Abstract
Background: Existing standardized biofilm assays focus on simple mono-species or bacterial-only models. Incorporating Candida albicans into complex biofilm models can offer a more appropriate and relevant polymicrobial biofilm for the development of oral health products. Aims: This study aimed to assess the importance of interkingdom interactions in polymicrobial oral biofilm systems with or without C. albicans, and test how these models respond to oral therapeutic challenges in vitro. Materials and Methods: Polymicrobial biofilms (two models containing 5 and 10 bacterial species, respectively) were created in parallel in the presence and absence of C. albicans and challenged using clinically relevant antimicrobials. The metabolic profiles and biomasses of these complex biofilms were estimated using resazurin dye and crystal violet stain, respectively. Quantitative PCR was utilized to assess compositional changes in microbial load. Additional assays, for measurements of pH and lactate, were included to monitor fluctuations in virulence “biomarkers.” Results: An increased level of metabolic activity and biomass in the presence of C. albicans was observed. Bacterial load was increased by more than a factor of 10 in the presence of C. albicans. Assays showed inclusion of C. albicans impacted the biofilm virulence profiles. C. albicans did not affect the biofilms’ responses to the short-term incubations with different treatments. Conclusions: The interkingdom biofilms described herein are structurally robust and exhibit all the hallmarks of a reproducible model. To our knowledge, these data are the first to test the hypothesis that yeasts may act as potential “keystone” components of oral biofilms.
Keywords: fungal–bacterial interactions, oral biofilm, high-throughput, polymicrobial, antimicrobials, biofilm models
1. Introduction
Biofilms are an integral part of a healthy oral microbiome, with a diverse range of constituents [1]. In dysbiotic states, such as lowered pH or increased plaque accumulation leading to host inflammation, these biofilms can cause a range of diseases, from dental caries, a disease highly prevalent in children, to periodontal disease in adulthood and denture-related infections in the elderly [2]. It has been projected that 90% of the population will need some form of disease intervention in the oral cavity throughout their life, and the World Health Organization defines oral diseases as the most common preventable disease burden worldwide [3,4,5]. This extensive and preventable occurrence of oral diseases highlights the need for further research and accurate clinical treatments for their prevention.
A wide range of bacterial colonizers have been confirmed within a healthy oral cavity through advanced molecular techniques such as next generation sequencing. From such studies, a number of key bacterial genera appear to be conserved amongst individuals, including Streptococcus, Veillonella, Granulicatella, Actinomyces, Fusobacterium and various anaerobic bacteria [6,7,8]. In addition, Candida and other fungal species have also been identified as colonizers in studies focusing on the mycobiome in the oral cavity [9,10,11,12]. Indeed, it is well documented that at mucosal surfaces, C. albicans has the ability to act as a symbiont in healthy individuals, transitioning to a pathobiont or dysbiotic entity in certain hosts under some conditions [13,14]. This is similarly the case for the oral cavity [15,16,17], whereby C. albicans is commonly associated with known constituents of the oral microbiome in both healthy and diseased individuals [18,19,20,21]. Despite this confirmation, many studies lack a crucial fungal element within in vitro biofilm testing, leading to unrealistic challenges of models designed for the oral cavity [22,23,24]. This lack of interkingdom polymicrobiality limits the advancement and improvement of commercial biofilm testing of novel agents in vitro.
As discussed above, studies have confirmed the presence of numerous fungal species within oral biofilms; however, their role is still disputed. Common commensal plaque constituents, such as Streptococcus and Actinomyces species, have been shown to grow synergistically with C. albicans, increasing biofilm production [25,26]. While this may indicate an increase in pathogenicity when Candida is present within plaque, strengthened by known interactions with periodontal pathogen Porphyomonas gingivalis (for example, [21]), C. albicans has been identified in healthy individuals, suggestive the organism possesses a symbiotic phenotype [9]. Indeed, the ability of C. albicans to shift from a “commensal state” as a yeast cell to a “pathogenic” hyphae-forming phenotype under certain conditions also impacts its invasiveness at mucosal sites such as the oral cavity [27,28]. Alternatively, antagonistic interkingdom interactions have also been described whereby pathogens such as Fusobacterium nucleatum can inhibit of hyphae formation in C. albicans, which leads to reduced virulence attributes of both organisms [29]. From this, it is evident that the interkingdom interactions in the oral cavity can both be beneficial or detrimental to the oral micro- and/or mycobiomes.
Clear evidence suggests that bacteria such as P. gingivalis can act as “keystone pathogens” in periodontitis [30]. However, Janus and colleagues (2016) have proposed that C. albicans acts as a “keystone commensal” given its close interactions with “health-associated” bacteria, offering a scaffold effect and influence on the local environment within the biofilm through pH buffering [15]. C. albicans has been found within and implicated in all aspects of oral disease from caries, periodontitis and denture stomatitis. Close association with Streptococcus mutans in caries patients has caused researchers to link Candida to a more severe cariogenic lesion in children [31]. Similarly, Candida spp. have been heavily implicated in soft tissue infections, such as denture stomatitis and periodontitis with its ability to adhere to and invade epithelial cells [32,33]. These implications may be substantial; however, the presence of C. albicans alone does not indicate disease, and so environmental factors are likely significant. The “ecological plaque hypothesis” focuses upon the relationships between the organisms present and the environment within the oral cavity, with disease occurring upon a dysbiotic “event” [34]. Therefore, physiological interventions alongside microbial control may offer beneficial therapeutics [35]. Ultimately, this may indicate that a role for C. albicans in health and disease is more closely linked to the interactions and overall environment of the oral cavity, as opposed to fungal burden leading to disease. Thus, including C. albicans in in vitro model systems is essential to truly understanding interkingdom relationships within these polymicrobial biofilms.
One aim of this study was to determine whether the inclusion of C. albicans within two oral models, a hard-tissue and soft-tissue biofilm, leads to changes in biofilm “profiles” and/or pathogenic “signatures.” Specifically, biomass quantification, metabolic profile, composition and ultrastructure of the biofilms were assessed with or without C. albicans. Secondly, an aim was to investigate whether inclusion of this organism will impact the biofilms’ responses to conventional therapeutics. To the authors knowledge, this is the first study to assess the importance of including a fungus in such in vitro systems to model interkingdom oral biofilms and in particular test the “keystone commensal” hypothesis postulated by Janus et al. (2016) previously [15]. Moving forward, results from this study will hopefully inform us of the importance of mimicking fungal–bacterial interactions in vitro for antimicrobial testing, particularly in a commercial setting.
2. Materials and Methods
All biofilm studies reported in this work were carried out in accordance with the minimum information guidelines specified for biofilm formation in microplates [36].
2.1. Growth and Standardization of Bacteria
The biofilm models used within this study have previously been published by the research group [24,37,38]. These models were created to encompass the well-documented main etiological agents of the oral diseases they are based upon [39,40]. To highlight the natural evolution of disease, sequential addition of the organisms was employed. Initial colonizers were used to attach to the surface of the plate; intermediate colonizers allowed bridging between organisms; pathogenic colonizers were added as a final stage of disease [41].
All pure culture organisms were stored prior to use in Microbank™ beads (Pro-lab Diagnostics, Birkenhead, UK) at −80 °C. Prior to culture preparation, organisms were revived from frozen stocks as follows: Streptococcus mitis NCTC 12261, Streptococcus intermedius ATCC 27335, Streptococcus oralis ATCC 35037, Streptococcus mutans ATCC 25,175 and Aggregatibacter actinomycetemcomitans DSMZ 1123 were grown and maintained at 37 °C 5% CO2 on Colombia blood agar (CBA (Oxoid, Basingstoke, UK)). C. albicans 3153A was maintained on Sabouraud’s dextrose agar (Oxoid, UK) at 30 °C under aerobic conditions for 48 h. Fusobacterium nucleatum ATCC 1096, F. nucleatum ssp. vincentii ATCC 49256, Actinomyces naeslundii ATCC 19039, Veillonella dispar ATCC 27335, Prevotella intermedia ATCC 25,611 and Porphyromonas gingivalis W83 were maintained at 37 °C on fastidious anaerobic agar (FAA (Lab M, Bury, UK)) in an anaerobic chamber (Don Whitley Scientific Limited, Bingley, UK) with an atmosphere of 85% N2, 10% CO2 and 5% H2 for 48 h or 72 h for strict anaerobes. All media and agar to be used for anaerobes were deoxygenated for 24 h prior to use. Lactobacillus casei DSMZ 20,011 was grown and maintained on MRS agar (Oxoid, UK) in 37 °C 5% CO2. Aerobic organisms were then stored at 4 °C for a maximum of 2 weeks prior to propagation, while anaerobic organisms were stored within the anaerobic chamber for 1 week prior to being re-streaked.
Culture broths for propagation were prepared as follows: Overnight (16–18 h) broths of S. mitis, S. intermedius, S. oralis, S. mutans and A. actinomycetemcomitans were grown statically in 10 mL tryptic soy broth (TSB, Sigma-Aldrich, Gillingham, UK) at 37 °C 5% CO2. C. albicans was grown for 16–18 h in 10 mL yeast peptone dextrose (YPD, Sigma-Aldrich, UK) at 30 °C in an orbital benchtop shaker at 200 rpm, 20 mm orbital diameter (IKA KS 4000 I control, IKA®-Werke GmbH & Co., Staufen, Germany). P. gingivalis, F. nucleatum and F. nucleatum ssp. vincentii were propagated in 10 mL deoxygenated Schaedlers anaerobic broth (Oxoid, UK). V. dispar, A. naeslundii, and P. intermedia were grown in 10 mL of brain heart infusion broth, (BHI, Sigma-Aldrich, UK) in anaerobic chamber 37 °C, 85% N2, 10% CO2 and 5% H2. L. casei was grown in 10 mL of MRS broth (Oxoid, UK), 37 °C, 5% CO2. Anaerobic cultures were grown for 48 h as necessary, then pelleted by centrifugation (VWR megastar 1.6R, VWR International GmbH. Darmstadt, Germany (3000× g)). Pellets were then washed via resuspension twice in phosphate buffered saline (PBS, Sigma-Aldrich, UK). Following washing the cells were standardized to 1 × 108 cells/mL using a spectrophotometer for bacteria and via haemocytometer counting for Candida (cell count × dilution factor × volume of square = colony forming unit [CFU/mL). Previously, to determining accurate absorbance readings at 550 nm that equate to 1 × 108 cells/mL for the bacteria, the Miles and Misra colony counting technique was employed [42] by serially diluting pure colonies to determine the correct absorbance per organism. Streptococcus spp., V. dispar and L. casei were read at an OD of 0.5. A. naeslundii, F. nucleatum, F. nucleatum ssp. vincentii, P. gingivalis, P. intermedia and A. actinomycetemcomitans were read at an OD of 0.2.
