Abstract
Most patellar dislocations are associated with disruption of the proximal medial patellar restraints (PMPRs). The PMPRs comprise the medial patellofemoral ligament (MPFL) and medial quadriceps tendon–femoral ligament (MQTFL). Although isolated MPFL reconstruction is the most frequently performed procedure for the surgical management of recurrent dislocation, recent studies have shown that the MQTFL has a synergistic role with the MPFL in resisting lateral patellar displacement close to full extension. It has therefore been suggested that surgical techniques that gain the benefits of both proximal and distal PMPR biomechanical behavior may be best. This article describes an established technique for combined MPFL and MQTFL reconstruction using semitendinosus autograft.
Most patellar dislocations are associated with disruption of the proximal medial patellar restraints (PMPRs).1,2 The PMPRs comprise the medial patellofemoral ligament (MPFL) and medial quadriceps tendon–femoral ligament (MQTFL).2 The MPFL is widely recognized as the primary restraint to lateral patellar translation, and the literature has predominantly focused on its isolated reconstruction.3 However, recent studies have shown that the MQTFL also has an important biomechanical role.3,4
In a cadaveric study, Spang et al.4 reported that isolated MQTFL reconstruction more closely restored the native state than isolated MPFL reconstruction with respect to resistance to lateral patellar translation testing. Furthermore, although Christian et al.3 confirmed that the MPFL was the primary restraint to lateral translation between 10° and 90° of knee flexion, they showed that close to full extension (<10°), the MPFL does not make a significantly greater contribution to restraining lateral translation than the MQTFL and both structures appear important. As a result, in a recent Arthroscopy editorial commentary, Fulkerson5 suggested that reconstructions to the midpoint of both the MPFL and MQTFL are probably optimal, given their different functions, combining the benefits of each. This article describes an established technique, used at Hospital Madre Teresa, Belo Horizonte, Brazil, since 2012, for combined MPFL and MQTFL reconstruction using semitendinosus autograft.
Surgical Technique
Patient Setup
The surgical technique is presented in Video 1. The patient is placed supine on the operating table in the standard arthroscopy position with a lateral post at the level of a padded tourniquet, using a foot roll to keep the knee flexed to 90° but allowing free range of motion during combined MPFL and MQTFL reconstruction. The landmarks for the surgical incisions are shown in Fig 1.
Fig 1.

Medial aspect of patient’s right knee. The patient is positioned supine with a padded tourniquet placed on the proximal right thigh. A surgical marking pen has been used to indicate the locations of the incisions that will follow: hamstring harvest 1.5 cm medial and distal to the anterior tibial tuberosity (blue star), at the medial proximal border of the patella (yellow star), and at the medial epicondyle of the femur (red star).
Graft Choice
Our preferred graft choice is ipsilateral semitendinosus tendon autograft. This is harvested in a standard manner, using a tendon stripper, via a 2-cm vertical skin incision, placed 1.5 cm medial to the tibial tuberosity (Fig 2).
Fig 2.

Anterior aspect of patient’s right knee. The semitendinosus tendon is harvested with an open tendon stripper via the incision pre-marked in Fig 1 (blue star). The tendon is carefully dissected and prepared by removing muscle tissue and whipstitching both ends.
Patellar and Quadriceps Preparation Including Graft Passage
A 3-cm incision is placed at the medial border of the proximal third of the patella. A bone tunnel is created at the transition between the upper and middle thirds of the medial border of the patella (approximately the midpoint of the patellar insertion of the MPFL). This is performed by drilling 2 interconnecting sockets of 3.5 to 4.5 mm, according to graft diameter. The first socket is drilled on the anterior surface of the patella 1 cm from its medial border. The second socket is created in the mid-axial plane on the medial side of the patella, joining the anterior tunnel at a 90° angle (Fig 3).
Fig 3.
