Abstract
Plantar fasciitis is a common condition of heel pain with a lifetime incidence up to 10%. For this entity, conservative treatment is considered the gold standard, involving non-steroidal anti-inflammatory drugs, stretching exercises of the plantar fascia, activity modifications, ice, and insoles. When patients do not respond to these treatments, partial or total plantar fascia release has been the mainstay of treatment, with success rates of approximately 70% to 90%. For this purpose, several techniques have been described, including open, percutaneous, and endoscopic release. The objective of this Technical Note is to describe the nonassisted 2-portal endoscopic plantar fascia release in a patient with recalcitrant plantar fasciitis.
Plantar fasciitis is a common condition of heel pain with a lifetime incidence up to 10%.1 It is the most common cause of heel pain, accounting for 80% of these cases.2 This condition tends to affect people between 40 and 60 years, showing a greater prevalence in women.1 Risk factors associated with plantar fasciitis include obesity, prolonged weight-bearing, and reduced ankle dorsiflexion, and it occurs bilaterally in one-third of cases.3,4
Although plantar fascia pathology is not completely understood, it seems to be a non-inflammatory structural breakdown secondary to myxoid degeneration with microtears within the fascia, collagen necrosis, and angiofibroblastic hyperplasia.5
For this entity, conservative treatment is considered the gold standard, involving non-steroidal anti-inflammatory drugs, stretching exercises of the plantar fascia, activity modifications, ice, and insoles.6 Moreover, steroid injections can be performed. For patients with recalcitrant plantar fasciopathy, focal extracorporeal shockwave can be used with success rates between 50% and 65%.2
Conservative treatment is effective in 90% of patients. When patients do not respond after 6 to 12 months, surgical treatment is required in 5% to 10% of patients.7 In these patients, partial or total plantar fascia release has been the mainstay of treatment, with success rates of approximately 70% to 90%.7 Different surgical treatments have been described to this purpose, including open fasciotomy or minimally invasive procedures that can be performed percutaneously or with the aid of an endoscope.8
Several clinical trials had reported previously that endoscopic plantar fascia release (EPFR) resulted in excellent relief of pain, with patient satisfaction ranges from 60% to 80% and low complication rates.9,10 The purpose of this Technical Note is to describe the 2-portal EPFR in a patient with recalcitrant plantar fasciitis.
Surgical Technique (With Video Illustration)
Endoscopic Plantar Fascia Release
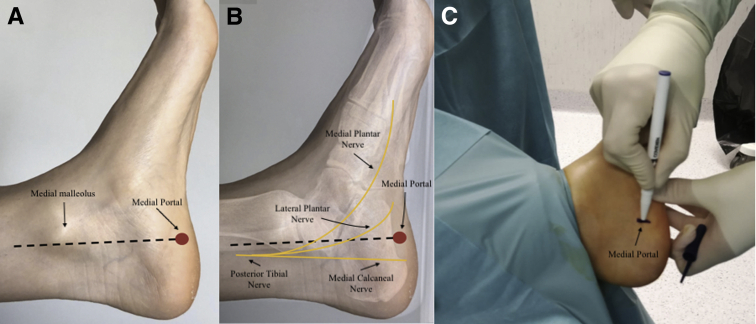
The procedure is performed with the patient under spinal anesthesia without a tourniquet applied. The patient is positioned supine with the ankle draped and hanging freely over the edge of the table (Fig 1). With the ankle in a neutral position, a line distally from the posterior aspect of the medial malleolus to the intersection of the medial origin of the plantar fascia at the calcaneal tuberosity is drawn (Fig 2 A and B). A medial portal is performed by creating a 5-mm skin incision at this location (Fig 2C).
Fig 1.

The patient’s left foot is positioned supine with the ankle draped and hanging freely over the edge of the table. Medial view.
Fig 2.
Left foot, medial view. (A) Draw a line distally from the posterior aspect of the medial malleolus to the intersection of the medial origin of the plantar fascia at the calcaneal tuberosity. (B) In yellow, schematic drawing of the posterior tibial nerve and its branches. (C) Medial portal skin incision.
