Abstract
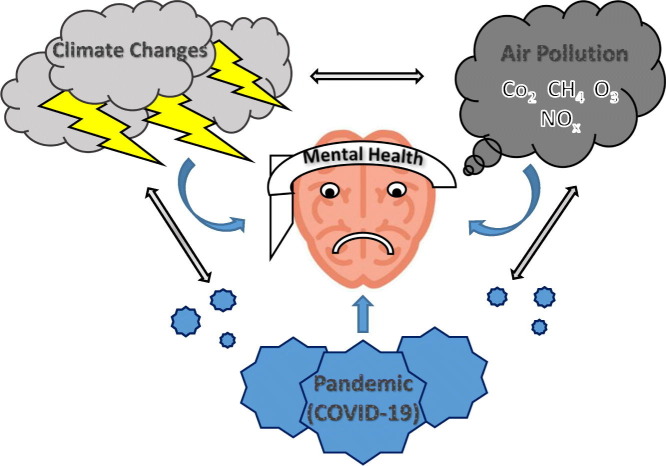
Converging data would indicate the existence of possible relationships between climate change, environmental pollution and epidemics/pandemics, such as the current one due to SARS-CoV-2 virus. Each of these phenomena has been supposed to provoke detrimental effects on mental health. Therefore, the purpose of this paper was to review the available scientific literature on these variables in order to suggest and comment on their eventual synergistic effects on mental health.
The available literature report that climate change, air pollution and COVID-19 pandemic might influence mental health, with disturbances ranging from mild negative emotional responses to full-blown psychiatric conditions, specifically, anxiety and depression, stress/trauma-related disorders, and substance abuse. The most vulnerable groups include elderly, children, women, people with pre-existing health problems especially mental illnesses, subjects taking some types of medication including psychotropic drugs, individuals with low socio-economic status, and immigrants.
It is evident that COVID-19 pandemic uncovers all the fragility and weakness of our ecosystem, and inability to protect ourselves from pollutants. Again, it underlines our faults and neglect towards disasters deriving from climate change or pollution, or the consequences of human activities irrespective of natural habitats and constantly increasing the probability of spillover of viruses from animals to humans.
In conclusion, the psychological/psychiatric consequences of COVID-19 pandemic, that currently seem unavoidable, represent a sharp cue of our misconception and indifference towards the links between our behaviour and their influence on the “health” of our planet and of ourselves. It is time to move towards a deeper understanding of these relationships, not only for our survival, but for the maintenance of that balance among man, animals and environment at the basis of life in earth, otherwise there will be no future.
Keywords: Climate Change, Environment Pollution, Epidemics, Pandemics, COVID-19 Pandemic, Mental Health
Graphical abstract
1. Introduction
According to the United Nations Framework Convention on Climate Change (UNFCCC), climate change is defined as “a change in the climate that is directly or indirectly attributable to human activities which alter the composition of the planetary atmosphere and add to the natural climatic variability observed on similar time intervals”. It is evaluated by measuring systematic variations in the statistical quantities of meteorological variables calculated over a period of time of several decades, and usually at least thirty years (Sands, 1992). Therefore, in assessing climate change, natural climatic variability should be considered in relation to complex natural processes of the planet. Several objective evidences recorded in the last centuries revealed dramatic climate changes: increase in air and ocean temperatures, rise in sea level, widespread melting of glaciers, increase in frequency and intensity of extreme weather phenomena, variation in ocean salinity, wind patterns and annual distribution of rainfall, increase of hydrogeological, flood, drought and fire risks (Hughes, 2000). Such phenomena provoke detrimental effects on natural, biological and anthropogenic systems (Steffen et al., 2015; Nogués-Bravo et al., 2018): changes in physiological responses and in phenology, modifications in individual species distribution and composition (i.e., migration, turnover of the ecological community, geographical reorganization, changes in population size, extinctions) (Müller et al., 2003; Tinner and Kaltenrieder, 2005; Yasuhara et al., 2008; Peros et al., 2008; Ampel et al., 2010; Anderson et al., 2011; Lothrop et al., 2011; Jackson et al., 2014), destruction of natural habitats, as well as variations in agricultural productivity and nutritional quality/capacity, and derangement of geopolitical, economical and social organizations (Botta et al., 2019).
Environmental pollution is defined as the unfavorable alteration of the environment through the direct or indirect action of man (Rai, 2016). It is considered the result of the urban-industrial and technologic revolution, with the rapid and ferocious exploitation of natural resources, and the huge increase in waste products (Hughes et al., 1980; Brunekreef and Holgate, 2002; Kampa and Castanas, 2008). Singh et al. (1991) defined it as “an unbalance condition from an equilibrium condition in any system”. With no doubt, environment pollution is a global problem, common to both developed and developing countries attracting increasing attention for its severe long-term consequences (Hughes et al., 1980; Brunekreef and Holgate, 2002; Kampa and Castanas, 2008). Air pollutants are gas or particles dispersed in the air, with different chemical and physical structures, and heterogeneous effects on air quality, climate and eventually human health (Hughes et al., 1980; Brunekreef and Holgate, 2002; Kampa and Castanas, 2008). Some of these substances do not directly damage the air quality, but through the reactions with other substances present in the atmosphere. Carbon dioxide (CO2), methane (CH4), ozone (O3), nitrogen oxides (NOx), and fluorinated gases 3 are the main sources of gaseous pollutants deriving from industrial, agricultural, traffic and energy-producing sources, including buildings' heating (Hughes et al., 1980; Brunekreef and Holgate, 2002; Kampa and Castanas, 2008). They are also called greenhouse gases, substances strengthening the earth's atmosphere's ability to capture long-wave radiation from the ground, and determining the phenomenon of global warming, the main cause of climate change (Botta et al., 2019). The terms particulate matters (PMs) or aerosol particles describe condensed (solid or liquid) materials suspended in the atmosphere (Mukherjee and Agrawal, 2018). They include crustal material, soot, combustion particles, nucleating clusters and biological material such as spores, but not by convention raindrops, hail or other hydrometeors (Mukherjee and Agrawal, 2018; Mukherjee and Agrawal, 2017). Primary PM is released into the atmosphere from sources such as incomplete combustion, dust and sea salts. Secondary PM is formed in the atmosphere from the condensation of low volatility gases, such as sulfuric acid, ammonia and organic compounds. Several airborne particles include both anthropogenic and natural components. Based on their aerodynamic equivalent diameter (AED), PMs of possible impact on human health are classified into: fine particles, with a diameter < 2.5 μm (PM2.5), coarse particles, with a diameter between 2.5 and 10 μm (PM10-2.5), and ultra-fine particles, with diameters <0.1 μm. These particles have a potentially harmful effect on different parts of the respiratory tract: the upper respiratory tract is affected by PM10, while the pulmonary alveoli are affected by ultra-fine particles aerodynamic equivalent diameter (AED) (Mukherjee and Agrawal, 2018; Mukherjee and Agrawal, 2017; Stanek et al., 2011; El Morabet, 2018).
It is now well known that environmental pollution and climate change might negatively impair several physiological systems and organs of individuals of all ages, possibly being involved in perinatal disorders, respiratory and cardiovascular disorders, allergies, cancer, and neurological and mental disorders (Kelishadi et al., 2009; Miller, 2020; Kelishadi and Poursafa, 2010; Eze et al., 2014).
In addition, the distribution, diffusion and transmission of diseases by water or vectors represent one of the most significant consequences of environment pollution and climate change (Lindahl and Grace, 2015). Indeed, infectious diseases, pollution and climate change seem to be connected in different ways, affecting each other, as there exist indications that variations of some meteorological parameters associated with climate change might favor the epidemics (Sajadi et al., 2020; Xie and Zhu, 2020; Shi et al., 2020a; Wang et al., 2010; Ruiz et al., 2010). Moreover, even the destruction of wild animal habitats over time may thins the natural barrier between humans and wild animals containing pathogenic microorganisms, creating new contact areas (bits of forest near areas inhabited by humans) and the possibility of triggering spill over (Ostfeld, 2009; Gibb et al., 2020). This is particularly relevant in this historical period with humanity facing the severe pandemic of a coronavirus called severe acute respiratory syndrome coronavirus (SARS-CoV-2) that originated in the Chinese region of Hubei and soon spread all over the world (Gorbalenya et al., 2020). Again, a growing bulk of studies revealed an association between diffusion, incidence, morbidity and mortality of the current COVID-19 pandemic, caused by this virus, and air pollutants, especially air PM levels (Petrosillo et al., 2020; Tavella and Da Silva Júnior, 2020; Conticini et al., 2020; Wu et al., 2020a).
Moreover, increasing evidence suggests that climate change (Berry et al., 2010; Bourque and Willox, 2014), environmental pollution (Buoli et al., 2018; Attademo and Bernardini, 2020), and pandemics (Buoli et al., 2018), including the ongoing COVID-19 one (Wang et al., n.d.; Liu et al., 2020a), might produce negative effects on mental health. It has long been known that air pollution and meteorological changes might induce psychopathological phenomena, such as meteoropathy (Cianconi et al., 2020), a term currently used to label any pathological dimension related to weather conditions (Balsamo et al., 1992; Zikic and Žikić, 2018). Furthermore, environmental pollutants, climate changes and SARS-CoV-2 infection have been associated with changes in the central nervous system (CNS) that could lead to mental and/or behavioral alterations through different physiopathological mechanisms: inflammatory processes, activation of the immune system, oxidative stress, damage to blood vessels, dysfunctions of neurotransmitter systems (Costa et al., 2020a; Chan et al., 2020; Paniz-Mondolfi et al., 2020; Steardo et al., 2020a; Calderón-Garcidueñas et al., 2008a; Calderón-Garcidueñas et al., 2011; Calderón-Garcidueñas et al., 2012; Guxens and Sunyer, 2012; Brockmeyer and D'Angiulli, 2016). However, it is difficult to establish the specific cause-effect relationships of these phenomena on mental health, as they result from the interactions of two complex systems: the environment, with everything (biotic and abiotic elements) populating it, and human beings (Torres and Casey, 2017; Gaddi et al., 2018).
Therefore, the purpose of this paper was to review and comment on the scientific literature on the possible interactions between climate change, environmental pollution and COVID-19 pandemic, as well as their eventual synergistic effects on mental health.
2. Materials and methods
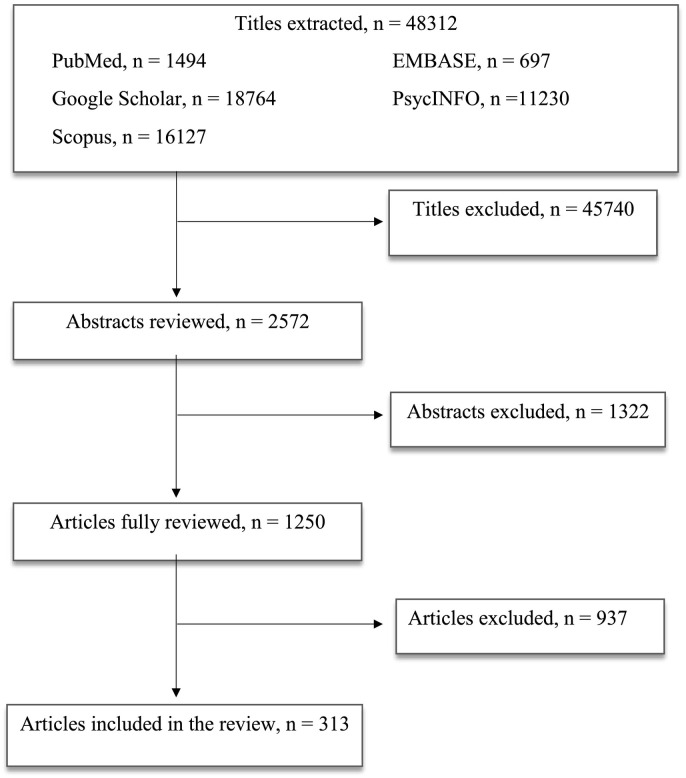
According to the PRISMA guidelines (Moher et al., 2009), the databases of PubMed, Scopus, Embase, PsycINFO and Google Scholar were accessed in order to research and collect articles that were published in English language only. Free text terms and MeSH headings were combined as it follows: “climate change OR environment pollution” AND “COVID-19 OR pandemics” OR “mental health”. In the paper, human and animal studies were considered. Moreover, studies of all design types were included, from the cross-sectional to longitudinal studies, as well as brief reviews and communications. All the authors agreed to include in the review conference abstracts, posters and case reports if published in indexed journals.
All the authors equally contributed in identifying potential information specific to this topic among the titles and abstracts of the publications. The first selection excluded 45,740 titles because: a) duplicates; b) not concerning the scope of the paper; c) not informative enough. The second selection excluded 1322 abstracts after being read and reviewed, as the information reported did not fulfill the scope of our paper and/or the presented information did not seem relevant to the discussed topic. Subsequently, 937 more publications were excluded after being completely read and evaluated, as they did not provide enough information and/or resulted sufficiently in line with our review. Finally, 313 papers were included in the present review (Table 1 ).
Table 1.
Article selection flow chart.
2.1. Effect of climate change and environment pollution on COVID-19
The analysis of the global distribution of COVID-19 pandemic underlined that, at least in the first phase of the pandemic the proportion of cases to population per 105 (PCP) and proportion of death to population per 105 (PDP) were higher in northern areas of the world, including some parts of North America, Asia and Europe, all located in higher latitudes and with a colder climate and better socio-economic condition (Sarmadi et al., 2020). Several environmental and demographic factors have been associated with this distribution pattern (Sarmadi et al., 2020). Certainly, a possible explanation might be in the different availability of diagnostic kits and health facilities between the north and south of the world (Bi et al., 2020). Furthermore, as for climate change, even for COVID19 urban slums with restricted living areas are at risk. Again, colder climates and higher population densities could also contribute to the greater spread of the disease (Sajadi et al., 2020; Xie and Zhu, 2020).
Despite still inconclusive, several data highlighted an association between COVID-19 outbreak transmission and spread and different environmental factors, such as temperature, humidity and climate latitude (Shi et al., 2020a; Poole, 2020; Guo et al., 2020; Chen et al., 2020a). Indeed, it has long been known that weather significantly influence respiratory infections (Sajadi et al., 2020; Wang et al., 2010; Ruiz et al., 2010; Vandini et al., 2013). Temperature, humidity, visibility, and wind speed can affect droplet stability in the environment, or affect survival of viruses, or impact epidemic transmission (Chen et al., 2020a). In China, temperature was proven to be an environmental driver of the COVID-19 outbreak. In particular, high temperature was observed to decrease the transmission rate of the infection and the incidence of new cases (Shi et al., 2020a). The authors also suggested that both lower and higher temperatures could be beneficial for decreasing the incidence of COVID-19 (Shi et al., 2020b). By contrast, no significant association between the incidence of COVID-19 and absolute humidity was reported (Shi et al., 2020a). In Indonesia, a study on Jakarta population led to similar results, showing that only temperature average was significantly correlated with COVID-19 spread (Tosepu et al., 2020). Another study based on data from Wuhan showed that COVID-19 basic reproduction number (R0), also called the basic reproduction ratio, an epidemiologic metric used to describe the contagiousness or transmissibility of infectious agents (Delamater et al., 2019), was negatively related to both temperature and humidity (Guo et al., 2020). Wang et al. (2020) confirmed that these two factors might reduce COVID-19 transmission (Wang et al., 2020a). A study carried out in seven metropolitan cities and nine provinces from South Korea also supported the link of COVID-19 incidence with temperature (Hoang and Anh, 2020). In particular, a significantly non-linear association between daily temperature and COVID-19 confirmed cases was recorded, whereby each 1 °C increase in temperature was related with a 9% increase in COVID-19 confirmed cases, when the temperature was below 8 °C. In addition, even increases in NO2, CO and SO2 concentrations were associated with an increase in COVID-19 confirmed cases (Hoang and Anh, 2020). In Norway, normal and maximum temperature recorded during study period and low precipitation (rainfall) levels were positively associated with the incidence of COVID-19 pandemic (Menebo, 2020). On the contrary, a Canadian study found no association of spread of COVID-19 and temperature and latitude (Jüni et al., 2020).
