Abstract
Background
Underweight, wasting, and stunting are the commonest nutritional disorders among children, especially in developing countries. The aim of this study was to assess the prevalence and determinant factors of underweight, wasting, and stunting among school-age children in 2019.
Methods
A cross-sectional study was conducted in the five special districts of South Gondar Zone, among 314 school-age children. WHO AnthroPlus software was used to build Z-scores from anthropometric measurement. The data were analyzed by SPSS Version 20. The degrees of association were assessed using adjusted odds ratio (AOR) and 95% confidence interval during multivariable logistic regression. A P-value less than 0.05 was considered to be statistically significant.
Results
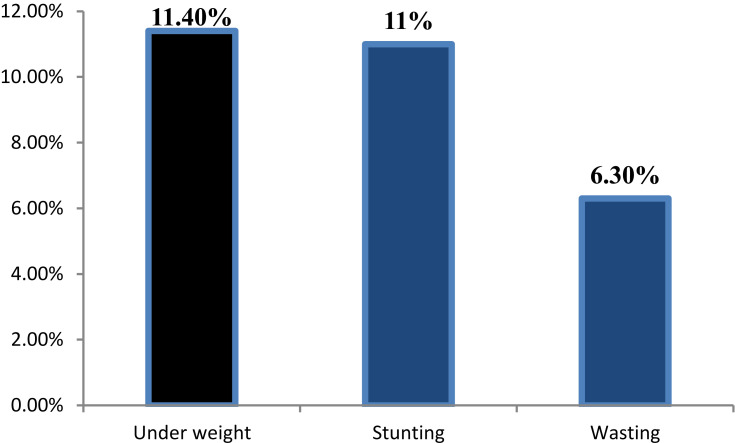
Of the total study participants, 232 (77.3%) were from public schools. The mean±standard deviation (SD) of height of children was 132.9±9.8 cm, and the mean±SD weight of children was 27.7±5.8 kg. The prevalence of stunting, wasting, and underweight was 11%, 6.3%, and 11.4%, respectively. Students who ate their breakfast rarely were 8-times more likely to be underweight than those who ate their breakfast always (AOR=7.9, 95% CI=4.8–14.8). Those who were sick in the past 2 weeks were more likely to be underweight than their counterparts (AOR=7.3, 95% CI=2.8–14.4). Those who never consume milk or milk products were 6.5 (AOR=6.5, 95% CI=1.7–23) times more likely to be stunted than those who consumed this always. Sickness in the past 2 weeks prior to data collection was significantly associated with thinness (AOR=6 0.9, 95% CI=4.1–10.1).
Conclusion
The overall prevalence of wasting, stunting, and underweight was a mild public health problem in the study area.
Keywords: wasting, stunting, underweight, school-age children, South Gondar, Ethiopia
Plain Language Summary
Underweight is defined as having a weight below the recommended level for a specific age; wasting is having a weight below the recommended level for a given height; whereas stunting is having a height below the recommended level for a specific age.
Underweight, wasting, and stunting are the commonest nutritional disorders among children, especially in developing countries.
The study was conducted in five special districts of south Gondar zone on 300 school-age children aged 6–12 years.
Of the total study participants, 77.3% were from public schools.
We found that
11% of children were underweight,
6.3% of children were wasted, and
11.4% of children were stunted.
The investigators decided that stunting, underweight, and wasting were mild public health problems in the study area.
Identified risk factors
Not eating breakfast,
Being sick in the past 2 weeks prior to data collection,
Not consuming milk or milk products, and
Lack of hand washing practice with soap.
Background
Malnutrition includes both under-nutrition and over-nutrition. Underweight, wasting, and stunting are categorized as under-nutrition. Under-nutrition might happen either due to long-term or short-term inadequate nutrient intake. In addition, it can also be caused by food unavailability or increased disease prevalence.1 The prevalence of stunting among school-age children in Ethiopia ranges from 29.2–42.7%. On the other hand the prevalence of wasting ranges from 8–21%. The identified determinants of under-nutrition in Ethiopia include age, sex, wealth quantiles, enrollment in schools, dietary diversity score, fever in the past 2 weeks, consumption of food from animal sources, consumption of the family’s own cattle products, years of schooling of the person in charge of food preparation, number of children living in the house, consumption of food from animal, and literacy of head of household.2–4 Anthropometry is a universally applicable method to assess nutritional status in resource limited areas5.