Blunt dissection is performed using a mosquito clamp and an elevator to clear the subcutaneous tissue from the plantar fascia. With this approach, care should be taken to avoid lesion of the calcaneal nerve medial branch.
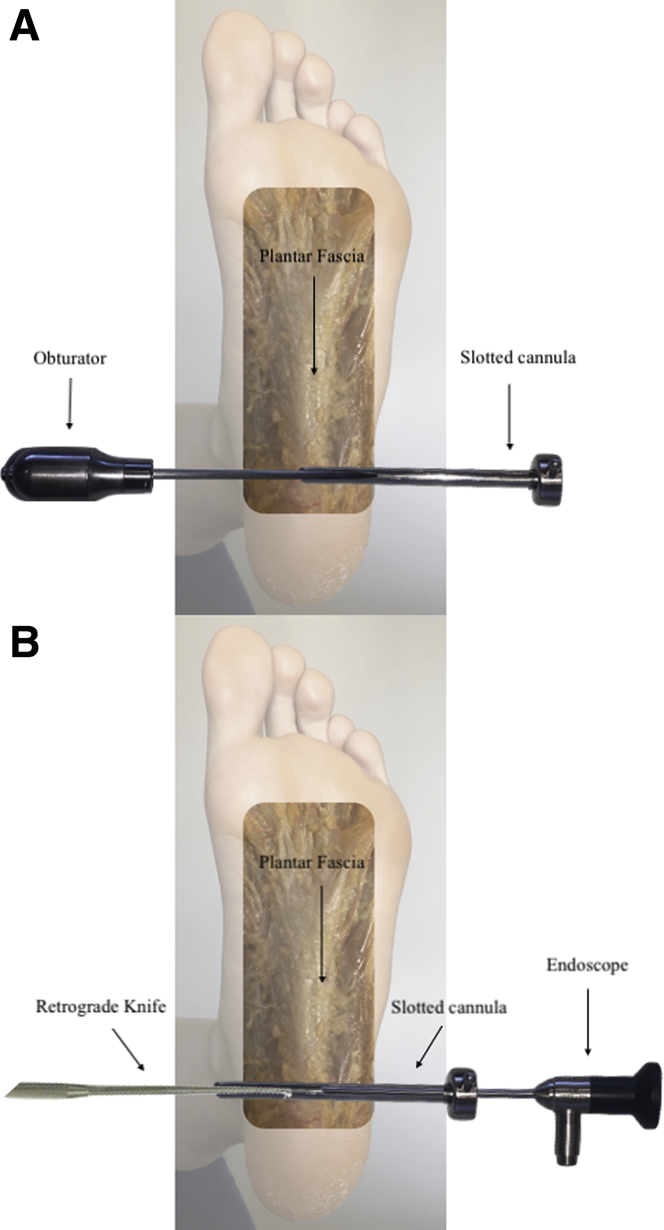
At this point, an obturator is inserted through the medial portal and progressed under the fascia until it is palpable in the lateral skin surface (Fig 3 A and B). The lateral incision is performed over the protruding obturator (Fig 3C), and slotted cannula (Smith & Nephew, Andover, MA) is placed over the obturator and introduced from lateral to medial (Fig 4 A and B).
Fig 3.
Left foot, plantar view. (A-B) An obturator is inserted through the medial portal and progressed under the fascia until it is palpable in the lateral skin surface. (C) Lateral portal skin incision.
Fig 4.
