Abstract
COVID-19 has caused over 300,000 US deaths thus far, but its long-term health consequences are not clear. Policies to contain the pandemic have led to widespread economic problems, which likely increase stress and resulting health risk behaviors, particularly among women, who have been hardest hit both by job loss and caregiving responsibilities. Further, women with pre-existing disadvantage (e.g., those without health insurance) may be most at risk for stress and consequent health risk behavior. Our objective was to estimate the associations between financial stressors from COVID-19 and health risk behavior changes since COVID-19, with potential effect modification by insurance status. We used multilevel logistic regression to assess the relationships between COVID-19-related financial stressors (job loss, decreases in pay, trouble paying bills) and changes in health risk behavior (less exercise, sleep, and healthy eating; more smoking/vaping and drinking alcohol), controlling for both individual-level and zip code-level confounders, among 90,971 US women who completed an online survey in March–April 2020. Almost 40% of women reported one or more COVID-19-related financial stressors. Each financial stressor was significantly associated with higher odds of each type of health risk behavior change. Overall, reporting one or more financial stressors was associated with 56% higher odds (OR = 1.56; 95% CI: 1.51, 1.60) of reporting two or more health risk behavior changes. This association was even stronger among women with no health insurance (OR = 2.46; 95% CI: 1.97, 3.07). COVID-19-related economic stress is thus linked to shifts in health risk behaviors among women, which may have physical health consequences for years to come. Further, the relationship between financial hardship and health risk behavior among women may be modified by health insurance status, as a marker for broader socioeconomic context and resources. The most socioeconomically vulnerable women are likely at highest risk for long-term health effects of COVID-19 financial consequences.
Keywords: Health risk behavior, Financial stress, COVID-19, Cardiovascular disease, Women’s health
Highlights
-
•
Over 1/3 of women in this study reported COVID-19-related financial stress.
-
•
Financial stress was associated with higher odds of health risk behavior changes.
-
•
This relationship was modified by health insurance status among women.
-
•
These behavior changes may eventually lead to cardiovascular disease.
-
•
Women who are already more vulnerable are likely at even higher risk.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic and its consequences have disrupted the world—straining health system capacities, harming global and local economies, and leading to unprecedented changes in the functioning of every-day life for many, on top of the physical health toll of the virus. As of mid-December 2020, in the United States (US), there were almost 17 million cases and over 300,000 deaths due to COVID-19 (Coronavirus Disease 2019 (COVID-19): Cases, Data, & Surveillance: Cases in the US. Centers for Disease Control and Prevention, 2020). Between March and April 2020, forty-two states issued shelter-in-place or stay-at-home orders (State Mandated Stay-at-Home Orders by Date of Implementation. Henry J Kaiser Family Foundation, 2020), leaving much of the American economy at a stand-still for weeks, and ultimately triggering the greatest economic crisis since the Great Depression (Zumbrun, 2020).
These events will have implications for the health of populations for years to come. In addition to the physical health burden from COVID-19, mental health problems and stress are and will continue to be substantially elevated during and after the pandemic, as suggested by emerging studies (Brooks et al., 2020; Cao et al., 2020; Czeisler et al., 2020; Ettman, Abdalla, et al., 2020; Lai et al., 2020; Liu et al., 2020; Wang et al., 2020), data from prior pandemics (Hawryluck et al., 2004; Jalloh et al., 2018; Ko et al., 2006), and other types of widespread mass traumatic events (Galea et al., 2002; Goldmann & Galea, 2014; Ni et al., 2020; Silver et al., 2002).
Fear and anxiety both about the virus itself and about the economic effects of closures of businesses and related financial hardship can influence mental health. One early COVID-19 study reported that about 15% of US respondents already had reduced wages or work hours in March 2020 and 1.5% had already lost their job (Nelson et al., 2020). A more recent study suggested that 40% of Americans had experienced one or more COVID-19-related financial stressors by mid-April 2020 (Ettman, Abdalla, et al., 2020). In one month between mid-March and mid-April, over 20 million Americans filed for unemployment, a record increase in claims (Tappe & Luhby, 2020). By August 20, there were over 57 million total Americans who had filed since the start of the pandemic (Reinicke, 2020).
It is clear from the general psychiatric literature—outside of a pandemic context—that lower income, economic volatility, and financial hardship are strongly associated with adverse mental health outcomes such as depression and suicide (Ettman, Cohen, et al., 2020; Karanikolos et al., 2013; Nandi et al., 2012). The relationship between financial stressors and poor mental health has also been observed after mass traumatic events such as hurricanes (Galea et al., 2008) and prior pandemics (Ko et al., 2006).
Prior literature has also suggested that traumatic or stressful events—such as living through a pandemic and the resulting economic effects described above—can result in populations changing their health risk behavior, often through pathways of stress and psychiatric symptoms. For example, many studies have shown that stress, trauma, and related posttraumatic stress disorder (PTSD) are associated with higher levels of smoking (Bergman et al., 2019; Koenen et al., 2006, 2008), heavier drinking (Dennis et al., 2014), poor diet quality (Brondolo et al., 2017; Hall et al., 2015; Sumner et al., 2015), trouble sleeping (Leskin et al., 2002), and lack of exercise (Chwastiak et al., 2011; Hall et al., 2015). Further, these relationships have been observed specifically among cohorts of women (Kubansky et al., 2009; Kubzansky et al., 2014; Sumner et al., 2015), for whom trauma and resulting stress disorders are more common, both in general and in the context of COVID-19 (Liu et al., 2020). Women also tend to be more likely to take on caretaking and other household responsibilities (Douglas et al., 2020; Power, 2020), which may compound financial stress in the current climate, as many children are home from school and elderly loved ones need to be cared for. Finally, early studies have shown that women have been disproportionately affected by COVID-19-related job loss compared to men (Alon et al., 2020; Financial Health Network, 2020).
COVID-19 as a mass traumatic event also carries with it the unique stress of social distancing, which likely further compounds effects on behavior (Brooks et al., 2020; Hawryluck et al., 2004), particularly for those who do not have accessible ways to exercise or eat healthy foods while quarantined. Health risk behavior changes such as exercising less, eating less healthily, and smoking more can eventually lead to poor physical health outcomes, including cardiovascular disease—the leading cause of death in the US and globally (Mensah & Brown, 2007; Mokdad et al., 2004). The relation between COVID-19-related financial hardship and health risk behavior changes also may be modified by factors such as existing social resources or services, given the known buffering effects of these types of resources on stress and physical health in general contexts outside of pandemics (Brondolo et al., 2017).
