Abstract
Surgical simulation offers a solution to the problems of reduced training time and surgical exposure by allowing trainees to develop surgical skills outside of the operating room in a safe, cost-effective environment. We developed a highly detailed, procedure-specific shoulder arthroscopy simulator using 3-dimesional printing with the aim of providing greater access to cost-effective simulation support to trainees.
Reduced working hours, reduced operating time,1,2 operating room costs—both time and equipment,3 and concerns regarding patient safety4 have all increased the pressure on both those learning and teaching. Surgical simulation offers a potential solution to many of these problems by allowing trainees to develop surgical skills outside of the operating room in a safe, cost-effective environment.5 Cadaveric models provide high-fidelity simulation1 and although transferability of operative skills has been demonstrated,6 they are expensive, time-consuming to prepare, and can be difficult to access.1 Virtual reality simulators do not enable more complex procedures to be rehearsed. “Bench-top” simulators, e.g., Alex II Shoulder Professor (Sawbones, Vason Island, WA), have been demonstrated to improve ability to perform arthroscopic Bankart repairs.7 Their versatility means that they sacrifice some anatomical accuracy, and they come at a cost. The Alex III Shoulder Professor is $1300, and replacement glenoid components are $30. Three-dimensional (3D) printing has been transformative in medicine and has been used for both surgical planning and printing of implants.8 The purpose of this study was to develop a low-cost, highly detailed, portable and reusable simulator that allows specific procedures to be performed.
Surgical Technique (With Video Illustration)
Development of the Simulator
For the purposes of development, the Simulator was designed to train one specific surgical procedure. Arthroscopic anterior stabilization was chosen, as this is relatively complex and is not represented by other models to any significant degree. A computed tomography scan of a normal left shoulder was processed using the Philips Intellispace PACS system (Philips, Amsterdam, Netherlands). The raw images were edited to leave only the glenoid and proximal humerus. The resultant data were exported in Dicom form to Autodesk Fusion 360 (Autodesk, San Raphael, CA). A 3D model of the humerus and glenoid was printed at 1:1 scale using a domestic Lulzbot Taz 5 3D printer (FAME 3D, Fargo, ND). Each component was made on a separate detachable base so that they could be replaced independently (Fig 1). A 3D box was printed that would house the inserts and simulated the volume and spacing of a normal shoulder (Fig 2). There were preplaced ports for the camera and the instruments to be inserted. An LED (light-emitting diodes) light source was placed in the roof of the box. A mold for the labrum was 3D printed and the labrum itself was manufactured from latex in the mold and glued onto the glenoid (Fig 3). These plans allow reliable, repeatable production of pieces for each simulation. The costs of the components are shown in Table 1.
Fig 1.
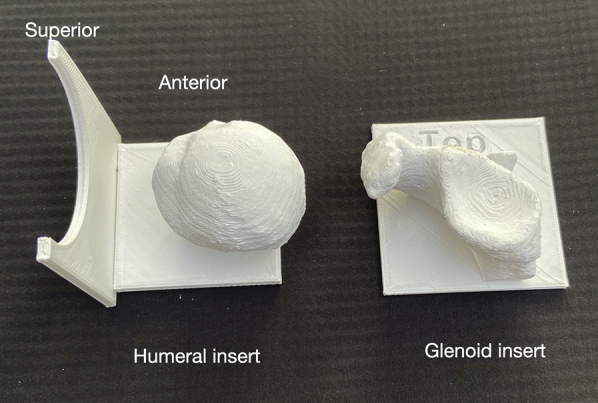
Three-dimensional printed glenoid and humeral inserts that slide into the box. Arrows on the inserts guide orientation
Fig 2.
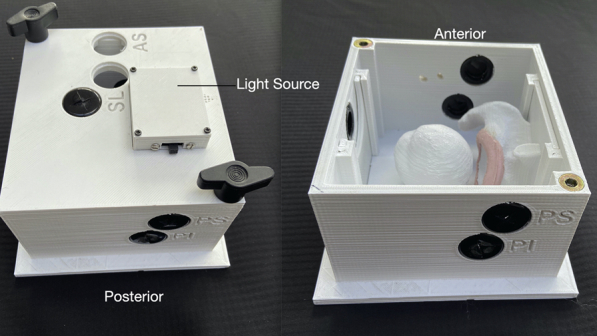
Three-dimensional printed box showing the portals with labels. The light source with switch can be seen on the closed model. The position of the inserts can be seen on the open model. (AS, anterosuperior; PI, posteroinferior; PS, posterosuperior; SL, superolateral.)
Fig 3.

Three-dimensional printed glenoid insert, molded glenoid, labrum, and composite product
Table 1.
