Abstract
Stereotactic radiosurgery (SRS) involves the delivery of a highly conformal ablative dose of radiation to both benign and malignant targets. This has traditionally been accomplished in a single fraction; however, fractionated approaches involving five or fewer treatments have been delivered for larger lesions, as well as lesions in close proximity to radiosensitive structures. The clinical utilization of SRS has overwhelmingly involved photon-based sources via dedicated radiosurgery platforms (e.g., Gamma Knife® and Cyberknife®) or specialized linear accelerators. While photon-based methods have been shown to be highly effective, advancements are sought for improved dose precision, treatment duration, and radiobiologic effect, among others, particularly in the setting of repeat irradiation. Particle-based techniques (e.g., protons and carbon ions) may improve many of these shortcomings. Specifically, the presence of a Bragg Peak with particle therapy at target depth allows for marked minimization of distal dose delivery, thus mitigating the risk of toxicity to organs at risk. Carbon ions also exhibit a higher linear energy transfer than photons and protons, allowing for greater relative biological effectiveness. While the data are limited, utilization of proton radiosurgery in the setting of brain metastases has been shown to demonstrate 1-year local control rates >90%, which are comparable to that of photon-based radiosurgery. Prospective studies are needed to further validate the safety and efficacy of this treatment modality. We aim to provide a comprehensive overview of clinical evidence in the use of particle therapy-based radiosurgery.
Keywords: radiosurgery, particle, carbon, proton, radiation therapy, radiation oncology, stereotactic, ablative, tumor, arteriovenous malformation
1. Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) blends radiation and neurosurgical techniques that were first proposed in 1951 at the Karolinska Institute in Stockholm, Sweden by Lars Leksell [1]. Stereotactic radiosurgery permits the delivery of an ablative dose of radiation in a highly conformal manner, allowing for minimization of dose to nearby tissues at risk. The original Gamma Knife® radiosurgery platform (Elekta AB, Stockholm), which utilized cobalt-60 sources, was developed by Leksell and colleagues in the 1960s. Traditionally, SRS delivery required placement of a stereotactic frame; however, Cyberknife® (Accuray, Sunnyvale), linear accelerator-based, and Gamma Knife ICON® technologies have incorporated frameless stereotactic delivery.
SRS was historically defined as treatment delivery in a single session. However, fractionated stereotactic radiation therapy (FSRT) and staged SRS are becoming increasingly common, particularly for larger targets and those located in eloquent locations [2,3,4,5,6,7,8,9,10]. Stereotactic radiosurgery is commonly utilized for multiple intracranial pathologies, such as brain metastases [2,3,8,9,10,11,12,13,14,15,16], meningiomas [17,18,19,20,21,22,23,24], pituitary adenomas [25,26,27,28,29,30], trigeminal neuralgia [31,32,33,34], vestibular schwannomas [35,36,37,38,39,40,41,42,43,44,45,46,47], and arteriovenous malformations [48,49,50,51,52]. Side effects of SRS are varied but can include alopecia, fatigue, cerebral edema, and radiation necrosis [53]. Cognitive sequelae from SRS is a rare occurrence and is much more commonly associated with the use of whole brain radiation therapy (WBRT) [11,12,13,54,55,56,57].
In recent years, the use of SRS in the management of brain metastases and its role in immune system modulation, particularly when combined with immune checkpoint inhibitors, has generated a great deal of interest within the scientific community [2,8]. While the central nervous system (CNS) was long viewed as “immunologically privileged,” this view has recently been challenged by evidence suggesting that robust peripheral immune responses can result in penetration of peripheral antigens through the blood–brain barrier. Furthermore, there is evidence suggesting that neuroinflammation can further amplify these effects. Additionally, there has been evidence to suggest that ablative doses of radiation therapy, such as those used with SRS allow for enhanced CD8+ T-cell activation [58,59]. While a detailed analysis of this topic is out of scope for this manuscript, combining these two therapeutic modalities remains a pivotal area of research in CNS oncology.
In the forthcoming sections, we provide a comprehensive review of the physics of heavy particle radiation therapy and the role of heavy particle radiosurgery in the management of common pathologies of the CNS. Likely due to the increasing density of proton centers, the existing body of literature largely involves the use of proton radiosurgery [60,61,62,63,64,65,66,67,68].
2. The Proposed Benefits of Proton and Carbon Ion Radiosurgery
Fundamentally, the goal of radiation therapy is to administer a lethal dose to a tumor while sparing surrounding healthy tissues. X-rays, utilized in photon radiation therapy, impart energy in a relatively diffuse manner. Energy is deposited along the entire path of a photon beam as it traverses the body, and the maximum dose delivered is generally located just below the surface of the skin. In order to properly target tumors, treatment planners often employ multiple X-ray beams, the intensities of which are frequently modulated. While treatment planners attempt to spare normal tissues as much as possible in order to minimize the risk of side effects, structures surrounding treatment targets may still receive significant doses of radiation [69,70]. Thus, for tumors adjacent to critical structures, such as the optic chiasm or brainstem, photon-based radiosurgery may carry a significant risk of injury.
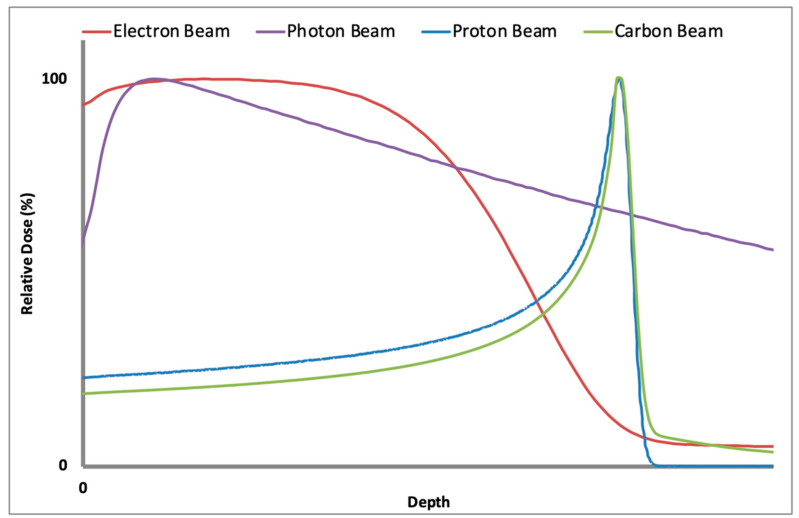
Proton and carbon ion radiation therapy, by contrast, offer dosimetric advantages over photon radiation therapy that create additional therapeutic possibilities [71]. Unlike photons, protons and carbon ions generate an initial low dose region as they traverse through the body. At the ends of their paths, they deposit their maximum dose in a narrow region known as the Bragg Peak. Beyond the Bragg Peak, the dose delivered falls off dramatically. Carbon ion beams have narrower Bragg Peaks than proton beams, and each carbon ion beam generates a fragmentation tail—a low-dose region past the Bragg Peak that results from the fragmentation of carbon ions as they interact with matter. These fragmentation products continue on their path and deposit dose distal to the Bragg Peak. When utilizing carbon ion radiation therapy, planners must take fragmentation tails into account when generating treatment plans to avoid excess dose deposition in critical structures [70,72]. Figure 1 depicts the different depth dose profiles for photons, electrons, carbon ions and protons. Note the presence of a Bragg Peak for both carbon ions and protons, as well as the fragmentation tail associated with the former.
Figure 1.
A graphical representation of tissue depth as a function of relative dose with the former on the x-axis and the latter on the y-axis. The purple graph depicts a photon beam, the red—an electron beam, the green—a carbon ion beam, and the blue—a proton beam. Both the proton and carbon ion beams exhibit significant Bragg Peaks, which are absent for photons and electrons. Additionally, the fragmentation tail associated with carbon ions is depicted. Note the absence of a sharp Bragg Peak for photons and its significant tissue penetration. Electron beams are largely used for superficial treatments (e.g., basal cell carcinomas of the skin) and exhibit a rapid dose fall-off and low tissue penetration.
Carbon ion beams possess an additional advantage. They have narrower penumbras than proton beams, a difference that becomes more pronounced with depth. This results in sharper dose drop-offs at the lateral edges of carbon ion beams [72].
Collectively, the advantages of proton and carbon ion dosimetry potentially allow these radiation therapy techniques to better target tumors and spare surrounding normal structures than photon radiation therapy. In particular, the compactness of the dose delivery relative to photon radiotherapy may allow for the delivery of higher doses of radiation to tumors that are close to critical structures than would otherwise be possible [73] and may also offer relatively low risks of secondary malignancies [74].
Radiobiology may also favor heavy ion therapy; carbon ions are adroit at killing tumor cells. They demonstrate higher linear energy transfer than either photons or protons. As a result, they create complex, clustered DNA damage along their tracks, which is less easily repaired by tumor cells. In fact, the relative biological effectiveness (RBE) of carbon ions is approximately three times that of photons and protons [75,76]. Even hypoxic tumor cells, which show resistance to both photon and proton radiation therapy, show significant sensitivity to carbon ion radiation therapy [69]. The efficacy of carbon ion radiation therapy is also less dependent upon variations in the radiosensitivity of various phases of the cell cycle or diverse tissue types [76]. While distal doses are minimized with both protons and carbon ions, the greater RBE of carbon ions is demonstrated by the greater concentration of high dose within the gross tumor volume.
While most dosimetric characteristics favor particle radiotherapy over photon radiotherapy, there are a few potential drawbacks for particle radiotherapy. One major drawback is range uncertainty, which refers to uncertainty in the depth of the Bragg Peak due to tissue inhomogeneities, anatomical motion, and calculation uncertainties. Due to particle radiotherapy techniques dose being concentrated on the targeted tissue via the Bragg Peak, any uncertainty in depth requires compensation to prevent underdosing the targeted tissue and overdosing tissue beyond the expected region of the Bragg Peak. This uncertainty is often mitigated through the use of treatment margins around targeted tissue and nearby organs at risk [77]. For similar reasons, an exquisite attention to patient setup and organ motion is critical as misalignment of areas of low or high density can have significant impact on the resultant dose deposition. As radiosurgery often involves treating small targets, the dosimetry of small fields becomes an important source of treatment uncertainty for both photon and particle techniques. This is particularly important for particle radiosurgery (especially proton radiosurgery) due to the effect of multiple Coulomb scattering, which causes a slow but steady blurring of the aperture edge with depth due to small changes in the trajectories of individual particles [78]. However, this is only an issue for double scatter systems as most modern systems utilize spot scanning technology which does not have this limitation.
Passive scattering (including single and double scattering) requires the production of a spread-out Bragg Peak (SOBP), which permits dose delivery to the distal margins of the treatment target. This is accomplished by passing the particle beam through a filter. With the use of lead scattering foils, the particle beam develops a uniform energy profile. The beam then passes through a patient-specific aperture and compensator, which is designed so the distal range of the proton beam does not extend beyond the distal margin of the treatment target [72]. Active scanning (also known as pencil beam scanning) is a newer technology and utilizes orthogonal magnets, which allows for dose delivery as a series of small spots that each have their own Bragg Peak of varying energy and intensity [72,79,80]. This method allows for both distal and proximal dose conformality, the latter of which is sacrificed when utilizing passive scattering. Therefore, intensity modulated proton therapy (IMPT) is possible with active scanning but not with passive scattering [72,80].