Building on the existing literature, our goals for this study were to a) document COVID-19 financial stressors, b) assess whether they are associated with health risk behavior changes, and c) test whether the presence of health insurance—as a marker for socioeconomic resources—may act as a modifier of this relationship, in a large, geographically diverse sample of US women.
2. Material and methods
2.1. Data collection and sample
The data for this study were derived from a web-based survey on the impact of COVID-19 in the general population, administered through the digital health company Sharecare, in collaboration with the School of Public Health at Boston University. Participants accessed the survey through social media advertisements and shares (on platforms such as Facebook, Instagram, and Twitter), organic searches via relevant keywords, newsletters and emails distributed through the Sharecare network, and word of mouth. The survey was available in the English language, for any individual over the age of 18. The questionnaire took an average of 7 min to complete.
The sample for this study included data collected in the US from March 20 through April 10, 2020. During this time there were 104,559 completed survey responses, representing 60% of the total number of individuals who had viewed the landing page of the survey. We removed the small sample of men and “other” gender responses (combined n = 11,819 or 11.3% of total respondents), for a resulting sample of 92,740 women.
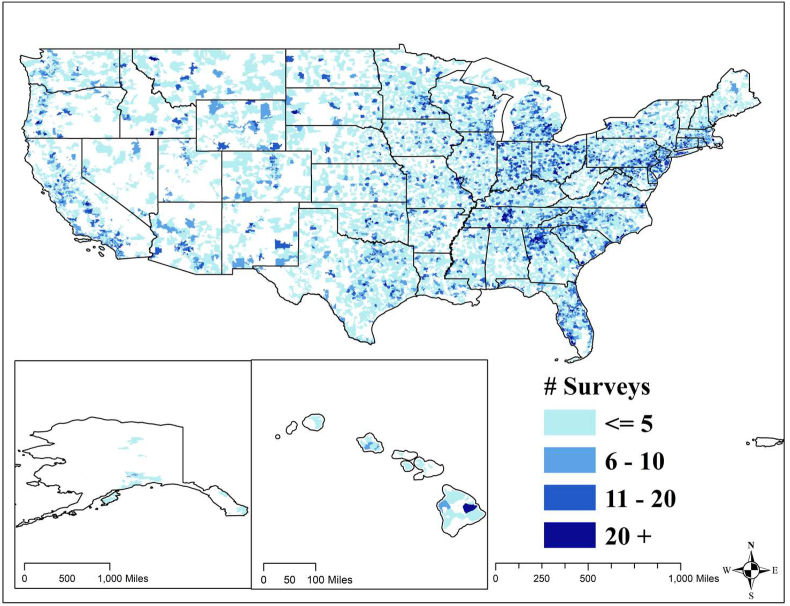
Respondent zip codes were then merged to Census zip code tabulation area (ZCTA) data from the US Census Bureau’s American Community Survey (ACS) 2018 five-year estimates (United States Census Bureau: American Community Survey, 2019). Over 98% of women reported a zip code that matched to a ZCTA, with unmatched zip codes primarily being from non-residential locations such as P.O. boxes, academic institutions, or businesses. It is also possible that some women mis-reported their zip code. Finally, a small proportion of zip codes (35 codes or 38 women) were in the ACS dataset but were missing on our key zip code-level confounders and were thus also excluded. These data are likely missing due to areas with small response rates that are suppressed through the Census. The final analytic sample included 90,971 women residing in 18,359 zip codes. These respondents were from all 50 states and the District of Columbia, with more than 50% of all US zip codes represented (see Fig. 1). The number of women living in each zip code ranged from 1 to 79, with a mean of 5 and median of 3 women per zip code.
Fig. 1.
Map of 18,359 US zip codes represented by 90,971 women in the analytic sample, by number of surveys completed (number of respondents) per zip code.
This study was approved by the Boston University Medical Campus Institutional Review Board.
2.2. Outcome variables
The primary outcomes for this study were reported health risk behavior changes since the start of the COVID-19 pandemic, including changes in eating, exercise, sleep, smoking/vaping, and drinking alcohol. These variables were derived from responses to survey questions such as, “Has your eating been more healthy, less healthy, or the same as before the COVID-19 pandemic started?” with response options “more healthy”, “less healthy” or the “same”.
We dichotomized these outcomes, comparing for example “less healthy” to “more healthy” and “the same”, such that the outcomes of interest represented having health risk behavior changes in the direction of known negative health effects. For sleeping and exercising habits, this was “less” compared to more or no change, whereas for drinking alcohol and smoking or vaping, this was “more” compared to less or no change.
We then combined these five health risk behaviors into a composite outcome for the final models. Since the majority of respondents (57.3%) reported one or more of these health risk behavior changes, we defined the primary outcome variable as having two or more health risk behavior changes—endorsed by 25.8% of respondents—in order to target a relatively more high-risk group.
2.3. Exposure variables
The primary exposures of interest in this study were reporting financial hardship since the COVID-19 pandemic, operationalized as three stressors: decrease in pay, likelihood of difficulty paying bills, and job loss or likelihood of job loss.
The question, “Has your pay changed since the COVID-19 pandemic?” was dichotomized as responding “pay has decreased” compared to “pay has increased” or “pay remains unchanged”. The question, “Because of the COVID-19 pandemic, how likely is it that you will have trouble paying your bills?” was dichotomized as “very likely” or “somewhat likely” compared to “not very likely” or “not likely at all”. Finally, the question, “How likely do you think you are to lose your job because of the COVID-19 pandemic?” was dichotomized as “very likely”, “somewhat likely”, or “I’ve already been laid off from my job because of COVID-19”, as compared to “not very likely”.
Responses of “not applicable” for both the pay decrease question and the job loss question were excluded for comparisons and models including only those stressors. We also excluded these respondents from the other comparisons and models as a sensitivity analysis.