Breakdown of Costs, USD($)
| Part | Construction | Cost |
|---|---|---|
| Simulation box/housing | Fused deposition modeling (3D printed) plastic | $55 |
| Glenoid | Fused deposition modeling (3D printed) plastic | $7 |
| Labrum | Fused deposition modeling (3D printed) elastoplastic | $12 |
| Humeral head | Fused deposition modeling (3D printed) plastic | $7 |
| Total: $81 | ||
| Consumables (Glenoid and labrum) | $19 |
3D, 3-dimesional.
A generic 0° USB camera (eBay, San Jose, CA) was attached to a laptop computer and generic camera software (AMCap, Noel Danjou Apps, www.noeld.com) used to view the output. To demonstrate the face validity of the Simulator, an arthroscopic anterior stabilization using a knotless suture/anchor system was used. This required all the steps in the procedure to be performed as would be undertaken in real surgery (Video 1). Total cost of the simulator was $81 and the consumables was $19.
Discussion
Simulation is an essential component of surgical education. The increased complexity of arthroscopic procedures requires increased time spent rehearsing and developing the skills, but there are very few commercially available simulators that will enable the trainee to rehearse specific procedures.
3D printing enables the rapid and cost-effective development of models, and this has been used to create a modular simulation of the shoulder with arthroscopic portals and a labrum for an anterior stabilization procedure.
Using the same technology, it would be possible to print components for almost any other shoulder procedure, e.g., a torn rotator cuff in any pattern to practice rotator cuff repair. These can then be made open access for training units or individuals to reproduce themselves. Using 3D printing and a modular system, the costs are kept to a minimum. The use of 3D printing to create this surgical simulator has a number of advantages but is not perfect. These are highlighted in Table 2. Surgical simulation has a vital role in surgical training. We have demonstrated that it is possible to produce a simulator with low setup and maintenance costs. Furthermore, ease of component manufacture allows for a variety of different procedures to be performed and practiced at minimal extra cost.
Table 2.
Advantages and Disadvantages
| Advantages |
| The simulator is inexpensive to manufacture |
| It is easy to assemble and use |
| Real instruments and implants can be used |
| The same procedure can be attempted using different implants |
| The simulator has high face validity and discriminates between novice and expert |
| Disadvantages |
| Requires 3D printer and printing skills |
| Development of a new model takes time and some 3D printing skills |
| The 0° USB endoscope is not representative of actual surgical practice |
3D, 3-dimensional.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Y.P. reports other from Arthrex, outside the submitted work. D.T. reports personal fees and other from Arthrex, outside the submitted work. In addition, he has a patent, ACJ TightRope, with royalties paid to Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic anterior stabilization using the Simbox and a knotless anchor/suture system.
References
- 1.Stirling E.R., Lewis T.L., Ferran N.A. Surgical skills simulation in trauma and orthopaedic training. J Orthop Surg Res. 2014;9:126. doi: 10.1186/s13018-014-0126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quillin R.C., III, Cortez A.R., Pritts T.A., Hanseman D.J., Edwards M.J., Davis B.R. Operative variability among residents has increased since implementation of the 80-hour workweek. J Am Coll Surg. 2016;222:1201–1210. doi: 10.1016/j.jamcollsurg.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Farnworth L.R., Lemay D.E., Wooldridge T. A comparison of operative times in arthroscopic ACL reconstruction between orthopaedic faculty and residents: the financial impact of orthopaedic surgical training in the operating room. Iowa Orthop J. 2001;21:31. [PMC free article] [PubMed] [Google Scholar]
- 4.Cannon W.D., Garrett W.E., Jr., Hunter R.E. Improving residency training in arthroscopic knee surgery with use of a virtual-reality simulator: a randomized blinded study. J Bone Joint Surg Am. 2014;96:1798–1806. doi: 10.2106/JBJS.N.00058. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher A.G., Ritter E.M., Champion H. Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg. 2005;241:364. doi: 10.1097/01.sla.0000151982.85062.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergeson R.K., Schwend R.M., DeLucia T., Silva S.R., Smith J.E., Avilucea F.R. How accurately do novice surgeons place thoracic pedicle screws with the free hand technique? Spine (Phila Pa 1976) 2008;33:E501–E507. doi: 10.1097/BRS.0b013e31817b61af. [DOI] [PubMed] [Google Scholar]
- 7.Howells N.R., Auplish S., Hand G.C., Gill H.S., Carr A.J., Rees J.L. Retention of arthroscopic shoulder skills learned with use of a simulator: Demonstration of a learning curve and loss of performance level after a time delay. J Bone Joint Surg Am. 2009;91:1207–1213. doi: 10.2106/JBJS.H.00509. [DOI] [PubMed] [Google Scholar]
- 8.Tack P., Victor J., Gemmel P., Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016;15:115. doi: 10.1186/s12938-016-0236-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic anterior stabilization using the Simbox and a knotless anchor/suture system.