2.2. Development of Multi-Species Biofilms
Bacteria and fungi were standardized (1 × 107 CFU/mL) in an equal volume of Roswell Park Memorial Institute-1640 (RPMI) with Todd Hewitt Broth (THB) supplemented with 0.01 mg/mL hemin and 0.2 µL/mL (2 µg/mL) menadione in a similar manner as previously described [43]. These preparations were generated by diluting bacteria 10× after the initial standardization following washing and diluting to appropriate OD. Candida dilution was carried out using the CFU/mL calculated previously and applying the C1V1 = C2V2 calculation. Biofilms formed to create the oral biofilm models were grown directly in a clear flat bottomed 96 well polystyrene plate (Corning, New York, US) using a 200 µL inoculation volume unless stated otherwise. Medium was replaced every 24 h using a multichannel pipette, carefully at a 45° angle and at the same point within the plate (bottom left of the well) to limit unnecessary disruption of the biofilm.
2.3. Hard Tissue (HT)—Caries Associated Biofilm
Initial pioneer species C. albicans and S. mutans were standardized together within an RPMI/THB aliquot and matured in 96 well flat bottom plates using 200 µL per well for 24 h in 5% CO2. The supernatant was then removed as described above and an RPMI/THB aliquot containing a mixture of standardized F. nucleatum, A. naeslundii, V. dispar and L. casei was added and incubated in the same conditions for 4 days. RPMI/THB medium was replaced daily to produce a 6-species biofilm. The supernatant was then removed, and biofilms were ready to be used for downstream experiments. In biofilms omitting Candida, the same sequential addition was used minus C. albicans in the initial step.
2.4. Soft Tissue (ST)—Periodontitis/Denture Stomatitis Associated Biofilm
Initial pioneer species C. albicans, S. oralis, S. mitis and S. intermedius were standardized together in an RPMI/THB aliquot and matured in 96 well flat bottom plates using 200 µL per well for 24 h in 5% CO2 The supernatant was removed as described above and an RPMI/THB aliquot containing a mixture of standardized F. nucleatum, F. nucleatum ssp vincentii, A. naeslundii and V. dispar was added and incubated in an anaerobic cabinet (85% N2, 10% CO2, 5% H2, (Don Whitley Scientific Limited, UK)) for 24 h. The supernatant was again removed and a deoxygenated RPMI/THB aliquot containing standardized P. gingivalis, P. intermedia, and A. actinomycetemcomitans added in an anaerobic cabinet. The medium was replaced daily for 4 days to produce an 11 species biofilm. The supernatant was then removed, and biofilms were ready to be used for downstream experiments. As above, in biofilms omitting Candida, the same sequential addition was used minus C. albicans in the initial step.
2.5. Testing of Oral Models
To establish the importance of incorporating C. albicans into the biofilms, assessment of metabolic testing alongside biomass determination was carried out. Additionally, qPCR was utilized to assess changes in bacterial load and composition. Scanning electron microscopy was also used to determine architectural differences. Changes in pathogenesis were also estimated by measuring fluctuations in pH, reactive oxygen species (ROS) and enzyme levels. To further define the differences in the biofilms with or without C. albicans, models were subjected to treatment as described below.
2.6. Metabolic Analysis of Oral Biofilms
Biofilms were analyzed for metabolic activity using alamarBlue™ cell viability dye (Invitrogen, Inchinnan, UK). Once matured or after treatment and neutralization, alamarBlue™ was added at 10% well volume in RPMI/THB (e.g., 20 µL per 200 µL RPMI/THB) using a multichannel pipette in dark conditions. Plates were then incubated at 37 °C 5% CO2, with a change from blue to pink indicative of a reduction in the fluorogenic dye resazurin to resorufin by enzymes involved in normal cellular respiration. The color change was read when the growth control reached a bright pink color to allow this to be used as a positive control or the latest after 3 h, depending on which occurred first. 100 µL from each well was transferred to a fresh 96 well flat bottom microtiter plate and top read using fluorescence 530/590 nm (FLOUstar™, BMG lab tech, Aylesbury, UK). A negative sterility control was also used on the same plate whereby no biofilm growth was initiated to use as a blank to normalize the fluorescence by an average of this value. In cases of treatment, a positive growth control (e.g., minus treatment) was included as a 100% growth value, to allow metabolic activity to be calculated as a percentage based on this growth control. All experiments assessing metabolic activity were completed using biofilms in triplicate or quadruplicate on three separate occasions.
2.7. Assessment of Oral Biofilms Biomass
The biomass of the biofilms were quantified using a crystal violet stain. Post metabolic assessment, spent cell viability dye was removed carefully with the pipette tip placed at the bottom left of the well, then biofilms were washed once with PBS and airdried overnight at RT. A stock solution of 1% crystal violet (CV) (Sigma-Aldrich, UK) was made using ddH2O and diluted to 0.05% for use. A total of 100 µL of 0.05% CV solution was added to each well and incubated at RT for 30 min. CV was then removed using a multichannel pipette, and biofilms washed twice using ddH2O removing excess dye. To limit unnecessary disruption of the biofilm, the wash steps were achieved by placing the pipette tip at 45º angle at the same point within the plate (bottom left of the well). Following wash steps, a volume of 100 µL of 100% ethanol was used to de-stain the biofilm; following addition to the biofilms (at the same point within the plate as above e.g., bottom left of the well), this suspension was mixed well with a pipette five times and 75 µL transferred to a fresh 96 well flat bottom microtiter plate for measurement. Biomass was quantified by reading absorbance at 570 nm (FLOUstar™, BMG lab tech, UK). A negative sterility control was also used on the same plate whereby no biofilm growth was initiated to use as a blank to normalize the absorbance by an average of this value. In cases of treatment, a positive growth control was included, to be used as an untreated comparison. All experiments assessing biomass were completed using biofilms in triplicate or quadruplicate on three separate occasions.
2.8. Quantitative Analysis of Biofilm Composition
Real-time quantitative PCR (qPCR) was performed to enumerate the relative composition of the biofilms. Briefly, bacterial biofilms were removed by using a pipette tip in 150 µL PBS to detach the cells from the 96-well plate and added to 850 µL PBS for further use. Initially, following removal of these biofilms using the pipette, a plate was stained with CV to ensure no biomass remained. Indeed, using this methodology, minimal biomass remained on the plate after removal. The homogenized suspension was then used for DNA extraction using the QIAamp DNA Mini Kit (Qiagen, Manchester, UK), following manufacturer’s instructions. Following on from this, 1 μL of extracted DNA was added to a mastermix containing 10 μL SYBR® GreenER™, 7 μL UV-treated RNase-free water and 1 μL of 10 μM forward/reverse primers for each bacterial genus or species. The primers used were previously published, as listed elsewhere [24,38], and are shown in Table 1. Three independent replicates from each parameter were analysed in duplicate using StepOnePlus Real-Time PCR system and StepOnePlus software (ThermoFisher, Loughborough, UK). PCR thermal profiles were as follows, holding stage at 50 °C for 2 min, followed by denaturation stage at 95 °C for 5 min and then 40 cycles of 95 °C for 3 s and 60 °C for 30 s. Samples were quantified to calculate the colony forming equivalent (CFE) based upon a previously established standard curve of bacterial colony forming units ranging from 1 × 103 to 108 CFU/mL. The R2 values for these standard curves ranged from 0.984 to 0.997. All samples from each triplicate experiment were run in duplicate within the qPCR plate and used as a mean to limit fluorescence variation. Two duplicate control samples containing mastermix only were used to assess for contamination.
Table 1.
Primers used in the study.
| Primer | Sequence (5′-3′) | References |
|---|---|---|
| A. actinomycetemcomitans | F-GAACCTTACCTACTCTTGACATCCGAA R-TGCAGCACCTGTCTCAAAGC |
[44] |
| A. naeslundii | F-GGCTGCGATACCGTGAGG R-TCTGCGATTACTAGCGACTCC |
[45] |
| C. albicans | F- CTCGTAGTTGAACCTTGGGC R- GGCCTGCTTTGAACACTCTA |
[38] |
| F. nucleatum spp. | F-GGATTTATTGGGCGTAAAGC R-GGCATTCCTACAAATATCTACGAA |
[46] |
| P. intermedia | F-CGGTCTGTTAAGCGTGTTGTG R-CACCATGAATTCCGCATACG |
[44] |
| P. gingivalis | F-GGAAGAGAAGACCGTAGCACAAGGA R-GAGTAGGCGAAACGTCCATCAGGTC |
[47] |
| Streptococcus spp. | F-GATACATAGCCGACCTGAG R-CCATTGCCGAAGATTCC |
[46] |
| V. dispar | F-CCGTGATGGGATGGAAACTGC R-CCTTCGCCACTGGTGTTCTTC |
[48] |
| L. casei | F-TGCACTGAGATTCGACTTAA R-CCCACTGCTGCCTCCCGTAGGAGT |
[49] |
| 16S | F-CGCTAGTAATCGTGGATCAGAATG R-TGTGACGGGCGGTGTGTA |
[50] |
| 18S | F-CTCGTAGTTGAACCTTGGGC R-GGCCTGCTTTGAACACTCTA |
[51] |
2.9. Visualization of Oral Biofilms
Scanning electron microscopy (SEM) was performed on intact biofilms grown on 13mm2 coverslips (Thermofisher, UK). Following maturation and treatment, biofilms were washed three times with PBS with the pipette tip placed in the bottom left of the well to avoid disruption of the biofilm. Following washing, fixative solution was then added to the biofilms containing 2% paraformaldehyde, 2% glutaraldehyde, 0.15 M sodium cacodylate and 0.15% w/v alcian blue (pH 7.4) and fixed overnight. A 0.15 M sodium cacodylate buffer was then used as a storage buffer and samples kept at 4 °C until processing. SEM processing of biofilm samples followed a series of fixation and dehydration steps preceding a final gold sputter coating allowing visualization as described elsewhere [52]. Briefly, samples were washed 3 × 5 min with 0.15 M sodium cacodylate to ensure glutaraldehyde removal. Samples were then treated with 1% osmium tetroxide solution containing 0.15 M sodium cacodylate (1:1) and incubated in a fume hood for 1 h. Samples were rinsed 3 × 10 min with distilled water and then treated with 0.5% uranyl acetate and incubated in the dark for 1 h. Uranyl acetate was removed from the samples and rinsed with water before a series of dehydration steps were carried out. 2 × 5 min rinses of 30, 50, 70 and 90% alcohol were followed by 4 × 10 min rinses of absolute and dried absolute alcohol. Critical point drying was then undertaken by soaking the biofilms in hexamethyldisilazane for 2 × 5 min rinses. Samples were then placed in a desiccator overnight to allow samples to be thoroughly dried. The specimens were then mounted and sputter-coated with gold in an argon filled chamber, and then viewed under a JEOL JSM-6400 scanning electron microscope.
