Abstract
Objective
Information about the adverse effects of the COVID-19 pandemic on adolescent and adult mental health is growing, yet the impacts on preschool children are only emerging. Importantly, environmental factors that augment or protect from the multidimensional and stressful influences of the pandemic on emotional development of young children are poorly understood.
Methods
Depressive symptoms in 169 preschool children (mean age 4.1 years) were assessed with the Preschool Feelings Checklist during a state-wide stay-at-home order in Southern California. Mothers (46% Latinx) also reported on externalizing behaviors with the Strengths & Difficulties Questionnaire. To assess the role of environmental factors in child mental health we examined household income, food insecurity, parental essential worker status and loss of parental job, as well as preservation of the structure of children's daily experiences with the Family Routines Inventory.
Results
Sixty-one percent of families' incomes were below the living wage and 50% had at least one parent who was an essential worker. Overall, preschoolers’ depressive and externalizing symptoms were elevated compared to pre-COVID norms. Practice of family routines robustly predicted better child mental health, and this protective effect persisted after covarying income, dual-parent status and food insecurity as well as maternal depression and stress.
Conclusion
The stress of the COVID-19 pandemic is exacting a significant toll on the mental health of preschool children. Importantly, maintaining a structured, predicable home environment by adherence to family routines appears to mitigate these adverse effects, providing empiric basis for public health recommendations.
Keywords: Stress, Trauma, Family routines, Depression, Conduct disorders, Early life adversity, Resilience, Pandemic, Child psychopathology
Abstract.
1. Introduction
Since the diagnosis of the first case of novel corona virus (COVID-19) in December of 2019, countries across the globe have been confronted with the largest public health crisis in the last century. In an effort to control the spread of the virus and the rapidly rising death toll, governments have implemented physical distancing and stay-at-home orders that have not only resulted in social isolation, but also soaring levels of unemployment and pervasive threats to financial well-being. Not surprisingly the pandemic appears to be negatively affecting the mental health of adults around the world and has been linked to increases in stress, loneliness, anxiety and depression (Wang et al., 2020; Twenge and Joiner, 2020).
While there is an emerging body of empirical studies focused on the adverse consequences for mental health of adults, less attention has been paid to understanding how this global catastrophe is affecting children, not only in terms of learning loss, but also for their mental health. However, speculation is widespread that the adverse effects will be pervasive and lasting (Golberstein et al., 2020; Roubinov et al., 2020). Children's health and well-being is dependent on the health and well-being of the family unit (Bronfenbrenner and Ceci, 1994) and this dependency may be even more pronounced in the context of the pandemic, when children no longer have access to external support systems such as those provided by daycare and school. It is likely that child well-being will be affected through disruptions to family relationships, detrimental effects on caregiver mental health and parental stress related to concerns about infection and illness, social distancing, stay at home orders and the widespread financial uncertainty that many families face (Prime et al., 2020).
Although the acute and persisting effects of the COVID-19 pandemic on children are unknown, there is evidence that other significant stress exposures such as natural disasters and macroeconomic crises profoundly affect family dynamics and leave a lasting imprint on children's development and mental health (Fonseca et al., 2016; Masten and Narayan, 2012). Previous disaster research suggests that exposed children exhibit emotional and behavior problems including aggression, anxiety, depression and PTSD (Felix et al., 2011; Durkin et al., 1993; Scott et al., 2014). Consistent with these findings, emerging data from the COVID-19 pandemic in China indicate that among primary school-aged children, mental health may be suffering (Duan et al., 2020; Xie et al., 2020). These adverse effects may be dependent on developmental period, and the effects on young children, who are experiencing rapid social and emotional development remain to be determined. Some of the first data to inform mental health in this age group are from the Rapid Assessment of Pandemic Impact on Development Early Childhood Household Survey Project (RAPID-EC), which began distributing weekly surveys in early April 2020 to a large representative sample of US households with children under 5. Findings from these surveys demonstrate that the COVID-19 pandemic was associated with elevations in child behavior problems and anxiety that were more pronounced among racial-ethnic minority families and economically disadvantaged households (Center for Translational Neuroscience, 2020a; Center for Translational Neuroscience, 2020b).
There is no question that COVID-19 has disrupted daily life and profoundly increased uncertainty about the future for many families. Given that there is some evidence that unpredictability in early life constitutes a significant source of stress that may contribute to disrupted neurodevelopment and risk for psychopathology (Davis et al., 2017; Glynn et al., 2019; Short and Baram, 2019; Glynn and Baram, 2019), it seems likely that this may be one pathway adversely affecting child mental health. Although many of the possible contributors to unpredictability in the family system are not readily modifiable (e.g. job loss, poverty), family routines represent one aspect of the family environment that is amenable to change. There exists empirical work highlighting the positive effects of family rituals and routines for optimizing child health and development (Fiese et al., 2002). There also is evidence specifically indicating that the routines may serve as protective factors in the context of significant challenge and adversity. For example, in families experiencing chronic illness, alcoholism or divorce, family routines predict child resilience (Crespo et al., 2013; Guidubaldi et al., 1986; Wolin and Bennett, 1984; Betancourt et al., 2013). Although these literatures suggest that routines might also be beneficial in the context of disaster, there is a lack of evidence documenting whether family routines exert similarly protective influences on children's mental health in the context of such crises. This seems an especially important question given that there are unique aspects of a global pandemic that undermine typical protective factors increasing the importance of the family context. Public health recommendations such as physical distancing and stay-at-home orders have reduced access to external support systems (e.g. childcare providers, extended family, teachers) and resulted in the loss of important developmental events and milestones (birthday parties, playdates, organized sports) for children. Our view is that family routines represent a promotive factor because of their associations with resilience in both low and high-risk conditions (Masten and Narayan, 2012; Hostinar and Miller, 2019) and thus we hypothesize that they will exert positive influences even during the distinct circumstances of the COVID-19 pandemic.
