Abstract
Dogs and cats play an important role as reservoirs of vector-borne pathogens, yet reports of canine and feline vector-borne diseases in Saudi Arabia are scarce. Blood samples were collected from 188 free-roaming dogs and cats in Asir (70 dogs and 44 cats) and Riyadh (74 dogs), Saudi Arabia. The presence of Anaplasma spp., Bartonella spp., hemotropic Mycoplasma spp., Babesia spp., and Hepatozoon spp. was detected using a multiplex tandem real-time PCR. PCR-positive samples were further examined with specific conventional and real-time PCR followed by sequencing. Dogs from Riyadh tested negative for all pathogens, while 46 out of 70 dogs (65.7%) and 17 out of 44 cats (38.6%) from Asir were positive for at least one pathogen. Positive dogs were infected with Anaplasma platys (57.1%), Babesia vogeli (30%), Mycoplasma haemocanis (15.7%), and Bartonella henselae (1.4%), and cats were infected with Mycoplasma haemofelis (13.6%), Candidatus Mycoplasma haemominutum (13.6%), B. henselae (9.2%), and A. platys (2.27%), all of which are reported for the first time in Saudi Arabia. Co-infection with A. platys and B. vogeli was detected in 17 dogs (24.28%), while coinfections were not detected in cats. These results suggest that effective control and public awareness strategies for minimizing infection in animals are necessary.
Keywords: Anaplasma, Babesia, Bartonella, Mycoplasma, one health, Saudi Arabia, vector-borne pathogens, zoonosis
1. Introduction
Vector-borne pathogens (VBPs) transmitted by ticks, fleas, and mosquitoes, are of global importance especially in the case of zoonotic infections which pose a direct threat to human health and animal welfare [1,2,3]. Vector-borne diseases (VBDs) as a result of infection with viral, bacterial, and protozoal VBPs are often widespread in tropical and subtropical regions [4], including in the Middle East, due to the optimal climatic conditions for the perpetuation of arthropods involved in their transmission [5]. In this context, vector-borne infections of dogs and cats—that have a close relationship with humans in both urban and rural areas—pose potential public health concerns [6]. However, data on the occurrence of canine and feline VBDs are only available in a few countries of the Middle East such as Qatar [7], Iraq [8], and Iran [9]. In a previous study from the Riyadh Province, 37% of dogs’ blood DNA samples (20/53) were suspected positive for B. vogeli, Mycoplasma haemocanis, and Candidatus Mycoplasma haematoparvum, yet none were confirmed using Sanger sequencing [10]. Unlike elsewhere in Saudi Arabia, Riyadh is a semi-arid area with low annual rainfall and relative humidity, making it unsuitable for tick species that prefer more temperate or tropical climates, such as Rhipicephalus sanguineus (Latreille, 1806) sensu lato (s.l.). While much of the country is similarly hot and dry, the coastal areas of Saudi Arabia and those at higher altitudes may be more accommodating to parasites capable of VBD transmission. Investigations into ectoparasite and VBP prevalence in these regions, however, remain lacking, which makes the impact of VBDs on animal and human populations difficult to quantify.
Scant scientific information is available regarding the tick fauna of dogs and cats in Saudi Arabia and the pathogens they harbor. Two tick species, Rh. sanguineus s.l. and Hyalomma dromedarii (Koch, 1844), commonly infest dogs in Saudi Arabia [10,11]. In regard to cats only Rh. sanguineus s.l. and H. dromedarii have been reported in Saudi Arabia [12]. Both tick species are known to be vectors and/or intermediate hosts of a variety of parasites, bacteria, and viruses, some of which are zoonotic agents [13]. For instance, Rh. sanguineus s.l. plays an important role in the transmission of numerous pathogens, including members of the genera Babesia, Hepatozoon, Anaplasma, Ehrlichia, Rickettsia, and hemotropic mycoplasmas [14,15]. Hyalomma dromedarii is also known to be a vector of Rickettsia aeschlimannii, Rickettsia africae, and the protozoan parasite Theileria annulata [16].
Likewise, there are no data on the fleas of dogs and cats in Saudi Arabia and the flea-borne infections in these animals. Fleas are vectors and intermediate hosts of various bacteria (e.g., hemotropic Mycoplasma spp., Bartonella spp., Rickettsia spp.) and parasites, e.g., Acanthocheilonema reconditum and Dipylidium caninum [17]. The cat flea Ctenocephalides felis (Bouche, 1835), one of the main vectors of Bartonella henselae—the causative agent of the “cat scratch disease”—is the predominant flea species found on cats and dogs worldwide [18]. Both C. felis [19] and human infection with B. henselae have been reported in Saudi Arabia [20]. However, there is no information about the prevalence of bartonellosis in dogs and cats in this country.
In previous studies from the Riyadh Province, the tested dogs’ blood DNA samples were found infected with VBPs [10]; and 49.5% of dogs and 13.8% of cats were infested with ticks, identified as H. dromedarii and Rh. sanguineus s.l. [10,11], the latter of which is a competent vector of several vector-borne pathogens [3,21]. Hence, the aim of the current study was to add to the existing knowledge on the identity, prevalence, and distribution of VBPs in Saudi Arabia by screening free roaming dogs and cats from two locations, one temperate and one semi-arid (Riyadh and Asir Provinces, respectively).
2. Results
2.1. Presence of VBPs in Dogs
Multiplex tandem real-time PCR (MT-PCR) revealed that dogs from the Riyadh Province tested negative for all the pathogens; however, 46 out of 70 dogs (65.7%) from the Asir Province were PCR-positive for at least one of the tested pathogens, i.e., Anaplasma spp., Babesia spp., Bartonella spp., and Mycoplasma spp. Specific PCRs showed that dogs (Table 1) were mainly infected with A. platys (57.1%), followed by B. vogeli (30.0%), M. haemocanis (15.7%), and B. henselae (1.4%). Co-infection with A. platys and B. vogeli was detected in 17 dogs (24.3%).
Table 1.