2.10. Assays to Assess Pathogenicity of the Oral Biofilms
Supernatants were collected from the biofilms on the final day of growth, centrifuged in microcentrifuge tubes at 8000× g for 5 min. Aliquots of the supernatant were used fresh for pH testing (FiveEasy meter and InLab® micro (Mettler Toledo, Columbus, OH, USA)) and the remainder frozen at −80 °C until further use for remaining assays. Biofilms were tested using lactate assay kit as per kit instructions (Sigma-Aldrich, UK). Briefly, 20 µL of sample was mixed with a master mix (1:1) consisting of assay buffer, enzyme mix and lactate probe in a 23:1:1 ratio. A standard curve was also prepared. Mixture was incubated in the dark for 15 min at room temperature and read at 570 nm (FLOUstar™, BMG Labtech, UK). ROS assessment was carried out using a superoxide determination kit as per manufacturers instruction, with the exception of incubation time (Sigma-Aldrich, UK). Briefly, 20 µL of sample was added to a 96-well microtiter plate and mixed with 200 µL of diluted WST working solution and 20 µL of diluted enzyme working solution. This was then incubated at 37 °C for 24 h and absorbance read at 450 nm (FLOUstar™, BMG Labtech, UK). Appropriate blanks were used according to instruction of the kit. Each replicate sample were run in duplicate. Superoxide dismutase enzyme from Escherichia coli (Sigma-Aldrich, UK) was used to achieve an inhibition standard curve to allow units/mL to be calculated from percentage inhibition. Protease release was determined using a protease fluorescent detection kit following manufacturer’s instructions (Sigma-Aldrich, UK). In a microcentrifuge tube, 10 µL of each sample was used neat and mixed with 20 µL of incubation buffer and 20 µL of fluorescent labelled casein and incubated for 1 h at 37 °C in the dark. A total of 150 µL of 0.6N Trichloroacetic acid solution was then added and mixed to precipitate larger fragments which have not been cleaved. After incubation at 37 °C for 30 min in the dark, the tubes were centrifuged for 10 min at 3000× g. The supernatant was transferred to a black 96-well microtiter plate and read as a fluorescent measurement at 485/535 nm, excitation/emission (FLOUstar™, BMG Labtech, UK). Serine protease trypsin was used as a control to generate a standard curve and negative controls used as appropriate.
2.11. Treatment of Oral Biofilms
To determine if the inclusion of C. albicans affected the susceptibility or tolerance of the oral biofilms to treatment, a range of both therapeutic challenges were used. The following concentrations and treatment preparations were used; 0.2% chlorhexidine gluconate (CHX, (Sigma-Aldrich, UK)) was used to mimic standard daily mouth-washing as a gold standard used within the dentistry industry and was used to mimic standard daily mouth washing [53], 4% Ethylenediaminetetraacetic acid (EDTA, (Sigma-Aldrich, UK)) a commonly used irrigant in endodontic treatments was used [54]. Potassium iodine at 1% served to mimic disinfection protocols in dentistry procedures [55]. Miconazole, an ergosterol inhibitor and anti-fungal agent was used at a concentration of 40 µg/mL based on previous studies [56]. All solutions were prepared fresh in sterile H2O prior to experimental use.
For the treatment studies, biofilms were grown in 96-well microtiter plates then washed three times to remove non-adherent cells as above. A total of 200 µL of testing compound was pipetted onto the biofilms at a 45° at the side of the well to avoid any disturbance to the biofilm. Biofilms were incubated at room temperature for 10 min. This incubation time was selected so that it partially mimicked the short treatment for oral health products, but long enough to ensure efficient action of the therapeutics, especially since this model utilized a static system (e.g., without combinative physical debridement). Following incubation, treatments were neutralized using 200 µL Dey Engley neutralizing broth (Sigma-Aldrich, UK) for 15 min and then washed once more with PBS using the same procedure as discussed above. A total of four wells within the microtiter plate were then used for metabolic analysis and biomass determination per experiment, while three others were used solely for biomass removal and DNA extraction for qPCR analyses. All experiments assessing metabolic activity were completed using biofilms in triplicate or quadruplicate on three separate occasions.
2.12. Statistical Analysis and Data Presentation
Graph production, data distribution and statistical analysis were performed using GraphPad Prism (version 8; La Jolla, CA, USA). After assessing whether data conformed to a normal distribution, unpaired Mann–Whitney t tests were used to investigate significant differences between independent groups of data. A Kruskal-Wallis was carried out with Dunn’s post-test analysis to assess differences between biofilms under treatment. Statistical significance was achieved upon p < 0.05.
3. Results
3.1. Metabolic, Biomass and Compositional Profiles of Oral Biofilm Models with or without C. albicans
Multi-species biofilms were grown in parallel in the presence or absence of C. albicans to determine the change to the overall metabolic rate and biomass of biofilms following incorporation of Candida (Figure 1). The results indicate that both metabolic activity and biomass were significantly increased upon the inclusion of C. albicans in both hard (HT) and soft tissue (ST) biofilms (p < 0.001). The fluorescence readings illustrating metabolic activity showed that HT biofilms increased by 2.8-fold, the mean output reading went from ~16,000 to ~45,000 Au (Figure 1A). Meanwhile, ST biofilms showed a 1.8-fold increase in metabolic activity when C. albicans was present, increasing from ~27,000 to ~50,000 Au. In a similar trend, the biomasses of the oral biofilm models were also significantly increased when Candida was included; HT biofilms increased almost 4-fold from an average O.D. of ~0.5 to ~2.0; and ST associated biofilm increased from ~0.8 O.D. to ~2.0, a 2.5-fold increase (Figure 1B). Overall, this data highlighted a thicker biofilm which is more metabolically active when C. albicans was present, in both models tested.
Figure 1.
Metabolic and biomass profiles of hard tissue (HT) and soft tissue (ST) biofilms plus or minus Candida albicans. Biofilms were grown in 96 well microtiter plates. Metabolic activity (A) was assessed using Alamar blue™ rezasurin dye to determine respiration rates, and biomass (B) was assessed using crystal violet as a disclosing stain to interpret differences in biofilm formation. Biofilms were grown and assayed in triplicate or quadruplicate on three separate occasions (a total of n = 11 biofilms from three separate experiments). Data represented as mean ± SD. Statistical analysis performed using an unpaired Mann–Whitney t-test to compare differences in mean (*** p < 0.001).
Crystal violet staining is unable to differentiate between cell numbers and composition and is just an overall estimate of the biomass of all components (cells, eDNA and extracellular matrix). Therefore, quantitative PCR was used to determine bacterial and fungal load using 16S and 18S primers (Figure 2A). Additionally, genus and species-specific primers detailed in Table 1 were also used to calculate overall percentage composition in HT (Figure 2B) and ST biofilms (Figure 2C). Results show that bacterial load was increased in both HT and ST biofilm models when C. albicans was present (both p < 0.001). A significant increase of more than one log was seen in the HT biofilm, ~6.0 × 107 CFE/mL, which increased to ~1.5 × 109 CFE/mL when C. albicans was included. Similarly, an increase from ~1.8 × 108 to ~9.0 × 108 CFE/mL was observed in ST-associated biofilms. The fungal load present in each of the biofilms was also assessed. Results showed that ~4.4 × 107 CFE/mL and ~6.2 × 106 CFE/mL of C. albicans were detected in HT and ST, respectively.
Figure 2.
Bacterial load of hard tissue (HT) and soft tissue (ST) biofilms in the presence or absence C. albicans. Following growth and removal from the microtiter plate, DNA was extracted using the QIAamp DNA Mini Kit, and bacterial load assessed using 16s PCR. Fungal load was also determined using 18s PCR. The total bacterial load is shown in white bars for hard tissue and grey shaded bars for soft tissue (A). The 18s fungal counts were 4.4 × 107 and 6.2 × 106 CFE/mL for HT and ST biofilms, respectively. Further compositional analysis was carried out using species specific primers, as described in Table 1. HT biofilm composition is shown in (B) and ST biofilm composition represented in (C). Data represented as mean ± SD; n = 3 in three independent experiments. A Mann–Whitney t test was carried out to assess differences between means of bacterial load in biofilms containing C. albicans compared to without (*** p < 0.001).
Following on from total bacterial load assessment, compositional analysis of the biofilms was done. In the HT biofilm, Figure 2B, the key change associated with the inclusion of C. albicans was the reduction of S. mutans from ~43.1% in biofilms without C. albicans, to ~29.0% in biofilms with C. albicans. However, this compositional change was not due to a reduction in microbial burden of S. mutans, which increased from 7.12 × 106 to 1.04 × 108 CFE/mL. A. naeslundii and L. casei also reduced in proportion, following inclusion of C. albicans, decreasing from ~7.8% to ~1.2%, and ~0.01% to ~0.001%, respectively. Again, this reduction was not associated with reduced numbers of this organisms (1.29 × 106 compared to 4.25 × 106 with C. albicans for A. naeslundii and 1.99 × 103 vs. 4.19 × 103 plus C. albicans for L. casei). All mean CFE/mL and compositional changes are documented in Table 2.
Table 2.
Mean colony forming equivalent per mL and average percentage composition for each genus or species in the hard and soft tissue biofilms. CFE/mL and percentage composition shown for each genus or species as an average of 9 independent biofilms (n = 3 from 3 separate experiments). All numbers shown in the table have been rounded to the first significant decimal place, where possible.
| Genus or Species |
Mean CFE/mL and Percentage Composition (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Hard Tissue | Soft Tissue | |||||||
| − C. albicans | + C. albicans | − C. albicans | + C. albicans | |||||
| CFE/mL | % | CFE/mL | % | CFE/mL | % | CFE/mL | % | |
| C. a | n/a | n/a | 4.60 × 107 | 12.81 | n/a | n/a | 6.08 × 106 | 4.00 |
| Strep | 7.12 × 106 | 43.10 | 1.04 × 108 | 29.00 | 2.87 × 106 | 14.40 | 4.96 × 106 | 3.26 |
| A. n | 1.29 × 106 | 7.82 | 4.25 × 106 | 1.18 | 9.50 × 105 | 4.76 | 2.36 × 106 | 1.55 |
| V. d | 8.10 × 106 | 49.05 | 2.03 × 108 | 56.63 | 1.58 × 107 | 79.27 | 1.36 × 108 | 89.87 |
| F. n | 2.91 × 103 | 0.02 | 1.38 × 106 | 0.38 | 2.80 × 103 | 0.014 | 5.12 × 103 | 0.05 |
| L. c | 1.99 × 103 | 0.01 | 4.19 × 103 | 0.001 | n/a | n/a | n/a | n/a |
| P. g | n/a | n/a | n/a | n/a | 1.23 × 102 | 0.001 | 1.74 × 104 | 0.011 |
| P. i | n/a | n/a | n/a | n/a | 5.49 × 102 | 0.003 | 5.12 × 103 | 0.003 |
| A. a | n/a | n/a | n/a | n/a | 3.11 × 105 | 1.56 | 1.90 × 106 | 1.25 |
Within the ST biofilm (Figure 2C), all bacterial genus or species increased in CFE/mL in the presence of C. albicans. Compositionally, V. dispar and Streptococci species (S. mitis, S. oralis and S. intermedius) remained the main constituents of the biofilm after the inclusion of C. albicans, although a reduction in the proportion of Streptococcus species was seen (~79.3% compared to ~89.9%, for V. dispar, and ~14.40% compared to ~3.26%, for Streptococci, respectively). Meanwhile, A. naeslundii (~4.76% to ~1.55%) and A. actinomycetemcomitans (~1.56% to ~1.25%) were both reduced in proportion following addition of C. albicans. The Socransky red complex constituent of P. gingivalis was present at low quantities, as expected in a periodontal biofilm [40]. with the organism increasing ten-fold in proportion and 100-fold in concentration after the addition of C. albicans (0.001% and 1.23 × 102 CFE/mL in bacterial-only biofilms, compared to 0.011% and 1.74 × 104 CFE/mL for Candida-containing biofilms, respectively). The bridging organism F. nucleatum also showed an increase from ~0.01% to ~0.05% in the presence of C. albicans, including a ~2-fold increase in bacterial numbers (2.80 × 103 compared to 5.12 × 103 CFE/mL). All CFE/mL and % changes are shown in Table 2. Overall, the results indicated that addition of C. albicans to the biofilm increased the bacterial load in both oral biofilm models. Changes associated with the composition showed a more diverse biofilm in HT biofilm, whilst ST biofilms were still dominated by V. dispar and Streptococcus spp. An increase in the periodontal pathogens such as F. nucleatum and P. gingivalis in the ST biofilms indicate a more diverse consortium with the inclusion of C. albicans.