An important component of radiosurgery is rigid immobilization that is reproducible. Some of the earliest applications of particle radiosurgery was with protons and deuterons and the Lawrence Berkeley National Laboratory for the treatment of pituitary tumors [81,82,83]. These early applications utilized a setup where the head was immobilized at the level of the sella with the use of a mask that was then tightened until the desired level of immobilization was reached. Similar immobilization systems were utilized in single or two-fraction helium ion radiosurgery of AVMs (arteriovenous malformations) [84,85]. However, any immobilization system, but particularly frame-based systems, should be considered carefully as they may limit beam angles in a way that has a much larger effect than in photon-based SRS. Subsequent developments in particle radiosurgery immobilization systems involved the incorporation of vacuum-enforced dental molds which would attach to the stereotactic frame. The Stereotactic Alignment in Radiosurgery (STAR) device at Massachusetts General Hospital allows for the head frame to be mounted to a rotating couch, allowing for increased degrees of freedom during treatment delivery [86].
While carbon radiosurgery has clear significant dosimetric advantages, its clinical application needs to be better elucidated. However, there are multiple retrospective series reporting on outcomes with proton radiosurgery, which are reviewed in the forthcoming sections [60,61,62,63,64,65,66,67,68].
3. The Drawbacks of Proton and Carbon Ion Radiosurgery
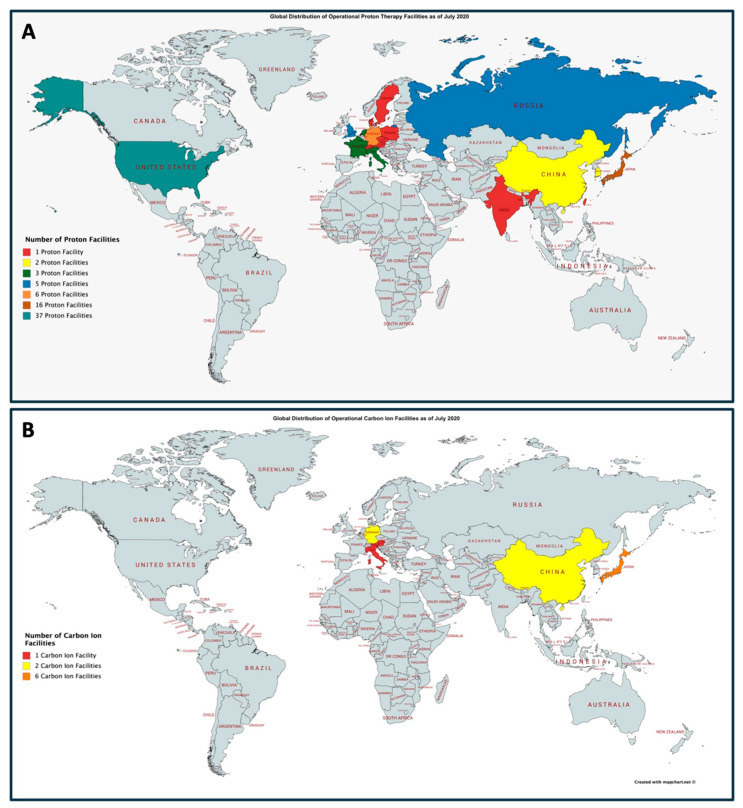
While there are potential dosimetric and radiobiological advantages in the utilization of protons and carbon ions in intracranial radiosurgery, there are several significant practical limitations in deploying these technologies. As shown in Figure 2A, there are a limited number of proton facilities throughout the world. As of July 2020, there are 90 operational proton therapy facilities throughout the world. The largest number of proton facilities are located in the United States with 37 presently operating. There is also marked limited availability of carbon ion therapy. Presently, there are 12 facilities that are operational throughout the world, as shown in Figure 2B. The largest concentration of carbon ion facilities is located within Japan with a total of six. While there are no carbon ion facilities presently operating in the United States, the Mayo Clinic in Jacksonville, Florida, has announced plans to construct a facility in the coming years.
Figure 2.
Global distribution of operation proton centers (A) and carbon ion centers (B) as of July 2020. Presently, there are 90 and 12 operational proton and carbon ion centers, respectively. Adopted from the Particle Therapy Co-Operative Group (https://www.ptcog.ch/index.php/facilities-in-operation). Figures generated using mapchart.net.
Another major drawback to the use of proton and carbon ion therapy are costs associated with treatment. The cost of building a proton facility can cost over $200 million, while photon-based linear accelerators capable of utilizing intensity modulated radiation therapy and SRS often cost less than $10 million [87]. However, in recent years, the development of compact pencil beam scanning proton systems, such as the Mevion S250®, which commonly cost $20–30 million, have allowed for the implantation of this technology at a markedly lower cost, although still much higher than a photon-based SRS system.
While the cost of delivering proton therapy is often upwards of 50% greater than that of photon therapy, comparative effectiveness research studies have suggested that the lifetime cost of protons may be lower than that of photons when accounting for management of radiation toxicities, which is particularly pronounced in pediatric patients [88]. However, due to limited data comparing protons to photons and greater upfront costs, insurance approval for proton therapy remains a challenge for certain indications.
4. Brain Metastases
4.1. Background
The incidence of brain metastases is on the rise, which is largely due to improved systemic therapies and widespread adoption of magnetic resonance imaging (MRI) [89,90]. Approximately 200,000 patients are diagnosed with brain metastases annually in the United States and it is estimated that 10–30% of cancer patients go on to develop brain metastases [91,92,93]. Traditionally, treatment for brain metastases involved the use of corticosteroids and WBRT [94,95], however, the benefits of WBRT in the context of supportive care has come under more scrutiny in recent years [96]. Stereotactic radiosurgery has emerged as a highly effective treatment option in many patients with brain metastases and is associated with fewer instances of treatment-related cognitive deterioration [11,12,13].
4.2. Photon Radiosurgery
In 2009, Chang et al. published a phase III randomized study of 58 patients with 1–3 brain metastases who were randomized to SRS alone (n = 30) and SRS + WBRT (n = 28) [13]. This study closed early due to a high risk of decline in learning and memory in the combination therapy group (mean posterior probability of decline 52%) versus the SRS alone group (mean posterior probability of decline 24%). However, local and distant CNS progression favored the SRS + WBRT arm over the SRS arm, with 73% and 27% of patients being free from CNS progression in the SRS + WBRT and SRS arms, respectively (p = 0.0003). In 2017, Brown et al. published the results of the N107C, a phase III randomized trial, which randomized patients with a single resected brain metastasis to adjuvant SRS or WBRT [11]. This study found a longer cognitive-deterioration-free survival favoring the SRS arm (HR: 0.47; 95% CI: 0.35–0.64; p < 0.0001). Additionally, cognitive deterioration at 6 months was 52% versus 85% (p < 0.0003) in the SRS versus WBRT arms, respectively. However, 12-month local control 61.8% versus 87.1% (p = 0.00068) and 12-month distant brain control 64.7% versus 89.2% (p = 0.00045) both favored the WBRT arm. Therefore, while SRS is associated with less cognitive sequelae and improved quality of life compared to WBRT, the likely need for retreatment is high, necessitating the need for regular follow-up volumetric MRI scans.
4.3. Particle Radiosurgery
Despite the widespread use of photon-based radiosurgery, there is a paucity of data available regarding the use of particle radiosurgery in the management of brain metastases. In 2018, the Massachusetts General Hospital published a retrospective series of 370 patients with 815 brain metastases that were treated with proton radiosurgery at the Harvard Cyclotron Laboratory (Cambridge, MA, USA) [60]. The median prescription dose was 17.3 GyRBE which was prescribed to the 90% isodose line. Strict brainstem and optic chiasm dose constraints were used. The median prescription target volume was 0.6 cc. With a median follow-up of 9.2 months, local and distant brain failure at 12 months was 8.5% (95% CI: 6.7–10.6) and 48.2% (95% CI: 43–53.2%). No grade 4 or 5 acute toxicities occurred, 40.5% (150 patients) experienced acute toxicities, the majority being grade 1 (109 patients), grade 2 (22 patients), and grade 3 (19 patients). Sixty-five patients underwent a craniotomy after proton SRS, 61.5% of whom were symptomatic prior to surgery and 29.2% of whom experienced asymptomatic radiographic progression. Pathologic radiation necrosis was found in 40% (n = 26) of these patients, of whom 54.8% (n = 14) were symptomatic prior to surgery. The 12-month cumulative incidence of radiation necrosis was 3.6% (95% CI: 2–5.8%). Patients who went on to develop radiation necrosis had a median SRS target volume of 2.1 cc. The only factor significantly associated with radiation necrosis on multivariate analysis was target volume size (HR: 1.13; 95% CI: 1.07–1.20). Further details are presented in Table 1 and Table 2.
Table 1.
Patient and treatment details in select studies utilizing particle radiosurgery.
