Abstract
Tears of the posterior medial meniscus root commonly result in extrusion of the meniscus and disruption of tibiofemoral contact mechanics. Transtibial pull-through repair of the root often results in healing of the tear, but postoperative extrusion may persist. In this scenario, the meniscus is unlikely to be chondroprotective. Therefore, an additional centralization procedure is necessary to improve the extrusion. Biomechanical studies have demonstrated that centralization can improve meniscus mechanics and potentially reduce the risk of osteoarthritis. This Technical Note describes an arthroscopic technique for medial meniscus posterior root repair that combines transtibial pullout and centralization sutures.
In recent years, the treatment of meniscus root tears has received much attention, given the deleterious effects that these injuries pose to tibiofemoral mechanics.1,2 Root disruption results in a loss of hoop strain resistance and increased articular cartilage contact pressure.3,4 Krych and colleagues5,6 reported that failure to recognize and repair posterior medial meniscus root tears (PMMRs) can result in rapid development of osteoarthritis in the medial compartment. Numerous studies have reported successful clinical outcomes and healing after transtibial pullout repair of the posterior root.7, 8, 9, 10 However, meniscus extrusion remains problematic. Extrusion develops rather rapidly,11 increases with age, body mass index (BMI), and varus alignment,12,13 and can persist despite well-performed anatomic root repair.10,14,15 Arthroscopic techniques have been developed to address this problem by centralizing the body of the meniscus to the tibial plateau,16,17 with promising early results.18 This Technical Note describes a technique for centralization of the medial meniscus, in conjunction with pull-through repair of the posterior meniscus root.
Surgical Technique
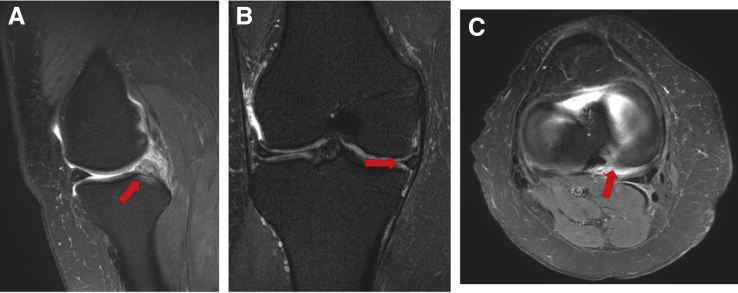
Before surgery, a thorough review of preoperative imaging is paramount to surgical planning. Fig 1 shows typical magnetic resonance imaging (MRI) images depicting a medial meniscus posterior root tear with associated extrusion. Equipment necessary to perform this surgery is listed in Table 1. Key steps, pearls, and pitfalls are summarized in Table 2. The Video details the technique, which is described below.
Fig 1.
(A) T2-weighted sagittal right knee magnetic resonance imaging (MRI) indicating medial meniscus (MM) posterior root tear with associated subchondral edema at the root footprint (arrow). (B) T2-weighted coronal MRI showing medial meniscus extrusion (arrow). (C) T2-weighted axial MRI showing MM posterior root tear (arrow).
Table 1.
Equipment Required for Medial Meniscus Posterior root Repair and Centralization
| General |
|
|
|
| Meniscus centralization |
|
|
|
|
|
|
|
| Posterior root repair |
|
|
|
|
|
|
Table 2.
Key Steps, Pearls, and Pitfalls
| Key steps |
|
|
|
|
|
|
|
| Pearls |
| Meniscus centralization |
|
|
|
|
|
|
|
| Meniscus root repair |
|
|
|
| Pitfalls |
|
|
|
Patient Positioning and Diagnostic Arthroscopy
Begin by performing an examination under anesthesia, evaluating the patient's Lachman, pivot shift, drawer test, dial test, and knee stability with varus and valgus stresses. Place the patient in a supine position, and prepared and drape the injured leg in the usual sterile manner. Perform a 3-portal diagnostic arthroscopy, evaluating for cartilage damage, loose bodies, and integrity of the cruciate ligaments and menisci.
