-related macular degeneration, myopic macular degeneration, or diabetic retinopathy (appendix p 7). 230 (61%) of these 376 data sources were RAABs.16 Many studies incorporated in the 2017 update1 have since submitted more granular levels of disaggregated data, enabling more precise estimates of the causes of global vision impairment in 2020 and their temporal changes. Data sources for blindness and MSVI caused by myopic macular degeneration were sparse globally with the majority of sources from China. For this reason, we reported estimates of myopic macular degeneration solely for China. Globally, data for children and young adults were also sparse, as were data for high-income locations. Because of the data sparsity at younger ages, we focused our analyses on adults aged 50 years and older.
To assess the success of the WHA GAP to reduce avoidable vision impairment, we calculated the change in avoidable vision impairment over the past decade. Crude prevalence of all moderate or worse avoidable vision impairment between 2010 and 2019 in adults aged 50 years and older did not change (percentage change of −0·2% [95% UI −1·5 to 1·0]); 2019 prevalence 95·8 cases per 1000 people [85·1 to 108·0], 2010 prevalence 96·0 cases per 1000 people [86·0 to 107·]), but it increased in all ages by 9·1% (7·6 to 10·7). Total cases of moderate or worse avoidable vision impairment increased in people aged 50 years and older by 29·2% (27·6 to 30·9) and in all ages by 20·8% (19·2 to 22·6) for a composite 211 million cases of moderate or worse vision impairment in 2010 to 254 million cases in 2019. Crude prevalence by cause and severity in 2020 is given in the appendix (pp 4–5).
Underlying the overall lack of change in crude prevalence of all moderate or worse avoidable vision impairment in people aged 50 years and older, avoidable MSVI showed little change between 2010 and 2019, with an increase of 1·6% (0·4 to 2·8), whereas avoidable blindness decreased by −14·4% (–15·9 to −13·2; table 1). Similarly, age-standardised prevalence of avoidable MSVI showed no change (0·5% [–0·8 to 1·6]), but blindness decreased (–15·4% [–16·8 to −14·3]). By contrast, the number of cases increased markedly for both avoidable MSVI (31·5% [30·0 to 33·1]) and avoidable blindness (10·8% [8·9 to 12·4]).
Table 1.
Percentage change in crude prevalence of moderate and severe vision impairment and blindness in adults aged 50 years and older between 2010 and 2019
|
Moderate and severe vision impairment |
Blindness |
|||||
|---|---|---|---|---|---|---|
| Crude prevalence | Number of cases | Age-standardised prevalence | Crude prevalence | Number of cases | Age-standardised prevalence | |
| All causes | 1·9% (0·8 to 3·1) | 32·0% (30·5 to 33·5) | 0·7% (−0·5 to 1·8) | −10·0% (−11·2 to −9·1) | 16·5% (15·0 to 17·8) | −11·4% (−12·3 to −10·6) |
| Avoidable* (cataract+ undercorrected refractive error) | 1·6% (0·4 to 2·8) | 31·5% (30·0 to 33·1) | 0·5% (−0·8 to 1·6) | −14·4% (−15·9 to −13·2) | 10·8% (8·9 to 12·4) | −15·4% (−16·8 to −14·3) |
| Cataract | 2·9% (1·5 to 4·2) | 33·2% (31·4 to 34·9) | 1·1% (−0·3 to 2·3) | −14·0% (−15·5 to −12·7) | 11·4% (9·5 to 13·1) | −15·1% (−16·4 to −13·9) |
| Undercorrected refractive error | 0·4% (−1·1 to 1·9) | 30·0% (28·1 to 31·9) | −0·1% (−1·5 to 1·3) | −17·5% (−19·2 to −15·7) | 6·9% (4·6 to 9·1) | −17·8% (−19·5 to −16·3) |
| Glaucoma | 10·7% (9·2 to 12·3) | 43·4% (41·4 to 45·5) | 8·0% (6·5 to 9·5) | −8·3% (−9·8 to −7·0) | 18·7% (16·9 to 20·4) | −10·8% (−11·9 to −9·9) |
| Age-related macular degeneration | 7·1% (5·2 to 9·0) | 38·7% (36·2 to 41·2) | 5·0% (3·2 to 6·7) | −9·1% (−11·4 to −7·0) | 17·7% (14·8 to 20·4) | −11·7% (−13·8 to −9·8) |
| Diabetic retinopathy | 0·8% (−0·9 to 2·6) | 30·6% (28·3 to 32·8) | −0·4% (−2·1 to 1·2) | −6·0% (−8·4 to −3·5) | 21·8% (18·7 to 25·0) | −6·6% (−9·0 to −4·1) |
| Residual causes of vision loss | 1·8% (0·7 to 3·1) | 31·9% (30·4 to 33·5) | 0·0% (−0·9 to 1·1) | −2·4% (−4·1 to −0·8) | 26·4% (24·2 to 28·5) | −3·7% (−5·2 to −2·3) |
Data in parentheses are 95% uncertainty intervals. Data for all ages are given in the appendix (p 6). Data presented in this table were calculated to assess the success of the World Health Assembly's global action plan to reduce avoidable vision impairment.
Classified as “avoidable” in the global action plan.
We then looked at the contribution of individual causes to global visual impairment in 2020. Among the global 33·6 million adults aged 50 years and older who were blind in 202016 the leading causes of blindness (table 2) were cataract (15·2 million cases [95% UI 12·7–18·0]), followed by glaucoma (3·6 million cases [2·8–4·4]), undercorrected refractive error (2·3 million cases [1·8–2·8]), age-related macular degeneration (1·8 million cases [1·3–2·4]), and diabetic retinopathy (0·9 million cases [0·6–1·2]). For the estimated 206 million aged 50 years and older adults with MSVI in 2020,16 the leading causes of MSVI (table 3) were undercorrected refractive error (86·1 million cases [74·2–101·0]), followed by cataract (78·8 million cases [67·2–91·4]), age-related macular degeneration (6·2 million cases [5·0–7·6]), glaucoma (4·1 million cases [3·2–5·2]), and diabetic retinopathy (2·9 million cases [2·1–3·9]).
Table 2.
Cases and age-standardised prevalence in 2020 for blindness and percentage changes from 1990 to 2020 in adults aged 50 years and older, by cause of blindness
|
Cases (thousands) |
Age-standardised prevalence (per 1000) |
|||
|---|---|---|---|---|
| 2020 | Percentage change from 1990 to 2020 | 2020 | Percentage change from 1990 to 2020 | |
| Cataract | ||||
| Global | 15 200 (12700 to 18000) | 55·7% (51·4 to 59·9) | 8·38 (7·04 to 9·93) | −31·7% (−33·2 to −30·1) |
| Central Europe, eastern Europe, and central Asia | 266 (211 to 332) | −4·3% (−7·3 to −1·4) | 1·88 (1·50 to 2·33) | −36·1% (−37·5 to −34·6) |
| High income | 456 (367 to 566) | 56·0% (48·2 to 64·6) | 0·877 (0·702 to 1·08) | −22·6% (−24·2 to −21·3) |
| Latin America and Caribbean | 1010 (826 to 1210) | 78·4% (73·2 to 83·7) | 7·85 (6·42 to 9·48) | −43·8% (−44·7 to −42·7) |
| North Africa and Middle East | 756 (593 to 941) | 30·0% (24·9 to 35·4) | 9·06 (7·13 to 11·4) | −53·7% (−55·3 to −52·0) |
| South Asia | 5910 (4990 to 6970) | 51·1% (44·7 to 57·6) | 22·3 (18·9 to 26·1) | −46·4% (−48·1 to −44·5) |
| Southeast Asia, east Asia, and Oceania | 5540 (4620 to 6590) | 67·2% (62·5 to 72·5) | 9·72 (8·14 to 11·5) | −43·8% (−45·6 to −41·6) |
| Sub-Saharan Africa | 1240 (1030 to 1490) | 54·4% (51·3 to 57·7) | 14·9 (12·4 to 17·8) | −30·5% (−31·7 to −29·2) |
| Undercorrected refractive error | ||||
| Global | 2290 (1790 to 2800) | 54·4% (48·7 to 60·6) | 1·22 (0·960 to 1·50) | −28·7% (−31·1 to −26·0) |
| Central Europe, eastern Europe, and central Asia | 16·8 (12·8 to 21·1) | 9·0% (5·7 to 12·0) | 0·121 (0·0912 to 0·150) | −17·0% (−19·2 to −14·6) |
| High income | 46·1 (35·7 to 56·9) | 35·1% (29·9 to 40·5) | 0·103 (0·079 to 0·128) | −23·1% (−24·8 to −21·4) |
| Latin America and Caribbean | 126 (97·5 to 153) | 97·3% (91·3 to 103·0) | 0·943 (0·731 to 1·14) | −31·2% (−32·9 to −29·6) |
| North Africa and Middle East | 84·2 (63·8 to 103) | 68·3% (61·5 to 74·7) | 0·875 (0·673 to 1·07) | −36·1% (−38·5 to −33·9) |
| South Asia | 976 (762 to 1190) | 25·8% (19·9 to 32·0) | 3·30 (2·59 to 4·00) | −52·3% (−54·0 to −50·5) |
| Southeast Asia, east Asia, and Oceania | 933 (728 to 1140) | 91·5% (82·8 to 101·5) | 1·47 (1·16 to 1·79) | −27·9% (−31·0 to −24·3) |
| Sub-Saharan Africa | 111 (84·5 to 136) | 91·4% (85·3 to 98·0) | 1·14 (0·881 to 1·41) | −15·0% (−17·2 to −12·8) |
| Glaucoma | ||||
| Global | 3600 (2800 to 4410) | 61·8% (57·2 to 66·8) | 2·04 (1·59 to 2·49) | −31·9% (−33·0 to −30·6) |
| Central Europe, eastern Europe, and central Asia | 178 (139 to 219) | 5·5% (1·9 to 9·3) | 1·25 (0·972 to 1·53) | −31·4% (−32·8 to −30·0) |
| High income | 785 (622 to 964) | 60·3% (53·0 to 69·0) | 1·41 (1·12 to 1·74) | −23·2% (−24·5 to −21·9) |
| Latin America and Caribbean | 334 (256 to 411) | 105·5% (98·4 to 113·6) | 2·63 (2·01 to 3·23) | −36·2% (−37·6 to −34·8) |
| North Africa and Middle East | 463 (354 to 578) | 64·8% (57·6 to 72·3) | 5·69 (4·37 to 7·10) | −40·9% (−43·0 to −39) |
| South Asia | 577 (439 to 726) | 75·7% (65·1 to 86·7) | 2·26 (1·71 to 2·83) | −38·7% (−41·0 to −36·1) |
| Southeast Asia, east Asia, and Oceania | 754 (575 to 957) | 52·4% (44·5 to 61·3) | 1·34 (1·02 to 1·67) | −48·6% (−51·3 to −45·6) |
| Sub-Saharan Africa | 510 (398 to 628) | 70·1% (65·1 to 75·2) | 6·64 (5·20 to 8·09) | −23·5% (−25·5 to −21·5) |
| Age-related macular degeneration | ||||
| Global | 1840 (1340 to 2420) | 69·8% (64·4 to 75·3) | 1·03 (0·755 to 1·36) | −28·0% (−30·0 to −25·6) |
| Central Europe, eastern Europe, and central Asia | 62·5 (43·2 to 84·0) | 21·8% (17·2 to 27·5) | 0·437 (0·305 to 0·587) | −16·8% (−18·5 to −14·9) |
| High income | 595 (455 to 768) | 48·3% (40·8 to 56·3) | 1·08 (0·828 to 1·39) | −28·6% (−30·0 to −27·3) |
| Latin America and Caribbean | 71·1 (49·1 to 97·1) | 142·1% (131·5 to 152·5) | 0·550 (0·379 to 0·747) | −21·2% (−23·3 to −18·8) |
| North Africa and Middle East | 194 (136 to 264) | 105·1% (95·0 to 115·8) | 2·23 (1·55 to 2·99) | −23·3% (−26·5 to −20·1) |
| South Asia | 296 (199 to 421) | 53·4% (42·4 to 65·4) | 1·05 (0·717 to 1·47) | −41·0% (−44·1 to −37·5) |
| Southeast Asia, east Asia, and Oceania | 492 (340 to 673) | 104·0% (91·8 to 116·5) | 0·835 (0·578 to 1·14) | −27·3% (−31·3 to −22·9) |
| Sub-Saharan Africa | 130 (91·4 to 178) | 78·5% (70·2 to 86·5) | 1·50 (1·05 to 2·04) | −19·1% (−23·0 to −15·7) |
| Diabetic retinopathy | ||||
| Global | 861 (592 to 1230) | 150·9% (143·3 to 159·0) | 0·459 (0·316 to 0·658) | 14·9% (11·4 to 18·4) |
| Central Europe, eastern Europe, and central Asia | 11·9 (7·96 to 17·3) | 26·6% (17·8 to 36·4) | 0·0842 (0·0565 to 0·121) | −6·1% (−11·8 to −0·2) |
| High income | 139 (97·2 to 196) | 53·2% (44·2 to 62·2) | 0·307 (0·215 to 0·433) | −13·7% (−17·6 to −9·7) |
| Latin America and Caribbean | 203 (142 to 283) | 130·7% (121·7 to 140·5) | 1·50 (1·05 to 2·09) | −17·9% (−20·5 to −15·2) |
| North Africa and Middle East | 61·0 (40·1 to 91·8) | 169·3% (149·2 to 193·1) | 0·621 (0·413 to 0·928) | 0·9% (−6·2 to 9·3) |
| South Asia | 152 (101 to 225) | 190·7% (162·6 to 222·9) | 0·487 (0·330 to 0·708) | 17·9% (7·8 to 30·1) |
| Southeast Asia, east Asia, and Oceania | 261 (171 to 387) | 286·7% (257·9 to 316·2) | 0·406 (0·269 to 0·602) | 44·5% (33·1 to 56·3) |
| Sub-Saharan Africa | 33·9 (23·0 to 49·2) | 177·4% (162·4 to 192·3) | 0·341 (0·234 to 0·498) | 25·7% (19·4 to 32·3) |
| Residual causes of vision loss | ||||
| Global | 9840 (8200 to 11500) | 69·3% (62·0 to 76·5) | 5·33 (4·46 to 6·24) | −24·2% (−27·3 to −21·3) |
| Central Europe, eastern Europe, and central Asia | 647 (545 to 754) | 11·7% (8·7 to 14·9) | 4·63 (3·92 to 5·38) | −22·5% (−23·9 to −21·1) |
| High-income | 551 (461 to 650) | 48·5% (43·1 to 54·9) | 1·22 (1·03 to 1·44) | −16·5% (−18·5 to −14·4) |
| Latin America and Caribbean | 1140 (940 to 1350) | 125·2% (117·5 to 133·1) | 8·69 (7·16 to 10·3) | −25·8% (−27·6 to −24·1) |
| North Africa and Middle East | 788 (631 to 959) | 73·7% (65·1 to 82·5) | 8·48 (6·79 to 10·4) | −35·6% (−38·8 to −32·8) |
| South Asia | 1670 (1370 to 2010) | 23·4% (12·1 to 36·5) | 5·93 (4·84 to 7·10) | −54·2% (−58·5 to −49·7) |
| Southeast Asia, east Asia, and Oceania | 3850 (3230 to 4500) | 117·0% (108·1 to 125·6) | 6·35 (5·33 to 7·40) | −23·0% (−26·2 to −19·8) |
| Sub-Saharan Africa | 1200 (973 to 1440) | 54·7% (49·4 to 60·0) | 12·9 (10·4 to 15·3) | −30·0% (−32·1 to −27·8) |
Data in parentheses are 95% uncertainty intervals. Data for all ages are given in the appendix (p 2).
