Introduction
The coronavirus disease 2019 (COVID-19) pandemic exemplifies the potential clash between policy, governance, and public health.1 Physicians and other healthcare professionals have critical expertise and important experiences to help shape public policy, yet, historically, have been less likely to engage in the political process as measured by their propensity to vote.2 We examine whether previous trends in low physician voter turnout persist, contrasting to similar occupational groups and the general population.
Methods
Data were from the 2004–2018 Current Population Survey (CPS) November Voter Supplement,3 a biennial nationally representative household survey that collects self-reported or reports by proxy (household member) voting rates and behavior from congressional and presidential elections. We identified five representative healthcare professionals (physicians, dentists, pharmacists, registered nurses, physician assistants) and five other comparison professions (postsecondary teachers, chief executives, civil engineers, social workers, lawyers) selected by similarities in income or educational backgrounds. The remaining population was considered the general public. Adjusted risk ratios (aRR) were estimated from multivariable logistic regressions comparing voting rates and behavior across occupations controlling for the year and sociodemographic characteristics associated with voting.4 To account for missing variables of income, duration at residence, and rural location (about 15% of the analysis sample), multiple imputation with five replications using chained equations was employed. All analyses were performed using STATA version 15 (StataCorp). Public, de-identified data is exempt from review by the University of Michigan institutional review board.
Results
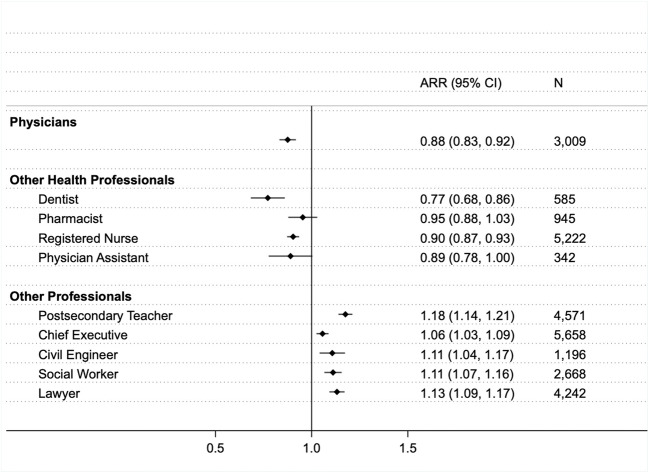
The pooled sample of US citizens age 18 and older (N = 750,236) included 3009 physicians, mean age 47.6 (SD, 14.9) years, 33.5% women (Table 1). Household-level response rates ranged from 84 to 92%. Physicians and other healthcare providers were significantly less likely to vote than comparison professions or the public after controlling for characteristics associated with voting (Fig. 1). Compared to the public, adjusted physician voting rates were 12% lower than expected: aRR of 0.88 (95% confidence interval [CI], 0.83–0.92) whereas comparison professions all demonstrated significantly higher voting rates, with postsecondary teachers showing the highest rates, aRR 1.18 (1.14–1.21). Physicians also exhibited different voting behaviors compared to the public. Physicians were 30% more likely to vote by mail, aRR 1.32 (1.12–1.42), and 15% more likely to vote prior to election day, aRR 1.15 (1.06–1.25). Physicians who did not vote or register were 70% more likely to report this was due to being “Too busy, conflicting work or school,” compared to the public, aRR 1.7 (1.36–1.96).
Table 1.
Characteristics of Participants by Physician vs. General Public
| General public | Physician | p value | |||||
|---|---|---|---|---|---|---|---|
| N = 747,227 | [95% CI] | N = 3009 | [95% CI] | ||||
| Age (SD) | 47.17 ( 20.61) | 47.64 (14.9) | 0.4 | ||||
| Female | 52.1% | 52.0% | 52.3% | 33.5% | 31.6% | 35.5% | < 0.001 |
| Married | 53.7% | 53.6% | 53.9% | 77.8% | 76.1% | 79.5% | < 0.001 |
| Non-rural | 84.0% | 83.9% | 84.1% | 92.7% | 91.8% | 93.7% | |
| Children in household | 37.5% | 37.4% | 37.6% | 52.2% | 50.2% | 54.2% | |
| Employed | 61.9% | 61.8% | 62.0% | 99.1% | 98.7% | 99.5% | |
| Race/ethnicity | |||||||
| White | 71.5% | 71.4% | 71.7% | 71.7% | 69.8% | 73.6% | < 0.001 |
| Black | 12.0% | 11.9% | 12.1% | 5.2% | 4.2% | 6.2% | |
| Native American | 0.7% | 0.7% | 0.7% | 0.2% | 0.0% | 0.4% | |
| Asian | 3.8% | 3.7% | 3.8% | 15.7% | 14.1% | 17.2% | |
| Other | 1.5% | 1.5% | 1.5% | 1.3% | 0.8% | 1.7% | |
| Hispanic | 10.5% | 10.4% | 10.6% | 6.0% | 4.9% | 7.0% | |
| Region | |||||||
| Northeast | 18.2% | 18.1% | 18.3% | 22.0% | 20.3% | 23.8% | < 0.001 |
| Midwest | 22.6% | 22.5% | 22.7% | 21.1% | 19.5% | 22.8% | |
| South | 37.1% | 37.0% | 37.2% | 34.6% | 32.7% | 36.6% | |
| West | 22.1% | 22.0% | 22.2% | 22.2% | 20.5% | 23.8% | |
| Household income | |||||||
| <20K | 15.7% | 15.6% | 15.8% | 1.7% | 1.1% | 2.3% | < 0.001 |
| 20–35K | 16.8% | 16.7% | 16.9% | 1.9% | 1.4% | 2.5% | |
| 35–50K | 14.1% | 14.0% | 14.2% | 4.1% | 3.2% | 5.0% | |
| 50–75K | 19.6% | 19.5% | 19.7% | 8.2% | 7.0% | 9.3% | |
| ≥ 75K | 33.8% | 33.7% | 33.9% | 84.0% | 82.4% | 85.7% | |
| Duration of residence | |||||||
| < 1 year | 13.7% | 13.6% | 13.8% | 13.1% | 11.5% | 14.8% | < 0.001 |
| 1–5 years | 27.1% | 27.0% | 27.2% | 30.7% | 28.8% | 32.7% | |
