Abstract
Introduction:
This study aimed to evaluate whether viewing digital treatment simulations influenced orthodontic treatment planning decisions or practitioners’ confidence in their selected plans.
Methods:
Records of 6 patients representing different case types (e.g., missing teeth, crowding, sagittal discrepancies) were collected. A total of 22 orthodontists and 7 orthodontic residents viewed these records and formulated treatment plans for each case, indicating their most recommended plan and up to two alternative plans. After treatment planning each case, digital setups of each treatment plan indicated by the practitioner were shown. The practitioners were then asked if they still recommended their original plan, or if they would now recommend a different plan. Their confidence levels in the success of their plans were recorded before and after viewing the setups.
Results:
After viewing the digital setups, there was a significant change in the treatment plan for 9.2% of the cases. These included modifications like changing the extraction pattern or proposing space closure rather than opening space for an implant. In an additional 14.4% of the cases, treatment plans underwent partial changes, like adding interproximal reduction or temporary anchorage devices. Practitioner confidence levels increased after viewing the setups. In cases where the treatment plan changed, the practitioner’s confidence level in the plan increased the most, and the final confidence level was uniformly high among all practitioners. Practitioners reported the most helpful features of digital setups were the ability to superimpose the setup with the original model, determine the amount of tooth movement needed, check the final incisal relationship (overjet and overbite), and establish the amount of interproximal reduction required.
Conclusions:
Viewing digital setups resulted in changes to the treatment plans in about 24% of the cases. The use of digital setups was associated with higher levels of confidence in the selected plans.
INTRODUCTION
Since Kesling first recommended their use in 1947, diagnostic setups have been used to simulate different treatment options and aid decision making when treatment planning.1 Creating multiple setups to represent different treatment plans can help when considering extraction patterns, interproximal reduction (IPR), anchorage management, and other treatment mechanics.2 Setups also help when presenting the case to the patient and planning treatment with other dentists.3
With the transition to digital study models, diagnostic setups can now be created digitally, which are as accurate and reliable as wax setups.4–7 Working with digital setups offers new advantages that were not possible with plaster, such as the ability to superimpose the setup with the original models and the ability to determine the precise amount of movement for each tooth.8 Many clinicians are already routinely creating digital setups as part of clinical practice because of the increased use of clear aligner therapy and other digital orthodontic techniques (i.e., custom brackets and custom wires).
When designing treatment with any digital orthodontic system, a digital setup must be created to set the final result. Although this digital setup can be seen as a byproduct of the manufacturing process, the setup actually represents an additional data point for clinicians to consider while treatment planning. Some clinicians may already generate multiple digital setups using clear aligner software when deciding between different treatment decisions. For example, in the case of mandibular anterior crowding, the clinician may ask for the first setup to be created with no IPR to evaluate the final proclination of the incisors and overjet, and then decide to add IPR to certain areas for the second setup. Or alternatively, the clinician may ask for one setup with mandibular IPR and then a second setup with the extraction of one mandibular incisor to compare the two options.
Although setups are generally regarded as useful, the magnitude of the effect of these digital setups on treatment planning has yet to be quantified. This study examined whether viewing a digital setup resulted in changes to an orthodontist’s treatment plan or in changes to the orthodontist’s level of confidence in the selected plan.
MATERIAL AND METHODS
This study was reviewed and approved by the University of Washington Institutional Review Board. A panel of four orthodontists reviewed cases treated at the UW Graduate Orthodontics Clinic and selected 6 cases for this study. Cases were selected based on multiple viable treatment options and a range of case difficulties. The panel felt that 6 cases were a reasonable number to ask a practitioner to the treatment plan without occupying too much time or causing fatigue.
Assembled records included intraoral and extraoral photos, panoramic and lateral cephalometric radiographs, cephalometric tracing and measurements, Bolton analysis, and digital models of the teeth. The digital models were imported into SureSmile software (OraMetrix, Richardson, TX) to generate digital setups. The same panel of four orthodontists identified as many potential treatment plans as possible for each case so that these setups could be prepared in advance. For 6 cases, a total of 44 digital setups were created, with an average of 7 setups per case. Each setup was reviewed by at least three orthodontists on the panel to ensure they simulated realistic biomechanics and anchorage management. Examples of digital setups in the software can be seen in Figures 1 and 2.