Table 3.
Cases and age-standardised prevalence in 2020 for moderate and severe vision impairment and percent changes from 1990 to 2020 in adults aged 50 years and older, by cause of vision impairment
|
Cases (thousands) |
Age-standardised prevalence (per 1000) |
|||
|---|---|---|---|---|
| 2020 | Percentage change from 1990 to 2020 | 2020 | Percentage change from 1990 to 2020 | |
| Cataract | ||||
| Global | 78 800 (67200 to 91400) | 175·2% (170·9 to 179·5) | 43·4 (37·1 to 50·2) | 19·2% (17·8 to 20·5) |
| Central Europe, eastern Europe, and central Asia | 3050 (2490 to 3620) | 49·7% (46·2 to 53·0) | 21·3 (17·5 to 25·2) | 0·4% (−1·1 to 1·9) |
| High income | 7880 (6660 to 9230) | 100·2% (94·0 to 106·5) | 14·6 (12·2 to 17·1) | −1·8% (−2·8 to −0·7) |
| Latin America and Caribbean | 4350 (3650 to 5090) | 208·6% (201·8 to 215·7) | 33·9 (28·5 to 39·6) | −1·2% (−2·4 to 0·14) |
| North Africa and Middle East | 5020 (4230 to 5920) | 181·0% (172·6 to 189·6) | 58·1 (49·2 to 68·0) | 0·6% (−2·1 to 3·6) |
| South Asia | 27200 (23200 to 31800) | 180·7% (171·8 to 189·6) | 94·6 (81·1 to 109) | 1·7% (−0·3 to 3·6) |
| Southeast Asia, east Asia, and Oceania | 26 800 (23000 to 30900) | 235·5% (228·3 to 242·7) | 47·1 (40·4 to 54·1) | 13·5% (11·7 to 15·3) |
| Sub-Saharan Africa | 4440 (3780 to 5160) | 150·8% (146·1 to 156·1) | 51·4 (44·0 to 59·3) | 11·4% (9·7 to 13·4) |
| Undercorrected refractive error | ||||
| Global | 86 100 (74200 to 101000) | 101·8% (98·9 to 104·9) | 45·8 (39·6 to 53·7) | −6·9% (−8·0 to −5·9) |
| Central Europe, eastern Europe, and central Asia | 6340 (5400 to 7480) | 25·8% (23·2 to 28·3) | 45·1 (38·5 to 53·1) | −4·4% (−5·5 to −3·3) |
| High income | 8940 (7680 to 10400) | 69·6% (66·3 to 72·9) | 19·4 (16·7 to 22·5) | −4·6% (−5·6 to −3·6) |
| Latin America and Caribbean | 5780 (4950 to 6780) | 162·3% (158·5 to 165·8) | 42·8 (36·8 to 50·0) | −7·7% (−8·8 to −6·6) |
| North Africa and Middle East | 4680 (3960 to 5550) | 140·5% (134·2 to 147·2) | 47·3 (40·2 to 55·4) | −10·7% (−13·2 to −8·0) |
| South Asia | 32 100 (27500 to 37900) | 94·1% (89·6 to 99·7) | 103 (88·2 to 121) | −23·4% (−24·9 to −21·9) |
| Southeast Asia, east Asia, and Oceania | 25 000 (21500 to 29300) | 143·7% (138·4 to 148·7) | 39·4 (33·9 to 45·6) | −8·8% (−10·6 to −7·1) |
| Sub-Saharan Africa | 3210 (2730 to 3800) | 131·7% (126·7 to 136·4) | 31·6 (27·3 to 37·0) | 2·4% (0·6 to 4·1) |
| Glaucoma | ||||
| Global | 4130 (3240 to 5170) | 151·2% (147·2 to 155·3) | 2·29 (1·80 to 2·86) | 8·3% (6·8 to 9·9) |
| Central Europe, eastern Europe, and central Asia | 213 (167 to 270) | 43·6% (40·0 to 47·6) | 1·47 (1·15 to 1·86) | −3·0% (−4·7 to −1·4) |
| High income | 596 (467 to 762) | 103·2% (95·7 to 111·5) | 1·09 (0·853 to 1·39) | −0·2% (−1·5 to 1·0) |
| Latin America and Caribbean | 498 (390 to 623) | 191·7% (185·2 to 199·2) | 3·86 (3·02 to 4·84) | −4·7% (−6·1 to −3·1) |
| North Africa and Middle East | 325 (251 to 419) | 148·1% (139·1 to 157·7) | 3·76 (2·87 to 4·85) | −9·7% (−12·8 to −6·5) |
| South Asia | 952 (745 to 1200) | 145·2% (136·4 to 154·5) | 3·38 (2·66 to 4·21) | −12·8% (−15·0 to −10·6) |
| Southeast Asia, east Asia, and Oceania | 1160 (916 to 1450) | 251·5% (242·0 to 262·0) | 2·01 (1·58 to 2·52) | 21·4% (18·3 to 24·8) |
| Sub-Saharan Africa | 391 (306 to 493) | 111·9% (107·1 to 116·8) | 4·57 (3·61 to 5·69) | −4·3% (−6·3 to −2·2) |
| Age-related macular degeneration | ||||
| Global | 6220 (5030 to 7570) | 150·2% (145·9 to 154·8) | 3·39 (2·75 to 4·12) | 10·6% (8·7 to 12·6) |
| Central Europe, eastern Europe, and central Asia | 228 (182 to 282) | 51·1% (47·8 to 54·3) | 1·57 (1·26 to 1·95) | 4·8% (3·13 to 6·51) |
| High income | 738 (584 to 917) | 76·8% (70·5 to 83·3) | 1·39 (1·11 to 1·72) | −9·4% (−11·2 to −7·5) |
| Latin America and Caribbean | 333 (269 to 407) | 202·2% (193·0 to 212·2) | 2·55 (2·07 to 3·13) | 1·5% (−1·2 to 4·5) |
| North Africa and Middle East | 493 (390 to 613) | 166·0% (156·5 to 175·6) | 5·48 (4·36 to 6·77) | −0·5% (−4·0 to 2·8) |
| South Asia | 1220 (968 to 1510) | 121·4% (112·8 to 130·2) | 4·18 (3·36 to 5·11) | −20·5% (−23·0 to −18·0) |
| Southeast Asia, east Asia, and Oceania | 2760 (2210 to 3380) | 214·6% (204·7 to 224·4) | 4·61 (3·73 to 5·61) | 13·8% (10·7 to 17·1) |
| Sub-Saharan Africa | 453 (359 to 565) | 132·2% (124·6 to 140·3) | 4·96 (3·98 to 6·14) | 5·6% (2·3 to 9·0) |
| Diabetic retinopathy | ||||
| Global | 2950 (2140 to 3950) | 129·5% (123·2 to 135·9) | 1·59 (1·15 to 2·12) | 3·3% (0·4 to 5·8) |
| Central Europe, eastern Europe, and central Asia | 134 (94·2 to 183) | 21·7% (17·3 to 25·9) | 0·942 (0·661 to 1·28) | −11·3% (−13·9 to −8·7) |
| High income | 386 (277 to 522) | 68·4% (63·5 to 74·1) | 0·802 (0·578 to 1·08) | −7·7% (−9·7 to −6·0) |
| Latin America and Caribbean | 396 (290 to 533) | 185·6% (177·6 to 193·6) | 2·97 (2·17 to 4·01) | −0·9% (−3·1 to 1·4) |
| North Africa and Middle East | 399 (288 to 540) | 115·9% (106·3 to 125·6) | 4·14 (3·00 to 5·53) | −19·6% (−23·2 to −16·0) |
| South Asia | 389 (279 to 527) | 123·7% (114·5 to 134·5) | 1·28 (0·921 to 1·72) | −15·8% (−19·2 to −12·4) |
| Southeast Asia, east Asia, and Oceania | 1100 (796 to 1500) | 182·7% (166·3 to 200·2) | 1·79 (1·29 to 2·42) | 3·2% (−2·6 to 9·0) |
| Sub-Saharan Africa | 138 (98·6 to 186) | 145·3% (138·2 to 152·4) | 1·44 (1·04 to 1·92) | 9·9% (7·1 to 12·8) |
| Residual causes of vision loss | ||||
| Global | 28 200 (24100 to 33000) | 104·4% (100·3 to 108·5) | 15·2 (13·0 to 17·8) | −8·3% (−9·7 to −6·9) |
| Central Europe, eastern Europe, and central Asia | 4180 (3540 to 4950) | 34·6% (31·9 to 37·5) | 29·1 (24·7 to 34·3) | −5·7% (−7·0 to −4·4) |
| High income | 3060 (2570 to 3630) | 82·6% (77·6 to 88·5) | 6·32 (5·34 to 7·50) | −1·6% (−2·9 to −0·3) |
| Latin America and Caribbean | 2710 (2260 to 3230) | 176·9% (171·1 to 183·2) | 20·5 (17·1 to 24·3) | −7·6% (−8·9 to −6·3) |
| North Africa and Middle East | 1090 (890 to 1330) | 112·1% (98·8 to 124·5) | 11·6 (9·40 to 14·1) | −22·1% (−26·7 to −17·6) |
| South Asia | 6900 (5780 to 8250) | 141·1% (132·4 to 151·1) | 22·9 (19·5 to 27·0) | −5·7% (−8·5 to −2·8) |
| Southeast Asia, east Asia, and Oceania | 7850 (6780 to 9100) | 158·1% (148·7 to 167·5) | 12·7 (11·0 to 14·7) | −5·9% (−8·7 to −3·1) |
| Sub-Saharan Africa | 2410 (2020 to 2880) | 49·0% (42·0 to 56·0) | 24·7 (20·8 to 29·2) | −32·4% (−35·5 to −29·3) |
Data in parentheses are 95% uncertainty intervals. Data for all ages are given in the appendix (p 3).