As far as mortality rate is concerned, collecting data on daily deaths from COVID-19 and weather conditions in Wuhan, a study showed a positive association between COVID-19 mortality and daytime temperature, and a negative association between COVID mortality-19 and relative humidity (Ma et al., 2020). A large study analyzed the associations between transmission and deaths caused by SARS-CoV-2 and meteorological variables worldwide. The results showed that an increase of one degree Fahrenheit in the mean daily temperature was related to a reduction in the number of COVID-19 cases. Moreover, a negative correlation between the mean temperature and number of COVID-19 cases, and a positive correlation between precipitation and SARS-CoV-2 transmission were reported. In addition, countries with higher rainfall showed an increased disease transmission, as compared with those with lower rainfall (Sobral et al., 2020).
As already mentioned, besides all these factors, the spread, the incidence and the mortality rates of COVID-19 seem have been associated with air pollution, especially PMs for their negative effects on health. Inhalable coarse particles with a diameter of between 2.5 and 10 μm, and inhalable fine particles, with a diameter of less than 2.5 μm seem to be the most dangerous PMs (Kim et al., 2015). Indeed, increased concentrations of PM2.5 and of pollutants, such as nitrogen dioxide and PM, were positively related to the number of infected individuals (Coccia, 2020), as well as to the hospital admissions due to respiratory viruses (Carugno et al., 2018; Glencross et al., 2020; Nenna et al., 2017; Andree, 2020). It was also suggested that this association could affect the progression and prognosis of the disease (Yao et al., 2020a). Wu et al. (Wu et al., 2020a) concluded that even small increases in PM2.5 levels could worsen the progression and prognosis of the disease, and was linked to a significant increase (approximately 15%) of COVID-19 deaths. In fact, immune dysregulation is considered the major cause of a worse outcome in respiratory infections, including those provoked by SARS and COVID-19. Again, air pollution is one of the best-known factors of prolonged inflammation, ultimately leading to innate over-activation of the immune system (Conticini et al., 2020; Wang et al., 2020b). Some evidences showed that exposure to environmental pollution may be associated with high COVID-19 lethality rates in individuals living in polluted areas around the world (Cui et al., 2003). A systematic review on the relationship between air pollution and increased risk of morbidity for COVID-19, including 15 papers among 450, and carried out using an adaptation of the Cochrane rapid review methodology, concluded that the risk of morbidity and mortality for COVID-19 increases with chronic and acute exposure to air pollution, especially particulate matter PM2.5 and PM10, and nitrogen dioxide (Félix-Arellano et al., 2020).
A recent report in China reported a substantial relationship between PM 2.5 and COVID-19 infection, which was revealed across 120 cities (Xie and Zhu, 2020). A study on the spatio-temporal spread of the COVID-19 epidemic in this country showed that the spread rate of the epidemic in Hubei province, and in general in economically more developed and more populated cities, was higher than in the rest of the China, and that the distribution of the epidemic areas tended to be stable over time. In addition, several factors, including the strength of economic connections, the population distribution, the accessibility to transport and medical facilities, as well as the average temperature (Xie et al., 2020), have been shown to exert a certain influence on the epidemic. Subsequently, while exploring the temporal correlation between the case mortality rate (CFR) of COVID-19 and particulate matter (PM) in Wuhan, the most hit city in the Hubei province, higher CFR of COVID-19 was observed with increasing concentrations of inhalable PM10 and PM2.5 (Xie et al., 2020).
In Italy, several researchers analyzed the relationship between COVID-19 pandemic and particulate pollution, starting from the observation that the course of the infection was very different throughout the country regions (Setti et al., 2020a; Setti et al., 2020b). Several data highlighted the possible association between elevated concentration of air pollutants and the high spread of COVID-19 in northern Italian regions (Coccia, 2020; Martelletti and Martelletti, 2020). A first observational study based on initial epidemic diffusion reported a relationship between exceeding the legal limits of PM10 concentrations and the number COVID-19 cases (Setti et al., 2020a). The analysis showed a direct relation between COVID-19 cases and PM10 pollution concentrations, in agreement with the previous literature on other viral infections (Setti et al., 2020a). An analysis conducted by the University of Bergamo concluded that SARS-CoV-2 RNA might be present in PM, suggesting it as a possible indicator of epidemic recurrence (Setti et al., 2020b). Another study investigated the correlation between the degree of accelerated diffusion and lethality of COVID-19 and surface air pollution in the metropolitan area of Milan, the greatest city of northern Italy (Zoran et al., 2020). The results showed that high levels of urban air pollution had a significant impact on increasing the rates of total cases of COVID-19, new daily cases and total deaths (Zoran et al., 2020). In particular, daily PM mean levels were reported to influence the number of COVID-19 cases. Furthermore, still in Milan the average temperature correlated positively, while the relative humidity negatively with cases of COVID-19 (Zoran et al., 2020).
The situations seem to be similar throughout the world. In USA an increase in PM2.5 concentrations was linked to a statistically significant increase in daily SARS-CoV-2 death rate (an increase of 1 μg/m3 of PM2.5 levels was associated with an 8% increase in the COVID-19 death rate) (Wu et al., 2020a). Overlapping results were obtained in an analysis conducted on 355 municipalities in the Netherlands, where PM2.5 resulted to be a significant predictor of both the number of confirmed COVID-19 cases and related hospital admissions per 100,000 inhabitants (Andree, 2020). There is also growing evidence of a positive correlation between PM2.5 levels and COVID-19 infection in India and Pakistan (Mehmood et al., 2020), two countries with the worst air pollution in the world (Lelieveld et al., 2015; Junaid et al., 2018), as recently, PM2.5 levels in these regions reached exceptionally high levels (Junaid et al., 2018; Li et al., 2018).
To summarize, although there are no conclusive results, some evidence would indicate that SARS-CoV-2 might use PM as a possible vector, while suggesting that countering air pollution might lead to a reduction in transmission and, therefore, in the spread of the disease (Wu et al., 2020a; Setti et al., 2020a). Additionally, since particulate pollution has also been associated with increased COVID-19 morbidity and mortality, the reduction of environmental pollutants could theoretically produce a decline in consequent severe cases and deaths.
2.2. Effects of climate change and air pollution on mental health
Climate change encompasses several environmental and weather modifications, including extreme natural events and gradual climate variations. Recently, there is a growing interest on the direct or indirect, short-term or long-term psychological/psychiatric consequences of climate change (Reifels et al., 2015).
The available data would suggest that the impact of climate change on mental health might range from mild stress and distress symptoms to clinical disorders, mainly including anxiety, sleep disturbances, depression, and stress/trauma-related disorders (Blanc et al., 2019; Hayes et al., 2018; Ursano et al., 2017). Further, it is well known that extreme natural events (including any situation out of the ordinary and unpredictable, such as hurricanes, fires due to high temperatures, floods, tsunamis, tornadoes, and even the total confinement of a city, country or the whole world due to the spread of an infection) are more frequently associated with psychiatric disorders with acute onset than gradual environmental changes, as they have an immediate and direct impact on mental health (Cianconi et al., 2020). The loss of the normal routine generates psychological fragility, with the prevalence of negative thoughts and emotions, such as fear, anxiety, lack of hope and uncertainty about the future (Cianconi et al., 2020; U.S Global Change, R.P., 2016). In a percentage ranging between 7 and 40% of predisposed and poorly resilient subjects, the psychological distress can easily become full-blown psychiatric disorders, specifically those related to stress and trauma (adaptation stress disorders, ASD, and post-traumatic stress disorder, PTSD) (Salcioglu et al., 2007), but also anxiety, depression, substance abuse, and suicidal thoughts, transient psychosis, and even relapse of Bipolar Disorder (BD) (U.S Global Change, R.P., 2016). Different types of extreme weather events might be related to acute, sub-acute, and long-term effects on mental health (Cianconi et al., 2020). In particular, long-term anxiety and depression, PTSD, aggression and suicide seem to be associated with floods (the most common disasters at global level) (Ahern et al., 2005). Again extreme heat events were associated with increased aggression (Anderson et al., 2000), suicide and psychiatric admissions (Nitschke et al., 2007). Long periods of heat were linked to higher rates of criminal and aggressive behaviors (Cheatwood, 1995; Cohn et al., 2004), mood disorders, anxiety, somatoforms disorders, psychophysical exhaustion, and suicide (Hansen et al., 2008; Parsons, 2002; Maes et al., 1994). Even the decrease in temperatures is associated with increased aggression (Howarth and Hoffman, 1984). High humidity rates have been associated with poor concentration and high fatigue (Howarth and Hoffman, 1984).
Unlike extreme weather events, the impact of gradual climate change on mental health, like the increase of temperatures and sea levels or precipitation pattern variations, is still unclear and more difficult to study, as it is less evident and essentially indirect (Berry et al., 2008). In these situations, affection and possessions loss, community removal, and social connections reduction may cause or amplify the development of mental health problems (Coêlho et al., 2004). The most frequent gradual climate changes are represented by long periods of extreme heat and/or drought, as several people are forced to migrate from their homeland (Berry et al., 2010). Involuntary migration is known to be a relevant stressor with the potential to impair both physical and mental health (Campbell and Campbell, 2007; Huq et al., 2007; Schwerdtle et al., 2017). In areas at risk of drought, enhanced rates of anguish and depression were reported (Campbell and Campbell, 2007; Huq et al., 2007), as well as high suicide rate among farmers living in these areas (Kjellstrom, 2009). Additionally, the extinction of animal and plant species, as well as the destruction of the native environment and landscape, in the long term could cause more complex psychopathological disorders, such as dissociative symptoms, identity disorders, and personality changes (Marshall et al., 2012; Woodbury, 2019; Wei et al., 2017).
Albeit to a lesser extent, global climate change can also indirectly affect mental health. Even just the awareness of the ongoing climate change can induce negative emotional responses, including guilt, pain, anxiety and demoralization. In this case, the most affected subjects are those who already experienced high levels of stress due to other factors, so that, the additional stressful load could overwhelm their ability to recover (Brugha and Cragg, 1990). Currently, there are no consistent and reliable objective tools for studying these responses, but several data showed a significant number of people reporting anxiety and stress associated with climate change (Clayton, 2020).
Since mental disorders associated with climate change are novel and still poorly understood entities, new terms were coined to define some of them, which represent a latest challenge for clinicians. The term “solastalgia” labels a psychic state in which people do not recognize as familiar the environment where they live and are unable to adapt to it (Albrecht et al., 2007). The term “eco-anxiety”, on the other hand, firstly denotes the stress that a subject experiences in perceiving nature as fragile and vulnerable, and secondly the frustration of not being able to face such a dramatic change (Gifford and Gifford, 2016; Arcanjo, 2019; Lee et al., 2019).
Besides the effects caused by climate change, air pollution by itself might also influence mental health, although this is topic just at its dawn, given the difficulties in establishing a causal relationship (Buoli et al., 2018). In any case, in the last few years, growing evidence suggested a link between environmental pollution and mental disorders (Buoli et al., 2018; Khan et al., 2019). Some studies on healthy people highlighted an association between high concentrations of PM2.5 and greater psychological distress (Sass et al., 2017) or impaired cognitive performance (Shehab and Pope, 2019). Long-term exposure to high concentrations of PM10, NO2, CO, and sulfur dioxide was positively associated with the prevalence of stress, poor quality of life, diagnosis of depression and suicidal ideation (Shin et al., 2018; Bernardini et al., 2020). Exacerbation of psychiatric disorders, increased number of emergency access for the onset of psychiatric symptoms, and suicidal ideation and behaviors were also reported in periods of the year and in geographic areas with higher levels of atmospheric pollutants (Lee et al., 2019; Szyszkowicz, 2007; Yackerson et al., 2014; Szyszkowicz et al., 2010; Kim et al., 2010; Lin et al., 2016; Oudin et al., 2018; Zhang and Zhou, 2020; Bernardini et al., 2019; Duan et al., 2018; Szyszkowicz et al., 2018; Wang et al., 2018; Gao et al., 2017; Strahilevitz et al., 1979; Kim et al., 2019; Bai et al., 2019; Song et al., 2018; Chen et al., 2018; Szyszkowicz et al., 2016; Szyszkowicz, 2010; Szyszkowicz et al., 2009; Qiu et al., 2019; Cho et al., 2015). Interestingly, recent data showed an association between air pollutants levels and emergency access for psychiatric symptoms even in relatively low-polluted geographic areas such as Umbria (Italy) and Göteborg (Sweden) (Bernardini et al., 2019).
Again, an association was noted between pollutants and psychotic disorders, in particular schizophrenia (Attademo and Bernardini, 2017; Attademo et al., 2017). Interestingly, extreme hot environment temperature, birth in winter or early spring, air pollution especially with PM10, PM2.5, SO2, NO2, lead, and tetrachlorethylene exposure have been related to the onset of schizophrenia (Agustina and Wulandari, 2019). Moreover, urbanicity (urban birth and current city living) has been described as one of the risk factors for the onset of psychosis (Heinz et al., 2013; Fett et al., 2019; Krabbendam and van Os, 2005; Radua et al., 2018). Social stress, exposure to environmental pollutants, and disease agents were proposed as potential mechanism that might underlie this association (Attademo and Bernardini, 2017; Heinz et al., 2013; Radua et al., 2018; Kirkbride et al., 2007). It is interesting to note that air pollution could be a potential mediator of the association between urbanicity and the risk of both schizophrenia and viral epidemics or pandemics (Attademo and Bernardini, 2017; Neiderud, 2015).
Several evidence revealed higher depression and anxiety rate among subjects exposed to air pollutants; in particular, increased risk of depressive symptoms were associated with high levels of NO2, O3, PM10, and PM2.5 (Vert et al., 2017; Lim et al., 2012; Kioumourtzoglou et al., 2017). Subjects exposed to high concentrations of PM10 and PM2.5 were more likely to suffer from significant anxiety symptoms (Power et al., 2015; Pun et al., 2017).
Different studies suggest that air pollution may contribute to the pathophysiology of neurodevelopmental disorders, while highlighting the association between air pollution and attention/deficit hyperactivity disorder (ADHD) (Saez et al., 2018), although a recent systematic review concluded that this association is weak (Donzelli et al., 2019). Again, autism spectrum disorders (ASD) were associated with traffic-related air pollution (Volk et al., 2011; Volk et al., 2013), diesel exhaust (DE) (Roberts et al., 2013), PM (Jung et al., 2013; Talbott et al., 2015; Jo et al., 2019; Kaufman et al., 2019), O3 (Kaufman et al., 2019; McGuinn et al., 2020). However, negative findings are also available (Yousefian et al., 2018).
In addition, pollutants were associated with increased expression of markers of neurodegenerative diseases, such as alpha-synuclein or beta-amyloid, and suggested to contribute to the pathophysiology of Alzheimer's (AD), Parkinson's diseases and multiple sclerosis (Costa et al., 2020a; Chen et al., 2017). Epidemiological studies reported that exposure to air pollution was associated with cognitive decline and pathological changes in the brain (Calderón-Garcidueñas et al., 2008a; Chen et al., 2017; Wilker et al., 2015; Chen et al., 2015; Clifford et al., 2016). In the Framingham Offspring study the brain volume of elderly subjects without dementia and stroke decreased with increasing PM2.5 concentration (Wilker et al., 2015). In the Women's Health Initiative Memory Study (WHIMS), not only the total brain volume, but also the white matter volume of subjects exposed to high concentration of PM2.5 was found reduced (Chen et al., 2015). In fact, the Lancet Commission for the prevention and treatment of dementia included air pollution in the list of potential risk factors for cognitive decline (Landrigan et al., 2018; Livingston et al., 2017). However, as highlighted by a recent systematic literature review, the evidence for this association is considered still inconclusive (Peters et al., 2019).
Further, animal and human studies suggest that air pollution may cause neurotoxicity (Calderón-Garcidueñas et al., 2008a; Calderón-Garcidueñas et al., 2011; Calderón-Garcidueñas et al., 2012; Guxens and Sunyer, 2012; Freire et al., 2010; Guxens et al., 2014). In animal studies, exposure to air pollutants produced neuro-inflammatory responses (Brockmeyer and D'Angiulli, 2016; Calderón-Garcidueñas et al., 2016; Block and Calderón-Garcidueñas, 2009). In particular, exposure to O3 and PM2.5 has been related to neurovascular to the damage and the production of autoantibodies against neural proteins (Brockmeyer and D'Angiulli, 2016; Calderón-Garcidueñas et al., 2016; Block and Calderón-Garcidueñas, 2009). Experimental and animal studies revealed that PM inhalation increased reactive oxygen species and activated inflammatory processes in the brain, as well as it was associated with amyloid beta protein (Aβ) and alpha-synuclein aggregates (Costa et al., 2020a), disruption of the blood-brain barrier, and microglial activation (Calderón-Garcidueñas et al., 2008b; Levesque et al., 2011; Block et al., 2004). Elevated levels of neuro-inflammatory markers were found in the brain of children exposed to high air pollution (Calderón-Garcidueñas et al., 2011; Calderón-Garcidueñas et al., 2008b; Calderón-Garcidueñas et al., 2013). Given the evidence indicating the presence of neuro-inflammation in some psychiatric disorders, it has been also speculated that pollutants might be involved in these processes. It is worth noting that neuro-inflammation processes seem particularly relevant in severe COVID-19 patients (Buemann et al., 2020).