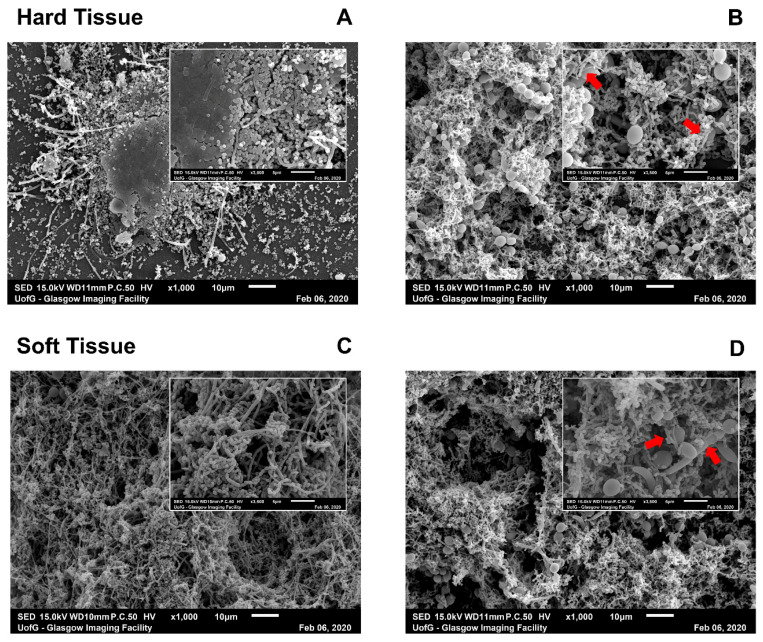
3.2. Scanning Electron Microscopy Visualization of Oral Biofilm Models with or without C. albicans
Next, the ultrastructures of the oral biofilm models were assessed using scanning electron microscopy (SEM). SEM imaging highlighted the change in architecture, particularly in HT biofilms wherein C. albicans was included (Figure 3). In HT biofilms without C. albicans (Figure 3A), the cells were clustered into complexes that were spaced out across the coverslip, in stark contrast to the network of cells and ECM within HT biofilms, including a fungal element (Figure 3B). ST biofilms (Figure 3C) demonstrated a complex and dense biofilm without the addition of C. albicans. Although it is clear from the bacterial load that there was still a small increase in bacterial numbers (as shown in Figure 2A), SEM pictures were comparable between the biofilms plus or minus C. albicans for the ST biofilms (Figure 3C,D). Nevertheless, there were clear physical interactions between the microbiota and the yeast and/or hyphae of the C. albicans in both models (indicated by the red arrows in the insets of Figure 3B,D).
Figure 3.
SEM images of hard tissue (HT) and soft tissue (ST) biofilms with or without C. albicans. Biofilms were processed after maturation and viewed on a JEOL JSM-6400 scanning electron microscope. Images were captured at ×1000 magnification (main image) and ×3500 magnification (inset). HT (A,B) and ST biofilms (C,D) were imaged without (A,C) and with C. albicans (B,D). Red arrows in insets of Candida-containing biofilms indicated visible attachment of bacterial cells with fungal hyphae or yeast cells. Images chosen were representative of duplicate samples.
3.3. Change in Pathogenic Biomarkers in Oral Biofilm Models in the Presence and Absence of C. albicans
Next, a range of biomarkers for virulence were assessed to determine if fungal addition to the oral biofilm models altered the pathogenicity of the biofilms. The pHs of the oral cavity and saliva have been established as markers for disease [57,58], whilst ROS and protease production may be linked to toxic metabolites and virulence [59,60]. Therefore, these markers were assessed in the two biofilm models (Figure 4). The pHs of both biofilm supernatants were significantly increased to a more neutral value in the presence of C. albicans (Figure 4A). HT biofilm supernatants had an average pH value of 5.8, which increased to 7.4 and ST biofilm supernatants increased by 1.5 units to a pH of 6.5 following inclusion of C. albicans. This was suggestive that the presence of a fungal element acts as a buffer to increase the environmental pH, which is in line with previous observations for C. albicans [61]. To corroborate these observations in pH measurements, lactate concentration was also determined. The modulation of lactate production by the microbial consortia is a common mechanism to generate acidic environments, which is likely occurring in the cariogenic HT biofilm. Results from Figure 4B demonstrate that in both HT and ST biofilms, C. albicans reduced lactate content in the supernatant collected from the biofilms. A 2-fold reduction was noted from HT biofilms, while a 14-fold decrease was apparent in ST biofilms following addition of C. albicans.
Figure 4.
Assessment of functional biomarkers in hard tissue (HT) and soft tissue (ST) biofilms with or without C. albicans. Supernatants were collected on the final day of maturation and stored at −80° C until required. Prior to freezing, pH was tested using a microprobe (A). Lactate assay kit was used to determine lactate content (B). Superoxide dismutase assay was carried out using WST-1 tetrazolium salt and xanthine as per assay instructions with a 100× sample dilution applied (C). Protease activity was assessed using a fluorescent protease detection kit. Trypsin was used as a standard curve as per manufacturer’s instructions (D). Data represented as mean ± SD, sampled in triplicate from three independent experiments. A Mann–Whitney t-test was used throughout to assess significant differences between the means of models with or without C. albicans (*** p < 0.001).
ROS within the oral cavity can be a marker for inflammation and cell damage [62], and therefore the activity of enzyme superoxide dismutase was determined in the biofilm supernatants. Interestingly, in HT biofilms, Candida decreased superoxide dismutase activity 5-fold, whilst conversely, the presence of C. albicans increased the activity in the ST biofilms 4-fold (Figure 4C). Finally, similarly to ROS, protease activity can be an indicator of a dysbiotic biofilm [63]. Figure 4D shows an increase in protease activity in HT biofilms when C. albicans is present, with a 9-fold increase in protease activity. In contrast, quantities remained low in both ST biofilms with a small 1.6-fold increase in those biofilms with C. albicans.
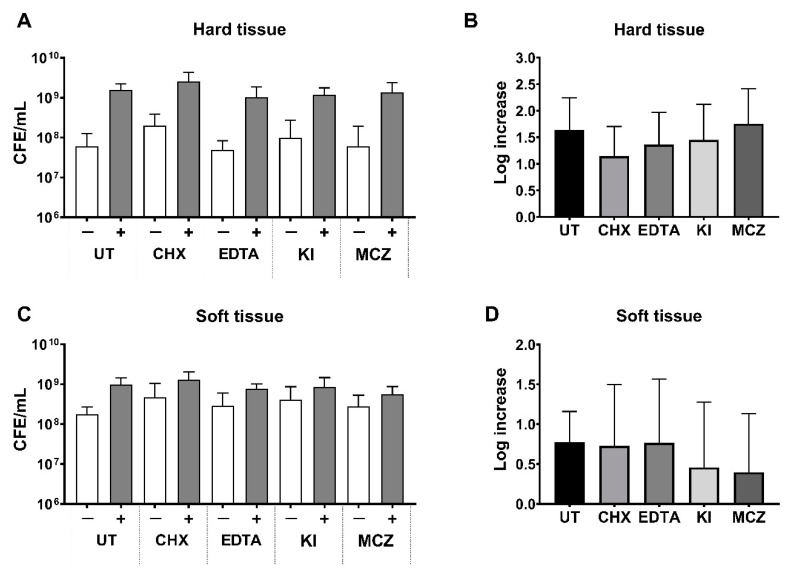
Figure 5, panels A and C, showed that the most effective treatment was CHX, which reduced the metabolic activity of both biofilms tested, irrespective of the inclusion of Candida. The metabolic activities of the remaining biofilms were comparable to untreated controls following treatment with EDTA, potassium iodine (KI) or miconazole (MCZ), even following the addition of C. albicans. Post-treatment with CHX, metabolic activity was reduced by about 50% compared to the control in HT (Figure 5A) and ~70% in the ST biofilms (Figure 5C) regardless of inclusion of a fungal element, which was a significant reduction when compared to each individual control (p < 0.01, p < 0.001). In contrast, average metabolic activity in the biofilms following treatments from EDTA, KI and MCZ showed small changes from the control, but not significantly different. For the CHX-treated ST biofilm minus C. albicans, significantly greater biomass was detected when compared to the controls, suggestive of possible artificial CV staining of CHX precipitate within these biofilms (p < 0.001). There were no significant differences in susceptibility profiles of the HT biofilms to the treatments compared to the untreated controls (Figure 5B). Interestingly, ST biofilms treated with EDTA were the only treated biofilm to become more susceptible to disruption compared to the UT following the inclusion of C. albicans (Figure 5D; # p < 0.05), while all other treatments remained comparable to the control. Overall, this highlights a similarity in the treatment responses of the biofilms, which following the inclusion of C. albicans, did not create a more resilient or susceptible biofilm in vitro.
Figure 5.
Treatment outcomes of hard and soft tissue biofilms with or without C. albicans. After maturation, biofilms were treated with 0.2% CHX, 4% EDTA, 1% KI or 40 µg/mL MCZ for 10 min at room temperature. Alamar blue™ dye was used to assess metabolic activity was calculated against an untreated control (HT biofilm (A) and ST biofilm (C)). Data represent mean ± SD, carried out in triplicate in three independent experiments. A Mann–Whitney t test was carried out on the raw metabolic activity data to assess significant differences between untreated (UT) and treated biofilms (## p < 0.01, ### p < 0.001). Following metabolic assessment, biofilms were dried overnight at room temperature and biomass was determined via crystal violet staining (HT biofilm (B) and ST biofilm (D)). A dotted black line has been drawn to illustrate the average results of the UT control—C. albicans, and a black solid line entered to show the UT control + C. albicans. Data represent mean ± SD, carried out in triplicate or quadruplicate on three independent experiments (a total of 11 replicates from 3 separate experiments). A Mann–Whitney t test was used to compare significant differences between UT biofilms and treated biofilms (# p < 0.05, ### p < 0.001, *** p < 0.001).