In terms of relative contribution to age-standardised prevalence of total blindness in adults aged 50 years and older (table 4), cataract caused 45·5% (41·7–49·0) of all global blindness, followed by glaucoma (11·0% [9·3–12·8]), undercorrected refractive error (6·6% [5·6–7·8]), age-related macular degeneration (5·6% [4·3–7·0]) and diabetic retinopathy (2·5% [1·7–3·7]). The leading contributor to global age-standardised prevalence of adult MSVI was undercorrected refractive error (table 4; 41·0% [38·0–44·1]), followed by cataract (38·9% [35·6–42·4]), age-related macular degeneration (3·0% [2·5–3·5]), glaucoma (2·1% [1·7–2·5]), and diabetic retinopathy (1·4% [1·0–1·9]).
Table 4.
Relative percentage contribution of each cause to age-standardised prevalence of blindness and moderate and severe vision impairment by superregion in 2020 in adults aged 50 years and older
| Cataract | Undercorrected refractive error | Glaucoma | Age-related macular degeneration | Diabetic retinopathy | Residual causes of vision loss | |
|---|---|---|---|---|---|---|
| Blindness | ||||||
| Global | 45·4% (41·7–49·0) | 6·6% (5·6–7·8) | 11% (9·3–12·8) | 5·6% (4·3–6·7) | 2·5% (1·7–3·7) | 28·9% (26·5–31·5) |
| Central Europe, eastern Europe, and central Asia | 22·4% (19·1–25·9) | 1·4% (1·2–1·8) | 14·8% (12·3–17·3) | 5·2% (3·8–6·7) | 1·0% (0·7–1·5) | 55·1% (51·0–59·6) |
| High income | 17·5% (14·9–20·5) | 2·1% (1·7–2·5) | 28·2% (24·0–32·3) | 21·6% (17·5–26·1) | 6·2% (4·2–8·8) | 24·5% (21·6–27·8) |
| Latin America and Caribbean | 35·4% (31·4–39·8) | 4·3% (3·6–5·0) | 11·8% (9·7–13·9) | 2·5% (1·8–3·2) | 6·8% (4·5–9·6) | 39·2% (35·5–43·4) |
| North Africa and Middle East | 33·6% (29·4–38·0) | 3·3% (2·7–3·8) | 21·1% (17·7–24·5) | 8·3% (6·2–10·5) | 2·3% (1·5–3·6) | 31·5% (27·8–36·0) |
| South Asia | 63·1% (59·4–66·8) | 9·4% (7·9–10·9) | 6·4% (5·2–7·7) | 3·0% (2·1–4·0) | 1·4% (0·9–2·1) | 16·8% (15·0–18·8) |
| Southeast Asia, east Asia, and Oceania | 48·3% (44·5–52·1) | 7·3% (6·2–8·5) | 6·7% (5·5–7·9) | 4·2% (3·0–5·4) | 2·0% (1·3–3·0) | 31·6% (29·0–34·3) |
| Sub-Saharan Africa | 39·8% (35·9–43·9) | 3·1% (2·6–3·6) | 17·8% (15·1–20·6) | 4·0% (3·0–5·1) | 0·9% (0·6–1·4) | 34·4% (31·4–37·7) |
| Moderate and severe vision impairment | ||||||
| Global | 38·9% (35·6–42·4) | 41% (38·0–44·1) | 2·1% (1·7–2·5) | 3·0% (2·5–3·5) | 1·4% (1·0–2·0) | 13·6% (12·3–15·2) |
| Central Europe, eastern Europe, and central Asia | 21·4% (18·8–24·2) | 45·3% (42·0–48·6) | 1·5% (1·2–1·8) | 1·6% (1·3–1·9) | 1·0% (0·7–1·3) | 29·3% (26·2–32·5) |
| High income | 33·5% (29·8–37·2) | 44·5% (41·1–48·0) | 2·5% (2·0–3·1) | 3·2% (2·7–3·8) | 1·9% (1·3–2·5) | 14·5% (12·7–16·8) |
| Latin America and Caribbean | 31·8% (28·4–35·3) | 40·2% (37·1–43·4) | 3·6% (3·0–4·4) | 2·4% (2·0–2·8) | 2·8% (2·0–3·8) | 19·2% (17·0–21·8) |
| North Africa and Middle East | 44·6% (40·6–48·8) | 36·3% (32·7–39·8) | 2·9% (2·3–3·6) | 4·2% (3·5–5·0) | 3·2% (2·3–4·3) | 8·9% (7·6–10·6) |
| South Asia | 41·3% (37·8–45) | 44·9% (41·3–48·1) | 1·5% (1·2–1·8) | 1·8% (1·5–2·2) | 0·6% (0·4–0·8) | 10% (8·9–11·2) |
| Southeast Asia, east Asia, and Oceania | 43·8% (40·4–47·2) | 36·6% (33·7–39·7) | 1·9% (1·5–2·3) | 4·3% (3·6–5·0) | 1·7% (1·2–2·3) | 11·8% (10·8–13·0) |
| Sub-Saharan Africa | 43·3% (39·8–46·8) | 26·7% (24·4–29·0) | 3·9% (3·2–4·8) | 4·2% (3·5–4·9) | 1·2% (0·9–1·6) | 20·8% (18·7–23·0) |
Data in parentheses are 95% uncertainty intervals.
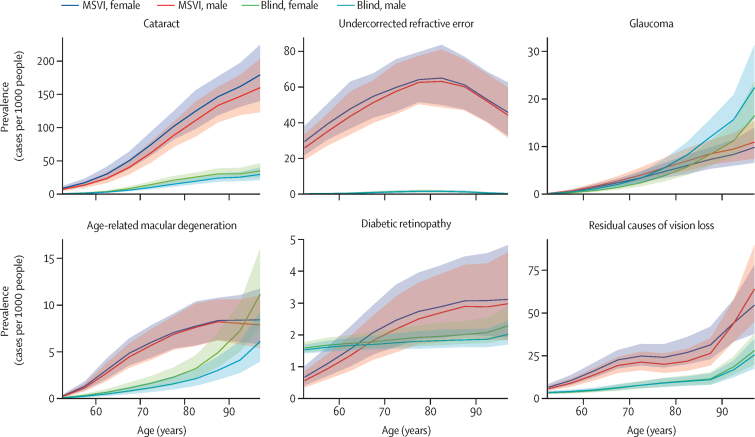
Overall, prevalence of vision impairment increased with age, although the pattern of age-specific prevalence varied by cause and severity (figure 1). MSVI prevalence was consistently higher than blindness for all causes, with the exception of glaucoma and age-related macular degeneration at the oldest ages. MSVI due to most causes increased from age 50 years onward, although MSVI due to undercorrected refractive error increased up to the age of around 80 years and decreased thereafter.
Figure 1.
Age-specific prevalence rates of distance blindness and MSVI by cause and sex in adults aged 50 years and older in 2020
Solid lines show sex-specific prevalence estimates, with shaded areas indicating 95% uncertainty intervals. MSVI=moderate to severe vision impairment.
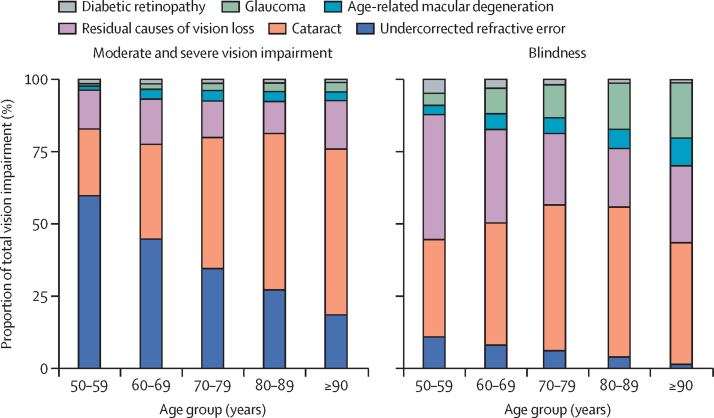
Of the explicitly modelled causes of global blindness, cataract was the principal cause of global blindness in all 10-year age groups for ages 50 years and older (figure 2). The contribution of glaucoma and age-related macular degeneration were greatest in the oldest age group, while the contributions of diabetic retinopathy to blindness decreased with age. For global MSVI, undercorrected refractive error was the principal contributor in the age groups 50–59 and 60–69 years, and cataract was the principal cause in those aged 70 years and older.
Figure 2.
Relative contribution of each cause to crude prevalence of blindness and moderate and severe vision impairment in 2020 by age group
We compared age-standardised prevalence between men and women aged 50 years and older for each cause of vision impairment and found that age-standardised prevalence of blindness was greater in women for cataract (difference between means: 0·19% [0·16 to 0·24]), undercorrected refractive error (0·006% [0·003 to 0·01]), age-related macular degeneration (0·037% [0·028 to 0·047]), and diabetic retinopathy (0·008% [0·005 to 0·001]), and greater in men for glaucoma (–0·072 [–0·086 to −0·058]. The same patterns were found for sex differences in causes of MSVI (data not shown).
When looking at geographical trends, in 2020, cataract was the largest contributor to blindness in adults aged 50 years and older in all super-regions except for the high-income super-region, where the largest contributor was glaucoma (table 4). This was primarily driven by two regions, western Europe (glaucoma: 32·5% [27·3 to 37·3] vs cataract: 11·4% [9·4 to 34·9]) and high-income Asia Pacific (glaucoma: 33·7% [29·4 to 37·7] vs cataract: 20·5% [17·7 to 23·9]). For MSVI (table 4), cataract was the leading contributor in western and eastern sub-Saharan Africa, southeast Asia, Oceania, and north Africa and Middle East. Cataract and undercorrected refractive error contributed similarly in central Asia, Andean Latin America, east Asia, and south Asia; undercorrected refractive error was the largest contributor everywhere else.
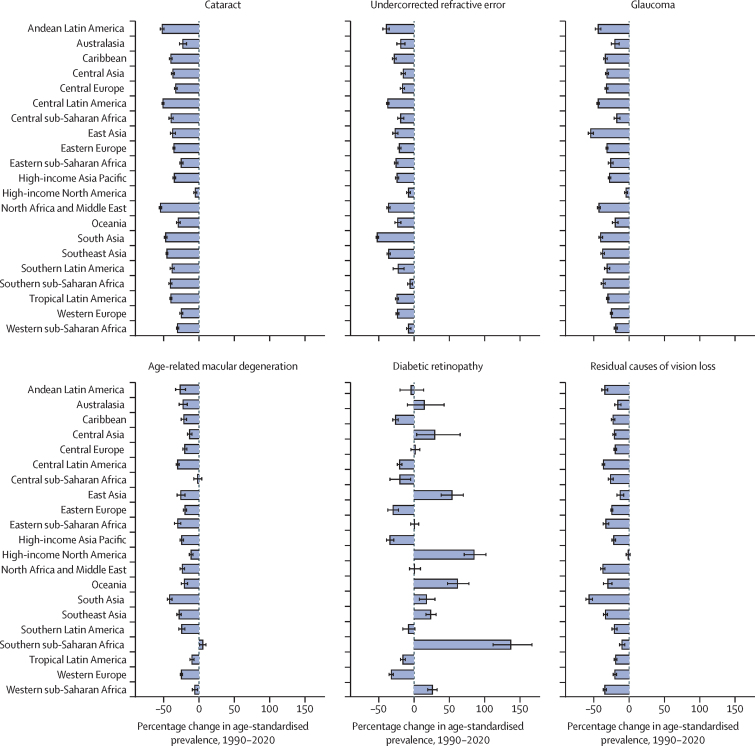
Age-standardised prevalence of blindness for all modelled causes consistently showed a regional decrease between 1990 and 2020 (figure 3). The notable exception to this trend was diabetic retinopathy, for which prevalence increased in many regions, with the largest increase in southern sub-Saharan Africa (percentage change 138·3% [113·0–168·5]). The pattern for MSVI was less consistent, with regional variation of increased, decreased, or no change to age-standardised prevalence between 1990 and 2020 for all modelled causes (appendix p 8). All age estimates and crude prevalence by sex are shown in the appendix (pp 3–5).