| Author, Year | Target | Particle | n (M/F) | Years | Patient Details | Treatment Details |
|---|---|---|---|---|---|---|
| Atkins et al., 2018 [60] | Brain Metastases | Protons | 370 (170/200) (815 BrM) |
1991–2016 | Median age (range): 61 (20–93) Histology: NSCLC: 34.1% (n = 126); Melanoma: 28.1% (n = 104); Breast: 17.3% (n = 64); RCC: 4.9% (n = 18); HN: 3.8% (n = 14); SCLC: 3.5% (n = 13); GI: 3.5% (n = 13); GYN: 2.2% (n = 8); other: 2.7% (n = 10) Prior cranial RT: 54.9% (n = 203) Neurologic symptoms at presentation: 51.6% (n = 191) Baseline KPS: 50–70: 11.1% (n = 41); 80–100: 67.6% (n = 250) Median target volume: 0.6 cc (range: 0.02–23.3 cc) Median F/U: 9.2 mos Institutions: Harvard Cyclotron Laboratory (Cambridge, MA, USA) and Francis H. Burr Proton Therapy Center at Massachusetts General Hospital (Boston, MA, USA) |
Median dose: 17.3 GyRBE Concurrent systemic therapy: 23.6% (n = 192) (chemotherapy: 39.6% (n = 76), immunotherapy: 17.2% (n = 33), targeted therapy: 33.9% (n = 65), unknown: 9.4% (n = 18)) |
| Sikuade et al., 2015 [65] | Choroidal Melanoma | Protons | 106 (64/43) |
2001–2011 | Median age (range): 59 (24–82) Median tumor diameter: 11 mm (range: 3.6–20.8 mm) Median tumor thickness: 4 mm (range: 1–11.6 mm) Median distance to the optic disc: 2 mm (range: 0–15 mm) Median F/U: 29 mos (range: 7–95 mos) Institution: Douglas Cycloton Clatterbridge Cancer Centre (Wirral, UK) |
59.4 CGE in 4 daily fractions |
| Halasz et al., 2011 [61] | Benign Meningioma | Protons | 50 (15/35) (51 tumors) |
1996–2007 | Median age (range): 60 (33–85) Location: posterior fossa: 24% (n = 12); middle fossa: 45% (n = 23); convexity: 6% (n = 3); other: 26% (n = 13) Presenting symptoms: none: 6% (n = 3); cranial neuropathy: 58% (n = 29); seizures: 12% (n = 6); dizziness: 10% (n = 5); headaches: 8% (n = 4); sensory deficit: 4% (n = 2); motor deficit: 4% (n = 2); other: 2% (n = 1); unknown: 6% (n = 3) Prior surgery: none: 64% (n = 32); STR: 28% (n = 14); GTR: 8% (n = 4) Prior RT: none: 96% (n = 48); fractionated: 4% (n = 2) Median F/U: 32 mos (range: 6–133 mos) Institutions: Harvard Cyclotron Laboratory (Cambridge, MA, USA) and Francis H. Burr Proton Therapy Center at Massachusetts General Hospital (Boston, MA, USA) |
Median dose: 13 GyRBE (range: 10–15.5 GyRBE) prescribed to the 90% isodose line Dmax brainstem 12 GyRBE Dmax optic chiasm 8 GyRBE Median prescription volume: 4.4 cc (range: 1.1–33 cc) |
| Petit et al., 2008 [63] | Pituitary Adenoma (ACTH-producing) | Protons | 38 (6/32) |
1992–2005 | Median age (range): 42 (14–60) Cushing disease (n = 33) and Nelson syndrome (n = 5), all patients underwent transsphenoidal surgery without biochemical cure, n = 4 had prior proton RT, and all Nelson syndrome patients underwent bilateral adrenalectomy 29–228 months prior to proton SRS Median F/U: 62 mos (range: 20–136 mos) Institution: Massachusetts General Hospital (Boston, MA, USA) |
Median dose: 20 CGE (range: 15–20 CGE) Prescribed at the 90% isodose line in n = 37 and the 100% isodose line in n = 1 Delivered in a single fraction Dmax to the optic chiasm < 8 CGE |
| Petit et al., 2007 [62] | Pituitary Adenoma (acromegaly) | Protons | 22 | 1992–2003 | Median age (range): 38 (18–53) All patients underwent prior transsphenoidal surgery without biochemical cure Median F/U: 6.3 years (range: 2.5–14.2 years) Institution: Massachusetts General Hospital (Boston, MA, USA) |
Median dose: 20 CGE (range: 15–24 CGE) |
| Vernimmen et al., 2005 [67] | Cerebral AVM | Protons | 64 (40/24) |
1993–2003 | Median age (range): 35 (7–59) <14 cc: 41% (n = 26); ≥14 cc: 59% (n = 38) AVM median volume: 16.3 cc (range: 1.7–110.6 cc) Presenting symptoms: headaches: 22% (n = 14), hemorrhage: 55% (n = 35), seizures: 30% (n = 19); neurological deficit: 6% (n = 4) SM Grade 1: 3% (n = 2), 2: 17% (n = 11), 3: 30% (n = 19), 4: 42% (n = 27), 5: 8% (n = 5) Median F/U: 62 mos Institution: iThemba Laboratory for Accelerator Based Sciences (LABS), Cape Town, South Africa |
Mean dose (<10 cc): 27.2 SFEcGyE Mean dose (10–13.9 cc): 23.2 SFEcGyE Mean dose (≥14 cc) 27 SFEcGyE |
| Weber et al., 2003 [68] | Vestibular Schwannoma | Protons | 88 (46/42) |
1992–2000 | Median age (range): 69 (36–92) Prior resection: 17% (n = 15); STR: 8% (n = 7), GTR: n = 9% (n = 8) Tumor volume: median 1.4 cc (range: 0.1–15.9 cc) GR Grade 1 or 2: 24% (n = 21); 3–5 or not tested 76% (n = 67) HB Grade 1: 89.8% (n = 79); 2–5: 10.2% (n = 9) Trigeminal nerve dysfunction: 10.2% (n = 9) Median F/U: 38.7 mos (range: 12–102.6) Institution: Harvard Cyclotron Laboratory (Cambridge, MA, USA) |
Median dose: 12 CGE (range: 10–18 CGE) Median maximum tumor dose: 17.1 CGE (range: 13.3–20 CGE) Median number of fractions: 3 (range: 2–4) Number of isocenters: 1 |
| Barker et al., 2003 [97] | Intracranial AVM | Protons | 1250 | 1965–1993 | Median age: 31 (0.02–69 years) Location: frontal lobe: 20% (248); parietal lobe: 36% (445); temporal lobe: 245 (20%); thalamus: 25% (316); brainstem: 4% (53); cerebellum: 6% (76) Median treatment volume: 33.7 cm3 |
Median dose: 10.5 Gy (range: 4–65 Gy) delivered in a single fraction |
| Silander et al., 2002 [66] | Cerebral AVM | Protons | 26 (14/12) |
1991–1997 | Median age (range): 38 (23–64) Nidus volume: 0.3–102 cc (median: 13 cc) SM Grade: 1–2 (n = 10); 3–5 (n = 14) Median F/U: 40 mos (range: 33–62) Institution: The Svedberg Laboratory (Uppsala, Sweden) |
20–25 Gy/2–4 fractions (nidus < 30 cc or > 30 cc) (n = 19) 21–25 Gy/4 fractions (nidus > 30 cc) (n = 6) 16 Gy/4 fractions (prior RT with helium ions) (n = 1) |
| Seifert et al., 1994 [64] | Cerebral AVM | Protons | 68 (30/38) |
1980–1990 | Mean age (range): 33 (14–60) 26.9% (n = 17) <3 cm; 58.7% (n = 37); 3–6 cm; 14.2% (n = 9) >6 cm SM Grade I: 4.4% (n = 3); II: 5.9% (n = 4); III: 42.6% (n = 29); IV: 36.8% (n = 25); V: 2.9% (n = 2); VI: 7.4% (n = 5) Presenting symptoms: seizures (n = 39); hemorrhage (n = 32); progressive neurological deficits (n = 16); headache (n = 9); incidental finding (n = 3) F/U available for 92.6% (n = 63) Institutions: Various radiosurgical centers in the United States |
NR |
| Steinberg et al., 1990 [98] | Cerebral AVM | Helium | 35 (20/15) |
1983–1989 | Age range: 13–64 Location: brainstem: 54% (n = 19); thalamus/internal capsule: 26% (n = 9); basal ganglia: 9% (n = 3); motor/language area: 9% (n = 3); cerebellopontine angle: 2% (n = 1) Mean F/U: 40 mos (range: 1–7 years) Institution: University of California (Berkeley, CA, USA) |
Initially, high doses of 45 GyE were used, which were changed to 10–15 GyE |
Abbreviations: ACTH: adrenocorticotropin hormone; AVM: arteriovenous malformation; BrM: brain metastases; cc: cubic centimeter; CGE: cobalt gray equivalents; F: number of female patients; F/U: follow-up; GI: gastrointestinal; GR: Gardner–Robertson; GTR: gross total resection; Gy: gray; GYN: gynecologic; HB: House– Brackmann; HN: head and neck; KPS: Karnofsky performance status; M: number of male patients; mos: months; n: total number of patients; NR: not reported; NSCLC: non-small cell lung cancer; pts: patients; RBE: relative biological effectiveness; RT: radiation therapy; SCLC: small cell lung cancer; SFEcGyE: single-fraction equivalent cobalt gray equivalent dose; SM: Spetzler–Martin; STR: subtotal resection; USA: United States of America.
Table 2.
Patient and treatment details in select studies utilizing particle radiosurgery.
| Author, Year | Outcomes |
|---|---|
| Atkins et al., 2018 [60] (Brain Metastases) |
|
| Sikuade et al., 2015 [65] (Choroidal Melanoma) |
|
| Halasz et al., 2011 [61] (Benign Meningioma) |
|
| Petit et al., 2007 [62] (Acromegaly—Pituitary Adenoma) |
|
| Petit et al., 2008 [63] (ACTH-producing Pituitary Adenoma) |
|
| Vernimmen et al., 2005 [67] (Cerebral AVM) |
|
| Weber et al., 2003 [68] (Vestibular Schwannoma) |
|
| Barker et al., 2003 [97] (Intracranial AVM) |
|
| Silander et al., 2002 [66] (Cerebral AVM) |
|
| Seifert et al., 1994 [64] (Cerebral AVM) |
|
| Steinberg et al., 1990 [98] (Cerebral AVM) |
|
Abbreviations: ACTH: adrenocorticotropin hormone; AVM: arteriovenous malformation; CI: confidence interval; F/U: follow-up; GKRS: Gamma Knife radiosurgery; HB: House–Brackmann; HR: hazard ratio; mos: months; n: number of patients; pts: patients; RN: radiation necrosis; RT: radiation therapy; SM: Spetzler–Martin; SRS: stereotactic radiosurgery.
5. Pituitary Adenoma
5.1. Background
Pituitary adenomas are a relatively common benign CNS neoplasm and account for roughly 10–20% of newly diagnosed brain tumors [99]. Approximately 12,000 cases are diagnosed annually in the United States with an incidence of 3–4 per 100,000 [100]. Pituitary adenomas are classified by their endocrine status, either as functional or nonfunctional, with the former referring to hormone hypersecretion and the latter referring to an absence of hormone production. Approximately 75% of pituitary adenomas are functional, the most common being prolactinomas [101]. While recurrence rates are highly dependent upon the extent of surgical resection, size of the tumor, and endocrine status, recurrence rates ranging from 10–60% have been observed [102,103,104,105]. Therefore, radiation therapy is a commonly used modality in the salvage setting. The choice of conventionally fractioned RT versus SRS is typically dictated by distance of the tumor from the anterior optic pathways. The former is commonly preferred for distances between the tumor and the optic chiasm of <3–5 mm, although consideration of hormonal status and visual symptoms is critical.
5.2. Photon Radiosurgery
Contemporary studies involving the use of photon SRS in the management of functional and non-functional pituitary adenomas have demonstrated excellent rates of local control with minimal rates of visual toxicity. In 2013, Sheehan et al. published a multicenter study of 512 patients diagnosed with nonfunctional pituitary adenomas who were treated with SRS to a mean dose of 16 Gy [30]. With a median follow-up of 36 months, 5-year tumor control rates were excellent at 95% with a 6.6% rate of visual toxicity and a 21% rate of hypopituitarism. In 2013, Sheehan et al. published their findings from the University of Virginia Gamma Knife Center, where 96 patients with Cushing’s Disease were treated with SRS to a mean dose of 16 Gy [29]. The tumor control rate at 5-years was 98% with hormone control rates of 70%. Visual toxicity was observed in 5.2% and hypopituitarism in 36%.