3.4. Bacterial Load Following Treatment in Oral Biofilm Models with or without C. albicans
Finally, the bioburden of bacteria and fungi were assessed following treatment using qPCR analyses. For all treatments, no significant difference was found when comparing bacterial load (16S) to the respective untreated controls in either biofilm model (Figure 6A,C, white bars). Similar results for bacterial counts were observed when C. albicans was included in the models (ns, p > 0.05; Figure 6A,C, grey bars). In both biofilm models, irrespective of treatment, log increases of between ~0.5 and ~1.5 units were seen in bacterial counts following inclusion of C. albicans (Figure 6B,D). No differences were also seen when comparing the fungal counts (18S) following treatment, with C. albicans maintaining a level of ~3–5 × 107 CFE/mL for HT, and ~3–6 × 107 CFE/mL for ST irrespective of treatment type (ns, p > 0.05). All average CFE/mL values for each biofilm with or without treatment are shown in Table 3. Taken together, the qPCR data indicated that the bacterial load was not affected by treatment with a variety of different agents following incorporation of C. albicans, suggesting that the fungal element did not convey protection for the microbiota against the variety of agents.
Figure 6.
Bacterial load following 10 min treatment of hard and soft tissue biofilms plus or minus C. albicans. Following growth and removal of the biofilm from the microtiter plate, DNA was extracted using the QIAamp DNA Mini Kit, and bacterial load was assessed using 16S PCR. Data represent mean ± SD, experiment carried out in duplicate from three independent experiments. The total bacterial load (shown as colony forming equivalent (CFE) per mL) is shown for HT biofilms (A) and ST associated biofilms (C). The white bars are indicative of bacterial-only biofilms, whilst grey bars show the biofilms containing C. albicans. The fungal loads (quantified using 18s qPCR) of the biofilms were also assessed in the C. albicans-containing biofilms and total CFE/mL counts are documented in Table 3. Log increase, HT, caries associated biofilms (B) and ST associated biofilms (D) of biofilms with or without C. albicans. No significant differences were observed between untreated and treated samples using a Mann–Whitney t test.
Table 3.
Average colony forming equivalent counts for total bacteria and fungi in the two biofilm models following treatment. The mean CFE/mL for each biofilm was calculated from an average of 9 independent biofilms (n = 3 from 3 separate experiments) following treatment with CHX, EDTA, KI and MCZ compared to untreated controls.
| Biofilm | Treatment | Average CFE/mL | |||
|---|---|---|---|---|---|
| 16S | 18S | ||||
| − C. a | + C. a | − C. a | + C. a | ||
| ST | UT | 1.77 × 108 | 9.96 × 108 | n/a | 6.08 × 106 |
| CHX | 4.74 × 108 | 1.30 × 109 | n/a | 4.31 × 106 | |
| EDTA | 2.91 × 108 | 7.66 × 108 | n/a | 3.91 × 106 | |
| KI | 4.13 × 108 | 8.46 × 108 | n/a | 3.32 × 106 | |
| MCZ | 2.79 × 108 | 5.60 × 108 | n/a | 3.21 × 106 | |
| HT | UT | 6.00 × 107 | 1.59 × 109 | n/a | 4.60 × 107 |
| CHX | 2.02 × 108 | 2.59 × 109 | n/a | 4.21 × 107 | |
| EDTA | 4.91 × 107 | 1.04 × 109 | n/a | 3.34 × 107 | |
| KI | 9.84 × 107 | 1.18 × 109 | n/a | 3.11 × 107 | |
| MCZ | 6.13 × 107 | 1.36× 109 | n/a | 3.52 × 107 | |
4. Discussion
Candida albicans is known as an opportunistic pathogen which colonizes many different sites of the human body, with an ability to cause severe disease through candidiasis in the immunocompromized [64]. C. albicans also has the ability to form biofilms on a range of surfaces in a medical setting, such as indwelling medical devices [65], and has also been found as a potent colonizer of various oral mucosal sites [66,67]. With known mortality rates of up to 60% in candidemia patients and studies highlighting the pathogenic nature of Candida biofilms [68,69], from a clinical standpoint, Candida infections and associated biofilms are viewed as highly problematic. Furthermore, in the context of biofilm research, the pathogenic mechanisms of many microbial diseases are now often viewed as interkingdom and polymicrobial in nature [70,71]. As such, it is perhaps no surprise that our understanding of fungal–bacterial interactions continues to progress, particularly in the oral cavity whereby C. albicans specifically has been implemented as potential “active accomplice” in different oral infections [11]. Hence this study aimed to investigate the biofilm “profiles” and/or pathogenic “signatures” of two oral biofilm models following incorporation of C. albicans.
Firstly, and perhaps unsurprisingly, results showed that metabolic activity and biomass were increased when C. albicans was included within the biofilms (Figure 1). Metabolic activity quantified via Alamar blue™ assay is a measurement of the rate of respiration in the reduction of resazurin to resorufin by electron acceptors such as NADPH and cytochromes [72]. Crystal violet staining, commonly used in Gram staining techniques, binds to the cell walls of bacteria and fungi, and lipopolysaccharides and DNA, both of which are large components of the extracellular matrix (ECM) [73]. Metabolic activity and biomass testing in biofilms in reality are crude measurements that can be useful when used with a variety of other techniques. Hence, it is essential to note that growth rates differ between organisms, and therefore metabolic output observations should be viewed with a certain level of caution. As such, metabolic activity may not be representative of the whole biofilm, but as an indicator of the fastest growing and thereby more metabolically active organism present in the consortia. However, it can still be used as an inclusive measurement tool with other techniques to assess changes in the biofilm environment [74,75]. Additionally, CV staining does not differentiate between additional components of the biofilm (e.g., extracellular matrix and eDNA) and cells within the biofilm [73,76]. Nevertheless, results from these simple methodologies highlight that a thicker, more metabolically active biofilm was formed in the presence of C. albicans.
From the results here, the increase in metabolic activity and biomass for biofilms grown with C. albicans could be multifactorial and not simply caused by more cells being present. Therefore, it was deemed pertinent to assess microbial cell numbers via qPCR. For the CV observations, the size difference of C. albicans to bacteria may influence the increase in CV values, with the average C. albicans cell being almost 150× larger than their bacterial counterparts, and so it would be logical that an increase in CV was detected [15,17]. Alternatively, the elevated biomass may be caused by an increase in ECM production from cells; studies have shown an increase in ECM production from bacteria in the presence of C. albicans [77]. As a culmination of factors, the addition of C. albicans may also reduce the amount of biofilm washed away during the CV experimental procedure, helping one to retain a more robust and metabolically active biofilm in vitro. Indeed, C. albicans has previously been shown to be a structural scaffold within dual-species biofilms [56]. This may be an effect we observed in this study, particularly with the increase in bacterial load, as shown in Figure 2, and confirmed through increased architecture in SEM images shown in Figure 3, particularly in the HT biofilms. Ultimately, it could be that a robust biofilm containing C. albicans would provide a better representation of the polymicrobial nature of the biofilms in the oral cavity, which may allow for more appropriate and accurate routine testing to be undertaken in vitro. At this juncture, it has been shown previously that mechanical removal through brushing alongside therapeutic activity is required to successfully manage these fungal–bacterial biofilms in vitro [38].
Alongside the increase in bacterial load there were compositional changes that accompanied the inclusion of C. albicans, as seen in Figure 2B,C. In HT biofilms, the main components remain similar; however, S. mutans and L. casei decreased in proportion after the addition of C. albicans, which may be a result of the increase in pH to a more neutral environment in the presence of the fungi (Figure 4). It has been shown elsewhere that C. albicans has the ability to neutralize an acidic environment, a process that will lead to induction of the yeast-hyphal transition, an important virulence mechanism used by the organism to promote survival and/or tissue invasion [61]. The presence of the remaining organisms within this model, even following incorporation of C. albicans, was deemed essential to include to provide a representative caries biofilm rather than focusing on S. mutans as a single species, a limitation of previous studies given the polymicrobial nature of the disease [78]. In ST biofilms, an increase in pathogens such as P. gingivalis was noted following addition of the fungi; therefore, in a similar manner to the HT model, it would allow a more appropriate biofilm to be used to study soft tissue diseases such as denture stomatitis and periodontitis. As such the ST biofilm incorporates anaerobic bacteria representing periodontitis and C. albicans in denture stomatitis alongside an interkingdom biofilm representative of that seen in ecological niche of these diseases [19]. C. albicans has been shown to generate hypoxic conditions in a biofilm microenvironment [79], which may explain the elevated number of anaerobic pathogens, such as P. gingivalis and F. nucleatum in the ST biofilms containing Candida. Overall, it could be argued that inclusion of any fungal element into such a polymicrobial biofilm would cause composition changes, simply due to the size and morphological phenotypes of such organisms. This, of course, raises the question: “can all oral fungal species serve as keystone commensals?” Such a postulation goes far beyond the remit of the current paper but definitely requires careful consideration moving forward.
The link between acidic conditions in the oral cavity and dental caries onset is well documented; however, periodontal biofilms have also been shown to acidic in nature [80]. As discussed above, C. albicans inclusion seemed to offer a buffering effect, as shown in the pH increase with the value closer to neutral in the supernatants collected (Figure 4). Such a buffering effect is not unheard of with C. albicans, an organism which prefers to maintain a cytosolic pH range of between 5.8 and 9 [81]. Lactate and lactic acid are common metabolites of oral bacteria, and often a dysbiosis in the utilization and production of these compounds can lead to disease [82]. Results showed here that lactate was reduced in biofilms with C. albicans (Figure 4B). C. albicans is able to utilize lactate as a substrate to produce an increased stress response and drug resistant properties [83]. Previous studies have also shown that through ammonia production, C. albicans cells are able to self-regulate pH to allow morphogenesis (the ability to shift from yeast to hyphae) and proliferation [61]. This rise in pH, likely through the regulation of lactate levels, may suggest that having C. albicans within an oral biofilm may provide a protective, more pH neutral environment within this model. Such observations may have implications on studies interested in health vs. disease models, whereby inclusion of C. albicans stabilizes the biofilm, making it more habitable by health-associated organisms.
ROS such as superoxide anion (SOD) and hydrogen peroxide are essential metabolites in cellular respiration; however, accumulation and failure to neutralize ROS leads to oxidative stress and cell death [84]. In that capacity, SOD was tested for in the oral biofilm models. Figure 4C shows that SOD is reduced in HT + C. albicans containing biofilms, possibly indicating less reactive oxygen species are present within the environment. On the contrary, ST biofilm + C. albicans showed an increase in SOD; this may have been due to the facultative anaerobic bacteria (such as F. nucleatum, V. dispar, A. naeslundii and A. actinomycetemcomitans) producing more SOD than aerotolerant species [85].
To assess overall hydrolytic qualities of the biofilm models, protease activity was quantified (Figure 4D). C. albicans containing HT biofilm showed increased levels of protease activity when compared to the C. albicans lacking biofilm. C. albicans pathogenicity depends on the secretion of proteinases to invade host cells through the damaging of cell membranes, and so this increase may be directly linked to C. albicans’ presence [86,87]. In order to fully assess the implication of this, additional work carried out under a high sugar environment would be required. Furthermore, these observations regarding protease activity may simply be due to the increased microbial load within the biofilms containing C. albicans. To investigate whether this was the case, experiments presented here would need to be repeated with (1) heat-inactivated Candida or (2) mutated isolates lacking specific protease genes (e.g., secreted aspartyl proteinase mutants).