However, to date results remain inconclusive, since other studies reported no consistent evidence for an association between air pollution and mental disorders (Buoli et al., 2018; Zijlema et al., 2016; Wang et al., 2014). Wang et al. found no association between depressive symptoms with both long-term exposure to traffic pollution and short-term changes in pollutant concentrations (Wang et al., 2014). Similar results were obtained in an analysis of four cohorts of the European general population (Zijlema et al., 2016).
To summarize, although different findings would suggest that climate change and environmental pollutions might provoke detrimental effects on mental health, reliable data are a few. However, with no doubt, this is an intriguing and emerging field requiring to be deepened in the future by controlled studies in larger and heterogeneous populations that might better reflect the clinical reality.
2.3. Effects of SARS-CoV-2 on mental health
Growing evidence showed the negative influence of SARS-CoV-2 pandemic on the worldwide population's psychological wellbeing, due to both biological and psychosocial factors (Xiang et al., 2020; Galea et al., 2020; Pfefferbaum and North, 2020; Reger et al., n.d.; Brooks et al., 2020). The imprecision about how many people have caught the disease, the fear of becoming infected and/or infecting family members, the fatality rate, the uncertainty about the effectiveness of treatments, generated a sense of bewilderment and insecurity in the whole world population (Xiang et al., 2020; Galea et al., 2020; Pfefferbaum and North, 2020; Reger et al., n.d.; Brooks et al., 2020). On the other hand, even the countermeasures taken to contain the spread of the infection, and the resulting socio-economic collapse, had an important impact on the overall mental health (Xiang et al., 2020; Galea et al., 2020; Pfefferbaum and North, 2020; Reger et al., n.d.; Brooks et al., 2020). In addition, the impact of fake rumors or news should not be underestimated. Indeed, the absence of clear messages increases fear and prompts people to seek information from less reliable sources (Yao, 2020; Marazziti and Stahl, 2020). Intense media exposure to COVID-19 news was associated with an even higher prevalence of depressive symptoms, anxiety and sleep disturbances (Peretti-Watel et al., 2020). The World Health Organization (WHO) defines this flow of misinformation as “infodemic” (World Health, O, 2020), underling the negative effect that bad information can have on world population psychology (Zarocostas, 2020).
Since the outbreak of the pandemic, there was an increase of psychological distress, feelings of anguish and uncertainty, fear of death, demoralization, anxiety, insomnia, distorted perceptions, dangerous behaviors including increased use of alcohol and abuse substances, as well as internet addiction conducts, among a large part of adults, children and adolescents everywhere (Wang et al., n.d.; Liu et al., 2020a; Peretti-Watel et al., 2020; World Health, O, 2020; Tang et al., 2020; Tian et al., 2020; McGinty et al., 2020; Holmes et al., 2020; Finlay and Gilmore, 2020; Sun et al., 2020). It was also noted that people living in areas with a high risk of infection were at greater risk for high psychological distress than those living in non-infected areas (Taylor et al., 2008).
Several data have been accumulated on the effects of confinement on mental health. Mass quarantine, a countermeasure applied in several countries to reduce the spread of the pandemic, was likely to increase community anxiety, as it increased perception of danger, reduced the sense of security and certainty, caused feelings of loneliness, unpredictability, and lack of control over one's life (Peretti-Watel et al., 2020). Furthermore, forced isolation imposed a drastic change in lifestyle, with the loss of habits, leisure and pleasure activities, social bonds, and some individuals with the loss of employment became more prone to boredom, frustration and failure (Peretti-Watel et al., 2020). Some of the first studies on effect of confinement showed an increased prevalence of psychiatric symptoms and disorders, especially depressive symptoms, anxiety and insomnia, as well as increased need of psychological support (Peretti-Watel et al., 2020). Woman and young adults resulted the most affected people by psychological distress, in accordance with previous research that concluded that these population groups are the most vulnerable to stress and more prone to develop PTSD (Peretti-Watel et al., 2020; Marazziti et al., 2020). These findings on quarantine psychological distress were confirmed by many recent studies carried out worldwide, from China to USA (Qiu et al., 2020; Lee, 2020; Richardson et al., 2020). Furthermore, lockdown was associated with an increased risk of eating disorders, including overweight and obesity (Siddiqui and Jakaria, 2020), as a result of depression, anxiety, loneliness, but also of fewer economic resources, that lead people to less healthy nutrition (Hamer and Stamatakis, 2008). This outcome was associated with a higher risk for COVID-19 infection and mortality, but also with a higher probability of a second wave of the COVID-19 pandemic (Siddiqui and Jakaria, 2020). Indeed, several studies observed that obesity is the second highest comorbid condition among COVID-19 patients (Siddiqui and Jakaria, 2020), while increasing the risk COVID-19 infection and mortality, as it is associated with systemic inflammation and over-activation of the immune system, and, as such, it might contribute to the damage of the lungs and of other organs (Ryan and Caplice, 2020). In addition, fatty tissue can act as a virus reservoir, resulting in a greater spread of the virus (Wilker et al., 2015).
Rising data reports the highest incidence of anxiety and depression in quarantined individuals, COVID-19 patients and their affections, as well as frontline workers (Xiang et al., 2020; Peretti-Watel et al., 2020; Qiu et al., 2020; Kisely et al., 2020). Different cross-sectional studies using self-report instruments on China (Lai et al., 2020) and Italy (Rossi et al., 2020a) health care workers exposed to COVID-19, reported a variety of psychiatric symptoms, from moderate to severe, the most common of which were anxiety, depression, insomnia and traumatic distress. This result was not verified in another cross-sectional study assessing on healthcare professionals exposed to COVID-19 in Singapore (Tan et al., 2020), maybe due to their previous experience with the SARS epidemic. In line with the data gathered from other natural disasters (Torales et al., 2020), the prevalence of ASD/PTSD symptoms in the general population during the COVID-19 pandemic seems to range from 7% to 53.8% (Benfante et al., 2020; Fekih-Romdhane et al., 2020; Rossi et al., 2020b; Shevlin et al., 2020; Alshehri et al., 2020; Xiong et al., 2020), with the highest rates reported in subjects directly exposed to the trauma of acute illness and loss, including COVID-19 patients, their family members, and frontline and health care workers (Liu et al., 2020a; Tang et al., 2020; Lai et al., 2020; Torales et al., 2020). There are many factors that might increase the risk of developing such conditions: female sex, lower socioeconomic status, interpersonal conflicts, frequent social media use and lower resilience and social support. Furthermore, it is important to consider that such dramatic situations can trigger relapses of pre-existing mental disorders, such as chronic mood or anxiety disorders and suicidal tendencies (Ćosić et al., 2020; Shah et al., 2020; Thome et al., 2020).
Some studies, primarily in small series, investigated neuropsychiatric symptoms and/or disorders directly in COVID-19 patients. Data on SARS reported that during acute epidemics approximately 20–40% of patients suffered from neuropsychiatric symptoms, including delirium, insomnia, anxiety, and depression (Rogers et al., 2020). The first cross-sectional studies on COVID-19 confirmed similar symptoms in COVID-19 patients (Romero-Sánchez et al., 2020). Different reports highlighted that COVID-19 patients could suffer from different neuropsychiatric conditions including acute cerebrovascular events (especially ischaemic stroke, intracerebral haemorrhage, and CNS vasculitis) (Varatharaj et al., 2020; Avula et al., 2020; Mao et al., 2020; Liu et al., 2020b; Helms et al., 2020), neurological symptoms (i.e. dysgeusia, dizziness, headache, and corticospinal tract signs) (Rogers et al., 2020; Varatharaj et al., 2020; Mao et al., 2020; Helms et al., 2020), and acute changes in behavior, cognition, and consciousness (Varatharaj et al., 2020; Mao et al., 2020; Liu et al., 2020b; Helms et al., 2020). Many patients with altered mental status showed unspecified encephalopathy and encephalitis, while others fulfilled psychiatric diagnoses, including new-onset psychosis, affective disorders, and dementia-like syndromes (Rogers et al., 2020). A UK surveillance study concluded that altered mental status was the second most common presentation of COVID-19 infection, associated with encephalopathy, encephalitis or primary psychiatric diagnoses (Varatharaj et al., 2020). Mao et al. (2020) retrospectively analyzed 214 COVID-19 patients from three different hospitals in China, showing that 36.4% had neuropsychiatric symptoms. The most common neurological symptoms were dizziness and headache, dysgeusia, and anosmia. Anxiety, depression, and delirium were the most common psychiatric manifestations (Mao et al., 2020). A recent systematic review and meta-analysis of psychiatric and neuropsychiatric presentations of severe coronavirus infections revealed that many patients with COVID-19 exhibited delirium, with confusion, agitation and altered consciousness (Rogers et al., 2020). The neuropsychiatric manifestations of COVID-19 were directly related to the increase in peripheral immunological markers, the severity of the infection and the death rate (Banerjee and Viswanath, 2020; Chen et al., 2020b; Yang et al., 2020), and could be explained by a specific neurotrophism of the virus (Banerjee and Viswanath, 2020), or by a unspecific encephalopathy secondary to the massive systemic inflammatory response (Filatov et al., 2020; Robinson and Busl, 2020). The neurotrophism of SARS-CoV-2 is still under discussion. However, in animal studies, the virus nasal inoculation was followed by its spread to the brain and its proliferation in oligodendrocytes and endothelial cells. In post mortem sections, viral particles were present in the piriform cortex, basal ganglia and hypothalamus (Chan et al., 2020). Animal and human studies on SARS-CoV-2 suggested different pathways of virus spreading to the CNS: hematogenous diffusion, olfactory bulb crossing, infection of the endothelial cells lining the cerebral vascular system, by using the perivascular spaces of the glymphatic system, or through the nerves, as the trigeminus or the vagus, by a retrograde axonal transport, (Paniz-Mondolfi et al., 2020; Banerjee and Viswanath, 2020; Bostancıklıoğlu, 2020; Lochhead and Thorne, 2012; Driessen et al., 2016; Perlman et al., 1989; Wu et al., 2020b; Desforges et al., 2014; de Wit et al., 2016; Fodoulian et al., 2020). Probably, the main SNC targets of the SARS-CoV-2 are represented by regions rich in angiotensin-converting enzyme 2 (ACE2) receptor (Steardo et al., 2020a; Gowrisankar and Clark, 2016; Xia and Lazartigues, 2010), currently recognized as the principal cellular access site of the virus (Liu et al., 2020c; Lu et al., 2020), that include, in particular, the circumventricular organs (i.e. the subfornical organ, paraventricular nucleus, solitary and ventrolateral rostral medulla) (Xia and Lazartigues, 2010), areas with poor protection from the blood brain barrier (BBB) and involved in cardiovascular and respiratory system regulation (Kristensson et al., 2013; Sisó et al., 2010; Takagi et al., 2019). Systemic inflammation is accompanied by a massive release of circulating cytokines (Filatov et al., 2020; Robinson and Busl, 2020), that can reach the CNS, damage the microcirculation, inducing edema and thrombosis (Klok et al., 2020), and cause neuroglial reactivity, altered neurochemical pathways, neuro-inflammation and pathological remodelling of neuronal networks (Steardo et al., 2020b; Sankowski et al., 2015; Schwartz and Deczkowska, 2016; Klein et al., 2019; Daniels et al., 2017; Manglani and McGavern, 2018; Pedersen and Ho, 2020; Taylor et al., 2016; Verkhratsky et al., 2017). Furthermore, inflammatory cytokines can activate the hypothalamic-pituitary-adrenal axis that might contribute to alterations of cerebral hemodynamics (Lippi et al., 2020; Alenina and Bader, 2019; Diz et al., 2008). Emerging evidence demonstrated the pathophysiological role that neuro-inflammation might play in different neuropsychiatric and neuro-cognitive diseases (Bright et al., 2019; Heppner et al., 2015; Rocha et al., 2018), depression (Bakunina et al., 2015), psychosis (Marques et al., 2019), drug abuse (Kohno et al., 2019), and sleep disorders (Nadjar et al., 2017). In this context, COVID infection represents an important risk factor that, together with environmental stress related to the fear of getting sick, hospitalization and social restrictions, could contribute to the onset and exacerbation of even greater neuropsychiatric disorders, especially depressive disorder, BD, psychosis, obsessive-compulsive disorder (OCD), and PTSD (Steardo et al., 2020b). The increase in IL-6 levels could represent the main inflammatory factor that links COVID-19 infection to the onset of many psychiatric disorders. In fact, numerous data reported that severe cases of COVID-19 displayed invariably an excessive immune response characterized by a massive increase of plasma IL-6 levels (Aziz et al., 2020). Likewise, it is known that high concentrations of IL-6 were found in different psychiatric disorders. Depression was associated with elevated IL-6 concentrations in both plasma and brain (Lindqvist et al., 2009; Sasayama et al., 2013; Kern et al., 2014; Enache et al., 2019; Boufidou et al., 2009; Hodes et al., 2016). An imbalance between pro-inflammatory and anti-inflammatory cytokines was observed in DB (Pinto et al., 2018; Felger, 2018), but still with unclear results. Some studies reported an increase in pro-inflammatory molecules, including IL-6, in the acute phases of the disease with a parallel reduction in anti-inflammatory factors (Sayana et al., 2017; Munkholm et al., 2013). However, these results were not confirmed in a subsequent study (Wang and Miller, 2018). Increased IL-6 levels were also revealed in subjects with schizophrenia (Sasayama et al., 2013; Corsi-Zuelli et al., 2020), and in a study on a group of adolescents, high Il-6 concentrations were positively correlated with the onset of psychosis later in life (Metcalf et al., 2017). Positive correlation with pro-inflammatory factors was also demonstrated in OCD (Murphy et al., 2006; Gray and Bloch, 2012). Indeed, OCD patients showed higher levels of pro-inflammatory cytokines, including IL-6, when compared with controls (Gray and Bloch, 2012; Karagüzel et al., 2019). Several studies indicated an association between inflammation and PTSD (Furtado and Katzman, 2015; Schelling et al., 2004). PTSD was often accompanied by low-grade inflammation (Spitzer et al., 2010), and patients with this disorder showed increased plasma and brain concentrations of pro-inflammatory factors, especially of IL-6 (Lindqvist et al., 2017; Bersani et al., 2016; Tursich et al., 2014).
COVID-19 may adversely affect disabled or more vulnerable individuals, such as patients with preexisting psychiatric disorders. In these subjects, psychiatric disorders may worsen (Holmes et al., 2020; Costa et al., 2020b), also due to the difficulty of access to routine visits (Zhou et al., 2020), with an increased incidence of relapses especially for psychotic and mood disorders. New psychiatric symptoms may also appear, including anxiety, depression, and insomnia, attributed to fear of infection, restrictions and isolation (Holmes et al., 2020; Costa et al., 2020b; Zhou et al., 2020; Kozloff et al., 2020). Moreover, psychiatric patients are at increased risk of infection compared with the general population, due to the difficulties in adhering to public health measures, such as frequent hand-washing and physical distancing, as well as to poor understanding of the infection risk (Zhou et al., 2020; Benson et al., 2020; Yao et al., 2020b; Zhu et al., 2020).
Finally, based on evidence from previous pandemics, the COVID-19 pandemic may also increase the risk for suicidal ideation and behavior (Holmes et al., 2020; Gunnell et al., 2020; Barbisch et al., 2015), linked to social isolation (Yip et al., 2010), economic losses (Vandoros et al., 2018; Kim and von dem Knesebeck, 2016), and psychiatric symptoms, especially depression and trauma-related disorders (Pfefferbaum and North, 2020; Reger et al., n.d.; Zhou et al., 2020; Gunnell et al., 2020; Bo et al., 2020; Martín-Carrasco et al., 2016; Ornell et al., 2020; Tapia Granados and Diez Roux, 2009). According to the report of the Well Being Trust (WBT) and the Robert Graham Center for Political Studies in Family Medicine and Primary Care, additional 75,000 Americans could die from suicide, drugs or alcohol abuse, mainly in connection with the high unemployment rate caused from the pandemic (Brooks, 2020; Petterson et al., 2020).