Finally, we combined the three financial stressors into one composite exposure measure that represented having experienced one or more COVID-19-related financial stressors (endorsed by 38% of respondents), compared to not having endorsed any stressors.
2.4. Covariates and modifiers
Individual-level potential confounders—identified from prior literature and domain knowledge but limited by a short survey without comprehensive demographic information—included age (Financial Health Network, 2020; Zanjani et al., 2006) (measured in years), whether the respondent has children who normally attend school (Bellows-Riecken & Rhodes, 2008; Nomaguchi & Bianchi, 2004; Robert Wood Johnson Foundation et al., 2020) (yes vs. no), whether the respondent lives alone (Joutsenniemi et al., 2007; Nomaguchi & Bianchi, 2004) (yes vs. no), and whether the respondent had been diagnosed with COVID-19 (which could cause financial stressors, as individuals may have lost income because they were unable to work for a period of time due to the illness, and could also cause health risk behavior changes, as individuals may have exercised less or slept more during this time period due to the illness).
To attempt to account for unmeasured confounding by factors such as individual-level race and income (Bulatao & Anderson, 2004; Financial Health Network, 2020; Jarvis & Wardle, 2009; Parks et al., 2003) which were not included in our survey, two area-level covariates were included: the proportion of non-white individuals (calculated as the inverse of the proportion of non-Hispanic white individuals) and the proportion of individuals with income below the poverty line in respondents’ residential zip code, both from the ACS 2018 five-year estimates (United States Census Bureau: American Community Survey, 2019).
Our effect modifier of interest was health insurance status (Brondolo et al., 2017), dichotomized as having no health insurance compared to having private insurance from an employer, private insurance from a state health exchange, Medicare, Medicaid, or “other” insurance.
2.5. Statistical analysis
We first generated descriptive statistics, comparing sample characteristics across exposures and outcomes, using means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. We assessed crude comparisons with bar graphs, showing the proportions of respondents who endorsed each health risk behavior outcome by each financial stressor exposure.
We then ran random-intercept-only logistic regression models for each health risk behavior outcome and the composite health risk behavior outcome, with an intercept varying at the zip code level, in order to calculate the intraclass correlation coefficients (ICC) for each outcome (Ene et al., 2015; Merlo et al., 2006). We used zip code as a random effect due to the large number of zip codes and relatively small number of respondents within each zip code, which precluded using it as a fixed effect. Next, we ran multilevel, multivariable logistic regression models for each outcome by each financial stressor and the composite financial stress variable (in separate models), adjusting for age, presence of children, living alone, whether diagnosed with COVID-19, proportion non-white in zip code, and proportion in poverty within zip code. A random intercept varying at the zip code level was included in all models. For each model, odds ratios (OR) and 95% confidence intervals (CI) were estimated.
We assessed potential effect modification by running the final model within each health insurance stratum, associating the composite health risk behavior outcome measure and the financial stressor composite measure, adjusting for all confounders.
Finally, as a sensitivity analysis, we repeated the modeling steps described above, but including residential state as a fixed effect as an additional potential confounder, to further account for geographic variability and differences in lockdown intensity.
3. Results
Table 1 provides sample characteristics. The average age was 58.4. The average proportion of non-white residents in the respondents’ zip codes (n = 18,359 zip codes) based on Census data was 26.3%, and the average zip-code level proportion of residents below the poverty line (also from the Census) was 11.6%. Just over 15% of respondents lived alone at the time of the survey, and 21.9% had children of school age. Only 0.2% of respondents (n = 171) had been diagnosed with COVID-19, and 2.9% reported no health insurance. Twenty-four percent of women reported a decrease in pay (among 57,616 who considered this question applicable); 27.1% indicated that they were likely to have trouble paying bills (among the full sample); and 34.4% reported that they had either already lost their job (13.1%) or thought it is likely that they would lose their job (21.3%) due to the COVID-19 pandemic (among 51,109 women who considered that question applicable).
Table 1.
Prevalence and means of covariates, exposures, and modifier among 90,971 women in 18,359 zip codes.
| Mean (SD) | n (%) | |
|---|---|---|
| Age | 58.38 (12.19) | – |
| Percent non-white in zip code | 26.25% (20.79%) | – |
| Percent below poverty in zip code | 11.57% (7.13%) | – |
| Have children who are normally in school | – | 19,889 (21.86%) |
| Live alone | – | 13,753 (15.12%) |
| Diagnosed with COVID-19 | – | 171 (0.19%) |
| Pay has decreaseda | – | 13,785 (23.93%) |
| Likely to have trouble paying bills | – | 24,692 (27.14%) |
| Lost job or likely to lose joba | – | 17,570 (34.38%) |
| One or more financial stressors | – | 34,319 (37.73%) |
| No health insurance | – | 2,666 (2.93%) |
SD = standard deviation.
Denominator for prevalence of pay decrease = 57,616 women; denominator for prevalence of being likely to lose job or already lost job = 51,109 women (not including “not applicable” responses).
The complete-case sample (n = 46,900; including only women who did not respond “not applicable” to the decrease in pay or job loss questions) were slightly younger on average than the full sample, more likely to have children of school age, less likely to live alone, more likely to say they are likely to have trouble paying bills, and slightly more likely to have a negative behavior change. However, the zip code-level variables (proportion non-white and proportion under the poverty line) were no different, suggesting that these individuals did not, on average, live in systematically different areas.