According to the World Health Organization (WHO), school-age comprises the ages between 6 and 12 years; and it is a pre-adolescent time. School-age children are affected by different nutritional and health problems due to high demand (requirement) for the rapid growth rate and high engagement in physical activity.6 So, adequate dietary intake is important for the physical and mental development during the primary school years.1
Due to malnutrition there is a high rate of morbidity and mortality of children in developing countries. Because of malnutrition, the cognitive function will be affected and impaired. Finally this may affect the economy of the household, the community, and the nation at large.6,7
Children gain up to 50% of their adult weight, 20% of their adult height, and 50% of their adult skeletal mass during school-age. Thus being malnourished at this age exposes them to serious short- and long-term health problems.8
Height has been found to be related to productivity, and 1% loss in adult height as a result of childhood stunting is associated with a 1.4% loss in productivity. Improved nutrition and health improves the mental and physical capabilities of children and thereby their future earning capacity.9
On the other hand, improved nutrition and health to children have long been recognized as fundamental human rights. For example, in one of the conventions that Ethiopia has ratified, we find the following: “States parties recognize the right of the child to the enjoyment of the highest attainable standard of health …“ and shall take appropriate measures “to combat disease and malnutrition … through the provision of adequate nutritious foods and clean drinking water …” and “health care”. Moreover, it is stated in the national nutrition strategy document. The right to the determinants of adequate nutrition is also upheld in the constitution of Ethiopia, entrusting the government to take appropriate measures to ensure that these rights are adequately protected, especially among the most vulnerable groups.10
For the control of malnutrition, a variety of actions are needed, such as agricultural interventions, provision of safe drinking water and sanitation, education, and health services. As part of the government’s strategy to increase school enrollment and reduce drop-out rates in drought-prone areas of Ethiopia, the ministry of education, with support from the World Food Program (WFP), began a project called “Improving Education through School Feeding” on a pilot basis in 1994 and currently WFP is actively working to alleviate malnutrition of school-age children and increasing school attendance. This program enroll 102,000 primary school children, in the highly food insecure areas of Tigray, Afar, Amhara, and Oromia Regions.11
Several studies have investigated the nutritional status of school-age children in different parts of the world. However, data on the growth of school-age children, generated in a consistent manner across countries and over time, is difficult to find.12 Lack of current reports on the prevalence of nutritional status in different areas of a given country may limit the rate at which decisions are made for intervention measures against these effects by concerned bodies such as national government and international organizations.13
In Ethiopia and particularly in the study area, even though many studies have been carried out on malnutrition of less than 5 years old children, there is no study conducted so far on assessment of nutritional status and the determinants among school-age children. Therefore, this study aimed to assess the school-age nutritional status and its associated factors in South Gondar Zone, special districts.
Methods and Materials
Study Area
The study was conducted in South Gondar zone, which is a zone in the Amhara region of Ethiopia. South Gondar zone is bordered on the South by East Gojam, on the Southwest by West Gojam and Bahir Dar, on the West by Lake Tana, on the North by North Gondar, on the North east by Wag Hemra, on the East by North Wollo, and on the Southeast by South Wollo. There are 18 districts (13 rural and five urban) in this zone.
Based on the 2007 national census conducted by the Central Statistical Agency of Ethiopia (CSA), this zone has a total population of 2,051,738, of whom 1,041,061 are men and 1,010,677 women; 195,619 (9.53%) are urban inhabitants. A total of 468,238 households were counted in this zone, which results in an average of 4.38 persons to a household. The main ethnic group reported in south Gondar was Amhara (99.7%). Amharic was spoken as a first language by 99.7% of the population. The majority of the inhabitants practiced Ethiopian Orthodox Christianity, with 96.14% reporting that as their religion, while 3.68% of the population said they were Muslim.
Study Design and Period
A cross-sectional study was conducted from October to November, 2019.
Study Population
All children aged between 6–12 years who were attending elementary school at the time of data collection were included in this study, but children having a visible physical deformity were excluded.
Sample Size Determination
The sample size was estimated using the single population proportion formula by using a confidence level of 95% (z=l1.96), marginal error of 5%, and proportions of stunting, wasting, and underweight. According to 2007 Ethiopia Demographic Health Survey (EDHS), the prevalence of stunting, wasting, and underweight was 22.3%, 17.9%, and 23.1% respectively.4 Among the calculated sample size, the highest sample size was from underweight (273). Then, the final sample size was 314, after adding 15% of none response rate.