5.3. Particle Radiosurgery
The particle radiosurgery experience in the management of pituitary adenomas is largely limited to the use of protons for functional lesions [62,63]. In 2007, Petit et al. published a retrospective series of 22 patients treated with proton SRS between 1992–2003 for persistent acromegaly at the Harvard Cyclotron Laboratory (Cambridge, MA, USA) [62]. All patients underwent transsphenoidal resection prior to SRS and median follow-up was 6.3 years (range: 2.5–14.2 years). The median dose was 20 CGE (range: 15–24 CGE). A complete response, which was defined as a sustained (≥3 month) normalization of insulin-like growth factor-1 without medical suppression, was observed in 59% of patients. No new visual complications, seizure disorders, brain injuries or secondary brain tumors were noted on follow-up imaging. Eight patients (38%) developed new hypopituitarism. In 2008, the same group published a retrospective study of 38 patients with Cushing’s Disease (n = 33) or Nelson’s Syndrome (n = 5) who previously underwent transsphenoidal surgery without biochemical cure and received proton SRS to a dose of 20 CGE (range: 15–20 CGE) [63]. In the Cushing’s Disease cohort, 52% achieved a complete response at a median time of 14 months post-SRS, 36% achieved stable urine cortisol levels but required continued medical therapy without tumor regrowth, and 12% had persistently elevated urine cortisol levels and radiographic evidence of disease progression that necessitated additional surgery. In the Nelson’s syndrome cohort, 100% achieved a complete response to treatment. No new visual complications were observed in any patients and 52% required hormone supplementation for hypopituitarism. Further details are presented in Table 1 and Table 2.
6. Vestibular Schwannoma
6.1. Background
Vestibular schwannomas (also commonly referred to as an acoustic neuroma) are benign Schwann cell-derived tumors involving the vestibular division of the vestibulocochlear nerve. The incidence of vestibular schwannomas in the general population is roughly 1:100,000 [106,107]. The most well-documented risk factor for the development of vestibular schwannomas is in patients diagnosed with neurofibromatosis type 2 (NF2); however, these patients typically develop bilateral disease as well as multiple other tumors [108]. Patients commonly present with tinnitus, gait abnormalities, vertigo, and hearing loss. Pain is a less common clinical manifestation and is due to involvement of the trigeminal nerve. Treatment approaches for vestibular schwannoma include SRS, conventional RT, surgery, and observation.
6.2. Photon Radiosurgery
Stereotactic radiosurgery is associated with excellent rates of tumor control. In 2013, Hasegawa et al. published a retrospective study of 440 patients with vestibular schwannoma who were treated with Gamma Knife radiosurgery [42]. With a median follow-up of 12.5 years, the 5- and 10-year progression-free survival was 93% and 92%, respectively. No patients experienced a treatment failure more than 10 years after treatment. The 10-year facial nerve preservation rate was 97% in patients treated to a margin dose >13 Gy and 100% in patients treated to a margin dose of ≤ 13Gy. Ten patients (2.3%) developed delayed cyst formation.
6.3. Particle Radiosurgery
In 2003, Weber et al. published a retrospective series of 88 patients with vestibular schwannoma who were treated with proton SRS at the Harvard Cyclotron Laboratory (Cambridge, MA) [68]. The median dose was 12 CGE (range: 10–18 CGE) delivered over a median of 3 fractions (range: 2–4). The median tumor volume was 1.4 cc. Twenty-one (24%) and 67 (76%) patients had Gartner–Robertson Grade 1 or 2 versus Grade 3–5 or unknown hearing loss, respectively. Seventy-nine (89.8%) and nine (10.2%) patients were House–Brackmann Grade 1 or 2–5, respectively, and nine (10.2%) patients presented with trigeminal nerve dysfunction. Five-year tumor control rate was 93.6% (95% CI: 88.3–99.3%). Seven of 21 patients retained functional hearing after treatment, and 5-year facial nerve function preservation was 91.1% (95% CI: 85–97.6%). The 5-year trigeminal nerve preservation rate was 89.4% (95% CI: 82–96.7%). One patient on anticoagulation developed an extratumoral hemorrhage within the choroid plexus that required a craniotomy 19.1 months after proton SRS. Further details are presented in Table 1 and Table 2.
7. Meningioma
7.1. Background
Meningiomas are the most commonly diagnosed brain tumors in adults, representing approximately 20–30% of primary brain tumor diagnoses, and are seen in 7.8 per 100,000 people [100,109,110]. They arise from arachnoid cap cells within the dura and are largely benign (WHO Grade I) in nature. However, atypical (WHO Grade II) and anaplastic (WHO Grade III) meningiomas are associated with more aggressive behavior. Surgical intervention aimed at achieving a gross total resection is the standard treatment; however, the risk of recurrence remains high. Radiation therapy is commonly employed in both the definitive, adjuvant, and salvage settings.
7.2. Photon Radiosurgery
The role of SRS is largely in the definitive, adjuvant, and salvage settings for WHO Grade I meningiomas, while conventionally fractionated radiation therapy is generally preferred for WHO Grade II and Grade III lesions. In 2008, Kondziolka et al. published a study conducted at The University of Pittsburgh, where 972 patients with 1045 intracranial meningiomas were treated with SRS to a mean margin dose of 14 Gy over an 18-year period [23]. The overall tumor control rate in patients with WHO Grade I meningiomas was 93%, while control rates of 50% and 17% were observed in patients with WHO Grade II and Grade III meningiomas, respectively. Complications attributable to radiosurgery were observed in 76 patients (7.7%) at an average time until presentation of 11 months. In 2002, a multicenter study published by Santacroce et al. evaluated 4565 patients with 5300 benign meningiomas across 15 institutions who were treated with SRS to a median margin dose of 14 Gy [24]. With a median imaging follow-up of 63 months, an overall control rate of 92.5% was observed. Additionally, permanent morbidity was seen in 6.6% of patients following SRS.
7.3. Particle Radiosurgery
In 2011, Halasz et al. published a prospective study where 51 patients with 50 benign meningiomas were treated with proton radiosurgery at the Harvard Cyclotron Laboratory (Cambridge, MA, USA) [61]. Patients were treated to a median dose of 13 GyRBE (range: 10–15.5 GyRBE) prescribed to the 90% isodose line with a median prescription volume of 4.4 cc (range: 1.1–33 cc). With a median follow-up of 32 months, a 3-year tumor control rate of 94% (95% CI: 77–98%) and a median time to progression of 48 months was observed. Three patients (5.9%) experienced transient adverse effects, including facial pain and seizures that resolved with steroids and antiepileptic medications, respectively. Three patients (5.9%) developed permanent adverse effects, which included seizures in two patients requiring long-term use of antiepileptic medications and panhypopituitarism in another. No new cranial nerve deficits were observed after proton SRS. On univariate analysis, the presence of atypical histologic features was associated with a greater risk of tumor recurrence (p = 0.03). Further details are presented in Table 1 and Table 2.
8. Arteriovenous Malformation
8.1. Background
Arteriovenous malformations are vascular lesions that occur when high pressure arterial blood is shunted to the low-pressure venous system without passing through a capillary network. These malformations have a risk of spontaneous rupture over time. Autopsy studies have demonstrated a 0.6% prevalence of intracranial AVMs [111]. The most widely-used system for grading AVMs is the Spetzler–Martin scale, which is graded from 1–5 with higher grades correlating with worse outcomes [112]. Stereotactic radiosurgery is a treatment option for AVMs, which has been shown to successfully achieve lesion obliteration in many clinical scenarios. However, a major limitation of SRS in this setting is that AVM obliteration can take up to 2–4 years following treatment [113].
8.2. Photon Radiosurgery
In 2014, Kano et al. published a study of 474 patients with Spetzler–Martin Grade 3 AVMs who were treated with SRS at the University of Pittsburgh [114]. This study further stratified patients into Grade 3a (59%), 3b (9%), and 3c (31%) subgroups. With a median follow-up of 89 months, total obliteration rates based on angiographic or MRI criteria were 48%, 69%, and 72% at 3-, 4-, and 5-years post-SRS, respectively. The cumulative hemorrhage rate at 10-years was 9%. In 2005, Maruyama et al. published a retrospective study of 500 patients with cerebral AVMs who were treated with Gamma Knife radiosurgery with a median Spetzler–Martin Grade of 3 [115]. This study was designed to assess the rate of hemorrhage that occurred before radiosurgery, between radiosurgery and obliteration (latency period), and after obliteration. Forty-two hemorrhages occurred before radiosurgery, 23 during the latency period, and 6 following obliteration. The risk of hemorrhage decreased by 54% during the latency period compared to before radiosurgery (HR: 0.46; 95% CI: 0.25–0.80; p = 0.006) and by 88% after obliteration compared to before radiosurgery (HR: 0.12; 95% CI: 0.05–0.29; p < 0.001).
8.3. Particle Radiosurgery
In 1994, Seifert et al. published a retrospective series of 68 patients treated between 1980–1990 who were treated with proton SRS [64]. Their results were associated with a significant amount of morbidity and mortality, where 28.6% of patients experienced worsening of symptoms after SRS, such as increased frequency of seizures (7 patients), hemorrhage of the irradiated AVM (6 patients of whom two died), and progressive neurologic deficits (6 patients). Additionally, no AVM larger than 3 cm was successfully obliterated with SRS. In 2005, Vernimmen et al. published a retrospective series of 64 patients who were treated for cerebral AVMs with proton SRS from 1993–2003 [67]. The median AVM volume was 16.3 cc (range: 1.7–110.6 cc); 3%, 17%, 30%, 42%, and 8% of AVMs were Spetzler–Martin Grade 1, 2, 3, 4, and 5, respectively, and the median follow-up was 62 months. Patients were treated in 2–3 fractions. Dose was based on AVM size: mean dose 27.2 SFEcGyE (<10 cc), mean dose 23.2 SFEcGyE (10–13.9 cc), and mean dose 27 SFEcGyE (≥14 cc). Patients were stratified by AVM size into two groups: (1) <14 cc and (2) ≥14 cc. In the former, 67% and 17% achieved an obliteration and partial response, respectively. In the latter, 43% and 21% achieved an obliteration and partial response, respectively. Transient late effects were observed in 23% of patients and 6% developed a permanent late Grade 3 or 4 toxicity, such as epilepsy and permanent neurologic deficits. In 1993, Barker et al. published a retrospective series of 1250 patients treated with proton SRS between 1965–1993 at the Harvard Cyclotron Laboratory (Cambridge, MA, USA) [97]. Patients were treated with a single fraction median dose of 10.5 Gy (range: 4–65 Gy). Treatment-related complications consisted of hemiparesis in 24 patients, visual field deficits in 11 patients, cognitive dysfunction in 8 patients, ataxia in 4 patients, speech deficits in 3 patients, hemisensory deficits in 2 patients, and hearing loss in 1 patient. Additionally, multiple patients had more than one of the aforementioned complications, three had a global deterioration in neurologic function, and four had a disabling increase in headache severity. Complications presented 0.2–6.8 years after treatment with a 10-year actuarial incidence of 4.5%.