Prevalence of vector-borne pathogens in stray dogs (n = 70) and cats (n = 44) in the Asir Province, Saudi Arabia, using multiplex tandem real-time PCR. Dogs from Riyadh tested negative for all the pathogens (not included in the table).
| Pathogen | No. of Infected Dogs (%) | No. of Infected Cats (%) | Accession Numbers * |
|---|---|---|---|
| Anaplasma platys | 40 (57.1%) | 1 (2.27%) | MW199129 |
| Babesia vogeli | 21 (30%) | 0 | MW204836 |
| Bartonella henselae | 1 (1.4%) | 4 (9.1%) | MW208843 |
| Mycoplasma haemocanis/Mycoplasma haemofelis | 11 (15.7%) | 6 (13.63%) | MW280822–MW280824 |
| Candidatus Mycoplasma haemominutum | 0 | 6 (13.63%) | ns |
* Primers are listed in Section 4.6. Specific pathogens’ detection and sequencing; ns = not sequenced.
The nucleotide sequences of A. platys isolate from a dog in Asir (accession number MW199129) was 100% identical to A. platys of dogs from China (MN630836), South Africa (MK814413–MK814421), and Cuba (KX792089) and from Armigeres subalbatus (Culicidae) from China (KU586175). The sequence of one B. vogeli (accession number MW204836) was 100% identical to B. vogeli of dogs from Malawi (LC556376–LC556377), China (MK881089) and from cats in China (MN067708–MN067709). The Mycoplasma haemocanis sequence (accession number MW280824) was 100% identical to isolates from dogs in South Korea (MT345534), Mexico (MN294708), Chile (KY117659), Taiwan (KJ858513), Thailand (KU765208), Brazil (KP715860) and cats in Brazil (KM275242, KM275246–KM275247).
2.2. Presence of VBPs in Cats
In total, 17 out of the 44 cats (38.6%) tested positive according to the MT-PCR, with a higher prevalence of M. haemofelis/M. haemocanis (13.6%) and Candidatus Mycoplasma haemominutum (13.6%), followed by B. henselae (9.1%) and A. platys (2.3%) (Table 1).
Nucleotide sequences of one B. henselae isolate from a cat (accession number MW208843) was >99% identical to B. henselae isolates from small Indian mongoose (Herpestes auropunctatus) in Grenada, West Indies (MG680299, MG680304, MG680305, MG680309, MG680313).
Nucleotide sequences of M. haemofelis from two cats (accession numbers MW280822–MW280823) were 100% identical to M. haemofelis isolates from cats in Brazil (KM275242, KM275246–KM275247) and one single-nucleotide polymorphism (SNP) different from the M. haemofelis strain Ohio2 (CP002808), also identical with M. haemocanis isolates from dogs in Iran (KU886264) and dogs in Turkey (KX641903) and Pulex irritans in Argentina (MK097143).
2.3. Risk Factor Analysis in Dogs
Summary statistics for the animals’ characteristics and risk factors are presented in Table 2. The presence of A. platys DNA was significantly associated with age, with more one-year-old dogs (78.9%, 15/19) considered PCR-positive than older age groups (49%, 25/51) (OR = 3.9, p-value = 0.03). In contrast to A. platys, the presence of M. haemocanis DNA was significantly higher in dogs older than 4-years-old (34.5%, 10/29) when compared to younger animals (2.4%, 1/41). Results of the multivariable binary logistic regression analysis showed that dogs older than 4-years-old were 18.6 times more likely to be PCR-positive for M. haemocanis than dogs 3-years-old and younger (OR = 18.6, p-value = 0.009); and symptomatic dogs were 8.3 times more likely to be PCR-positive than asymptomatic ones (OR = 8.28, p-value = 0.038).
Table 2.
Characteristics of 188 stray dogs and cats for study of the vector-borne pathogens in the Asir and Riyadh Provinces, Saudi Arabia.
| Variable | Asir Province | Riyadh Province | |
|---|---|---|---|
| Dogs (n = 70) | Cats (n = 44) | Dogs (n = 74) | |
| Age (years) | |||
| ≤1 | 19 (27.1%) | 24 (54.6%) | 17 (23%) |
| 2–3 | 22 (31.4%) | 10 (22.7%) | 19 (25.7%) |
| 4–5 | 8 (11.4%) | 0 (0.0%) | 10 (13.5%) |
| ≥6 | 21 (30.0%) | 10 (22.7) | 28 (37.8%) |
| Sex | |||
| male | 38 (54.3%) | 28 (63.6%) | 42 (56.8%) |
| female | 32 (45.7%) | 16 (36.4%) | 32 (43.2%) |
| Health status | |||
| symptomatic | 7 (10.0%) | 5 (11.4%) | 7 (9.5%) |
| asymptomatic | 63 (90.0%) | 39 (88.6%) | 67 (90.5%) |
| Infestation with ectoparasites | |||
| ticks | 27 (38.6%) | 11 (25.0%) | 18 (24.3%) |
| fleas | 22 (31.4%) | 11 (25.0%) | 29 (39.2%) |
| lice | 6 (8.6%) | 10 (22.7%) | 15 (20.3%) |
When the presence of DNA from any VBPs was considered as an outcome variable, male dogs (76.3%, 29/38) were more prone to being infected in comparison with female dogs (53.1%, 17/32). Odds of infection were 2.8 times higher in male dogs compared to females (OR = 2.8, p-value = 0.045). In addition, dogs positive for M. haemocanis DNA were more often symptomatic (36.4%, 4/11) than those PCR-negative (5.1%, 3/59). No other significant association was observed between infection with other hemoparasites and gender, health status, and infestation with ectoparasites.
2.4. Risk Factor Analysis in Cats
The only significant association in cats was between health status and infection with Candidatus Mycoplasma haemominutum. Three out of a total of six infected cats were symptomatic compared with two of the 38 uninfected ones (OR = 18, p-value = 0.008). No significant association was detected between infection with VBPs in cats and the studied risk factors including sex, age, health status, and infestation with ectoparasites.
2.5. Symptoms Associated with Pathogens
In 6/7 dogs and 3/5 cats that were PCR-positive for VBPs, fever, anorexia, emaciation, colics, and red eyes were observed. One dog and two cats with one or more symptoms, however, were PCR-negative for all the VBPs tested (Supplementary Table S1).