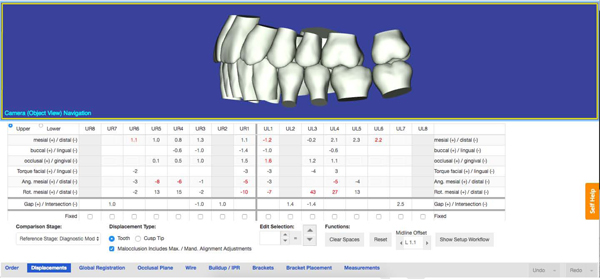
Figure 1:
Digital setup with tooth movement chart showing the exact movements of each tooth in the maxillary arch. In this case, the maxillary left second molar was not moved in order to indicate the anchorage loss required visually.
Figure 2:
Overlay of the initial (teal) and final (white) tooth positions of the maxillary arch for bilateral canine substitution in a case with missing maxillary lateral incisors. The maxillary second molars were not moved to visualize anchorage loss needed.
In order to participate, practitioners must be enrolled in or have graduated from an orthodontic residency program and must not have been involved with the treatment of any of the cases selected for the study.
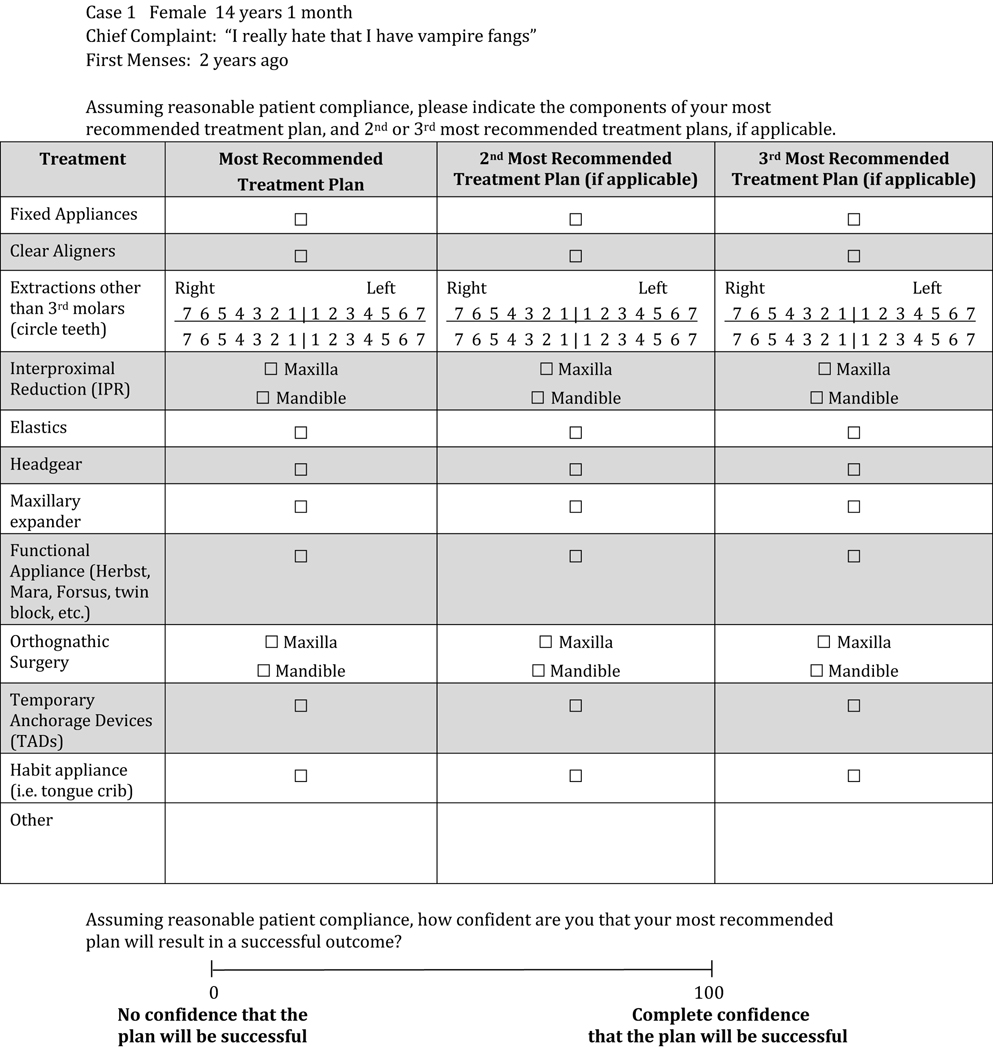
Orthodontists were shown the records of the 6 selected cases in random order. Upon viewing the records, orthodontists were asked to list up to 3 treatment plans (the most recommended plan, the second most recommended plan, and the third most recommended plan) using a treatment planning worksheet (Figure 3). Practitioners were asked to indicate their confidence level in the successful outcome of their most recommended plan on a visual analogue scale.