Sampling Techniques
All elementary schools found in the five special districts of South Gondar zone were included. In each school a list of children was prepared to have a sampling frame of students aged between 6–12 years. The calculated sample was allocated to each school proportionally based on their respective number of school-age children in the 2019 academic year. Then, a sample from each school was selected by simple random sampling (by random table method).
Data Collection Instruments
A semi-structured questionnaire was developed after thorough review of different literatures. A height measuring length board which has a scale and sliding head piece and a 2 meters measuring capacity, with a precision of 0.1 cm was used for measuring the height, and UNICEF’s digital weighting scale (SECA) which has a capacity of 150 kg and with a precision of 0.1 kg was used for measuring weight.
Data Collection Procedure
Ten nurses were recruited for data collection. The questionnaire was originally developed in English and was translated to local language (Amharic). The questionnaire was pretested in Gasay Primary School (out of the study area). Then, appropriate modifications and corrections were done before data collection. Data related to socio-demographics, socio-economic, dietary intake, and hygiene were collected from parents and caregivers.
Anthropometric measurement of children was done. Weights were taken using a digital portable weighing calibrated SECA scale to the nearest 0.1 kg and the height was measured by using a length board to the nears 0.1 cm in Frankfurt position. Children were weighed having lightly clothing/with school uniforms, without shoes and with empty pockets.
Data Quality Assurance
Three days of training were provided to data collectors and supervisors. The training was on how to consent the study participants, on the questionnaire, on anthropometric measuring tools and measurements. Data was collected under the supervision of the principal investigator and supervisors. Incomplete questionnaires were completed by making second visits to the schools. A weighing scale was calibrated to the zero before taking every measurement to reduce errors. Weight and height measurement were done twice and the average value was used for the analysis.
Data Processing and Analysis
After data collection was completed, the data were checked for completeness and then recoding and categorization was done. Software program WHO AnthroPlus was used to convert nutritional data from anthropometric measurement into Z-scores of the indices; H/A, W/H, and W/A, taking age and sex into consideration using WHO reference curves. EPI-info Version 3.5.2 was used to enter the anthropometric and other data and then, the data was exported to SPSS Version 20 software for windows to conduct further descriptive and analytical analysis. Variables having a P-value of <0.2 in the bivariable logistic regression were entered into multivariable logistic regression analysis. The degrees of association between dependent and independent variables was assessed using OR and 95% CI. Finally a P-value<0.05 was used to declare statistical significance.
Operational Definition
Nutritional status: Refers to the physicality of a child in weight and height.
Malnutrition: Refers to under-nutrition that include wasting, stunting, and underweight.
Stunting: If the child’s height for age Z-scores of <-2 SD of the median WHO reference values.
Underweight: if the child’s weight for age Z-score is <-2 SD from the median WHO reference values.
Wasting: if the child weight for height Z-score is <-2 SD from the median WHO reference values.
Results
Data was collected from 300 students; 232 (77.3%) were from public schools. One hundred and fifty-nine (53%) children were females. Two hundred and ninety-nine (99.7%) of the students were Amhara in ethnicity. Religionwise, 296 (98.7%) of them were Orthodox Christianity followers. From the total, 130 (43.3%) of them were in birth order of 2–3. The mean age±standard deviation (SD) of children was 9.9867±1.48 months.
Regarding family size, 220 (73.3%) of the children live in a family size of five or above. Two hundred and nine (69.7%) of the children live with both mother and father, and about 83 (27.7%) mothers of school-age children cannot read and write (Table 1).
Table 1.