In 1990, Steinberg et al. published a retrospective study of 35 patients treated from 1983–1989 with helium ion radiosurgery to cerebral angiographically occult vascular malformations [98]. Initially, high doses of 45 GyE were used, which were subsequently changed to 10–15 GyE. While the data were limited, 27 patients in “excellent” or “good” condition prior to SRS remained stable or improved neurologically, 2 patients in “poor” condition who received previous fractionated RT died at 9- and 14-months post-SRS, 7 patients experienced neurologic deterioration due to recurrent AVM hemorrhage, and 4 patients worsened clinically 3–12 months after SRS. Further details are presented in Table 1 and Table 2.
9. Conclusions
Stereotactic radiosurgery with the use of photons is a highly effective and safe treatment modality for managing multiple benign and malignant intracranial pathologies. There exists limited data utilizing particle radiosurgery for intracranial lesions. The vast majority of available data are single institution retrospective studies that utilized protons. Furthermore, there is a marked paucity of data exploring the use of heavy particles in the radiosurgical setting. While there are theoretical benefits to using particles over photons for intracranial radiosurgical applications, prospective data are needed to validate the safety and efficacy of this treatment modality. Presently, there are a great paucity of prospective trials studying this therapeutic modality in the intracranial setting. However, there has been an increased focus on utilizing this therapy in extracranial locations. As such, there are presently clinical trials underway utilizing proton stereotactic body radiation therapy in the management of NSCLC and liver metastases. Particle-based radiosurgery offers opportunities to improve the therapeutic ratio through, amongst other factors, dose escalation to the target, reduction in dose to surrounding tissues, and more favorable radiobiological effects, regardless of target tissue type or cell cycle. However, the therapeutic ratio remains excellent for photon radiosurgery and further studies aimed at comparative effectiveness between these two modalities are needed to further elucidate the validity these hypotheses. In select patients who have received previous radiation therapy and have lesions located in highly eloquent locations, particle radiosurgery may be a suitable alternative to photons. Additionally, further study exploring dose relationships in the setting of proton SRS are needed.
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| DOAJ | Directory of Open Access Journals |
| SRS | Stereotactic radiosurgery |
| FSRT | Fractionated stereotactic radiation therapy |
| WBRT | Whole brain radiation therapy |
| CNS | Central nervous system |
| STAR | Stereotactic alignment in radiosurgery |
| SOBP | Spread out Bragg Peak |
| IMPT | Intensity modulated proton therapy |
| DNA | Deoxyribonucleic acid |
| RBE | Relative biological effectiveness |
| Gy | Gray |
| MRI | Magnetic resonance imaging |
| CI | Confidence interval |
| USA | United States of America |
| cc | Cubic centimeters |
| HR | Hazard ratio |
| NSCLC | Non-small cell lung cancer |
| RCC | Renal cell carcinoma |
| HN | Head and neck |
| SCLC | Small cell lung cancer |
| GI | Gastrointestinal |
| GYN | Gynecologic |
| RT | Radiation therapy |
| KPS | Karnofsky Performance Status |
| BrM | Brain metastases |
| F/U | Follow up |
| STR | Subtotal resection |
| GTR | Gross total resection |
| ACTH | Adrenocorticotropic hormone |
| AVM | Arteriovenous malformation |
| CGE | Cobalt gray equivalent |
| SM | Spetzler–Martin |
| GR | Gardner–Robertson |
| HB | House–Brackmann |
| Pt | Patient |
| GKRS | Gamma Knife radiosurgery |
| NF2 | Neurofibromatosis type 2 |
| WHO | World Health Organization |
Author Contributions
Conceptualization, E.J.L. and D.M.T.; methodology, E.J.L. and D.M.T.; software, E.J.L.; investigation, E.J.L.; resources, D.M.T.; writing—original draft preparation, E.J.L., A.V.P., K.K.S. and D.M.T.; writing—review and editing, E.J.L., A.V.P., K.K.S., S.L., H.R.-G., J.L.P., C.B., K.F., D.S., J.P.S. and D.M.T.; visualization, E.J.L. and D.M.T.; supervision, D.M.T.; project administration, D.M.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951;102:316–319. [PubMed] [Google Scholar]
- 2.Lehrer E.J., McGee H.M., Sheehan J.P., Trifiletti D.M. Integration of immuno-oncology with stereotactic radiosurgery in the management of brain metastases. J. Neuro Oncol. 2020:1–10. doi: 10.1007/s11060-020-03427-6. [DOI] [PubMed] [Google Scholar]
- 3.Lehrer E.J., Snyder M.H., Desai B., Li C.E., Narayan A., Trifiletti D.M., Schlesinger D., Sheehan J.P. Clinical and radiographic adverse events after Gamma Knife radiosurgery for brainstem lesions: A dosimetric analysis. Radiother. Oncol. 2020;147:200–209. doi: 10.1016/j.radonc.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Minniti G., Esposito V., Clarke E., Scaringi C., Lanzetta G., Salvati M., Raco A., Bozzao A., Enrici R.M. Multidose stereotactic radiosurgery (9 Gy × 3) of the postoperative resection cavity for treatment of large brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 2013;86:623–629. doi: 10.1016/j.ijrobp.2013.03.037. [DOI] [PubMed] [Google Scholar]
- 5.Minniti G., Scaringi C., Paolini S., Lanzetta G., Romano A., Cicone F., Osti M., Enrici R.M., Esposito V. Single-Fraction Versus Multifraction (3 × 9 Gy) Stereotactic Radiosurgery for Large (>2 cm) Brain Metastases: A Comparative Analysis of Local Control and Risk of Radiation-Induced Brain Necrosis. Int. J. Radiat. Oncol. Biol. Phys. 2016;95:1142–1148. doi: 10.1016/j.ijrobp.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Trifiletti D.M., Lee C.-C., Kano H., Cohen J., Janopaul-Naylor J., Alonso-Basanta M., Lee J.Y., Simonova G., Liscak R., Wolf A., et al. Stereotactic Radiosurgery for Brainstem Metastases: An International Cooperative Study to Define Response and Toxicity. Int. J. Radiat. Oncol. 2016;96:280–288. doi: 10.1016/j.ijrobp.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kotecha R., Sahgal A., Rubens M., De Salles A., Fariselli L., E Pollock B., Levivier M., Ma L., Paddick I., Regis J., et al. Stereotactic radiosurgery for non-functioning pituitary adenomas: Meta-analysis and International Stereotactic Radiosurgery Society practice opinion. Neuro Oncol. 2020;22:318–332. doi: 10.1093/neuonc/noz225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lehrer E.J., McGee H.M., Peterson J.L., Vallow L., Garcia H.R., Zaorsky N.G., Sharma S., Trifiletti D.M. Stereotactic Radiosurgery and Immune Checkpoint Inhibitors in the Management of Brain Metastases. Int. J. Mol. Sci. 2018;19:3054. doi: 10.3390/ijms19103054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehrer E.J., Peterson J., Brown P.D., Sheehan J.P., Quiñones-Hinojosa A., Zaorsky N.G., Trifiletti D.M. Treatment of brain metastases with stereotactic radiosurgery and immune checkpoint inhibitors: An international meta-analysis of individual patient data. Radiother Oncol. 2018;130:104–112. doi: 10.1016/j.radonc.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 10.Lehrer E.J., Peterson J.L., Zaorsky N.G., Brown P.D., Sahgal A., Chiang V.L., Chao S.T., Sheehan J.P., Trifiletti D.M. Single versus Multifraction Stereotactic Radiosurgery for Large Brain Metastases: An International Meta-analysis of 24 Trials. Int. J. Radiat. Oncol. 2019;103:618–630. doi: 10.1016/j.ijrobp.2018.10.038. [DOI] [PubMed] [Google Scholar]
- 11.Brown P.D., Ballman K.V., Cerhan J.H., Anderson S.K., Carrero X.W., Whitton A.C., Greenspoon J., Parney I.F., Laack N.N.I., Ashman J.B., et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC.3): A multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017;18:1049–1060. doi: 10.1016/S1470-2045(17)30441-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown P.D., Jaeckle K., Ballman K.V., Farace E., Cerhan J.H., Anderson S.K., Carrero X.W., Barker F.G., 2nd, Deming R., Burri S.H., et al. Effect of Radiosurgery Alone vs Radiosurgery With Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial. JAMA. 2016;316:401–409. doi: 10.1001/jama.2016.9839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang E.L., Wefel J.S., Hess K.R., Allen P.K., Lang F.F., Kornguth D.G., Arbuckle R.B., Swint J.M., Shiu A.S., Maor M.H., et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol. 2009;10:1037–1044. doi: 10.1016/S1470-2045(09)70263-3. [DOI] [PubMed] [Google Scholar]
- 14.Andrews D.W., Scott C.B., Sperduto P.W., Flanders A.E., Gaspar L.E., Schell M.C., Werner-Wasik M., Demas W., Ryu J., Bahary J.P., et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: Phase III results of the RTOG 9508 randomised trial. Lancet. 2004;363:1665–1672. doi: 10.1016/S0140-6736(04)16250-8. [DOI] [PubMed] [Google Scholar]
- 15.Shaw E., Scott C., Souhami L., Dinapoli R., Bahary J.P., Kline R., Wharam M., Schultz C., Davey P., Loeffler J., et al. Radiosurgery for the treatment of previously irradiated recurrent primary brain tumors and brain metastases: Initial report of radiation therapy oncology group protocol (90-05) Int. J. Radiat. Oncol. Biol. Phys. 1996;34:647–654. doi: 10.1016/0360-3016(95)02106-X. [DOI] [PubMed] [Google Scholar]
- 16.Shaw E., Scott C., Souhami L., Dinapoli R., Kline R., Loeffler J., Farnan N. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: Final report of RTOG protocol 90-05. Int. J. Radiat. Oncol. Biol. Phys. 2000;47:291–298. doi: 10.1016/S0360-3016(99)00507-6. [DOI] [PubMed] [Google Scholar]
