Abstract
There is growing evidence of the challenges with adherence to COVID-19 prevention measures and the effect of the prevention measures on the health of populations in various parts of the world but with limited documentation in sub-Saharan Africa. We assessed COVID-19 awareness, adoption of COVID-19 prevention measures, and the effects of COVID-19 lockdown on the mental health status, socio-economic disruptions and engagement in unhealthy behaviours among 2500 in- and out-of-school adolescent boys and young men (ABYM) aged 10–24 years in Kampala, Uganda. 74.8% (n = 1869) were in-school; nearly half (47.3%, n = 1182) were aged 15–19 years. Although > 80% were aware of at least two COVID-19 prevention measures, only 22.2% (n = 555) reported that they always wore a face mask while in a public place; 40.9% (n = 1023) always washed their hands with soap and running water while 17.6% (n = 440) always avoided gatherings of more than five people. COVID-19 lockdown led to: (a) increased mental health challenges (e.g. 1.2% [n = 31] contemplated committing suicide); (b) limited ability to meet basic needs (e.g. 62.0% [n = 1549] found it difficult to afford a diverse/balanced diet); (c) socio-economic disruptions (e.g. 30.3% [n = 756] experienced a reduction in income) and (d) engagement in unhealthy behaviours (e.g. 62% [n = 1554] reported a sedentary life style such as excessive watching of TV). These effects were more pronounced among older adolescent boys (15–19 years) and young men (20–24 years) and out-of-school compared to in-school ABYM. Our findings suggest a need for appropriate health promotion, mental health and socio-economic interventions targeting ABYM in Kampala, Uganda.
Keywords: COVID-19, Lockdown, Adolescent boys and young men, Kampala, Uganda
Background
Globally, there were 42,549,383 cumulative cases of COVID-19 by October 24, 2020 [1]. Of these, a cumulative total of 1,150,163 (2.7%) patients had died of the disease while 31,456,279 cases had recovered from the disease. Although earlier studies suggested that about 80% of those who died were over the age of 60 [2, 3], the World Health Organization (WHO) recognizes that people of all ages can be infected by the novel coronavirus. However, older people, and people with pre-existing medical conditions (such as asthma, diabetes, heart disease) appear to be more vulnerable to becoming severely ill and to die of COVID-19 than other at-risk populations.
While the virus was slow in reaching the African continent compared to other parts of the world, infection has grown exponentially in recent months and continues to spread throughout Africa. Africa’s first COVID-19 case was recorded in Egypt on February 14, 2020. By October 24, 2020, there were 1,696,285 cases of COVID-19 in Africa, with 40,922 (2.4%) deaths and 1,394,094 recoveries [4]. There are more cases of COVID-19 in the Southern Africa region contributing 788,070 (46.4%) of the cases, with the Eastern Africa region responsible for 201,216 cases (11.9%). Within the East Africa region, Ethiopia (92,229) has the highest number of cases followed by Kenya (47,843) with the lowest cases reported in Eritrea (461).
The first case of COVID-19 was reported in Uganda on March 21, 2020. The government of Uganda introduced up to 33 COVID-19 prevention measures to curb the spread of the pandemic including closure of schools, colleges and universities; prohibition of gatherings of 10 or more people; country-wide travel restrictions and a curfew running between 19:00 and 06:30 h, among other measures. A countrywide home confinement was announced on March 30, 2020 and remained in effect until June 26, 2020. The number of COVID-19 cases remained low between March and June 2020; however, when these measures were relaxed towards the end of June 2020, reported cases increased sharply: between 23 July and 19 August, Uganda saw an 88% average increase in the number of new cases reported each week, with the majority of new cases reported in Kampala [5]. By October 24, 2020, the cumulative number of COVID-19 cases was 11,163 with 99 (0.9%) deaths and 7269 recoveries. A majority of cases have been reported in Kampala, the Capital City of Uganda. By December 26, 2020, the cumulative number of cases in Kampala constituted up to 54% (n = 13,823) of the national caseload and of the cumulative number of people that have so far died of COVID-19 48.2% (n = 118) died in Kampala alone [6]. Nearly 70% of the cases reported in Kampala were local transmissions with up to 90% attributed to the use of public means of transport, including taxis [7].
By end of October 2020, several businesses had been opened and schools and tertiary teaching institutions reopened for candidate classes. However, some of the businesses, including bars and other hospitality establishments were yet to resume while several businesses were struggling financially. The informal sector workers are often hardest hit as reported elsewhere [8–10]. With a youth unemployment rate of 13% in Uganda [11] and 90.5% of the youth in Kampala engaged in the informal sector businesses, it is likely that COVID-19 lockdown could have had devastating effects on their incomes and general livelihoods. In this paper, we describe COVID-19 awareness, uptake of COVID-19 prevention measures, and the effects of COVID-19 lockdown on the mental health status, socio-economic disruptions and engagement in unhealthy behaviours among adolescent boys and young men aged 10–24 years in Kampala, Uganda.
Methods
Study Site
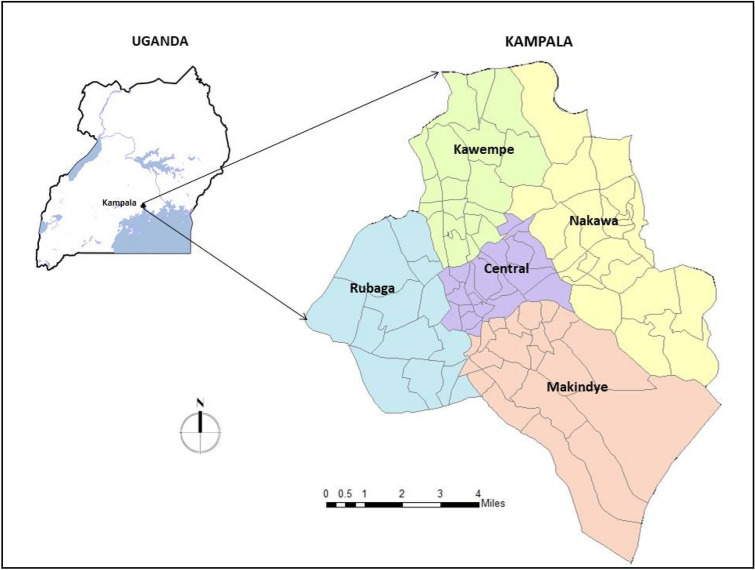
The questions analysed for this paper were embedded into a larger formative study conducted to assess the health status of adolescent boys and young men aged 10–24 years in Kampala, the Capital City of Uganda (Fig. 1). Kampala is located along the shores of Lake Victoria in the central region of Uganda and is administratively divided into five urban divisions, namely: Kawempe, Nakawa, Rubaga, Central and Makindye division. Kampala has a projected population of 1,650,800 according to the 2019 Uganda Bureau of Statistics (UBOS) Statistical Abstracts [12]. Of these, 47% (n = 781,700) are males. Adolescents and young people (both males and females) aged 10–24 years constitute 38.8% (n = 640,510) of Kampala’s total population. Given that 47% of Kampala’s population are males; we estimate that there were 301,040 adolescent boys and young men in Kampala in 2019.