Left foot, plantar view. (A) Slotted cannula placed over the obturator and introduced from lateral to medial. (B) Endoscope is placed in the lateral portal, and a retrograde knife is placed in the medial portal
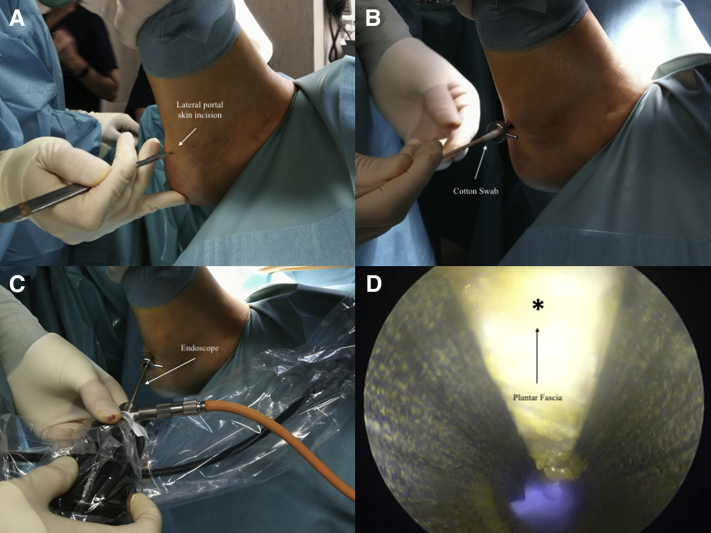
Cotton swabs can be used to remove debris and fluid inside the cannula (Fig 5 A and B). An endoscope is placed laterally and plantar fascia is visualized proximally as a pearl-shaped soft tissue (Fig 5 C and D).
Fig 5.
Left foot, lateral view. (A) Lateral portal skin incision. (B) Use cotton swabs to remove debris and fluid from inside the cannula. (C) The endoscope is placed laterally. (D) Plantar fascia (∗) is visualized proximally as a pearl-shaped soft tissue.
Before performing plantar fascia release, it is important to measure the width of the plantar fascia to release only the medial aspect and respect the lateral as well. For this purpose, a ruler is introduced through the medial portal.
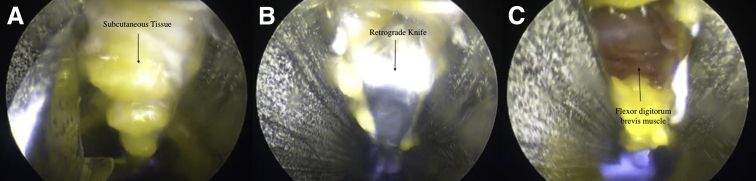
To place tension over the fascia, the foot and ankle are dorsiflexed. A triangle knife (ECTRA II; Smith & Nephew) is inserted through the medial portal and an incision is made at the lateral limit of the fasciotomy. Then, the retrograde knife (ECTRA II; Smith & Nephew) is inserted through the medial portal and release of the fascia is performed from lateral to medial. It is important to tighten the fascia by dorsiflexing the foot before release (Fig 6 A and B).
Fig 6.
Plantar fascia, endoscopic view. (A) Subcutaneous tissue and triangle knife. (B) A retrograde knife inserted through the medial portal. (C) Once the fascia is released, the flexor digitorum brevis muscle is exposed.
The flexor digitorum brevis muscle is seen when complete release is performed (Fig 6C). Wound are closed with nonabsorbable suture, and a soft bandage is applied.
To perform this technique, neither ultrasound or radioscopy assistance is necessary. This reduces surgical time, radiographic exposure, and avoids the learning curve needed to use the ultrasound.
Partial weight bearing with crutches is allowed immediately if tolerated. Full weight bearing is allowed after wound healing and stretching exercises are recommended at this moment.
A step-by-step description of the surgical technique is summarized in Table 1.
Table 1.