Figure 3:
Treatment Planning Worksheet, Part 1
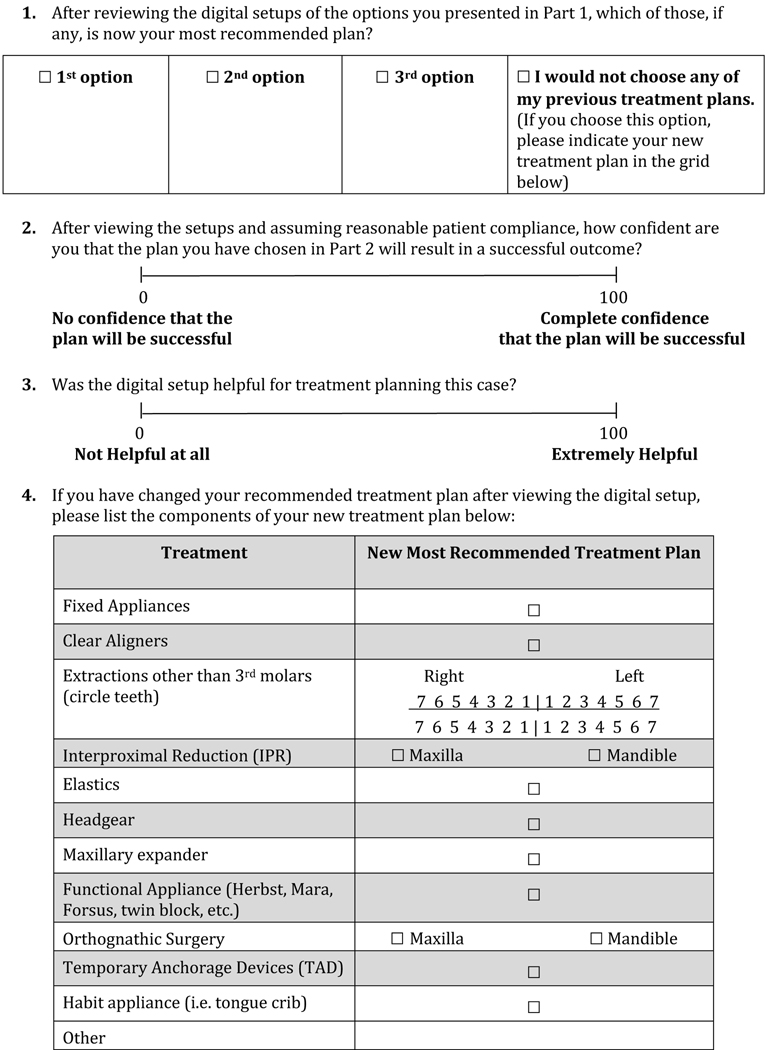
After writing down their treatment plans, practitioners were shown the digital setups for only the plans that they had indicated on the treatment planning worksheet. If a practitioner proposed a treatment plan that had not been previously anticipated, the setup was created and shown to the practitioner within several days. After viewing the setups, practitioners were asked which plan was now their most recommended treatment plan and to state their confidence level in the successful outcome of this plan (Figure 4).