Anterior aspect of right knee. (A) Retraction of the skin edges of the incision made over the proximal third of the medial border of the patella allows visualization of the bone tunnel that has been created at the junction between the upper (blue star) and middle (yellow star) thirds of the medial border of the patella (approximately the midpoint of the patellar insertion of the medial patellofemoral ligament). This tunnel was created by drilling 2 interconnecting sockets. The first socket was drilled on the anterior surface of the patella 1 cm from its medial border. The second socket was created in the mid-axial plane on the medial side of the patella, joining the anterior tunnel at a 90° angle. (B) Drill bits are positioned to show the trajectory of the sockets.
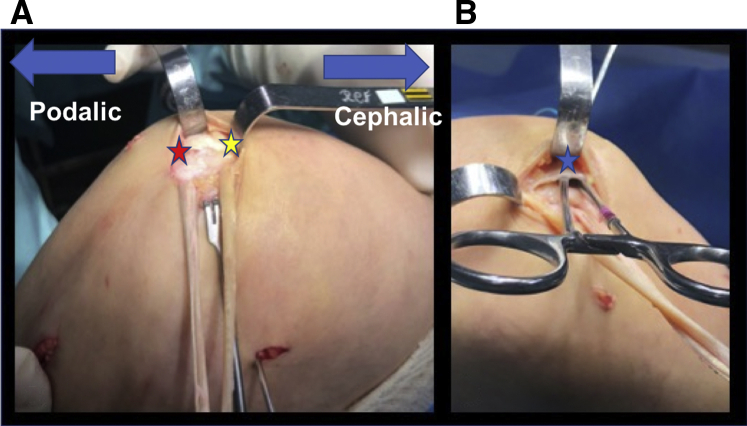
A soft-tissue tunnel is created in the medial and distal third of the quadriceps tendon with a Mixter right-angle forceps. This tunnel is placed 1.5 cm proximal to the superior pole of the patella, close to the midpoint of the MQTFL insertion.6 One end of the graft is passed into the soft-tissue tunnel created in the quadriceps tendon. The other end of the graft is introduced into the patellar tunnel by pulling downward from anterior to medial (Fig 4).
Fig 4.
Right knee. (A) The medial aspect of the knee is shown. The semitendinosus graft has been passed into both the patellar tunnel (red star) and the tunnel created in the distal quadriceps tendon (yellow star). The 2 free ends have then been sutured together. (B) The lateral aspect of the knee is shown to observe the creation of a tunnel deep to the vastus medialis muscle (blue star), between the second and third layers of the retinaculum, in which the graft will pass from the patella to the medial epicondylar incision.
Femoral Attachment
A 2-cm skin incision is made between the medial epicondyle and the adductor tubercle (Fig 5). For femoral tunnel positioning, a true lateral fluoroscopic image of the knee is obtained, aiming for perfect overlapping of the posterior femoral condyles. Under fluoroscopic visualization, the tip of the drill guide is positioned over the Schöttle point6 and an eyelet guidewire is inserted (Fig 6). A femoral tunnel of 7 mm is created by overdrilling the wire. The tunnel is typically drilled to a depth of 5 cm, but the depth is increased if required to avoid bottoming out of the graft.
Fig 5.

Medial aspect of knee. A 2-cm skin incision has been made over the medial epicondyle (blue star). The medial epicondyle and adductor tubercle are palpated, and a guidewire is positioned slightly posterior to the midpoint of these 2 landmarks.
Fig 6.

A true lateral fluoroscopic image of the knee is used to ensure that the tip of the guidewire is located at the Schöttle point prior to drilling.
Equal tension is applied to both ends of the graft, and they are whipstitched together with a Krackow technique using a No. 2 high-strength suture (Hi-Fi; ConMed, Largo, FL). The graft is passed under the vastus medialis muscle, between the second and third layers of the retinaculum, and then to the medial epicondylar region. A passing suture is placed in the eyelet guidewire and used to pull the graft into the knee. With the knee flexed to 60° and the patella in a central position on the trochlea, slack is removed from the graft, and the graft is fixed in the femoral tunnel with a 7 × 25–mm soft-tissue interference screw (Arthrex, Naples, FL) (Fig 7). Normalized patellar tracking and a hard endpoint to the MPFL reconstruction are confirmed prior to terminating the procedure. Advantages, risks, and limitations of the procedure are listed in Table 1, and pearls and pitfalls are shown in Table 2.