Medial Meniscus Centralization Preparation
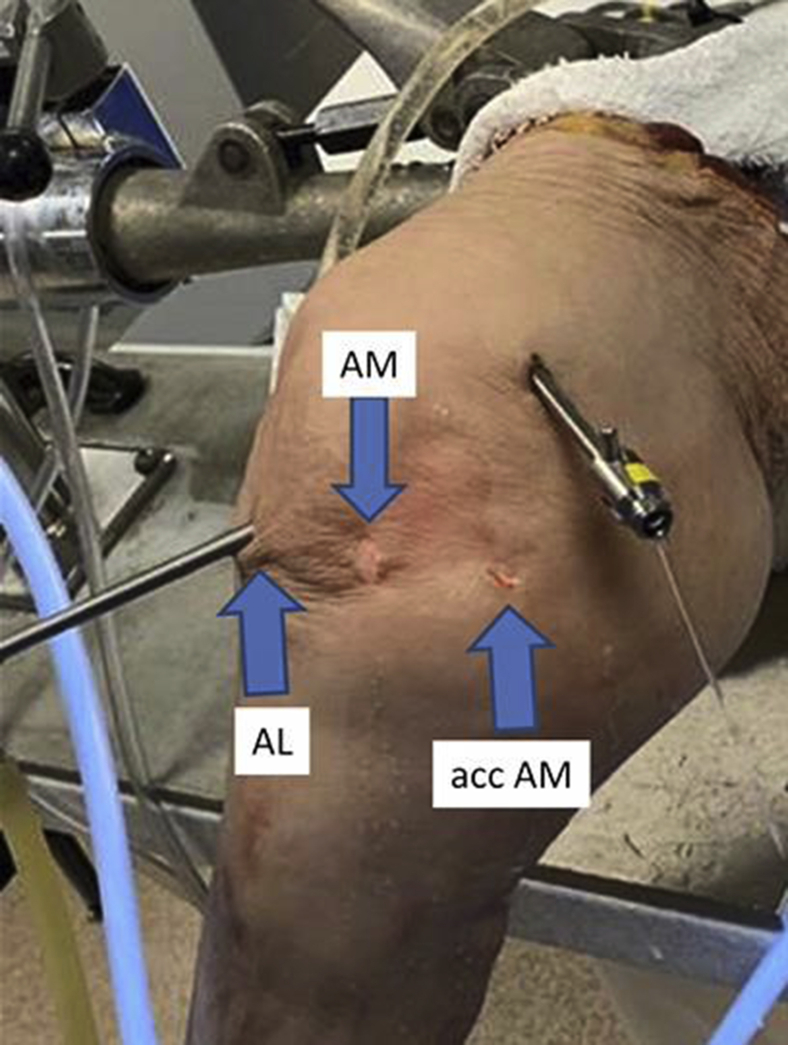
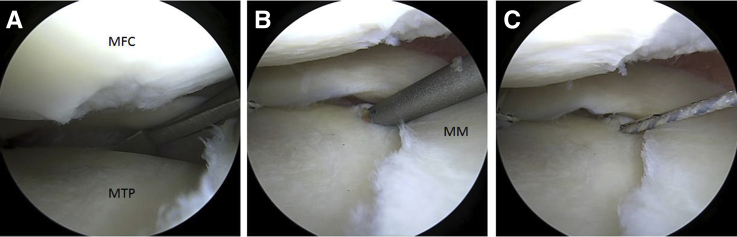
Create an accessory anteromedial (AM) portal that is proximal and ∼2 cm more medial than the standard AM portal (Fig 2). The portal is just anterior to the medial collateral ligament (MCL) fibers. Enter the medial compartment while applying valgus force to open the medial compartment of the knee, having a low threshold to perform percutaneous MCL lengthening to improve exposure, and reduce risk to damage of iatrogenic cartilage damage. Through the accessory AM portal and anterolateral (AL) portal, use a curved Bankart elevator to release the meniscotibial (MT) ligaments along the periphery of the medial tibial plateau (Fig 3). Check the mobility of the medial meniscus, as this should be increased once adequate MT ligament release is achieved.
Fig 2.