Fig. 1.
Map of Kampala, showing the five divisions where the study was conducted
Study Design and Population
This was a cross-sectional study that was conducted among 2500 in- and out-of-school adolescent boys and young men aged 10–24 years, resident in the five urban divisions of Kampala, between July and August 2020.
Sample Size Determination
The sample size was determined using the formula suggested by Cochran 1977 [13]. Assuming a type-1 error of 5%, p = 0.14 (the proportion of adolescent boys that have ever used drugs in Kampala, Uganda [14]); a design effect of 2.0; a margin of error of 0.05, five divisions in Kampala and a non-response of 0.10, we estimated that we would need to enrol a minimum of 2060 ABYM. This sample size was adjusted to 2500 ABYM to ensure adequate numbers of interviews conducted within each division. We used probability proportionate to size to allocate the sample size to the five divisions (Table 1). In the absence of individualized data from Uganda Bureau of Statistics (UBOS) on ABYM 10–24 years, we used the proportion of the division’s total population out of the total population in Kampala as a proxy for the proportion of ABYM in the division. The sample size allocated to each division was distributed among in- and out-of-school ABYM using the percentage of children 6–12 years who were not in school, obtained from the UBOS National Population and Housing Census report [15].
Table 1.
Sample size allocation by division in Kampala, Uganda
| KCCA division | Population percentage out of total KCCA population (2014) | % not-in-school (6–12 years) in 2014 | Sample size allocation out of 2500 ABYM | N1 for ABYM not-in-school | N2 for ABYM in-school |
|---|---|---|---|---|---|
| Kawempe | 24.4 | 29.6 | 617 | 188 | 429 |
| Rubaga | 20 | 30.8 | 501 | 159 | 342 |
| Makindye | 15.6 | 30.2 | 405 | 132 | 273 |
| Central | 11.2 | 17.5 | 257 | 51 | 206 |
| Nakawa | 28.8 | 14.2 | 720 | 101 | 619 |
| Total | 2500 | 631 | 1869 |
Sampling Procedures
Selection of Wards and Cells in Each Urban Division
We used a multi-stage sampling technique to guide the selection of wards/parishes within each division and cells/villages within each ward/parish. Kampala is made up of 96 wards/parishes across the five divisions. During the first stage, we obtained a list of all wards/parishes within each division from the Division Town Clerks. We then purposely selected 50% of the wards/parishes in each division, for a total of 48 wards/parishes in all the five divisions (Table 2). During the second stage of sampling, we purposely selected 20% of the total number of cells/villages within each ward/parish using a random number generator. This exercise was done repeatedly until all the selected wards/parishes had been covered. During the third stage, we obtained a list of households within each cell/village from the area local leaders. From each cell/village, the total number of households needed to be included in the survey was determined by sampling proportionate to size.
Table 2.
Number of selected wards/parishes included in the study
| Division | Total number of wards/parishes | Number of wards/parishes selected for inclusion |
|---|---|---|
| 1. Rubaga | 13 | 7 |
| 2. Nakawa | 23 | 12 |
| 3. Makindye | 21 | 10 |
| 4. Kawempe | 19 | 9 |
| 5. Central division | 20 | 10 |
| Total | 96 | 48 |
Sampling Procedures
After selecting the households, we conducted a mini-census in each household and listed down the names, age and schooling status of all ABYM aged 10–24 years that were found in each household. Only one eligible ABYM (age 10–24 years, resident in the selected cell/village, and enrolled in a school within the division) was interviewed per household. If a household had more than one eligible in-school ABYM, we wrote their names of all eligible ABYM on pieces of paper, placed them in a box; churned thoroughly, and one paper was picked at random. The name of the ABYM on the selected piece of paper was then invited for interview. To be interviewed as in-school ABYM, a respondent had to have been a pupil or student in a pre-selected school within each division prior to the COVID-19 lockdown in March 2020. Lists of pre-selected schools per division were made available to the study team to guide them in making the right decision on who qualified to be interviewed as an in-school ABYM.
On the other hand, since out-of-school ABYM were less likely to be found at home at the time of the survey, we conducted a pre-study visit to each division to list the areas of location and/or types of occupation (such as garages, boda-boda [motorcycle taxi] stages, mobile traders, quarries, construction sites) that were likely to have a heavy presence of out-of-school ABYM aged 10–24 years within the same wards/parishes as those selected for in-school ABYM (Table 2). The number of areas of locations or occupation types varied by ward within each division, and the exact number of areas of location or occupation types per ward was determined pragmatically, while taking into consideration the need to balance out participants by socio-economic status and area of residence (e.g. slums, affluent areas and peri-urban locations). The identified locations and/or types of occupations were considered to constitute sampling lots with each ward/parish. Using Lot Quality Assurance Sampling (LQAS) methodology [16, 17], we enrolled a minimum of 19 respondents from each lot within a ward until the required number of out-of-school ABYM in each division was attained. Where the number of eligible respondents selected from each lot was deemed to fall below the number of ABYM needed in each division, the number of respondents per lot was adjusted upwards (> 19) to reach the needed sample size within the division. However, where the number of eligible respondents per lot was lower than 19, we interviewed all the respondents within the selected lot but over-sampled in the subsequent lots to balance out the number of out-of-school ABYM interviews for each division.
Data Collection Procedures and Methods
Data were collected through face-to-face interviews conducted by trained Research Assistants in the five divisions of Kampala while observing COVID-19 prevention measures. We used a pilot-tested questionnaire that was loaded on mobile phones enabled with Kobo collect; a data collection application. Data collection took place between July and August 2020. All Research Assistants had a minimum of a Bachelor’s degree with more than 5 years of field data collection experience. Data were collected on ABYM’s awareness of how COVID-19 is spread and prevented; uptake of COVID-19 prevention measures, and the effects of COVID-19 lockdown on ABYM’s mental health status, socio-economic disruptions and engagement in unhealthy behaviours.