- 17.Stafford S.L., Perry A., Suman V.J., Meyer F.B., Scheithauer B.W., Lohse C.M., Shaw E.G. Primarily resected meningiomas: Outcome and prognostic factors in 581 Mayo Clinic patients, 1978 through 1988. Mayo. Clin. Proc. 1998;73:936–942. doi: 10.4065/73.10.936. [DOI] [PubMed] [Google Scholar]
- 18.Kano H., Takahashi J.A., Katsuki T., Araki N., Oya N., Hiraoka M., Hashimoto N. Stereotactic radiosurgery for atypical and anaplastic meningiomas. J. Neurooncol. 2007;84:41–47. doi: 10.1007/s11060-007-9338-y. [DOI] [PubMed] [Google Scholar]
- 19.Choi C.Y., Soltys S.G., Gibbs I.C., Harsh G.R., Jackson P.S., Lieberson R.E., Chang S.D., Adler J.R. Cyberknife stereotactic radiosurgery for treatment of atypical (WHO grade II) cranial meningiomas. Neurosurgery. 2010;67:1180–1188. doi: 10.1227/NEU.0b013e3181f2f427. [DOI] [PubMed] [Google Scholar]
- 20.Lee J.Y., Niranjan A., McInerney J., Kondziolka D., Flickinger J.C., Lunsford L.D. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. J. Neurosurg. 2002;97:65–72. doi: 10.3171/jns.2002.97.1.0065. [DOI] [PubMed] [Google Scholar]
- 21.Spiegelmann R., Cohen Z.R., Nissim O., Alezra D., Pfeffer R. Cavernous sinus meningiomas: A large LINAC radiosurgery series. J. Neurooncol. 2010;98:195–202. doi: 10.1007/s11060-010-0173-1. [DOI] [PubMed] [Google Scholar]
- 22.Skeie B.S., Enger P.O., Skeie G.O., Thorsen F., Pedersen P.H. Gamma knife surgery of meningiomas involving the cavernous sinus: Long-term follow-up of 100 patients. Neurosurgery. 2010;66:661–668; discussion 668–669. doi: 10.1227/01.NEU.0000366112.04015.E2. [DOI] [PubMed] [Google Scholar]
- 23.Kondziolka D., Mathieu D., Lunsford L.D., Martin J.J., Madhok R., Niranjan A., Flickinger J.C. Radiosurgery as definitive management of intracranial meningiomas. Neurosurgery. 2008;62:53–58; discussion 58–60. doi: 10.1227/01.NEU.0000311061.72626.0D. [DOI] [PubMed] [Google Scholar]
- 24.Santacroce A., Walier M., Regis J., Liscak R., Motti E., Lindquist C., Kemeny A., Kitz K., Lippitz B., Martinez Alvarez R., et al. Long-term tumor control of benign intracranial meningiomas after radiosurgery in a series of 4565 patients. Neurosurgery. 2012;70:32–39; discussion 39. doi: 10.1227/NEU.0b013e31822d408a. [DOI] [PubMed] [Google Scholar]
- 25.Sheehan J.P., Pouratian N., Steiner L., Laws E.R., Vance M.L. Gamma Knife surgery for pituitary adenomas: Factors related to radiological and endocrine outcomes. J. Neurosurg. 2011;114:303–309. doi: 10.3171/2010.5.JNS091635. [DOI] [PubMed] [Google Scholar]
- 26.Minniti G., Osti M.F., Niyazi M. Target delineation and optimal radiosurgical dose for pituitary tumors. Radiat. Oncol. 2016;11:135. doi: 10.1186/s13014-016-0710-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kong D.S., Lee J.I., Lim D.H., Kim K.W., Shin H.J., Nam D.H., Park K., Kim J.H. The efficacy of fractionated radiotherapy and stereotactic radiosurgery for pituitary adenomas: Long-term results of 125 consecutive patients treated in a single institution. Cancer. 2007;110:854–860. doi: 10.1002/cncr.22860. [DOI] [PubMed] [Google Scholar]
- 28.Singh R., Didwania P., Lehrer E.J., Sheehan D., Sheehan K., Trifiletti D.M., Sheehan J.P. Stereotactic radiosurgery for acromegaly: An international systematic review and meta-analysis of clinical outcomes. J. Neurooncol. 2020 doi: 10.1007/s11060-020-03552-2. [DOI] [PubMed] [Google Scholar]
- 29.Sheehan J.P., Xu Z., Salvetti D.J., Schmitt P.J., Vance M.L. Results of gamma knife surgery for Cushing’s disease. J. Neurosurg. 2013;119:1486–1492. doi: 10.3171/2013.7.JNS13217. [DOI] [PubMed] [Google Scholar]
- 30.Sheehan J.P., Starke R.M., Mathieu D., Young B., Sneed P.K., Chiang V.L., Lee J.Y., Kano H., Park K.J., Niranjan A., et al. Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: A multicenter study. J. Neurosurg. 2013;119:446–456. doi: 10.3171/2013.3.JNS12766. [DOI] [PubMed] [Google Scholar]
- 31.Flickinger J.C., Pollock B.E., Kondziolka D., Phuong L.K., Foote R.L., Stafford S.L., Lunsford L.D. Does increased nerve length within the treatment volume improve trigeminal neuralgia radiosurgery? A prospective double-blind, randomized study. Int. J. Radiat. Oncol. Biol. Phys. 2001;51:449–454. doi: 10.1016/S0360-3016(01)01606-6. [DOI] [PubMed] [Google Scholar]
- 32.Kotecha R., Kotecha R., Modugula S., Murphy E.S., Jones M., Kotecha R., Reddy C.A., Suh J.H., Barnett G.H., Neyman G., et al. Trigeminal Neuralgia Treated With Stereotactic Radiosurgery: The Effect of Dose Escalation on Pain Control and Treatment Outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2016;96:142–148. doi: 10.1016/j.ijrobp.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 33.Smith Z.A., Gorgulho A.A., Bezrukiy N., McArthur D., Agazaryan N., Selch M.T., De Salles A.A. Dedicated linear accelerator radiosurgery for trigeminal neuralgia: A single-center experience in 179 patients with varied dose prescriptions and treatment plans. Int. J. Radiat. Oncol. Biol. Phys. 2011;81:225–231. doi: 10.1016/j.ijrobp.2010.05.058. [DOI] [PubMed] [Google Scholar]
- 34.Herman J.M., Petit J.H., Amin P., Kwok Y., Dutta P.R., Chin L.S. Repeat gamma knife radiosurgery for refractory or recurrent trigeminal neuralgia: Treatment outcomes and quality-of-life assessment. Int. J. Radiat. Oncol. Biol. Phys. 2004;59:112–116. doi: 10.1016/j.ijrobp.2003.10.041. [DOI] [PubMed] [Google Scholar]
- 35.Leon J., Lehrer E.J., Peterson J., Vallow L., Ruiz-Garcia H., Hadley A., Herchko S., Lundy L., Chaichana K., Vibhute P., et al. Observation or stereotactic radiosurgery for newly diagnosed vestibular schwannomas: A systematic review and meta-analysis. J. Radiosurg. SBRT. 2019;6:91–100. [PMC free article] [PubMed] [Google Scholar]
- 36.Leon J., Trifiletti D.M., Waddle M.R., Vallow L., Ko S., May B., Tzou K., Ruiz-Garcia H., Lundy L., Chaichana K., et al. Trends in the initial management of vestibular schwannoma in the United States. J. Clin. Neurosci. 2019;68:174–178. doi: 10.1016/j.jocn.2019.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Breivik C.N., Nilsen R.M., Myrseth E., Pedersen P.H., Varughese J.K., Chaudhry A.A., Lund-Johansen M. Conservative management or gamma knife radiosurgery for vestibular schwannoma: Tumor growth, symptoms, and quality of life. Neurosurgery. 2013;73:48–56; discussion 56–57. doi: 10.1227/01.neu.0000429862.50018.b9. [DOI] [PubMed] [Google Scholar]
- 38.Pollock B.E., Driscoll C.L., Foote R.L., Link M.J., Gorman D.A., Bauch C.D., Mandrekar J.N., Krecke K.N., Johnson C.H. Patient outcomes after vestibular schwannoma management: A prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery. 2006;59:77–85; discussion 77–85. doi: 10.1227/01.NEU.0000219217.14930.14. [DOI] [PubMed] [Google Scholar]
- 39.Maniakas A., Saliba I. Microsurgery versus stereotactic radiation for small vestibular schwannomas: A meta-analysis of patients with more than 5 years’ follow-up. Otol. Neurotol. 2012;33:1611–1620. doi: 10.1097/MAO.0b013e31826dbd02. [DOI] [PubMed] [Google Scholar]
- 40.Regis J., Pellet W., Delsanti C., Dufour H., Roche P.H., Thomassin J.M., Zanaret M., Peragut J.C. Functional outcome after gamma knife surgery or microsurgery for vestibular schwannomas. J. Neurosurg. 2002;97:1091–1100. doi: 10.3171/jns.2002.97.5.1091. [DOI] [PubMed] [Google Scholar]
- 41.Lunsford L.D., Niranjan A., Flickinger J.C., Maitz A., Kondziolka D. Radiosurgery of vestibular schwannomas: Summary of experience in 829 cases. J. Neurosurg. 2005;102:195–199. doi: 10.3171/sup.2005.102.s_supplement.0195. [DOI] [PubMed] [Google Scholar]
- 42.Hasegawa T., Kida Y., Kato T., Iizuka H., Kuramitsu S., Yamamoto T. Long-term safety and efficacy of stereotactic radiosurgery for vestibular schwannomas: Evaluation of 440 patients more than 10 years after treatment with Gamma Knife surgery. J. Neurosurg. 2013;118:557–565. doi: 10.3171/2012.10.JNS12523. [DOI] [PubMed] [Google Scholar]
- 43.Carlson M.L., Jacob J.T., Pollock B.E., Neff B.A., Tombers N.M., Driscoll C.L., Link M.J. Long-term hearing outcomes following stereotactic radiosurgery for vestibular schwannoma: Patterns of hearing loss and variables influencing audiometric decline. J. Neurosurg. 2013;118:579–587. doi: 10.3171/2012.9.JNS12919. [DOI] [PubMed] [Google Scholar]
- 44.Yang H.C., Kano H., Awan N.R., Lunsford L.D., Niranjan A., Flickinger J.C., Novotny J., Jr., Bhatnagar J.P., Kondziolka D. Gamma Knife radiosurgery for larger-volume vestibular schwannomas. Clinical article. J. Neurosurg. 2011;114:801–807. doi: 10.3171/2010.8.JNS10674. [DOI] [PubMed] [Google Scholar]
- 45.Andrews D.W., Suarez O., Goldman H.W., Downes M.B., Bednarz G., Corn B.W., Werner-Wasik M., Rosenstock J., Curran W.J., Jr. Stereotactic radiosurgery and fractionated stereotactic radiotherapy for the treatment of acoustic schwannomas: Comparative observations of 125 patients treated at one institution. Int. J. Radiat. Oncol. Biol. Phys. 2001;50:1265–1278. doi: 10.1016/S0360-3016(01)01559-0. [DOI] [PubMed] [Google Scholar]
- 46.Combs S.E., Welzel T., Schulz-Ertner D., Huber P.E., Debus J. Differences in clinical results after LINAC-based single-dose radiosurgery versus fractionated stereotactic radiotherapy for patients with vestibular schwannomas. Int. J. Radiat. Oncol. Biol. Phys. 2010;76:193–200. doi: 10.1016/j.ijrobp.2009.01.064. [DOI] [PubMed] [Google Scholar]