Figure 3.
Change in regional age-standardised prevalence of blindness between 1990 and 2020 in adults aged 50 years and older, by cause of blindness
Data for moderate and severe vision impairment are presented in appendix (p 8).
For myopic macular degeneration, we only produced estimates in China because of data sparsity. In 2020, the all-age crude prevalence of vision loss due to myopic macular degeneration was 0·02% (95% UI 0·01–0·03) for blindness and 0·21% (0·14–0·31) for MSVI. The number of people blind due to myopic macular degeneration increased by approximately 200% from 0·103 million (95% UI 0·0678–0·154) people in 1990 to 0·310 million (0·203–0·472) people in 2020. The number of people with MSVI due to myopic macular degeneration increased by approximately 340% from 0·659 million (0·433–1·01) people in 1990 to 2·93 million (1·96–4·38) people in 2020. In 2020, blindness due to myopic macular degeneration was more prevalent than blindness due to diabetic retinopathy (0·232 million people [0·156–0·348]), and similar to age-related macular degeneration (0·327 million people [0·226–0·447], while MSVI due to myopic macular degeneration was more prevalent than diabetic retinopathy (0·882 million people [0·632–1·18]), glaucoma (0·889 million people [0·700–1·11]), and age-related macular degeneration (2·36 million people [1·88–2·89]).
Discussion
Our results show that both cataract and undercorrected refractive error are among the three leading causes of blindness and MSVI in 2020. We estimate that worldwide there are over 15 million adults aged 50 years and older who are blind due to cataract, and more than 86 million who have MSVI due to undercorrected refractive error. In 2020, blindness due to cataract and undercorrected refractive error composes 50% of all global blindness, and MSVI due to cataract and undercorrected refractive error composes 75% of all global MSVI. The burden of total blindness due to cataract and undercorrected refractive error has notable regional variability, but it has not been fully addressed in any world region, including high-income regions. The other main causes—glaucoma, age-related macular degeneration, and diabetic retinopathy—collectively contribute to over 6 million blind adults aged 50 years and older and over 13 million adults aged 50 years and older with MSVI in 2020. With the exception of diabetic retinopathy, age-standardised prevalence due to all of the causes of blindness we report here has decreased between 1990 and 2020. Given that the vast majority of vision impairment and blindness caused by cataract, undercorrected refractive error, diabetic retinopathy, and glaucoma can be avoided with early detection and timely intervention, a large potential in reducing morbidity for these causes remains.
The WHA defined cataracts and refractive error as avoidable causes of vision impairment because they are so effectively treated with surgery and spectacles, respectively. The WHA GAP set a target of a 25% reduction in crude prevalence of avoidable vision impairment from 2010 to 2019. It specifically highlighted the importance of reducing avoidable vision impairment prevalence in those aged 50 years and older given the majority of vision impairment occurs at older ages.8 We estimated that there has been an increase in all-age prevalence of avoidable vision impairment and no change in prevalence for adults aged 50 years and older during this time period, demonstrating that the WHA GAP goal was not met. This lack of change was driven primarily by almost no change in crude and age-standardised prevalence of avoidable MSVI, and a lower-than-necessary decrease in the age-standardised prevalence of avoidable blindness. Cases of avoidable blindness and MSVI both increased in people aged 50 years and older. We therefore note that the GAP target was not met and that ageing populations and the strong association between vision impairment and age were an important barrier in reaching the target. With increasing need for prevention and treatment, eye care services have not managed to sufficiently keep up with demand to meet the target. However, the fact that the change in crude prevalence was better for avoidable blindness (–14·4%) than for avoidable MSVI (1·6%) suggests that the resources put into reducing blindness and visual impairment have been appropriately targeted at reducing blindness ahead of MSVI.
In 2020, cataract remained the first or second leading cause of blindness and MSVI in all world regions.1 Cataract can at present only be treated operatively, by a trained surgeon within a system that has capacity to deliver surgeries and manage any postoperative complications. Alleviation efforts have taken the form of mass campaigns, especially in remote areas, and increasing the capacity for and accessibility of surgical services. Because prevalence increases with age, and is higher in women than in men, it remains an important focus for vision loss alleviation and for addressing gender equity. Outreach screening has been shown to enhance equity of access among underserved groups such as women and the elderly.19 We therefore recommend developing robust eye care systems supplemented by community outreach as principal strategies.
Undercorrected refractive error is an important cause of vision impairment and is easily treatable by spectacles, contact lenses, or refractive surgery. Myopia, hyperopia, and astigmatism are the main causes of distance vision impairment. Uncorrected aphakia has greatly declined since 1990 because of the use of intraocular lenses during cataract surgery.20 Conversely, the prevalence of myopia has been rapidly increasing, especially in urban areas.21 The development of refractive services, including the provision of affordable spectacles are the main strategies to address uncorrected refractive errors.
Although cataract and undercorrected refractive error accounted for the majority of blindness and MSVI, glaucoma, age-related macular degeneration, and diabetic retinopathy also caused moderate or worse vision impairment in almost 20 million people aged 50 years and older in 2020. These diseases are not easily treatable.
Glaucoma was ranked as the second leading cause of blindness and fourth leading cause of MSVI, and therefore the most common cause of irreversible blindness, and the second most common cause of irreversible MSVI. Glaucoma in eyes with dense cataract might not be detected, and therefore glaucoma-related irreversible blindness was probably undercounted. With respect to the prevention of glaucoma-related vision impairment, tonometry has not proven to be a useful screening technique and visual acuity assessment is not useful because vision impairment is a late symptom of glaucomatous optic neuropathy.22 Once detected, therapy for glaucoma can arrest or slow its deterioration in the majority of cases,23 hence the importance of improving systems of surveillance, highlighting risk among family members of cases, and effectiveness of care once treatment is initiated.
The age-standardised prevalence of blindness due to age-related macular degeneration declined by almost 30% from 1990 to 2020. This decrease was probably associated with the widespread clinical introduction of anti-VEGF therapy for exudative age-related macular degeneration.24 Since the majority of patients with age-related macular degeneration show the currently untreatable non-exudative form that can progress to atrophy of the foveal centre (geographic atrophy), the development of treatments and prophylactic measures specifically against non-exudative age-related macular degeneration are warranted.
Although diabetic retinopathy was the smallest contributor to blindness in 2020 compared with undercorrected refractive error, cataract, age-related macular degeneration, and glaucoma, it was the only cause of blindness that showed a global increase in age-standardised prevalence between 1990 and 2020. With a projected more than 600 million people living with diabetes by 2040,25 and because people with diabetes live increasingly longer, the number of people with diabetic retinopathy and resulting vision impairment is expected to rapidly rise.26, 27 Our study shows that diabetic retinopathy continues to be an identifiable cause of vision impairment. This is of particular concern in younger, economically active age groups. Our study also shows regional differences in temporal change of blindness due to diabetic retinopathy, with increases in many regions of Asia and sub-Saharan Africa, as well as high-income North America. Of concern is that, in comparison with cataract and undercorrected refractive error, the management of severe diabetic retinopathy requires a disproportionate amount of resources, including availability of ophthalmologists who are trained in laser and surgery.28, 29
The strengths of this updated review and analysis for 2020 include the substantial addition of new data sources disaggregated by cause and the wider geographical region that these sources cover. In particular, the addition of new RAAB surveys improved geographic coverage, and the age disaggregation of many of these surveys improved the fitting of age patterns to the data. However, there remain several regions such as central sub-Saharan Africa, central and eastern Europe, and central Asia, with little or no population-based data where estimates rely on extrapolation from other regions. There are surprisingly few data from high-income regions—only 19 studies included here reported cause-specific vision impairment in a high-income location, and all but three of these took place more than a decade ago. Sparse data also limited the certainty of estimates of temporal trends and age patterns, particularly in children and young adults for undercorrected refractive error. Minimum ages set for inclusion of data by different causes was agreed with members of the VLEG but this consensus approach could be considered a limitation. A considerable proportion of the blindness burden was listed as “residual causes”. This “other” category is the result of a number of factors such as surveys not committing to a cause for each reported case of vision loss, the truncated list of causes given in published materials, and causes for which we have very limited data such as onchocerciasis, trachoma, xerophthalmia, ocular trauma, corneal diseases, amblyopia, and retinopathy of prematurity. With trachoma, for example, WHO reports that the numbers at risk have dropped from 1·5 billion in 2002 to 142 million in 2019 and the number with trichiasis from 7·6 million to 2·5 million.30 RAAB studies were adjusted to reference non-RAAB studies using adjustments generated for all-causes of MSVI and blindness impairment combined because these models were more data rich. However, these adjustments might not be the same for conditions affecting the fundus. Regional-level data might be misleading by masking the diversity of existing situations within countries and even within communities.31, 32 Greater sociodemographic granularity in data collection is needed to identify populations at risk and capture actual progress in the provision of equitable eye care services.
This report highlights a need for more data on the causes of vision impairment, where we found data sources to be sparse, particularly in children and young adults, high-income locations, and in sub-Saharan Africa. The development of RAABs has led to increasing coverage of low-income and middle-income countries, but not for younger age groups. Also, up-to-date, population-representative data from high-income settings has lagged behind. Better age and geographical data coverage would allow for more detailed analyses of individual country differences and a breakdown of which diseases most impact vision in children.
This report represents a major update of global and regional data on the causes of prevalence of blindness and vision impairment and adds to our understanding of temporal change over 30 years. Over the past decade the prevalence of avoidable visual impairment has decreased in adults aged 50 years and older, but it has not reached the targeted 25% reduction delineated in the WHA GAP. The principal reason from a global perspective is the failure of eye care services to keep pace with the ageing and growth of populations, yet the reduction in age-standardised prevalence of blindness due to causes such as cataract, glaucoma, age-related macular degeneration, and undercorrected refractive error was a reassuring change in the right direction. The report demonstrates the considerable inter-regional differences that exist and highlights areas which require particular attention, such as blindness due to diabetic retinopathy, which was the only cause to increase in age-standardised blindness prevalence over three decades.
Correspondence to: Prof Rupert R A Bourne, Vision and Eye Research Institute, Anglia Ruskin University, Cambridge CB1 1PT, UK rb@rupertbourne.co.uk
Data sharing
More than ten authors have accessed and verified the data. To download the data used in these analyses, please visit the Global Health Data Exchange GBD 2019 website.
Acknowledgments
Acknowledgments
This manuscript was produced as part of the GBD Collaborator Network and in accordance with the GBD protocol. T W Bärnighausen was supported by the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor award, funded by the German Federal Ministry of Education and Research. R R A Bourne received institutional support from Anglia Ruskin University, Cambridge, UK. G Gazzard is employed by University College London (London, UK) and supported by grants from the NIHR (HTA 09/104/40), Moorfields Eye Charity, British Council to Prevent Blindness, and Fight for Sight and the International Glaucoma Association. M E R Hartnett's work is supported by grants from NIH R01 EY015130, NIH R01 EY017011, and NIH EY014800 Unrestricted Grant from Research to Prevent Blindness (NY, USA) to the Department of Ophthalmology & Visual Sciences, University of Utah (Salt Lake City, UT, USA). S M S Islam received funding from National Health and Medical Research Council (NHMRC) and National Heart Foundation. J H Kempen received support from the Massachusetts Eye and Ear Global Surgery Program; Sight for Souls. Y J Kim received support by the Research Management Centre, Xiamen University Malaysia [XMUMRF/2020-C6/ITCM/0004]. I Landires is a member of the Sistema Nacional de Investigación (SNI), which is supported by the Secretaría Nacional de Ciencia, Tecnología e Innovación (SENACYT), Panamá. A M Samy received support from a fellowship from the Egyptian Fulbright Mission Program. D Stambolia received research support from the National Eye Institute of the NIH under Award Number R01EY031209.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Contributors
Please see the appendix (pp 9–11) for more detailed information on authors' contributions to the research, divided into the following categories: managing the estimation process; writing the first draft of the manuscript; providing data or critical feedback on data sources; development of methods or computational machinery; providing critical feedback on methods or results; extracting, cleaning, or cataloguing data; designing or coding figures and tables; drafting the manuscript or revising it critically for important intellectual content; and managing the overall research enterprise.