Step-by Step Nonassisted Endoscopic Plantar Fascia Release for Recalcitrant Fasciitis
| Step | Description |
|---|---|
| 1 | The patient is positioned supine with the ankle draped and hanging freely over the edge of the table. |
| 2 | With the ankle in a neutral position, a line distally from the posterior aspect of the medial malleolus to the intersection of the medial origin of the plantar fascia at the calcaneal tuberosity is drawn. |
| 3 | We routinely use an accessory posterolateral portal, 1 cm proximal to the conventional posterolateral portal. |
| 4 | A medial portal is performed by creating a 5-mm skin incision at this location. |
| 5 | Blunt dissection is performed using a mosquito clamp and an elevator to clear the subcutaneous tissue from the plantar fascia. |
| 6 | An obturator is inserted through the medial portal and progressed under the fascia until it is palpable in the lateral skin surface. |
| 7 | The lateral incision is performed over the protruding obturator, and a slotted cannula is placed over the obturator and introduced from lateral to medial. Cotton swabs can be used to remove debris and fluid inside the cannula. |
| 8 | The endoscope is placed laterally, and the plantar fascia is visualized proximally as a pearl-shaped soft tissue. |
| 9 | The foot and ankle are dorsiflexed. A triangle knife is inserted through the medial portal and incision is made at the lateral limit of the fasciotomy. Then, the retrograde knife is inserted through the medial portal and release of the fascia is performed from lateral to medial. |
| 10 | The flexor digitorum brevis muscle is seen when complete release is performed. Wounds are closed with a nonabsorbable suture, and a soft bandage is applied. |
Table 2 shows advantages and limitations. Table 3 provides pearls and pitfalls in performing this procedure. Video 1 shows the whole technique in detail.
Table 2.
Advantages and Limitations
| Advantages |
| Minimally invasive technique |
| Neither ultrasound or radioscopy assistance is necessary. This reduces surgical time, radiographic exposure, and avoids the learning curve needed to use the ultrasound |
| Avoids damaging the articular cartilage |
| Minimizes soft-tissue injury, allows direct visualization of plantar fascia, and minimizes possible neurovascular complications. |
| Shorter recovery time and early postoperative mobilization. |
| Clear visualization of the anatomy, monitoring the amount of fascia incised. |
| Limitations |
| Risk of lesion of the calcaneal nerve medial branch. |
| Moderate learning curve. |
| Specific materials needed. |
| Experience in foot and ankle endoscopy. |
Table 3.
Pearls, Pitfalls, and Risks
| Pearls |
| Cotton swabs can be used to remove debris and fluid inside the slotted cannula. |
| It is important to measure the width of the plantar fascia to release only the medial aspect and respect the lateral side. |
| It is important to tighten the fascia by dorsiflexing the foot before release. |
| To perform this technique, neither ultrasound or radioscopy assistance is necessary. This reduces surgical time, radiographic exposure, and avoids the learning curve needed to use the ultrasound. |
| To minimize nerve entrapment, is important to perform a blunt dissection in the medial portal before introduce the cannula and, once established, not to mobilize the cannula to prevent nerve injuries secondary to instrumental manipulation. |
| We recommend having previous experience in foot and ankle arthroscopy/endoscopy, as it is a particularly demanding technique. |
| Pitfalls and risks |
| Risk of nerve injury, secondary to the proximity between the primary medial portal and the posterior tibial nerve and its branches. |
| Flattening of the longitudinal arch and pain in the lateral column if the resected fascia is more than 40% to 50% of the total width. |
| Risk of heel pain, calcaneal stress fractures, incisional pain, and postoperative infection. |
Discussion
Several trials have reported good-to-excellent postoperative results after plantar fascia release in patients in whom conservative treatment has failed.11 Related to these techniques, EPFR was initially described by Barrett and Day.12 The main advantages of this technique compared with others are that EPFR minimizes soft-tissue injury, neither ultrasound or radioscopy assistance is necessary, it allows direct visualization of plantar fascia, and it minimizes possible neurovascular complications.
EPFR is a minimally invasive technique that minimizes complications related to open surgery such as plantar heel hypertrophic scar formation, infection, or wound dehiscence. As a result, a shorter recovery time and early postoperative mobilization therapy has been reported.13
One of the keys to successful outcome in plantar fascia release is the amount of fascia incised. Originally, Saxena et al.14 recommended complete resection of the plantar fascia but, with continuous experience and evaluation of the complications, they concluded that extent of plantar fascia resected is an important contributing factor to the rate of complications, and they recommended only partial fascia release of the medial third. The main reason is that plantar fascia resections more than 40% to 50% of the total width have been associated with flattening of the longitudinal arch and pain in the lateral column.3,15 This complication accounts for more than 50% of chronic complications.7 For this fact, we recommended to perform a medial partial release, maximum of 50%, keeping the lateral portion intact. On this matter, EPFR offers the surgeons clear visualization of the anatomy, monitoring the amount of fascia incised, and minimizing complications related to extensive resections.