Consistent with other recent conceptualizations in the literature (Prime et al., 2020; Masten and Motti-Stefanidi, 2020; Stark et al., 2020), the design of this study rests on the assumption that the COVID-19 pandemic presents a significant multisystem challenge to families that will likely have pervasive negative effects on mental health and well-being and further that the identification of factors that support resilience in the face of the pandemic is critical. Within this context, the study had two goals: First, to investigate mental health symptoms in American preschool children during the COVID-19 pandemic. Second, to test the hypothesis that maintenance of family routines serves as a protective factor for children's mental health during the pandemic crisis.
2. Methods
Study participants included 169 mother-child pairs who are part of an ongoing longitudinal study examining prenatal and early life influences and child development conducted in Southern California (CA; N = 203). An online survey was initially distributed on May 5, 2020 and those mothers who completed the survey by June 9, 2020 were included in the analyses (N = 169). The participants were contacted via text and email and were compensated $30 for completion of the survey. The mothers who completed the survey were older and their household incomes were higher than the mothers who did not, but they did not differ in terms of race/ethnicity or likelihood that they were living with the child's father. On March 19, 2020, CA Governor Gavin Newsom issued a statewide stay at home order in which residents were instructed to stay at home indefinitely and to leave only for essential work, errands and outdoor exercise. This stay at home order was in place until May 8th, when Governor Newsom announced that the state was moving to early Stage 2, which allowed the opening (with public health safety modifications) of select businesses and services including: curbside retail, logistics and office-based businesses where remote work was not possible. By the end of May 2020, all counties in southern CA had approval from the Governor's office to move into late stage 2, which included further opening of establishments such as dine in restaurants and salons. Therefore, the survey was completed at the conclusion of the 7-week stay at home order, as CA began the first stages of reopening.
2.1. Participants
At the time of the survey, the mean child age was 4.1 years and ranged from 2.6 to 6.0 years. Eighty three percent of the households were dual parent and the predominant racial-ethnic identification of the parents was Latinx. The majority of the families lived in Orange County (68.0%), with the next most common counties of residence being Los Angeles (10.7%) and Riverside (8.3%). The pre-pandemic median annual household income was $60,000 (range $6000 to $650,000) and 61% of the families were living below the estimated living wage for their county of residence (estimated living wage for a family of four: Orange, $87,715; Los Angeles, $84,352; Riverside, $76,708) (Living Wage Calculator. M, 2020). Additional description of the families is provided in Table 1.
Table 1.
Family characteristics.
| n (%), Mean (SD), or Median | |
|---|---|
| Maternal Education Level (n,%) | |
| High School or Less | 38 (22.5) |
| Some College, Associates or Vocational Degree | 71 (42.0) |
| College Degree | 27 (16.0) |
| Graduate Degree | 33 (19.5) |
| Maternal Race/Ethnicity (n,%) | |
| Latina | 77 (45.6) |
| Non-Hispanic White | 55 (32.5) |
| Asian | 18 (10.7) |
| Multi-Ethnic | 12 (7.1) |
| Paternal Education Level (n,%) | |
| High School or Less | 60 (40.3) |
| Some College, Associates or Vocational Degree | 40 (26.8) |
| College Degree | 25 (16.7) |
| Graduate Degree | 24 (16.1) |
| Paternal Race/Ethnicity (n,%) | |
| Latino | 81 (47.9) |
| Non-Hispanic White | 54 (32.0) |
| Asian | 19 (11.2) |
| Multi-Ethnic | 10 (5.9) |
| Dual Parent Household (n,%) | 140 (83.3) |
| Annual Household Income (Median US $) | 60,000 |
| Internet Access in Home (n,%) | 165 (97.6) |
| Food Insecure Household (n,%) | 50 (29.6) |
| Pandemic Work Status (n,%) | |
| At Least One Parent Currently Working for Paya | 139 (82.2) |
| Both Parents Currently Working for Paya | 53 (31.4) |
| At Least One Parent an Essential Worker | 85 (50.3) |
| Both Parents Essential Workers | 18 (10.7) |
| At Least One Parent Laid Off or Furloughed due to Pandemic | 39 (23.1) |
| Both Parents Laid Off or Furloughed due to Pandemic | 2 (1.2) |
| Exposure to COVID-19˄(n,%) | |
| Respondent (mother) | 17 (10.1) |
| Child | 4 (2.4) |
| Diagnosed with COVID-19 (n,%) | |
| Respondent (mother) | 2 (1.2) |
| Child | 1 (0.6) |
| Close Friend or Family Member with a Positive Diagnosis (n,%) | 6 (3.6) |
| Close Friend or Family Member Hospitalized Due to COVID-19 (n,%) | 1 (0.6) |
| Child Characteristics | |
| Age (Mean, SD) | 4.1 (0.93) |
| Gender (n, % Female) | 79 (46.7) |
| Birth Order (n, % First Born) | 80 (47.3) |
| School/Childcare Status Prior to Pandemic (n,%) | |
| Daycare | 32 (18.9) |
| Preschool | 94 (44.4) |
| Transitional Kindergarten/Kindergarten | 21 (12.4) |
| No Regular Care or School Outside the Home | 64 (37.9) |
This includes those on leave with pay; §Quarantine due to suspected exposure and/or symptoms; ˄Due to either suspected or confirmed case.
2.2. Measures
2.2.1. Child depressive symptoms
Mothers completed the Preschool Feelings Checklist (PFC), a 16-item screening questionnaire for identifying children at high risk for preschool-onset depression or other forms of psychopathology (Luby et al., 2004). The PFC is a yes/no checklist that includes symptoms such as “frequently appears sad or says he/she feels sad”, “seems not to be as excited about play or activities as other kids” and “often seems to be very tired and has low energy” (α = 0.68 in this sample). The scale exhibits good psychometric properties and is superior to the widely used Child Behavior Checklist (Achenbach and Rescorla, 2000) in terms of its sensitivity and specificity for depression (Luby et al., 2004). A cutoff of 3 or greater is indicative of clinically relevant symptoms, with a sensitivity of 0.92 and specificity of .84 for clinically diagnosed major depressive disorder. Two participants skipped an item on this measure and so were not included in the analyses with this outcome.