3. Discussion
The high occurrence of VBD-causing pathogens in free-roaming dogs (65.7%) and cats (38.6%) in the Asir Province indicates that animal populations are exposed to multiple VBPs, including those of zoonotic importance, posing both a companion animal and a public health risk. In comparison, however, the absence of all the pathogens in the dogs from Riyadh Province suggests that the climate is less conducive to the survival of ticks compared to the Asir Province, which may in turn contribute to a reduction in the transmission of VBDs. The absence of VBPs in the dogs from Riyadh in the current study is similar to the findings of a previous study, where 53 blood DNA samples from dogs in Riyadh were ultimately considered free from specific pathogen DNA [10]. The lack of VBPs in the previous study was attributed to the low prevalence of Rh. sanguineus s.l. parasitising dogs in Riyadh, likely due to its arid climate. Lower numbers of ticks were observed in Riyadh in the current study, providing further evidence that the low annual rainfall and relative humidity restricts the distribution of ectoparasites and the pathogens they vector in Riyadh.
In the Middle East, little information is available about the prevalence of canine and feline VBDs; however, results of previous studies in Qatar, Iraq, and Iran showed that stray dogs and cats often act as reservoirs of zoonotic pathogens with the prevalence of 18.8%, 38.1%, 54.6% in dogs [7,8,22] and 20.6%, 39.1% in cats [7,8] from Qatar, Iraq, and Iran. The prevalence of the A. platys infection in the dogs (57.1%) from the Asir Province is much higher in the present study than in the previous reports from the Middle East, e.g., 1.6% in Qatar [7], 3.33% in Iraq [8,23], 3.67% in Iran [22], 0.5% in Turkey [24], and 9.63% in Palestine [25]. Camels have also been found to be infected with A. platys in Saudi Arabia, making it the most prevalent tick-borne pathogen in the region [26] and suggesting that other mammalian hosts might play role in the epizootology of this parasite. In dogs, this infection is usually mild or asymptomatic, but animals may develop clinical signs such as anorexia, weight loss, lymphadenomegaly, hyperthermia, and hemorrhage, which can be fatal [27]. Not much is known, however, about the A. platys infection in cats. In two reports, naturally-infected cats exhibited anorexia, apathy, anuria, constipation, and jaundice [28,29]. Our statistical analyses revealed that infection with A. platys was more common in younger dogs, although breed, age, and sex have all been identified as risk factors for A. platys infections [30]. Although tick-borne transmission of A. platys remains the main route of circulation of this parasite, vertical transmission of A. platys from pregnant dogs to their offspring [31,32] suggests that controlling this infection in free-roaming dog populations might not be easy.
In this study, hemoplasmas were detected in 27.2% of cats (13.6%, M. haemofelis, and 13.6%, Candidatus Mycoplasma haemominutum) and 15.7% of dogs (M. haemocanis). The above prevalence is higher than in the previous reports from Qatar, i.e., 2.9% for M. haemofelis, 2.9% for Candidatus Mycoplasma haemominutum, and 5.9% for Mycoplasma spp. in cats and 7.8% for Mycoplasma spp. in dogs [7]. However, the prevalence of hemoplasmosis in Saudi Arabia as determined in the current study is similar to that recorded in Iran, where 22–25.4% cats and 6.25–22% of dogs with single or multiple hemoplasmas have been reported [33,34,35,36,37]. Statistical analyses revealed that older dogs were infected more often than younger ones. It has been documented that other than the older age, cross-breeding, and mange infection, presence of vectors, bite wounds, neoplastic diseases, and rural vs. urban localities are risk factors for hemoplasmosis in dogs and cats [38,39]. Since hemotropic Mycoplasma spp. including Candidatus Mycoplasma haematoparvum can infect humans [40,41] and arthropods are considered major players in the epidemiology of hemoplasmas, control of fleas and ticks on dogs and cats is advocated.
Bartonella henselae is herein reported for the first time in 9.1% of cats and 1.4% of dogs from Saudi Arabia. There is not much known about the epidemiology of bartonellosis in the Middle East. In Iran, infection of 7.14–12.5% of cats with B. henselae [42,43,44] and 12.5–24.24% of dogs with Bartonella rochalimae, Candidatus Bartonella merieuxii and Bartonella vinsonii subsp. berkhoffii has been confirmed by molecular analyses [9,45]. Overall seroprevalence of 74.2% for B. henselae, Bartonella clarridgeiae, and B. vinsonii subsp. berkhoffii was recorded in dogs [9]. Similarly, in Iraq, a seroprevalence of 15% for B. henselae and 12.6% for B. clarridgeiae in stray cats [46] and an overall seroprevalence of 47.4% in dogs for B. henselae, B. clarridgeiae, B. vinsonii subsp. berkhoffii, and Bartonella bovis was reported [47]. In Saudi Arabia, bartonellosis has been reported in 68% of Balochistan jirds (Gerbillus nanus), 60.33% of Libyan jirds (Meriones libycus), 13.39% of desert hedgehogs (Paraechinus aethiopicus), and one human patient [20,48,49]. Considering that in cats and dogs, the asymptomatic course with persistent bacteremia is a frequent outcome of infection [50], infected animals may pose high infection risks to owners or veterinary healthcare workers in endemic areas.
The prevalence of B. vogeli-infected dogs (i.e., 29.9%) is higher than previously reported from Middle Eastern countries, e.g., 3.2% in Qatar [7], 1.5% in Palestine [51], 0.1% in Turkey [24], 0% in Iraq [8], and 1.13% in different regions of Iran [22]. Although B. vogeli and Babesia canis are known to infect cats [52], we could not detect DNA of either Babesia species in the blood of cats. Further molecular studies are needed to better understand canine and feline babesiosis in Saudi Arabia because the MT-PCR used to screen samples in the current study could only detect B. vogeli and Babesia gibsoni.