3. Conclusions
Climate change, pollution, and virus-triggered outbreaks, such as the current COVID-19 pandemic are all naturally occurring, catastrophic events involving the whole world, with different timescales, but similar consequences on individuals and collectivity, in terms of both health and socio-economic aspects. Although far from reaching a clear conclusion, some evidence highlighted the possible connection between climate change, environmental pollution and COVID-19 pandemic. Air pollutants, in particular CO2, CH4, O3, and NOx, are indeed considered the main cause of the climate change (Botta et al., 2019). Furthermore, both air pollution, especially from fine PM, and destruction of the environment resulting from climate change have been associated with COVID-19 pandemic. To confirm these hypothesis, in countries like China and India, among the most polluted countries in the world, it has been shown that traffic restrictions and self-quarantine measures to control COVID-19, reduced environmental pollution (Chen et al., 2020c; Agarwal et al., 2020), especially NO2 and PM2.5 concentrations, the main pollutants related to traffic, and, consequently, decreased non-COVID-19 deaths, especially from cardiovascular disease and chronic respiratory diseases, the diseases most related to the environmental pollution (Chen et al., 2020c; Agarwal et al., 2020). Public health interventions such as school closures have obviously also reduced the growth of the epidemic (Jüni et al., 2020).
Not surprisingly, increasing recent observations authorize to hypothesize that climate change, environmental pollution, COVID-19 pandemic and mental health might be intertwined.
The effects of climate change on mental health range from high rates of negative emotional responses, including guilt, pain, anxiety and demoralization, to full-blown psychiatric disorders, particularly anxiety and depression disorders, stress/trauma-related disorders, substance abuse, and suicidal thoughts and intentions (U.S Global Change, R.P., 2016; Salcioglu et al., 2007; Kjellstrom, 2009; Brugha and Cragg, 1990). It should be noted that the health consequences of climate change are highly variable, as they are influenced by many factors (Hayes et al., 2019). First, there is a physiological vulnerability to climatic factors, so that some people are more sensitive than others to climate changes (i.e., subjects less able to cope with high levels of heat and/or defend against disease) (Hayes et al., 2019). Among the most vulnerable groups there are elderly subjects, children, women, people with pre-existing health problems especially mental illnesses, subjects taking some types of medications including psychotropic drugs, individuals with low socio-economic status, immigrants, and natives (Schwerdtle et al., 2017; Hayes et al., 2019; Cianconi et al., 2019; Furberg et al., 2011). Moreover, a heterogeneous meteosensitivity is present among the general population (Zikic and Žikić, 2018; Mazza et al., 2012). Middle aged people and women seem to be more sensitive than the other groups (Mazza et al., 2012; Hedge and Collis, 1987). Finally, a geographical vulnerability must be also considered: those subjects living on the plains, on the coast, or in areas prone to desertification or fires, seem to the most vulnerable to the environmental problems, as these areas are the most affected by climate disasters (Cianconi et al., 2020; Torres and Casey, 2017).
Air pollutants were associated to the pathophysiology of different psychiatric disorders, such as psychotic, depression, anxiety, and neuropsychiatric disorders (Attademo and Bernardini, 2020; Costa et al., 2020a; Shin et al., 2018; Attademo and Bernardini, 2017; Attademo et al., 2017; Lim et al., 2012; Power et al., 2015; Pun et al., 2017; Saez et al., 2018; Volk et al., 2013; Jung et al., 2013), as well as with the exacerbation of psychiatric symptoms (Shin et al., 2018; Bernardini et al., 2020; Szyszkowicz, 2007; Yackerson et al., 2014; Szyszkowicz et al., 2010; Kim et al., 2010; Lin et al., 2016; Oudin et al., 2018; Lim et al., 2012; Jung et al., 2013). Certainly it should be considered that air pollutants impacts on human health depends on wide range of factors: pollutant type, sources and concentration, time and way of exposure, interaction between different pollutants, as well as biological and socio-cultural factors, such as age, sex, ethnicity, previous illnesses, income, education, and neighbourhood, city, or country in which subject lives (Gaddi et al., 2018; Stewart et al., 2015). All these variables may in part explain the still inconclusive results of the influence of environmental pollution on mental health.
It is evident that COVID-19 pandemic uncovers all the fragility and weakness of our ecosystem and inability to protect ourselves from bio-pollutants as part of a broader fight against air pollution. At the same time, it highlights that “every catastrophe has its own origin” (Nyerat, 2008). Therefore, we must reflect on its meaning in order to prevent similar events in the future. Genetic and molecular analysis supported that Sars-CoV-2 could be originated from bats after passaging in intermediate hosts, highlighting the high zoonotic potential of coronaviruses (Salata et al., 2019; Malik et al., 2020). The large animal farms, requiring the destruction of natural habitat of several wild species are considered crucial for the spillover of the virus from animals to humans. It is also suspected that bat species commercialized and used in traditional Chinese medicine represent the natural reservoirs of the virus are represented by the (Wassenaar and Zou, 2020). As trade in these bats could be a potential risk of spreading zoonoses, it is strongly recommended that these practices be changed (Wassenaar and Zou, 2020).
One of the biggest obstacles for the positive interaction between the environment and health is the misperception of climate change, often resulting from psychological barriers of human beings (Gifford et al., 2011). Gifford identified some main psychological barriers that limit active behaviors against climate change, including limited knowledge about the problem, ideologies that oppose pro-environmental behavior, high cost of solution strategies, discrediting of experts and authorities (Gifford, 2011). Therefore, it would be essential to promote change of common people‘s behaviour, through correct information together with an adequate and effective “green” policy worldwide, and not fearing to take effective, albeit unpopular measures to decrease pollutants (Gaddi and Capello, 2020), and focused interventions to reduce the effects of dramatic climate change. As already underlined, “Rather than simply attempting to react to crises like COVID-19 after death and destruction are already upon us, we need to address the fundamental underlying causes and act now to prevent the numerous disasters that are literally waiting to happen” (Wiebers and Feigin, 2020).
In conclusion, the psychological/psychiatric consequences of COVID-19 pandemic, that currently seem unavoidable, represent a sharp cue of our misconception and indifference towards the links between our behaviors and the “health” of our planet and of ourselves, given that, at some point, the sudden emergence of stochastic effects may lead to irreversible disasters (Prigogine and Stengers, 1979). It is time to move towards a deeper understanding of these relationships, not only for our survival, but also for the maintenance of that balance between man, animals and environment at the basis of life on the earth (Marazziti, 2020). Without the promotion of a real ecological awareness worldwide, together with appropriate countermeasures to at least reduce, if not revert, climate change, air pollution, and intensive and destructive human activities, there will be no sustainable future.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or nonprofit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Scott Sheridan
References
- Agarwal A., Kaushik A., Kumar S., Mishra R.K. Comparative study on air quality status in Indian and Chinese cities before and during the COVID-19 lockdown period. Air Qual. Atmos. Health. 2020:11–12. doi: 10.1007/s11869-020-00881-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agustina L., Wulandari R. Environment as risk factors of schizophrenia: a systematic review. Life Sci. 2019;4:420. doi: 10.18502/kls.v4i10.3747. [DOI] [Google Scholar]
- Ahern M., Kovats R.S., Wilkinson P., Few R., Matthies F. Global health impacts of floods: epidemiologic evidence. Epidemiol. Rev. 2005;27:36–46. doi: 10.1093/epirev/mxi004. [DOI] [PubMed] [Google Scholar]
- Albrecht G., Sartore G.M., Connor L., Higginbotham N., Freeman S., Kelly B., Stain H., Tonna A., Pollard G. Solastalgia: the distress caused by environmental change. Australas. Psychiatry. 2007;15(Suppl. 1):S95–S98. doi: 10.1080/10398560701701288. [DOI] [PubMed] [Google Scholar]
- Alenina N., Bader M. ACE2 in brain physiology and pathophysiology: evidence from transgenic animal models. Neurochem. Res. 2019;44:1323–1329. doi: 10.1007/s11064-018-2679-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshehri F.S., Alatawi Y., Alghamdi B.S., Alhifany A.A., Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharm J. 2020 doi: 10.1016/j.jsps.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ampel L., Wohlfarth B., Risberg J., Veres D., Leng M.J., Tillman P.K. Diatom assemblage dynamics during abrupt climate change: the response of lacustrine diatoms to Dansgaard–Oeschger cycles during the last glacial period. J. Paleolimnol. 2010;44:397–404. doi: 10.1007/s10933-009-9350-7. [DOI] [Google Scholar]
- Anderson C.A., Anderson K.B., Dorr N., DeNeve K.M., Flanagan M. Adv. Exp. Soc. Psychol. Vol. 32. Academic Press; San Diego, CA, US: 2000. Temperature and aggression; pp. 63–133. [DOI] [Google Scholar]
- Anderson D.G., Goodyear A.C., Kennett J., West A. Multiple lines of evidence for possible human population decline/settlement reorganization during the early Younger Dryas. Quat. Int. 2011;242:570–583. doi: 10.1016/j.quaint.2011.04.020. [DOI] [Google Scholar]
- Andree B. Incidence of COVID-19 and connections with air pollution exposure: evidence from the Netherlands. World Bank Working Paper. 2020;WPS9221:1–30. doi: 10.6084/m9.figshare.12220895. [DOI] [Google Scholar]
- Arcanjo, M.J.W.D.A.C.I.P.P. Eco-anxiety: mental health impacts of environmental disasters and climate change. 2019, A Climate Institute Publication, 1201 New York Avenue.
- Attademo L., Bernardini F. Air pollution and urbanicity: common risk factors for dementia and schizophrenia? Lancet Planet Health. 2017;1:e90–e91. doi: 10.1016/s2542-5196(17)30042-6. [DOI] [PubMed] [Google Scholar]
- Attademo L., Bernardini F. Air pollution as risk factor for mental disorders: in search for a possible link with Alzheimer’s disease and schizophrenia. J. Alzheimers Dis. 2020;76:825–830. doi: 10.3233/jad-200289. [DOI] [PubMed] [Google Scholar]
- Attademo L., Bernardini F., Garinella R., Compton M.T. Environmental pollution and risk of psychotic disorders: a review of the science to date. Schizophr. Res. 2017;181:55–59. doi: 10.1016/j.schres.2016.10.003. [DOI] [PubMed] [Google Scholar]
- Avula A., Nalleballe K., Narula N., Sapozhnikov S., Dandu V., Toom S., Glaser A., Elsayegh D. COVID-19 presenting as stroke. Brain Behav. Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aziz M., Fatima R., Assaly R. Elevated interleukin-6 and severe COVID-19: A metaanalysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai L., Zhang X., Zhang Y., Cheng Q., Duan J., Gao J., Xu Z., Zhang H., Wang S., Su H. Ambient concentrations of NO(2) and hospital admissions for schizophrenia. Occup. Environ. Med. 2019;76:125–131. doi: 10.1136/oemed-2018-105162. [DOI] [PubMed] [Google Scholar]
- Bakunina N., Pariante C.M., Zunszain P.A. Immune mechanisms linked to depression via oxidative stress and neuroprogression. Immunology. 2015;144:365–373. doi: 10.1111/imm.12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsamo V., Sirtori P.G., Miani A., Jr., Di Francesco A., Franceschini R., Mauro F., Alberti G., Grassi G. Meteoropathy: a syndrome continuously on the increase. Clin. Ter. 1992;141:3–8. [PubMed] [Google Scholar]
- Banerjee D., Viswanath B. Neuropsychiatric manifestations of COVID-19 and possible pathogenic mechanisms: insights from other coronaviruses. Asian J. Psychiatr. 2020;54:102350–102,350. doi: 10.1016/j.ajp.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbisch D., Koenig K.L., Shih F.Y. Is there a case for quarantine? Perspectives from SARS to Ebola. Disaster Med Public Health Prep. 2015;9:547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic stress in healthcare workers during COVID-19 pandemic: a review of the immediate impact. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson N.M., Öngür D., Hsu J. COVID-19 testing and patients in mental health facilities. Lancet Psychiatry. 2020;7:476–477. doi: 10.1016/S2215-0366(20)30198-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardini F., Attademo L., Trezzi R., Gobbicchi C., Balducci P.M., Del Bello V., Menculini G., Pauselli L., Piselli M., Sciarma T., et al. Air pollutants and daily number of admissions to psychiatric emergency services: evidence for detrimental mental health effects of ozone. Epidemiol. Psychiatr. Sci. 2019;29:e66. doi: 10.1017/s2045796019000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardini F., Attademo L., Trezzi R., Gobbicchi C., Balducci P., Del Bello V., Menculini G., Pauselli L., Piselli M., Sciarma T., Moretti P., Tamantini A., Quartesan R., Compton M.T., Tortorella A. Air pollutants and daily number of admissions to psychiatric emergency services: evidence for detrimental mental health effects of ozone. Epidemiol Psychiatr Sci. 2020;29, E66 doi: 10.1017/S2045796019000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry H., Kelly B., Hanigan I., Coates J., McMichael A., Welsh J., Kjellstrom T. Rural mental health impacts of climate change. Commissioned report for the Garnaut Climate Change Review, Australian National University (Canberra, Australia). 2008:1–31. [Google Scholar]
- Berry H., Bowen K., Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. 2010;55:123–132. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- Bersani F.S., Wolkowitz O.M., Lindqvist D., Yehuda R., Flory J., Bierer L.M., Makotine I., Abu-Amara D., Coy M., Reus V.I., et al. Global arginine bioavailability, a marker of nitric oxide synthetic capacity, is decreased in PTSD and correlated with symptom severity and markers of inflammation. Brain Behav. Immun. 2016;52:153–160. doi: 10.1016/j.bbi.2015.10.015. [DOI] [PubMed] [Google Scholar]
- Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., Liu X., Wei L., Truelove S., Zhang T., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect. Dis. 2020;20, 8:911–919. doi: 10.1016/S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanc J., Spruill T., Butler M., Casimir G., Jean-Louis G. 0885 Is resilience a protective factor for sleep disturbances among earthquake survivors? Sleep. 2019;42:A356. doi: 10.1093/sleep/zsz067.883. [DOI] [Google Scholar]
- Block M.L., Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009;32:506–516. doi: 10.1016/j.tins.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block M.L., Wu X., Pei Z., Li G., Wang T., Qin L., Wilson B., Yang J., Hong J.S., Veronesi B. Nanometer size diesel exhaust particles are selectively toxic to dopaminergic neurons: the role of microglia, phagocytosis, and NADPH oxidase. FASEB J. 2004;18:1618–1620. doi: 10.1096/fj.04-1945fje. [DOI] [PubMed] [Google Scholar]
- Bo H.-X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.-T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostancıklıoğlu M. SARS-CoV2 entry and spread in the lymphatic drainage system of the brain. Brain Behav. Immun. 2020;87:122–123. doi: 10.1016/j.bbi.2020.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botta F., Dahl-Jensen D., Rahbek C., Svensson A., Nogués-Bravo D. Abrupt change in climate and biotic systems. Curr. Biol. 2019;29:R1045–r1054. doi: 10.1016/j.cub.2019.08.066. [DOI] [PubMed] [Google Scholar]
- Boufidou F., Lambrinoudaki I., Argeitis J., Zervas I.M., Pliatsika P., Leonardou A.A., Petropoulos G., Hasiakos D., Papadias K., Nikolaou C. CSF and plasma cytokines at delivery and postpartum mood disturbances. J. Affect. Disord. 2009;115:287–292. doi: 10.1016/j.jad.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Bourque F., Willox A.C. Climate change: the next challenge for public mental health? Int Rev. Psychiatry. 2014;26:415–422. doi: 10.3109/09540261.2014.925851. [DOI] [PubMed] [Google Scholar]
- Bright F., Werry E.L., Dobson-Stone C., Piguet O., Ittner L.M., Halliday G.M., Hodges J.R., Kiernan M.C., Loy C.T., Kassiou M., et al. Neuroinflammation in frontotemporal dementia. Nat. Rev. Neurol. 2019;15:540–555. doi: 10.1038/s41582-019-0231-z. [DOI] [PubMed] [Google Scholar]
- Brockmeyer S., D’Angiulli A. How air pollution alters brain development: the role of neuroinflammation. Transl. Neurosci. 2016;7:24–30. doi: 10.1515/tnsci-2016-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, M. US ‘deaths of despair’ from COVID-19 could top 75,000, experts warn 2020.