2.2.2. Child externalizing symptoms
Child externalizing symptoms were measured with the 5-item conduct problems subscale of the Strengths & Difficulties Questionnaire (SDQ) (Goodman, 1997). Using a 3-point Likert scale (“Not true”, “Somewhat true” and “Certainly true”), parents report the extent to which each of the following applies to their child: “Often has temper tantrums or hot tempers”, “Generally obedient”, Often fights with siblings/other children”, “Often argumentative with adults” and “Can be spiteful to others”. This subscale has adequate psychometric properties (α = 0.69 in the current sample) and a score above the recommended cutoff is predictive of clinical diagnosis of conduct and oppositional defiance disorders (sensitivity = 0.68, specificity = .91) (Goodman, 2001).
2.2.3. Change in externalizing symptoms
For each of the five externalizing behaviors assessed with the SDQ, mothers were additionally asked whither this behavior had “increased”, “decreased” or “stayed the same” since the beginning of the pandemic.
2.2.4. Family routines
Six items were given from the Family Routines Inventory (Jensen et al., 1983), which measures the degree of routinization within a family. These items included: “Working parent(s) have a regular play time with the children after work”, “Children do the same things each morning as soon as they wake up”, “Family has certain ‘family time’ each week when they do things together at home”, “Children have special things they do or ask for each night at bedtime (e.g., a story, a good night kiss, a drink of water)”, “Children go to bed at the same time” and “Whole family eats dinner together”. Mothers were asked to report the extent to which these routines had been in place since the start of the pandemic. Responses are given on a four-point scale and are summed to create a total score, with a possible range of 0–18. This scale exhibits good construct and test-retest reliability (Jensen et al., 1983) and the Chronbach's Alpha in the current sample was .68.
2.2.5. Maternal stress and depressive symptoms
Maternal depressive symptoms were characterized using the nine-item short form of the Center for Epidemiologic Studies Depression Scale (Santor and Coyne, 1997). This measure has been extensively used, and published studies demonstrate acceptable internal consistency and validity (Santor and Coyne, 1997; Marcus et al., 2003). The bivariate scoring strategy was applied because it demonstrates stronger associations with clinical diagnoses (Yim et al., 2009). Maternal generalized or non-specific stress was measured with the 10-item version of the Perceived Stress Scale (Cohen et al., 1983). This widely used and validated scale has good psychometric properties (Cohen et al., 1983; Lee, 2012).
2.2.6. Food insecurity
To measure the degree to which households were food insecure, 5-questions that comprise the USDA food security module short form were given (Bickel et al., 2000). This instrument addresses household food quality and quantity. Questions were asked with the reference time frame “since the beginning of the pandemic” and include items such as “Did you or other adults in your household ever cut the size of your meals or skip meals because there wasn't enough money for food” and “Were you ever hungry but didn't eat because you couldn't afford enough food?” Answers were summed with a possible range of scores from 0 to 5.
2.2.7. Analytic plan
Descriptive analyses were initially performed to describe the prevalence of depressive and externalizing symptoms, as well as reports of pandemic-related increases in externalizing behaviors. Pearson correlations were then conducted to examine associations between the primary predictor (Family Routines Inventory scores) and outcomes (externalizing behaviors and depressive symptoms), as well as other child, maternal and household characteristics. Subsequently, linear regression models were used to examine the association between family routines and child mental health indicators while considering possible third variable explanations including: child age and sex, dual parent household status, pre-pandemic annual household income, food security during the pandemic, maternal perceived stress and maternal depressive symptoms. The association between family routines and change in externalizing behaviors was examined with binary logistic regressions (no reported increases in externalizing vs. reported increases in at least one category). These models also considered the possible confounding factors described above. In all models we tested whether associations between routines and child mental health symptoms were dependent on child sex, however, there was no evidence of moderation.
3. Results
3.1. Family characteristics in the COVID pandemic context
Ninety seven percent of families reported that they had internet access in their homes at the time of the survey. Nearly 30 percent of the families were experiencing some food insecurity and 23.9 percent of families had at least one parent who had been laid off or furloughed as a result of the pandemic. Half of families had at least one parent working as an essential worker (50.3%) and in 10.7% of families both parents were classified as essential workers. Neither essential worker status nor parental layoff/furlough were associated with child mental health symptoms (Table 2). Two mothers and one child were reported to have had a coronavirus diagnosis.
Table 2.
Associations between child mental health, demographic and household characteristics.
| Mean (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child Depressive Symptoms | 2.47 (2.3) | – | ||||||||||
| 2. Child Externalizing Behaviors | 3.7 (2.2) | .40** | – | |||||||||
| 3. Family Routines | 14.6 (3.2) | -.27** | -.19* | – | ||||||||
| 4. Child Age | 4.1 (.9) | .05 | .04 | -.12 | – | |||||||
| 5. Child Sex | – | -.01 | .07 | -.04 | -.07 | – | ||||||
| 6. Dual Parent Household | – | -.16* | .01 | .18* | -.18* | .06 | – | |||||
| 7. Household Income | 95,739 (105,567) | .02 | -.09 | .12 | -.16* | -.18* | .25* | – | ||||
| 8. Food Insecurity | .76 (1.4) | .21* | .15¥ | -.28** | .20* | .09 | -.19* | -.27** | – | |||
| 9. Parent an Essential Worker | – | -.03 | .01 | .04 | .01 | .01 | .10 | .19* | -.16* | – | ||
| 10. Furlough or Layoff of Parent | – | .03 | .05 | -.10 | .04 | -.01 | .10 | -.17* | .13 | -.30* | – | |
| 11. Maternal Depressive Symptoms | 2.0 (2.4) | .40** | .34** | -.20* | .04 | .02 | -.03 | .04 | .22** | .01 | .09 | – |
| 12. Maternal Perceived Stress | 15.9 (6.7) | .43** | .40** | -.23** | .05 | .08 | .02 | -.03 | .29** | -.04 | .08 | .71** |
Child sex coded male = 0, female = 1; Dual parent, Essential worker and Furlough/Layoff coded 1 = yes, 0 = no; **p < .01, *p < .05, ¥p < .01.