GBD 2019 Blindness Causes Collaborators
Jaimie D Steinmetz*, Rupert R A Bourne*, Paul Svitil Briant, Seth Flaxman, Hugh R Taylor, Jost B Jonas, Amir Abdoli, Woldu Aberhe Abrha, Ahmed Abualhasan, Eman Abu-Gharbieh, Tadele Girum Adal, Ashkan Afshin, Hamid Ahmadieh, Wondu Alemayehu, Sayyed Amirpooya Alemzadeh, Ahmed Samir Alfaar, Vahid Alipour, Sofia Androudi, Jalal Arabloo, Aries Arditi, Brhane Berhe Aregawi, Alessandro Arrigo, Charlie Ashbaugh, Elham Ashrafi, Desta Debalkie Atnafu, Eleni Bagli, Atif Amin Baig, Till Winfried Bärnighausen, Maurizio Battaglia Parodi, Mahya Beheshti, Akshaya Srikanth Bhagavathula, Nikha Bhardwaj, Pankaj Bhardwaj, Krittika Bhattacharyya, Ali Bijani, Mukharram Bikbov, Michele Bottone, Tasanee Braithwaite, Alain M Bron, Sharath Burugina Nagaraja, Zahid A Butt, Florentino Luciano Caetano dos Santos, Vera L A Carneiro, Robert James Casson, Ching-Yu Cheng, Jee-Young Jasmine Choi, Dinh-Toi Chu, Maria Vittoria Cicinelli, João M Coelho, Nathan G Congdon, Rosa A S Couto, Elizabeth A Cromwell, Saad M A Dahlawi, Xiaochen Dai, Reza Dana, Lalit Dandona, Rakhi Dandona, Monte A Del Monte, Meseret Derbew Molla, Nikolaos Dervenis, Abebaw Alemayehu Desta, Jenny P Deva, Daniel Diaz, Shirin Djalalinia, Joshua R Ehrlich, Rajesh Elayedath, Hala Rashad Elhabashy, Leon B Ellwein, Mohammad Hassan Emamian, Sharareh Eskandarieh, Farshad Farzadfar, Arthur G Fernandes, Florian Fischer, David S Friedman, João M Furtado, Shilpa Gaidhane, Gus Gazzard, Berhe Gebremichael, Ronnie George, Ahmad Ghashghaee, Syed Amir Gilani, Mahaveer Golechha, Samer Hamidi, Billy Randall Hammond, Mary Elizabeth R Hartnett, Risky Kusuma Hartono, Abdiwahab Hashi, Simon I Hay, Khezar Hayat, Golnaz Heidari, Hung Chak Ho, Ramesh Holla, Mowafa Househ, John J Huang, Segun Emmanuel Ibitoye, Irena M Ilic, Milena D Ilic, April D Ingram, Seyed Sina Naghibi Irvani, Sheikh Mohammed Shariful Islam, Ramaiah Itumalla, Shubha Jayaram, Ravi Prakash Jha, Rim Kahloun, Rohollah Kalhor, Himal Kandel, Ayele Semachew Kasa, Taras Kavetskyy, Gbenga A Kayode, John H Kempen, Moncef Khairallah, Rovshan Khalilov, Ejaz Ahmad Khan, Rohit C Khanna, Mahalaqua Nazli Khatib, Tawfik Ahmed Muthafer Khoja, Gyu Ri Kim, Judy E Kim, Yun Jin Kim, Adnan Kisa, Sezer Kisa, Soewarta Kosen, Ai Koyanagi, Burcu Kucuk Bicer, Vaman Kulkarni, Om P Kurmi, Iván Landires, Van Charles Lansingh, Janet L Leasher, Kate E LeGrand, Nicolas Leveziel, Hans Limburg, Xuefeng Liu, Shilpashree Madhava Kunjathur, Shokofeh Maleki, Navid Manafi, Kaweh Mansouri, Colm McAlinden, Gebrekiros Gebremichael Meles, Abera M Mersha, Irmina Maria Michalek, Ted R Miller, Sanjeev Misra, Yousef Mohammad, Seyed Farzad Mohammadi, Jemal Abdu Mohammed, Ali H Mokdad, Mohammad Ali Moni, Ahmed Al Montasir, Alan R Morse, Getahun Fentaw Mulaw, Mehdi Naderi, Homa Naderifar, Kovin S Naidoo, Mukhammad David Naimzada, Vinay Nangia, Sreenivas Narasimha Swamy, Muhammad Naveed, Hadush Negash, Huong Lan Thi Nguyen, Virginia Nunez-Samudio, Felix Akpojene Ogbo, Kolawole Ogundimu, Andrew T Olagunju, Obinna E Onwujekwe, Nikita Otstavnov, Mayowa O Owolabi, Keyvan Pakshir, Songhomitra Panda-Jonas, Utsav Parekh, Eun-Cheol Park, Maja Pasovic, Shrikant Pawar, Konrad Pesudovs, Tunde Peto, Hai Quang Pham, Marina Pinheiro, Vivek Podder, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Rahman, Pradeep Y Ramulu, Priya Rathi, David Laith Rawaf, Salman Rawaf, Lal Rawal, Nickolas Reinig, Andre M N Renzaho, Aziz Rezapour, Alan L Robin, Luca Rossetti, Siamak Sabour, Sare Safi, Amirhossein Sahebkar, Mohammad Ali Sahraian, Abdallah M Samy, Brijesh Sathian, Ganesh Kumar Saya, Mete Saylan, Amira A Shaheen, Masood Ali Shaikh, Tueng T Shen, Kenji Shibuya, Wondimeneh Shibabaw Shiferaw, Mika Shigematsu, Jae Il Shin, Juan Carlos Silva, Alexander Silvester, Jasvinder A Singh, Deepika Singhal, Rita S Sitorus, Eirini Skiadaresi, Valentin Yurievich Skryabin, Anna Aleksandrovna Skryabina, Amin Soheili, Muluken Bekele Sorrie, Raúl A R C Sousa, Chandrashekhar T Sreeramareddy, Dwight Stambolian, Eyayou Girma Tadesse, Nina Tahhan, Md Ismail Tareque, Fotis Topouzis, Bach Xuan Tran, Gebiyaw Wudie Tsegaye, Miltiadis K Tsilimbaris, Rohit Varma, Gianni Virgili, Avina Vongpradith, Giang Thu Vu, Ya Xing Wang, Ningli Wang, Abrha Hailay Weldemariam, Sheila K West, Temesgen Gebeyehu Wondmeneh, Tien Y Wong, Mehdi Yaseri, Naohiro Yonemoto, Chuanhua Yu, Mikhail Sergeevich Zastrozhin, Anasthasia Zastrozhina, Zhi-Jiang Zhang, Stephanie R M Zimsen, Serge Resnikoff†, Theo Vos†.
*Contributed equally. †Joint last authors.
GBD 2019 Blindness Causes Affiliations
Institute for Health Metrics and Evaluation (J D Steinmetz PhD, P S Briant BS, A Afshin MD, C Ashbaugh MA, E A Cromwell PhD, X Dai PhD, Prof L Dandona MD, Prof R Dandona PhD, Prof S I Hay FMedSci, K E LeGrand MPH, Prof A H Mokdad PhD, M Pasovic MA, N Reinig BS, A Vongpradith BA, S R M Zimsen MA, Prof T Vos PhD), Department of Health Metrics Sciences, School of Medicine (A Afshin MD, E A Cromwell PhD, Prof R Dandona PhD, Prof S I Hay FMedSci, Prof A H Mokdad PhD, Prof T Vos PhD), Department of Ophthalmology (Prof T T Shen MD), University of Washington, Seattle, WA, USA; Vision and Eye Research Institute (Prof R R A Bourne MD, A Silvester MSc), Anglia Ruskin University, Cambridge, UK; Department of Mathematics (S Flaxman PhD, M Bottone PhD), WHO Collaborating Centre for Public Health Education and Training (D L Rawaf MD), Department of Primary Care and Public Health (Prof S Rawaf MD), Imperial College London, London, UK; School of Population and Global Health (Prof H R Taylor MD), University of Melbourne, Carlton, VIC, Australia; Department of Ophthalmology (Prof J B Jonas MD, S Panda-Jonas MD), Heidelberg Institute of Global Health (HIGH) (Prof T W Bärnighausen MD), Heidelberg University, Heidelberg, Germany; Beijing Institute of Ophthalmology (Prof J B Jonas MD, Y Wang MD), Beijing Tongren Eye Center (Prof N Wang PhD), Beijing Tongren Hospital, Beijing, China; Department of Parasitology and Mycology (A Abdoli PhD), Jahrom University of Medical Sciences, Jahrom, Iran; Department of Adult Health Nursing (W A Abrha MSc, A H Weldemariam MSc), Aksum University, Aksum, Ethiopia; Department of Neurology (A Abualhasan MD), Neurophysiology Unit (Prof H R Elhabashy MD), Cairo University, Cairo, Egypt; Department of Clinical Sciences (E Abu-Gharbieh PhD), University of Sharjah, Sharjah, United Arab Emirates; Department of Public Health (T G Adal MPH), Wolkite University, Wolkite, Ethiopia; Ophthalmic Research Center (H Ahmadieh MD, S Safi PhD, M Yaseri PhD), Department of Ophthalmology (H Ahmadieh MD), Research Institute for Endocrine Sciences (S N Irvani MD), Department of Epidemiology (S Sabour PhD), Ophthalmic Epidemiology Research Center (S Safi PhD), Shahid Beheshti University of Medical Sciences, Tehran, Iran; The Fred Hollows Foundation, Sydney, NSW, Australia (W Alemayehu MD); Berhan Public Health & Eye Care Consultancy, Addis Ababa, Ethiopia (W Alemayehu MD); Eye Research Center (S Alemzadeh MD), Health Management and Economics Research Center (V Alipour PhD, J Arabloo PhD, A Ghashghaee BSc, A Rezapour PhD), Health Economics Department (V Alipour PhD), Student Research Committee (A Ghashghaee BSc), School of Medicine (N Manafi MD), Iran University of Medical Sciences, Tehran, Iran; Department of Ophthalmology (A S Alfaar MD), University of Leipzig Medical Center, Leipzig, Germany; Department of Ophthalmology (A S Alfaar MD), Charité Medical University Berlin, Berlin, Germany; Department of Medicine (S Androudi PhD), University of Thessaly, Volos, Greece; Department of Research (A Arditi PhD), Visibility Metrics LLC, Chappaqua, NY, USA; College of Medicine and Health Sciences (B B Aregawi PhD), Department of Medical Laboratory Sciences (H Negash MSc), Adigrat University, Adigrat, Ethiopia; Department of Ophthalmology (A Arrigo MD), San Raffaele Hospital, Milano, Italy; Department of Ophthalmology (A Arrigo MD, Prof M Battaglia Parodi MD), Vita-Salute San Raffaele University, Milano, Italy; Translational Ophthalmology Research Center (E Ashrafi PhD, S Mohammadi MD), Multiple Sclerosis Research Center (S Eskandarieh PhD, Prof M Sahraian MD), Non-communicable Diseases Research Center (Prof F Farzadfar DSc), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD), Department of Epidemiology and Biostatistics (M Yaseri PhD), Tehran University of Medical Sciences, Tehran, Iran; Department of Health System and Health Economics (D D Atnafu MPH), Department of Adult Health Nursing (A Kasa MSc), College of Medicine and Health Sciences (G W Tsegaye MPH), Bahir Dar University, Bahir Dar, Ethiopia; Department of Ophthalmology (E Bagli PhD), University Hospital of Ioannina, Ioannina, Greece; Institute of Molecular Biology & Biotechnology (E Bagli PhD), Foundation for Research & Technology, Ioannina, Greece; Unit of Biochemistry (A A Baig PhD), Sultan Zainal Abidin University, Kuala Terengganu, Malaysia; T H Chan School of Public Health (Prof T W Bärnighausen MD), Department of Ophthalmology (Prof R Dana MD, Prof D S Friedman MD, Prof J H Kempen MD), Harvard University, Boston, MA, USA; Department of Physical Medicine and Rehabilitation (M Beheshti MD), New York University, New York, NY, USA; Department of Social and Clinical Pharmacy (A S Bhagavathula PharmD), Charles University, Hradec Kralova, Czech Republic; Institute of Public Health (A S Bhagavathula PharmD), United Arab Emirates University, Al Ain, United Arab Emirates; Department of Anatomy (Prof N Bhardwaj MD), Government Medical College Pali, Pali, India; Department of Community Medicine and Family Medicine (P Bhardwaj MD), School of Public Health (P Bhardwaj MD), Department of Surgical Oncology (Prof S Misra MCh), All India Institute of Medical Sciences, Jodhpur, India; Department of Statistical and Computational Genomics (K Bhattacharyya MSc), National Institute of Biomedical Genomics, Kalyani, India; Department of Statistics (K Bhattacharyya MSc), University of Calcutta, Kolkata, India; Social Determinants of Health Research Center (A Bijani PhD), Babol University of Medical Sciences, Babol, Iran; Epidemiology Department (Prof M Bikbov PhD), Ufa Eye Research Institute, Ufa, Russia; Department of Computer Science (M Bottone PhD), Middlesex University London, London, UK; Ophthalmology Department (T Braithwaite PhD), Moorfields Eye Hospital NHS Foundation Trust, London, UK; International Centre for Eye Health (T Braithwaite PhD), London School of Hygiene & Tropical Medicine, London, UK; Department of Ophthalmology (Prof A M Bron MD), University Hospital Dijon, Dijon, France; Eye and Nutrition Research Group (Prof A M Bron MD), Université Bourgogne Franche-Comté, Dijon, France; Department of Community Medicine (Prof S Burugina Nagaraja MD), Employee State Insurance Post Graduate Institute of Medical Sciences and