Finally, to assess whether the inclusion of C. albicans affected the biofilms response to treatments, the efficacies of different antimicrobials were tested. The antimicrobials chosen represent a series of agents with different mode of actions and purposes, a gold-standard mouthwash (CHX), irrigants (EDTA/KI) and an antifungal agent (MCZ). Following treatment, the metabolic activity, biomass and fungal/bacterial load of each biofilm were assessed. Such parameters were chosen for analyses as previous evidence has indicated that biofilm viability and metabolic activity are reduced following short-term treatment with certain therapeutics (e.g., CHX) [88,89,90], whilst others have shown components such as EDTA can destabilize and degrade extracellular matrix [91], possibly leading to detachment of the biofilm and loss of overall bioburden. From the actives tested, CHX was the only agent which significantly reduced metabolic activity in comparison with the UT control (Figure 5A,C), although this reduction did not equate to detachment since biomass data and bacterial load data are not decreased and similar to the UT control (Figure 5B,D). Furthermore, the efficacy of CHX did not change in biofilms with or without C. albicans. EDTA significantly reduced the biomass of the Candida-containing biofilm, suggestive that the antimicrobial is effective against the fungal element, which is in line with previous observations [92,93]. The lack of reduction in metabolic activity, biomass and/or cell number for any of the other treatments tested highlights the importance of treatment time and the potential adjunctive use of mechanical disruption alongside antimicrobial therapies, even in the context of in vitro studies. Standard overnight incubations usually employed in minimum biofilm eradication studies may overestimate the effectiveness of the active [94] and so a short incubation time was favored for this study. It may be that longer incubation times would result in differences in tolerance levels of the biofilms to such therapeutics following inclusion of C. albicans. It should also be noted that only normal qPCR, and not live/dead qPCR, was used to quantify the bacterial and fungal load in the models following treatment. This live/dead methodology has been used with great effect to assess the level of “viability” of oral microorganisms in plaque samples and in vitro biofilm models [38,44,95]. Therefore, it could be that no changes were observed in the total bacterial or fungal load in this study, but there may have been reductions in the number of viable cells present in the biofilm (which could corroborate with the metabolic activity changes particularly for CHX treatment for example). It is not uncommon for dead microbial cells to remain in the biofilm even following treatment [88,89,96]. Therefore, this poses the question: “does the biofilm require some degree of mechanical disruption for sufficient removal of dead and viable cells?” Indeed, in the case of most oral diseases of microbial origin, particularly for dental caries and periodontitis, the primary aim for clinicians is physical debridement of the biofilm, before administering antimicrobials to prevent the regrowth of microorganisms. This ultimately highlights the need for mechanical removal of biofilms in vitro to truly provide realistic model systems as shown with previous studies conducted [38,97]. Sherry et al. (2016) highlighted the importance of adjunctive therapies of biofilm testing in vitro. In this study, the 11- species biofilm used here (ST) was subject to cleaning regimes involving a denture cleansing treatment. Mechanical disruption by brushing alone was not sufficient to reduce bioburden on the denture substrates, whereby only when used in conjunction with the denture cleanser was significant reductions in viable microbial cells observed [38]. Future studies must consider using these “disrupt and inhibit” experiments with such in vitro oral biofilm model systems.
From this work it can be concluded that future studies should consider incorporation of a fungal element to fully encompass the polymicrobial nature of the oral cavity. The emerging postulations that C. albicans may serve as a “keystone commensal” in multispecies oral communities highlights its importance in the context of oral health (and disease) [15]. This study, to the authors knowledge, was the first to truly assess whether C. albicans serves as a “keystone” component in oral biofilm models in vitro. From the data, the importance of including Candida in such biofilm models is attributed to a more robust structure of the mixed species consortia, while not affecting the tolerance of the biofilm to short-term exposure of conventional oral therapeutics. Indeed, further studies are required to truly understand what role C. albicans, and other fungal inhabitants, play in homeostasis of the oral cavity, and we hope this study will provide a platform for further research into said phenomenon. In the long term, inclusion of such an organism in otherwise bacterial-only biofilms should hopefully generate a more applicable model system for testing conventional and/or novel therapeutics.
Acknowledgments
The authors would like to acknowledge internal funding support from University of Glasgow and Blutest laboratories for TY. Additionally, the authors would like to thank the oral sciences research group at University of Glasgow, and continued support from GSK for their insight and feedback on the manuscript and Emma Millhouse and Yan Zhou for the optimized biofilm methodology used in this study. Special thanks to Margaret Mullin at the Glasgow Imaging Facility for help with the processing and imaging of the biofilm samples for SEM.
Author Contributions
Conceptualization, T.Y., R.K., G.R. and J.L.B.; methodology and investigation, T.Y. and O.-A.A.; formal analysis, T.Y., O.-A.A., R.K. and J.L.B.; data curation, T.Y. and J.L.B.; writing—original draft preparation, T.Y. and J.L.B.; writing—review and editing, T.Y., R.K., D.B., J.P., C.W. (Craig Williams), C.W. (Chris Woodall), G.R. and J.L.B.; supervision, R.K., D.B., J.P., C.W. (Craig Williams), C.W. (Chris Woodall), G.R. and J.L.B.; funding acquisition, C.W. (Chris Woodall) and G.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dewhirst F.E., Chen T., Izard J., Paster B.J., Tanner A.C.R., Yu W.-H., Lakshmanan A., Wade W.G. The Human Oral Microbiome. J. Bacteriol. 2010;192:5002–5017. doi: 10.1128/JB.00542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marsh P.D. The commensal microbiota and the development of human disease—An introduction. J. Oral Microbiol. 2015:7. doi: 10.3402/jom.v7.29128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jin L.J., Lamster I.B., Greenspan J.S., Pitts N.B., Scully C., Warnakulasuriya S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2016;22:609–619. doi: 10.1111/odi.12428. [DOI] [PubMed] [Google Scholar]
- 4.Vos T., Abajobir A.A., Abate K.H., Abbafati C., Abbas K.M., Abd-Allah F., Abdulkader R.S., Abdulle A.M., Abebo T.A., Abera S.F., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.W.H.O. What is the Burden of Oral Disease. [(accessed on 30 January 2020)]; Available online: https://www.who.int/oral_health/disease_burden/global/en/
- 6.Zaura E., Keijser B.J.F., Huse S.M., Crielaard W. Defining the healthy "core microbiome" of oral microbial communities. BMC Microbiol. 2009;9:259. doi: 10.1186/1471-2180-9-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bik E.M., Long C.D., Armitage G.C., Loomer P., Emerson J., Mongodin E.F., Nelson K.E., Gill S.R., Fraser-Liggett C.M., Relman D.A. Bacterial diversity in the oral cavity of 10 healthy individuals. ISME J. 2010;4:962–974. doi: 10.1038/ismej.2010.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zarco M.F., Vess T.J., Ginsburg G.S. The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis. 2012;18:109–120. doi: 10.1111/j.1601-0825.2011.01851.x. [DOI] [PubMed] [Google Scholar]
- 9.Ghannoum M.A., Jurevic R.J., Mukherjee P.K., Cui F., Sikaroodi M., Naqvi A., Gillevet P.M. Characterization of the oral fungal microbiome (mycobiome) in healthy individuals. PLoS Pathog. 2010;6:e1000713. doi: 10.1371/journal.ppat.1000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dupuy A.K., David M.S., Li L., Heider T.N., Peterson J.D., Montano E.A., Dongari-Bagtzoglou A., Diaz P.I., Strausbaugh L.D. Redefining the Human Oral Mycobiome with Improved Practices in Amplicon-based Taxonomy: Discovery of Malassezia as a Prominent Commensal. PLoS ONE. 2014;9:e90899. doi: 10.1371/journal.pone.0090899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delaney C., O’Donnell L.E., Kean R., Sherry L., Brown J.L., Calvert G., Nile C.J., Cross L., Bradshaw D.J., Brandt B.W., et al. Interkingdom interactions on the denture surface: Implications for oral hygiene. Biofilm. 2019;1:100002. doi: 10.1016/j.bioflm.2019.100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Witherden E.A., Shoaie S., Hall R.A., Moyes D.L. The Human Mucosal Mycobiome and Fungal Community Interactions. J. Fungi. 2017;3:56. doi: 10.3390/jof3040056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iliev I.D., Leonardi I. Fungal dysbiosis: Immunity and interactions at mucosal barriers. Nat. Rev. Immunol. 2017;17:635–646. doi: 10.1038/nri.2017.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hall R.A., Noverr M.C. Fungal interactions with the human host: Exploring the spectrum of symbiosis. Curr. Opin. Microbiol. 2017;40:58–64. doi: 10.1016/j.mib.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janus M.M., Willems H.M., Krom B.P. Candida albicans in Multispecies Oral Communities; A Keystone Commensal? Adv. Exp. Med. Biol. 2016;931:13–20. doi: 10.1007/5584_2016_5. [DOI] [PubMed] [Google Scholar]
- 16.O’Donnell L.E., Millhouse E., Sherry L., Kean R., Malcolm J., Nile C.J., Ramage G. Polymicrobial Candida biofilms: Friends and foe in the oral cavity. FEMS Yeast Res. 2015:15. doi: 10.1093/femsyr/fov077. [DOI] [PubMed] [Google Scholar]
- 17.Delaney C., Kean R., Short B., Tumelty M., McLean W., Nile C.J., Ramage G. Fungi at the Scene of the Crime: Innocent Bystanders or Accomplices in Oral Infections? Curr. Clin. Microbiol. Rep. 2018;5:190–200. doi: 10.1007/s40588-018-0100-3. [DOI] [Google Scholar]