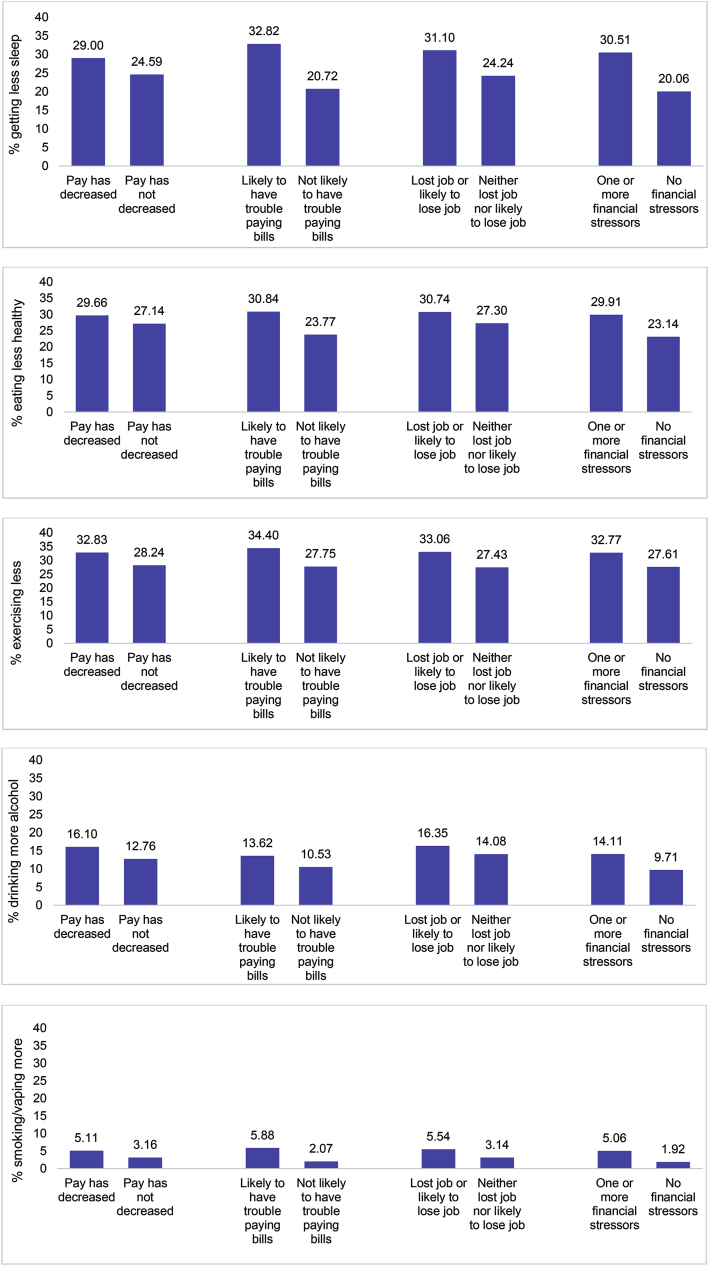
Fig. 2 shows the prevalence of each health risk behavior outcome by each financial stressor, including the composite measure of one or more stressors. For each comparison, a higher proportion of the health risk behavior was reported among those who experienced the stressor. For example, 32.8% of women who reported likelihood of having trouble paying bills said they were getting less sleep since the start of the pandemic, compared to only 20.7% getting less sleep among women who did not report potential difficulty paying bills. About 33% among women who lost their job or thought it was likely that they would lose their job reported that they were exercising less, compared to 27.4% exercising less among those who did not endorse this stressor. For substance use, 16.1% of women with a decrease in pay reported drinking more alcohol since the pandemic, compared to 12.8% among women who did not report a decrease in pay. Similarly, almost three times as many women who reported likelihood of difficulty paying bills indicated they were smoking or vaping more since the start of the pandemic (5.9%), compared to those without likelihood of trouble paying bills (2.1%).
Fig. 2.
Prevalence of each health risk behavior change since COVID-19 (outcomes), by each COVID-19-related financial stressor (exposures) among 90,971 women. Denominator for pay decrease comparisons = 57,616 women; denominator for job stress comparisons = 51,109 women (not including “not applicable” responses).
ICCs (calculated from random-intercept only models) for each outcome were as follows: 0.011 for getting less sleep, 0.009 for eating less healthy, 0.02 for exercising less, 0.092 for drinking more alcohol, 0.198 for smoking or vaping more, and 0.016 for two or more negative health risk behavior changes. These values indicate that residential zip codes were associated with the highest proportion of variation for increases in smoking or vaping (19.8%), and the lowest proportion of variation for less healthy eating (0.9%)
Table 2 presents ORs and corresponding 95% CIs from the multilevel, multivariable logistic regression models with each financial stressor and the composite financial stress measure as independent variables (in separate models), and each of the health risk behavior change measures as the dependent variables, with each model controlling for age, presence of children, whether living alone, whether diagnosed with COVID-19, proportion non-white in zip code, and proportion in poverty within zip code. In every model, there was a statistically significant, positive association between the financial stressor of interest and the health risk behavior change of interest, with magnitudes of association ranging from OR = 1.07 (95% CI: 1.02, 1.12) for the relationship between trouble paying bills and drinking more alcohol since COVID-19, to OR = 2.52 (95% CI: 2.33, 2.73) for the relationship between that same financial exposure and smoking or vaping more since COVID-19. When assessing the two composite measures in one model, reporting one or more financial stressors was associated with 56% higher odds (OR = 1.56; 95% CI: 1.51, 1.60) of reporting two or more health risk behavior changes (endorsed by 25.79% of total women), compared to having no financial stressors.
Table 2.
Adjusteda multilevel logistic regression models for the relationships between COVID-19-related financial stressors (exposures) and health risk behavior changes since COVID-19 (outcomes), among 90,971 womenb in 18,359 zip codes.
| Exposures |
||||||||
|---|---|---|---|---|---|---|---|---|
| Pay has decreased |
Likely to have trouble paying bills |
Lost job or likely to lose job |
One or more financial stressors |
|||||
| Outcomes | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Getting less sleep | 1.23 | (1.18, 1.29) | 1.73 | (1.67, 1.78) | 1.40 | (1.35, 1.46) | 1.60 | (1.55, 1.66) |
| Eating less healthy | 1.12 | (1.07, 1.17) | 1.32 | (1.28, 1.36) | 1.18 | (1.13, 1.23) | 1.30 | (1.26, 1.34) |
| Exercising less | 1.25 | (1.20, 1.30) | 1.37 | (1.33, 1.41) | 1.30 | (1.25, 1.35) | 1.30 | (1.25, 1.33) |
| Drinking more alcohol | 1.26 | (1.19., 1.33) | 1.07 | (1.02, 1.12) | 1.17 | (1.11, 1.23) | 1.18 | (1.13, 1.24) |
| Smoking/vaping more | 1.66 | (1.51, 1.82) | 2.52 | (2.33, 2.73) | 1.79 | (1.63, 1.96) | 2.30 | (2.12, 2.50) |
| Two or more negative health risk behavior changes | 1.32 | (1.27, 1.38) | 1.65 | (1.59, 1.70) | 1.41 | (1.36, 1.47) | 1.56 | (1.51, 1.60) |
OR = odds ratio.