Fig 7.
Right knee. (A) The knee is flexed to 60° to centralize the patella in the trochlea; slack is removed from the graft. (B) The graft is fixed in the femoral tunnel with a 7 × 25–mm soft-tissue interference screw (Arthrex).
Table 1.
Advantages, Risks, and Limitations of Combined Anatomic Medial Patellofemoral Complex Reconstruction
| Advantages |
| The technique allows the reconstruction of both the MPFL and MQTFL, taking advantage of the different biomechanical roles of each. |
| The technique can be used concomitantly with other bony procedures (e.g., trochleoplasty or anterior tibial tuberosity realignment). |
| Risks and limitations |
| There is inherent residual pain resulting from harvesting the semitendinosus tendon. |
| Capsular breach can result from improper identification of the subvastus space in the second layer or the intratendinous plane (for the MQTFL part of the procedure), each of which can result in an incorrect graft position. |
| There is a risk of patellar fracture. |
| There is a potential risk of anterior knee pain resulting from passing the MQTFL graft through the quadriceps tendon. |
MPFL, medial patellofemoral ligament; MQTFL, medial quadriceps tendon–femoral ligament.
Table 2.
Pearls and Pitfalls of Combined Anatomic Medial Patellofemoral Complex Reconstruction
| Pearls |
| In the proximal two-thirds of the patella, the surgeon should drill 2 convergent holes with the minimum diameter needed to pass the graft. |
| A cortical bone bridge of 10 mm should be left between the tunnels made in the patella to minimize the risk of fracture. |
| The graft should always be passed into the patellar tunnel by pulling downward from anterior to medial to avoid stress on the tunnel’s roof (anterior surface of the patella). |
| The graft should be passed through the interval between layers 2 and 3 of the medial retinaculum toward the area of the medial femoral origin. |
| Pitfalls |
| Failure to recognize and correct other major causal factors of patellar maltracking must be avoided. |
| Nonanatomic tunnel or fixation placement, related to an inadequate understanding of the anatomy or inaccurate radiographic localization, must be avoided. |
| During preparation of the 2 patellar tunnels or during passage of an oversized tendon graft through a tight patellar tunnel, the bone bridge overlying the patellar tunnel is at risk of fracture. |
Postoperative Care
Postoperatively, patients are allowed to immediately start active knee motion as tolerated. Partial weight bearing is maintained until good pain control and good quadriceps and gluteus muscle activation are achieved. After 4 to 6 weeks, full range of motion and full weight bearing are allowed as tolerated. Rehabilitation is then focused on further quadriceps muscle activation and strengthening, effusion control, pain management, patellar mobilization, and functional range-of-motion restoration. Return to sport is not permitted for a minimum of 4 months. Beyond that time, return to sport is allowed when the findings of isokinetic and functional testing of the operated limb are at least 90% of those of the contralateral limb.7,8
Discussion
The described technique allows reconstruction of both the MPFL and MQTFL. The rationale for the procedure is to replicate the native anatomy and biomechanics of the PMPRs in their entirety. Although the MPFL is widely recognized as the primary restraint to lateral patellar translation, it has recently been shown that the MQTFL has an equally important role near full extension and is more effective in restoring native patellar stability than isolated MPFL reconstruction.3,4 Additionally, Song et al.9 showed on 4-dimensional computed tomography that the superior-most fibers of the medial patellofemoral complex resist dislocation at low flexion angles whereas the inferior-most fibers maintain tilt in mid flexion. These findings may partly explain why isolated MPFL reconstruction fails to abolish symptoms of persistent apprehension in an important proportion (>8%) of patients.10 Similarly to Fulkerson,5 we believe that reconstructions including both the MPFL and MQTFL, given their different functions, are probably optimal.