3.2. Child mental health symptoms
The mean score on the Preschool Feelings Checklist was 2.47 (sd = 2.3). In this sample, 39.9% of the children scored above the recommended cutoff (≥3) for referral for further evaluation for clinical depression. The proportion of children scoring above the cutoff was elevated compared to those reported in a pre-COVID German population–based sample (5.7%) (Fuhrmann et al., 2014) and more similar to a pre-COVID high risk U.S. sample enriched for depression (43.7%) (Luby et al., 2012). The mean score on the conduct problems subscale of the Strengths and Difficulties Questionnaire was 3.7 (sd = 2.2), which is higher than the pre-COVID US population mean for 4–7 year olds (M = 1.2, sd = 1.6) and the mean for a pre-COVID large community sample of 3–4 year olds in Spain (M = 2.08, sd = 1.8) (Ezpeleta, 2011; youthinmind, 2004). Across pre-COVID preschool-aged large community samples in the US, UK and Spain the cutoff score is defined as the 90 percentile, which is a score of 5 or greater (Ezpeleta, 2011; youthinmind, 2015). In our COVID-19 sample, 36.1% of the children scored at or above this cutoff.
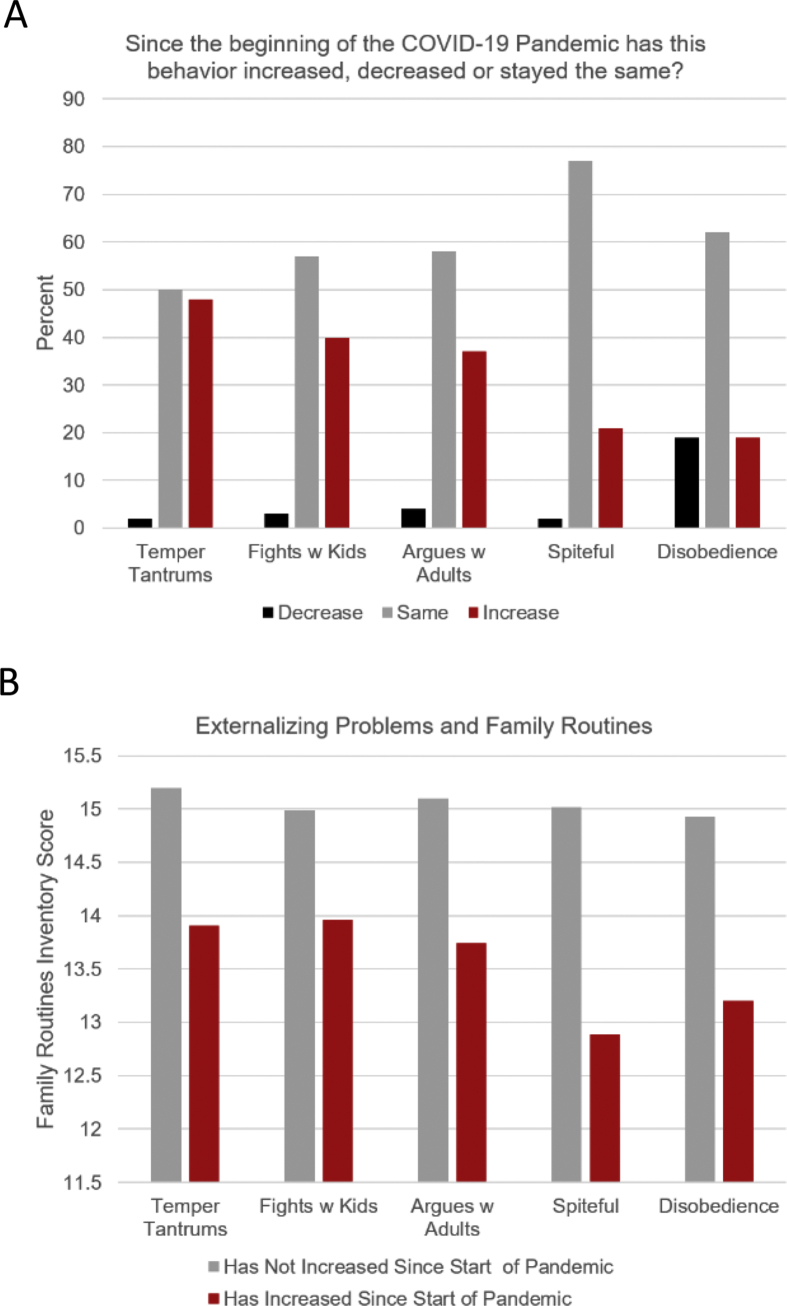
Fig. 1A shows the percent of mothers reporting increases in conduct problems compared to pre-pandemic levels. For each of the five behavior categories, a sizeable proportion of mothers reported increases (range 18.9–47.9%, M = 32.8%). In contrast, reports of improvements in these behaviors were relatively rare (range 1.8–18.3%, M = 5.7%). In sum, close to two thirds (64%) of mothers reported an increase in externalizing behaviors in at least one behavior category since the start of the pandemic.
Fig. 1.
Conduct problems during the COVID-19 pandemic among preschoolers are elevated (1A), however, family routines appear to offset these adverse consequences (1B). Note: The item by item data presented in 1B are presented for illustrative purposes only. Regression analyses were conducted with summary scores.