Measurement of Variables
Awareness of COVID-19 was assessed using the question, ‘Have you heard of corona virus/COVID-19?’ If respondents indicated that they had ever heard of COVID-19, they were asked about how the novel coronavirus can be prevented from spreading from person to person. Respondents were then asked specific questions on how often (never, rarely, sometimes, always) they adopted the COVID-19 prevention measures. Specific questions were asked about the effects of COVID-19 lockdown on: (a) mental health status and various forms of depression (e.g. did the COVID-19 lockdown make you feel so sad that nothing could cheer you up?) including whether or not the lockdown led ABYM to contemplate committing suicide; (b) various forms of violence (e.g. due to COVID-19 lockdown, did you experience more of the following forms of violence—being punched, kicked or beaten up by peers or someone pressuring you to have sex through harassment, threats or tricks?); (c) access to basic needs (e.g. due to the effects of COVID-19 lockdown, did you find it more difficult to afford the price of food?); (d) socio-economic disruptions (e.g. with regard to your source of livelihood, did COVID-19 lockdown lead to loss of a job?); and (e) engagement in unhealthy behaviours (e.g. due to the effects of COVID-19 lockdown, did you engage in smoking or chewing tobacco much more than before?).
Data Analysis
We computed descriptive statistics to describe ABYM’s awareness of how COVID-19 is spread and prevented, their adoption of COVID-19 prevention measures, and effects of COVID-19 lockdown on ABYM’s mental health status and various forms of depression; socio-economic disruptions and engagement in unhealthy behaviours. Data are reported as frequencies and percentages, unless otherwise stated. Selected statistical comparisons were done using Chi Square tests. Data analysis was conducted using STATA (version 15).
Ethical Considerations
The study protocol was approved by the Higher Degrees Research and Ethics Committee of Makerere University School of Public Health (Protocol#: 757) and the Uganda National Council for Science and Technology (SS#: 5240). Written informed consent was sought from each of the individuals before participating in the survey. Parental consent was waived for emancipated minors (i.e. those below 18 years of age) who were married, had a child or catered for their own livelihood, as defined in the Uganda National Council for Science and Technology guidelines [18]. Consent from parents/guardians was sought for participants aged 10–17 years who were also asked to provide their own assent prior to participation in the survey.
Results
Respondents’ Characteristics
Table 3 shows the socio-demographic characteristics of the respondents. Of the 2,500 respondents, 74.8% (n = 1869) were in-school; 19.3% (n = 483) were aged 10–14 years; 47.3% (n = 1182) were aged 15–19 years while 33.4% (n = 835) were aged 20–24 years. Most of the respondents were living in Nakawa (28.8%, n = 720), Kawempe (24.7%, n = 617) and Rubaga (20.0%, n = 501) in that order with the Central Division having the lowest number of respondents (10.3%, n = 257).
Table 3.
Socio-demographic characteristics of adolescent boys and young men (10–24 years) in Kampala, Uganda
| Variable | In-school (n = 1869, %) |
Out-of-school (n = 631, %) | Total (N = 2500, %) |
|---|---|---|---|
| Age-group | |||
| 10–14 | 475 (25.4) | 8 (1.3) | 483 (19.3) |
| 15–19 | 983 (52.6) | 199 (31.5) | 1182 (47.3) |
| 20–24 | 411 (49.2) | 424 (50.8) | 835 (33.4) |
| Class at time of interview (n = 1869) | |||
| < P5 | 158 (8.5) | – | – |
| P6–P7 | 262 (14.0) | – | – |
| S1–S2 | 346 (18.5) | – | – |
| S3–S4 | 481 (25.7) | – | – |
| S5–S6 | 397 (21.2) | – | – |
| Tertiary/University | 225 (12.0) | – | – |
| Residence during school (n = 1869) | |||
| School | 437 (23.4) | – | – |
| Home | 1303 (69.7) | – | – |
| Hostel/Hall of residence | 129 (6.9) | – | – |
| Division | |||
| Central | 206 (11.0) | 51 (8.1) | 257 (10.3) |
| Kawempe | 429 (23.0) | 188 (29.8) | 617 (24.7) |
| Makindye | 273 (14.6) | 132 (20.9) | 405 (16.2) |
| Nakawa | 619 (33.1) | 101 (16.0) | 720 (28.8) |
| Rubaga | 342 (18.3) | 159 (25.2) | 501 (20.0) |
Awareness of COVID-19 Prevention Measures
Table 4 shows the proportion of respondents who were aware of how COVID-19 is spread and prevented and the proportion of respondents who practiced the recommended COVID-19 prevention measures. All respondents regardless of schooling status or age-group had ever heard of COVID-19. Nearly three-quarters (74.9%, n = 1872) of the respondents were aware that the new coronavirus is spread through sneezing or coughing (droplet infection); 72.1% (n = 1802) were aware that the virus is spread through human-to-human contact while 52.4% (n = 266) were aware that the virus is spread through contact with contaminated surfaces.
Table 4.