The recent interest in isolated MQTFL reconstruction has, to some extent, been driven by a desire to use techniques that avoid drilling the patella. This is a logical goal because even though patellar fracture is uncommon, it is a major complication of MPFL reconstruction.10 The technique for combined MPFL and MQTFL described in this article does not avoid a patellar tunnel and therefore does not share this potential advantage of an isolated MQTFL reconstruction. However, it should be noted that the consequences of avoiding a tunnel in terms of graft integration and function (beyond time-zero biomechanical studies) are not well studied. Concern regarding the value of avoiding a tunnel has been raised by a recent systematic review that highlighted that MPFL techniques that did not use a tunnel had a higher rate of recurrent dislocation or subluxation (4.8% vs 3.3%) and apprehension or hypermobility (24.0% vs 8.6%) than techniques that used a tunnel.10 Clearly, avoiding a patellar tunnel is not necessarily better, and further clinical study is required to precisely understand the risk-benefit ratios and complication profiles of the respective procedures. Despite this, there are some circumstances in which avoiding a patellar tunnel is clearly advantageous; these include some cases of revision in which multiple previous tunnels are present, as well as pediatric patients in whom the risk of patellar fracture is highest. Spang et al.11 reported favorable short-term results with a combined MPFL and MQTFL technique (using suture anchors rather than a patellar tunnel) in children and adolescents, but to our knowledge, clinical outcomes of this technique in an adult population have not been reported to date.
A further reason to consider an alternative to isolated MPFL reconstruction is that these procedures have been associated with overconstraint.4,12 Spang et al.4 found significantly less lateral translation after MPFL reconstruction than either in the native state or after MQTFL reconstruction. Furthermore, Rood et al.12 reported that static MPFL fixation techniques (rigid fixation to bone) caused 3- to 5-fold increases in patellofemoral contact pressures (between 60° and 110° of knee flexion) compared with dynamic techniques (soft-tissue fixation).8 The current technique uses a patellar tunnel but also a soft-tissue tunnel in the quadriceps (Fig 8). Although this particular technique has not been evaluated in a biomechanical study, we believe that its more anatomic nature (reconstructing the PMPRs in their entirety), as well as the use of patellar and quadriceps tunnels (the latter providing dynamic fixation), provides an excellent opportunity for graft integration while minimizing the risk of overconstraint.
Fig 8.
Tunnel positions and graft location for described technique of combined reconstruction of medial patellofemoral ligament and medial quadriceps tendon–femoral ligament.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Combined reconstruction of medial patellofemoral ligament (MPFL) and medial quadriceps tendon–femoral ligament (MQTFL). A 3-cm incision is placed at the medial border of the proximal third of the patella. A bone tunnel is created at the junction between the upper and middle thirds of the medial border of the patella (approximately the midpoint of the patellar insertion of the MPFL). This is performed by drilling 2 interconnecting sockets. The first socket is drilled on the anterior surface of the patella 1 cm from its medial border. The second socket is created in the mid-axial plane on the medial side of the patella, joining the anterior tunnel at a 90° angle. Next, a tunnel is created in the medial and distal third of the quadriceps tendon close to the midpoint of the MQTFL insertion. Through a 2-cm medial incision, a tunnel is drilled at the Schöttle point using fluoroscopy. The graft is passed through the patellar and quadriceps tendon tunnels and to the region of the medial epicondyle between layers 2 and 3, where it is docked in the femoral tunnel. With the knee flexed to 60° and the patella in a central position on the trochlea, the graft tension is determined by the confirmation of a hard endpoint to lateral translation while maintaining the ability to lateralize the patella by 1 to 2 quadrants. Once graft tension is confirmed, an 7 × 25–mm absorbable soft-tissue interference screw (Arthrex) is used to fix the graft in the femoral tunnel.