| > 5 years | 59.2% | 59.1% | 59.3% | 56.1% | 54.0% | 58.3% | |
| Education | |||||||
| High school or less | 41.3% | 41.2% | 41.4% | 0.8% | 0.5% | 1.2% | < 0.001 |
| Some college | 29.6% | 29.5% | 29.7% | 1.7% | 1.2% | 2.2% | |
| Bachelor’s degree | 19.4% | 19.3% | 19.5% | 2.3% | 1.6% | 2.9% | |
| Graduate degree | 9.7% | 9.6% | 9.8% | 95.2% | 94.3% | 96.1% | |
Note: The imputed dataset accounting for missing variables of income, duration at residence, and rural location was used for this tabulation. P values were calculated based on Pearson’s chi-squared test for the hypothesis that the distribution of each covariate is independent from the groups—general public vs. physician group
Figure 1.
Adjusted risk ratio for voting by physicians, healthcare professionals, and non-healthcare professionals compared to the general public, 2004–2018. Note: The total number of respondents was 750,236 individuals including 3009 physicians, 7094 healthcare professionals, and 18,335 non-healthcare professionals. Adjusted risk ratio (ARR) is estimated from multivariable logistic regression against the comparison group of the general population, controlling for the following: year, household income, age, gender, marital status, rural, employment, race/ethnicity, education, duration at residence, region, and number of children.
Discussion
Over 2004–2018, adjusted analysis find physicians and other healthcare professionals were significantly less likely to vote, whereas comparative professions were more likely to vote than the general public. As noted in other studies,5 this may be for a variety of reasons: inflexibility of clinical schedules and responsibilities, transient and intense nature of medical training distances trainees from their community, ambivalence towards advocacy, intrinsic social value of medicine as a substitute to other community-engagement responsibilities. Indeed, physicians in this study were more likely to attribute not voting to work commitments and instead were more likely to use early voting and vote by mail. Whether Election Day flexible scheduling, healthcare organization campaigns to emphasize the social value of voting, voter registration drives, and education on mail-in voting can improve healthcare professional voting rates merits further research. Study limitations were reliance on self-reported data, no information on other civic activities, and limited details of barriers to voting. Civil society is better when all citizens participate in the political process by voting. As the COVID-19 pandemic has revealed, healthcare professionals have important expertise and experiences that should be used to inform and shape public policy.
Authors’ Contributions
Dr. Solnick had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Solnick, Choi
Acquisition, analysis, or interpretation of data: Solnick, Choi, Kocher
Drafting of the manuscript: Solnick, Choi, Kocher
Critical revision of the manuscript for important intellectual content: Solnick, Choi, Kocher
Statistical analysis: Solnick, Choi
Obtained funding: Solnick
Administrative, technical, or material support: Solnick, Kocher
Supervision: Kocher
Funding
Dr. Solnick was supported by the University of Michigan National Clinician Scholars Program at the Institute for Healthcare Policy and Innovation.
The University of Michigan National Clinical Scholars Program but had no role in the conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; the decision to submit the manuscript for publication; or the decision as to which journal the manuscript was submitted. No other funding sources had a role in the study.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rachel E. Solnick, Email: solnick@umich.edu.
Hwajung Choi, Email: hwajungc@med.umich.edu.
Keith E. Kocher, Email: kkocher@med.umich.edu.
References
- 1.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff. Published online May 14, 2020:101377hlthaff202000608. 10.1377/hlthaff.2020.00608 [DOI] [PubMed]
- 2.Grande D, Asch DA, Armstrong K. Do doctors vote? J Gen Intern Med. 2007;22(5):585–589. doi: 10.1007/s11606-007-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flood S, King M, Rodgers R, Ruggles S, Warren JR. Integrated Public Use Microdata Series, Current Population Survey: Version 7.0 [dataset]. Published online 2020. 10.18128/D030.V7.0
- 4.File T. Who Votes? Congressional Elections and the American Electorate: 1978–2014. US Census Bureau; 2015. https://www.census.gov/content/dam/Census/library/publications/2015/demo/p20-577.pdf. Accessed 21 Sept 2020.
- 5.Grande D, Armstrong K. Community volunteerism of US physicians. J Gen Intern Med. 2008;23(12):1987–1991. doi: 10.1007/s11606-008-0811-x. [DOI] [PMC free article] [PubMed] [Google Scholar]