- Brooks S., Webster R., Smith L., Woodland L., Wessely S., Greenberg N., Rubin G. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugha T.S., Cragg D. The list of threatening experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr. Scand. 1990;82:77–81. doi: 10.1111/j.1600-0447.1990.tb01360.x. [DOI] [PubMed] [Google Scholar]
- Brunekreef B., Holgate S.T. Air pollution and health. Lancet. 2002;360:1233–1242. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- Buemann B., Marazziti D., Uvnäs-Moberg K. Can intravenous oxytocin infusion counteract hyperinflammation in COVID-19 infected patients? World J Biol Psychiatry. 2020:1–12. doi: 10.1080/15622975.2020.1814408. [DOI] [PubMed] [Google Scholar]
- Buoli M., Grassi S., Caldiroli A., Carnevali G.S., Mucci F., Iodice S., Cantone L., Pergoli L., Bollati V. Is there a link between air pollution and mental disorders? Environ. Int. 2018;118:154–168. doi: 10.1016/j.envint.2018.05.044. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Solt A.C., Henríquez-Roldán C., Torres-Jardón R., Nuse B., Herritt L., Villarreal-Calderón R., Osnaya N., Stone I., García R., et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol. Pathol. 2008;36:289–310. doi: 10.1177/0192623307313011. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Mora-Tiscareño A., Ontiveros E., Gómez-Garza G., Barragán-Mejía G., Broadway J., Chapman S., Valencia-Salazar G., Jewells V., Maronpot R.R., et al. Air pollution, cognitive deficits and brain abnormalities: a pilot study with children and dogs. Brain Cogn. 2008;68:117–127. doi: 10.1016/j.bandc.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Engle R., Mora-Tiscareño A., Styner M., Gómez-Garza G., Zhu H., Jewells V., Torres-Jardón R., Romero L., Monroy-Acosta M.E., et al. Exposure to severe urban air pollution influences cognitive outcomes, brain volume and systemic inflammation in clinically healthy children. Brain Cogn. 2011;77:345–355. doi: 10.1016/j.bandc.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Kavanaugh M., Block M., D’Angiulli A., Delgado-Chávez R., Torres-Jardón R., González-Maciel A., Reynoso-Robles R., Osnaya N., Villarreal-Calderon R., et al. Neuroinflammation, hyperphosphorylated tau, diffuse amyloid plaques, and down-regulation of the cellular prion protein in air pollution exposed children and young adults. J. Alzheimers Dis. 2012;28:93–107. doi: 10.3233/jad-2011-110722. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Cross J.V., Franco-Lira M., Aragón-Flores M., Kavanaugh M., Torres-Jardón R., Chao C.-K., Thompson C., Chang J., Zhu H., et al. Brain immune interactions and air pollution: macrophage inhibitory factor (MIF), prion cellular protein (PrP(C)), Interleukin-6 (IL-6), interleukin 1 receptor antagonist (IL-1Ra), and interleukin-2 (IL-2) in cerebrospinal fluid and MIF in serum differentiate urban children exposed to severe vs. low air pollution. Front. Neurosci. 2013;7:183. doi: 10.3389/fnins.2013.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L., Leray E., Heydarpour P., Torres-Jardón R., Reis J. Air pollution, a rising environmental risk factor for cognition, neuroinflammation and neurodegeneration: the clinical impact on children and beyond. Rev. Neurol. (Paris) 2016;172:69–80. doi: 10.1016/j.neurol.2015.10.008. [DOI] [PubMed] [Google Scholar]
- Campbell T., Campbell A. Emerging disease burdens and the poor in cities of the developing world. Journal of urban health: bulletin of the New York Academy of Medicine. 2007;84:54–64. doi: 10.1007/s11524-007-9181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carugno M., Dentali F., Mathieu G., Fontanella A., Mariani J., Bordini L., Milani G.P., Consonni D., Bonzini M., Bollati V., et al. PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy, Italy. Environ. Res. 2018;166:452–457. doi: 10.1016/j.envres.2018.06.016. [DOI] [PubMed] [Google Scholar]
- Chan J.F.-W., Zhang A.J., Yuan S., Poon V.K.-M., Chan C.C.-S., Lee A.C.-Y., Chan W.-M., Fan Z., Tsoi H.-W., Wen L., et al. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamstermodel: implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheatwood D. The effects of weather on homicide. J. Quant. Criminol. 1995;11:51–70. doi: 10.1007/BF02221300. [DOI] [Google Scholar]
- Chen J.C., Wang X., Wellenius G.A., Serre M.L., Driscoll I., Casanova R., McArdle J.J., Manson J.E., Chui H.C., Espeland M.A. Ambient air pollution and neurotoxicity on brain structure: evidence from women’s health initiative memory study. Ann. Neurol. 2015;78:466–476. doi: 10.1002/ana.24460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Kwong J.C., Copes R., Tu K., Villeneuve P.J., van Donkelaar A., Hystad P., Martin R.V., Murray B.J., Jessiman B., et al. Living near major roads and the incidence of dementia, Parkinson's disease, and multiple sclerosis: a population-based cohort study. Lancet. 2017;389:718–726. doi: 10.1016/s0140-6736(16)32399-6. [DOI] [PubMed] [Google Scholar]
- Chen C., Liu C., Chen R., Wang W., Li W., Kan H., Fu C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Sci. Total Environ. 2018;613-614:324–330. doi: 10.1016/j.scitotenv.2017.09.098. [DOI] [PubMed] [Google Scholar]
- Chen B., Liang H., Yuan X., Hu Y., Xu M., Zhao Y., Zhang B., Tian F., Zhu X. 2020. Roles of meteorological conditions in COVID-19 transmission on a worldwide scale. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/s0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K., Wang M., Huang C., Kinney P.L., Anastas P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4:e210–e212. doi: 10.1016/s2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho J., Choi Y.J., Sohn J., Suh M., Cho S.K., Ha K.H., Kim C., Shin D.C. Ambient ozone concentration and emergency department visits for panic attacks. J. Psychiatr. Res. 2015;62:130–135. doi: 10.1016/j.jpsychires.2015.01.010. [DOI] [PubMed] [Google Scholar]
- Cianconi P., Lesmana C., Ventriglio A., Janiri L. Mental health issues among indigenous communities and the role of traditional medicine. Int J Soc Psychiatry. 2019;65(4):289–299. doi: 10.1177/0020764019840060. [DOI] [PubMed] [Google Scholar]
- Cianconi P., Betrò S., Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front Psychiatry. 2020;11:74. doi: 10.3389/fpsyt.2020.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayton S. Climate anxiety: psychological responses to climate change. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102263. [DOI] [PubMed] [Google Scholar]
- Clifford A., Lang L., Chen R., Anstey K.J., Seaton A. Exposure to air pollution and cognitive functioning across the life course–a systematic literature review. Environ. Res. 2016;147:383–398. doi: 10.1016/j.envres.2016.01.018. [DOI] [PubMed] [Google Scholar]
- Coccia, M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020, 729: 138474, doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed]
- Coêlho A., Adair J., Mocellin J. Psychological responses to drought in northeastern Brazil. Revista Interamericana de Psicología. 2004;38(1):95–103. [Google Scholar]
- Cohn E., Rotton J., Peterson A., Tarr D. Temperature. City size, and the southern subculture of violence: support for social escape/avoidance (SEA) Theory1. J. Appl. Soc. Psychol. 2004;34:1652–1674. doi: 10.1111/j.1559-1816.2004.tb02792.x. [DOI] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in northern Italy. Environ. Pollut. 2020;261:114,465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi-Zuelli F., Loureiro C.M., Shuhama R., Fachim H.A., Menezes P.R., Louzada-Junior P., Mondelli V., Del-Ben C.M. Cytokine profile in first-episode psychosis, unaffected siblings and community-based controls: the effects of familial liability and childhood maltreatment. Psychol. Med. 2020;50:1139–1147. doi: 10.1017/s0033291719001016. [DOI] [PubMed] [Google Scholar]
- Ćosić K., Popović S., Šarlija M., Kesedžić I. Impact of human disasters and COVID-19 pandemic on mental health: potential of digital psychiatry. Psychiatr. Danub. 2020;32:25–31. doi: 10.24869/psyd.2020.25. [DOI] [PubMed] [Google Scholar]
- Costa L.G., Cole T.B., Dao K., Chang Y.C., Coburn J., Garrick J.M. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 2020;210 doi: 10.1016/j.pharmthera.2020.107523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa M., Pavlo A., Reis G., Ponte K., Davidson L. COVID-19 concerns among persons with mental illness. Psychiatr. Serv. 2020 doi: 10.1176/appi.ps.202000245. [DOI] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.F., Froines J., Zhao J., Wang H., Yu S.Z., Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ. Health. 2003;2(1):15. doi: 10.1186/1476-069x-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels B.P., Jujjavarapu H., Durrant D.M., Williams J.L., Green R.R., White J.P., Lazear H.M., Gale M., Jr., Diamond M.S., Klein R.S. Regional astrocyte IFN signaling restricts pathogenesis during neurotropic viral infection. J. Clin. Invest. 2017;127:843–856. doi: 10.1172/jci88720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delamater P.L., Street E.J., Leslie T.F., Yang Y.T., Jacobsen K.H. Complexity of the basic reproduction number (R0) Emerg infec Dis. 2019;25(1):1–4. doi: 10.3201/eid2501.171901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desforges M., Le Coupanec A., Brison E., Meessen-Pinard M., Talbot P.J. Neuroinvasive and neurotropic human respiratory coronaviruses: potential neurovirulent agents in humans. Adv. Exp. Med. Biol. 2014;807:75–96. doi: 10.1007/978-81-322-1777-0_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diz D.I., Garcia-Espinosa M.A., Gegick S., Tommasi E.N., Ferrario C.M., Ann Tallant E., Chappell M.C., Gallagher P.E. Injections of angiotensin-converting enzyme 2 inhibitor MLN4760 into nucleus tractus solitarii reduce baroreceptor reflex sensitivity for heart rate control in rats. Exp. Physiol. 2008;93:694–700. doi: 10.1113/expphysiol.2007.040261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donzelli G., Llopis-Gonzalez A., Llopis-Morales A., Cioni L., Morales Suárez-Varela M. Particulate matter exposure and attention-deficit/hyperactivity disorder in children: a systematic review of epidemiological studies. Int. J. Environ. Res. Public Health. 2019;17(1):67. doi: 10.3390/ijerph17010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driessen A.K., Farrell M.J., Mazzone S.B., McGovern A.E. Multiple neural circuits mediating airway sensations: recent advances in the neurobiology of the urge-to-cough. Respir. Physiol. Neurobiol. 2016;226:115–120. doi: 10.1016/j.resp.2015.09.017. [DOI] [PubMed] [Google Scholar]
- Duan J., Cheng Q., Luo X., Bai L., Zhang H., Wang S., Xu Z., Gao J., Zhang Y., Su H. Is the serious ambient air pollution associated with increased admissions for schizophrenia? Sci. Total Environ. 2018;644:14–19. doi: 10.1016/j.scitotenv.2018.06.218. [DOI] [PubMed] [Google Scholar]
- El Morabet R. Elsevier; 2018. Effects of outdoor air pollution on human health. In reference module in earth systems and environmental sciences. [DOI] [Google Scholar]
- Enache D., Pariante C.M., Mondelli V. Markers of central inflammation in major depressive disorder: a systematic review and meta-analysis of studies examining cerebrospinal fluid, positron emission tomography and post-mortem brain tissue. Brain Behav. Immun. 2019;81:24–40. doi: 10.1016/j.bbi.2019.06.015. [DOI] [PubMed] [Google Scholar]
- Eze I.C., Schaffner E., Fischer E., Schikowski T., Adam M., Imboden M., Tsai M., Carballo D., von Eckardstein A., Künzli N., et al. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ. Int. 2014;70:95–105. doi: 10.1016/j.envint.2014.05.014. [DOI] [PubMed] [Google Scholar]
- Fekih-Romdhane F., Ghrissi F., Abbassi B., Cherif W., Cheour M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felger J.C. Imaging the role of inflammation in mood and anxiety-related disorders. Curr. Neuropharmacol. 2018;16:533–558. doi: 10.2174/1570159X15666171123201142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Félix-Arellano E., Schilmann A., Magali H.-D., Texcalac Sangrador J.L., Riojas-Rodriguez H. Revisión rápida: contaminación del aire y morbimortalidad por Covid-19. Salud Publica Mex. 2020 doi: 10.21149/11481. [DOI] [PubMed] [Google Scholar]
- Fett A.-K.J., Lemmers-Jansen I.L.J., Krabbendam L. Psychosis and urbanicity: a review of the recent literature from epidemiology to neurourbanism. Curr Opin Psychiatry. 2019;32:232–241. doi: 10.1097/YCO.0000000000000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filatov A., Sharma P., Hindi F., Espinosa P.S. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12:e7352. doi: 10.7759/cureus.7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay I., Gilmore I. Covid-19 and alcohol—a dangerous cocktail. BMJ. 2020;369, m1987 doi: 10.1136/bmj.m1987. [DOI] [PubMed] [Google Scholar]
- Fodoulian L., Tuberosa J., Rossier D., Landis B., Carleton A., Rodriguez I. SARS-CoV-2 receptor and entry genes are expressed by sustentacular cells in the human olfactory neuroepithelium. bioRxiv. 2020 doi: 10.1101/2020.03.31.013268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire C., Ramos R., Puertas R., Lopez-Espinosa M.J., Julvez J., Aguilera I., Cruz F., Fernandez M.F., Sunyer J., Olea N. Association of traffic-related air pollution with cognitive development in children. J. Epidemiol. Community Health. 2010;64:223–228. doi: 10.1136/jech.2008.084574. [DOI] [PubMed] [Google Scholar]
- Furberg M., Evengård B., Nilsson M. Facing the limit of resilience: perceptions of climate change among reindeer herding Sami in Sweden. Glob. Health Action. 2011;4 doi: 10.3402/gha.v4i0.8417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furtado M., Katzman M.A. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229:37–48. doi: 10.1016/j.psychres.2015.05.036. [DOI] [PubMed] [Google Scholar]
- Gaddi A., Capello F. 2020. Particulate does matter: is Covid-19 another air pollution related disease? [DOI] [Google Scholar]
- Gaddi A.V., Sabatini I., Capello F. In: Clinical Handbook of Air Pollution-Related Diseases. Capello F., Gaddi A.V., editors. Springer International Publishing; Cham: 2018. Complexity in Pollution/Disease Management; pp. 253–262. [DOI] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gao Q., Xu Q., Guo X., Fan H., Zhu H. Particulate matter air pollution associated with hospital admissions for mental disorders: a time-series study in Beijing, China. Eur Psychiatry. 2017;44:68–75. doi: 10.1016/j.eurpsy.2017.02.492. [DOI] [PubMed] [Google Scholar]
- Gibb R., Franklinos L.H.V., Redding D.W., Jones K.E. Ecosystem perspectives are needed to manage zoonotic risks in a changing climate. BMJ. 2020;371 doi: 10.1136/bmj.m3389. m3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford R. The dragons of inaction: psychological barriers that limit climate change mitigation and adaptation. Am Psychol. 2011;66:290–302. doi: 10.1037/a0023566. [DOI] [PubMed] [Google Scholar]
- Gifford E., Gifford R. The largely unacknowledged impact of climate change on mental health. Bull. At. Sci. 2016;72:292–297. doi: 10.1080/00963402.2016.1216505. [DOI] [Google Scholar]
- Gifford R., Kormos C., McIntyre A. Behavioral dimensions of climate change: drivers, responses, barriers, and interventions. Wiley Interdiscip. Rev. Clim. Chang. 2011;2(6):801–827. doi: 10.1002/wcc.143. [DOI] [Google Scholar]
- Glencross D.A., Ho T.R., Camiña N., Hawrylowicz C.M., Pfeffer P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020;151:56–68. doi: 10.1016/j.freeradbiomed.2020.01.179. [DOI] [PubMed] [Google Scholar]
- Gorbalenya A., Baker S., Baric R., de Groot R., Drosten C., Gulyaeva A., Haagmans B., Lauber C., Leontovich A., Neuman B., et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiology. 2020;5 doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowrisankar Y.V., Clark M.A. Angiotensin II regulation of angiotensin-converting enzymes in spontaneously hypertensive rat primary astrocyte cultures. J. Neurochem. 2016;138:74–85. doi: 10.1111/jnc.13641. [DOI] [PubMed] [Google Scholar]
- Gray S.M., Bloch M.H. Systematic review of proinflammatory cytokines in obsessive-compulsive disorder. Curr Psychiatry Rep. 2012;14:220–228. doi: 10.1007/s11920-012-0272-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/s2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X.-J., Zhang H., Zeng Y.-P. 2020. Transmissibility of COVID-19 and its association with temperature and humidity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guxens M., Sunyer J. A review of epidemiological studies on neuropsychological effects of air pollution. Swiss Med. Wkly. 2012;141, w13322 doi: 10.4414/smw.2011.13322. [DOI] [PubMed] [Google Scholar]
- Guxens M., Garcia-Esteban R., Giorgis-Allemand L., Forns J., Badaloni C., Ballester F., Beelen R., Cesaroni G., Chatzi L., de Agostini M., et al. Air pollution during pregnancy and childhood cognitive and psychomotor development: six European birth cohorts. Epidemiology. 2014;25:636–647. doi: 10.1097/ede.0000000000000133. [DOI] [PubMed] [Google Scholar]
- Hamer M., Stamatakis E. Inflammation as an intermediate pathway in the association between psychosocial stress and obesity. Physiol. Behav. 2008;94:536–539. doi: 10.1016/j.physbeh.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Hansen A., Bi P., Nitschke M., Ryan P., Pisaniello D., Tucker G. The effect of heat waves on mental health in a temperate Australian city. Environ. Health Perspect. 2008;116:1369–1375. doi: 10.1289/ehp.11339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes K., Blashki G., Wiseman J., Burke S., Reifels L. Climate change and mental health: risks, impacts and priority actions. Int J Ment Health Syst. 2018;12:28. doi: 10.1186/s13033-018-0210-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes K., Berry P., Ebi K.L. Factors influencing the mental health consequences of climate change in Canada. Int. J. Environ. Res. Public Health. 2019;16(9):1583. doi: 10.3390/ijerph16091583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedge A., Collis M.D. Do negative air ions affect human mood and performance? Ann Occup Hyg. 1987;31:285–290. doi: 10.1093/annhyg/31.3.285. [DOI] [PubMed] [Google Scholar]
- Heinz A., Deserno L., Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. 2013;12:187–197. doi: 10.1002/wps.20056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., Collange O., Boulay C., Fafi-Kremer S., Ohana M., et al. Neurologic features in severe SARS-CoV-2 infection. N. Engl. J. Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppner F.L., Ransohoff R.M., Becher B. Immune attack: the role of inflammation in Alzheimer’s disease. Nat. Rev. Neurosci. 2015;16:358–372. doi: 10.1038/nrn3880. [DOI] [PubMed] [Google Scholar]
- Hoang T., Anh T. Ambient air pollution, meteorology, and COVID-19 infection in Korea. J. Med. Virol. 2020 doi: 10.1002/jmv.26325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodes G.E., Ménard C., Russo S.J. Integrating Interleukin-6 into depression diagnosis and treatment. Neurobiol Stress. 2016;4:15–22. doi: 10.1016/j.ynstr.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/s2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howarth E., Hoffman M.S. A multidimensional approach to the relationship between mood and weather. Br. J. Psychol. 1984;75:15–23. doi: 10.1111/j.2044-8295.1984.tb02785.x. [DOI] [PubMed] [Google Scholar]
- Hughes I.I. Biological consequences of global warming: is the signal already apparent? Trends Ecol. Evol. 2000;15:56–61. doi: 10.1016/s0169-5347(99)01764-4. [DOI] [PubMed] [Google Scholar]
- Hughes T.J., Pellizzari E., Little L., Sparacino C., Kolber A. Ambient air pollutants: collection, chemical characterization and mutagenicity testing. Mutat. Res. Rev. Mutat. Res. 1980;76:51–83. doi: 10.1016/0165-1110(80)90003-2. [DOI] [PubMed] [Google Scholar]
- Huq S., Kovats S., Reid H., Satterthwaite D. London, England: SAGE Publications Sage UK; 2007. Reducing risks to cities from disasters and climate change.