A risk of nerve injury has been reported with EPFR, secondary to the proximity between the primary medial portal and the posterior tibial nerve and its branches. To prevent this risk, some authors have described performing this technique under ultrasound assistance.9 The main problem is the requirement of a high-frequency ultrasound device and longer intraoperative times. To minimize complications secondary to nerve entrapment, we consider that is important to perform a blunt dissection in the medial portal before introduce the cannula and, once established, not to mobilize the cannula to prevent nerve injuries secondary to instrumental manipulation. Other potential complications after EPFR include heel pain, calcaneal stress fractures, incisional pain, and postoperative infection, but the complication rate is rather low.9,16
In conclusion, for patients with plantar fasciitis and no response after 12 months of conservative treatment (including focal extracorporeal shockwave), nonassisted partial EPFR is a safe and reproducible treatment option, with good results in terms of pain and complication rate.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The procedure is performed with the patient under spinal anesthesia without a tourniquet applied. The patient is positioned supine with the left ankle draped and hanging freely over the edge of the table. With the ankle in a neutral position, a line distally from the posterior aspect of the medial malleolus to the intersection of the medial origin of the plantar fascia at the calcaneal tuberosity is drawn. A medial portal is performed by creating a 5-mm skin incision at this location. Blunt dissection is performed using a mosquito clamp and an elevator to clear the subcutaneous tissue from the plantar fascia. With this approach, care should be taken to avoid lesion of the calcaneal nerve medial branch. At this point, the obturator is inserted through the medial portal and progressed under the fascia until it is palpable in the lateral skin surface. The lateral incision is performed over the protruding obturator, and a slotted cannula is placed over the obturator and introduced from lateral to medial. Cotton swabs can be used to remove debris and fluid inside the cannula. The endoscope is placed laterally and plantar fascia is visualized proximally as a pearl-shaped soft tissue. It is important to measure the width of the plantar fascia to release only the medial aspect. For this purpose, a ruler is introduced through the medial portal. To place tension over the fascia, the foot and ankle are dorsiflexed. A triangle knife is inserted through the medial portal, and an incision is made at the lateral limit of the fasciotomy. Then, the retrograde knife is inserted through the medial portal and release of the fascia is performed from lateral to medial. It is important to tighten the fascia by dorsiflexing the foot before release. The flexor digitorum brevis muscle is seen when complete release is performed. Wound are closed with nonabsorbable suture and soft bandage is applied. To perform this technique, neither ultrasound or radioscopy assistance is necessary.
