Abstract
Anterior cruciate ligament intra-articular reconstruction may require extra-articular reinforcement in certain situations. As knee lateral region anatomical and biomechanical knowledge has increased with new research, it has been reported that the iliotibial band is important in the anterolateral stabilization of the knee. Possible indications for a “more anatomical” extra-articular tenodesis focusing on capsulo-osseous layer tensioning and distal Kaplan fibers reconstruction are reported, surgical approach details are described, and scientific data that gives support for this procedure are discussed.
Lateral extra-articular tenodesis (LET) was used in the past for the surgical treatment of anterior cruciate ligament (ACL) instability, and postoperatively the knee was immobilized in flexion and the tibia in external rotation. This condition could cause stiffness and development of degenerative changes in the knee lateral compartment. With the advent of arthroscopy, a return to intra-articular ACL reconstruction occurred.
However, a small percentage of patients have reported continued instability despite ACL intra-articular reconstruction.1,2 There is a current trend that anterolateral soft-tissue extra-articular reconstruction may be used complementary to ACL intra-articular reconstruction in select patients.
The contribution of the Kaplan's fibers to knee pivot shift was reported by Jakob et al. in 1981.3 The authors also stated that the lateral capsular ligament might secondarily stretch in an ACL deficient knee, increasing a chronic anterolateral instability. Godin et al.4 identified a distinct capsulo-osseous layer of the distal iliotibial band (ITB) that was intimately associated with the knee lateral capsule. They reported that the Kaplan fibers had a strong attachment to the distal femur and so should play a role in rotational knee stability. More recently, Berthold et al.5 recommended that the integrity of Kaplan fibers should be routinely reviewed on magnetic resonance imaging because of its possible clinical repercussions. In another perspective, Amis6 showed biomechanical evidence suggesting that tenodesis or reconstructive surgery should be done to restore the restraint supplied by the ITB, rather than that provided by the anterolateral ligament, and Smith et al.,7 in a biomechanical study, reported that pivot shift control is better performed by the deep ITB rather than by anterolateral ligament. We described a LET surgical technique performed by capsulo-osseous layer retensioning and distal Kaplan fibers reconstruction, aiming to reproduce the original anatomy more accurately.
Surgical Technique (With Video Illustration)
Indications
Currently, the indications for an extra-articular procedure for patients who will undergo an ACL intra-articular reconstruction are variable, although some of them are common among the authors' opinion. Sonnery-Cottet et al.8 recommend adding extra-articular surgery for patients participating in sports involving rotational movements, high-level sports, pivot shift test equal or more than 2+, chronic ACL injuries, ACL revision, notch sign of lateral femoral condyle greater than 2 mm, in cases with a Segond fracture, and for patients younger than 20 years. Geeslin et al.9 advocated it for patients with biological or physiological impairment (ACL allograft reconstruction, ACL revision, patients with knee hyperextension, patients with increased tibial plateau slope tilt in the sagittal plane) and for those at high risk of new ACL injury (high-level sports, where there are cutting and pivoting movements).
Knee hyperextension and greater preoperative pivot shift under anesthesia,10 persistence of a grade ≥2 pivot shift after revision ACL reconstruction,11 patients presenting more than 12 months after injury for surgery,12 and residual pivot shift at the time of surgery13 also are considered suggestions for extra-articular reinforcement. More recently, Getgood et al.14 published their indications for extra-articular complementary surgeries—ACL revision, high-grade pivot shift, generalized ligament laxity, knee hyperextension, and for young athlete participants in pivoting sports—and Redler et al.15 showed that revision ACL reconstruction plus LET provides enhancement in clinical and radiologic results at mid-to long-term follow-up.
Procedure
With the patient anesthetized and lying supine, arthroscopic anatomic single-bundle ACL reconstruction is performed initially. Hamstring graft is fixed in the femur with an ENDOBUTTON (Smith & Nephew, Memphis, TN). The sutures passing through the ENDOBUTTON (Smith & Nephew) and skin are maintained to help locate the graft femoral exit. An incision of about 12 cm in length is made in the skin and through the subcutaneous tissues of the distal and lateral thigh, over the location of the middle portion of the ITB, slightly curved toward the Gerdy tubercle.