- Jackson S.T., Booth R.K., Reeves K., Andersen J.J., Minckley T.A., Jones R.A. Inferring local to regional changes in forest composition from Holocene macrofossils and pollen of a small lake in central Upper Michigan. Quat. Sci. Rev. 2014;98:60–73. doi: 10.1016/j.quascirev.2014.05.030. [DOI] [Google Scholar]
- Jo H., Eckel S.P., Wang X., Chen J.C., Cockburn M., Martinez M.P., Chow T., Molshatzki N., Lurmann F.W., Funk W.E., et al. Sex-specific associations of autism spectrum disorder with residential air pollution exposure in a large Southern California pregnancy cohort. Environ. Pollut. 2019;254 doi: 10.1016/j.envpol.2019.113010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junaid M., Syed J.H., Abbasi N.A., Hashmi M.Z., Malik R.N., Pei D.S. Status of indoor air pollution (IAP) through particulate matter (PM) emissions and associated health concerns in South Asia. Chemosphere. 2018;191:651–663. doi: 10.1016/j.chemosphere.2017.10.097. [DOI] [PubMed] [Google Scholar]
- Jung C.R., Lin Y.T., Hwang B.F. Air pollution and newly diagnostic autism spectrum disorders: a population-based cohort study in Taiwan. PLoS One. 2013;8 doi: 10.1371/journal.pone.0075510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jüni P., Rothenbühler M., Bobos P., Thorpe K.E., da Costa B.R., Fisman D.N., Slutsky A.S., Gesink D. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ: Canadian Medical Association journal. 2020;192:E566–e573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampa M., Castanas E. Human health effects of air pollution. Environ. Pollut. 2008;151:362–367. doi: 10.1016/j.envpol.2007.06.012. [DOI] [PubMed] [Google Scholar]
- Karagüzel E., Arslan F.C., Uysal E.K., Demir S., Aykut D.S., Tat M., Karahan S.C. Blood levels of interleukin-1 beta, interleukin-6 and tumor necrosis factor-alpha and cognitive functions in patients with obsessive compulsive disorder. Compr. Psychiatry. 2019;89:61–66. doi: 10.1016/j.comppsych.2018.11.013. [DOI] [PubMed] [Google Scholar]
- Kaufman J.A., Wright J.M., Rice G., Connolly N., Bowers K., Anixt J. Ambient ozone and fine particulate matter exposures and autism spectrum disorder in metropolitan Cincinnati, Ohio. Environ. Res. 2019;171:218–227. doi: 10.1016/j.envres.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelishadi R., Poursafa P. Air pollution and non-respiratory health hazards for children. Arch Med Sci: AMS. 2010;6:483–495. doi: 10.5114/aoms.2010.14458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelishadi R., Mirghaffari N., Poursafa P., Gidding S.S. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis. 2009;203:311–319. doi: 10.1016/j.atherosclerosis.2008.06.022. [DOI] [PubMed] [Google Scholar]
- Kern S., Skoog I., Börjesson-Hanson A., Blennow K., Zetterberg H., Ostling S., Kern J., Gudmundsson P., Marlow T., Rosengren L., et al. Higher CSF interleukin-6 and CSF interleukin-8 in current depression in older women. Results from a population-based sample. Brain Behav. Immun. 2014;41:55–58. doi: 10.1016/j.bbi.2014.05.006. [DOI] [PubMed] [Google Scholar]
- Khan A., Plana-Ripoll O., Antonsen S., Brandt J., Geels C., Landecker H., Sullivan P.F., Pedersen C.B., Rzhetsky A. Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLoS Biol. 2019;17(8) doi: 10.1371/journal.pbio.3000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T.J., von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int. Arch. Occup. Environ. Health. 2016;89:561–573. doi: 10.1007/s00420-015-1107-1. [DOI] [PubMed] [Google Scholar]
- Kim C., Jung S.H., Kang D.R., Kim H.C., Moon K.T., Hur N.W., Shin D.C., Suh I. Ambient particulate matter as a risk factor for suicide. Am. J. Psychiatry. 2010;167:1100–1107. doi: 10.1176/appi.ajp.2010.09050706. [DOI] [PubMed] [Google Scholar]
- Kim K.H., Kabir E., Kabir S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015;74:136–143. doi: 10.1016/j.envint.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Kim S.H., Shin S.D., Song K.J., Ro Y.S., Kong S.Y., Kim J., Ko S.Y., Lee S.Y. Association between ambient PM(2.5) and emergency department visits for psychiatric emergency diseases. Am. J. Emerg. Med. 2019;37:1649–1656. doi: 10.1016/j.ajem.2018.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kioumourtzoglou M.A., Power M.C., Hart J.E., Okereke O.I., Coull B.A., Laden F., Weisskopf M.G. The association between air pollution and onset of depression among middle-aged and older women. Am. J. Epidemiol. 2017;185:801–809. doi: 10.1093/aje/kww163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkbride J.B., Morgan C., Fearon P., Dazzan P., Murray R.M., Jones P.B. Neighbourhood-level effects on psychoses: re-examining the role of context. Psychol. Med. 2007;37:1413–1425. doi: 10.1017/s0033291707000499. [DOI] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369, m1642 doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Glob. Health Action. 2009;2:10. doi: 10.3402/gha.v2i0.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein R.S., Garber C., Funk K.E., Salimi H., Soung A., Kanmogne M., Manivasagam S., Agner S., Cain M. Neuroinflammation during RNA viral infections. Ann Rev Immunol. 2019;37:73–95. doi: 10.1146/annurev-immunol-042718-041417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klok F.A., Kruip M., van der Meer N.J.M., Arbous M.S., Gommers D., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohno M., Link J., Dennis L.E., McCready H., Huckans M., Hoffman W.F., Loftis J.M. Neuroinflammation in addiction: a review of neuroimaging studies and potential immunotherapies. Pharmacol. Biochem. Behav. 2019;179:34–42. doi: 10.1016/j.pbb.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The covid-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020;46:752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krabbendam L., van Os J. Schizophrenia and urbanicity: amajor environmental influence—conditional on genetic risk. Schizophr. Bull. 2005;31:795–799. doi: 10.1093/schbul/sbi060. [DOI] [PubMed] [Google Scholar]
- Kristensson K., Masocha W., Bentivoglio M. Mechanisms of CNS invasion and damage by parasites. Handb. Clin. Neurol. 2013;114:11–22. doi: 10.1016/b978-0-444-53490-3.00002-9. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan P.J., Fuller R., Acosta N.J.R., Adeyi O., Arnold R., Basu N.N., Baldé A.B., Bertollini R., Bose-O’Reilly S., Boufford J.I., et al. The lancet commission on pollution and health. Lancet. 2018;391:462–512. doi: 10.1016/s0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44:393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Lee S., Lee W., Kim D., Kim E., Myung W., Kim S.Y., Kim H. Short-term PM(2.5) exposure and emergency hospital admissions for mental disease. Environ. Res. 2019;171:313–320. doi: 10.1016/j.envres.2019.01.036. [DOI] [PubMed] [Google Scholar]
- Lelieveld J., Evans J.S., Fnais M., Giannadaki D., Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- Levesque S., Taetzsch T., Lull M.E., Kodavanti U., Stadler K., Wagner A., Johnson J.A., Duke L., Kodavanti P., Surace M.J., et al. Diesel exhaust activates and primes microglia: air pollution, neuroinflammation, and regulation of dopaminergic neurotoxicity. Environ. Health Perspect. 2011;119:1149–1155. doi: 10.1289/ehp.1002986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Wang N., Wang J., Li H. Spatiotemporal evolution of the remotely sensed global continental PM(2.5) concentration from 2000 to 2014 based on Bayesian statistics. Environ. Pollut. 2018;238:471–481. doi: 10.1016/j.envpol.2018.03.050. [DOI] [PubMed] [Google Scholar]
- Lim Y.H., Kim H., Kim J.H., Bae S., Park H.Y., Hong Y.C. Air pollution and symptoms of depression in elderly adults. Environ. Health Perspect. 2012;120:1023–1028. doi: 10.1289/ehp.1104100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin G.Z., Li L., Song Y.F., Zhou Y.X., Shen S.Q., Ou C.Q. The impact of ambient air pollution on suicide mortality: a case-crossover study in Guangzhou, China. Environ. Health. 2016;15(1):90. doi: 10.1186/s12940-016-0177-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl J.F., Grace D. The consequences of human actions on risks for infectious diseases: a review. Infec. Ecol. Epidemiol. 2015;5:30048–30,048. doi: 10.3402/iee.v5.30048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindqvist D., Janelidze S., Hagell P., Erhardt S., Samuelsson M., Minthon L., Hansson O., Björkqvist M., Träskman-Bendz L., Brundin L. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol. Psychiatry. 2009;66:287–292. doi: 10.1016/j.biopsych.2009.01.030. [DOI] [PubMed] [Google Scholar]
- Lindqvist D., Dhabhar F.S., Mellon S.H., Yehuda R., Grenon S.M., Flory J.D., Bierer L.M., Abu-Amara D., Coy M., Makotkine I., et al. Increased pro-inflammatory milieu in combat related PTSD - a new cohort replication study. Brain Behav. Immun. 2017;59:260–264. doi: 10.1016/j.bbi.2016.09.012. [DOI] [PubMed] [Google Scholar]
- Lippi G., Wong J., Henry B.M. Hypertension in patients with coronavirus disease 2019 (COVID-19): a pooled analysis. Pol Arch Intern Med. 2020;130:304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J. Inf. Secur. 2020;80:e14–e18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Xiao X., Wei X., Li J., Yang J., Tan H., Zhu J., Zhang Q., Wu J., Liu L. Composition and divergence of coronavirus spike proteins and host ACE2 receptors predict potential intermediate hosts of SARS-CoV-2. J. Med. Virol. 2020;92:595–601. doi: 10.1002/jmv.25726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Sommerlad A., Orgeta V., Costafreda S.G., Huntley J., Ames D., Ballard C., Banerjee S., Burns A., Cohen-Mansfield J., et al. Dementia prevention, intervention, and care. Lancet. 2017;390:2673–2734. doi: 10.1016/s0140-6736(17)31363-6. [DOI] [PubMed] [Google Scholar]
- Lochhead J.J., Thorne R.G. Intranasal delivery of biologics to the central nervous system. Adv. Drug Deliv. Rev. 2012;64:614–628. doi: 10.1016/j.addr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Lothrop J.C., Newby P.E., Spiess A.E., Bradley J.W. Paleoindians and the younger Dryas in the New England-Maritimes region. Quat. Int. 2011;242:546–569. doi: 10.1016/j.quaint.2011.04.015. [DOI] [Google Scholar]
- Lu, R., Zhao, X., Li, J., Niu, P., Yang, B., Wu, H., Wang, W., Song, H., Huang, B., Zhu, N., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020, 395, 565-574, doi: 10.1016/s0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Luo B. Effects of temperature variation and humidity on the mortality of COVID-19 in Wuhan. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M., De Meyer F., Thompson P., Peeters D., Cosyns P. Synchronized annual rhythms in violent suicide rate, ambient temperature and the light-dark span. Acta Psychiatr. Scand. 1994;90:391–396. doi: 10.1111/j.1600-0447.1994.tb01612.x. [DOI] [PubMed] [Google Scholar]
- Malik Y.S., Sircar S., Bhat S., Sharun K., Dhama K., Dadar M., Tiwari R., Chaicumpa W. Emerging novel coronavirus (2019-nCoV)-current scenario, evolutionary perspective based on genome analysis and recent developments. Veterinary Quart. 2020;40:68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manglani M., McGavern D.B. New advances in CNS immunity against viral infection. Curr Opin Virol. 2018;28:116–126. doi: 10.1016/j.coviro.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marazziti Donatella. Psychological and psychiatric consequences of the COVID-19 pandemic. Commentary on Wiebers & Feigin on Covid Crisis. Animal Sentience. 2020:394–397. [Google Scholar]
- Marazziti D., Stahl S.M. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. 2020;19:261. doi: 10.1002/wps.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marazziti D., Pozza A., Di Giuseppe M., Conversano C. The psychosocial impact of COVID-19 pandemic in Italy: a lesson for mental health prevention in the first severely hit European country. Psychol. Trauma. 2020;12:531–533. doi: 10.1037/tra0000687. [DOI] [PubMed] [Google Scholar]
- Marques T.R., Ashok A.H., Pillinger T., Veronese M., Turkheimer F.E., Dazzan P., Sommer I.E.C., Howes O.D. Neuroinflammation in schizophrenia: meta-analysis of in vivo microglial imaging studies. Psychol. Med. 2019;49:2186–2196. doi: 10.1017/s0033291718003057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall N., Park S., Adger W., Brown K., Howden S. Transformational capacity and the influence of place and identity. Environ. Res. Lett. 2012;7(3) doi: 10.1088/1748-9326/7/3/034022. [DOI] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel Covid-19 disease: a putative disease risk factor. SN Compr Clin Med. 2020:1–5. doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Carrasco M., Evans-Lacko S., Dom G., Christodoulou N., Samochowiec J., González-Fraile E., Bienkowski P., Gomez-Beneyto M., Heitor dos Santos M.J., Wasserman D. EPA guidance on mental health and economic crises in Europe. Eur. Arch. Psychiatry Clin. Neurosci. 2016;266:89–124. doi: 10.1007/s00406-016-0681-x. [DOI] [PubMed] [Google Scholar]
- Mazza M., Di Nicola M., Catalano V., Callea A., Martinotti G., Harnic D., Bruschi A., Battaglia C., Janiri L. Description and validation of a questionnaire for the detection of meteoropathy and meteorosensitivity: the METEO-Q. Compr. Psychiatry. 2012;53:103–106. doi: 10.1016/j.comppsych.2011.02.002. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuinn L.A., Windham G.C., Kalkbrenner A.E., Bradley C., Di Q., Croen L.A., Fallin M.D., Hoffman K., Ladd-Acosta C., Schwartz J., et al. Early life exposure to air pollution and autism spectrum disorder: findings from a multisite case-control study. Epidemiology. 2020;31:103–114. doi: 10.1097/ede.0000000000001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmood K., Saifullah, Abrar M.M., Iqbal M., Haider E., Shoukat H.M.H. Can PM(2.5) pollution worsen the death rate due to COVID-19 in India and Pakistan? Sci. Total Environ. 2020;742:140557. doi: 10.1016/j.scitotenv.2020.140557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M. Temperature andprecipitationassociatewith Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metcalf S.A., Jones P.B., Nordstrom T., Timonen M., Mäki P., Miettunen J., Jääskeläinen E., Järvelin M.R., Stochl J., Murray G.K., et al. Serum C-reactive protein in adolescence and risk of schizophrenia in adulthood: a prospective birth cohort study. Brain Behav. Immun. 2017;59:253–259. doi: 10.1016/j.bbi.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M.R. Oxidative stress and the cardiovascular effects of air pollution. Free Radic. Biol. Med. 2020;151:69–87. doi: 10.1016/j.freeradbiomed.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee A., Agrawal M. World air particulate matter: sources, distribution and health effects. Environ. Chem. Lett. 2017;15:283–309. doi: 10.1007/s10311-017-0611-9. [DOI] [Google Scholar]