Socio-Demographic and Socio-Economic Status of School-Age Children Aged 6–12 Years in, South Gondar, Ethiopia, 2019
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Age of the student | 6 | 1 | 0.3 |
| 7 | 16 | 5.3 | |
| 8 | 45 | 15.0 | |
| 9 | 32 | 10.7 | |
| 10 | 91 | 30.3 | |
| 11 | 60 | 20.0 | |
| 12 | 55 | 18.3 | |
| Total | 300 | 100 | |
| Birth order | 1 | 99 | 33.0 |
| 2–3 | 130 | 43.3 | |
| 4–5 | 47 | 15.7 | |
| 6 and above | 24 | 8.0 | |
| Total | 300 | 100 | |
| Educational status of the mother | Cannot read and write | 83 | 27.7 |
| Can read and write | 28 | 9.3 | |
| Grade 1–4 | 26 | 8.7 | |
| Grade 5–8 | 59 | 19.7 | |
| Grade 9–12 | 39 | 13.0 | |
| Above 12 | 65 | 21.7 | |
| Total | 300 | 100 | |
| Occupation of mothers | Housewife | 139 | 46.3 |
| Farmer | 4 | 1.3 | |
| Merchant | 53 | 17.7 | |
| Government employee | 71 | 23.7 | |
| Daily labourers | 29 | 9.7 | |
| Others | 4 | 1.3 | |
| Total | 300 | 100 | |
| Age of the mother/caregivers | Below 25 | 7 | 2.3 |
| 25–29 | 39 | 13.0 | |
| 30–34 | 92 | 30.7 | |
| 35–39 | 90 | 30.0 | |
| 40–44 | 33 | 11.0 | |
| 45–49 | 17 | 5.7 | |
| 50–54 | 11 | 3.7 | |
| 55 and above | 7 | 2.3 | |
| Total | 296 | 98.7 | |
| Educational status of the father | Cannot read and write | 34 | 11.3 |
| Read and write | 39 | 13.0 | |
| 1–4 | 19 | 6.3 | |
| 5–8 | 57 | 19.0 | |
| 9–12 | 42 | 14.0 | |
| 12 and above | 87 | 29.0 | |
| Total | 278 | 92.6 | |
| Monthly income in birr | <1,500 | 68 | 22.7 |
| 1,500–3,000 | 126 | 42.0 | |
| >3,000 | 105 | 35.0 | |
| Do not know | 1 | 0.3 | |
| Total | 300 | 100 |
Dietary Habit and Water Sources of Households of School-Age Children
Regarding dietary habits, the staple food among 268 (89.3%) of the households was Teff, and 278 (92.7%) of the children were never hungry in the past 1 month. One hundred and sixty-three (54.3%) of the children ate three times per day. And 144 (48%) of the children ate breakfast always; 129 (43%) of them ate sometimes; 26 (8.7%) ate rarely, and one (0.3%) almost never ate breakfast. One hundred and forty two (47.3%) children eat fruits once per week and 104 (34.7%) of children never consumed milk or milk products (Table 2).
Table 2.
Dietary Habits of School-Age Children Aged 6–12 Years in South Gondar Zone, Ethiopia, 2019
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Meal frequency | Once | 3 | 1.0 |
| Twice | 24 | 8.0 | |
| Three | 163 | 54.3 | |
| Four and above | 110 | 36.7 | |
| Total | 300 | 100 | |
| Fruit eating frequency | Not at all | 55 | 18.3 |
| Once | 142 | 47.3 | |
| Twice | 63 | 21.0 | |
| ≥Three | 40 | 13.3 | |
| Total | 300 | 100 | |
| Milk consumption | Never | 104 | 34.7 |
| Sometimes | 95 | 31.7 | |
| Most of the days | 35 | 11.7 | |
| Always | 66 | 22.0 | |
| Total | 300 | 100 |
Of all household food sources, 271 (90.3%) of them were purchased from a market; 14 (4.7%) were their own products; 12 (4%) were both from their own product and purchasing, and two (0.7%) were from aid. Two hundred and eighty-eight (96%) of them had a latrine at their home. From the total, 267 (89%) of the households do not treat drinking water and, from these, the source of drinking water for 258 (86%) households was tap water.
Hygienic Practice and Illness
Concerning hand washing habits, 236 (78.7%) of school-age children always wash their hands before eating. From all children, 203 (67.7%) of them were using soap sometimes. One hundred and fifty three (51%) children washed unpeeled fruits sometimes before eating (Table 3).
Table 3.
Sanitation and Hygiene Status of School-Age Children Aged 6–12 Years in South Gondar Zone, Ethiopia
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Waste disposal system | Collection by municipality | 50 | 16.7 |
| Burial | 80 | 26.7 | |
| Private collector | 24 | 8.0 | |
| Thrown on the road or free space | 20 | 6.7 | |
| Collected in the compound | 5 | 1.7 | |
| Thrown on the farm place | 5 | 1.7 | |
| Burned | 114 | 38.0 | |
| Others | 2 | 0.7 | |
| Total | 300 | 100 | |
| Hand washing habit | Never | 3 | 1.0 |
| Rarely | 4 | 1.3 | |
| Sometimes | 28 | 9.3 | |
| Most of the days | 29 | 9.7 | |
| Always | 236 | 78.7 | |
| Total | 300 | 100 | |
| Soap usage while hand washing | Never | 18 | 6.0 |
| Rarely | 29 | 9.7 | |
| Sometimes | 203 | 67.7 | |
| Most of the days | 16 | 5.3 | |
| Always | 34 | 11.3 | |
| Total | 300 | 100 | |
| Washing unpeeled fruits | Never | 26 | 8.7 |
| Sometimes | 153 | 51.0 | |
| Most of the days | 24 | 8.0 | |
| Always | 97 | 32.3 | |
| Total | 300 | 100 | |
Fifty-eight (19.3%) children had been sick in the past 2 weeks prior to data collection. The cause of sickness was stomach ache in 25 (27.6%), followed by common cold in 12 (20.7%).