Awareness of COVID-19 spread and prevention and uptake of COVID-19 prevention measures, stratified by schooling status
| Variable | In-school (n = 1869, %) |
Out-of-school (n = 631, %) | Total (N = 2500, %) |
|---|---|---|---|
| Have you ever heard of the coronavirus/COVID-19? (Yes) | 1869 (100.0) | 631 (100.0) | 2500 (100.0) |
| How is the coronavirus spread? | |||
| Through sneezing or coughing (droplet infection) | 1370 (73.3) | 502 (79.6) | 1872 (74.9) |
| Human-to-human contact | 1350 (72.3) | 452 (71.6) | 1802 (72.1) |
| Contact with contaminated surfaces | 965 (51.7) | 345 (54.7) | 1310 (52.4) |
| Other transmission routes | 214 (11.5) | 52 (8.2) | 266 (10.6) |
| How can you prevent COVID-19? | |||
| Handwashing with soap and water | 1570 (84.0) | 567 (89.9) | 2137 (85.5) |
| Use of a hand sanitizer | 1025 (54.9) | 328 (52.0) | 1063 (42.5) |
| Sneezing through a bent elbow | 482 (25.8) | 167 (26.5) | 649 (26.0) |
| Wearing a face mask | 1613 (86.3) | 536 (84.9) | 2149 (86.0) |
| Social distancing | 1328 (71.1) | 431 (68.3) | 1759 (70.4) |
| Avoid touching mouth, eyes, nose with unwashed hands | 422 (22.6) | 119 (18.9) | 541 (21.6) |
| How often do you wear a face mask when in a public place? | |||
| Never | 154 (8.2) | 56 (8.9) | 210 (8.4) |
| Rarely | 505 (27.0) | 169 (26.8) | 674 (27.0) |
| Sometimes | 786 (42.1) | 274 (43.4) | 1060 (42.4) |
| Always | 423 (22.6) | 132 (20.9) | 555 (22.2) |
| How often do you sanitize your hands with an alcohol-based hand rub? | |||
| Never | 169 (9.0) | 73 (11.6) | 242 (9.7) |
| Rarely | 525 (28.1) | 198 (31.4) | 723 (28.9) |
| Sometimes | 751 (40.2) | 232 (36.8) | 983 (39.3) |
| Always | 423 (22.6) | 128 (20.3) | 551 (22.0) |
| How often do you wash your hands with soap and running water? | |||
| Never | 31 (1.7) | 7 (1.1) | 38 (1.5) |
| Rarely | 233 (12.5) | 96 (15.2) | 329 (13.2) |
| Sometimes | 822 (44.0) | 287 (45.5) | 1109 (44.4) |
| Always | 782 (41.9) | 241 (38.2) | 1023 (40.9) |
| How often do you cover your mouth with a bent elbow when you cough or sneeze? | |||
| Never | 413 (22.1) | 158 (25.0) | 571 (22.8) |
| Rarely | 476 (25.5) | 169 (26.8) | 645 (25.8) |
| Sometimes | 571 (30.6) | 202 (32.0) | 773 (30.9) |
| Always | 408 (21.8) | 102 (16.2) | 510 (20.4) |
| How often do you avoid gatherings of more than 5 people? | |||
| Never | 413 (22.1) | 163 (25.8) | 576 (23.0) |
| Rarely | 429 (23.0) | 138 (21.9) | 567 (22.7) |
| Sometimes | 679 (36.3) | 237 (37.6) | 916 (36.7) |
| Always | 347 (18.6) | 93 (14.7) | 440 (17.6) |
Awareness of COVID-19 prevention measures varied according to the measure being explored. Eighty-six per cent (n = 2137) of the respondents were aware that hand-washing with soap and running water could prevent the acquisition or spread of the novel coronavirus, with a similar percentage reporting that wearing a face mask in public places was equally important. Seventy per cent (n = 1759) reported that COVID-19 can be prevented through social distancing (i.e. maintaining a physical distance of up to 2 m between people and reducing the number of times people come into close contact with each other). However, only 42.5% (n = 1063) of the respondents were aware that use of an alcohol-based hand-sanitizer was one of the preventive measures and 26% were aware that sneezing through a bent elbow was one of the COVID-19 prevention measures. Only 22% (n = 541) reported that avoiding touching the mouth, eyes and nose with unwashed hands was a COVID-19 prevention measure. However, a slightly higher proportion of in-school (22.6%, n = 422) than out-of-school respondents (18.9%, n = 119) were aware that not touching the mouth, eyes and nose with contaminated hands was protective against the spread of COVID-19.
Uptake of COVID-19 Prevention Measures
We found low uptake of COVID-19 prevention measures despite a high level of awareness of prevention measures. For instance, only 22.2% (n = 555) of the respondents reported that they always used a face mask in a public place. When these results were stratified by age-group, the proportion of ABYM who always used a face mask in a public place increased with increasing age; 17% (n = 82) among those aged 10–14 years; 19.6% (n = 232) among the 15–19 year-olds and 28.9% (n = 241) among those aged 20–24 year-olds. Only 22% (n = 551) of the respondents reported that they always used an alcohol-based hand rub while 40.9% (n = 1023) reported that they always washed their hands with soap and running water. There was no significant difference between in-school and out-of-school ABYM with regard to hand-washing with soap and running water as a COVID-19 prevention measure (Risk Ratio [RR] = 1.04; 95% Confidence Interval [95%CI] 0.99, 1.09). Only 20.4% (n = 510) of the respondents reported that they always cover their mouth with a bent elbow while coughing or sneezing, while 17.6% (n = 440) always avoid gatherings of more than five people as a COVID-19 prevention measure.
Effect of COVID-19 Lockdown on the Mental Health Status and Various Forms of Depression and Violence
Table 5 shows the effect of COVID-19 lockdown on the mental health status and various forms of depression and violence among ABYM in Kampala. Overall, 70.3% (n = 1758) reported that they felt more nervous as a result of COVID-19 lockdown than ever before with those out-of-school reporting higher levels of nervousness (77.5%, n = 489) than those that were in-school (67.9%, n = 1269). Sixty-three per cent (n = 1575) of the respondents reported that they felt so sad that nothing could cheer them up while 55.7% (n = 1392) reported that they felt more hopeless as a result of COVID-19 lockdown than ever before. In general, out-of-school ABYM reported higher levels of each condition than their in-school counterparts. When we stratified these results by age-group, we observed that older adolescent boys and young men seemed to report higher levels of each condition than their younger counterparts (Fig. 2). For instance, the proportion of ABYM who felt so sad that nothing could cheer them up was 56.5% (n = 273) among 10–14 year-olds, 63.3% (n = 747) among those aged 15–19 years, and 66.5% (n = 555) among those aged 20–24 years. Similarly, the proportion that felt nervous was 59.8% (n = 289) among those aged 10–14 years, 69.4% (n = 820) among those aged 15–19 years, and 77.7% (n = 649) among those aged 20–24 years.
Table 5.