- Mukherjee A., Agrawal M. A global perspective of fine particulate matter pollution and its health effects. Rev. Environ. Contam. Toxicol. 2018;244:5–51. doi: 10.1007/398_2017_3. [DOI] [PubMed] [Google Scholar]
- Müller U.C., Pross J.ö., Bibus E. Vegetation response to rapid climate change in central europe during the past 140,000 yr based on evidence from the Füramoos pollen record. Quat. Res. 2003;59:235–245. doi: 10.1016/S0033-5894(03)00005-X. [DOI] [Google Scholar]
- Munkholm K., Braüner J.V., Kessing L.V., Vinberg M. Cytokines in bipolar disorder vs. healthy control subjects: a systematic review and meta-analysis. J. Psychiatr. Res. 2013;47:1119–1133. doi: 10.1016/j.jpsychires.2013.05.018. [DOI] [PubMed] [Google Scholar]
- Murphy T.K., Sajid M.W., Goodman W.K. Immunology of obsessive-compulsive disorder. Psychiatr Clin North Am. 2006;29:445–469. doi: 10.1016/j.psc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Nadjar A., Wigren H.-K.M., Tremblay M.-E. Roles of microglial phagocytosis and inflammatory mediators in the pathophysiology of sleep disorders. Front. Cell. Neurosci. 2017;11:250. doi: 10.3389/fncel.2017.00250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neiderud C.-J. How urbanization affects the epidemiology of emerging infectious diseases. Infect. Ecol. Epidemiol. 2015;5:27060–27,060. doi: 10.3402/iee.v5.27060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nenna R., Evangelisti M., Frassanito A., Scagnolari C., Pierangeli A., Antonelli G., Nicolai A., Arima S., Moretti C., Papoff P., et al. Respiratory syncytial virus bronchiolitis, weather conditions and air pollution in an Italian urban area: an observational study. Environ. Res. 2017;158:188–193. doi: 10.1016/j.envres.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitschke M., Tucker G., Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med. J. Aust. 2007;187:662–665. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- Nogués-Bravo D., Rodríguez-Sánchez F., Orsini L., de Boer E., Jansson R., Morlon H., Fordham D.A., Jackson S.T. Cracking the code of biodiversity responses to past climate change. Trends Ecol. Evol. 2018;33:765–776. doi: 10.1016/j.tree.2018.07.005. [DOI] [PubMed] [Google Scholar]
- Nyerat, F. Biopoltitic des catastrophe. 2008, Dehors (Paris).
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. "Pandemic fear" and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42:232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostfeld R.S. Biodiversity loss and the rise of zoonotic pathogens. Clin. Microbiol. Infect. 2009;15:40–43. doi: 10.1111/j.1469-0691.2008.02691.x. [DOI] [PubMed] [Google Scholar]
- Oudin A., Åström D.O., Asplund P., Steingrimsson S., Szabo Z., Carlsenal H.K. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study. Environ. Health. 2018;17:4. doi: 10.1186/s12940-017-0348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paniz-Mondolfi A., Bryce C., Grimes Z., Gordon R.E., Reidy J., Lednicky J., Sordillo E.M., Fowkes M. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J. Med. Virol. 2020;92:699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons K. Third Edition. CRC Press; Boca Raton: 2002. Human thermal environment. The effects of hot, moderate and cold temperatures on human health, comfort and performance. [DOI] [Google Scholar]
- Pedersen S.F., Ho Y.C. SARS-CoV-2: a storm is raging. J. Clin. Invest. 2020;130:2202–2205. doi: 10.1172/jci137647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel P., Alleaume C., Léger D., Beck F., Verger P. Anxiety, depression and sleep problems: a second wave of COVID-19. Gen. Psychiatr. 2020;33(5) doi: 10.1136/gpsych-2020-100299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman S., Jacobsen G., Afifi A. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology. 1989;170:556–560. doi: 10.1016/0042-6822(89)90446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peros M.C., Gajewski K., Viau A.E. Continental-scale tree population response to rapid climate change, competition and disturbance. Glob. Ecol. Biogeogr. 2008;17:658–669. doi: 10.1111/j.1466-8238.2008.00406.x. [DOI] [Google Scholar]
- Peters R., Ee N., Peters J., Booth A., Mudway I., Anstey K.J. Air pollution and dementia: a systematic review. J. Alzheimers Dis. 2019;70:S145–S163. doi: 10.3233/JAD-180631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin. Microbiol. Infect. 2020;26:729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petterson S.W., John M., Miller Benjamin F. 2020. Projected deaths of despair during the coronavirus recession. [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pinto J.V., Passos I.C., Librenza-Garcia D., Marcon G., Schneider M.A., Conte J.H., da Silva J.P.A., Lima L.P., Quincozes-Santos A., Kauer-Sant Anna M., et al. Neuron-glia interaction as a possible pathophysiological mechanism of bipolar disorder. Curr. Neuropharmacol. 2018;16:519–532. doi: 10.2174/1570159X15666170828170921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole, L. Seasonal Influences On The Spread Of SARS-CoV-2 (COVID19), Causality, and forecastabililty (3-15-2020).
- Power M.C., Kioumourtzoglou M.-A., Hart J.E., Okereke O.I., Laden F., Weisskopf M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: observational cohort study. BMJ. 2015;350 doi: 10.1136/bmj.h1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigogine I., Stengers I. Gallimard; Paris: 1979. La nouvelle alliance: métamorphose de la science. [Google Scholar]
- Pun V.C., Manjourides J., Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the nshap study. Environ. Health Perspect. 2017;125:342–348. doi: 10.1289/ehp494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H., Zhu X., Wang L., Pan J., Pu X., Zeng X., Zhang L., Peng Z., Zhou L. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: a time-series study in Chengdu, China. Environ. Res. 2019;170:230–237. doi: 10.1016/j.envres.2018.12.019. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radua J., Ramella-Cravaro V., Ioannidis J.P.A., Reichenberg A., Phiphopthatsanee N., Amir T., Yenn Thoo H., Oliver D., Davies C., Morgan C., et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. 2018;17:49–66. doi: 10.1002/wps.20490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai P.K. In: Biomagnetic Monitoring of Particulate Matter. Rai P.K., editor. Elsevier; 2016. Chapter One - Particulate Matter and Its Size Fractionation; pp. 1–13. [DOI] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Reifels L., Bassilios B., Spittal M.J., King K., Fletcher J., Pirkis J. Patterns and predictors of primary mental health service use following bushfire and flood disasters. Disaster Med Public Health Prep. 2015;9:275–282. doi: 10.1017/dmp.2015.23. [DOI] [PubMed] [Google Scholar]
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with covid-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A.L., Lyall K., Hart J.E., Laden F., Just A.C., Bobb J.F., Koenen K.C., Ascherio A., Weisskopf M.G. Perinatal air pollutant exposures and autism spectrum disorder in the children of Nurses’ Health Study II participants. Environ. Health Perspect. 2013;121:978–984. doi: 10.1289/ehp.1206187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson C.P., Busl K.M. Neurologic manifestations of severe respiratory viral contagions. Crit Care Explor. 2020;2:e0107. doi: 10.1097/CCE.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha E.M., De Miranda B., Sanders L.H. Alpha-synuclein: pathology, mitochondrial dysfunction and neuroinflammation in Parkinson’s disease. Neurobiol. Dis. 2018;109:249–257. doi: 10.1016/j.nbd.2017.04.004. [DOI] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–627. doi: 10.1016/s2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero-Sánchez C.M., Díaz-Maroto I., Fernández-Díaz E., Sánchez-Larsen Á., Layos-Romero A., García-García J., González E., Redondo-Peñas I., Perona-Moratalla A.B., Del Valle-Pérez J.A., et al. Neurologic manifestations in hospitalized patients with COVID-19: the ALBACOVID registry. Neurology. 2020;95(8):e1060–e1070. doi: 10.1212/wnl.0000000000009937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R., Socci, V., Pacitti, F., Di Lorenzo, G., Di Marco, A., Siracusano, A., Rossi, A. Mental health outcomes among frontline and second-line health careworkers during the coronavirus disease 2019 (covid-19) pandemic in Italy. JAMA Netw. Open 2020a, 3, e2010185, doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed]
- Rossi, R., Socci, V., Talevi, D., Niolu, C., Pacitti, F., Marco, A., Rossi, A., Siracusano, A., Di Lorenzo, G., Olff, M. Trauma-spectrum symptoms among the Italian general population in the time of the COVID-19 outbreak. 2020b, 10.1101/2020.06.01.20118935. [DOI] [PMC free article] [PubMed]
- Ruiz M.O., Chaves L.F., Hamer G.L., Sun T., Brown W.M., Walker E.D., Haramis L., Goldberg T.L., Kitron U.D. Local impact of temperature and precipitation on West Nile virus infection in Culex species mosquitoes in northeast Illinois, USA. Parasit. Vectors. 2010;3:19. doi: 10.1186/1756-3305-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan P.M. Caplice, N.M. Is adipose tissue a reservoir for viral spread, immune activation, and cytokine amplification in coronavirus disease 2019? Obesity (Silver Spring) 2020;28:1191–1194. doi: 10.1002/oby.22843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez M., Barceló M.A., Farrerons M., López-Casasnovas G. The association between exposure to environmental factors and the occurrence of attention-deficit/hyperactivity disorder (ADHD). A population-based retrospective cohort study. Environ. Res. 2018;166:205–214. doi: 10.1016/j.envres.2018.05.009. [DOI] [PubMed] [Google Scholar]
- Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature, Humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw. Open. 2020;3:e2011834. doi: 10.1001/jamanetworkopen.2020.11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salata C., Calistri A., Parolin C., Palù G. Coronaviruses: a paradigmof newemerging zoonotic diseases. Pathog. Dis. 2019;77(9) doi: 10.1093/femspd/ftaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salcioglu E., Basoglu M., Livanou M. Post-traumatic stress disorder and comorbid depression among survivors of the 1999 earthquake in Turkey. Disasters. 2007;31:115–129. doi: 10.1111/j.1467-7717.2007.01000.x. [DOI] [PubMed] [Google Scholar]
- Sands, P.J.R.E.C, L., I.l.E . Vol. 1. 1992. The United Nations framework convention on climate change; p. 270. [Google Scholar]
- Sankowski R., Mader S., Valdés-Ferrer S.I. Systemic inflammation and the brain: novel roles of genetic, molecular, and environmental cues as drivers of neurodegeneration. Front. Cell. Neurosci. 2015;9:28. doi: 10.3389/fncel.2015.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M., Marufi N., Kazemi Moghaddam V. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ. Res. 2020;188:109748–109,748. doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasayama D., Hattori K., Wakabayashi C., Teraishi T., Hori H., Ota M., Yoshida S., Arima K., Higuchi T., Amano N., et al. Increased cerebrospinal fluid interleukin-6 levels in patients with schizophrenia and those with major depressive disorder. J. Psychiatr. Res. 2013;47:401–406. doi: 10.1016/j.jpsychires.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Sass V., Kravitz-Wirtz N., Karceski S.M., Hajat A., Crowder K., Takeuchi D. The effects of air pollution on individual psychological distress. Health Place. 2017;48:72–79. doi: 10.1016/j.healthplace.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayana P., Colpo G.D., Simões L.R., Giridharan V.V., Teixeira A.L., Quevedo J., Barichello T. A systematic review of evidence for the role of inflammatory biomarkers in bipolar patients. J. Psychiatr. Res. 2017;92:160–182. doi: 10.1016/j.jpsychires.2017.03.018. [DOI] [PubMed] [Google Scholar]
- Schelling G., Kilger E., Roozendaal B., de Quervain D.J., Briegel J., Dagge A., Rothenhäusler H.B., Krauseneck T., Nollert G., Kapfhammer H.P. Stress doses of hydrocortisone, traumatic memories, and symptoms of posttraumatic stress disorder in patients after cardiac surgery: a randomized study. Biol. Psychiatry. 2004;55:627–633. doi: 10.1016/j.biopsych.2003.09.014. [DOI] [PubMed] [Google Scholar]
- Schwartz M., Deczkowska A. Neurological disease as a failure of brain-immune crosstalk: the multiple faces of neuroinflammation. Trends Immunol. 2016;37:668–679. doi: 10.1016/j.it.2016.08.001. [DOI] [PubMed] [Google Scholar]
- Schwerdtle P., Bowen K., McMichael C. The health impacts of climate-related migration. BMC Med. 2017;16:1. doi: 10.1186/s12916-017-0981-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., de Gennaro G., Barbieri P., Licen S., Perrone M., Piazzalunga A., Borelli M., Palmisani J., Gilio A., et al. Potential role of particulate matter in the spreading of COVID-19 in northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti, L., Passarini, F., De Gennaro, G., Baribieri, P., Perrone, M.G., Borelli, M., Palmisani, J., Di Gilio, A., Torboli, V., Pallavicini, A., et al. SARS-Cov-2 RNA found on particulate matter of Bergamo in northern Italy: first preliminary evidence. Environ. Res. 2020b, 188: 109754, doi 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed]
- Shah K., Kamrai D., Mekala H., Mann B., Desai K., Patel R.S. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12:e7405. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehab M., Pope F. Effects of short-term exposure to particulate matter on cognitive performance. Sci. Rep. 2019;9:8237. doi: 10.1038/s41598-019-44561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M., McBride O., Murphy J., Miller J.G., Hartman T.K., Levita L., Mason L., Martinez A.P., McKay R., Stocks T.V.A., et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6:e125. doi: 10.1192/bjo.2020.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, P., Dong, Y., Yan, H., Li, X., Zhao, C., Liu, W., He, M., Tang, S., Xi, S. The impact of temperature and absolute humidity on the coronavirus disease 2019 (COVID-19) outbreak - evidence from China. 2020, 10.1101/2020.03.22.20038919%J medRxiv, 2020.2003.2022.20038919, doi: 10.1101/2020.03.22.20038919%J medRxiv.