3.3. Family routines and child mental health symptoms
Bivariate correlations between family routines and child depressive symptoms on the PFC and externalizing behaviors on the SDQ can be seen in Table 2. In households in which more routines were practiced, lower levels of both depressive symptoms (r = −0.27, p < .01) and externalizing behaviors (r = −0.19, p < .05) were observed. Adjustment for child (age and sex) and family (income, food security, dual parent household) characteristics did not alter the association between family routines and either of the child mental health indicators (Table 3, Models 1a and 2a). Notably, the association between family routines and child depressive symptoms remained statistically significant when the contributions of maternal psychological distress (depressive symptoms and perceived stress) were covaried (Table 3, Models 1b and 1c). In contrast, the inclusion of maternal depressive symptoms and perceived stress attenuated the association between family routines and externalizing behaviors, rendering them above our a priori cutoff for statistical significance (p's = 0.10 and 0.15 respectively; Table 3, Models 2b and 2c).
Table 3.
Linear regressions testing associations between family routines and child mental health.
| Child Depressive Symptoms |
Child Externalizing Symptoms |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1a |
Model 1b |
Model 1c |
Model 2a |
Model 2b |
Model 2c |
|||||||||||||
| B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | |
| Family Routines | -.16 | .06 | -.22** | -.12 | .05 | -.17* | -.11 | .05 | -.15* | -.12 | .06 | -.18** | -.09 | .05 | -.13¥ | -.08 | .05 | -.11 |
| Child Agerowhead | -.02 | .19 | -.01 | -.04 | .18 | -.02 | -.02 | .18 | -.01 | .06 | .19 | .03 | .05 | .18 | .02 | .06 | .17 | .03 |
| Child Sex | .07 | .34 | .02 | -.01 | .33 | -.00 | -.09 | .33 | -.02 | .21 | .35 | .05 | .17 | .33 | .04 | .12 | .33 | .03 |
| Dual Parent Household | -.71 | .49 | -.12 | -.73 | .46 | -.12 | -.91 | .45 | -.15* | .47 | .48 | .08 | .46 | .46 | .08 | .28 | .45 | .05 |
| Household Income | .00 | .00 | .13 | .00 | .00 | .09 | .00 | .00 | .10 | .00 | .00 | -.05 | .00 | .00 | -.09 | .00 | .00 | -.07 |
| Food Insecurity | .27 | .13 | .17* | .15 | .13 | .09 | .10 | .13 | .06 | .16 | .13 | .10 | .06 | .13 | .04 | .00 | .13 | .00 |
| Maternal Depressive Symptoms | – | – | – | .32 | .07 | .34** | – | – | – | – | – | – | .29 | .07 | .32** | – | – | – |
| Maternal Perceived Stress | – | – | – | – | – | – | .13 | .03 | .38** | – | – | – | – | – | – | .82 | .17 | .37** |
**p < .01, *p < .05.
3.4. Family routines and increases in externalizing behaviors
Children who exhibited an increase in conduct problems since the start of the pandemic measured by change in SDQ behaviors were more likely to have families exercising fewer routines (Exp(B) = 0.86, 95% CI 0.77-0.97, p < .05; Fig. 1B). Further, this association remained after adjusting for child and family sociodemographic factors, maternal depressive symptoms and perceived stress (Table 4). This association also persisted after adjusting for level of externalizing problems assessed with the SDQ (Table 4, Model 1d), indicating that the relation between fewer family routines and pandemic-related increases externalizing behaviors were independent from absolute levels of these behaviors.
Table 4.
Binary logistic regressions predicting increases in child externalizing behaviors.
| Model 1a |
Model 1b |
Model 1c |
Model 1d |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exp(B) | 95% CI | Wald | Exp(B) | 95% CI | Wald | Exp(B) | 95% CI | Wald | Exp(B) | 95% CI | Wald | |
| Family Routines | .85* | 0.75–.96 | 6.43 | .86* | 0.72–0.98 | 5.24 | .86* | 0.75–.98 | 5.06 | .86* | 0.74–0.99 | 4.38 |
| Child Age | 1.03 | 0.71–1.48 | 0.02 | 1.04 | 0.71–1.51 | 0.03 | 1.04 | 0.71–1.52 | 0.04 | 1.06 | 0.70–1.59 | 0.07 |
| Child Sex | 1.25 | 0.64–2.45 | 0.42 | 1.24 | 0.62–2.45 | 0.37 | 1.18 | 0.59–2.35 | 0.22 | 1.14 | 0.54–2.43 | 0.12 |
| Dual Parent Household | 1.14 | 0.44 | 0.72 | 1.20 | 0.45–3.12 | 0.13 | 1.06 | 0.40–2.81 | 0.02 | .87 | 0.29–2.55 | 0.18 |
| Household Income | 1.0 | 1.0–1.0 | 0.28 | 1.0 | 1.00–1.00 | 0.70 | 1.0 | 1.0–1.0 | .43 | 1.0 | 1.0–1.0 | 0.18 |
| Food Insecurity | .94 | 0.73–1.21 | 0.23 | .88 | 0.67–1.15 | 0.94 | .86 | 0.66–1.12 | 1.23 | .86 | 0.64–1.16 | 0.98 |
| Maternal Depressive Symptoms | – | – | – | 1.21* | 1.02–1.45 | 5.01 | – | – | – | – | – | – |
| Maternal Perceived Stress | – | – | – | – | – | – | 1.07* | 1.01–1.13 | 5.73 | – | – | – |
| SDQ Sum Score | – | – | – | – | – | – | – | – | – | 1.68** | 1.37–2.06 | 25.78 |