Nutritional Status
The mean±tandard deviation (SD) of height of children was 132.9±9.8 cm and the mean±SD of weight of children was 27.6±5.8 kg. In this study, 21 (11.4%, 95% CI=6.8−15.9) children aged 6–10 years were under-weight. Thirty-three (11%, 95% CI=7.3–15) of the children were stunted; and 19 (6.3%, 95% CI=3.5–9.3) of the children were wasted (Figure 1). Overall, the likelihood to have a severe form of malnutrition was rare among these age groups in the study area.
Figure 1.
Nutritional status of school-age children aged 6–12 years in South Gondar, Ethiopia, 2019.
Factors Associated with Underweight
In the multivariable logistic regression analysis, educational status of the father, children’s breakfast eating habit, consumption of milk, and having sickness in the past 2 weeks were significant variables. Here, educational status of a father being grade 9–12 was a protective factor for not to be underweight as compared to fathers who cannot read and write (AOR=0.09; 95% CI=0.01–0.94). Students who rarely ate their breakfast were more likely to be underweight than those who eat breakfast always (AOR=7.94; 95% CI=4.82−14.80). Those who never consumed milk or milk products were more likely to be underweight as compared to those who consumed always (AOR=5.46; 95% CI=4.02–6.90). In addition, those who were sick 2 weeks before data collection were more likely to be underweight than their counterparts (AOR=7.3; 95% CI=2.8–14.4) (Table 4).
Table 4.
Factors Associated with Underweight Among School-Age Children Aged 6–12 Years in South Gondar Zone, Ethiopia
| Variables | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|
| Educational status of the father | Cannot read and write | 1 | 1 | 1 |
| Read and write | 0.43 (0.07–2.80) | 0.3 (0.24–8.31) | 0.357 | |
| 1–4 | 0.75 (0.12–4.75) | 0.22 (0.02 −2.39) | 0.214 | |
| 5–8 | 0.38 (0.03–4.12) | 0.24 (0.01–9.07) | 0.441 | |
| 9–12 | 0.22 (0.05–0.97) | 0.09 (0.01 −0.95) | 0.045 | |
| 12 and above | 0.41 (0.08–2.19) | 0.45 (0.04–4.76) | 0.506 | |
| Sex of the student | Male | 1 | 1 | 1 |
| Female | 0.45 (0.17–1.18) | 1.30 (0.31–5.53) | 0.720 | |
| Breakfast eating habit | Rarely | 12.60 (3.14–50.02) | 7.94 (4.82 −14.80) | 0.002 |
| Some times | 10.44 (2.99–36.01) | 13.40 (1.70–15.38) | 0.014 | |
| Always | 1 | 1 | 1 | |
| Milk consumption | Never | 13.11 (2.90–16.78) | 5.46 (4.03–6.96) | 0.002 |
| Some times | 13.30 (1.69–15.39) | 5.85 (2.26–9.31) | 0.013 | |
| Most of the days | 63.21 (0.01–71.24) | 16 (0.01–22.86) | 0.998 | |
| Always | 1 | 1 | 1 | |
| Water treatment | Yes | 1 | 1 | 1 |
| No | 0.32 (0.10–1.01) | 7.44 (0.71–77.97) | 0.094 | |
| Sickness in the past two weeks | Yes | 13.50 (11.01–23.54) | 7.32 (2.87 −14.41) | 0.002 |
| No | 1 | 1 | 1 | |
Factors Associated with Stunting
In multivariable analysis those who never consume milk or milk products are more likely to be stunted than those who consumed it always (AOR=6.5; 95% CI=1.7–23) and those who never use soap for hand washing are more likely to be stunted than those who used soap always (AOR=4.5; 95% CI=1.7–12) (Table 5).
Table 5.