- 47.Meijer O.W., Vandertop W.P., Baayen J.C., Slotman B.J. Single-fraction vs. fractionated linac-based stereotactic radiosurgery for vestibular schwannoma: A single-institution study. Int. J. Radiat. Oncol. Biol. Phys. 2003;56:1390–1396. doi: 10.1016/S0360-3016(03)00444-9. [DOI] [PubMed] [Google Scholar]
- 48.Kurita H., Kawamoto S., Sasaki T., Shin M., Tago M., Terahara A., Ueki K., Kirino T. Results of radiosurgery for brain stem arteriovenous malformations. J. Neurol. Neurosurg. Psychiatry. 2000;68:563–570. doi: 10.1136/jnnp.68.5.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Starke R.M., Yen C.P., Ding D., Sheehan J.P. A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: Analysis of 1012 treated patients. J. Neurosurg. 2013;119:981–987. doi: 10.3171/2013.5.JNS1311. [DOI] [PubMed] [Google Scholar]
- 50.Pollock B.E., Gorman D.A., Brown P.D. Radiosurgery for arteriovenous malformations of the basal ganglia, thalamus, and brainstem. J. Neurosurg. 2004;100:210–214. doi: 10.3171/jns.2004.100.2.0210. [DOI] [PubMed] [Google Scholar]
- 51.Kano H., Kondziolka D., Flickinger J.C., Yang H.C., Flannery T.J., Niranjan A., Novotny J., Jr., Lunsford L.D. Stereotactic radiosurgery for arteriovenous malformations, Part 4: Management of basal ganglia and thalamus arteriovenous malformations. J. Neurosurg. 2012;116:33–43. doi: 10.3171/2011.9.JNS11175. [DOI] [PubMed] [Google Scholar]
- 52.Cohen-Inbar O., Starke R.M., Lee C.-C., Kano H., Huang P., Kondziolka D., Grills I.S., Silva D., Abbassy M., Missios S., et al. Stereotactic Radiosurgery for Brainstem Arteriovenous Malformations: A Multicenter Study. Neurosurgery. 2017;81:910–920. doi: 10.1093/neuros/nyx189. [DOI] [PubMed] [Google Scholar]
- 53.Vellayappan B., Tan C.L., Yong C., Khor L.K., Koh W.Y., Yeo T.T., Detsky J., Lo S., Sahgal A. Diagnosis and Management of Radiation Necrosis in Patients With Brain Metastases. Front. Oncol. 2018;8:395. doi: 10.3389/fonc.2018.00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown P.D., Gondi V. Irrational fear of whole-brain radiotherapy: Are we doing our patients a disservice? Cancer. 2018;124:3468–3473. doi: 10.1002/cncr.31649. [DOI] [PubMed] [Google Scholar]
- 55.Brown P.D., Pugh S., Laack N.N., Wefel J.S., Khuntia D., Meyers C., Choucair A., Fox S., Suh J.H., Roberge D., et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: A randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15:1429–1437. doi: 10.1093/neuonc/not114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gondi V., Pugh S.L., Tome W.A., Caine C., Corn B., Kanner A., Rowley H., Kundapur V., DeNittis A., Greenspoon J.N., et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): A phase II multi-institutional trial. J. Clin. Oncol. 2014;32:3810–3816. doi: 10.1200/JCO.2014.57.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brown P.D., Gondi V., Pugh S., Tome W.A., Wefel J.S., Armstrong T.S., Bovi J.A., Robinson C., Konski A., Khuntia D., et al. Hippocampal Avoidance During Whole-Brain Radiotherapy Plus Memantine for Patients With Brain Metastases: Phase III Trial NRG Oncology CC001. J. Clin. Oncol. 2020;38:1019–1029. doi: 10.1200/JCO.19.02767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Golden E.B., Demaria S., Schiff P.B., Chachoua A., Formenti S.C. An abscopal response to radiation and ipilimumab in a patient with metastatic non-small cell lung cancer. Cancer Immunol. Res. 2013;1:365–372. doi: 10.1158/2326-6066.CIR-13-0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Golden E.B., Pellicciotta I., Demaria S., Barcellos-Hoff M.H., Formenti S.C. The convergence of radiation and immunogenic cell death signaling pathways. Front. Oncol. 2012;2:88. doi: 10.3389/fonc.2012.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Atkins K.M., Pashtan I.M., Bussiere M.R., Kang K.H., Niemierko A., Daly J.E., Botticello T.M., Hurd M.C., Chapman P.H., Oh K., et al. Proton Stereotactic Radiosurgery for Brain Metastases: A Single-Institution Analysis of 370 Patients. Int. J. Radiat. Oncol. Biol. Phys. 2018;101:820–829. doi: 10.1016/j.ijrobp.2018.03.056. [DOI] [PubMed] [Google Scholar]
- 61.Halasz L.M., Bussiere M.R., Dennis E.R., Niemierko A., Chapman P.H., Loeffler J.S., Shih H.A. Proton stereotactic radiosurgery for the treatment of benign meningiomas. Int. J. Radiat. Oncol. Biol. Phys. 2011;81:1428–1435. doi: 10.1016/j.ijrobp.2010.07.1991. [DOI] [PubMed] [Google Scholar]
- 62.Petit J.H., Biller B.M., Coen J.J., Swearingen B., Ancukiewicz M., Bussiere M., Chapman P., Klibanski A., Loeffler J.S. Proton stereotactic radiosurgery in management of persistent acromegaly. Endocr. Pract. 2007;13:726–734. doi: 10.4158/EP.13.7.726. [DOI] [PubMed] [Google Scholar]
- 63.Petit J.H., Biller B.M., Yock T.I., Swearingen B., Coen J.J., Chapman P., Ancukiewicz M., Bussiere M., Klibanski A., Loeffler J.S. Proton stereotactic radiotherapy for persistent adrenocorticotropin-producing adenomas. J. Clin. Endocrinol. Metab. 2008;93:393–399. doi: 10.1210/jc.2007-1220. [DOI] [PubMed] [Google Scholar]
- 64.Seifert V., Stolke D., Mehdorn H.M., Hoffmann B. Clinical and radiological evaluation of long-term results of stereotactic proton beam radiosurgery in patients with cerebral arteriovenous malformations. J. Neurosurg. 1994;81:683–689. doi: 10.3171/jns.1994.81.5.0683. [DOI] [PubMed] [Google Scholar]
- 65.Sikuade M.J., Salvi S., Rundle P.A., Errington D.G., Kacperek A., Rennie I.G. Outcomes of treatment with stereotactic radiosurgery or proton beam therapy for choroidal melanoma. Eye. 2015;29:1194–1198. doi: 10.1038/eye.2015.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Silander H., Pellettieri L., Enblad P., Montelius A., Grusell E., Vallhagen-Dahlgren C., Isacsson U., Nyberg G., Mostrom U., Lilja A., et al. Fractionated, stereotactic proton beam treatment of cerebral arteriovenous malformations. Acta Neurol. Scand. 2004;109:85–90. doi: 10.1046/j.1600-0404.2003.00154.x. [DOI] [PubMed] [Google Scholar]
- 67.Vernimmen F.J., Slabbert J.P., Wilson J.A., Fredericks S., Melvill R. Stereotactic proton beam therapy for intracranial arteriovenous malformations. Int. J. Radiat. Oncol. Biol. Phys. 2005;62:44–52. doi: 10.1016/j.ijrobp.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 68.Weber D.C., Chan A.W., Bussiere M.R., Harsh G.R.T., Ancukiewicz M., Barker F.G., 2nd, Thornton A.T., Martuza R.L., Nadol J.B., Jr., Chapman P.H., et al. Proton beam radiosurgery for vestibular schwannoma: Tumor control and cranial nerve toxicity. Neurosurgery. 2003;53:577–586. doi: 10.1227/01.NEU.0000079369.59219.C0. [DOI] [PubMed] [Google Scholar]
- 69.Allen C., Borak T.B., Tsujii H., Nickoloff J.A. Heavy charged particle radiobiology: Using enhanced biological effectiveness and improved beam focusing to advance cancer therapy. Mutat. Res. 2011;711:150–157. doi: 10.1016/j.mrfmmm.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Weber U., Kraft G. Comparison of carbon ions versus protons. Cancer J. 2009;15:325–332. doi: 10.1097/PPO.0b013e3181b01935. [DOI] [PubMed] [Google Scholar]
- 71.Lin M.H., Yang M., Dougherty J., Tasson A., Zhang Y., Mohamad O., Dan T., Yan Y., Gu X., Timmerman R., et al. Radiation Therapy for Pediatric Brain Tumors using Robotic Radiation Delivery System and Intensity Modulated Proton Therapy. Pract. Radiat. Oncol. 2020;10:e173–e182. doi: 10.1016/j.prro.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 72.Suit H., DeLaney T., Goldberg S., Paganetti H., Clasie B., Gerweck L., Niemierko A., Hall E., Flanz J., Hallman J., et al. Proton vs carbon ion beams in the definitive radiation treatment of cancer patients. Radiother. Oncol. 2010;95:3–22. doi: 10.1016/j.radonc.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 73.Mitin T., Zietman A.L. Promise and pitfalls of heavy-particle therapy. J. Clin. Oncol. 2014;32:2855–2863. doi: 10.1200/JCO.2014.55.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Malouff T.D., Mahajan A., Krishnan S., Beltran C., Seneviratne D.S., Trifiletti D.M. Carbon Ion Therapy: A Modern Review of an Emerging Technology. Front. Oncol. 2020;10:82. doi: 10.3389/fonc.2020.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nickoloff J.A. Photon, light ion, and heavy ion cancer radiotherapy: Paths from physics and biology to clinical practice. Ann. Transl. Med. 2015;3:336. doi: 10.3978/j.issn.2305-5839.2015.12.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ebner D.K., Kamada T. The Emerging Role of Carbon-Ion Radiotherapy. Front. Oncol. 2016;6:140. doi: 10.3389/fonc.2016.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Paganetti H. Range uncertainties in proton therapy and the role of Monte Carlo simulations. Phys. Med. Biol. 2012;57:R99–R117. doi: 10.1088/0031-9155/57/11/R99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Newhauser W.D., Zhang R. The physics of proton therapy. Phys. Med. Biol. 2015;60:R155–R209. doi: 10.1088/0031-9155/60/8/R155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chuong M., Badiyan S.N., Yam M., Li Z., Langen K., Regine W., Morris C., Snider J., 3rd, Mehta M., Huh S., et al. Pencil beam scanning versus passively scattered proton therapy for unresectable pancreatic cancer. J. Gastrointest Oncol. 2018;9:687–693. doi: 10.21037/jgo.2018.03.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chang J.Y., Zhang X., Knopf A., Li H., Mori S., Dong L., Lu H.M., Liu W., Badiyan S.N., Both S., et al. Consensus Guidelines for Implementing Pencil-Beam Scanning Proton Therapy for Thoracic Malignancies on Behalf of the PTCOG Thoracic and Lymphoma Subcommittee. Int. J. Radiat. Oncol. Biol. Phys. 2017;99:41–50. doi: 10.1016/j.ijrobp.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 81.Wroe A.J., Bush D.A., Schulte R.W., Slater J.D. Clinical immobilization techniques for proton therapy. Technol. Cancer Res. Treat. 2015;14:71–79. doi: 10.7785/tcrt.2012.500398. [DOI] [PubMed] [Google Scholar]