Effects of COVID-19 lockdown on psychological wellbeing, various forms of violence and depression, and access to basic needs
| Effects of COVID-19 lockdown | In-school (n = 1869, %) | Out-of-school (n = 631, %) | Total (N = 2500, %) |
|---|---|---|---|
| Did COVID-19 lockdown make you feel more of the following psychological conditions? (Yes) | |||
| Nervousness | 1269 (67.9) | 489 (77.5) | 1758 (70.3) |
| Hopelessness | 983 (52.6) | 409 (64.8) | 1392 (55.7) |
| Feeling so sad that nothing could cheer you up | 1134 (60.7) | 441 (69.9) | 1575 (63.0) |
| Worthless | 649 (34.7) | 323 (51.2) | 972 (38.9) |
| Due to COVID-19 lockdown, did you experience more of the following forms of depression or violence? (Yes) | |||
| Various forms of depression | |||
| Someone telling you that you are not loved | 165 (8.8) | 88 (13.9) | 253 (10.1) |
| Someone wishing you were dead or had never been born | 64 (3.4) | 33 (5.2) | 97 (3.9) |
| Contemplate committing suicide | 18 (1.0) | 13 (2.1) | 31 (1.2) |
| Various forms of violence | |||
| Being punched, kicked, or beaten up by your peers | 151 (8.1) | 48 (7.6) | 199 (8.0) |
| Being punched, kicked, or beaten up by your intimate partner | 15 (0.8) | 14 (2.2) | 29 (1.2) |
| Someone pressured you to have sex through harassment, threats or tricks | 20 (1.1) | 15 (2.4) | 35 (1.4) |
| Someone physically forced you to have sex against your will | 04 (0.2) | 07 (1.1) | 11 (0.4) |
Fig. 2.
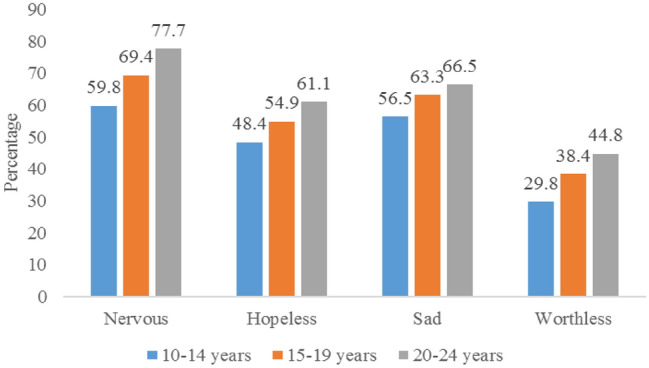
Psychological effects of COVID-19 among ABYM in Kampala, Uganda
Nearly four per cent of ABYM (n = 97) reported that someone wished that they were dead or had never been born, 10.1% (n = 253) reported that someone told them that they were not loved while approximately 1.2% (n = 31) of the respondents reported that they contemplated committing suicide as a result of COVID-19 lockdown, with a slightly higher proportion of out-of-school ABYM reporting that they contemplated committing suicide than their in-school counterparts (out-of-school: 2.1%, n = 13 vs. in-school: 1.0%, n = 18). The proportion that contemplated committing suicide increased with increasing age; 0.6% (n = 3) among those aged 10–14 years, 0.9% (n = 11) among those aged 15–19 years, and 2.0% (n = 17) among those aged 20–24 years. With regard to violence, we found that ABYM experienced very low levels of physical or intimate partner violence (0.4–1.2%) across three of the five forms of violence assessed, i.e., being punched, kicked or beaten by an intimate partner; someone pressuring them to have sex with them through harassment, threats or tricks; and someone physically forcing them to have sex with them against their will. However, 8% (n = 199) reported that they were punched, kicked, or beaten up by their peers.
Effect of COVID-19 Lockdown on Ability to Meet Basic Needs and Health Services
Table 6 shows the effect of COVID-19 lockdown on ABYM’s ability to meet basic needs and access basic health services. Sixty-two per cent (n = 1549) of ABYM reported that they found it difficult to afford a diverse or balanced diet as a result of COVID-19 lockdown, with a higher proportion reported among those who were out-of-school (75.8%, n = 478) than those who were in-school (57.3%, n = 1071). Fifty-five per cent (n = 1364) of the respondents found it difficult to afford food; 53.9% (n = 1346) found it difficult to afford fuel for cooking food while 46.9% (n = 1171) could not afford the travel to a food market to buy food. Nearly 13% (n = 316) could not access HIV/STI testing services while 8% (n = 198) could not access condoms as a result of COVID-19 lockdown. In general, a higher proportion of out-of-school and older ABYM reported that they found it hard to meet their basic needs or to access basic health services than their in-school or younger counterparts. As shown in Fig. 3, the proportion of those who could not afford a diverse/ balanced diet was 49.7% (n = 240) among those aged 10–14 years, 61.6% (n = 727) among those aged 15–19 years and 69.7% (n = 582) among those aged 20–24 years. Similarly, the proportion of those who could not afford food was higher among the older young men; 46.8% (n = 226) among those aged 10–14 years, 52.8% (n = 624) among those aged 15–19 years, and 61.6% (n = 514) among those aged 20–24 years.
Table 6.
Effect of COVID-19 lockdown on access to basic needs and health services among ABYM
| Effects of COVID-19 lockdown | In-school (n = 1869, %) | Out-of-school (n = 631, %) | Total (N = 2500, %) |
|---|---|---|---|
| Due to COVID-19 lockdown, did you or your family find it more difficult to access the following basic needs? (Yes) | |||
| Afford the price of food | 924 (49.5) | 440 (69.7) | 1364 (54.6) |
| Have a diverse/balanced diet | 1071 (57.3) | 478 (75.8) | 1549 (62.0) |
| Afford travel to a food market | 785 (42.0) | 386 (61.2) | 1171 (46.9) |
| Afford fuel for cooking food | 922 (49.4) | 424 (67.2) | 1346 (53.9) |
| Did COVID-19 lockdown make it more difficult for you (or your partner) to access the following services? | |||
| HIV/STI testing | 200 (10.7) | 116 (18.4) | 316 (18.6) |
| Condoms | 110 (5.9) | 88 (13.9) | 198 (7.9) |
Fig. 3.