Factors Associated with Stunting Among School-Age Children Aged 6–12 Years in South Gondar Zone, Ethiopia
| COR (95% CI) | AOR (95% CI) | P-value | ||
|---|---|---|---|---|
| Meal frequency per day | Once | 3.5 (0.24–5.14) | 4.65 (0.25–16.14) | 0.302 |
| Twice | 3.57 (0.31–4.13) | 4.33 (0.32–9.65) | 0.273 | |
| Three times | 5.6 (0.46–8.04) | 6.456 (0.45–13.66) | 0.172 | |
| ≥Four times | 1 | 1 | 1 | |
| Milk consumption habit | Never | 5.99 (3.69–11.65) | 6.49 (1.76–23.945) | 0.005 |
| Some times | 1.17 (0.39–3.45) | 1.23 (0.36–4.19) | 0.736 | |
| Most of the days | 1.42 (0.57–3.49) | 1.63 (0.613–4.31) | 0.329 | |
| Always | 1 | 1 | 1 | |
| How often you use soap during hand washing | Never | 6.12 (0.71–28.50) | 4.546 (1.70–12.14) | 0.003 |
| Occasionally | 10.08 (9.21–25.65) | 20.40 (2.06–28.24) | 0.010 | |
| Sometimes | 3.29 (1.35–5.67) | 7.826 (0.812–75.48) | 0.075 | |
| Most of the time | 2.52 (0.48–10.33) | 3.326 (0.560–19.76) | 0.186 | |
| Always | 1 | 1 | 1 | |
| Washing of unpeeled fruits | Never | 2.8 (0.35–5.41) | 0.299 (0.033–2.681) | 0.281 |
| Occasionally | 3.42 (0.36–8.7) | 4.16 (0.512–16.71) | 0.26 | |
| Sometimes | 0.15 (0.02–1.41) | 0.13 (0.01–1.38) | 0.091 | |
| Most of the time | 0.35 (0.042–2.85) | 0.38 (0.04–3.53) | 0.398 | |
| Always | 1 | 1 | 1 |
Factors Associated with Wasting (Low BAZ)
In the bivariate analysis, fruit eating frequency per week, milk consumption habit, and sickness in the past 2 weeks were associated with low BAZ or wasting. Finally in the multivariable analysis those who never consumed milk were more likely to be wasted than those who consumed it always, and sickness in the past 2 weeks is significantly associated with low BAZ (Table 6).
Table 6.
Factors Associated with Wasting Among School-Age Children Aged 6–12 Years in South Gondar Zone, Ethiopia
| COR (95% CI) | AOR (95% CI) | P-value | ||
|---|---|---|---|---|
| Milk consumption habit | Always | 1 | 1 | 1 |
| Most of the days | 2.73 (0.74–10.1) | 2.39 (0.455–12.49) | 0.304 | |
| Sometimes | 2.15 (0.46–10.12) | 2.26 (0.35–14.47) | 0.391 | |
| Never | 6.06 (1.35–8.55) | 9.02 (1.56–51.98) | 0.014 | |
| Fruit eating pattern per week | Never | 1 | 1 | 1 |
| Once | 0.44 (0.045–4.43) | 0.591 (0.044–8.009) | 0.693 | |
| Twice | 0.37 (0.04–3.08) | 0.226 (0.023–2.256) | 0.205 | |
| Three and above | 0.19 (0.24–2.10) | 0.213 (0.019–2.443) | 0.214 | |
| Sickness in the past 2 weeks | Yes | 8.4 (4.01–12.32) | 6 0.93 (4.12–10.06) | 0.000 |
| No | 1 | 1 | 1 |
Discussion
This study showed that the prevalence of stunting, wasting, and underweight were 11%, 6.3%, and 11.4%, respectively. In Ethiopia, a cross-sectional survey which was aimed at estimating the prevalence of chronic health and nutritional conditions of school-age children in 2008 reported that the prevalence of stunting, wasting, and underweight were 22.3%, 17.9%, and 23.1%, respectively.4 The report is higher than the finding of the current study. The reason might be due to difference in geographic area and the time gap. Another study on Prevalence and factors associated with stunting and thinness among school-age children in Arba Minch health and demographic surveillance site, Southern Ethiopia, in 2016, showed prevalence of stunting and thinness were 41.9% (95% CI=37–47) and 8.0% (95% CI=5.4–10.8), respectively. This is also higher than the current study, and the variation might be due to geographical difference and sample size difference.3
Nutrition and infectious diseases are commonly shown to go hand-in-hand. There is a bi-directional influence in which malnutrition may predispose to infection or increase its severity, while infection itself results in nutritional abnormalities. In any population, the impact of malnutrition depends on the prevalence of infection, and the impact of infection depends upon the nutritional base.14 As per the UNICEF’s conceptual framework of malnutrition, infection or disease is the immediate cause of malnutrition.12 The finding of this study supports this idea, as sickness in the past 2 weeks was the best predictor of wasting.