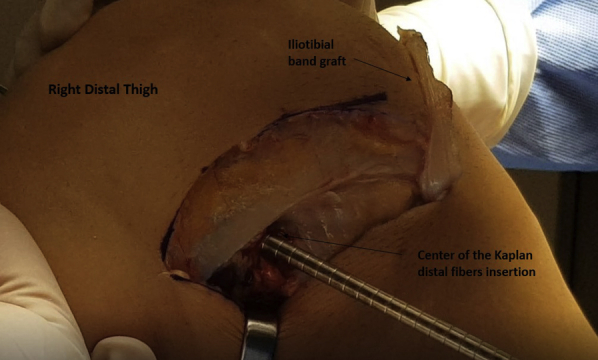
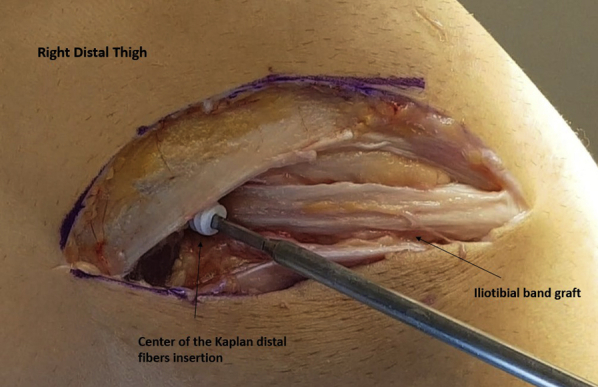
After hemostasis is obtained, the skin flaps are retracted, and delicate dissection is performed to identify the posterior portion of the ITB. An incision of about 10 cm of length is made 1 cm above the ITB posterior edge, from distal to proximal, up to its Gerdy tubercle insertion. Another similar parallel incision is performed on the ITB, 1 cm anterior to the first one (Fig 1). Then a vertical incision on the most proximal region of the other cuts is performed to release a 10-cm × 1-cm ITB strip, maintaining its tibial insertion (Fig 2). ETHIBOND (Ethicon, Somerville, NJ) #2 sutures are passed through the free edge of the ITB strip (Fig 3).
Fig 1.
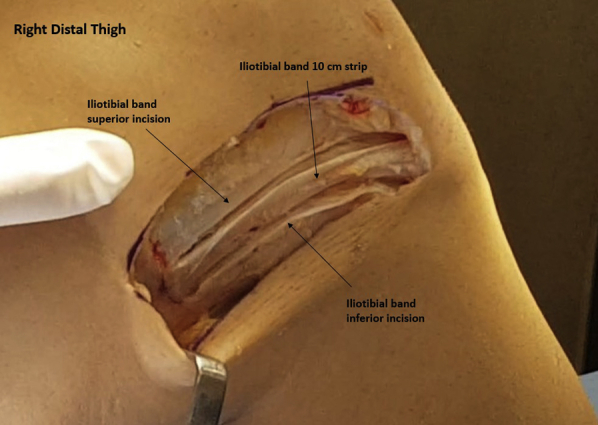
Lateral view of a right knee demonstrating the 2 parallel incisions to create a strip of iliotibial band of about 10 cm of length for the graft.
Fig 2.
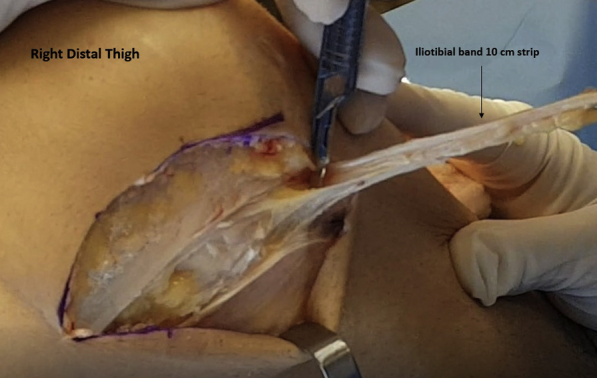
A 10-cm × 1-cm iliotibial band strip being dissected, keeping its tibial insertion at the Gerdy tubercle (lateral view, right knee).
Fig 3.
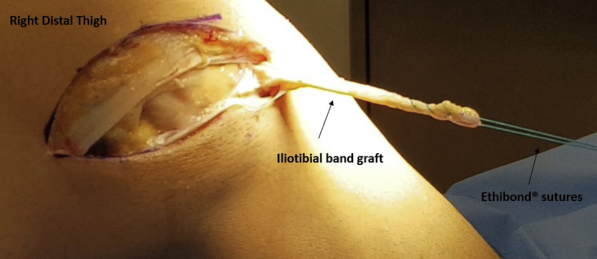
ETHIBOND (Ethicon, Somerville, NJ) sutures passed through the iliotibial band graft to serve as a passing stitch (lateral view, right knee).