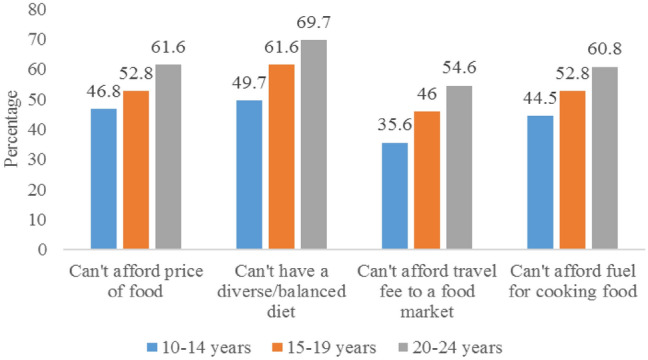
COVID-19 effects on access to basic needs among ABYM in Kampala, Uganda
Effect of COVID-19 Lockdown on the Socio-economic Status and Engagement in Unhealthy Behaviours
Table 7 shows the effect of COVID-19 lockdown on the socio-economic status and health behaviours of ABYM in Kampala. Overall, 30.3% (n = 756) of the respondents experienced a reduction in income as a result of COVID-19 lockdown (out-of-school: 79.9%, n = 504 vs. in-school: 13.5%, n = 252; RR = 9.15, 95%CI 7.68, 10.90). Sixteen per cent (n = 407) of the respondents reported loss of a job while 14.8% (n = 370) reported closure of business as a result of COVID-19 lockdown. In general, the socio-economic effects of COVID-19 lockdown were more strongly felt among out-of-school than their in-school counterparts and among older ABYM than their younger counterparts. For instance, while only 2.1% (n = 10) of 10–14 year-olds reported a reduction in income, it was much higher at 20.4% (n = 241) among those who were aged 15–19 years and 60.5% (n = 505) among those aged 20–24 years.
Table 7.
Effect of COVID-19 lockdown on socio-economic status and health behaviours
| Effects of COVID-19 lockdown | In-school (n = 1869, %) | Out-of-school (n = 631, %) | Total (N = 2500) |
|---|---|---|---|
| Due to COVID-19 lockdown, did you experience any of the following economic challenges? (Yes) | |||
| Loss of a job | 127 (6.8) | 280 (44.4) | 407 (16.3) |
| Reduction in income | 252 (13.5) | 504 (79.9) | 756 (30.3) |
| Closure of business | 103 (5.5) | 267 (42.3) | 370 (14.8) |
| Due to the effects of COVID-19 lockdown, did you practice more of the following behaviours? (Yes) | |||
| Smoking or chewing tobacco | 14 (0.8) | 37 (5.9) | 51 (2.0) |
| Use alcohol such as waragi or beer | 59 (3.2) | 98 (15.5) | 157 (6.3) |
| Use of substances such as khat or marijuana | 37 (2.0) | 76 (12.1) | 113 (4.5) |
| Physical activity such as jogging or other sports | 881 (47.2) | 279 (44.4) | 1160 (46.5) |
| Binge eating | 510 (27.3) | 118 (18.7) | 628 (25.2) |
| Sedentary life style such as excessive watching of TV | 1220 (65.3) | 334 (53.0) | 1554 (62.2) |
Our findings show that COVID-19 lockdown led to an increase in sedentary life styles, binge eating, the use of substances such as khat and marijuana and engaging in smoking or chewing tobacco. Sixty-two per cent (n = 1554) of ABYM reported that they maintained a sedentary life style such as excessive watching of television (TV), and this was higher among in-school than out-of-school ABYM (in-school: 65.3%, n = 1220 vs. out-of-school: 53.0%, n = 334). The proportion of ABYM who reported engaging more in a sedentary life style due to COVID-19 was higher among those aged 10–14 years (65.4%, n = 316) than in those aged 15–19 years (61.0%, n = 719) and 20–24 years (62.2%, n = 519). We also found that 25.2% (n = 628) of the respondents engaged more in binge eating (i.e. consuming unusually large amounts of food in one sitting) than before; 6.3% (n = 157) engaged in the use of alcohol such as waragi (a local potent gin) or beer; 4.5% (n = 113) engaged in the use of substances such as khat or marijuana while 2.0% (n = 51) engaged in smoking or chewing tobacco. The engagement in unhealthy behaviours increased with increasing age. For instance, the proportion of respondents who reported more use of alcohol such as waragi or beer increased from 0.4% (n = 2) among those aged 10–14 years and 3.9% (n = 46) among those aged 15–19 years to 13.1% (n = 109) among those aged 20–24 years. Conversely, the proportion of ABYM that reported binge eating decreased from 29.7% (n = 143) among those aged 10–14 years and 25.0% (n = 295) among those aged 15–19 years to 22.8% (n = 190) among those aged 20–24 years.
Discussion
Our study of the COVID-19 awareness, adoption of preventive measures, and effects of COVID-19 lockdown on the mental health status, socio-economic disruptions and engagement in unhealthy behaviours among adolescent boys and young men (ABYM) aged 10–24 years in Kampala, Uganda, yielded three interesting perspectives: (a) although awareness of how COVID-19 can be prevented is very high, with eight in ten respondents being able to name at least two primary COVID-19 prevention measures, self-reported uptake of COVID-19 prevention measures was very low; (b) the COVID-19 lockdown resulted in increased mental health challenges; limited the ability for people to meet their basic needs; and resulted in socio-economic disruptions (including loss of jobs) and engagement in unhealthy behaviours; and (c) the effects of the COVID-19 lockdown among ABYM were more pronounced among older adolescent boys (15–19 years), young men (20–24 years) and those that were out-of-school compared to those that were in-school. Similar findings have been reported in other countries in Africa, including Ghana [19] and Zambia [20], among others.
Our observation that uptake of COVID-19 prevention measures was low (ranging between 17 and 41%) amidst high awareness of how COVID-19 is spread and prevented raises serious public health concerns. Evidence shows that use of face-masks can reduce the spread of the coronavirus by up to 99.9% through reducing exhalation of large respiratory droplets [21], suggesting that universal use of face-masks, along with social distancing and hand-washing with soap and running water can substantially reduce the risk of coronavirus transmission at population level. Indeed, Bandiera et al. [21] found that a person standing 2 m from someone coughing without a mask is exposed to over 10,000 times more respiratory droplets than from someone standing 0.5 m away wearing a basic single-layer mask. The low uptake of COVID-19 prevention measures reported among ABYM in Kampala, Uganda, could be related to low perceived risk of COVID-19 coupled with misinformation in some population sub-groups [22]. Thus, although a recent study found that 84% of Ugandans were aware of COVID-19, there were still doubts about its existence in Uganda [23]. It is likely that our respondents did not think that they were at risk of contracting COVID-19 or if they contracted the disease, they did not think that it could result in serious consequences, given that there were very few people that had died of COVID-19 at the time of the study. Besides, some Ugandans thought that COVID-19 was a disease of the whites that could not affect them [24]. This low risk perception may have influenced ABYM’s limited uptake of COVID-19 prevention measures, which could explain why only about 17–41% indicated that they always followed the recommended COVID-19 prevention measures.