Photograph of the portals used for the procedure on a right knee. Note the location of the accessory (acc) anteromedial (AM) portal slightly proximal and 2 cm more medial than the AM portal.
Fig 3.
(A) Elevation/release of the MT ligament with Bankart elevator (right knee, viewing from AM portal). (B) FiberTak anchor drill guide (Arthrex) placed at the periphery of the MTP. (C) Deployed anchor with sutures exiting the accessory (acc) AM portal. Abbreviations: AM, anteromedial; MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau.
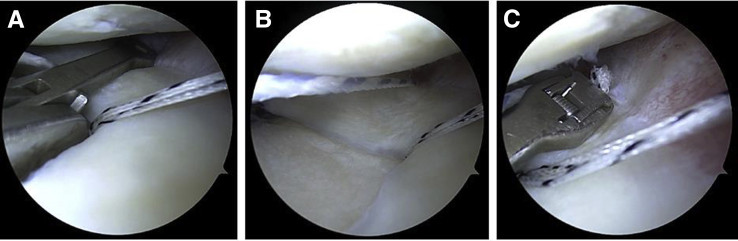
Medial Meniscus Centralization
Introduce the Knotless FiberTak curved drill guide (Arthrex, Naples, FL) through the accessory AM portal. Position the guide at the posteromedial aspect of the MM body just central to the peripheral rim of the tibial articular surface, and drill and deploy the FiberTak suture anchor (Fig 3). Retrieve only the white/blue repair FiberTak suture through the AL portal. Next, from the AL portal using a self-retrieving suture passer (Knee Scorpion; Arthrex), pass the white/blue repair suture through the meniscocapsular junction from inferior to superior, and back through the AL cannula. Use the Scorpion to pass a 0 FiberLink (Arthrex) suture through the meniscus in a mattress fashion and again retrieve that through the AL portal (Fig 4). Use this 0 FiberLink as a shuttle suture to then pass the white/blue repair suture back down and through the meniscocapsular junction in a mattress fashion (either vertical or horizontal). Shuttle the white/blue repair suture down to the anchor using the looped white/black shuttle suture from the anchor by pulling on the nonlooped black/white tape suture from the anchor. Finally, tension down the centralization suture to reduce the meniscus, using an arthroscopic knot pusher or a pusher-cutter device (Fig 5). The same steps are repeated 1 to 2 times, more anteriorly along the medial tibial rim.
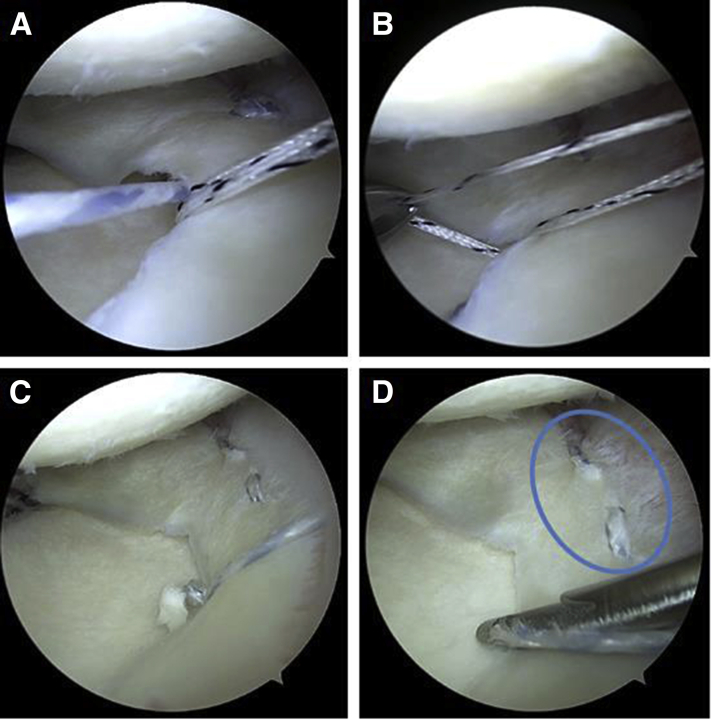
Fig 4.