The ITB is now retracted anteriorly to expose the lateral and distal femur. By blunt dissection, a bony prominence on the supracondylar flare of the distal femur is located, about 31.4 mm proximal to the lateral epicondyle.4 It corresponds to the distal Kaplan fibers attachment. Care must be taken to avoid injury to the superior lateral genicular artery because it passes distal and posterior to the distal Kaplan fibers femoral insertion.
A 2.4-mm eyelet tipped Kirschner wire is drilled in the center of bony prominence above described, crossing the lateral femoral cortex and exiting in the anteromedial thigh (Fig 4). A cannulated 7.0-mm drill is used to overream a tunnel of 35 mm in length (Fig 5), and the ETHIBOND (Ethicon) sutures are passed through the Kirschner wire holes. Next, the wire is pulled out, bringing the sutures outside the anteromedial thigh. The 10-cm × 1-cm ITB strip is passed over the fibular collateral ligament (FCL) and driven inside the tunnel by pulling the passing sutures.
Fig 4.
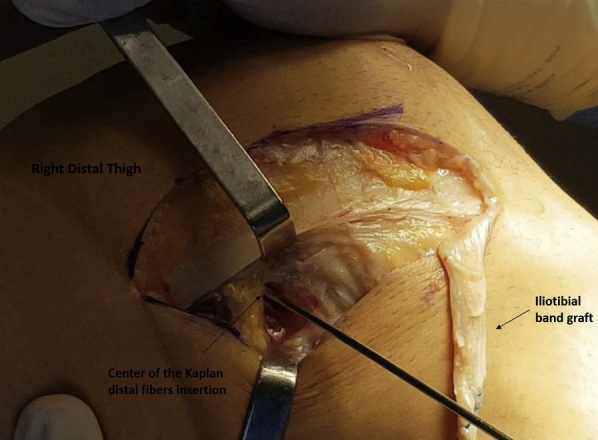
An eyelet tipped pin passed anteromedially across the femur through the center of the Kaplan distal fibers insertion (lateral view, right knee).
Fig 5.
A cannulated drill is placed over the guide pin to overream the reconstruction graft tunnel to a depth of 35 mm (lateral view, right knee).
The knee is kept in 70° of flexion and neutral rotation. A guidewire is introduced in the femoral tunnel, over the ITB strip, and it is fixed to the femur with a 7 × 25-mm absorbable interference screw (Fig 6). A curved Kelly forceps is used to press the medial side of the thigh where the ETHIBOND (Ethicon) sutures exit is located, and they are cut with the tip of a scalpel blade. The guidewire is removed, the ITB defect is closed with VICRYL (Ethicon) #2 (Fig 7), and the wound is closed with Nylon (Ethicon) #4 and covered with a bandage. No drain is used. Table 1 shows this technique's pearls and pitfalls, and the surgical approach can be seen in Video 1.
Fig 6.
Reconstruction graft fixation with a 7 × 25-mm absorbable interference screw (lateral view, right knee).
Fig 7.
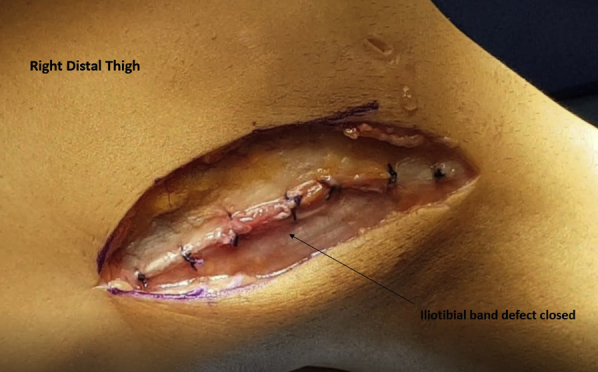
Photograph of the iliotibial band graft defect closed (lateral view, right knee).
Table 1.