References
- 1.MacInnes A., Roberts S.C., Kimpton J., Pillai A. Long-term outcome of open plantar fascia release. Foot Ankle Int. 2016;37:17–23. doi: 10.1177/1071100715603189. [DOI] [PubMed] [Google Scholar]
- 2.Gollwitzer H., Saxena A., DiDomenico L.A. Clinically relevant effectiveness of focused extracorporeal shock wave therapy in the treatment of chronic plantar fasciitis: A randomized, controlled multicenter study. J Bone Joint Surg Am. 2015;97:701–708. doi: 10.2106/JBJS.M.01331. [DOI] [PubMed] [Google Scholar]
- 3.Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350:2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 4.Riddle D.L., Pulisic M., Pidcoe P., Johnson R.E. Risk factors for plantar fasciitis: A matched case-control study. J Bone Joint Surg Am. 2003;85:872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Lemont H., Ammirati K.M., Usen N. Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 6.Oliva F. Percutaneous release of the plantar fascia. New surgical procedure. Muscles Ligaments Tendons J. 2017;7:338. doi: 10.11138/mltj/2017.7.2.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahu R.L. Percutaneous planter fasciitis release under local anesthesia: A prospective study. Chin J Traumatol. 2017;20:87–89. doi: 10.1016/j.cjtee.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malahias M.-A., Cantiller E.B., Kadu V.V., Müller S. The clinical outcome of endoscopic plantar fascia release: A current concept review. Foot Ankle Surg. 2020;26:19–24. doi: 10.1016/j.fas.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Ohuchi H., Ichikawa K., Shinga K., Hattori S., Yamada S., Takahashi K. Ultrasound-assisted endoscopic partial plantar fascia release. Arthrosc Tech. 2013;2:e227–e230. doi: 10.1016/j.eats.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Othman A.M.A., Hegazy I.H.A. Endoscopic plantar fasciotomy versus injection of platelet-rich plasma for resistant plantar fasciopathy. J Orthop. 2015;12:S176–S181. doi: 10.1016/j.jor.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saxena A. Uniportal endoscopic plantar fasciotomy: A prospective study on athletic patients. Foot Ankle Int. 2004;25:882–889. doi: 10.1177/107110070402501207. [DOI] [PubMed] [Google Scholar]
- 12.Barrett S.L., Day S.V. Endoscopic plantar fasciotomy for chronic plantar fasciitis/heel spur syndrome: Surgical technique—early clinical results. J Foot Surg. 1991;30:568–570. [PubMed] [Google Scholar]
- 13.Fallat L.M., Cox J.T., Chahal R., Morrison P., Kish J. A retrospective comparison of percutaneous plantar fasciotomy and open plantar fasciotomy with heel spur resection. J Foot Ankle Surg. 2013;52:288–290. doi: 10.1053/j.jfas.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Saxena A., Fournier M., Gerdesmeyer L., Gollwitzer H. Comparison between extracorporeal shockwave therapy, placebo ESWT and endoscopic plantar fasciotomy for the treatment of chronic plantar heel pain in the athlete. Muscles Ligaments Tendons J. 2012;2:312–316. [PMC free article] [PubMed] [Google Scholar]
- 15.Morsy M., Elsheikh M. Endoscopic release of resistant plantar fasciitis. Egypt Orthop J. 2014;49:250. [Google Scholar]
- 16.Healey K., Chen K. Plantar fasciitis: Current diagnostic modalities and treatments. Clin Podiatr Med Surg. 2010;27:369–380. doi: 10.1016/j.cpm.2010.03.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The procedure is performed with the patient under spinal anesthesia without a tourniquet applied. The patient is positioned supine with the left ankle draped and hanging freely over the edge of the table. With the ankle in a neutral position, a line distally from the posterior aspect of the medial malleolus to the intersection of the medial origin of the plantar fascia at the calcaneal tuberosity is drawn. A medial portal is performed by creating a 5-mm skin incision at this location. Blunt dissection is performed using a mosquito clamp and an elevator to clear the subcutaneous tissue from the plantar fascia. With this approach, care should be taken to avoid lesion of the calcaneal nerve medial branch. At this point, the obturator is inserted through the medial portal and progressed under the fascia until it is palpable in the lateral skin surface. The lateral incision is performed over the protruding obturator, and a slotted cannula is placed over the obturator and introduced from lateral to medial. Cotton swabs can be used to remove debris and fluid inside the cannula. The endoscope is placed laterally and plantar fascia is visualized proximally as a pearl-shaped soft tissue. It is important to measure the width of the plantar fascia to release only the medial aspect. For this purpose, a ruler is introduced through the medial portal. To place tension over the fascia, the foot and ankle are dorsiflexed. A triangle knife is inserted through the medial portal, and an incision is made at the lateral limit of the fasciotomy. Then, the retrograde knife is inserted through the medial portal and release of the fascia is performed from lateral to medial. It is important to tighten the fascia by dorsiflexing the foot before release. The flexor digitorum brevis muscle is seen when complete release is performed. Wound are closed with nonabsorbable suture and soft bandage is applied. To perform this technique, neither ultrasound or radioscopy assistance is necessary.