Dogs were not examined for Ehrlichia canis and Anaplasma phagocytophilum, the causative agents of monocytic ehrlichiosis and granulocytic anaplasmosis in dogs and humans [3,21]. While canine monocytic ehrlichiosis (CME) is a worldwide distributed tick-borne infection, A. phagocytophilum is more common in Europe and North America [30]. In a previous study from an eastern region of Saudi Arabia, CME was diagnosed by serology in nine dogs from a colony, while only one dog was PCR-positive [53]. In another study from Saudi Arabia, DNA from the blood of 53 dogs living in Riyadh tested negative for E. canis [10]. There are few reports on the prevalence of E. canis-infected dogs from other Middle Eastern countries, e.g., 2/64 in Qatar [7], 9/240 and 0/354 in Iran [22,54], 0/97 in Iraq [8]. Similarly, A. phagocytophilum does not seem to be prevalent in dogs of the region since in previous studies from Saudi Arabia, Qatar, Iraq, and five regions of Iran, the infection could not be detected [7,8,10,22]. However, DNA of A. phagocytophilum was found in the blood of camels from Riyadh [55]. Further studies are needed to determine domestic and wild reservoir hosts for E. canis and A. phagocytophilum in this country [3] as well as the tick species acting as vectors. However, the small number of samples examined in the current study prevent wider conclusions to be drawn regarding the prevalence of VBPs in Saudi Arabia.
4. Materials and Methods
4.1. Study Area and Sampling
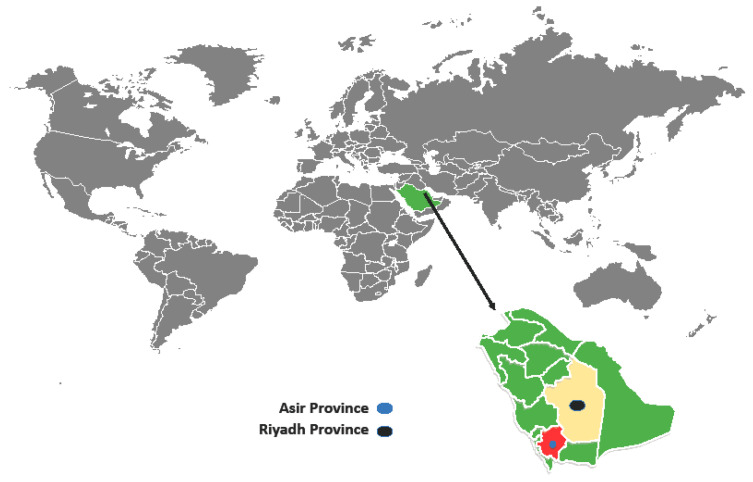
The investigation was conducted from November 2018 to August 2019 in the Asir (19.0969° N, 42.8638° E) and Riyadh (24.7136° N, 46.6753° E) Provinces, located in southwestern and central Saudi Arabia, respectively (Figure 1). The Asir Province borders the Red Sea and Yemen, has an area of 76,690 km2, and is situated on a high plateau that receives more rainfall than the rest of the country and contains the country’s highest peaks, which rise to almost 3000 m above sea level. According to the Köppen-Geiger climate classification, this province has different climates, but the most prevalent ones are BWh (hot desert climates) and BSk (cold semi-arid climates). The average annual rainfall in the highlands ranges from 300 to 500 mm across two rainy seasons. As a result, there is much more natural vegetation and forests. Riyadh region’s climate, however, is BWh with virtually no rainfall during the year (http://www.pme.gov.sa).
Figure 1.
Map showing the study sites of the Riyadh Province and the Asir Province, Saudi Arabia.
4.2. Sampling of Dogs and Cats and Blood Collections
A total of 188 free-roaming dogs and cats in two provinces of Asir (70 dogs and 44 cats) and Riyadh (74 dogs) (Table 2) were trapped with a live animal trap (Havahart, Lancaster, PA, USA). Treats were provided for animals in the trap and they were restrained after having calmed down. From each animal, 0.5–3 mL blood samples were collected from the cephalic or saphenous vein in vacutainer tubes containing an EDTA anticoagulant (BD Vacutainer® Tube, Gribbles Veterinary Pathology, Clayton, Victoria, Australia). Dogs and cats were set free after the blood collection. Animal data including age estimated by examination of teeth (1–6 years) and sex were recorded. All of the animals except seven dogs and five cats were apparently healthy. The symptoms of the sick animals were moderate or high fever, anorexia, emaciation, colics, and reddish eyes, though they were general and not exclusively related to the specific conditions caused by VBD-causing pathogens. Infestation of the animals with ticks, fleas, and lice was also recorded. Blood samples were refrigerated and transported to the Laboratory of Parasitology, Department of Biological Sciences, Faculty of Science and Humanities, Shaqra University.
4.3. DNA Extraction
Total genomic DNA (gDNA) was isolated from the blood samples using a Wizard® Genomic DNA Purification Kit (Promega, Madison, WI, USA) and eluted into 50 μL or 100 μL of the elution buffer according to the manufacturer’s instructions. Aliquots of DNA were sent to the Veterinary Pathology Diagnostic Services (VPDS), Sydney School of Veterinary Science, The University of Sydney for molecular diagnostic processing and pathogen identification. Upon arrival at the VPDS, gDNA was stored at −20 ˚C for up to 1 month prior to screening.
4.4. Screening of VBPs by Multiplex Tandem Real-Time PCR (MT-PCR)
The diagnostics of VBPs was performed using the AusDiagnostics real-time quantitative MT-PCR panel for small animals’ anemia (Mascot, New South Wales, Australia) on the AusDiagnostics Easy-PlexTM platform (Mascot, New South Wales, Australia). This automated two-step nested PCR simultaneously detects A. platys, B. vogeli, B. gibsoni, Bartonella spp., Mycoplasma haemofelis, M. haemocanis, Candidatus Mycoplasma haemominutum, and Candidatus Mycoplasma haematoparvum [56]. The assay was run using a 10 μL undiluted gDNA sample and each pathogen was detected during a short (10 cycles) conventional PCR (cPCR) followed by a second longer SYBR-based qPCR.