Technique Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| An incision of about 10 cm of length should be performed 1 cm above the posterior edge of the ITB. | Difficulty to close ITB graft defect. |
| The 10 × 1-cm ITB strip should be carefully released until its tibial insertion. | Inadvertent ITB strip sectioning. |
| Distal Kaplan fibers femoral attachment site should be located by careful blunt dissection. | Superior lateral genicular artery injury and consequent bleeding, possible hematoma formation, facilitating infection occurrence. |
| ITB strip is passed over the FCL. | Nonanatomical reconstruction. |
| The ITB strip should be fixed to the femur with the knee at 70° of flexion and neutral rotation. | Joint overconstrained, lateral patellar tilt and patellofemoral contact pressures alterations, graft overtension. |
FCL, fibular collateral ligament; ITB, iliotibial band.
Postoperative Care
The patient is discharged the day after the surgery, and recommendations include immediate weight-bearing with a pair of crutches, straight leg raises, isometric contraction of the quadriceps, and knee flexion exercises. Crutches are discontinued after 7 days, when the patient is referred to physiotherapy, which follows the same regimen as the one performed for isolated ACL reconstruction.
Discussion
Information obtained from scientific studies may help to choose the type of extra-articular surgery to be performed. The ACL is the primary restraint to anterior tibial translation, but as this ligament is centrally located, it has a very small moment arm to control internal tibial rotation, which is mainly restricted by the ITB. In the intact knee, internal rotation laxity increases with joint flexion, and soft-tissue injuries may increase this laxity.5 When there is an injury to the ACL and anterolateral complex structures, an ACL reconstruction alone may result in a residual abnormal rotational laxity of the tibiofemoral joint.16
Terry et al.17 reported that lesions of the iliotibial tract anatomical components were confirmed in 76 (93%) of the knees of 82 patients with acute ACL injury. The deep layer was damaged in 84% of cases and the capsulo-osseous layer in 71% of patients. ITB injuries correlated significantly with the grade of the pivot-shift, while on the contrary, ACL lesions did not. =17
The distal Kaplan fibers and lateral intermuscular septum connect ITB to the lateral aspect of the femur.18 The ITB is the primary restraint to tibial internal rotation when their superficial and deep layers were included together and responded to 74% of the total resistance to internal rotation with the knee at 60° of flexion.19 According to Rahnemai-Azar, et al.20 a 10-mm wide strip of the ITB was 50% stronger than a 20-mm wide area of the anterolateral joint capsule. The aforementioned data provide support for using a 10-mm ITB wide strip for Kaplan fiber surgical reconstruction and a lateral extra-articular tenodesis in conjunction with an ACL intra-articular reconstruction.
Our depicted technique uses a 10-mm wide ITB graft strip, which is fixed by an interference screw in a tunnel created at the distal osseous insertion of the Kaplan fibers. The surgical approach usually allows viewing an anatomical ACL reconstruction's femoral tunnel cortex exit, which may avoid tunnel convergence. This is similar to what happens when MacIntosh technique is used for a LET.21 If the tunnel exit is not visible, it is advisable to drill the LET's tunnel in at 20° axial/20° coronal angulation to avoid tunnels collision.22
Regarding the passage of the ITB band over or under the FCL, our technique suggests that it should be passed over this ligament because this can replicate the normal anatomy, that is, the capsule-osseous layer passes over the FCL and not underneath. However, Spencer et al.23 supported that passing the graft deep to the lateral collateral ligament when performing an LET because it would be the most efficient form of reconstruction.
Inderhaug et al.16 reported that graft passage under the FCL in the Lemaire LET procedure significantly resulted in knee overconstraint, which means a tibial internal rotation and anterior translation reduction compared with an uninjured knee.9 By following an alternative pathway, when the graft was passed deep the FCL, it did not occur.16
The passage of the graft under the FCL also has been described by other authors, fixing it by a Richards staple 2 cm proximal and slightly posterior to the native FCL femoral insertion,24 at Kaplan's fibers distal femoral insertion,25 or just anterior to the distal Kaplan fiber attachment.26 Nevertheless, a graft passed under the FCL is nonanatomical.27
For graft fixation, one surgical team's member holds the knee flexed at 70°, because this degree is the best one for LET graft fixation,7 and in neutral position, where only limited changes in lateral patellar tilt and patellofemoral contact pressures were verified,16 another one applies mild to moderate manual traction on the graft's ETHIBOND (Ethicon) sutures to avoid overconstraining the joint, while the surgeon advances the screw into the tunnel for graft fixation. However, Noyes et al. have found that low-tension ITB tenodesis may not affect the pivot shift and recommended appropriate tension to avoid overconstrain internal tibial rotation.28
We observed that graft relaxes during leg external rotation and is tensioned in internal rotation, therefore acting to prevent anterolateral rotation instability. Bone fixation of the graft with an interference screw allows for early mobilization to avoid joint stiffness.