Figure 4:
Treatment Planning Worksheet, Part 2
Based on simulation modeling, a sample size of 29 orthodontists and orthodontic residents was set. This number of participants would provide an expected margin of error between 5% and 6% if the probability of switching treatment plans after viewing digital setups was between 10% and 30%.
For further statistical analysis, the orthodontists were divided into three groups: current residents, those with ≤5 years in practice, and those with >5 years in practice. The study was focused on answering three specific questions: (1) how often did practitioners change their most recommended plan after viewing the setups; (2) did practitioners’ confidence level in their treatment plan change after viewing the setups; and (3) did the rate of treatment plan change and confidence level change differ among the three groups of orthodontists.
Data were analyzed using SPSS version 19 (IBM Corp, Armonk, NY). The probability of changing the most recommended treatment plan and associated confidence intervals were estimated using a binomial regression model with a log link using a generalized estimating equation for accounting multiple observations per practitioner. This technique was also used to compare changes among the different experience levels. A linear regression on change in confidence using a generalized estimating equation was used with case and plan change incorporated into the model to determine the change in the confidence interval.
RESULTS
A total of 29 practitioners were recruited to participate in this study. The practitioners were stratified into 3 groups based on experience (Table I), with 7 second- or third-year orthodontic residents (residents), 13 orthodontists with 5 or fewer years in practice (newer practitioners), and 9 orthodontists with more than 5 years in practice (experienced practitioners). The group of newer practitioners had an average of 2.1 years in practice with a range of 1 to 4 years of experience. The group of experienced practitioners had an average of 25.1 years in practice with a range of 8 to 40 years of experience.
Table I:
Description of practitioners in the study
| Parameters | No. of practitioners | Average years in practice (range) | Average years in residency |
|---|---|---|---|
| Residents | 7 | 2.3 (2–3) | |
| ≤5 years in practice | 13 | 2.1 (1–4) | |
| >5 years in practice | 9 | 25.1 (8–40) |
The six cases selected for study and the top two most recommended treatment plans by the practitioners in the study are described in Table II. Of the 6 cases selected, 3 were adolescent patients and 3 were adult patients. In addition, 3 cases were Class I, 2 cases were Class II, and 1 case was a Class III tendency.
Table II:
Description of cases and most recommended treatment plans.
| Case no. | Description of case | Most recommended treatment plans |
|---|---|---|
| 1 | 15-year-old female, Class I, full profile, proclined incisors, mild maxillary and mandibular crowding | (1) Extract all first premolars (2) Extract all second premolars |
| 2 | 21-year-old female, Class I, thin upper lip, 95% overbite, moderate mandibular anterior crowding | (1) Non-extraction with mandibular IPR (2) Extract one mandibular incisor |
| 3 | 36-year-old male, Class I, excess overjet and overbite, retained maxillary left primary canine, missing maxillary left permanent canine, missing one mandibular incisor, moderate mandibular arch length deficiency | (1) Replace missing UL3 with an implant and maxillary IPR (2) Close UL3 space by protracting maxillary left posterior teeth |
| 4 | 13-year-old male, Class II subdivision, straight profile, thin lips, severe maxillary and mandibular crowding | (1) Extract all first premolars (2) Extract 4 over 5 on right and 4 over 4 on left |
| 5 | 12-year-old female, end-on Class II, convex profile, thin lips, excess overjet, minimal overbite, and missing maxillary lateral incisors | (1) Bilateral canine substitution to close missing lateral incisor space (2) Open space for maxillary lateral implants |
| 6 | 48-year-old female, Class III tendency, increased overjet and overbite, severe mandibular anterior crowding, recently extracted tooth #10 due to root fracture | (1) Non-extraction with mandibular IPR (2) Extract one mandibular incisor |
In this study, 29 practitioners made treatment plans for each of the 6 cases, generating a total of 174 most recommended treatment plans. After the practitioners viewed digital setups, the most recommended plan was substantially changed 16 times (9.2%). These major changes were a change in extraction pattern or change from opening space for implants to closing space for bilateral canine substitution. There were an additional 25 partial changes to treatment plans (14.4%), such as adding or removing IPR, adding temporary anchorage devices or miniscrews to help with anchorage, or switching from clear aligners to fixed appliances or vice versa. In total, the treatment plan was modified in 41 out of 174 cases, resulting in an overall change rate of 23.6% (Table III). When the treatment plan change rate was analyzed on the basis of the level of practitioner experience, the difference in change rate based on experience was not statistically significant.