We found that the lockdown which was instituted by the government to curb the spread of COVID-19 affected ABYM in diverse ways: over 60% felt more nervous or sad that nothing could cheer them up as a result of COVID-19; 1.2% contemplated committing suicide while 62% found it difficult to afford a diverse/balanced diet. In addition, 30% reported a loss in income while 16% lost a job. Reports from the Uganda Bureau of Statistics show that up to 69% of persons aged 10–30 years in Kampala are engaged in some form of work, with 90.5% of them engaged in the informal sector [11]. The informal sector was heavily affected by the lockdown since most of the informal businesses—which employ a majority of the ABYM in Kampala—were closed between March and June 2020, and some of them, including bars and hospitality places, remain closed to-date. It is, therefore, not surprising that the effects of COVID-19 were more marked among the older adolescents and young men who were more likely to be engaged in these businesses. Besides, although only 1.2% contemplated committing suicide as a result of COVID-19, reports from other countries show increases in suicides with a recent Voice of America news report reporting a 57% increase in suicides linked to COVID-19 lockdown in Malawi [25]. Thus, the effect of COVID-19 lockdown on the mental health of ABYM may be greater than reported in this study, calling for mental health interventions to help adolescent boys and young men to cope with the consequences of the lockdown.
Our findings further show a deleterious effect of COVID-19 on healthy behaviours, with 62% engaging in sedentary life styles and 25% reporting binge eating as a result of COVID-19. Patterson et al. [26] found that sedentary behaviour was associated with greater risk for cardiovascular and cancer mortality, and incident type 2 diabetes while Zhao et al. [27] found that increased sitting and TV viewing time significantly increased the risk of cardiovascular, cancer, and mortality risk. Collectively, study findings have implications on the need for increased health education and health promotion of healthy behaviours, as well as the need for interventions that provide economic support incentives, including soft loans, to enable ABYM who lost jobs or who suffered reductions in income to set up viable businesses in order to continue to cope with the COVID-19 situation as it evolves.
Our study had a number of limitations and strengths. The study was conducted a month after the lockdown was lifted; so, people’s perception of the disease and its likely effects could have changed as people learnt how to live with it. Besides, we did not include questions to assess what the situation was before the lockdown, and only relied on questions that asked if the lockdown resulted in increased or higher likelihood of the effects happening without a comparative point measure in the past. Thus, the responses to questions asking about the respondents’ ability to cope with the situation largely depended on how they perceived of the situation at time of the study rather than a comparison of the pre- and COVID-19 lockdown situation. However, we tried to overcome these limitations by specifying that the questions referred to what the respondents went through as a result of COVID-19 lockdown. We believe that respondents were able to weigh the situation before and after the COVID-19 lockdown and that their responses reflect the effects that they actually experienced as a result of COVID-19 lockdown. These limitations notwithstanding, our study was the first study ever to assess uptake of COVID-19 prevention measures and the effects of COVID-19 lockdown among ABYM in Kampala, Uganda. Besides, since this study was conducted about 4 months after the first case was reported in Uganda, study findings present more realistic rather than anticipated effects of COVID-19 lockdown. Given the high youth unemployment rate in Kampala [11], coupled with income and job losses as reported in this study, we believe that these findings will help the government of Uganda, and Kampala Capital City Authority (the body that manages the affairs of Kampala City) in particular, to come up with interventions that can help to improve the socio-economic and mental health status of ABYM in Kampala, Uganda.
Conclusion
Our study shows that while awareness of how COVID-19 can be prevented is high, uptake of COVID-19 prevention measures remains sub-optimal. We also found that the COVID-19 lockdown had devastating mental, socio-economic and healthy effects. COVID-19 lockdown led to increased mental health challenges; inability to access basic needs and access to essential health services; and led to income and job losses due to the closure of businesses during the lockdown. Respondents reported increased engagement in unhealthy behaviours including sedentary life styles characterized by excessive watching of TV and binge eating. These findings suggest a need for continuous health education and health promotion to improve uptake of COVID-19 prevention measures and socio-economic support provided to ABYM to help them to cope with the effects of COVID-19 lockdown. Interventions that provide economic support to ABYM to start or resume their businesses and those that can help to improve their health and mental wellbeing are urgently needed.
Acknowledgements
This study was made possible with funding from the Government of the Republic of Uganda through Makerere University Research and Innovations Fund (Mak-RIF). We would like to thank the data collectors who collected the data from all the five divisions of Kampala and the respondents for accepting to participate in this study.
Authors’ Contributions
JKBM conceived the study, designed the study tools, supervised data collection, wrote the first draft of the paper, and revised the paper for substantial intellectual content. SK contributed to study design, designed the study tools, contributed to data analysis, and revised the paper for substantial intellectual content. TS supervised data collection, contributed to the design of the study tools, and reviewed the paper for substantial intellectual content. JS contributed to data analysis and revised the paper for substantial intellectual content. RW contributed to the study design, contributed to the design of the study tools, and reviewed the paper for substantial intellectual content. All authors led and approved the final version for submission.
Data Availability
The dataset used during the current study is available from the corresponding author on reasonable request.
Compliance with Ethical Standards
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
The study protocol was reviewed and approved by the Higher Degrees Research and Ethics Committee of Makerere University School of Public Health (Protocol#: 757) and cleared by the Uganda National Council for Science and Technology (SS#: 5240).
Informed Consent
Written informed consent was sought from each of the individuals before participating in the quantitative interviews. Parental consent was waived for mature minors below 18 years who had drug or alcohol dependency or a sexually transmitted infection. Parental consent was also waived for emancipated minors who were married, had a child or catered for their own livelihood, as defined in the Uganda National Council for Science and Technology guidelines. Consent from parents/guardians was sought for ‘un-emancipated’ participants below 18 years of age. Participants aged 10–17 years were asked to provide their own assent in addition to the parental consent form. Administrative clearance was sought from the local council chair persons in the villages where participants were selected.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Joseph K. B. Matovu, Email: matovujkb@gmail.com, Email: jmatovu@musph.ac.ug
Stephen N. Kabwama, Email: skabwama@musph.ac.ug
Tonny Ssekamatte, Email: ssekamattet.toca@gmail.com.
John Ssenkusu, Email: jssenkusu@musph.ac.ug.
Rhoda K. Wanyenze, Email: rwanyenze@musph.ac.ug
References
- 1.Worldometers. (2020). COVID-19 coronavirus pandemic. Retrieved December 14, 2020, from https://www.worldometers.info/coronavirus/.