In this study not eating breakfast was associated with underweight. In line with this, a study which assessed the nutritional status of primary school children and their awareness in slum areas of urban and rural areas in 2007 in Giza governorate of Egyptian showed that 76.9% of urban and 69.3% of rural children were underweight, and 9.8% urban and 12.8% rural were stunted (P<0.05 for both underweight and stunting). Only 33.9% of urban children and 29.3% of rural ones have eaten breakfast.15 This might be because breakfast consumption is an important remedy to obtain adequate calorie intake throughout the day.
In this study not using soap for hand washing was associated with stunting. A case study in Bangladesh on underweight children showed that the practice of washing hands with soap and water after defecation was 23% more likely to reduce being underweight.16 This might be because infection which is mainly caused by poor personal hygiene is the immediate cause of malnutrition.
More education will improve the mother’s knowledge and health practices and have a greater impact on child nutrition. There are many study findings supporting the idea that when parents are more educated, their children are less likely to be malnourished.17–19
In this study the educational status of a father was associated with being underweight. In agreement with this, a study from West Bengal, India, in 2010 showed that underweight was significantly associated with fathers’ educational status.17 On the other hand, a study in Abeokuta, Southwest Nigeria found that low maternal education was the major contributory factor for stunting.20 This might be because the ability of each parent to obtain and use information about appropriate caring practices and health services for the child depends on their educational status.
In this study milk consumption status was significantly associated with low wasting, stunting,and underweight. In line with this, a cross-sectional study which was conducted in Fogera and Libo Kemkem Districts, Ethiopia, in 2012 reported that thinness was statistically associated with consumption of food from animal sources (OR=0.26; 95% CI=0.10–0.67).2 This might be because animal source foods including milk and milk products are the main sources of protein and fat which are important for the maintenance of appropriate nutritional status.
Conclusions and Recommendations
In this study, the magnitude of stunting, wasting, and underweight was a mild public health problem. Stunting among school-age children was statistically associated with not consuming milk or milk products and not using soap for hand washing. The rate of wasting was high among children who did not consume milk and among those who became sick in the past 2 weeks. The magnitude of underweight among school-age children was statistically associated with the educational status of the father, children’s breakfast eating habit, consumption of milk, and having sickness in the past 2 weeks.
From the result of this study we recommend introduction of interventions aiming at improving the living standard, hygienic practice, intake of milk and milk products, and dietary diversity practice to improve the nutritional status of the school-age children.
Acknowledgment
The authors would like to express our sincere gratitude to those study participants for their willingness to participate in this study.
Funding Statement
There was no financial support for this study.
Abbreviations
AOR, adjusted odds ratio; BAZ, body mass index for age Z-score; BMI, body mass index; CI, confidence interval; COR, crude odds ratio; EDHS, Ethiopian Demographic Health Survey; H/A, height for age; HAZ, height for age Z-score; NCHS, National Centre for Health Statistics; OR, odds ratio; SD, standard deviation; SPSS, Statistical Package for Social Sciences; UNICEF, United National International Children’s Fund; W/A, weight for age; WAZ, weight for age Z-score; WFP, World Food Program; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from the Debre Tabor University Ethical Review committee. The ethical approval and clearance for this study have been obtained from Debre Tabor University College of Health Sciences Institutional Research Ethics Review Committee (IRERC) with reference number of DTU/re/143/98/2019. A permission letter was received from the respective elementary schools. Written informed consent was obtained from each study participant parents/caregivers after explaining the purpose of the study. The right of a participant to withdraw from the study at any time, without any precondition was disclosed unequivocally. Moreover, the confidentiality of information obtained was guaranteed by all data collectors and investigators using code numbers and by keeping the questionnaire locked. The weight and height were measured in private rooms. Nutrition education and counseling were provided to all study participants after the data collection process completed.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. Author publishing agreement: All authors agreed.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Nandy S, Irving M, Gordon D, et al. Poverty, child undernutrition and morbidity: new evidence from India. Bull World Health Organ. 2005;83:210–216. [PMC free article] [PubMed] [Google Scholar]