Table III:
Changing treatment plan by practitioner experience
| Parameters | n | Changing (%) | Relative risk of changing | 95% confidence interval | P* | |
|---|---|---|---|---|---|---|
| Residents | 7 | 21.4 | 1 | - | - | 0.199 |
| ≤ 5 years in practice | 13 | 29.5 | 1.38 | 0.82 | 2.32 | |
| > 5 years in practice | 9 | 16.7 | 0.80 | 0.38 | 1.65 | |
| Total | 29 | 23.6 | ||||
Adjusted for case in binomial regression model with log link using a generalized estimating equation for accounting of multiple observations per judge
When practitioners were asked, “How confident are you that your most recommended plan will result in a successful outcome?” on a visual analogue scale, there was an overall confidence level of 83 before viewing the digital setups and 89 after viewing the digital setups (Table IV). Case 3 had the largest change in confidence level, going from 74 to 87, and Case 1 had the smallest change in confidence level, going from 89 to 90. When the treatment plan did not change, the confidence level increased from 84 to 89, whereas when the treatment plan did change, the confidence level increased from 77 to 88. When broken out by experience level of the practitioner, residents had the lowest initial confidence level of 72 compared with a confidence level of 86 for newer and experienced practitioners. The final confidence levels in all 3 groups increased to 81 for residents, 91 for newer orthodontists, and 92 for experienced orthodontists.
Table IV:
Change in confidence level before and after viewing setups
| Confidence before |
Confidence after |
Change in confidence |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameters | n | Mean (%) | 95% CI | P* | Mean (%) | 95% CI | P* | Mean (%) | 95% CI | P* | |||
| Total | 174 | 83 | 78 | 87 | 89 | 86 | 91 | 6 | 4 | 9 | <0.001** | ||
| Case | |||||||||||||
| 1 | 29 | 89 | 85 | 93 | <0.001 | 90 | 86 | 93 | 0.001 | 1 | −2 | 4 | <0.001 |
| 2 | 29 | 85 | 80 | 90 | 92 | 89 | 95 | 7 | 3 | 10 | |||
| 3 | 29 | 74 | 67 | 81 | 87 | 83 | 90 | 13 | 8 | 18 | |||
| 4 | 29 | 83 | 79 | 87 | 86 | 82 | 90 | 3 | −0.2 | 6.7 | |||
| 5 | 29 | 81 | 76 | 87 | 89 | 85 | 93 | 8 | 4 | 12 | |||
| 6 | 29 | 83 | 76 | 90 | 90 | 86 | 93 | 7 | 2 | 12 | |||
| Change in treatment plan | |||||||||||||
| Kept original plan | 133 | 84 | 80 | 88 | 0.003 | 89 | 86 | 92 | 0.37 | 5 | 3 | 7 | 0.003 |
| Changed plan | 41 | 77 | 71 | 84 | 88 | 84 | 91 | 10 | 6 | 15 | |||
| Experience of practitioners | |||||||||||||
| Residents | 42 | 72 | 60 | 83 | 0.067 | 81 | 76 | 86 | <0.001 | 9 | 1 | 18 | 0.55 |
| ≤ 5 years in practice | 78 | 86 | 82 | 91 | 91 | 88 | 94 | 5 | 3 | 7 | |||
| > 5 years in practice | 54 | 86 | 81 | 91 | 92 | 89 | 95 | 6 | 3 | 9 | |||
Linear regression using generalized estimating equations
Comparing before vs. after
When practitioners were asked which features of the digital setup were most helpful in treatment planning these cases, the top four responses were the abilities to: superimpose the setup with the original model, determine the amount of tooth movement needed, check the final incisal relationship (overjet and overbite), and plan the amount of IPR required.