**p < .01, *p < .05.
4. Discussion
The impact of the COVID-19 pandemic on children's health and development of strategies to minimize its adverse effects are just beginning to emerge (Wang and Bair, 2020). Here we examined specific child mental health symptom profiles with age-appropriate, validated, standardized measures documenting elevated levels of both internalizing (depressive symptoms) and externalizing (conduct problems) symptoms among children ages 2–6 during the pandemic. These observations extend beyond existing COVID-19 pandemic surveys with single questions addressing “behavior problems” and “anxiety” in preschool children (Center for Translational Neuroscience, 2020a; Patrick et al., 2020) and are consistent with reports of pandemic-related increases in internalizing symptoms (depression and anxiety) in school-aged children and adolescents (Duan et al., 2020; Hawke et al., 2020) as well as findings examining the effects of disasters, both natural and manmade on child mental health (Masten and Narayan, 2012). We further report that in families employing more routines, rates of child depressive symptoms are lower and increases in conduct problems during the pandemic less likely. It is important to note that the associations between routines and child mental health symptoms persist after accounting for household characteristics (e.g. income, food security, dual parent household status) and maternal psychological distress (perceived stress and depressive symptoms).
In contrast to the protective effects of family routines, elevated maternal perceived stress and depressive symptoms each predicted poorer child mental health in both internalizing and externalizing domains. These findings are consistent with a broad literature demonstrating the fundamental role of maternal mental health in child risk for psychopathology (Monk et al., 2019; Glynn et al., 2018; Goodman et al., 2011). It also is notable that they are consistent with the few studies that have examined child well-being during pandemics. In the context of the H1N1 pandemic in the US (Sprang and Silman, 2013), and the COVID-19 pandemic in Italy (Spinelli et al., 2020), parental mental health was a strong predictor of child symptoms and in the case of H1N1, longer-term adjustment as well.
As with any study, ours has both strengths and limitations. The sample is predominantly racial-ethnic minority and economically disadvantaged, which we view as a strength. It is anticipated that the impacts of COVID-19 will be patterned by income and race/ethnicity, with those children in minority and economically disadvantaged families receiving a disproportionate share of the burden (Dooley et al., 2020). In addition, we examined the association between routines and mental health in preschool-aged children, providing among the first mental health data in this age group. This may be of particular importance because there is initial evidence that the costs to mental health may be more significant among younger children, with the largest effects in children under 5, such as those studied here (Patrick et al., 2020). Conversely, because of the unique aspects of this cohort, future studies will have to confirm whether family routines are equally protective for other sociodemographic groups and for children in other developmental stages (e.g. infancy, middle childhood and adolescence). There are a few other potential limitations that should be considered when evaluating our findings. Our conclusion that child mental health appears to be suffering in the face of the pandemic, must be weighed in the context of the cross-sectional nature of the data. This is particularly true for our measure of internalizing for which we did not have mothers' reports of increases in symptoms and rather had to rely on comparisons to rates on the same measure in other studies. However, although we do believe the elevated internalizing symptoms are in part likely due to the nature of the sample, they were concordant with a similarly low SES sample that was enriched for depression, which we would expect to have significantly higher levels. Further, although these children are at greater risk for depressive symptoms given their SES status, they and their families also are at greater risk for experiencing the adverse effects of the pandemic. Given these facts and the findings from national and community surveys of children's behavioral and mental health during the COVID-19 pandemic (Golberstein et al., 2020; Center for Translational Neuroscience, 2020a) as well as longitudinal studies in adults for which pre-pandemic mental health data are available for comparison (Twenge and Joiner, 2020), we believe it is reasonable to conclude that some of the elevations are likely attributable to the pandemic. Additionally, because of the cross-sectional nature of the data, we are unable to draw conclusions regarding whether routines are more or less protective in the context of the pandemic compared to pre- or non-pandemic conditions. Last, we acknowledge that causality cannot be assumed because what we describe here are naturally occurring routines. An alternative view is that families who are able to maintain routines in the face of a challenge such as a pandemic differ in other ways that promote child resilience, such as less relational conflict or different belief systems (Masten and Narayan, 2012).
There are multiple pathways through which family routines could influence child mental health, and these include parental mental health, parenting efficacy, behavior monitoring, family cohesion and child sleep, each of which are likely to be bolstered by family routines (Fiese et al., 2002; Mindell and Williamson, 2018; Porter and Hsu, 2003; Chang and Qin, 2018). In addition, predictability may directly foster neurodevelopment and more optimal mental health (Glynn and Baram, 2019). Animal models indicate that unpredictable sensory signals in early life influence the maturation of systems governing emotional and cognitive function, provoking aberrant behaviors in these domains (Short and Baram, 2019). These findings are complemented by accumulating evidence in humans demonstrating that unpredictability in early life is a novel form of adversity that uniquely predicts risk for psychopathology (Davis et al., 2017, 2019; Glynn et al., 2018, 2019; Howland et al., 2020; Doom et al., 2016; Brumbach et al., 2009).
In summary, our findings in a 2020 cohort of preschool children indicate that the impact of the COVID-19 pandemic on the mental health of these children may be ameliorated by the presence of family routines. Nearly three quarters of a century ago, Bossard and Boll (1950) made the observation that family routines are integral organizers of family life with the potential to protect families in times of uncertainty and adversity. Our data are consistent with their premise and provide empirical support for public health recommendations directing families to support children by adhering to daily routines. Although the mental health of children does appear to be suffering due to the pandemic and the long-term sequelae are likely to be significant, family routines represent one resilience-promoting factor with the potential to mitigate these adverse influences.
Funding
This study was supported by National Institutes of Health Grant MH096889.
CRediT authorship contribution statement
Laura M. Glynn: Conceptualization, designed the study, oversaw data collection, conducted the analyses, drafted the initial manuscript, made revisions. Elysia Poggi Davis: helped in study design, interpretation of data, revised the article for intellectual content. Joan L. Luby: helped in study design, interpretation of data, revised the article for intellectual content. Tallie Z. Baram: helped in study design, interpretation of data, revised the article for intellectual content. Curt A. Sandman: helped in study design, interpretation of data, revised the article for intellectual content.