(A) Knee Scorpion (Arthrex) from the anterolateral (AL) portal piercing the meniscocapsular junction to pass the FiberTak blue repair suture. (B) FiberTak suture retrieved through AL portal. (C) Knee Scorpion passing the 0 FiberLink (Arthrex) shuttle suture in mattress fashion anterior to FiberTak suture to allow for second passage of repair suture to create horizontal mattress.
Fig 5.
(A) FiberTak suture shuttled under the medial meniscus (MM) by the 0 FiberLink shuttle suture, and retrieved through the anterolateral (AL) portal. (B) Remaining 0 Fiberloop shuttle suture retrieved through AL portal. (C) FiberTak suture shuttled down to the anchor by pulling on the 0 Fiberloop shuttle suture through the accessory anteromedial (acc AM) portal. (D) FiberTak sutures tensioned down with arthroscopic knot pusher or pusher cutter (see position of sutures in meniscocapsular junction in the blue oval).
Alternatively, sutures can be passed with a Micro SutureLasso, Straight (Arthrex), again introduced through the accessory AM portal. Pass the Micro SutureLasso from the periphery of the meniscocapsular junction, down over the articular surface, and retrieve it. Shuttle the white/blue repair Fibertak suture with the use of the Micro SutureLasso, and then repeat the steps previously mentioned for tensioning down the suture.
Medial Meniscus Posterior Root Tear Preparation
To improve visualization of the MM posterior root footprint, a small resection of the medial tibial spine and a small reverse notchplasty can be performed. Using a 3.5-mm full-radius shaver (Stryker, San Jose, CA) and a double-sided rasp (Linvatec, ConMed, Largo, FL), debride the edges of the posterior root tear until bleeding occurs, in an effort to enhance healing. We debride devascularized tissue at the edges of the tear to promote vascular infiltration. Also, use of a curved arthroscopic scissor can be helpful to release the posterior capsular attachment of the root to improve overall mobility.
Medial Meniscus Posterior Root Suture Passage
Insert the Arthrex meniscus root repair tibial guide through the AM portal and hook the guide on the posterior aspect of the tibia, directly behind the root attachment site (Fig 6). Swivel the drill guide to the anteromedial face of the tibia. One can measure the distance from the posterior aspect of the tibial plateau to the anatomic footprint of the meniscal root, and adjust the guide to that distance for accurate drilling (Fig 5). Drill the 3.5-mm-diameter FlipCutter (Arthrex) pin through the tibia; it should exit at the anatomic footprint. Convert the FlipCutter to a 6.0-mm reamer, and retrodrill the tibia 10 mm. Advance the FlipCutter back into the joint, convert it back to a 3.5-mm-diameter pin, and remove it from the tibia.
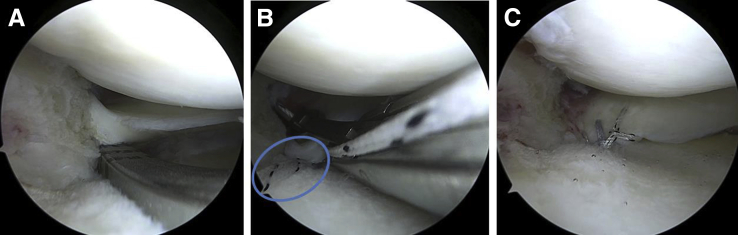
Fig 6.
(A) Root guide (Arthrex) via anteromedial (AM) portal in position at the anatomic footprint of the medial meniscus (MM) posterior root (viewing from anterolateral [AL] portal). (B) Cinch suture passage with self-retrieving suture passer. Note the looped passing suture (circled) that was previously brought through the tibial tunnel and out the AL portal for later use. (C) Three cinch sutures delivered through the tibial tunnel and tensioned down to the posterior root footprint.
Advance a no. 2 FiberStick shuttle suture in its red sheath (Arthrex) through the tibial tunnel and retrieve the shuttle suture through the AL portal. Through the AM portal, pass the loop end of a 0 FiberLink (Arthrex) through the meniscal root using a Knee Scorpion. Withdraw the suture from the portal and pass the free end through to loop to create a cinch-type suture. Repeat this step several millimeters lateral to the initial suture, using a 0 TigerLink (Arthrex) suture to aid in suture management. Shuttle these sutures back through the tibial tunnel with the FiberStick shuttle suture.