4.5. Specific Pathogens’ Detection and Sequencing
The most positive samples for Babesia spp. (5 dogs), Anaplasma spp. (5 dogs), and Mycoplasma spp. (5 dogs and 5 cats) in addition to all the positive samples for Bartonella (4 cats and 1 dog) were further examined specifically by either cPCR using primers PLATYSF (5′-GATTTTTGTCGTAGCTTGCTATG-3′) and EHR16SR (5′-TAGCACTCATCGTTTACAGC-3′) for A. platys [28], HBT-F (5′-ATACGGCCCATATTCCTACG-3′) and HBT-R (5′-TGCTCCACCACTTGTTCA-3′) for Mycoplasma spp. [57], PIRO-A (5′-AATACCCAATCCTGACACAGGG-3′) and PIRO-B (5′-TTAAATACGAATGCCCC-3′) for Babesia spp. [58], or a multiplex TaqMan probe real-time PCR targeting the ssrA gene of Bartonella spp. with primers ssrA-F (5′-GCTATGGTAATAAATGGACAATGAAATAA-3′), ssrA-R (5′-GCTTCTGTTGCCAGGTG-3′), and 6-carboxyfluorescein (FAM)-labeled probe (5′-ACCCCGCTTAAACCTGCGACG-3′-BHQ1) [59]. All the cPCR reactions were run using the MyTaqTM Red Mix (Bioline, Rhodes, Australia) in a VeritiTM thermal cycler (Thermo Fisher Scientific, North Ryde, Australia) and real-time PCR reactions were run using a SensiFASTTM Probe No-ROX Kit (Meridian Bioscience, Eveleigh, Australia) that does not need a passive reference signal of carboxy-X-rhodamine (ROX) for normalization of the data on a CFX95 TouchTM Real-Time PCR detection system (Meridian Bioscience, Eveleigh, Australia). A negative control and a positive control were included in each run.
All PCR products were separated by electrophoresis in 2% agarose gel stained with GelRedTM (Biotium, Fremont, CA, USA) and visualized using UV light. Samples that displayed discrete bands of expected sizes were sent to Macrogen Ltd. in Seoul, South Korea, for bidirectional sequencing using amplification primers. Unambiguous sequences were assembled and compared to the closely related NCBI GenBank sequences using CLC Main Workbench ver. 6.8.1 (CLC bio, Vedbæk, Denmark). Representative sequences of pathogens detected in this study were deposited in GenBank (Table 1).
4.6. Statistical Analysis
Statistical analyses were performed with the statistics package SPSS ver. 25.0 (IBM, Armonk, NY, USA). A positive PCR test was set as an outcome variable and the independent variables were age, gender, health status, and infestation with ticks, fleas, or lice. The association of independent variables with outcome variables were evaluated by the chi-squared test, the Fisher’s exact test, and binary logistic regression analysis for calculation of the odds ratio. Differences were considered significant if the p-value was < 0.05.
5. Conclusions
All of the VBPs of dogs (A. platys, B. vogeli, M. haemocanis, and B. henselae), and in cats (M. haemofelis, Candidatus Mycoplasma haemominutum, B. henselae, and A. platys) are reported for the first time from these species in Saudi Arabia. The connection between these VBPs and their arthropod vectors in Saudi Arabia remains unknown and warrants further investigation. Climate appears to be the limiting factor affecting distribution of these pathogens, which may or may not be related to the distribution of their associated ectoparasite hosts. Considering that B. henselae and A. platys are known zoonotic pathogens and that dogs and cats pose human infection risks, effective ectoparasite control strategies are advocated.
Acknowledgments
The authors would like to thank the staff members of the Biological Science Department, Faculty of Science and Humanities, Shaqra University, and the staff members of the Veterinary Pathology Diagnostic Services, Sydney School of Veterinary Science, The University of Sydney, for kind technical support. We are also grateful to Jan Šlapeta (The University of Sydney). Although he supervised the PCRs, he did not follow our invitation to become co-author. Nevertheless, many thanks for his help.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-0817/10/1/25/s1, Table S1: Symptoms of dogs and cats from the Asir Province, Saudi Arabia, infected with VBPs detected via multiplex tandem real-time PCR.
Author Contributions
Conceptualization, A.D.A.; methodology, A.D.A., A.S.A., M.S.A., M.Y.A., H.H.A.M.A., S.A.-S., M.A.-L. and N.E.D.C.; writing—original draft preparation, A.S., M.A.-L., A.D.A. and N.E.D.C.; writing—review and editing, A.S., D.O., M.A.-L. and N.E.D.C.; supervision, A.D.A. and M.S.A.; project administration and funding acquisition, A.D.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Researcher Supporting Project, King Saud University, Riyadh, Saudi Arabia, number RSP-2020-192, and by the Deanship of Scientific Research, King Khalid University, Saudi Arabia, number G.R.P2/78-40.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethical Research Committee, Deanship of Scientific Research, King Khalid University (protocol code ECM #2020-198/HAPO-06-B-001).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yuasa Y., Hsu T.-H., Chou C.-C., Huang C.-C., Huang W.-C., Chang C.-C. The comparison of spatial variation and risk factors between mosquito-borne and tick-borne diseases: Seroepidemiology of Ehrlichia canis, Anaplasma species, and Dirofilaria immitis in dogs. Comp. Immunol. Microbiol. Infect. Dis. 2012;35:599–606. doi: 10.1016/j.cimid.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 2.de la Fuente J., Antunes S., Bonnet S., Cabezas-Cruz A., Domingos A.G., Estrada-Peña A., Johnson N., Kocan K.M., Mansfield K.L., Nijhof A.M. Tick-pathogen interactions and vector competence: Identification of molecular drivers for tick-borne diseases. Front. Cell. Infect. Microbiol. 