Declaration of competing interest
The authors have no conflicts of interest to declare.
References
- Achenbach T.M., Rescorla L.A. University of Vermont, Research Center for Children, Youth, & Families; Burlington: 2000. Manual for ASEBA Preschool Forms & Profiles. [Google Scholar]
- Betancourt T.S., Meyers-Ohki S.E., Charrow A., Hansen N. Annual Research Review: mental health and resilience in HIV/AIDS-affected children-- a review of the literature and recommendations for future research. JCPP (J. Child Psychol. Psychiatry) 2013;54(4):423–444. doi: 10.1111/j.1469-7610.2012.02613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel G., Nord M., Price C., Hamilton W., Cook J. Guide to measuring household food security. In: Alexandria V.A., editor. US Department of Agriculture. 2000. [Google Scholar]
- Bossard J., Boll E. University of Pennsylvania Press; Philadelphia: 1950. Ritual in Family Living. [Google Scholar]
- Bronfenbrenner U., Ceci S.J. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol. Rev. 1994;101(4):568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- Brumbach B.H., Figueredo A.J., Ellis B.J. Effects of harsh and unpredictable environments in adolescence on development of life history strategies: a longitudinal test of an evolutionary model. Hum. Nat. 2009;20(1):25–51. doi: 10.1007/s12110-009-9059-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Translational Neuroscience . 2020. Why Households with Young Children Warrant Our Attention and Support during (And after) the COVID-19 Pandemic.https://medium.com/rapid-ec-project/why-households-with-young-children-warrant-our-attention-and-support-during-and-after-the-b7cee9b76184 [Google Scholar]
- Center for Translational Neuroscience . 2020. Flattening the Other Curve: Trends for Young Children's Mental Health Are Good for Some, but Concerning for Others.https://medium.com/rapid-ec-project/flattening-the-other-curve-7be1e574b340 [Google Scholar]
- Chang T.F., Qin D.B. Maternal monitoring knowledge change and adolescent externalizing behaviors in low-income african American and latino families. Psychol. Rep. 2018;121(4):635–668. doi: 10.1177/0033294117738022. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Crespo C., Santos S., Canavarro M.C., Kielpikowski M., Pryor J., Feres-Carneiro T. Family routines and rituals in the context of chronic conditions: a review. Int. J. Psychol. 2013;48(5):729–746. doi: 10.1080/00207594.2013.806811. [DOI] [PubMed] [Google Scholar]
- Davis E.P., Stout S.A., Molet J. Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proc. Natl. Acad. Sci. U. S. A. 2017;114(39):10390–10395. doi: 10.1073/pnas.1703444114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis E.P., Korja R., Karlsson L. Across continents and demographics, unpredictable maternal signals are associated with children's cognitive function. EBioMedicine. 2019;46:256–263. doi: 10.1016/j.ebiom.2019.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley D.G., Bandealy A., Tschudy M.M. Low-income children and coronavirus disease 2019 (COVID-19) in the US. JAMA Pediatr. 2020;174:922–923. doi: 10.1001/jamapediatrics.2020.2065. [DOI] [PubMed] [Google Scholar]
- Doom J.R., Vanzomeren-Dohm A.A., Simpson J.A. Early unpredictability predicts increased adolescent externalizing behaviors and substance use: a life history perspective. Dev. Psychopathol. 2016;28(4pt2):1505–1516. doi: 10.1017/S0954579415001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin M.S., Khan N., Davidson L.L., Zaman S.S., Stein Z.A. The effects of a natural disaster on child behavior: evidence for posttraumatic stress. Am. J. Publ. Health. 1993;83(11):1549–1553. doi: 10.2105/ajph.83.11.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezpeleta L. 2011. Spanish Norms for the Strengths & Difficulties Questionnaire (SDQ) for 3 and 4 Year Old Children.https://www.sdqinfo.org/norms/Spanish_norms_for_3-4_year-old.pdf [Google Scholar]
- Felix E., Hernandez L.A., Bravo M., Ramirez R., Cabiya J., Canino G. Natural disaster and risk of psychiatric disorders in Puerto Rican children. J. Abnorm. Child Psychol. 2011;39(4):589–600. doi: 10.1007/s10802-010-9483-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiese B.H., Tomcho T.J., Douglas M., Josephs K., Poltrock S., Baker T. A review of 50 years of research on naturally occurring family routines and rituals: cause for celebration? J. Fam. Psychol. 2002;16(4):381–390. doi: 10.1037//0893-3200.16.4.381. [DOI] [PubMed] [Google Scholar]
- Fonseca G., Cunha D., Crespo C., Relvas A.P. Families in the context of macroeconomic crises: a systematic review. J. Fam. Psychol. 2016;30(6):687–697. doi: 10.1037/fam0000230. [DOI] [PubMed] [Google Scholar]
- Fuhrmann P., Equit M., Schmidt K., von Gontard A. Prevalence of depressive symptoms and associated developmental disorders in preschool children: a population-based study. Eur. Child Adolesc. Psychiatr. 2014;23(4):219–224. doi: 10.1007/s00787-013-0452-4. [DOI] [PubMed] [Google Scholar]
- Glynn L.M., Baram T.Z. The influence of unpredictable, fragmented parental signals on the developing brain. Front. Neuroendocrinol. 2019;53:100736. doi: 10.1016/j.yfrne.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn L.M., Howland M.A., Sandman C.A. Prenatal maternal mood patterns predict child temperament and adolescent mental health. J. Affect. Disord. 2018;228:83–90. doi: 10.1016/j.jad.2017.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn L.M., Stern H.S., Howland M.A. Measuring novel antecedents of mental illness: the Questionnaire of Unpredictability in Childhood. Neuropsychopharmacology. 2019;44(5):876–882. doi: 10.1038/s41386-018-0280-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: a research note. JCPP (J. Child Psychol. Psychiatry) 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman S.H., Rouse M.H., Connell A.M., Broth M.R., Hall C.M., Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin. Child Fam. Psychol. Rev. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Guidubaldi J., Cleminshaw H.K., Perry J.D., Nastasi B.K., Lightel J. The role of selected family environment factors in children's post-divorce adjustment. Fam. Relat. 1986;35:141–151. [Google Scholar]