Research, Bangalore, India; School of Public Health and Health Systems (Z A Butt PhD), University of Waterloo, Waterloo, ON, Canada; Al Shifa School of Public Health (Z A Butt PhD), Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan; Institute of Microengineering (F L Caetano dos Santos PhD), Federal Polytechnic School of Lausanne, Lausanne, Switzerland; School of Sciences (V L A Carneiro MSc), University of Minho, Braga, Portugal; Directive Board (R A R C Sousa FEAOO), Association of Licensed Optometry Professionals, Linda-a-Velha, Portugal (V L A Carneiro MSc); Department of Ophthalmology (Prof R J Casson PhD), School of Public Health (V Podder HSC), University of Adelaide, Adelaide, SA, Australia; Ocular Epidemiology Research Group (Prof C Cheng MD), Singapore Eye Research Institute, Singapore, Singapore; Ophthalmology & Visual Sciences Academic Clinical Program (Prof C Cheng MD), Duke-NUS Medical School (Prof T Y Wong MD), Singapore, Singapore; Biomedical Informatics (J J Choi PhD), Seoul National University Hospital, Seoul, South Korea; Faculty of Biology (D Chu PhD), Hanoi National University of Education, Hanoi, Vietnam; Department of Ophthalmology (M Cicinelli MD), San Raffaele Scientific Institute, Milano, Italy; University Hospital Center of Porto (J M Coelho MD), Department of Chemical Sciences (R A S Couto MD), Department of Chemistry (M Pinheiro PhD), University of Porto, Porto, Portugal; Centre for Public Health (Prof N G Congdon MD, G Virgili MD), Queen's University, Belfast, UK; Orbis International, New York, NY, USA (Prof N G Congdon MD); Environmental Health Department (S M A Dahlawi PhD), Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; Public Health Foundation of India, Gurugram, India (Prof L Dandona MD, Prof R Dandona PhD); Indian Council of Medical Research, New Delhi, India (Prof L Dandona MD); Department of Ophthalmology and Visual Sciences (Prof M A Del Monte MD, J R Ehrlich MD, A L Robin MD), Institute for Health Care Policy and Innovation (J R Ehrlich MD), Department of Systems, Populations, and Leadership (X Liu PhD), University of Michigan, Ann Arbor, MI, USA; Department of Biochemistry (M Derbew Molla MSc), Department of Surgical Nursing (A A Desta MSc), University of Gondar, Gondar, Ethiopia; St Paul's Eye Unit (N Dervenis MD), Royal Liverpool University Hospital, Liverpool, UK; Department of Ophthalmology (N Dervenis MD), 1st Department of Ophthalmology (Prof F Topouzis PhD), Aristotle University of Thessaloniki, Thessaloniki, Greece; Department of Ophthalmology (Prof J P Deva MD), Universiti Tunku Abdul Rahman, Kajang, Malaysia; Center of Complexity Sciences (Prof D Diaz PhD), National Autonomous University of Mexico, Mexico City, Mexico; Faculty of Veterinary Medicine and Zootechnics (Prof D Diaz PhD), Autonomous University of Sinaloa, Culiacán Rosales, Mexico; Development of Research and Technology Center (S Djalalinia PhD), Ministry of Health and Medical Education, Tehran, Iran; School of Behavioural Sciences (R Elayedath MSc), Mahatma Gandhi University of Medical Sciences and Technology, Kottayam, India; National Eye Institute (L B Ellwein PhD), National Institute of Health, Bethesda, MD, USA; Ophthalmic Epidemiology Research Center (M Emamian PhD), Shahroud University of Medical Sciences, Shahroud, Iran; Department of Ophthalmology and Visual Sciences (A G Fernandes PhD), Federal University of São Paulo, São Paulo, Brazil; Institute of Gerontological Health Services and Nursing Research (F Fischer PhD), Ravensburg-Weingarten University of Applied Sciences, Weingarten, Germany; Division of Ophthalmology (J M Furtado MD), University of São Paulo, Ribeirão Preto, Brazil; Department of Medicine (S Gaidhane PhD), Global Evidence Synthesis Initiative (Prof M Khatib PhD), Department of Ophthalmology (Prof D Singhal MD), Datta Meghe Institute of Medical Sciences, Wardha, India; Institute of Ophthalmology (Prof G Gazzard MD), University College London, London, UK; School of Public Health (B Gebremichael MPH), Haramaya University, Harar, Ethiopia; Glaucoma Services (R George MS), Sankara Nethralaya Medical Research Foundation, Chennai, India; Faculty of Allied Health Sciences (Prof S Gilani PhD), The University of Lahore, Lahore, Pakistan; Afro-Asian Institute, Lahore, Pakistan (Prof S Gilani PhD); Health Systems and Policy Research (M Golechha PhD), Indian Institute of Public Health Gandhinagar, Gandhinagar, India; School of Health and Environmental Studies (Prof S Hamidi DrPH), Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates; Brain and Behavioral Sciences Program (Prof B R Hammond PhD), University of Georgia, Athens, GA, USA; Moran Eye Center (Prof M E R Hartnett MD), University of Utah, Salt Lake City, UT, USA; Sekolah Tinggi Ilmu Kesehatan Indonesia Maju (Indonesian Advanced College of Health Sciences) (R K Hartono MPH), Institution of Public Health Sciences, Jakarta, Indonesia; Department of Public Health (A Hashi PhD), Jigjiga University, Jijiga, Ethiopia; Institute of Pharmaceutical Sciences (K Hayat MS), University of Veterinary and Animal Sciences, Lahore, Pakistan; Department of Pharmacy Administration and Clinical Pharmacy (K Hayat MS), Xian Jiaotong University, Xian, China; Independent Consultant 4, Santa Clara, CA, USA (G Heidari MD); Department of Urban Planning and Design (H Ho PhD), University of Hong Kong, Hong Kong, China; Kasturba Medical College (R Holla MD, P Rathi MD), Manipal Academy of Higher Education, Manipal, India; College of Science and Engineering (Prof M Househ PhD), Hamad Bin Khalifa University, Doha, Qatar; Department of Ophthalmology and Visual Science (Prof J J Huang MD), Department of Genetics (S Pawar PhD), Yale University, New Haven, CT, USA; Department of Health Promotion and Education (S E Ibitoye MPH), Department of Medicine (Prof M O Owolabi DrM), University of Ibadan, Ibadan, Nigeria; Faculty of Medicine (I M Ilic PhD), University of Belgrade, Belgrade, Serbia; Department of Epidemiology (Prof M D Ilic PhD), University of Kragujevac, Kragujevac, Serbia; Independent Consultant 1, Kelowna, BC, Canada (A D Ingram MSc); Institute for Physical Activity and Nutrition (S M S Islam PhD), Deakin University, Burwood, VIC, Australia; Sydney Medical School (S M S Islam PhD), Ophthalmology Department (H Kandel PhD), University of Sydney, Sydney, NSW, Australia; Department of Health Management (R Itumalla PhD), University of Hail, Hail, Saudi Arabia; School of Management Studies (R Itumalla PhD), University of Hyderabad, Hyderabad, India; Department of Biochemistry (Prof S Jayaram MD), Government Medical College, Mysuru, India; Department of Community Medicine (R P Jha MSc), Dr. Baba Saheb Ambedkar Medical College & Hospital, Delhi, India; Department of Community Medicine (R P Jha MSc), Banaras Hindu University, Varanasi, India; Les Ophtalmologistes Associés de Monastir, Monastir, Tunisia (R Kahloun MD); Institute for Prevention of Non-communicable Diseases (R Kalhor PhD), Health Services Management Department (R Kalhor PhD), Qazvin University of Medical Sciences, Qazvin, Iran; Ophthalmology Department (H Kandel PhD), Sydney Local Health District, Sydney, NSW, Australia; Department of Applied Physics (Prof T Kavetskyy PhD), The John Paul II Catholic University of Lublin, Lublin Voivodeship, Poland; Department of Biology & Chemistry (Prof T Kavetskyy PhD), Drohobych Ivan Franko State Pedagogical University, Drohobych, Ukraine; International Research Center of Excellence (G A Kayode PhD), Institute of Human Virology Nigeria, Abuja, Nigeria; Julius Centre for Health Sciences and Primary Care (G A Kayode PhD), Utrecht University, Utrecht, Netherlands; Eye Unit (Prof J H Kempen MD), MyungSung Medical College, Addis Ababa, Ethiopia; Department of Ophthalmology (Prof M Khairallah MD), Fattouma Bourguiba University Hospital, Monastir, Tunisia; Department of Biophysics and Molecular Biology (Prof R Khalilov PhD), Baku State University, Baku, Azerbaijan; Institute of Radiation Problems (Prof R Khalilov PhD), Azerbaijan National Academy of Sciences, Baku, Azerbaijan; Department of Epidemiology and Biostatistics (E A Khan MPH), Health Services Academy, Islamabad, Pakistan; Allen Foster Community Eye Health Research Centre (R C Khanna MPH), L V Prasad Eye Institute, Hyderabad, India; School of Optometry and Vision Science (R C Khanna MPH, Prof K S Naidoo PhD, Prof K Pesudovs PhD, N Tahhan PhD, Prof S Resnikoff MD), UNSW, Sydney, NSW, Australia; Executive Board of the Health Ministers' Council for the Gulf Cooperation Council States, Riyadh, Saudi Arabia (Prof T A M Khoja FRCP); Department of Preventive Medicine (G R Kim PhD, Prof E Park PhD), Institute of Health Services Research (Prof E Park PhD), College of Medicine (Prof J Shin MD), Yonsei University, Seoul, South Korea; Department of Ophthalmology and Visual Sciences (J E Kim MD), Medical College of Wisconsin, Milwaukee, WI, USA; School of Traditional Chinese Medicine (Y J Kim PhD), Xiamen University Malaysia, Sepang, Malaysia; School of Health Sciences (Prof A Kisa PhD), Kristiania University College, Oslo, Norway; Global Community Health and Behavioral Sciences (Prof A Kisa PhD), Tulane University, New Orleans, LA, USA; Department of Nursing and Health Promotion (S Kisa PhD), Oslo Metropolitan University, Oslo, Norway; Independent Consultant 2, Jakarta, Indonesia (S Kosen MD); Biomedical Research Networking Center for Mental Health Network (A Koyanagi MD), San Juan de Dios Sanitary Park, Sant Boi de Llobregat, Spain; Catalan Institution for Research and Advanced Studies (ICREA), Barcelona, Spain (A Koyanagi MD); Faculty of Medicine (B Kucuk Bicer PhD), Gazi University, Ankara, Turkey; Department of Community Medicine (V Kulkarni MD), Manipal Academy of Higher Education, Mangalore, India; Faculty of Health and Life Sciences (O P Kurmi PhD), Coventry University, Coventry, UK; Department of Medicine (O P Kurmi PhD), Department of Psychiatry and Behavioural Neurosciences (A T Olagunju MD), McMaster University, Hamilton, ON, Canada; Unit of Genetics and Public Health (Prof I Landires MD), Unit of Microbiology and Public Health (V Nunez-Samudio PhD), Institute of Medical Sciences, Las Tablas, Panama; Department of Public Health (V Nunez-Samudio PhD), Ministry of Health, Herrera, Panama (Prof I Landires MD); HelpMeSee, New York, NY, USA (Prof V C Lansingh PhD); Mexican Institute of Ophthalmology, Queretaro, Mexico (Prof V C Lansingh PhD); College of Optometry (J L Leasher OD), Nova Southeastern University, Fort Lauderdale, FL, USA; Ophthalmology Department (N Leveziel MD), CHU de Poitiers, Poitiers, France; Unité 1084 (N Leveziel MD), National Institute of Health and Medical Research (INSERM), Poitiers, France; Health Information Services, Grootebroek, Netherlands (H Limburg MPH); Department of Biochemistry (S Madhava Kunjathur