The described technique has some limitations: it requires an additional skin incision to perform the capsulo-osseous layer retensioning and distal Kaplan fibers reconstruction, there is the possibility of the confluence between the tunnels to fix the ITB strip and the one for the ACL reconstruction and besides this, adding a LET results in small increase in pain, slight reduction in quadriceps strength, and diminished subjective functional recovery up to 6 months after the surgery.26
In contrast, this technique may allow proper ITB retensioning while creating a new ITB femoral insertion similar to the distal Kaplan fibers and may be an option for an anatomically positioned LET.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: R.F.L. reports grants and personal fees from Arthrex, International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine, Knee Surgery, Sports Traumatology, Arthroscopy; grants and personal from fees from Ossur; and grants and personal fees from Smith & Nephew, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Capsulo-osseous layer retensioning and distal Kaplan fibers surgical reconstruction.
References
- 1.Freedman K.B., D'Amato M.J., Nedeff D.D., Kaz A., Bach B.R., Jr. Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 2.Ardern C.L., Webster K.E., Taylor N.F., Feller J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 3.Jakob R.P., Hassler H., Staeubli H.U. Observations on rotatory instability of the lateral compartment of the knee. Experimental studies on the functional anatomy and the pathomechanism of the true and the reversed pivot shift sign. Acta Orthop Scand Suppl. 1981;191:1–32. doi: 10.3109/ort.1981.52.suppl-191.01. [DOI] [PubMed] [Google Scholar]
- 4.Godin J.A., Chahla J., Moatshe G. A comprehensive reanalysis of the distal iliotibial band: Quantitative anatomy, radiographic markers, and biomechanical properties. Am J Sports Med. 2017;45:2595–2603. doi: 10.1177/0363546517707961. [DOI] [PubMed] [Google Scholar]
- 5.Berthold D.P., Willinger L., Muench L.N. Visualization of proximal and distal Kaplan fibers using 3-dimensional magnetic resonance imaging and anatomic dissection. Am J Sports Med. 2020;48:1929–1936. doi: 10.1177/0363546520919986. [DOI] [PubMed] [Google Scholar]
- 6.Amis A.A. Anterolateral knee biomechanics. Knee Surg Sports Traumatol Arthrosc. 2017;25:1015–1023. doi: 10.1007/s00167-017-4494-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith P.A., Thomas D.M., Pomajzl R.J., Bley J.A., Pfeiffer F.M., Cook J.L. A biomechanical study of the role of the anterolateral ligament and the deep iliotibial band for control of a simulated pivot shift with comparison of minimally invasive extra-articular anterolateral tendon graft reconstruction versus modified Lemaire reconstruction after anterior cruciate ligament reconstruction. Arthroscopy. 2019;35:1473–1483. doi: 10.1016/j.arthro.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 8.Sonnery-Cottet B., Daggett M., Helito C.P., Fayard J.M., Thaunat M. Combined anterior cruciate ligament and anterolateral ligament reconstruction. Arthrosc Tech. 2016;5:e1253–e1259. doi: 10.1016/j.eats.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geeslin A.G., Moatshe G., Chahla J. Anterolateral knee extra-articular stabilizers: A robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46:607–616. doi: 10.1177/0363546517745268. [DOI] [PubMed] [Google Scholar]
- 10.Ueki H., Nakagawa Y., Ohara T. Risk factors for residual pivot shift after anterior cruciate ligament reconstruction: Data from the MAKS group. Knee Surg Sports Traumatol Arthrosc. 2018;26:3724–3730. doi: 10.1007/s00167-018-5005-4. [DOI] [PubMed] [Google Scholar]
- 11.Porter M.D., Shadbolt B., Pomroy S. The augmentation of revision anterior cruciate ligament reconstruction with modified iliotibial band tenodesis to correct the pivot shift: A computer navigation study. Am J Sports Med. 2018;46:839–845. doi: 10.1177/0363546517750123. [DOI] [PubMed] [Google Scholar]
- 12.Helito C.P., Camargo D.B., Sobrado M.F. Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26:3652–3659. doi: 10.1007/s00167-018-4934-2. [DOI] [PubMed] [Google Scholar]