2017;7:114. doi: 10.3389/fcimb.2017.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dantas-Torres F., Chomel B.B., Otranto D. Ticks and tick-borne diseases: A one health perspective. Trends Parasitol. 2012;28:437–446. doi: 10.1016/j.pt.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen V., Colella V., Greco G., Fang F., Nurcahyo W., Hadi U., Venturina V., Tong K., Tsai Y., Taweethavonsawat P., et al. Molecular detection of pathogens in ticks and fleas collected from companion dogs and cats in East and Southeast Asia. Parasit. Vectors. 2020;13 doi: 10.1186/s13071-020-04288-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilpatrick A.M., Randolph S.E. Drivers, dynamics, and control of emerging vector-borne zoonotic diseases. Lancet. 2012;380:1946–1955. doi: 10.1016/S0140-6736(12)61151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otranto D., Dantas-Torres F. Canine and feline vector-borne diseases in Italy: Current situation and perspectives. Parasit. Vectors. 2010;3:2. doi: 10.1186/1756-3305-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alho A.M., Lima C., Latrofa M.S., Colella V., Ravagnan S., Capelli G., de Carvalho L.M., Cardoso L., Otranto D. Molecular detection of vector-borne pathogens in dogs and cats from Qatar. Parasit. Vectors. 2017;10:298. doi: 10.1186/s13071-017-2237-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Otranto D., Iatta R., Baneth G., Cavalera M.A., Bianco A., Parisi A., Dantas-Torres F., Colella V., McMillan-Cole A.C., Chomel B. High prevalence of vector-borne pathogens in domestic and wild carnivores in Iraq. Acta Trop. 2019;197:105058. doi: 10.1016/j.actatropica.2019.105058. [DOI] [PubMed] [Google Scholar]
- 9.Greco G., Sazmand A., Goudarztalejerdi A., Zolhavarieh S.M., Decaro N., Lapsley W.D., Otranto D., Chomel B.B. High prevalence of Bartonella sp. in dogs from Hamadan, Iran. Am. J. Trop. Med. Hyg. 2019;101:749–752. doi: 10.4269/ajtmh.19-0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandra S., Smith K., Alanazi A.D., Alyousif M.S., Emery D., Šlapeta J. Rhipicephalus sanguineus sensu lato from dogs and dromedary camels in Riyadh, Saudi Arabia: Low prevalence of vector-borne pathogens in dogs detected using multiplexed tandem PCR panel. Folia Parasitol. 2019;66:007. doi: 10.14411/fp.2019.007. [DOI] [PubMed] [Google Scholar]
- 11.Alanazi A.D., Al-Mohammed H.I., Alyousif M.S., Said A.E., Salim B., Abdel-Shafy S., Shaapan R.M. Species diversity and seasonal distribution of hard ticks (Acari: Ixodidae) infesting mammalian hosts in various districts of Riyadh province, Saudi Arabia. J. Med. Entomol. 2019;56:1027–1032. doi: 10.1093/jme/tjz036. [DOI] [PubMed] [Google Scholar]
- 12.Alanazi A., Al-Mohamed H., Alysousif M., Puschendorf R., Abdel-Shafy S. Ticks (Acari: Ixodidae) infesting domestic and wild mammalians on the Riyadh province, Saudi Arabia. J. Entomol. 2018;15:75–82. doi: 10.3923/je.2018.75.82. [DOI] [Google Scholar]
- 13.Estrada-Peña A., Mihalca A.D., Petney T.N. Ticks of Europe and North Africa: A guide to species identification. Springer; Cham, Switzerland: 2018. [Google Scholar]
- 14.Dantas-Torres F. The brown dog tick, Rhipicephalus sanguineus (Latreille, 1806)(Acari: Ixodidae): From taxonomy to control. Vet. Parasitol. 2008;152:173–185. doi: 10.1016/j.vetpar.2007.12.030. [DOI] [PubMed] [Google Scholar]
- 15.Willi B., Boretti F.S., Meli M.L., Bernasconi M.V., Casati S., Hegglin D., Puorger M., Neimark H., Cattori V., Wengi N. Real-time PCR investigation of potential vectors, reservoirs, and shedding patterns of feline hemotropic mycoplasmas. Appl. Environ. Microbiol. 2007;73:3798–3802. doi: 10.1128/AEM.02977-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mihalca A., Pfäffle M., Petney T. Hyalomma dromedarii Koch, 1844. In: Estrada-Peña A., Mihalca A.D., Petney T.N., editors. Ticks of Europe and North Africa: A Guide to Species Identification. Springer; Cham, Switzerland: 2018. p. 366. [Google Scholar]
- 17.Bitam I., Dittmar K., Parola P., Whiting M.F., Raoult D. Fleas and flea-borne diseases. Int. J. Infect. Dis. 2010;14:e667–e676. doi: 10.1016/j.ijid.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Beugnet F., Halos L., Guillot J. Textbook of Clinical Parasitology in Dogs and Cats. Servet Publishing; Zaragoza, Spain: 2018. [Google Scholar]
- 19.el Bahrawy A., Al Dakhil M. Studies on the ectoparasites (fleas and lice) on rodents in Riyadh and its surroundings, Saudi Arabia. J. Egypt. Soc. Parasitol. 1993;23:723–735. [PubMed] [Google Scholar]
- 20.Eiger-Moscovich M., Amer R., Oray M., Tabbara K.F., Tugal-Tutkun I., Kramer M. Retinal artery occlusion due to Bartonella henselae infection: A case series. Acta Ophthalmol. 2016;94:e367–e370. doi: 10.1111/aos.12932. [DOI] [PubMed] [Google Scholar]
- 21.Otranto D., Dantas-Torres F., Breitschwerdt E.B. Managing canine vector-borne diseases of zoonotic concern: Part one. Trends Parasitol. 2009;25:157–163. doi: 10.1016/j.pt.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Iatta R., Sazmand A., Nguyen V.-L., Nemati F., Bahiraei Z., Mazhar Ayaz M., Giannico A., Dantas-Torres F., Otranto D. Vector-borne pathogens in dogs of different regions of Iran and Pakistan. Parasitol. Res. 2021 doi: 10.1007/s00436-020-06992-x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al–Obaidi S.S.A. Molecular detection of some anaplasma species in blood of dogs in Baghdad province, Iraq. Iraqi J. Vet. Med. 2020;44:39–45. doi: 10.30539/ijvm.v44i1.933. [DOI] [Google Scholar]