DISCUSSION
Revisiting our original hypotheses, practitioners made a substantial change in 9.2% of cases after viewing the digital setups. Changes include changing from extracting second premolars to first premolars, from symmetrical to asymmetrical premolar extractions, from non-extraction with IPR to extracting one mandibular incisor, and from opening space for lateral incisor implants to closing space for canine substitution. Some of these changes are irreversible, such as a change in extraction pattern, whereas other changes would decrease efficiency and increase treatment time, such as closing space instead of opening space.
When all changes to treatment plans are included, practitioners made at least some change in 23.6% of cases, such as adding or removing IPR or adding temporary anchorage devices to help with anchorage requirements. These findings indicate that setups have a strong impact on treatment planning, especially for more challenging cases. Although many of these changes could have been made during the treatment, knowing the definitive treatment plan from the start could result in more efficient treatment and decreased treatment time.
As this study was based on 6 cases that are slightly more challenging, the change rate that we found might be lower when applied to a more general patient population. However, the benefits of evaluating a digital setup as part of the treatment planning process would still hold.
Overall, practitioners’ confidence levels in their treatment plan increased after viewing the setups. The greatest increase in confidence level was found when the practitioner started with a lower initial confidence level, which occurred in 3 main categories of situations–a difficult case, an eventual change in treatment plan after viewing the setups, and among residents. Case 3 had the lowest initial confidence level and the biggest gain in confidence after viewing the setup. This case was an adult interdisciplinary case involving a missing maxillary canine and mandibular incisor. This case was the most complex one in the study, so it was no surprise that practitioners had the lowest initial confidence in their treatment plan for this case.
The second category describes practitioners who changed their plans after viewing the setup. These practitioners might have lacked confidence in their plans to begin with, which more readily led to their change in most recommended treatment plan after viewing the setup. Finally, residents had the lowest initial confidence level of the three experience level groups, and subsequently had the largest increase in confidence after viewing the setup. Regardless of what the initial confidence level was, the final confidence level was uniformly high for all individuals after viewing the setups. The setups helped to bridge the gap in confidence level and allowed practitioners to have a stronger level of confidence in their treatment plan, even if they began with a lower confidence level.
As other authors have stressed,3 a setup is only realistic and helpful if it can simulate the practitioner’s treatment goals. For some of the setups, practitioners wanted to modify how the setup was created. However, because all the setups were created ahead of time for this study, we were unable to modify the setup to the exact preferences of each practitioner. The most common desire was to increase or decrease the amount of IPR. This lack of customization unlikely affected the results of this study but conveyed the importance of allowing the treating orthodontist to be able to quickly and easily modify the parameters of the digital setup to suit their treatment goals.
During the study, practitioners proposed 10 treatment plans that were not initially identified by the panel. Once digital setups were created for these 10 treatment plans and shown to the practitioners who suggested them, the practitioners generally remarked that their recommended plan was unreasonable or that they initially missed something when treatment planning the case. None of these 10 treatment plans were selected as the most recommended plan after viewing the setups. Interestingly, the digital setup served its purpose, as it helped practitioners recognize shortcomings in those proposed plans. For example, for Case 6, the patient had a slight Class III tendency. A small number of practitioners selected extraction of the mandibular right first premolar or extraction of both mandibular first premolars as a treatment plan. After viewing the setups, these same practitioners realized that the Class III relationship was not as significant as they had thought and that there was too much space to close. Therefore, they did not select these plans in the end. This finding also validated the work of the panel before recruiting practitioners, as all of the treatment plans finally selected by the practitioners were predicted ahead of time.
Previous studies have examined the effect of each component of the records on treatment planning,9 and the digital setup appears to have as much of or an even greater effect than other records that are routinely taken. Nijkamp et al10 examined the effect of lateral cephalometric radiographs and found no significant differences in treatment planning with or without cephalometric information for adolescents with Class II Division 1 malocclusion. Han et al11 examined the incremental benefit of facial photographs, panoramic radiograph, lateral cephalogram, and cephalometric tracing on treatment planning and found that the majority of cases (55%) could be treatment planned with study models alone and that each of the other records provided had a small benefit. When treatment planning a case with impacted maxillary canines, Haney et al12 found that the 3-dimensional cone-beam computed tomography image changed the treatment plan for the impacted tooth 27% of the time when compared with conventional 2-dimensional radiographs.12
These findings suggest that setups have a strong impact on treatment planning, especially for more challenging cases and software which allows setups to be created simply, quickly, and accurately, could make digital setups a routine and desirable part of the treatment planning process.