References
- 1.Loeb A.E., Tanaka M.J. The medial patellofemoral complex. Curr Rev Musculoskelet Med. 2018;11:201–208. doi: 10.1007/s12178-018-9475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baumann C.A., Hinckel B.B., Tanaka M.J. Update on patellofemoral anatomy and biomechanics. Oper Tech Sports Med. 2019;27:150683. [Google Scholar]
- 3.Christian D.R., Redondo M.L., Cancienne J.M. Differential contributions of the quadriceps and patellar attachments of the proximal medial patellar restraints to resisting lateral patellar translation. Arthroscopy. 2020;36:1670–1676. doi: 10.1016/j.arthro.2020.01.058. [DOI] [PubMed] [Google Scholar]
- 4.Spang R., Egan J., Hanna P. Comparison of patellofemoral kinematics and stability after medial patellofemoral ligament and medial quadriceps tendon–femoral ligament reconstruction. Am J Sports Med. 2020;48:2252–2259. doi: 10.1177/0363546520930703. [DOI] [PubMed] [Google Scholar]
- 5.Fulkerson J.P. Editorial Commentary: The best medial patellofemoral reconstruction may include components of both quadriceps and patellar attachments. Arthroscopy. 2020;36:1677–1678. doi: 10.1016/j.arthro.2020.02.034. [DOI] [PubMed] [Google Scholar]
- 6.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 7.McGee T.G., Cosgarea A.J., McLaughlin K., Tanaka M., Johnson K. Rehabilitation after medial patellofemoral ligament reconstruction. Sports Med Arthrosc Rev. 2017;25:105–113. doi: 10.1097/JSA.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 8.Manske R.C., Prohaska D. Rehabilitation following medial patellofemoral ligament reconstruction for patellar instability. Int J Sports Phys Ther. 2017;12:494–511. [PMC free article] [PubMed] [Google Scholar]
- 9.Song S.Y., Pang C.H., Kim C.H., Kim J., Choi M.L., Seo Y.J. Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med. 2015;43:1165–1171. doi: 10.1177/0363546514567061. [DOI] [PubMed] [Google Scholar]
- 10.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spang R.C., Tepolt F.A., Paschos N.K., Redler L.H., Davis E.A., Kocher M.S. Combined reconstruction of the medial patellofemoral ligament (MPFL) and medial quadriceps tendon-femoral ligament (MQTFL) for patellar instability in children and adolescents. J Pediatr Orthop. 2019;39:e54–e61. doi: 10.1097/BPO.0000000000001259. [DOI] [PubMed] [Google Scholar]
- 12.Rood A., Hannink G., Lenting A. Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med. 2015;43:2538–2544. doi: 10.1177/0363546515594447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Combined reconstruction of medial patellofemoral ligament (MPFL) and medial quadriceps tendon–femoral ligament (MQTFL). A 3-cm incision is placed at the medial border of the proximal third of the patella. A bone tunnel is created at the junction between the upper and middle thirds of the medial border of the patella (approximately the midpoint of the patellar insertion of the MPFL). This is performed by drilling 2 interconnecting sockets. The first socket is drilled on the anterior surface of the patella 1 cm from its medial border. The second socket is created in the mid-axial plane on the medial side of the patella, joining the anterior tunnel at a 90° angle. Next, a tunnel is created in the medial and distal third of the quadriceps tendon close to the midpoint of the MQTFL insertion. Through a 2-cm medial incision, a tunnel is drilled at the Schöttle point using fluoroscopy. The graft is passed through the patellar and quadriceps tendon tunnels and to the region of the medial epicondyle between layers 2 and 3, where it is docked in the femoral tunnel. With the knee flexed to 60° and the patella in a central position on the trochlea, the graft tension is determined by the confirmation of a hard endpoint to lateral translation while maintaining the ability to lateralize the patella by 1 to 2 quadrants. Once graft tension is confirmed, an 7 × 25–mm absorbable soft-tissue interference screw (Arthrex) is used to fix the graft in the femoral tunnel.