MD), BGS Global Institute of Medical Sciences, Bengaluru, India; Clinical Research Development Center (S Maleki MSc, M Naderi PhD), Kermanshah University of Medical Sciences, Kermanshah, Iran; School of Medicine (N Manafi MD), University of Manitoba, Winnipeg, MB, Canada; Swiss Visio, Montchoisi Clinic (Prof K Mansouri MD), Glaucoma Research Center, Lausanne, Switzerland; Department of Ophthalmology (Prof K Mansouri MD), University of Colorado, Denver, Denver, USA; Department of Ophthalmology (C McAlinden PhD), Singleton Hospital, Swansea, UK; School of Public Health (G G Meles MPH), Mekelle University, Mekelle, Ethiopia; Department of Nursing (A M Mersha MSc), Department of Public Health (M B Sorrie MPH), Department of Biomedical Sciences (E G Tadesse MSc), Arba Minch University, Arba Minch, Ethiopia; Woman-Mother-Child Department (I Michalek PhD), Lausanne University Hospital, Lausanne, Switzerland; Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); School of Public Health (T R Miller PhD), Curtin University, Perth, WA, Australia; Internal Medicine Department (Y Mohammad MD), King Saud University, Riyadh, Saudi Arabia; Department of Public Health (J A Mohammed MPH, T G Wondmeneh MPH), Samara University, Samara, Ethiopia; World Health Organization (WHO) Centre on eHealth, Sydney, NSW, Australia (M Moni PhD); Department of Medicine (A A Montasir FMD), TMSS Medical College, Bogura, Bangladesh; Department of Medicine (A A Montasir FMD), Sofia Ismail Memorial Medical Centre, Bogura, Bangladesh; Lighthouse Guild, New York, NY, USA (A R Morse PhD); Harkness Eye Institute (A R Morse PhD), Columbia University, New York, NY, USA; Department of Public Health (G F Mulaw MPH), Woldia University, Woldia, Ethiopia; Department of Orgonomy (H Naderifar PhD), Hamadan University of Medical Sciences, Hamadan, Iran; Discipline of Optometry (Prof K S Naidoo PhD), University of KwaZulu-Natal, Durban, South Africa; Laboratory of Public Health Indicators Analysis and Health Digitalization (M Naimzada MD, N Otstavnov BA), Moscow Institute of Physics and Technology, Dolgoprudny, Russia; Experimental Surgery and Oncology Laboratory (M Naimzada MD), Kursk State Medical University, Kursk, Russia; Suraj Eye Institute, Nagpur, India (V Nangia MD); Mysore Medical College and Research Institute (Prof S Narasimha Swamy MD), Government Medical College, Mysore, India; Department of Biotechnology (D M Naveed PhD), University of Central Punjab, Lahore, Pakistan; Institute for Global Health Innovations (H L T Nguyen MPH, H Q Pham MD), Duy Tan University, Hanoi, Vietnam; Translational Health Research Institute (F A Ogbo PhD), Western Sydney University, Sydney, NSW, Australia; Policy and Programme Systems (K Ogundimu MD), Sightsavers, Haywards Heath, UK; Department of Psychiatry (A T Olagunju MD), University of Lagos, Lagos, Nigeria; Department of Pharmacology and Therapeutics (Prof O E Onwujekwe PhD), University of Nigeria Nsukka, Enugu, Nigeria; Department of Medicine (Prof M O Owolabi DrM), University College Hospital, Ibadan, Ibadan, Nigeria; Department of Parasitology and Mycology (Prof K Pakshir PhD), Shiraz University of Medical Sciences, Shiraz, Iran; Department of Forensic Medicine & Toxicology (U Parekh MD), Pramukhswami Medical College, Anand, India; Centre for Public Health (Prof T Peto PhD), Queen's University Belfast, Belfast, UK; Medical College (V Podder HSC), Tairunnessa Memorial Medical College and Hospital, Gazipur, Bangladesh; Department of Community Medicine (M Rahman PhD), Maharishi Markandeshwar Medical College & Hospital, Solan, India; Department of Ophthalmology (P Y Ramulu MD, Prof S K West PhD), Wilmer Eye Institute (A L Robin MD), Johns Hopkins University, Baltimore, MD, USA; University College London Hospitals, London, UK (D L Rawaf MD); Academic Public Health England (Prof S Rawaf MD), Public Health England, London, UK; School of Health, Medical and Applied Sciences (L Rawal PhD), CQ University, Sydney, NSW, Australia; School of Social Sciences and Psychology (Prof A M N Renzaho PhD), Translational Health Research Institute (Prof A M N Renzaho PhD), Western Sydney University, Penrith, NSW, Australia; Department of Ophthalmology (Prof L Rossetti MD), University of Milan, Milano, Italy; Halal Research Center (A Sahebkar PhD), Food and Drug Administration of the Islamic Republic of Iran, Tehran, Iran; Neurogenic Inflammation Research Center (A Sahebkar PhD), Mashhad University of Medical Sciences, Mashhad, Iran; Department of Entomology (A M Samy PhD), Ain Shams University, Cairo, Egypt; Department of Geriatrics and Long Term Care (B Sathian PhD), Hamad Medical Corporation, Doha, Qatar; Faculty of Health & Social Sciences (B Sathian PhD), Bournemouth University, Bournemouth, UK; Department of Preventive and Social Medicine (G Saya MD), Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India; Market Access (M Saylan MD), Bayer, Istanbul, Turkey; Public Health Division (A A Shaheen PhD), An-Najah National University, Nablus, Palestine; Independent Consultant 3, Karachi, Pakistan (M A Shaikh MD); Institute for Population Health (Prof K Shibuya MD), King's College London, London, UK; Department of Nursing (W S Shiferaw MSc), Debre Berhan University, Debre Berhan, Ethiopia; National Institute of Infectious Diseases, Tokyo, Japan (M Shigematsu PhD); Family, Health Promotion, and Life Course Department (J Silva MPH), Pan American Health Organization, Washington, DC, USA; Ophthalmology Department (A Silvester MSc), SpaMedica, Bolton, UK; School of Medicine (Prof J A Singh MD), University of Alabama at Birmingham, Birmingham, AL, USA; Medicine Service (Prof J A Singh MD), US Department of Veterans Affairs (VA), Birmingham, AL, USA; Department of Ophthalmology (Prof D Singhal MD), Gmers Medical College and Civil Hospital, Ahmedabad, India; Department of Ophthalmology (Prof R S Sitorus PhD), University of Indonesia, Jakarta, Indonesia; Department of Ophthalmology (Prof R S Sitorus PhD), Cipto Mangunkusumo National Hospital, Jakarta, Indonesia; Department of Ophthalmology (E Skiadaresi MD), Hywel Dda University Health Board, Llanelli, UK; Department No.16 (V Y Skryabin MD), Laboratory of Genetics and Genomics (Prof M S Zastrozhin PhD), Moscow Research and Practical Centre on Addictions, Moscow, Russia; Therapeutic Department (A A Skryabina MD), Balashiha Central Hospital, Balashikha, Russia; Nursing Care Research Center (A Soheili PhD), Semnan University of Medical Sciences, Semnan, Iran; Division of Community Medicine (C T Sreeramareddy MD), International Medical University, Kuala Lumpur, Malaysia; Department of Ophthalmology (Prof D Stambolian MD), University of Pennsylvania, Philadelphia, PA, USA; Department of Population Science and Human Resource Development (Prof M I Tareque PhD), University of Rajshahi, Rajshahi, Bangladesh; Department of Health Economics (B X Tran PhD), Hanoi Medical University, Hanoi, Vietnam; Medical School (Prof M K Tsilimbaris MD), University of Crete, Heraklion, Greece; Southern California Eye Institute, Los Angeles, CA, USA (R Varma MD); NEUROFARBA Dipartimento di Neuroscienze, Psicologia, Area del Farmaco e Salute del Bambino (G Virgili MD), University of Florence, Florence, Italy; Center of Excellence in Behavioral Medicine (G T Vu BA), Nguyen Tat Thanh University, Ho Chi Minh City, Vietnam; Singapore Eye Research Institute (Prof T Y Wong MD), Singapore National Eye Centre, Singapore, Singapore; Department of Neuropsychopharmacology (N Yonemoto MPH), National Center of Neurology and Psychiatry, Kodaira, Japan; Department of Public Health (N Yonemoto MPH), Juntendo University, Tokyo, Japan; Department of Epidemiology and Biostatistics (Prof C Yu PhD), School of Medicine (Z Zhang PhD), Wuhan University, Wuhan, China; Addictology Department (Prof M S Zastrozhin PhD), Pediatrics Department (A Zastrozhina PhD), Russian Medical Academy of Continuous Professional Education, Moscow, Russia; Brien Holden Vision Institute, Sydney, NSW, Australia (Prof S Resnikoff MD).
Declaration of interests
A M Bron reports personal fees from Aerie, Allergan, Bausch & Lomb, Santen, and Théa, outside the submitted work. D S Friedman reports personal fees from W L Gore, Bausch & Lomb, Life Biosciences, and Théa, outside the submitted work. G Gazzard reports grants from National Institute for Health Research (NIHR) Health Technology Assessment (HTA); personal fees, non-financial support and speaker fees, honoraria, and consulting fees from Alcon, Allergan, Bausch & Lomb, Belkin, Ellex, Equinox Genentech, Glaukos, Haag-Streit, Ivantis, Lumenis, McKinsey, Santen, Sight Science, and Théa; personal fees, non-financial support and membership on an advisory panel, committee and board of directors from Allergan, Belkin, Equinox Genentech, Glaukos, Ivantis, McKinsey, Santen, Sight Science, and Théa; and participation in clinical trial from Hydrus & Preserflo trials, outside the submitted work. M E R Hartnett reports grants from the National Eye Institute and grants from the National Institutes of Health (NIH), outside the submitted work. S M S Islam reports grants from the National Health and Medical Research Council and from the National Heart Foundation of Australia, outside the submitted work. J H Kempen Kempen reports equity ownership with Betaliq and personal fees from Gilead, outside the submitted work. K S Naidoo is employed by Essilor—an optical company. P Y Ramulu reports grants from the NIH and personal fees from Aerie Pharmaceuticals, W L Gore, Théa, and Ivantis, outside the submitted work. J A Singh reports having received personal fees from Crealta/Horizon, Medisys, Fidia, UBM LLC, Trio health, Medscape, WebMD, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, Practice Point communications, NIH, the American College of Rheumatology, and Simply Speaking; owning stock from Amarin, Viking, Moderna, Vaxart pharmaceuticals, and Charlotte's Web Holdings; and having received non-financial support from FDA Arthritis Advisory Committee, from Steering committee of OMERACT (an international organisation that develops measures for clinical trials and receives arm's length funding from 12 pharmaceutical companies), from Veterans Affairs Rheumatology Field Advisory Committee, and from the Editor and the Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis, outside the submitted work. F Topouzis reports grants from Pfizer, Théa, Novartis, Rheon, Omikron, Pharmaten, Bayer, and Bausch & Lomb; and personal fees from Novartis and Omikron; outside the submitted work. M K Tsilimbaris reports grants from Novartis Hellas, Bayer Hellas, Mavrogenis, Allergan Hellas, and Johnson & Johnson; personal fees from Novartis Hellas, Bayer Hellas, and Allergan Hellas; and non-financial support from Novartis Hellas, Alcon Hellas, Bayer Hellas, Mavrogenis, and Allergan Hellas.