Fixation of Transtibial Posterior Root Sutures
Attain tibial fixation with a 4.75-mm Bio Composite SwiveLock anchor (Arthrex). One centimeter distal to the transosseous FlipCutter hole in the anteromedial tibial, create the pilot hole for the SwiveLock using a 4.5-mm stepped drill to a depth of 20 mm. Tap the tibial cortex using a 4.5-mm tap. Cycle the knee from 0° to 90° 10 times to remove creep from the system, and pass the free ends of the cinch sutures into a SwiveLock anchor. Confirm that the meniscal root is well reduced with the knee in 90° flexion with applied tension and advance the SwiveLock anchor into the reamed, tapped tibial hole. Fig 7 shows the final construct. Please see Video 1 for the full arthroscopic technique.
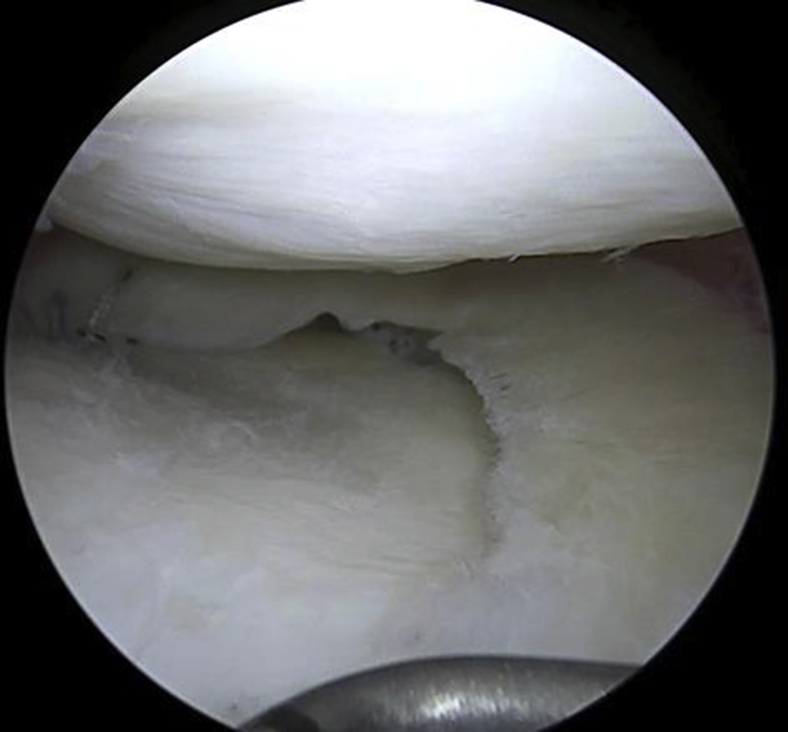
Fig 7.
Final construct of right knee medial meniscus (MM) centralization and root repair. Note the improved meniscal extrusion.
Postoperative Rehabilitation
Depending on concomitant injuries and surgery, such as anterior cruciate ligament (ACL) reconstruction, rehabilitation may differ from patient to patient. Typically, we use a complex meniscus protocol for the first 6 weeks, with toe-touch weightbearing only. During this time, the patient can perform quad sets and straight leg raises. For the first 4 weeks, range of motion is limited to 90°. After 4 weeks, range of motion progresses as tolerated. At 6 weeks, the patient transitions to a more typical ACL rehabilitation protocol. However, jogging and impact activities are delayed until 4 to 6 months instead of the typical 3 months.