- 2.Herrador Z, Sordo L, Gadisa E, et al. Cross-sectional study of malnutrition and associated factors among school aged children in rural and urban settings of Fogera and Libo Kemkem districts, Ethiopia. PLoS One. 2014;9(9):e105880. doi: 10.1371/journal.pone.0105880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tariku EZ, Abebe GA, Melketsedik ZA, et al. Prevalence and factors associated with stunting and thinness among school-age children in Arba Minch Health and Demographic Surveillance Site, Southern Ethiopia. PLoS One. 2018;13(11):e0206659. doi: 10.1371/journal.pone.0206659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall A, Kassa T, Demissi T, Degefie T, Lee S. National survey of the health and nutrition of schoolchildren in Ethiopia. Trop Med Int Health. 2008;13(12):1518–1526. doi: 10.1111/j.1365-3156.2008.02168.x [DOI] [PubMed] [Google Scholar]
- 5.WHO. World health organization United Nations The use and interpretation of anthropometry. WHO Tech Rep Ser. 1995;854(9). [PubMed] [Google Scholar]
- 6.WHO, Word Health organization. School policy framework: implementation of the WHO global strategy on diet, physical activity and health. World Health Organization; 2008. [Google Scholar]
- 7.Abudayya A, Thoresen M, Abed Y, et al. Overweight, stunting, and anemia are public health problems among low socioeconomic groups in school adolescents (12–15 years) in the North Gaza Strip. Nutr Res. 2007;27(12):762–771. doi: 10.1016/j.nutres.2007.09.017 [DOI] [Google Scholar]
- 8.Gaur R, Boparai G, Saini K. Effect of under-nutrition on permanent tooth emergence among Rajputs of Himachal Pradesh, India. Ann Hum Biol. 2011;38(1):84–92. doi: 10.3109/03014460.2010.497499 [DOI] [PubMed] [Google Scholar]
- 9.Ethiopia, T.F.D.R.o. Welfare Monitoring Survey (WMS), 2004, Analytical Report. Central Statistical Authority Addis Ababa; 2004 [Google Scholar]
- 10.Ethiopia, T.F.D.R. National Nutrition Strategy, F.M.o. Health., Editor. Addis Ababa; January 2008. [Google Scholar]
- 11.Kraemer KAZ. Nutritional Anemia. Switzerland: Sight and Life press; 2007:1–400. [Google Scholar]
- 12.UNICEF. United Nations Children’s Fund Policy Review: strategy for improved nutrition of children and women in developing countries. New York USA: UNICEF; 2003. [Google Scholar]
- 13.Brooker S, Clements AC, Bundy DA. Global epidemiology, ecology and control of soil-transmitted helminth infections. Adv Parasitol. 2006;62:221–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brundtland GH. Nutrition and infection: malnutrition and mortality in public health. Nutr Rev. 2000;58(2Pt 2):S1–S4; discussion S63–S73. doi: 10.1111/j.1753-4887.2000.tb07797.x [DOI] [PubMed] [Google Scholar]
- 15.Emam S, Mostafa R, Wassef O, et al. Assessment of nutritional status of some primary school children & their awareness in slum areas. Alexandria J Pediatr. 2005;19(1):113–119. [Google Scholar]
- 16.Karim R, Khan MN, Akhtaruzzaman M. Nutritional status of young children in a Bangladesh national nutrition program area, a case study. Bangladesh Dev Stud. 2008;30(1/2):129–136. [Google Scholar]
- 17.Mondal PR, Biswas S, Bose K. Gender discrimination in undernutrition with mediating factors among Bengalee school children from Eastern India. Homo. 2012;63(2):126–135. doi: 10.1016/j.jchb.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 18.Sánchez-Pérez HJ, Hernán MA, Ríos-González A, et al. Malnutrition among children younger than 5 years-old in conflict zones of Chiapas, Mexico. Am J Public Health. 2007;97(2):229–232. doi: 10.2105/AJPH.2005.070409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hs J, Gupta R, Joshi M, Vipul M. Determinants of nutritional status of school children - a cross sectional study in the western region of Nepal. Nutr J IRM. 2011;2(1). [Google Scholar]
- 20.Senbanjo IO, Oshikoya KA, Odusanya OO, et al. Prevalence of and risk factors for stunting among school children and adolescents in Abeokuta, Southwest Nigeria. J Health Popul Nutr. 2011;29(4):364–370. doi: 10.3329/jhpn.v29i4.8452 [DOI] [PMC free article] [PubMed] [Google Scholar]