- 24.Aktas M., Özübek S., Altay K., Ipek N.D.S., Balkaya İ., Utuk A.E., Kırbas A., Şimsek S., Dumanlı N. Molecular detection of tick-borne rickettsial and protozoan pathogens in domestic dogs from Turkey. Parasit. Vectors. 2015;8:157. doi: 10.1186/s13071-015-0763-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zaid T., Ereqat S., Nasereddin A., Al-Jawabreh A., Abdelkader A., Abdeen Z. Molecular characterization of Anaplasma and Ehrlichia in ixodid ticks and reservoir hosts from Palestine: A pilot survey. Vet. Med. Sci. 2019;5:230–242. doi: 10.1002/vms3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alanazi A.D., Nguyen V.L., Alyousif M.S., Manoj R.R., Alouffi A.S., Donato R., Sazmand A., Mendoza-Roldan J.A., Dantas-Torres F., Otranto D. Ticks and associated pathogens in camels (Camelus dromedarius) from Riyadh Province, Saudi Arabia. Parasit. Vectors. 2020;13:110. doi: 10.1186/s13071-020-3973-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouzouraa T., René-Martellet M., Chêne J., Attipa C., Lebert I., Chalvet-Monfray K., Cadoré J.-L., Halos L., Chabanne L. Clinical and laboratory features of canine Anaplasma platys infection in 32 naturally infected dogs in the Mediterranean basin. Tick Tick-Borne Dis. 2016;7:1256–1264. doi: 10.1016/j.ttbdis.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Lima M., Soares P., Ramos C., Araújo F., Ramos R., Souza I., Faustino M., Alves L. Molecular detection of Anaplasma platys in a naturally-infected cat in Brazil. Brazil. J. Microbiol. 2010;41:381–385. doi: 10.1590/S1517-83822010000200019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Salakij C., Lertwatcharasarakul P., Salakij J., Nunklang K., Rattanakunuprakarn J. Molecular characterization of Anaplasma platys in a domestic cat from Thailand. Comp. Clin. Pathol. 2012;21:345–348. doi: 10.1007/s00580-011-1378-1. [DOI] [Google Scholar]
- 30.Sainz Á., Roura X., Miró G., Estrada-Peña A., Kohn B., Harrus S., Solano-Gallego L. Guideline for veterinary practitioners on canine ehrlichiosis and anaplasmosis in Europe. Parasit. Vectors. 2015;8:75. doi: 10.1186/s13071-015-0649-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Latrofa M.S., Dantas-Torres F., de Caprariis D., Cantacessi C., Capelli G., Lia R.P., Breitschwerdt E.B., Otranto D. Vertical transmission of Anaplasma platys and Leishmania infantum in dogs during the first half of gestation. Parasit. Vectors. 2016;9:269. doi: 10.1186/s13071-016-1545-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matei I., Stuen S., Modrý D., Degan A., D’Amico G., Mihalca A. Neonatal Anaplasma platys infection in puppies: Further evidence for possible vertical transmission. Vet. J. 2017;219:40–41. doi: 10.1016/j.tvjl.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 33.Sharifiyazdi H., Abbaszadeh Hasiri M., Radmanesh M. Development of RFLP-PCR and simple multiplex PCR assays for detection and differentiation of two species of hemotropic mycoplasmas in naturally infected dogs. Comp. Clin. Pathol. 2016;25:847–853. doi: 10.1007/s00580-016-2272-7. [DOI] [Google Scholar]
- 34.Vahedi S., Bolourchian M., Abolghasempour S., Mazaheri Nezhad Fard R., Akbarein H., Zahraei Salehi T., Aldavood S. Molecular characterization and phylogenetic analysis of feline hemotropic mycoplasmas. J. Fac. Vet. Med. Univ. Tehran. 2014;69:213–217. [Google Scholar]
- 35.Ghazisaeedi F., Atyabi N., Zahraei Salehi T., Ashrafi Tamai I., Tabatabaei S., Chegeni S. Molecular characterization and phylogenetic analysis of feline hemoplasmas in domestic cats in Iran. Vet. Res. Forum. 2017;8:67–73. [PMC free article] [PubMed] [Google Scholar]
- 36.Ghazisaeedi F., Atyabi N., Zahrai Salehi T., Gentilini F., Ashrafi Tamai I., Akbarein H., Tasker S. A molecular study of hemotropic mycoplasmas (hemoplasmas) in cats in Iran. Comp. Clin. Pathol. 2014;43:381–386. doi: 10.1111/vcp.12166. [DOI] [PubMed] [Google Scholar]
- 37.Torkan S., Aldavood S.J., Sekhavatmandi A., Moshkelani S. Detection of haemotropic Mycoplasma (Haemobartonella) using multiplex PCR and its relationship with epidemiological factors in dogs. Comp. Clin. Pathol. 2014;23:669–672. doi: 10.1007/s00580-012-1668-2. [DOI] [Google Scholar]
- 38.Ravagnan S., Carli E., Piseddu E., Da Rold G., Porcellato E., Zanardello C., Carminato A., Vascellari M., Capelli G. Prevalence and molecular characterization of canine and feline hemotropic mycoplasmas (hemoplasmas) in northern Italy. Parasit. Vectors. 2017;10:132. doi: 10.1186/s13071-017-2069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Willi B., Novacco M., Meli M.L., Wolf-Jäckel G.A., Boretti F.S., Wengi N., Lutz H., Hofmann-Lehmann R. Haemotropic mycoplasmas of cats and dogs: Transmission, diagnosis, prevalence and importance in Europe. Schweiz. Arch. Tierheilkd. 2010;152:237. doi: 10.1024/0036-7281/a000055. [DOI] [PubMed] [Google Scholar]