CI = confidence interval.
Each model is adjusted for age, presence of children, whether living alone, whether diagnosed with COVID-19, proportion non-white in zip code, proportion in poverty within zip code, and a random intercept varying at the zip code level.
Denominator for pay decrease models = 57,616 women; denominator for job stress models = 51,109 women (not including responses of “not applicable”).
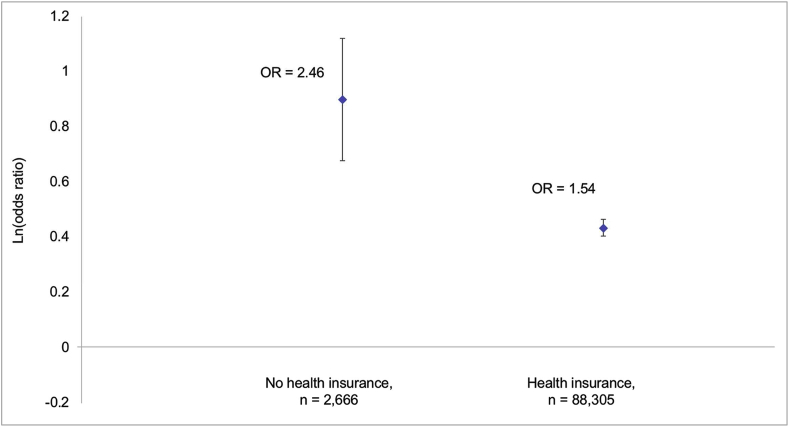
Fig. 3 displays this final adjusted model using the composite measures, stratified by health insurance status, and graphed on the log odds scale. Respondents with no health insurance had an OR of 2.46 (95% CI: 1.97, 3.07) for the relationship between one or more financial stressors and two or more health risk behavior changes, while respondents with health insurance had an OR of 1.54 (95% CI: 1.50, 1.59) for this relationship, without overlapping confidence intervals.
Fig. 3.
Adjusted a multilevel logistic regression models (odds ratios presented on the log scale) for the relationships between one or more COVID-19-related financial stressors (composite exposure) and two or more health risk behavior changes (composite outcome) since COVID-19, by health insurance status.
Ln = natural log. OR = odds ratio. a Each model is adjusted for age, presence of children, whether living alone, whether diagnosed with COVID-19, proportion non-white in zip code, proportion in poverty within zip code, and a random intercept varying at the zip code level.
In the sensitivity analyses run among only the complete-case sample (n = 46,900; including only women who did not respond “not applicable” to either the decrease in pay or job loss question), the OR for one or more financial stressors in the final summary model was slightly lower than in the full sample (1.46 compared to 1.56). Similarly, the stratified OR among those with no health insurance in the complete-case sample was slightly lower than in the full sample (2.24 compared to 2.46) but remained higher than those with health insurance in the complete-case sample (1.45), showing the same overall pattern as in the main analyses, with non-overlapping confidence intervals.
Appendix Table 1 shows the results of the sensitivity analyses of the models including state as a fixed effect. Overall, the results were extremely similar to the main results, only slightly attenuated. The stratified model run only among individuals with no health insurance did not converge, due to the small sample size and many cells for the state variable. However, given that the stratum of individuals with health insurance produced a nearly identical estimate for the relationship between one or more financial stressors and two or more behavior changes (OR = 1.53; 95% CI: 1.48, 1.58; not shown in table) when compared to this same stratum in the main version without state as a fixed effect (OR = 1.54; 95% CI: 1.50, 1.59), we would expect the relationship to be equally similar among those without health insurance, if there was enough variation across cells to measure it.
4. Discussion
In this study, we found that almost 40% of women who responded to a large national survey in Spring 2020 reported one or more financial stressors related to COVID-19; 57% reported one or more health risk behavior changes since COVID-19; and 26% reported two or more health risk behavior changes. Financial hardship was consistently associated with higher likelihood of reporting health risk behavior changes, both individually and when combined into composite measures. Finally, the overall relationship between financial hardship and health risk behaviors was modified by health insurance status, as a likely marker for broader socioeconomic context and resources.
This is the first study to our knowledge to evaluate these relationships in the US during the COVID-19 pandemic. Nelson and colleagues surveyed US respondents on stressors and concerns earlier in the pandemic (March 14–16, 2020), and found that 14.7% reported reduced wages or work hours and 1.5% reported that they had lost their job (Nelson et al., 2020). By contrast, we found that 23.9% reported a pay decrease and 13.1% had lost or been laid off from their job. The higher proportions in our study are likely due to the later assessment time of the survey, which aligns with national trends and more recent studies that suggest greater proportions of individuals lost their jobs over time (Ettman, Abdalla, et al., 2020; Tappe & Luhby, 2020).
One recent study of health behavior and financial and food security among Canadian families during COVID-19 observed that eating more snack foods and screen time each increased for the large majority of families surveyed, while physical activity decreased, and both of these changes were more pronounced among mothers compared to fathers (Carroll et al., 2020). Although these trends of reported health risk behaviors are consistent with those found in our study, the study by Carroll and colleagues did not assess these changes by levels of financial stressors. Financial stress was also less commonly reported in the study out of Canada, which may be explained by the smaller economic burden accrued in Canada compared to the US, and the less specific way in which financial stress was measured in that study. (though again it was more commonly reported among mothers, 19%, than fathers, 14%).
There is a paucity of studies on the relation between these types of financial stressors during pandemics and health risk behavior changes. However, there is emerging evidence that stress in general during COVID-19 is associated with less sleep. One study of posttraumatic stress symptoms (PTSS) in China during COVID-19 found that PTSS was associated with poor sleep quality (Liu et al., 2020). Similarly, a study of healthcare workers in China during this same time assessed stress, anxiety, and sleep quality, and found that sleep quality was low overall and significantly associated with stress levels (Xiao et al., 2020). These findings are potentially consistent with our conclusions that financial hardship (a different type of stress than healthcare work, but still in the context of COVID-19) was associated with less reported sleep, though we were not able to examine sleep quality specifically, or the potential buffering effects of social support and self-efficacy as the latter study did. We did, however, find a potential buffering effect of health insurance, as a likely marker for a broader set of resources and support.