- Hawke L.D., Barbic S.P., Voineskos A. Impacts of COVID-19 on Youth Mental Health, Substance Use, and Well-being: a Rapid Survey of Clinical and Community Samples: repercussions de la COVID-19 sur la sante mentale, l’utilisation de substances et le bien-etre des adolescents : un sondage rapide d’echantillons cliniques et communautaires. Can. J. Psychiatr. 2020;65:701–709. doi: 10.1177/0706743720940562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar C.E., Miller G.E. Protective factors for youth confronting economic hardship: current challenges and future avenues in resilience research. Am. Psychol. 2019;74(6):641–652. doi: 10.1037/amp0000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howland M.A., Sandman C.A., Davis E.P. Prenatal maternal mood entropy is associated with child neurodevelopment. Emotion. 2020 doi: 10.1037/emo0000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen E.W., James S.A., Boyce W.T., Hartnett S.A. The family routines inventory: development and validation. Soc. Sci. Med. 1983;17(4):201–211. doi: 10.1016/0277-9536(83)90117-x. [DOI] [PubMed] [Google Scholar]
- Lee E.H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Living Wage Calculator. Massachusetts Institute of Technology; 2020. https://livingwage.mit.edu/ [Google Scholar]
- Luby J.L., Heffelfinger A., Koenig-McNaught A.L., Brown K., Spitznagel E. ThePreschool Feelings Checklist: a brief and sensitive screening measure for depression in young children. J. Am. Acad. Child Adolesc. Psychiatry. 2004;43(6):708–717. doi: 10.1097/01.chi.0000121066.29744.08. [DOI] [PubMed] [Google Scholar]
- Luby J., Lenze S., Tillman R. A novel early intervention for preschool depression: findings from a pilot randomized controlled trial. JCPP (J. Child Psychol. Psychiatry) 2012;53(3):313–322. doi: 10.1111/j.1469-7610.2011.02483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus S.M., Flynn H.A., Blow F.C., Barry K.L. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt). 2003;12(4):373–380. doi: 10.1089/154099903765448880. [DOI] [PubMed] [Google Scholar]
- Masten A.S., Motti-Stefanidi F. Multisystem resilience for children and youth in disaster: reflections in the context of COVID-19. Adversity and Resilience Science. 2020;1:95–106. doi: 10.1007/s42844-020-00010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten A.S., Narayan A.J. Child development in the context of disaster, war, and terrorism: pathways of risk and resilience. Annu. Rev. Psychol. 2012;63:227–257. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell J.A., Williamson A.A. Benefits of a bedtime routine in young children: sleep, development, and beyond. Sleep Med. Rev. 2018;40:93–108. doi: 10.1016/j.smrv.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk C., Lugo-Candelas C., Trumpff C. Prenatal developmental origins of future psychopathology: mechanisms and pathways. Annu. Rev. Clin. Psychol. 2019;15:317–344. doi: 10.1146/annurev-clinpsy-050718-095539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Porter C.L., Hsu H.C. First-time mothers' perceptions of efficacy during the transition to motherhood: links to infant temperament. J. Fam. Psychol. 2003;17(1):54–64. [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75:631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Roubinov D., Bush N.R., Boyce W.T. How a pandemic could advance the science of early adversity. JAMA Pediatr. 2020;174:1131–1132. doi: 10.1001/jamapediatrics.2020.2354. [DOI] [PubMed] [Google Scholar]
- Santor D.A., Coyne J.A. Shortening the CES-D to improve its ability to detect cases of depression. Psychol. Assess. 1997;9(3):233–243. [Google Scholar]
- Scott B.G., Lapre G.E., Marsee M.A., Weems C.F. Aggressive behavior and its associations with posttraumatic stress and academic achievement following a natural disaster. J. Clin. Child Adolesc. Psychol. 2014;43(1):43–50. doi: 10.1080/15374416.2013.807733. [DOI] [PubMed] [Google Scholar]
- Short A.K., Baram T.Z. Early-life adversity and neurological disease: age-old questions and novel answers. Nat. Rev. Neurol. 2019;15(11):657–669. doi: 10.1038/s41582-019-0246-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents' stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020;11:1713. doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Stark A.M., White A.E., Rotter N.S., Basu A. Shifting from survival to supporting resilience in children and families in the COVID-19 pandemic: lessons for informing U.S. mental health priorities. Psychol Trauma. 2020;12(S1):S133–S135. doi: 10.1037/tra0000781. [DOI] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E.U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020:1–3. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.J., Bair H. Operational considerations on the American academy of pediatrics guidance for K-12 school reentry. JAMA Pediatr. 2020;(Aug 11) doi: 10.1001/jamapediatrics.2020.3871. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolin S.J., Bennett L.A. Family rituals. Fam. Process. 1984;23(3):401–420. doi: 10.1111/j.1545-5300.1984.00401.x. [DOI] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in hubei province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim I.S., Glynn L.M., Dunkel-Schetter C., Hobel C.J., Chicz-DeMet A., Sandman C.A. Risk of postpartum depressive symptoms with elevated corticotropin-releasing hormone in human pregnancy. Arch. Gen. Psychiatr. 2009;66(2):162–169. doi: 10.1001/archgenpsychiatry.2008.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- youthinmind . 2004. Normative SDQ Data from the USA. [Google Scholar]
- youthinmind . 2015. Scoring the Strengths & Difficulties Questionnaire for 2-4 Year Olds.https://www.sdqinfo.org/py/sdqinfo/c0.py [Google Scholar]