- 18.Xiao J., Huang X., Alkhers N., Alzamil H., Alzoubi S., Wu T.T., Castillo D.A., Campbell F., Davis J., Herzog K., et al. Candida albicans and Early Childhood Caries: A Systematic Review and Meta-Analysis. Caries Res. 2018;52:102–112. doi: 10.1159/000481833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Negrini T.d.C., Koo H., Arthur R.A. Candida–Bacterial Biofilms and Host–Microbe Interactions in Oral Diseases. In Proceedings of the Oral Mucosal Immunity and Microbiome. Adv. Exp. Med. Biol. 2019;1197:119–141. doi: 10.1007/978-3-030-28524-1_10. [DOI] [PubMed] [Google Scholar]
- 20.Thurnheer T., Karygianni L., Flury M., Belibasakis G.N. Fusobacterium Species and Subspecies Differentially Affect the Composition and Architecture of Supra- and Subgingival Biofilms Models. Front. Microbiol. 2019;10:1716. doi: 10.3389/fmicb.2019.01716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sztukowska M.N., Dutton L.C., Delaney C., Ramsdale M., Ramage G., Jenkinson H.F., Nobbs A.H., Lamont R.J. Community Development between Porphyromonas gingivalis and Candida albicans Mediated by InlJ and Als3. MBio. 2018:9. doi: 10.1128/mBio.00202-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chu Chun H., Mei L.E.I., Seneviratne Chaminda J., Lo Edward Chin M.A.N. Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int. J. Paediatr. Dent. 2011;22:2–10. doi: 10.1111/j.1365-263X.2011.01149.x. [DOI] [PubMed] [Google Scholar]
- 23.Peyyala R., Kirakodu S.S., Novak K.F., Ebersole J.L. Oral Epithelial Cell Responses to Multispecies Microbial Biofilms. J. Dent. Res. 2013;92:235–240. doi: 10.1177/0022034512472508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Y., Millhouse E., Shaw T., Lappin D.F., Rajendran R., Bagg J., Lin H., Ramage G. Evaluating Streptococcus mutans Strain Dependent Characteristics in a Polymicrobial Biofilm Community. Front. Microbiol. 2018;9:1498. doi: 10.3389/fmicb.2018.01498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diaz P.I., Xie Z., Sobue T., Thompson A., Biyikoglu B., Ricker A., Ikonomou L., Dongari-Bagtzoglou A. Synergistic interaction between Candida albicans and commensal oral streptococci in a novel in vitro mucosal model. Infect. Immun. 2012;80:620–632. doi: 10.1128/IAI.05896-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cavalcanti I.M., Nobbs A.H., Ricomini-Filho A.P., Jenkinson H.F., Del Bel Cury A.A. Interkingdom cooperation between Candida albicans, Streptococcus oralis and Actinomyces oris modulates early biofilm development on denture material. Pathog. Dis. 2016:74. doi: 10.1093/femspd/ftw002. [DOI] [PubMed] [Google Scholar]
- 27.Tang S.X., Moyes D.L., Richardson J.P., Blagojevic M., Naglik J.R. Epithelial discrimination of commensal and pathogenic Candida albicans. Oral Dis. 2016;22(Suppl. 1):114–119. doi: 10.1111/odi.12395. [DOI] [PubMed] [Google Scholar]
- 28.Desai J.V. Candida albicans Hyphae: From Growth Initiation to Invasion. J. Fungi. 2018;4:10. doi: 10.3390/jof4010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bor B., Cen L., Agnello M., Shi W., He X. Morphological and physiological changes induced by contact-dependent interaction between Candida albicans and Fusobacterium nucleatum. Sci. Rep. 2016;6:27956. doi: 10.1038/srep27956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajishengallis G., Darveau R.P., Curtis M.A. The keystone-pathogen hypothesis. Nat. Rev. Microbiol. 2012;10:717–725. doi: 10.1038/nrmicro2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fakhruddin K.S., Perera Samaranayake L., Egusa H., Chi Ngo H., Panduwawala C., Venkatachalam T., Kumarappan A., Pesee S. Candida biome of severe early childhood caries (S-ECC) and its cariogenic virulence traits. J. Oral Microbiol. 2020;12:1724484. doi: 10.1080/20002297.2020.1724484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sardi J.C., Duque C., Mariano F.S., Peixoto I.T., Hofling J.F., Goncalves R.B. Candida spp. in periodontal disease: A brief review. J. Oral Sci. 2010;52:177–185. doi: 10.2334/josnusd.52.177. [DOI] [PubMed] [Google Scholar]
- 33.Puryer J. Denture Stomatitis—A Clinical Update. Dent. Update. 2016;43 doi: 10.12968/denu.2016.43.6.529. [DOI] [PubMed] [Google Scholar]
- 34.Marsh P.D. Microbial ecology of dental plaque and its significance in health and disease. Adv. Dent. Res. 1994;8:263–271. doi: 10.1177/08959374940080022001. [DOI] [PubMed] [Google Scholar]
- 35.Marsh P.D. Are dental diseases examples of ecological catastrophes? Microbiology. 2003;149:279–294. doi: 10.1099/mic.0.26082-0. [DOI] [PubMed] [Google Scholar]
- 36.Allkja J., Bjarnsholt T., Coenye T., Cos P., Fallarero A., Harrison J.J., Lopes S.P., Oliver A., Pereira M.O., Ramage G., et al. Minimum information guideline for spectrophotometric and fluorometric methods to assess biofilm formation in microplates. Biofilm. 2019 doi: 10.1016/j.bioflm.2019.100010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Millhouse E., Jose A., Sherry L., Lappin D.F., Patel N., Middleton A.M., Pratten J., Culshaw S., Ramage G. Development of an in vitro periodontal biofilm model for assessing antimicrobial and host modulatory effects of bioactive molecules. BMC Oral Health. 2014;14:80. doi: 10.1186/1472-6831-14-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherry L., Lappin G., O’Donnell L.E., Millhouse E., Millington O.R., Bradshaw D.J., Axe A.S., Williams C., Nile C.J., Ramage G. Viable Compositional Analysis of an Eleven Species Oral Polymicrobial Biofilm. Front. Microbiol. 2016;7:912. doi: 10.3389/fmicb.2016.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pitts N.B., Zero D.T., Marsh P.D., Ekstrand K., Weintraub J.A., Ramos-Gomez F., Tagami J., Twetman S., Tsakos G., Ismail A. Dental caries. Nat. Rev. Dis. Primers. 2017;3:17030. doi: 10.1038/nrdp.2017.30. [DOI] [PubMed] [Google Scholar]
- 40.Socransky S.S., Haffajee A.D., Cugini M.A., Smith C., Kent Jr R.L. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998;25:134–144. doi: 10.1111/j.1600-051X.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 41.Brown J.L., Johnston W., Delaney C., Rajendran R., Butcher J., Khan S., Bradshaw D., Ramage G., Culshaw S. Biofilm-stimulated epithelium modulates the inflammatory responses in co-cultured immune cells. Sci. Rep. 2019;9:15779. doi: 10.1038/s41598-019-52115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miles A.A., Misra S.S., Irwin J.O. The estimation of the bactericidal power of the blood. J. Hyg. 1938;38:732–749. doi: 10.1017/S002217240001158X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Montelongo-Jauregui D., Srinivasan A., Ramasubramanian A.K., Lopez-Ribot J.L. An In Vitro Model for Oral Mixed Biofilms of Candida albicans and Streptococcus gordonii in Synthetic Saliva. Front. Microbiol. 2016;7:686. doi: 10.3389/fmicb.2016.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loozen G., Boon N., Pauwels M., Quirynen M., Teughels W. Live/dead real-time polymerase chain reaction to assess new therapies against dental plaque-related pathologies. Mol. Oral. Microbiol. 2011;26:253–261. doi: 10.1111/j.2041-1014.2011.00615.x. [DOI] [PubMed] [Google Scholar]
- 45.Periasamy S., Chalmers N.I., Du-Thumm L., Kolenbrander P.E. Fusobacterium nucleatum ATCC 10953 requires Actinomyces naeslundii ATCC 43146 for growth on saliva in a three-species community that includes Streptococcus oralis 34. Appl. Enviorn. Microbiol. 2009;75:3250–3257. doi: 10.1128/AEM.02901-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sherry L., Millhouse E., Lappin D.F., Murray C., Culshaw S., Nile C.J., Ramage G. Investigating the biological properties of carbohydrate derived fulvic acid (CHD-FA) as a potential novel therapy for the management of oral biofilm infections. BMC Oral Health. 2013;13:47. doi: 10.1186/1472-6831-13-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park S.N., Park J.Y., Kook J.K. Development of Porphyromonas gingivalis-specific quantitative real-time PCR primers based on the nucleotide sequence of rpoB. J. Microbiol. 2011;49:315–319. doi: 10.1007/s12275-011-1028-y. [DOI] [PubMed] [Google Scholar]
- 48.Periasamy S., Kolenbrander P.E. Mutualistic biofilm communities develop with Porphyromonas gingivalis and initial, early, and late colonizers of enamel. J. Bacteriol. 2009;191:6804–6811. doi: 10.1128/JB.01006-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Desai A.R., Shah N.P., Powell I.B. Discrimination of dairy industry isolates of the Lactobacillus casei group. J. Dairy Sci. 2006;89:3345–3351. doi: 10.3168/jds.S0022-0302(06)72371-2. [DOI] [PubMed] [Google Scholar]
- 50.Suzuki N., Yoshida A., Saito T., Kawada M., Nakano Y. Quantitative microbiological study of subgingival plaque by real-time PCR shows correlation between levels of Tannerella forsythensis and Fusobacterium spp. J. Clin. Microbiol. 2004;42:2255–2257. doi: 10.1128/JCM.42.5.2255-2257.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rajendran R., Borghi E., Falleni M., Perdoni F., Tosi D., Lappin D.F., O’Donnell L., Greetham D., Ramage G., Nile C. Acetylcholine Protects against Candida albicans Infection by Inhibiting Biofilm Formation and Promoting Hemocyte Function in a Galleria mellonella Infection Model. Eukaryot Cell. 2015;14:834–844. doi: 10.1128/EC.00067-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Erlandsen S.L., Kristich C.J., Dunny G.M., Wells C.L. High-resolution visualization of the microbial glycocalyx with low-voltage scanning electron microscopy: Dependence on cationic dyes. J. Histochem. Cytochem. 2004;52:1427–1435. doi: 10.1369/jhc.4A6428.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.James P., Worthington H.V., Parnell C., Harding M., Lamont T., Cheung A., Whelton H., Riley P. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst. Rev. 2017;3:Cd008676. doi: 10.1002/14651858.CD008676.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McComb D., Smith D.C. A preliminary scanning electron microscopic study of root canals after endodontic procedures. J. Endod. 1975;1:238–242. doi: 10.1016/S0099-2399(75)80226-3. [DOI] [PubMed] [Google Scholar]
- 55.Safavi K.E., Spangberg L.S., Langeland K. Root canal dentinal tubule disinfection. J. Endod. 1990;16:207–210. doi: 10.1016/S0099-2399(06)81670-5. [DOI] [PubMed] [Google Scholar]
- 56.Kean R., Rajendran R., Haggarty J., Townsend E.M., Short B., Burgess K.E., Lang S., Millington O., Mackay W.G., Williams C., et al. Candida albicans Mycofilms Support Staphylococcus aureus Colonization and Enhances Miconazole Resistance in Dual-Species Interactions. Front. Microbiol. 2017;8:258. doi: 10.3389/fmicb.2017.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marsh P.D. Sugar, fluoride, pH and microbial homeostasis in dental plaque. Proc. Finn. Dent. Soc. 1991;87:515–525. [PubMed] [Google Scholar]