A 2003 study that surveyed persons in Taiwan directly after the severe acute respiratory syndrome (SARS) outbreak found that respondents who experienced an economic impact related to the epidemic had higher levels of depression than those with no economic impact (Ko et al., 2006). Although we were not able to assess depression in this study, it is plausible that unmeasured depression and other mental health problems were contributors to the observed changes in health risk behavior in our study, potentially working as mediators between financial problems and these behaviors.
Our findings might also be compared to prior studies in non-pandemic contexts, which have found that high levels of stress (and PTSD, which we were unable to measure in this study) are associated with health risk behavior changes among women, such as decreased exercise and healthy eating, on the pathway to cardiovascular disease (Kubansky et al., 2009; Kubzansky et al., 2014; Sumner et al., 2015). For substance use specifically, studies in non-pandemic contexts have found that financial hardship is associated with greater drinking or smoking. For example, one study from the International Tobacco Control Four Country Survey found that even though smokers who reported financial stress were more likely to report an interest in quitting smoking at baseline compared to those without financial stress, they were also less likely to have attempted to quit smoking at the follow-up assessment (Siahpush et al., 2009).
Our study should be interpreted in light of five primary limitations. First, our sample is likely not representative of the US female population as a whole. Our prevalence estimates may be higher or lower than in a random sample of women, if those who were more affected by COVID-19 were more or less likely to participate in the survey, respectively. However, our estimate of financial stressor prevalence was almost identical to that of a nationally representative survey conducted during the same time period (Ettman, Abdalla, et al., 2020).
Second, all of our measures are self-reported and from one source. Thus, it is possible that some individuals over-reported or under-reported financial problems or changes in behavior, and this type of misclassification may be correlated across different measures, due to use of the same method for collecting both exposure and outcome information. It would be ideal—though not practical—to validate these reported experiences and behaviors through less subjective methods such as job records for financial stressors or longitudinal food frequency diaries for changes in eating. However, given the large magnitudes of association we observed and consistency across all measures, misclassification is unlikely to account for the entirety of these relationships.
A third limitation is the lack of additional demographic measures due to the short overall survey. There are potentially key confounders that we were unable measure such as race, income, education, and marital status. To address this issue, we included in our models measures of family composition (whether the respondent has children or lives alone) and also zip code-level percent non-white and percent below the poverty line to partially adjust for unmeasured confounding at the individual level. In addition to more data on confounders, it would similarly be ideal to have information on mental health diagnoses such as depression, PTSD, and anxiety, which are likely mediators on the pathway from financial stressors to health risk behaviors.
A fourth limitation of this study is that respondents may have changed their health risk behaviors not only through pathways of stress, but rather (or also) out of necessity, due to shutdowns and other population-level restrictions. For example, individuals may normally exercise via their commute to work, which they may no longer do because of job loss or work-from-home policies, or via sports or leisure activities that are no longer possible. We were unable to measure the reasons behind changes in behavior but expect that they are multi-faceted.
Finally, this was a cross-sectional study and we do not have information on the exact timing of our measures, other than that the knowledge they all occurred after the start of COVID-19 pandemic (which was up to the interpretation of the respondent). It is possible, then, that health risk behaviors started changing before financial stressors occurred. Further, individuals who responded to the survey earlier (e.g., in March) likely had different experiences from those who responded later (e.g., in April), depending on where in the country they were located. Future studies should assess these relationships longitudinally if possible, with specific timing of measures. It would also be informative to collect data temporally later in the pandemic, such that longer-term effects of our exposures of interest—as well as COVID-19 diagnosis—would be more clear and these experiences would be more prevalent, given the rising case count of COVID-19 over time. COVID-19 diagnosis could be a modifier in addition to a potential confounder, but we did not have enough COVID-19 cases in our sample from Spring 2020 to measure this.
Despite these limitations, our preliminary study highlights the importance of considering long-term and downstream health effects of the COVID-19 pandemic and its sequelae among women, in addition to the short-term effects (i.e., of the virus itself), which rightly take precedence during a pandemic. In other words, it is incumbent on us not to overlook the full range of consequences of the pandemic, such as the health risk behavior changes that economic fallout from social distancing may cause. These behavior changes may eventually lead to cardiovascular disease and other physical health problems, particularly because health risk behaviors are notoriously difficult for individuals to improve. Further, women who are already more vulnerable—for example, those without health insurance—may be the most affected by this mass-traumatic event (Patel et al., 2020).
Author statement
Laura Sampson: Conceptualization, methodology, formal analysis, data curation, writing – original draft, visualization. Catherine Ettman: Conceptualization, data curation, writing – review & editing. Salma Abdalla: Conceptualization, writing – review & editing. Elizabeth Colyer: Investigation, project administration, funding acquisition, data curation, writing – review & editing. Kimberly Dukes: Methodology, supervision, funding acquisition, writing – review & editing. Kevin Lane: Methodology, formal analysis, funding acquisition, data curation, visualization, writing – review & editing. Sandro Galea: Conceptualization, supervision, funding acquisition, writing – review & editing.
Funding
Laura Sampson was supported by the National Institutes of Health [T32 HL 098048]. Catherine K. Ettman was supported by the National Institutes of Health [T32 AG 23482–15]. Kimberly Dukes and Kevin J. Lane each received funding from Sharecare, Inc. These funding sources did not have any role in study design, analysis, writing, interpretation of data, or the decision to submit this manuscript for publication. No other authors have funding to declare.
Declaration of competing interest
Elizabeth Colyer is an employee of Sharecare, Inc.; Kimberly Dukes and Kevin J. Lane each received funding from Sharecare, Inc.; and data collection was carried out by Sharecare, Inc. However, this organization did not have any role in study design, analysis, writing, interpretation of data, or the decision to submit this manuscript for publication. No other authors have any interests to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100734.
Contributor Information
Laura Sampson, Email: Lasampson@hsph.harvard.edu, Lsamps@bu.edu.
Catherine K. Ettman, Email: cettman@bu.edu.
Salma M. Abdalla, Email: abdallas@bu.edu.