- 40.Maggi R.G., Compton S.M., Trull C.L., Mascarelli P.E., Mozayeni B.R., Breitschwerdt E.B. Infection with hemotropic Mycoplasma species in patients with or without extensive arthropod or animal contact. J. Clin. Microbiol. 2013;51:3237–3241. doi: 10.1128/JCM.01125-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maggi R.G., Mascarelli P.E., Havenga L.N., Naidoo V., Breitschwerdt E.B. Co-infection with Anaplasma platys, Bartonella henselae and Candidatus Mycoplasma haematoparvum in a veterinarian. Parasit. Vectors. 2013;6:103. doi: 10.1186/1756-3305-6-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oskouizadeh K., Zahraei-Salehi T., Aledavood S. Detection of Bartonella henselae in domestic cats’ saliva. Iran. J. Microbiol. 2010;2:80–84. [PMC free article] [PubMed] [Google Scholar]
- 43.Oskouizadeh K., Mahzounieh M., Ziaie B., Zahraei-Salehi T., Ashrafi-Tamaei I. Isolation and identification of Bartonella henselae from domestic cats in Shahrekord-Iran. Iran. Vet. J. 2011;7:5–12. [Google Scholar]
- 44.Mazaheri Nezhad Fard R., Vahedi S.M., Ashrafi I., Alipour F., Sharafi G., Akbarein H., Aldavood S.J. Molecular identification and phylogenic analysis of Bartonella henselae isolated from Iranian cats based on gltA gene. Vet. Res. Forum. 2016;7:69–72. [PMC free article] [PubMed] [Google Scholar]
- 45.Samsami S., Ghaemi M., Sharifiyazdi H. Molecular detection and phylogenetic analysis of ‘Candidatus Bartonella merieuxii’in dogs and its effect on hematologic parameters. Comp. Immunol. Microbiol. Infect. Dis. 2020;72:101504. doi: 10.1016/j.cimid.2020.101504. [DOI] [PubMed] [Google Scholar]
- 46.Switzer A.D., McMillan-Cole A.C., Kasten R.W., Stuckey M.J., Kass P.H., Chomel B.B. Bartonella and Toxoplasma infections in stray cats from Iraq. Am. J. Trop. Med. Hyg. 2013;89:1219–1224. doi: 10.4269/ajtmh.13-0353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chomel B.B., McMillan-Cole A.C., Kasten R.W., Stuckey M.J., Sato S., Maruyama S., Diniz P.P., Breitschwerdt E.B. Candidatus Bartonella merieuxii, a potential new zoonotic Bartonella species in canids from Iraq. PLoS Negl. Trop. Dis. 2012;6:e1843. doi: 10.1371/journal.pntd.0001843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kleynhans D.J., Sarli J., Hatyoka L.M., Alagaili A.N., Bennett N.C., Mohammed O.B., Bastos A.D. Molecular assessment of Bartonella in Gerbillus nanus from Saudi Arabia reveals high levels of prevalence, diversity and co-infection. Infect. Genet. Evol. 2018;65:244–250. doi: 10.1016/j.meegid.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 49.Alharbi B. Arthropod-Borne Infections in the United Kingdom and Saudi Arabia. University of Salford; Salford, UK: 2018. [Google Scholar]
- 50.Cheslock M.A., Embers M.E. Human bartonellosis: An underappreciated public health problem? Trop. Med. Infect. Dis. 2019;4:69. doi: 10.3390/tropicalmed4020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Azmi K., Al-Jawabreh A., Nasereddin A., Abdelkader A., Zaid T., Ereqat S., Sawalha S.S., Baneth G., Abdeen Z. Detection and molecular identification of Hepatozoon canis and Babesia vogeli from domestic dogs in Palestine. Parasitology. 2017;144:613–621. doi: 10.1017/S0031182016002201. [DOI] [PubMed] [Google Scholar]
- 52.Vilhena H., Martinez-Díaz V.L., Cardoso L., Vieira L., Altet L., Francino O., Pastor J., Silvestre-Ferreira A.C. Feline vector-borne pathogens in the north and centre of Portugal. Parasit. Vectors. 2013;6:99. doi: 10.1186/1756-3305-6-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sacchini F., Cessford R.J., Robinson B.M. Outbreak of canine monocytic ehrlichiosis in Saudi Arabia. Vet. Clin. Pathol. 2007;36:331–335. doi: 10.1111/j.1939-165X.2007.tb00436.x. [DOI] [PubMed] [Google Scholar]
- 54.Maazi N., Malmasi A., Shayan P., Nassiri S.M., Zahraei Salehi T., Sharifian Fard M. Molecular and serological detection of Ehrlichia canis in naturally exposed dogs in Iran: An analysis on associated risk factors. Rev. Bras. Parasitol. Vet. 2014;23:16–22. doi: 10.1590/S1984-29612014002. [DOI] [PubMed] [Google Scholar]
- 55.Alanazi A.D., Abdullah S., Helps C., Wall R., Puschendorf R., ALHarbi S.A., Abdel-Shafy S., Shaapan R.M. Tick-borne pathogens in ticks and blood samples collected from camels in Riyadh province, Saudi Arabia. Int. J. Zool. Res. 2018;14:30–36. [Google Scholar]
- 56.Calvani N.E., Bell L., Carney A., De La Fuente C., Stragliotto T., Tunstall M., Šlapeta J. The molecular identity of fleas (Siphonaptera) carrying Rickettsia felis, Bartonella clarridgeiae and Bartonella rochalimae from dogs and cats in Northern Laos. Heliyon. 2020;6:e04385. doi: 10.1016/j.heliyon.2020.e04385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Criado-Fornelio A., Martinez-Marcos A., Buling-Sarana A., Barba-Carretero J. Presence of Mycoplasma haemofelis, Mycoplasma haemominutum and piroplasmids in cats from southern Europe: A molecular study. Vet. Microbiol. 2003;93:307–317. doi: 10.1016/S0378-1135(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 58.Olmeda A., Armstrong P., Rosenthal B., Valladares B., Del Castillo A., De Armas F., Miguelez M., Gonzalez A., Rodrıguez J.R., Spielman A. A subtropical case of human babesiosis. Acta Tropica. 1997;67:229–234. doi: 10.1016/S0001-706X(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 59.Diaz M.H., Bai Y., Malania L., Winchell J.M., Kosoy M.Y. Development of a novel genus-specific real-time PCR assay for detection and differentiation of Bartonella species and genotypes. J. Clin. Microbiol. 2012;50:1645–1649. doi: 10.1128/JCM.06621-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article.