Contributor Information
GBD 2019 Blindness and Vision Impairment Collaborators:
Jaimie D Adelson, Rupert R A Bourne, Paul Svitil Briant, Seth R Flaxman, Hugh R B Taylor, Jost B Jonas, Amir Aberhe Abdoli, Woldu Aberhe Abrha, Ahmed Abualhasan, Eman Girum Abu-Gharbieh, Tadele Girum Adal, Ashkan Afshin, Hamid Ahmadieh, Wondu Alemayehu, Sayyed Amirpooya Samir Alemzadeh, Ahmed Samir Alfaar, Vahid Alipour, Sofia Androudi, Jalal Arabloo, Aries Berhe Arditi, Brhane Berhe Aregawi, Alessandro Arrigo, Charlie Ashbaugh, Elham Debalkie Ashrafi, Desta Debalkie Atnafu, Eleni Amin Bagli, Atif Amin Winfried Baig, Till Winfried Bärnighausen, Maurizio Battaglia Parodi, Mahya Srikanth Beheshti, Akshaya Srikanth Bhagavathula, Nikha Bhardwaj, Pankaj Bhardwaj, Krittika Bhattacharyya, Ali Bijani, Mukharram Bikbov, Michele Bottone, Tasanee M Braithwaite, Alain M Bron, Sharath A Burugina Nagaraja, Zahid A Butt, Florentino Luciano L Caetano dos Santos, Vera L James Carneiro, Robert James Casson, Ching-Yu Jasmine Cheng, Jee-Young Jasmine Choi, Dinh-Toi Chu, Maria Vittoria M Cicinelli, João M G Coelho, Nathan G A Congdon, Rosa A A Couto, Elizabeth A M Cromwell, Saad M Dahlawi, Xiaochen Dai, Reza Dana, Lalit Dandona, Rakhi A Dandona, Monte A Del Monte, Meseret Derbew Molla, Nikolaos Alemayehu Dervenis, Abebaw Alemayehu P Desta, Jenny P Deva, Daniel Diaz, Shirin E Djalalinia, Joshua R Ehrlich, Rajesh Rashad Elayedath, Hala Rashad B Elhabashy, Leon B Ellwein, Mohammad Hassan Emamian, Sharareh Eskandarieh, Farshad G Farzadfar, Arthur G Fernandes, Florian S Fischer, David S M Friedman, João M Furtado, Shilpa Gaidhane, Gus Gazzard, Berhe Gebremichael, Ronnie George, Ahmad Ghashghaee, Syed Amir Gilani, Mahaveer Golechha, Samer Randall Hamidi, Billy Randall R Hammond, Mary Elizabeth R Kusuma Hartnett, Risky Kusuma Hartono, Abdiwahab I Hashi, Simon I Hay, Khezar Hayat, Golnaz Heidari, Hung Chak Ho, Ramesh Holla, Mowafa J Househ, John J Emmanuel Huang, Segun Emmanuel M Ibitoye, Irena M D Ilic, Milena D D Ilic, April D Naghibi Ingram, Seyed Sina Naghibi Irvani, Sheikh Mohammed Shariful Islam, Ramaiah Itumalla, Shubha Prakash Jayaram, Ravi Prakash Jha, Rim Kahloun, Rohollah Kalhor, Himal Kandel, Ayele Semachew Kasa, Taras A Kavetskyy, Gbenga A H Kayode, John H Kempen, Moncef Khairallah, Rovshan Ahmad Khalilov, Ejaz Ahmad C Khan, Rohit C Khanna, Mahalaqua Nazli Ahmed Khatib, Tawfik Ahmed E Khoja, Judy E Kim, Yun Jin Kim, Gyu Ri Kim, Sezer Kisa, Adnan Kisa, Soewarta Kosen, Ai Koyanagi, Burcu Kucuk Bicer, Vaman P Kulkarni, Om P Kurmi, Iván Charles Landires, Van Charles L Lansingh, Janet L E Leasher, Kate E LeGrand, Nicolas Leveziel, Hans Limburg, Xuefeng Liu, Shilpashree Madhava Kunjathur, Shokofeh Maleki, Navid Manafi, Kaweh Mansouri, Colm Gebremichael McAlinden, Gebrekiros Gebremichael M Meles, Abera M Mersha, Irmina Maria R Michalek, Ted R Miller, Sanjeev Misra, Yousef Mohammad, Seyed Farzad Abdu Mohammadi, Jemal Abdu H Mohammed, Ali H Mokdad, Mohammad Ali Al Moni, Ahmed Al R Montasir, Alan R Fentaw Morse, Getahun Fentaw C Mulaw, Mehdi Naderi, Homa S Naderifar, Kovin S Naidoo, Mukhammad David Naimzada, Vinay Nangia, Sreenivas Muhammad Narasimha Swamy, Dr Muhammad Naveed, Hadush Lan Negash, Huong Lan Nguyen, Virginia Akpojene Nunez-Samudio, Felix Akpojene Ogbo, Kolawole T Ogundimu, Andrew T E Olagunju, Obinna E Onwujekwe, Nikita O Otstavnov, Mayowa O Owolabi, Keyvan Pakshir, Songhomitra Panda-Jonas, Utsav Parekh, Eun-Cheol Park, Maja Pasovic, Shrikant Pawar, Konrad Pesudovs, Tunde Quang Peto, Hai Quang Pham, Marina Pinheiro, Vivek Podder, Vafa Rahimi-Movaghar, Mohammad Hifz Ur Y Rahman, Pradeep Y Ramulu, Priya Rathi, Salman Laith Rawaf, David Laith Rawaf, Lal Rawal, Nickolas M Reinig, Andre M Renzaho, Aziz L Rezapour, Alan L Robin, Luca Rossetti, Siamak Sabour, Sare Safi, Amirhossein Sahebkar, Mohammad Ali M Sahraian, Abdallah M Samy, Brijesh Sathian, Ganesh Kumar Saya, Mete A Saylan, Amira A Ali Shaheen, Masood Ali T Shaikh, Tueng T Shen, Kenji Shibabaw Shibuya, Wondimeneh Shibabaw Shiferaw, Mika Shigematsu, Jae Il Shin, Juan Carlos Silva, Alexander A Silvester, Jasvinder A Singh, Deepika S Singhal, Rita S Sitorus, Eirini Yurievich Skiadaresi, Valentin Yurievich Aleksandrovna Skryabin, Anna Aleksandrovna Skryabina, Amin Bekele Soheili, Muluken Bekele A R C Sorrie, Raúl A R C T Sousa, Chandrashekhar T Sreeramareddy, Dwight Girma Stambolian, Eyayou Girma Tadesse, Nina Ismail Tahhan, Md Ismail Tareque, Fotis Xuan Topouzis, Bach Xuan Tran, Gebiyaw K Tsegaye, Miltiadis K Tsilimbaris, Rohit Varma, Gianni Virgili, Avina Thu Vongpradith, Giang Thu Vu, Ya Xing Wang, Ningli Hailay Wang, Abrha Hailay K Weldemariam, Sheila K Gebeyehu West, Temesgen Gebeyehu Y Wondmeneh, Tien Y Wong, Mehdi Yaseri, Naohiro Yonemoto, Chuanhua Sergeevich Yu, Mikhail Sergeevich Zastrozhin, Zhi-Jiang R Zhang, Stephanie R Zimsen, Serge Resnikoff, and Theo Vos
Supplementary Material
References
- 1.Flaxman SR, Bourne RRA, Resnikoff S. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234. doi: 10.1016/S2214-109X(17)30393-5. [DOI] [PubMed] [Google Scholar]
- 2.Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. 1971. Milbank Q. 2005;83:731–757. doi: 10.1111/j.1468-0009.2005.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pezzullo L, Streatfeild J, Simkiss P, Shickle D. The economic impact of sight loss and blindness in the UK adult population. BMC Health Serv Res. 2018;18:63. doi: 10.1186/s12913-018-2836-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reddy PA, Congdon N, MacKenzie G. Effect of providing near glasses on productivity among rural Indian tea workers with presbyopia (PROSPER): a randomised trial. Lancet Glob Health. 2018;6:e1019–e1027. doi: 10.1016/S2214-109X(18)30329-2. [DOI] [PubMed] [Google Scholar]
- 5.Horton S, Gelband H, Jamison D, Levin C, Nugent R, Watkins D. Ranking 93 health interventions for low- and middle-income countries by cost-effectiveness. PLoS One. 2017;12 doi: 10.1371/journal.pone.0182951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–1678. doi: 10.1016/j.ophtha.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Tahhan N, Papas E, Fricke TR, Frick KD, Holden BA. Utility and uncorrected refractive error. Ophthalmology. 2013;120:1736–1744. doi: 10.1016/j.ophtha.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 8.WHO . World Health Organization; Geneva: 2013. Universal eye health: a global action plan 2014–2019.http://www.who.int/blindness/actionplan/en/ [Google Scholar]
- 9.Bourne RRA, Flaxman SR, Braithwaite T. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 10.WHO . World Health Organization; Geneva: 2019. World report on vision.https://www.who.int/publications-detail-redirect/world-report-on-vision [Google Scholar]
- 11.Jonas JB, Wang YX, Xu L, Wei WB. Age-related macular degeneration in China: a population-based and clinical study. Lancet. 2018;392:S86. [Google Scholar]
- 12.Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157:9–25.e12. doi: 10.1016/j.ajo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–2090. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Wong WL, Su X, Li X. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–e116. doi: 10.1016/S2214-109X(13)70145-1. [DOI] [PubMed] [Google Scholar]
- 15.Stevens GA, Alkema L, Black RE. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 16.Bourne RRA, Adelson J, Flaxman S. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2020 doi: 10.1016/S2214-109X(20)30425-3. published online Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zheng P, Aravkin AY, Barber R, Sorensen RJD, Murray CJL. Trimmed constrained mixed effects models: formulations and algorithms. ArXiv190910700 Math Stat. 2019 http://arxiv.org/abs/1909.10700 published online Sept 23. [Google Scholar]
- 18.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehta MC, Narayanan R, Thomas Aretz H, Khanna R, Rao GN. The L V Prasad Eye Institute: a comprehensive case study of excellent and equitable eye care. Healthc (Amst) 2020;8 doi: 10.1016/j.hjdsi.2019.100408. [DOI] [PubMed] [Google Scholar]
- 20.Bourne RRA, Dineen BP, Ali SM, Huq DMN, Johnson GJ. Outcomes of cataract surgery in Bangladesh: results from a population based nationwide survey. Br J Ophthalmol. 2003;87:813–819. doi: 10.1136/bjo.87.7.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He M, Zheng Y, Xiang F. Prevalence of myopia in urban and rural children in mainland China. Optom Vis Sci. 2009;86:40–44. doi: 10.1097/OPX.0b013e3181940719. [DOI] [PubMed] [Google Scholar]
- 22.Hernández RA, Burr JM, Vale LD. Economic evaluation of screening for open-angle glaucoma. Int J Technol Assess Health Care. 2008;24:203–211. doi: 10.1017/S0266462308080288. [DOI] [PubMed] [Google Scholar]
- 23.Garway-Heath DF, Crabb DP, Bunce C. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–1304. doi: 10.1016/S0140-6736(14)62111-5. [DOI] [PubMed] [Google Scholar]
- 24.Bloch SB, Larsen M, Munch IC. Incidence of legal blindness from age-related macular degeneration in Denmark: year 2000 to 2010. Am J Ophthalmol. 2012;153:209. doi: 10.1016/j.ajo.2011.10.016. 13.e2. [DOI] [PubMed] [Google Scholar]
- 25.Ogurtsova K, da Rocha Fernandes JD, Huang Y. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 26.Leasher JL, Bourne RRA, Flaxman SR. Global estimates on the number of people blind or visually impaired by diabetic retinopathy: a meta-analysis from 1990 to 2010. Diabetes Care. 2016;39:1643–1649. doi: 10.2337/dc15-2171. [DOI] [PubMed] [Google Scholar]
- 27.Yau JWY, Rogers SL, Kawasaki R. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teo ZL, Tham Y-C, Yu M, Cheng C-Y, Wong TY, Sabanayagam C. Do we have enough ophthalmologists to manage vision-threatening diabetic retinopathy? A global perspective. Eye (Lond) 2020;34:1255–1261. doi: 10.1038/s41433-020-0776-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong TY, Sun J, Kawasaki R. Guidelines on diabetic eye care: the International Council of Ophthalmology Recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–1622. doi: 10.1016/j.ophtha.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 30.WHO . World Health Organization; Geneva: 2020. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030.http://www.who.int/neglected_diseases/resources/who-ucn-ntd-2020.01/en/ [Google Scholar]
- 31.Bourne RRA, Jonas JB, Resnikoff S. Looking within rather than between countries to understand the risk factors for vision impairment. JAMA Ophthalmol. 2019;137:158–159. doi: 10.1001/jamaophthalmol.2018.5448. [DOI] [PubMed] [Google Scholar]
- 32.Ehrlich JR, Stagg BC, Andrews C, Kumagai A, Musch DC. Vision impairment and receipt of eye care among older adults in low- and middle-income countries. JAMA Ophthalmol. 2019;137:146–158. doi: 10.1001/jamaophthalmol.2018.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
More than ten authors have accessed and verified the data. To download the data used in these analyses, please visit the Global Health Data Exchange GBD 2019 website.