- Shi P., Dong Y., Yan H., Li X., Zhao C., Liu W., He M., Tang S., Xi S. The impact of temperature and absolute humidity on the coronavirus disease 2019 (COVID-19) outbreak - evidence from China. medRxiv: the preprint server for health sciences. 2020 doi: 10.1101/2020.03.22.20038919. [DOI] [Google Scholar]
- Shin J., Park J.Y., Choi J. Long-term exposure to ambient air pollutants andmental health status: a nationwide population-based cross-sectional study. PLoS One. 2018;13(4) doi: 10.1371/journal.pone.0195607. e0195607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui S., Jakaria M. Lockdown leading obesity and its possible impacts on the second wave of COVID-19. Bangladesh J. Med. Sci. 2020 doi: 10.3329/bjms.v19i0.48172. [DOI] [Google Scholar]
- Singh S.K., Rao D.N., Agrawal M., Pandey J., Naryan D. Air pollution tolerance index of plants. J. Environ. Manag. 1991;32:45–55. doi: 10.1016/S0301-4797(05)80080-5. [DOI] [Google Scholar]
- Sisó S., Jeffrey M., González L. Sensory circumventricular organs in health and disease. Acta Neuropathol. 2010;120:689–705. doi: 10.1007/s00401-010-0743-5. [DOI] [PubMed] [Google Scholar]
- Sobral M., Duarte G., Sobral A., Marinho M.L., Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J., Zheng L., Lu M., Gui L., Xu D., Wu W., Liu Y. Acute effects of ambient particulate matter pollution on hospital admissions for mental and behavioral disorders: a time-series study in Shijiazhuang, China. Sci. Total Environ. 2018;636:205–211. doi: 10.1016/j.scitotenv.2018.04.187. [DOI] [PubMed] [Google Scholar]
- Spitzer C., Barnow S., Völzke H., Wallaschofski H., John U., Freyberger H.J., Löwe B., Grabe H.J. Association of posttraumatic stress disorder with low-grade elevation of C-reactive protein: evidence from the general population. J. Psychiatr. Res. 2010;44:15–21. doi: 10.1016/j.jpsychires.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Stanek L.W., Brown J.S., Stanek J., Gift J., Costa D.L. Air pollution toxicology - a brief review of the role of the science in shaping the current understanding of air pollution health risks. Toxicol. Sci. 2011;120(Suppl 1):S8–S27. doi: 10.1093/toxsci/kfq367. [DOI] [PubMed] [Google Scholar]
- Steardo L., Steardo L., Jr., Zorec R., Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol (Oxford) 2020;229 doi: 10.1111/apha.13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steardo L., Jr., Steardo L., Verkhratsky A. Psychiatric face of COVID-19. Transl. Psychiatry. 2020;10:261. doi: 10.1038/s41398-020-00949-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen W., Richardson K., Rockström J., Cornell S.E., Fetzer I., Bennett E.M., Biggs R., Carpenter S.R., de Vries W., de Wit C.A., et al. Planetary boundaries: guiding human development on a changing planet. Science. 2015;347:6223. doi: 10.1126/science.1259855. [DOI] [PubMed] [Google Scholar]
- Stewart J.A., Mitchell M.A., Edgerton V.S., VanCott R. Environmental justice and health effects of urban air pollution. J. Natl. Med. Assoc. 2015;107:50–58. doi: 10.1016/s0027-9684(15)30009-2. [DOI] [PubMed] [Google Scholar]
- Strahilevitz M., Strahilevitz A., Miller J.E. Air pollutants and the admission rate of psychiatric patients. Am. J. Psychiatry. 1979;136:205–207. doi: 10.1176/ajp.136.2.205. [DOI] [PubMed] [Google Scholar]
- Sun Y., Li Y., Bao Y., Meng S., Sun Y., Schumann G., Kosten T., Strang J., Lu L., Shi J. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am. J. Addict. 2020;29:268–270. doi: 10.1111/ajad.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyszkowicz M. Air pollution and emergency department visits for depression in Edmonton, Canada. Int. J. Occup. Med. Environ. Health. 2007;20:241–245. doi: 10.2478/v10001-007-0024-2. [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M. Ambient sulfur dioxide and female ED visits for depression. Air Qual. Atmos. Health. 2010;4:259–262. doi: 10.1007/s11869-010-0081-8. [DOI] [Google Scholar]
- Szyszkowicz M., Rowe B.H., Colman I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. Health. 2009;22:355–362. doi: 10.2478/v10001-009-0031-6. [DOI] [PubMed] [Google Scholar]
- Szyszkowicz M., Willey J.B., Grafstein E., Rowe B.H., Colman I. Air pollution and emergency department visits for suicide attempts in Vancouver, Canada. Environ Health Insights. 2010;4:79–86. doi: 10.4137/ehi.S5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyszkowicz M., Kousha T., Kingsbury M., Colman I. Air pollution and emergency department visits for depression: a multicity case-crossover study. Environ Health Insights. 2016;10:155–161. doi: 10.4137/ehi.S40493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyszkowicz M., Thomson E.M., Colman I., Rowe B.H. Ambient air pollution exposure and emergency department visits for substance abuse. PLoS One. 2018;13 doi: 10.1371/journal.pone.0199826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takagi S., Furube E., Nakano Y., Morita M., Miyata S. Microglia are continuously activated in the circumventricular organs of mouse brain. J. Neuroimmunol. 2019;331:74–86. doi: 10.1016/j.jneuroim.2017.10.008. [DOI] [PubMed] [Google Scholar]
- Talbott E.O., Arena V.C., Rager J.R., Clougherty J.E., Michanowicz D.R., Sharma R.K., Stacy S.L. Fine particulate matter and the risk of autism spectrum disorder. Environ. Res. 2015;140:414–420. doi: 10.1016/j.envres.2015.04.021. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., Zhang K., Chin H.K., Ahmad A., Khan F.A., et al. Psychological impact of the covid-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020;173:317–320. doi: 10.7326/m20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Dis. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapia Granados J.A., Diez Roux A.V. Life and death during the great depression. Proc. Natl. Acad. Sci. U. S. A. 2009;106:17290–17295. doi: 10.1073/pnas.0904491106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavella R., Da Silva Júnior F. COVID-19 and air pollution: what do we know so far? VITTALLE - Revista de Ciências da Saúde. 2020;32:22–31. doi: 10.14295/vittalle.v32i1.11522. [DOI] [Google Scholar]
- Taylor M.R., Agho K.E., Stevens G.J., Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia's first outbreak of equine influenza. BMC Public Health. 2008;8:347. doi: 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C.T., Doherty G., Fallon P.G., Cummins E.P. Hypoxia-dependent regulation of inflammatory pathways in immune cells. J. Clin. Invest. 2016;126:3716–3724. doi: 10.1172/jci84433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thome J., Coogan A.N., Simon F., Fischer M., Tucha O., Faltraco F., Marazziti D., Butzer H. The impact of the COVID-19 outbreak on the medico-legal and human rights of psychiatric patients. Eur Psychiatry. 2020;63:e50. doi: 10.1192/j.eurpsy.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288:112992. doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinner W., Kaltenrieder P. Rapid responses of high-mountain vegetation to early Holocene environmental changes in the Swiss Alps. J. Ecol. 2005;93:936–947. doi: 10.1111/j.1365-2745.2005.01023.x. [DOI] [Google Scholar]
- Torales J., O'Higgins M., Rios-González C.M., Barrios I., García-Franco O., Castaldelli-Maia J.M., Ventriglio A. 2020. Considerations on the mental health impact of the novel coronavirus outbreak (COVID-19) [DOI] [Google Scholar]
- Torres J.M., Casey J.A. The centrality of social ties to climate migration and mental health. BMC Public Health. 2017;17:600. doi: 10.1186/s12889-017-4508-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tursich M., Neufeld R.W., Frewen P.A., Harricharan S., Kibler J.L., Rhind S.G., Lanius R.A. Association of trauma exposure with proinflammatory activity: a transdiagnostic meta-analysis. Transl. Psychiatry. 2014;4 doi: 10.1038/tp.2014.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S Global Change, R.P . Global Change Research Program; Washington: U.S.: 2016. The impacts of climate change on human health in the United States: a scientific assessment; p. 25. [Google Scholar]
- Ursano R.J., Morganstein J.C., Cooper R. Resource document on mental health and climate change. APA Resource Document. 2017:1–4. [Google Scholar]
- Vandini S., Corvaglia L., Alessandroni R., Aquilano G., Marsico C., Spinelli M., Lanari M., Faldella G. Respiratory syncytial virus infection in infants and correlation with meteorological factors and air pollutants. Ital. J. Pediatr. 2013;39:1. doi: 10.1186/1824-7288-39-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandoros S., Avendano M., Kawachi I. The association between economic uncertainty and suicide in the short-run. Social Sci. Med. 2018;220 doi: 10.1016/j.socscimed.2018.11.035. [DOI] [PubMed] [Google Scholar]
- Varatharaj A., Thomas N., Ellul M.A., Davies N.W.S., Pollak T.A., Tenorio E.L., Sultan M., Easton A., Breen G., Zandi M., et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7:875–882. doi: 10.1016/s2215-0366(20)30287-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkhratsky A., Zorec R., Parpura V. Stratification of astrocytes in healthy and diseased brain. Brain Pathol. (Zurich, Switzerland) 2017;27:629–644. doi: 10.1111/bpa.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vert C., Sánchez-Benavides G., Martínez D., Gotsens X., Gramunt N., Cirach M., Molinuevo J.L., Sunyer J., Nieuwenhuijsen M.J., Crous-Bou M., et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: a cross-sectional study. Int. J. Hyg. Environ. Health. 2017;220:1074–1080. doi: 10.1016/j.ijheh.2017.06.009. [DOI] [PubMed] [Google Scholar]
- Volk H.E., Hertz-Picciotto I., Delwiche L., Lurmann F., McConnell R. Residential proximity to freeways and autism in the CHARGE study. Environ. Health Perspect. 2011;119:873–877. doi: 10.1289/ehp.1002835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volk H.E., Lurmann F., Penfold B., Hertz-Picciotto I., McConnell R. Traffic-related air pollution, particulate matter, and autism. JAMA Psychiatry. 2013;70:71–77. doi: 10.1001/jamapsychiatry.2013.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang A.K., Miller B.J. Meta-analysis of cerebrospinal fluid cytokine and tryptophan catabolite alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder, and depression. Schizophr. Bull. 2018;44:75–83. doi: 10.1093/schbul/sbx035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Minnis R.B., Belant J.L., Wax C.L. Dry weather induces outbreaks of human West Nile virus infections. BMC Infect. Dis. 2010;10:38. doi: 10.1186/1471-2334-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Eliot M.N., Koutrakis P., Gryparis A., Schwartz J.D., Coull B.A., Mittleman M.A., Milberg W.P., Lipsitz L.A., Wellenius G.A. Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. Environ. Health Perspect. 2014;122:553–558. doi: 10.1289/ehp.1205909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Liu H., Li H., Liu J., Guo X., Yuan J., Hu Y., Wang J., Lu L. Ambient concentrations of particulate matter and hospitalization for depression in 26 Chinese cities: a case-crossover study. Environ. Int. 2018;114:115–122. doi: 10.1016/j.envint.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Wang, J., Tang, K., Feng, K., Lv,W. High temperature and high humidity reduce the transmission of COVID-19. SSRN Electron. J. 2020a, 10.2139/ssrn.3551767. [DOI]
- Wang B., Chen H., Chan Y.L., Oliver B.G. Is there an association between the level of ambient air pollution and COVID-19? Am J Physiol Lung Cell Mol Physiol. 2020;319(3):L416–L421. doi: 10.1152/ajplung.00244.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassenaar T.M., Zou Y. 2019_nCoV/SARS-CoV-2: rapid classification of betacoronaviruses and identification of traditional chinese medicine as potential origin of zoonotic coronaviruses. Lett. Appl. Microbiol. 2020;70:342–348. doi: 10.1111/lam.13285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei W., Lu J.G., Galinsky A.D., Wu H., Gosling S.D., Rentfrow P.J., Yuan W., Zhang Q., Guo Y., Zhang M., et al. Regional ambient temperature is associated with human personality. Nat. Hum. Behav. 2017;1:890–895. doi: 10.1038/s41562-017-0240-0. [DOI] [PubMed] [Google Scholar]
- Wiebers D., Feigin V. What the COVID-19 pandemic is telling humanity. Animal Sentience. 2020;30:1. doi: 10.1159/000508654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilker E.H., Preis S.R., Beiser A.S., Wolf P.A., Au R., Kloog I., Li W., Schwartz J., Koutrakis P., DeCarli C., et al. Long-term exposure to fine particulate matter, residential proximity to major roads and measures of brain structure. Stroke. 2015;46:1161–1166. doi: 10.1161/STROKEAHA.114.008348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodbury Z. Climate trauma: towards a new taxonomy of trauma. Ecopsychology. 2019;11(1):1–8. doi: 10.1089/eco.2018.0021. [DOI] [Google Scholar]
- World Health O. Geneva: World Health Organization; 2020. Coronavirus disease 2019 (COVID-19): situation report, 73. 2020-04-02.
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. 2020. Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. (medRxiv: the preprint server for health sciences). [DOI] [Google Scholar]
- Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia H., Lazartigues E. Angiotensin-converting enzyme 2: central regulator for cardiovascular function. Curr. Hypertens. Rep. 2010;12:170–175. doi: 10.1007/s11906-010-0105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.-T., Jin Y., Cheung T. Joint international collaboration to combat mental health challenges during the coronavirus disease 2019 pandemic. JAMA Psychiatry. 2020;77:989–990. doi: 10.1001/jamapsychiatry.2020.1057. [DOI] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities fromChina. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie Z., Qin Y., Li Y., Shen W., Zheng Z., Liu S. Spatial and temporal differentiation of COVID-19 epidemic spread in mainland China and its influencing factors. Sci. Total Environ. 2020;744:140929. doi: 10.1016/j.scitotenv.2020.140929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yackerson N.S., Zilberman A., Todder D., Kaplan Z. The influence of air-suspended particulate concentration on the incidence of suicide attempts and exacerbation of schizophrenia. Int. J. Biometeorol. 2014;58:61–67. doi: 10.1007/s00484-012-0624-9. [DOI] [PubMed] [Google Scholar]
- Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H. The more exposure to media information about COVID-19, the more distressed you will feel. Brain Behav. Immun. 2020;87:167–169. doi: 10.1016/j.bbi.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan, China. Environ. Res. 2020;189 doi: 10.1016/j.envres.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/s2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasuhara M., Cronin T.M., deMenocal P.B., Okahashi H., Linsley B.K. Abrupt climate change and collapse of deep-sea ecosystems. Proc. Natl. Acad. Sci. 2008;105(5):1556–1560. doi: 10.1073/pnas.0705486105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip P.S., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010;31:86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
- Yousefian F., Mahvi A.H., Yunesian M., Hassanvand M.S., Kashani H., Amini H. Long-term exposure to ambient air pollution and autism spectrum disorder in children: a case-control study in Tehran, Iran. Sci. Total Environ. 2018;643:1216–1222. doi: 10.1016/j.scitotenv.2018.06.259. [DOI] [PubMed] [Google Scholar]
- Zarocostas J. How to fight an infodemic. Lancet. 2020;395:676. doi: 10.1016/s0140-6736(20)30461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P., Zhou X. Health and economic impacts of particulate matter pollution on hospital admissions for mental disorders in Chengdu, southwestern China. Sci. Total Environ. 2020;733 doi: 10.1016/j.scitotenv.2020.139114. [DOI] [PubMed] [Google Scholar]
- Zhou J., Liu L., Xue P., Yang X., Tang X. Mental health response to the covid-19 outbreak in China. Am. J. Psychiatry. 2020;177:574–575. doi: 10.1176/appi.ajp.2020.20030304. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Chen L., Ji H., Xi M., Fang Y., Li Y. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 2020;36:299–302. doi: 10.1007/s12264-020-00476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijlema W.L., Wolf K., Emeny R., Ladwig K.H., Peters A., Kongsgård H., Hveem K., Kvaløy K., Yli-Tuomi T., Partonen T., et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. Int. J. Hyg. Environ. Health. 2016;219:212–219. doi: 10.1016/j.ijheh.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Zikic, M., Žikić, T. Meteoropathy and Meteorosensitive Persons. Medicinski pregled 2018, LXXI, doi: 10.2298/MPNS1804131Z. [DOI]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738 doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]