Discussion
Medial meniscus posterior root tears result in a loss of hoop strain resistance and increased articular cartilage contact pressure within the medial compartment,3,4 leading to rapid progression of osteoarthritis within ≥1 year of injury.6 It is thus important to restore the anatomy and function of the medial meniscus in these cases. However, even with well-executed anatomic repair of the posterior root, persistent meniscus extrusion may exist postoperatively.10,14,15
There are multiple theories as to why extrusion persists. There may be adhesion of the preoperatively extruded meniscus and adjacent capsule to the medial tibial plateau, distal to the medial edge. This would be somewhat analogous to anterior labral periosteal sleeve avulsion (ALPSA) lesion in the shoulder. Alternatively, a degenerative torn edge may not be able to hold the MM in the anatomically reduced position.
The purpose of meniscus centralization is to reduce the risk of postoperative extrusion. Koga et al.18 reported good 2-year clinical and radiographic outcomes for the lateral meniscus and significantly reduced meniscus extrusion 3 months postoperatively on MRI that is maintained at 1 year postoperatively. The same group also previously described their centralization technique for the MM.16 In the current Technical Note, we present our preferred technique for augmentation of a MM posterior root tear with centralization of the medial meniscus. Although long-term, large group studies are lacking, the centralization procedure has the theoretical benefit of restoring meniscus function after anatomic root repair. There is a theoretical risk of decreasing knee motion, but this not been borne out in the literature or in our experience thus far. It is a technically demanding procedure, but with a methodical approach and avoidance of pitfalls, we have anecdotally seen good short-term results in our patients.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.A.S. reports other, American Orthopaedic Society for Sports Medicine, Journal of Knee Surgery, Spinal Simplicity; personal fees, Arthrex. A.J.K. reports grants, Aesculp/B.Braun, Arthritis Foundation, Ceterix, Histogenics; other American Journal of Sports Medicine; grants, personal fees and other, Arthrex, International Cartilage Repair Society, International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine, Minnesota Orthopedic Society; personal fees and other, Musculoskeletal Transplantation Foundation; personal fees, Vericel, Depuy, JRF Ortho. M.J.S. reports other, American Journal of Sports Medicine; personal fees and other, Arthrex; grants and other, Stryker; nonfinancial support, Gemini Medical LLC. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic centralization of the extruded medial meniscus. Begin with diagnostic arthroscopy. Create an accessory medial portal that is proximal and medial to the standard anteromedial portal, to allow for the correct angulation of instruments. Perform a release of the meniscotibial ligaments off of the periphery of the tibial plateau using a curved Bankart elevator. Introduce an Arthrex knotless Fibertak suture anchor through the accessory anteromedial portal and place the anchor just central to the peripheral rim of the tibial articular surface. Retrieve only the blue/white repair Fibertak suture through the anterolateral (AL) portal. With a self-retrieving suture passing device, pass the repair suture through the meniscocapsular junction from inferior to superior. Use the Scorpion to pass the black/white shuttle suture in a mattress fashion and again retrieve it through the AL portal. Use the shuttle suture to pass the repair suture back down and through the meniscocapsular junction in a mattress fashion. Shuttle the repair suture down to the anchor using the remaining black/white shuttle suture. Tension the centralization suture down with an arthroscopic knot pusher or with a pusher-cutter device. Repeat this process to create a total of 2 to 3 centralization sutures. Once the centralization is complete, move on to the transtibial root repair. Use the Arthrex root repair guide through the anteromedial (AM) portal, determine the distance of the anatomic footprint of the root to the posterior aspect of the tibial plateau (5, 7.5, or 10 mm) and set the guide accordingly. Drill through the anteromedial surface of the tibia, up to the root footprint. Shuttle a looped passing suture up with a Fiberstick. Prepare the bony surface with flipcutter or curette. With a knee Scorpion, pass 2 to 3 simple cinch sutures. Then use the looped shuttle suture to pull the cinch sutures down through the tibial tunnel and secure to the AM tibia with a SwiveLock anchor.