Elizabeth Colyer, Email: ecolyer@sharecare.com.
Kimberly Dukes, Email: dukeska@bu.edu.
Kevin J. Lane, Email: klane@bu.edu.
Sandro Galea, Email: sgalea@bu.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Adjusted a multilevel logistic regression models for the relationships between COVID-19-related financial stressors (exposures) and health risk behavior changes since COVID-19 (outcomes), among 90,971 women b in 18,359 zip codes, with state as a fixed effect. OR = odds ratio. CI = confidence interval. a Each model is adjusted for state of residence, age, presence of children, whether living alone, whether diagnosed with COVID-19, proportion non-white in zip code, proportion in poverty within zip code, and a random intercept varying at the zip code level. b Denominator for pay decrease models = 57,616 women; denominator for job stress models = 51,109 women (not including responses of “not applicable”).
References
- Alon T., Doepke M., Olmstead-Rumsey J., Tertilt M. 2020. This time it's different: The role of women's employment in a pandemic recession. [DOI] [Google Scholar]
- Bellows-Riecken K.H., Rhodes R.E. Vol. 46. 2008. A birth of inactivity? A review of physical activity and parenthood; pp. 99–110. (Preventive medicine). Issue 2. Prev Med. [DOI] [PubMed] [Google Scholar]
- Bergman H., Chan P., Cooper A., Shirley E., Goto T., Fine T., Cohen G., Sampson L., Ganocy S., Tamburrino M., Liberzon L., Calabrese J., Galea S., Feeny N. Military Behavioral Health; 2019. Examining the impact of PTSD symptomatology on cigarette smoking among Ohio Army National Guard soldiers. [Google Scholar]
- Brondolo E., Byer K., Gianaros P.J., Liu C., Prather A.A., Thomas K., Woods-Giscombé C.L., Beatty L.A., Puryear Keita G. American Psychological Association Working Group Report; 2017. Stress and health disparities: Contexts, mechanisms, and interventions among racial/ethnic minority and low socioeconomic status populations. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulatao R.A., Anderson N.B., editors. Understanding racial and ethnic differences in health in late life: A research agenda. National research council (US) panel on race, ethnicity, and health in later life. National Academies Press (US); 2004. Behavior risk factors. [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/J.PSYCHRES.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll N., Sadowski A., Laila A., Hruska V., Nixon M., Ma D.W.L., Haines J., Study, on behalf of the G. F. H The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12(8):2352. doi: 10.3390/nu12082352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chwastiak L.A., Rosenheck R.A., Kazis L.E. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230–236. doi: 10.1016/J.PSYM.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronavirus disease 2019 (COVID-19): Cases, data, & surveillance: Cases in the US. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, june 24–30. MMWR Morb Mortal Wkly Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis P.A., Watkins L.L., Calhoun P.S., Oddone A., Sherwood A., Dennis M.F., Rissling M.B., Beckham J.C. Posttraumatic stress, heart rate variability, and the mediating role of behavioral health risks. Psychosomatic Medicine. 2014;76(8):629–637. doi: 10.1097/PSY.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ (Clinical Research Ed.) 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ene M., Leighton E.A., Blue G.L., Bell B.A. 2015. Paper 3430-2015 multilevel models for categorical data using SAS ® PROC GLIMMIX: The basics. [Google Scholar]
- Ettman C., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. Journal of Epidemiology & Community Health. 2020 doi: 10.1136/jech-2020-215213. 0, jech-2020-215213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. JAMA Network Open; 2020. Prevalence of depression symptoms in U.S. Adults before and during the COVID-19 pandemic. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Cohen G.H., Galea S. Is wealth associated with depressive symptoms in the United States? Annals of Epidemiology. 2020;43:25–31. doi: 10.1016/J.ANNEPIDEM.2020.02.001. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Financial Health Network . Financial Health Network; 2020. Income, age, race, and gender are key factors as new data shows 1 in 3 Americans earning less during COVID-19.https://finhealthnetwork.org/research/income-age-race-and-gender-are-key-factors-as-new-data-shows-1-in-3-americans-earning-less-during-covid-19/ [Google Scholar]
- Galea S., Ahern J., Resnick H., Kilpatrick D., Bucuvalas M., Gold J., Vlahov D. Psychological sequelae of the september 11 terrorist attacks in New York city. New England Journal of Medicine. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Galea S., Tracy M., Norris F., Coffey S.F. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. Journal of Traumatic Stress. 2008;21(4):357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annual Review of Public Health. 2014;35(1):169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Hall K.S., Hoerster K.D., Yancy W.S. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiologic Reviews. 2015;37(1):103–115. doi: 10.1093/epirev/mxu011. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation, NPR. Harvard T.H. The impact of coronavirus on households with children; 2020. Chan school of public health.https://drive.google.com/file/d/13Z9HD5V9_Ir7Udmlgqkw5aSVi_TLv0rF/view [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS Control and psychological effects of quarantine, toronto, Canada. Emerging Infectious Diseases. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O'Leary A., Hageman K.M., Sengeh P., Jalloh M.B., Morgan O., Hersey S., Marston B.J., Dafae F., Redd J.T. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Global Health. 2018;3(2) doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvis M.J., Wardle J. Social determinants of health. Oxford University Press; 2009. Social patterning of individual health behaviours: The case of cigarette smoking. [DOI] [Google Scholar]
- Joutsenniemi K., Martelin T., Kestilä L., Martikainen P., Pirkola S., Koskinen S. Living arrangements, heavy drinking and alcohol dependence. Alcohol and Alcoholism. 2007;42(5):480–491. doi: 10.1093/alcalc/agm011. [DOI] [PubMed] [Google Scholar]
- Karanikolos M., Mladovsky P., Cylus J., Thomson S., Basu S., Stuckler D., Mackenbach J.P., McKee M. Financial crisis, austerity, and health in Europe. The Lancet. 2013;381(9874):1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- Koenen K.C., Hitsman B., Lyons M.J., Stroud L., Niaura R., McCaffery J., Goldberg J., Eisen S.A., True W., Tsuang M. Posttraumatic stress disorder and late-onset smoking in the Vietnam era twin registry. Journal of Consulting and Clinical Psychology. 2006;74(1):186–190. doi: 10.1037/0022-006X.74.1.186. [DOI] [PubMed] [Google Scholar]