- 2.British Broadcasting Corporation (BBC). (2020). Coronavirus: Window of opportunity to act, World Health Organization says. London: BBC. Retrieved December 15, 2020, from https://www.bbc.com/news/world-asia-china-51368873.
- 3.Mohammed M, Muhammad S, Mohammed FZ, et al. Risk factors associated with mortality among patients with novel coronavirus disease (COVID-19) in Africa. Journal of Racial and Ethnic Health Disparities. 2020 doi: 10.1007/s40615-020-00888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Africa CDC. (2020). Coronavirus disease 2019 (COVID-19): Latest updates on the COVID-19 crisis from Africa CDC. Retrieved December 28, 2020, from https://africacdc.org/covid-19/.
- 5.Africa CDC. (2020). Finding the balance: Public health and social measures in Uganda. Retrieved December 15, 2020, from https://africacdc.org/resources/.
- 6.The New Vision. (2020). COVID-19: Kampala City a hot spot. Retrieved December 26, 2020, from https://www.newvision.co.ug/news/1536286/covid-19-kampala-city-hot-spot.
- 7.The Independent. (2020). COVID-19: 90% of Kampala cases used a taxi before infection. Retrieved December 1, 2020, from https://www.independent.co.ug/covid-19-90-of-kampala-cases-used-a-taxi-before-infection/.
- 8.Machida M, Nakamura I, Saito R, Nakaya T, Hanibuchi T, Takamiya T, et al. Adoption of personal protective measures by ordinary citizens during the COVID-19 outbreak in Japan. International Journal of Infectious Diseases. 2020;202(94):139–144. doi: 10.1016/j.ijid.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Komin W, Thepparp R, Subsing B, Engstrom D. Covid-19 and its impact on informal sector workers: a case study of Thailand. Asia Pacific Journal of Social Work and Development. 2020 doi: 10.1080/02185385.2020.1832564. [DOI] [Google Scholar]
- 10.Megersa, K. (2020). The informal sector and COVID-19. K4D Helpdesk Report 890. Brighton, UK: Institute of Development Studies. Retrieved December 27, 2020, from https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/15725.
- 11.Uganda Bureau of Statistics (UBOS). (2018). The national labour force survey 2016/17—Main report. Kampala: UBOS. Retrieved December 9, 2020, from https://www.ubos.org/wp-content/uploads/publications/10_2018Report_national_labour_force_survey_2016_17.pdf.
- 12.Uganda Bureau of Statistics (UBOS). (2019). 2019 Statistical abstract for Kampala city. Kampala: UBOS. Retrieved December 14, 2020, from https://www.kcca.go.ug/media/docs/Statistical-Abstract-2019.pdf.
- 13.Cochran WG. Sampling techniques. New York: Wiley; 1977. [Google Scholar]
- 14.Swahn MH, Buchongo P, Kasirye R. Risky behaviors of youth living in the slums of Kampala: A closer examination of youth participating in vocational training programs. Vulnerable Children and Youth Studies. 2018;13(3):276–290. doi: 10.1080/17450128.2018.1489168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uganda Bureau of Statistics (UBOS). (2016). National population and housing census 2014—Main report. Kampala: UBOS. Retrieved December 9, 2020, from https://www.ubos.org/wp-content/uploads/publications/03_20182014_National_Census_Main_Report.pdf.
- 16.Robertson SE, Anker M, Roisin AJ, Macklai N, Engstrom K. The lot quality technique: A global review of applications in the assessment of health services and diseases surveillance. World Health Statistical Quarterly. 1997;50:199–209. [PubMed] [Google Scholar]
- 17.Valadez JJ, Weiss W, Leburg C, Davis R. Assessing community health programs. A trainer’s guide. Using LQAS for baseline survey and regular monitoring, TALC, 2003, 0954489403. The International Journal of Health Planning and Management. 2007;22(4):357–359. doi: 10.1002/hpm.908. [DOI] [Google Scholar]
- 18.Uganda National Council for Science and Technology (UNCST). (2014). National guidelines for research involving humans as research participants. Kampala: UNCST. Retrieved December 14, 2020, from https://www.uncst.go.ug/guidelines-and-forms/.
- 19.Asiamah N, Opuni FF, Mends-Brew E, Mensah SW, Mensah HK, Quansah F. Short-term changes in behaviors resulting from COVID-19-related social isolation and their influences on mental health in Ghana. Community Mental Health Journal. 2020 doi: 10.1007/s10597-020-00722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nyashanu M, Ikhile D, Thamary K, Chireshe R. The impact of COVID-19 lockdown in a developing country: Narratives of self-employed women in Ndola, Zambia. Health Care for Women International. 2020 doi: 10.1080/07399332.2020.1823983. [DOI] [PubMed] [Google Scholar]
- 21.Bandiera L, Pavar G, Pisetta G, Otomo S, Mangano E, Seckl JR, et al. Face coverings and respiratory tract droplet dispersion. Royal Society Open Science. 2020 doi: 10.1098/rsos.201663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ChimpReports. (2020). Covid-19: Kampala slum dwellers ditch face masks, report to ‘liquor-based prevention’. Kampala: ChimpReports. Retrieved December 19, 2020, from https://chimpreports.com/covid-19-kampala-slum-dwellers-ditch-face-masks-resort-to-liquor-based-prevention/.
- 23.The New Vision. (2020). 84% of Ugandans know about COVID-19 preventive measures—Report. Retrieved December 27, 2020, from https://www.newvision.co.ug/news/1527894/ugandans-about-covid-19-preventive-measures-report.
- 24.Kasozi KI, MacLeod E, Ssempijja F, et al. Misconceptions on COVID-19 risk among Ugandan men: Results from a rapid exploratory survey, April 2020. Frontiers in Public Health. 2020;8:416. doi: 10.3389/fpubh.2020.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masina, L. Rise in Malawi Suicide Cases Linked to COVID-19. Retrieved December 19, 2020, from https://www.voanews.com/africa/rise-malawi-suicide-cases-linked-covid-19.
- 26.Patterson R, McNamara E, Tainio M, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. European Journal of Epidemiology. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao R, Bu W, Chen Y, Chen X. The dose-response associations of sedentary time with chronic diseases and the risk for all-cause mortality affected by different health status: A systematic review and meta-analysis. The Journal of Nutrition, Health and Aging. 2020;24(1):63–70. doi: 10.1007/s12603-019-1298-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used during the current study is available from the corresponding author on reasonable request.