References
- 1.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hein C.N., Deperio J.G., Ehrensberger M.T., Marzo J.M. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18:189–192. doi: 10.1016/j.knee.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 4.Moatshe G., Chahla J., Slette E., Engebretsen L., Laprade R.F. Posterior meniscal root injuries. Acta Orthop. 2016;87:452–458. doi: 10.1080/17453674.2016.1202945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krych A.J., Reardon P.J., Johnson N.R. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25:383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 6.Krych A.J., Johnson N.R., Mohan R. Arthritis progression on serial MRIs following diagnosis of medial meniscal posterior horn root tear. J Knee Surg. 2018;31:698–704. doi: 10.1055/s-0037-1607038. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 8.Lee J.H., Lim Y.J., Kim K.B., Kim K.H., Song J.H. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: Radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 10.Moon H.K., Koh Y.G., Kim Y.C., Park Y.S., Jo S.B., Kwon S.K. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40:1138–1143. doi: 10.1177/0363546511435622. [DOI] [PubMed] [Google Scholar]
- 11.Okazaki Y., Furumatsu T., Shimamura Y. Time-dependent increase in medial meniscus extrusion after medial meniscus posterior root tear analyzed by using magnetic resonance imaging. Knee Surg Relat Res. 2019;31:120–125. doi: 10.5792/ksrr.18.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Achtnich A., Petersen W., Willinger L. Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc. 2018;26:2282–2288. doi: 10.1007/s00167-018-4885-7. [DOI] [PubMed] [Google Scholar]
- 13.Willinger L., Lang J.J., von Deimling C. Varus alignment increases medial meniscus extrusion and peak contact pressure: A biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2020;28:1092–1098. doi: 10.1007/s00167-019-05701-1. [DOI] [PubMed] [Google Scholar]
- 14.Furumatsu T., Kodama Y., Kamatsuki Y., Hino T., Okazaki Y., Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29:295–301. doi: 10.5792/ksrr.17.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaplan D.J., Alaia E.F., Dold A.P. Increased extrusion and ICRS grades at 2-year follow-up following transtibial medial meniscal root repair evaluated by MRI. Knee Surg Sports Traumatol Arthrosc. 2018;26:2826–2834. doi: 10.1007/s00167-017-4755-8. [DOI] [PubMed] [Google Scholar]
- 16.Koga H., Watanabe T., Horie M. Augmentation of the pullout repair of a medial meniscus posterior root tear by arthroscopic centralization. Arthrosc Tech. 2017;6:e1335–e1339. doi: 10.1016/j.eats.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koga H., Muneta T., Yagishita K. Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech. 2012;1:e209–e212. doi: 10.1016/j.eats.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koga H., Muneta T., Watanabe T. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32:2000–2008. doi: 10.1016/j.arthro.2016.01.052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic centralization of the extruded medial meniscus. Begin with diagnostic arthroscopy. Create an accessory medial portal that is proximal and medial to the standard anteromedial portal, to allow for the correct angulation of instruments. Perform a release of the meniscotibial ligaments off of the periphery of the tibial plateau using a curved Bankart elevator. Introduce an Arthrex knotless Fibertak suture anchor through the accessory anteromedial portal and place the anchor just central to the peripheral rim of the tibial articular surface. Retrieve only the blue/white repair Fibertak suture through the anterolateral (AL) portal. With a self-retrieving suture passing device, pass the repair suture through the meniscocapsular junction from inferior to superior. Use the Scorpion to pass the black/white shuttle suture in a mattress fashion and again retrieve it through the AL portal. Use the shuttle suture to pass the repair suture back down and through the meniscocapsular junction in a mattress fashion. Shuttle the repair suture down to the anchor using the remaining black/white shuttle suture. Tension the centralization suture down with an arthroscopic knot pusher or with a pusher-cutter device. Repeat this process to create a total of 2 to 3 centralization sutures. Once the centralization is complete, move on to the transtibial root repair. Use the Arthrex root repair guide through the anteromedial (AM) portal, determine the distance of the anatomic footprint of the root to the posterior aspect of the tibial plateau (5, 7.5, or 10 mm) and set the guide accordingly. Drill through the anteromedial surface of the tibia, up to the root footprint. Shuttle a looped passing suture up with a Fiberstick. Prepare the bony surface with flipcutter or curette. With a knee Scorpion, pass 2 to 3 simple cinch sutures. Then use the looped shuttle suture to pull the cinch sutures down through the tibial tunnel and secure to the AM tibia with a SwiveLock anchor.