CONCLUSIONS
Viewing the digital setups resulted in a substantial change in treatment plans for 9.2% of cases in this study and a partial change in 14.4% of cases.
Viewing the digital setups increased the overall confidence level of the practitioners, especially for challenging cases and residents.
Creating digital setups could be a helpful addition to the treatment planning process and could be routinely incorporated in the future as more practices adopt digital intraoral scanners, and as the digital setup software improves.
ACKNOWLEDGEMENTS
This study was supported by the University of Washington Orthodontic Alumni Association and, by the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under Award Number KL2TR000421. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
SureSmile provided assistance with creating the digital setups and did not provide direct funding. Align Technology provided the use of an iTero digital scanner for one year and did not provide direct funding.
All authors completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the following were reported: Dr. Huang reports non-financial support from SureSmile and from Align Technology during the conduct of the study; Dr. Hou reports non-financial support from SureSmile (OraMetrix) and from Align Technology, during the conduct of the study. The other authors had nothing to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Kesling HD. Coordinating the predetermined pattern and tooth positioner with conventional treatment. Am J Orthod Dentofacial Orthop 1946;32:285–93. [DOI] [PubMed] [Google Scholar]
- 2.Kesling HD. The diagnostic setup with consideration of the third dimension. Am J Orthod Dentofacial Orthop 1956;42:740–8. [Google Scholar]
- 3.Mattos CT, Gomes AC, Ribeiro AA, Nojima LI, Nojima MCG. The importance of the diagnosticsetup in the orthodontic treatment plan. Int J Orthod Milwaukee 2012;23:35–9. [PubMed] [Google Scholar]
- 4.Peluso MJ, Josell SD, Levine SW, Lorei BJ. Digital models: An introduction. Semin Orthod 2004;10:226–38. [Google Scholar]
- 5.Macchi A, Carrafiello G, Cacciafesta V, Norcini A. Three-dimensional digital modeling and setup. Am J Orthod Dentofacial Orthop 2006;129:605–10. [DOI] [PubMed] [Google Scholar]
- 6.Kihara T, Tanimoto K, Michida M, Yoshimi Y, Nagasaki T, Murayama T, et al. Construction of orthodontic setup models on a computer. Am J Orthod Dentofacial Orthop 2012;141:806–13. [DOI] [PubMed] [Google Scholar]
- 7.Im J, Cha JY, Lee KJ, Yu HS, Hwang CJ. Comparison of virtual and manual tooth setups with digital and plaster models in extraction cases. Am J Orthod Dentofacial Orthop 2014;145:434–42. [DOI] [PubMed] [Google Scholar]
- 8.Barreto MS, Faber J, Vogel CJ, Araujo TM. Reliability of digital orthodontic setups. Angle Orthod 2016;86:255–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rischen RJ, Breuning KH, Bronkhorst EM, Kuijpers-Jagtman AM. Records Needed for Orthodontic Diagnosis and Treatment Planning: A Systematic Review. PloS One 2013;8:e74186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nijkamp PG, Habets LL, Aartman IH, Zentner A. The influence of cephalometrics on orthodontic treatment planning. Eur J Orthod 2008;30:630–5. [DOI] [PubMed] [Google Scholar]
- 11.Han UK, Vig KW, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofacial Orthop 1991;100:212–9. [DOI] [PubMed] [Google Scholar]
- 12.Haney E, Gansky SA, Lee JS, Johnson E, Maki K, Miller AJ, et al. Comparative analysis of traditional radiographs and cone-beam computed tomography volumetric images in the diagnosis and treatment planning of maxillary impacted canines. Am J Orthod Dentofacial Orthop 2010;137:590–7. [DOI] [PubMed] [Google Scholar]