- 58.Zaura E., Brandt B.W., Prodan A., Teixeira de Mattos M.J., Imangaliyev S., Kool J., Buijs M.J., Jagers F.L., Hennequin-Hoenderdos N.L., Slot D.E., et al. On the ecosystemic network of saliva in healthy young adults. ISME J. 2017;11:1218–1231. doi: 10.1038/ismej.2016.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tomofuji T., Irie K., Sanbe T., Azuma T., Ekuni D., Tamaki N., Yamamoto T., Morita M. Periodontitis and increase in circulating oxidative stress. Jpn. Dent. Sci. Rev. 2009;45:46–51. doi: 10.1016/j.jdsr.2008.12.002. [DOI] [Google Scholar]
- 60.Culp E., Wright G.D. Bacterial proteases, untapped antimicrobial drug targets. J. Antibiot. 2017;70:366–377. doi: 10.1038/ja.2016.138. [DOI] [PubMed] [Google Scholar]
- 61.Vylkova S., Carman A.J., Danhof H.A., Collette J.R., Zhou H., Lorenz M.C. The fungal pathogen Candida albicans autoinduces hyphal morphogenesis by raising extracellular pH. mBio. 2011;2:e00055-11. doi: 10.1128/mBio.00055-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dahiya P., Kamal R., Gupta R., Bhardwaj R., Chaudhary K., Kaur S. Reactive oxygen species in periodontitis. J. Indian Soc. Periodontol. 2013;17:411–416. doi: 10.4103/0972-124X.118306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sonesson A., Przybyszewska K., Eriksson S., Mörgelin M., Kjellström S., Davies J., Potempa J., Schmidtchen A. Identification of bacterial biofilm and the Staphylococcus aureus derived protease, staphopain, on the skin surface of patients with atopic dermatitis. Sci. Rep. 2017;7:8689. doi: 10.1038/s41598-017-08046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Huffnagle G.B., Noverr M.C. The emerging world of the fungal microbiome. Trends Microbiol. 2013;21:334–341. doi: 10.1016/j.tim.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ramage G., Martínez J.P., López-Ribot J.L. Candida biofilms on implanted biomaterials: A clinically significant problem. FEMS Yeast Res. 2006;6:979–986. doi: 10.1111/j.1567-1364.2006.00117.x. [DOI] [PubMed] [Google Scholar]
- 66.Singh A., Verma R., Murari A., Agrawal A. Oral candidiasis: An overview. J. Oral Maxillofac. Pathol. 2014;18:S81–S85. doi: 10.4103/0973-029X.141325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kirchner F.R., Littringer K., Altmeier S., Tran V.D.T., Schonherr F., Lemberg C., Pagni M., Sanglard D., Joller N., LeibundGut-Landmann S. Persistence of Candida albicans in the Oral Mucosa Induces a Curbed Inflammatory Host Response That Is Independent of Immunosuppression. Front. Immunol. 2019;10:330. doi: 10.3389/fimmu.2019.00330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Enoch D.A., Yang H., Aliyu S.H., Micallef C. The Changing Epidemiology of Invasive Fungal Infections. Methods Mol. Biol. 2017;1508:17–65. doi: 10.1007/978-1-4939-6515-1_2. [DOI] [PubMed] [Google Scholar]
- 69.Bassetti M., Righi E., Montravers P., Cornely O.A. What has changed in the treatment of invasive candidiasis? A look at the past 10 years and ahead. J. Antimicrob. Chemother. 2018;73:i14–i25. doi: 10.1093/jac/dkx445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Costa-Orlandi C.B., Sardi J.C.O., Pitangui N.S., de Oliveira H.C., Scorzoni L., Galeane M.C., Medina-Alarcon K.P., Melo W., Marcelino M.Y., Braz J.D., et al. Fungal Biofilms and Polymicrobial Diseases. J. Fungi. 2017;3:22. doi: 10.3390/jof3020022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rodrigues M.E., Gomes F., Rodrigues C.F. Candida spp./Bacteria Mixed Biofilms. J. Fungi. 2019;6:5. doi: 10.3390/jof6010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rampersad S.N. Multiple Applications of Alamar Blue as an Indicator of Metabolic Function and Cellular Health in Cell Viability Bioassays. Sensors. 2012;12:12347–12360. doi: 10.3390/s120912347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haney E.F., Trimble M.J., Cheng J.T., Vallé Q., Hancock R.E.W. Critical Assessment of Methods to Quantify Biofilm Growth and Evaluate Antibiofilm Activity of Host Defence Peptides. Biomolecules. 2018;8:29. doi: 10.3390/biom8020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ramage G. Comparing apples and oranges: Considerations for quantifying candidal biofilms with XTT [2,3-bis(2-methoxy-4-nitro-5-sulfo-phenyl)-2H-tetrazolium-5-carboxanilide] and the need for standardized testing. J. Med. Microbiol. 2016;65:259–260. doi: 10.1099/jmm.0.000237. [DOI] [PubMed] [Google Scholar]
- 75.Azeredo J., Azevedo N.F., Briandet R., Cerca N., Coenye T., Costa A.R., Desvaux M., Di Bonaventura G., Hébraud M., Jaglic Z., et al. Critical review on biofilm methods. Crit. Rev. Microbiol. 2017;43:313–351. doi: 10.1080/1040841X.2016.1208146. [DOI] [PubMed] [Google Scholar]
- 76.Costerton J.W., Lewandowski Z., Caldwell D.E., Korber D.R., Lappin-Scott H.M. Microbial biofilms. Annu. Rev. Microbiol. 1995;49:711–745. doi: 10.1146/annurev.mi.49.100195.003431. [DOI] [PubMed] [Google Scholar]
- 77.Falsetta M.L., Klein M.I., Colonne P.M., Scott-Anne K., Gregoire S., Pai C.-H., Gonzalez-Begne M., Watson G., Krysan D.J., Bowen W.H., et al. Symbiotic Relationship between Streptococcus mutans and Candida albicans Synergizes Virulence of Plaque Biofilms In Vivo. Infect. Immun. 2014;82:1968. doi: 10.1128/IAI.00087-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gross E.L., Beall C.J., Kutsch S.R., Firestone N.D., Leys E.J., Griffen A.L. Beyond Streptococcus mutans: Dental caries onset linked to multiple species by 16S rRNA community analysis. PLoS ONE. 2012;7:e47722. doi: 10.1371/journal.pone.0047722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fox E.P., Cowley E.S., Nobile C.J., Hartooni N., Newman D.K., Johnson A.D. Anaerobic bacteria grow within Candida albicans biofilms and induce biofilm formation in suspension cultures. Curr. Biol. 2014;24:2411–2416. doi: 10.1016/j.cub.2014.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Baliga S., Muglikar S., Kale R. Salivary pH: A diagnostic biomarker. J. Indian Soc. Periodontol. 2013;17:461–465. doi: 10.4103/0972-124X.118317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rane H.S., Hayek S.R., Frye J.E., Abeyta E.L., Bernardo S.M., Parra K.J., Lee S.A. Candida albicans Pma1p Contributes to Growth, pH Homeostasis, and Hyphal Formation. Front. Microbiol. 2019;10:1012. doi: 10.3389/fmicb.2019.01012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Periasamy S., Kolenbrander P.E. Central Role of the Early Colonizer Veillonella sp. in Establishing Multispecies Biofilm Communities with Initial, Middle, and Late Colonizers of Enamel. J. Bacteriol. 2010;192:2965. doi: 10.1128/JB.01631-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ene I.V., Adya A.K., Wehmeier S., Brand A.C., MacCallum D.M., Gow N.A., Brown A.J. Host carbon sources modulate cell wall architecture, drug resistance and virulence in a fungal pathogen. Cell Microbiol. 2012;14:1319–1335. doi: 10.1111/j.1462-5822.2012.01813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gambino M., Cappitelli F. Mini-review: Biofilm responses to oxidative stress. Biofouling. 2016;32:167–178. doi: 10.1080/08927014.2015.1134515. [DOI] [PubMed] [Google Scholar]
- 85.Tally F.P., Goldin B.R., Jacobus N.V., Gorbach S.L. Superoxide dismutase in anaerobic bacteria of clinical significance. Infect. Immun. 1977;16:20–25. doi: 10.1128/IAI.16.1.20-25.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fotedar R., Al-Hedaithy S.S.A. Comparison of phospholipase and proteinase activity in Candida albicans and C. dubliniensis. Mycoses. 2005;48:62–67. doi: 10.1111/j.1439-0507.2004.01057.x. [DOI] [PubMed] [Google Scholar]
- 87.Cassone A., De Bernardis F., Mondello F., Ceddia T., Agatensi L. Evidence for a correlation between proteinase secretion and vulvovaginal candidosis. J. Infect. Dis. 1987;156:777–783. doi: 10.1093/infdis/156.5.777. [DOI] [PubMed] [Google Scholar]
- 88.Shen Y., Zhao J., de la Fuente-Nunez C., Wang Z., Hancock R.E., Roberts C.R., Ma J., Li J., Haapasalo M., Wang Q. Experimental and Theoretical Investigation of Multispecies Oral Biofilm Resistance to Chlorhexidine Treatment. Sci. Rep. 2016;6:27537. doi: 10.1038/srep27537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hope C.K., Wilson M. Analysis of the effects of chlorhexidine on oral biofilm vitality and structure based on viability profiling and an indicator of membrane integrity. Antimicrob. Agents Chemother. 2004;48:1461–1468. doi: 10.1128/AAC.48.5.1461-1468.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhou Y., Wang S., Zhou X., Zou Y., Li M., Peng X., Ren B., Xu H.H.K., Weir M.D., Cheng L., et al. Short-Time Antibacterial Effects of Dimethylaminododecyl Methacrylate on Oral Multispecies Biofilm In Vitro. Biomed. Res. Int. 2019;2019:6393470. doi: 10.1155/2019/6393470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cavaliere R., Ball J.L., Turnbull L., Whitchurch C.B. The biofilm matrix destabilizers, EDTA and DNaseI, enhance the susceptibility of nontypeable Hemophilus influenzae biofilms to treatment with ampicillin and ciprofloxacin. Microbiologyopen. 2014;3:557–567. doi: 10.1002/mbo3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ramage G., Wickes B.L., Lopez-Ribot J.L. Inhibition on Candida albicans biofilm formation using divalent cation chelators (EDTA) Mycopathologia. 2007;164:301–306. doi: 10.1007/s11046-007-9068-x. [DOI] [PubMed] [Google Scholar]
- 93.Liu F., Hansra S., Crockford G., Koster W., Allan B.J., Blondeau J.M., Lainesse C., White A.P. Tetrasodium EDTA Is Effective at Eradicating Biofilms Formed by Clinically Relevant Microorganisms from Patients’ Central Venous Catheters. mSphere. 2018:3. doi: 10.1128/mSphere.00525-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Castaneda P., McLaren A., Tavaziva G., Overstreet D. Biofilm Antimicrobial Susceptibility Increases With Antimicrobial Exposure Time. Clin. Orthop. Relat. Res. 2016;474:1659–1664. doi: 10.1007/s11999-016-4700-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Arias L.S., Brown J.L., Butcher M.C., Delaney C., Monteiro D.R., Ramage G. A nanocarrier system that potentiates the effect of miconazole within different interkingdom biofilms. J. Oral. Microbiol. 2020;12:1771071. doi: 10.1080/20002297.2020.1771071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chatzigiannidou I., Teughels W., Van de Wiele T., Boon N. Oral biofilms exposure to chlorhexidine results in altered microbial composition and metabolic profile. NPJ Biofilms Microbiomes. 2020;6:13. doi: 10.1038/s41522-020-0124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sahni K., Khashai F., Forghany A., Krasieva T., Wilder-Smith P. Exploring Mechanisms of Biofilm Removal. Dent. (Sunnyvale) 2016;6:371. doi: 10.4172/2161-1122.1000371. [DOI] [PMC free article] [PubMed] [Google Scholar]