- 13.Ueki H., Katagiri H., Otabe K. Contribution of additional anterolateral structure augmentation to controlling pivot shift in anterior cruciate 0ligament reconstruction. Am J Sports Med. 2019;47:2093–2101. doi: 10.1177/0363546519854101. [DOI] [PubMed] [Google Scholar]
- 14.Getgood A., Brown C., Lording T. ALC Consensus group. The anterolateral complex of the knee: Results from the International ALC Consensus group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019;27:166–176. doi: 10.1007/s00167-018-5072-6. [DOI] [PubMed] [Google Scholar]
- 15.Redler A., Iorio R., Monaco E. Revision anterior cruciate ligament reconstruction with hamstrings and extra-articular tenodesis: A mid- to long-term clinical and radiological study. Arthroscopy. 2018;34:3204–3213. doi: 10.1016/j.arthro.2018.05.045. [DOI] [PubMed] [Google Scholar]
- 16.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Effect of anterolateral complex sectioning and tenodesis on patellar kinematics and patellofemoral joint contact pressures. Am J Sports Med. 2018;46:2922–2928. doi: 10.1177/0363546518790248. [DOI] [PubMed] [Google Scholar]
- 17.Terry G.C., Norwood L.A., Hughston J.C., Caldwell K.M. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med. 1993;21:55–60. doi: 10.1177/036354659302100110. [DOI] [PubMed] [Google Scholar]
- 18.Terry G.C., Hughston J.C., Norwood L.A. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39–45. doi: 10.1177/036354658601400108. [DOI] [PubMed] [Google Scholar]
- 19.Kittl C., El-Daou H., Athwal K.K. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee: Response. Am J Sports Med. 2016;44:NP15–NP18. doi: 10.1177/0363546516638070. [DOI] [PubMed] [Google Scholar]
- 20.Rahnemai-Azar A.A., Miller R.M., Guenther D. Structural properties of the anterolateral capsule and iliotibial band of the knee. Am J Sports Med. 2016;44:892–897. doi: 10.1177/0363546515623500. [DOI] [PubMed] [Google Scholar]
- 21.Jaecker V., Ibe P., Endler C.H., Pfeiffer T.R., Herbort M., Shafizadeh S. High risk of tunnel convergence in combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis. Am J Sports Med. 2019;47:2110–2115. doi: 10.1177/0363546519854220. [DOI] [PubMed] [Google Scholar]
- 22.Gali J.C., Bernardes Ade P., dos Santos L.C., Ferreira T.C., Almagro M.A., da Silva P.A. Tunnel collision during simultaneous anterior cruciate ligament and posterolateral corner reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:195–200. doi: 10.1007/s00167-014-3363-0. [DOI] [PubMed] [Google Scholar]
- 23.Spencer L., Burkhart T.A., Tran M.N. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:2189–2197. doi: 10.1177/0363546515589166. [DOI] [PubMed] [Google Scholar]
- 24.Kwapisz A., Mollison S., McRae S., MacDonald P. Lateral extra-articular tenodesis with proximal staple fixation. Arthrosc Tech. 2019;8:e821–e825. doi: 10.1016/j.eats.2019.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernholt D.L., Kennedy M.I., Crawford M.D., DePhillipo N.N., LaPrade R.F. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis. Arthrosc Tech. 2019;8:e855–e859. doi: 10.1016/j.eats.2019.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Getgood A., Hewison C., Bryant D. No difference in functional outcomes when lateral extra-articular tenodesis is added to anterior cruciate ligament reconstruction in young active patients: The Stability Study. Arthroscopy. 2020;36:1690–1701. doi: 10.1016/j.arthro.2020.02.015. [DOI] [PubMed] [Google Scholar]
- 27.Hewison C.E., Tran M.N., Kaniki N., Remtulla A., Bryant D., Getgood A.M. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: A systematic review of the literature. Arthroscopy. 2015;31:2022–2034. doi: 10.1016/j.arthro.2015.04.089. [DOI] [PubMed] [Google Scholar]
- 28.Noyes F.R., Huser L.E., West J., Jurgensmeier D., Walsh J., Levy M.S. Two different knee rotational instabilities occur with anterior cruciate ligament and anterolateral ligament injuries: A robotic study on anterior cruciate ligament and extra-articular reconstructions in restoring rotational stability. Arthroscopy. 2018;34:2683–2695. doi: 10.1016/j.arthro.2018.04.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Capsulo-osseous layer retensioning and distal Kaplan fibers surgical reconstruction.