- Koenen K.C., Stellman S.D., Sommer J.F., Stellman J.M. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in vietnam veterans: A 14-year follow-up. Journal of Traumatic Stress. 2008;21(1):49–57. doi: 10.1002/jts.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C.-H., Yen C.-F., Yen J.-Y., Yang M.-J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry and Clinical Neurosciences. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Kubansky L.D., Koenen K.C., Jones C., Eaton W.W. A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychology. 2009;28(1):125–130. doi: 10.1037/0278-6133.28.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubzansky L.D., Bordelois P., Jun H.J., Roberts A.L., Cerda M., Bluestone N., Koenen K.C. The weight of traumatic stress. JAMA Psychiatry. 2014;71(1):44. doi: 10.1001/jamapsychiatry.2013.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leskin G.A., Woodward S.H., Young H.E., Sheikh J.I. Effects of comorbid diagnoses on sleep disturbance in PTSD. Journal of Psychiatric Research. 2002;36(6):449–452. doi: 10.1016/S0022-3956(02)00025-0. [DOI] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Research. 2020;287:112921. doi: 10.1016/J.PSYCHRES.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah G.A., Brown D.W. An overview of cardiovascular disease burden in the United States. Health Affairs. 2007;26(1):38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- Merlo J., Chaix B., Ohlsson H., Beckman A., Johnell K., Hjerpe P., Råstam L., Larsen K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. Journal of Epidemiology & Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. BMJ Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A.H., Marks J.S., Stroup D.F., Gerberding J.L. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Nandi A., Prescott M.R., Cerdá M., Vlahov D., Tardiff K.J., Galea S. Economic conditions and suicide rates in New York City. American Journal of Epidemiology. 2012;175(6):527–535. doi: 10.1093/aje/kwr355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson L.M., Simard J.F., Oluyomi A., Nava V., Rosas L.G., Bondy M., Linos E. US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA Internal Medicine. 2020;190(7):1020–1022. doi: 10.1001/jamainternmed.2020.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M., Kim Y., McDowell I., Wong S., Qiu H., Wong I., Galea S., Leung G. Mental health during and after protests, riots and revolutions: A systematic review. Australian and New Zealand Journal of Psychiatry. 2020;54(3) doi: 10.1177/0004867419899165. [DOI] [PubMed] [Google Scholar]
- Nomaguchi K.M., Bianchi S.M. Exercise time: Gender differences in the effects of marriage, parenthood, and employment. Journal of Marriage and Family. 2004;66(2):413–430. doi: 10.1111/j.1741-3737.2004.00029.x. [DOI] [Google Scholar]
- Parks S.E., Housemann R.A., Brownson R.C. Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. Journal of Epidemiology & Community Health. 2003;57(1):29–35. doi: 10.1136/jech.57.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J.A., Nielsen F.B.H., Badiani A.A., Assi S., Unadkat V.A., Patel B., Ravindrane R., Wardle H. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health. 2020;183:110–111. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy. 2020;16(1):67–73. doi: 10.1080/15487733.2020.1776561. [DOI] [Google Scholar]
- Reinicke C. Business Insider; 2020, August 20. US weekly jobless claims defy economists and climb back above 1 million as the labor-market recovery slows.https://www.businessinsider.com/us-weekly-jobless-claims-insurance-filings-labor-market-unemployment-coronavirus-2020-8 [Google Scholar]
- Siahpush M., Yong H.-H., Borland R., Reid J.L., Hammond D. Smokers with financial stress are more likely to want to quit but less likely to try or succeed: Findings from the international Tobacco Control (ITC) four country survey. Addiction. 2009;104(8):1382–1390. doi: 10.1111/j.1360-0443.2009.02599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver R., Holman E., McIntosh D., Poulin M., Gil-Rivas V. Nationwide longitudinal study of psychological responses to september 11. Journal of the American Medical Association. 2002;288(10) doi: 10.1001/JAMA.288.10.1235. [DOI] [PubMed] [Google Scholar]
- State mandated stay-at-home orders by date of implementation. Henry J Kaiser Family Foundation; 2020. https://www.kff.org/wp-content/uploads/2020/04/Figure-State-Actions-by-Date.png [Google Scholar]
- Sumner J.A., Kubzansky L.D., Elkind M.S.V., Roberts A.L., Agnew-Blais J., Chen Q., Cerdá M., Rexrode K.M., Rich-Edwards J.W., Spiegelman D., Suglia S.F., Rimm E.B., Koenen K.C. Trauma exposure and posttraumatic stress disorder symptoms predict onset of cardiovascular events in women. Circulation. 2015;132(4):251–259. doi: 10.1161/CIRCULATIONAHA.114.014492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tappe A., Luhby T. CNN Business; 2020. April 16). 22 million Americans have filed for unemployment benefits in the last four weeks.https://www.cnn.com/2020/04/16/economy/unemployment-benefits-coronavirus/index.html [Google Scholar]
- United States Census Bureau . 2019. American community survey.https://www.census.gov/programs-surveys/acs [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanjani F.A.K., Schaie K.W., Willis S.L. Age group and health status effects on health behavior change. Behavioral Medicine. 2006;32(2):36–46. doi: 10.3200/BMED.32.2.36-46. [DOI] [PubMed] [Google Scholar]
- Zumbrun J. 2020, May 10. Coronavirus slump is worst since Great depression. Will it be as painful? The wall street journal.https://www.wsj.com/articles/coronavirus-slump-is-worst-since-great-depression-will-it-be-as-painful-11589115601 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Adjusted a multilevel logistic regression models for the relationships between COVID-19-related financial stressors (exposures) and health risk behavior changes since COVID-19 (outcomes), among 90,971 women b in 18,359 zip codes, with state as a fixed effect. OR = odds ratio. CI = confidence interval. a Each model is adjusted for state of residence, age, presence of children, whether living alone, whether diagnosed with COVID-19, proportion non-white in zip code, proportion in poverty within zip code, and a random intercept varying at the zip code level. b Denominator for pay decrease models = 57,616 women; denominator for job stress models = 51,109 women (not including responses of “not applicable”).