- 82.Tobias C.A., Anger H.O., Lawrence J.H. Radiological use of high energy deuterons and alpha particles. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1952;67:1–27. [PubMed] [Google Scholar]
- 83.Lawrence J.H., Tobias C.A., Born J.L., Mc C.R., Roberts J.E., Anger H.O., Low-Beer B.V., Huggins C.B. Pituitary irradiation with high-energy proton beams: A preliminary report. Cancer Res. 1958;18:121–134. [PubMed] [Google Scholar]
- 84.Lyman J.T., Phillips M.H., Frankel K.A., Fabrikant J.I. Stereotactic frame for neuroradiology and charged particle Bragg peak radiosurgery of intracranial disorders. Int. J. Radiat. Oncol. Biol. Phys. 1989;16:1615–1621. doi: 10.1016/0360-3016(89)90971-1. [DOI] [PubMed] [Google Scholar]
- 85.Fabrikant J.I., Levy R.P., Steinberg G.K., Phillips M.H., Frankel K.A., Lyman J.T., Marks M.P., Silverberg G.D. Charged-particle radiosurgery for intracranial vascular malformations. Neurosurg. Clin. N Am. 1992;3:99–139. doi: 10.1016/S1042-3680(18)30685-5. [DOI] [PubMed] [Google Scholar]
- 86.DeLaney T.F. Clinical proton radiation therapy research at the Francis H. Burr Proton Therapy Center. Technol. Cancer Res. Treat. 2007;6:61–66. doi: 10.1177/15330346070060S410. [DOI] [PubMed] [Google Scholar]
- 87.Furlow B. Dosimetric promise versus cost: Critics question proton therapy. Lancet Oncol. 2013;14:805–806. doi: 10.1016/S1470-2045(13)70314-0. [DOI] [PubMed] [Google Scholar]
- 88.Verma V., Shah C., Rwigema J.C., Solberg T., Zhu X., Simone C.B., 2nd Cost-comparativeness of proton versus photon therapy. Chin. Clin. Oncol. 2016;5:56. doi: 10.21037/cco.2016.06.03. [DOI] [PubMed] [Google Scholar]
- 89.Arvold N.D., Lee E.Q., Mehta M.P., Margolin K., Alexander B.M., Lin N.U., Anders C.K., Soffietti R., Camidge D.R., Vogelbaum M.A., et al. Updates in the management of brain metastases. Neuro Oncol. 2016;18:1043–1065. doi: 10.1093/neuonc/now127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nabors L.B., Portnow J., Ammirati M., Baehring J., Brem H., Butowski N., Fenstermaker R.A., Forsyth P., Hattangadi-Gluth J., Holdhoff M., et al. NCCN Practice Guidelines in Oncology—Central Nervous System Cancers, Version 1.2017. J. Natl. Compregensive Cancer Netw. 2017;15:1311–1345. doi: 10.6004/jnccn.2017.0166. [DOI] [PubMed] [Google Scholar]
- 91.Barnholtz-Sloan J.S., Sloan A.E., Davis F.G., Vigneau F.D., Lai P., Sawaya R.E. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J. Clin. Oncol. 2004;22:2865–2872. doi: 10.1200/JCO.2004.12.149. [DOI] [PubMed] [Google Scholar]
- 92.Kohler B.A., Ward E., McCarthy B.J., Schymura M.J., Ries L.A., Eheman C., Jemal A., Anderson R.N., Ajani U.A., Edwards B.K. Annual report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. J. Natl. Cancer Inst. 2011;103:714–736. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Singh R., Stoltzfus K.C., Chen H., Louie A.V., Lehrer E.J., Horn S.R., Palmer J.D., Trifiletti D.M., Brown P.D., Zaorsky N.G. Epidemiology of synchronous brain metastases. Neurooncol. Adv. 2020;2:vdaa041. doi: 10.1093/noajnl/vdaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Patchell R.A., Tibbs P.A., Regine W.F., Dempsey R.J., Mohiuddin M., Kryscio R.J., Markesbery W.R., Foon K.A., Young B. Postoperative radiotherapy in the treatment of single metastases to the brain: A randomized trial. JAMA. 1998;280:1485–1489. doi: 10.1001/jama.280.17.1485. [DOI] [PubMed] [Google Scholar]
- 95.Patchell R.A., Tibbs P.A., Walsh J.W., Dempsey R.J., Maruyama Y., Kryscio R.J., Markesbery W.R., Macdonald J.S., Young B. A randomized trial of surgery in the treatment of single metastases to the brain. N. Engl. J. Med. 1990;322:494–500. doi: 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]
- 96.Mulvenna P., Nankivell M., Barton R., Faivre-Finn C., Wilson P., McColl E., Moore B., Brisbane I., Ardron D., Holt T., et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): Results from a phase 3, non-inferiority, randomised trial. Lancet. 2016;388:2004–2014. doi: 10.1016/S0140-6736(16)30825-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Barker F.G., 2nd, Butler W.E., Lyons S., Cascio E., Ogilvy C.S., Loeffler J.S., Chapman P.H. Dose-volume prediction of radiation-related complications after proton beam radiosurgery for cerebral arteriovenous malformations. J. Neurosurg. 2003;99:254–263. doi: 10.3171/jns.2003.99.2.0254. [DOI] [PubMed] [Google Scholar]
- 98.Steinberg G.K., Levy R.P., Fabrikant J.I., Frankel K.A., Phillips M.H., Marks M.P. Stereotactic helium ion Bragg peak radiosurgery for angiographically occult intracranial vascular malformations. Stereotact. Funct. Neurosurg. 1991;57:64–71. doi: 10.1159/000099556. [DOI] [PubMed] [Google Scholar]
- 99.Ezzat S., Asa S.L., Couldwell W.T., Barr C.E., Dodge W.E., Vance M.L., McCutcheon I.E. The prevalence of pituitary adenomas: A systematic review. Cancer. 2004;101:613–619. doi: 10.1002/cncr.20412. [DOI] [PubMed] [Google Scholar]
- 100.Ostrom Q.T., Cioffi G., Gittleman H., Patil N., Waite K., Kruchko C., Barnholtz-Sloan J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. Neuro Oncol. 2019;21:v1–v100. doi: 10.1093/neuonc/noz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mehta G.U., Lonser R.R. Management of hormone-secreting pituitary adenomas. Neuro Oncol. 2017;19:762–773. doi: 10.1093/neuonc/now130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hoybye C., Rahn T. Adjuvant Gamma Knife radiosurgery in non-functioning pituitary adenomas; low risk of long-term complications in selected patients. Pituitary. 2009;12:211–216. doi: 10.1007/s11102-008-0163-x. [DOI] [PubMed] [Google Scholar]
- 103.Pomeraniec I.J., Dallapiazza R.F., Xu Z., Jane J.A., Jr., Sheehan J.P. Early versus late Gamma Knife radiosurgery following transsphenoidal resection for nonfunctioning pituitary macroadenomas: A matched cohort study. J. Neurosurg. 2016;125:202–212. doi: 10.3171/2015.5.JNS15581. [DOI] [PubMed] [Google Scholar]
- 104.Erturk E., Tuncel E., Kiyici S., Ersoy C., Duran C., Imamoglu S. Outcome of surgery for acromegaly performed by different surgeons: Importance of surgical experience. Pituitary. 2005;8:93–97. doi: 10.1007/s11102-005-3280-9. [DOI] [PubMed] [Google Scholar]
- 105.Yamada S., Fukuhara N., Horiguchi K., Yamaguchi-Okada M., Nishioka H., Takeshita A., Takeuchi Y., Ito J., Inoshita N. Clinicopathological characteristics and therapeutic outcomes in thyrotropin-secreting pituitary adenomas: A single-center study of 90 cases. J. Neurosurg. 2014;121:1462–1473. doi: 10.3171/2014.7.JNS1471. [DOI] [PubMed] [Google Scholar]
- 106.Lin D., Hegarty J.L., Fischbein N.J., Jackler R.K. The prevalence of “incidental” acoustic neuroma. Arch. Otolaryngol. Head Neck Surg. 2005;131:241–244. doi: 10.1001/archotol.131.3.241. [DOI] [PubMed] [Google Scholar]
- 107.Propp J.M., McCarthy B.J., Davis F.G., Preston-Martin S. Descriptive epidemiology of vestibular schwannomas. Neuro Oncol. 2006;8:1–11. doi: 10.1215/S1522851704001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Roche P.H., Bouvier C., Chinot O., Figarella-Branger D. Genesis and biology of vestibular schwannomas. Prog. Neurol. Surg. 2008;21:24–31. doi: 10.1159/000156556. [DOI] [PubMed] [Google Scholar]
- 109.Wiemels J., Wrensch M., Claus E.B. Epidemiology and etiology of meningioma. J. Neurooncol. 2010;99:307–314. doi: 10.1007/s11060-010-0386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Marosi C., Hassler M., Roessler K., Reni M., Sant M., Mazza E., Vecht C. Meningioma. Crit. Rev. Oncol. Hematol. 2008;67:153–171. doi: 10.1016/j.critrevonc.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 111.Al-Shahi R., Bhattacharya J.J., Currie D.G., Papanastassiou V., Ritchie V., Roberts R.C., Sellar R.J., Warlow C.P., Scottish Intracranial Vascular Malformation Study Collaborators Prospective, population-based detection of intracranial vascular malformations in adults: The Scottish Intracranial Vascular Malformation Study (SIVMS) Stroke. 2003;34:1163–1169. doi: 10.1161/01.STR.0000069018.90456.C9. [DOI] [PubMed] [Google Scholar]
- 112.Spetzler R.F., Martin N.A. A proposed grading system for arteriovenous malformations. J. Neurosurg. 1986;65:476–483. doi: 10.3171/jns.1986.65.4.0476. [DOI] [PubMed] [Google Scholar]
- 113.Solomon R.A., Connolly E.S., Jr. Arteriovenous Malformations of the Brain. N. Engl. J. Med. 2017;376:1859–1866. doi: 10.1056/NEJMra1607407. [DOI] [PubMed] [Google Scholar]
- 114.Kano H., Flickinger J.C., Yang H.C., Flannery T.J., Tonetti D., Niranjan A., Lunsford L.D. Stereotactic radiosurgery for Spetzler-Martin Grade III arteriovenous malformations. J. Neurosurg. 2014;120:973–981. doi: 10.3171/2013.12.JNS131600. [DOI] [PubMed] [Google Scholar]
- 115.Maruyama K., Kawahara N., Shin M., Tago M., Kishimoto J., Kurita H., Kawamoto S., Morita A., Kirino T. The risk of hemorrhage after radiosurgery for cerebral arteriovenous malformations. N. Engl. J. Med. 2005;352:146–153. doi: 10.1056/NEJMoa040907. [DOI] [PubMed] [Google Scholar]