Abstract
Background
COVID-19, the syndrome caused by the novel SARS-CoV2, is associated with high rates of acute kidney injury requiring renal replacement therapy (RRT). It is well known that despite the ease of bedside insertion, the use of nontunneled dialysis catheters (NTDCs) is associated with increased complications compared to tunneled dialysis catheters (TDCs). Our objective was to develop a strategy for TDC placement at the bedside to provide effective dialysis access, conserve resources and decrease personnel exposure at our medical center in an epicenter of the COVID-19 pandemic.
Methods
A technique for bedside TDC insertion with ultrasound and plain radiographs in the intensive care unit was developed. Test or clinically COVID-19-positive patients requiring RRT were evaluated for bedside emergent NTDC or nonemergent TDC placement. Patients who underwent NTDC placement were monitored for ongoing RRT needs and were converted to TDC at the bedside after 3–5 days. We prospectively collected patient data focusing on complications and mortality.
Results
Of the 36 consultations for dialysis access in COVID-positive patients from March 19 through June 5, 2020, a total of 24 bedside TDCs were placed. Only one patient developed a complication, which was pneumothorax and cardiac tamponade during line placement. In-hospital mortality in the cohort was 63.9%.
Conclusions
Bedside TDC placement has served to conserve resources, prevent complications with transport to and from the operating room, and decrease personnel exposure during the COVID-19 pandemic. This strategy warrants further consideration and could be used in critically ill patients regardless of COVID status.
INTRODUCTION
In late 2019, the rapid spread of a severe respiratory illness was first noted in Wuhan City, Hubei Province, China.1 A novel coronavirus, now known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), was identified as the pathogen, and the World Health Organization (WHO) termed the illness it caused COVID-19 (coronavirus disease 2019).2 The first confirmed case of COVID-19 in the United States was in January 2020,3 and by March 2020 the continued rapid spread of the virus was categorized as a pandemic.1
As the number of patients with COVID-19 increased, it became evident that there were systemic effects of the virus beyond the respiratory syndrome that was initially described. The association of severe COVID-19 with depressed renal function was first noted in small patient cohorts in China and verified in subsequent international series with acute kidney injury (AKI) documented in 5.1–40% of patients with COVID-19.4., 5., 6., 7., 8., 9., 10., 11. Pei et al. closely examined the serum and urine of patients with COVID-19 and found that that 75.4% had some form of new renal abnormalities.9 Pre-renal causes from COVID-19-associated sepsis and septic shock likely contribute to this observed kidney injury, but intrinsic renal disease due to direct viral destruction of tubular cells and the bystander effect of the virus-induced inflammatory response by macrophages and complement deposition are major factors causing renal failure.5 , 12 , 13 Additionally, patients with COVID-19 were shown to have a higher than predicted risk of thrombosis, which had an impact on the patency of dialysis catheters and circuits.14 , 15 Due to the sheer number of COVID-19-positive patients in hospitals worldwide, and the associated demand for renal replacement therapy (RRT), an interest in developing systems to meet this need grew.16., 17., 18.
As the COVID-19 pandemic grew, hospitals and health systems nationwide began canceling nonemergent surgery in order to conserve healthcare resources and decrease exposures. A variety of professional organizations, including the American College of Surgeons (ACS) and the Society for Vascular Surgery (SVS) issued guidelines related to which surgeries should be performed and how to best protect healthcare personnel and resources.19., 20., 21. Renal failure with the need for dialysis access was categorized as a Tier 3 procedure (“Do not postpone”) by the SVS, though recommendations for minimizing the number of staff involved in order to conserve personal protective equipment and reduce exposure remained an important consideration.20., 21., 22.
Given ongoing interest in proceeding directly to tunneled dialysis catheters (TDC) for patients with acute kidney injury (AKI) requiring RRT, including the currently-accruing randomized-controlled BACKDOOR trial (NCT03496935),23 , 24 we developed a strategy and technique for inserting tunneled dialysis catheters at the bedside for COVID-19 positive patients in the intensive care unit (ICU) requiring RRT. The goals of this strategy were to establish well-functioning dialysis access, limit resource utilization, and personnel exposure to the virus, and to avoid moving critically ill (and sometimes tenuous) patients out of the ICU or even off the ICU bed onto a fluoroscopy-compatible table. Here we describe our technique and the short-term outcomes of our case series at a tertiary community-based medical center located in a SARS-CoV2 epicenter.
METHODS
Setting, Patient Population and Data Collection
Our institution is a 331-bed tertiary care teaching hospital located in suburban Philadelphia, PA. Pennsylvania, the fifth largest state, recorded the seventh largest number of SARS-CoV2 infections in the nation, the seventeenth largest in terms of per capita cases, and the tenth largest number in per capita deaths attributed to COVID-19 during the first wave of infection from March through June, 2020.25 Philadelphia and its surrounding counties were the epicenter of COVID-19 in Pennsylvania. At our institution, vascular surgery historically performs nearly all nontunneled (bedside) and tunneled (operating room) dialysis catheter insertions.
After Institutional Review Board (IRB) approval, we developed a prospective database of all COVID-19 clinically or confirmed positive patients for whom the vascular surgery service was consulted for new hemodialysis access. Informed consent was waived by the IRB. Data collection began March 19, 2020, immediately after the first COVID-19 case was confirmed and continued through June 5, 2020. The clinical data collected included demographics, pre-hospital renal function, COVID-19 testing, type and location of hemodialysis catheter placement, hemodialysis modality and complications, whether hemodialysis was needed at the time of hospital discharge, and in-hospital mortality
Bedside Hemodialysis Catheter Placement
At the time of consultation for dialysis access cases were reviewed individually with the nephrology and medical ICU teams to determine how emergently RRT was needed. If the patient required emergent dialysis, a femoral or internal jugular nontunneled dialysis catheter (NTDC) was placed; if the clinical situation allowed, arrangements were made for the placement of a TDC at the bedside. If ongoing RRT needs were noted after 3–5 days in patients with NTDC, arrangements were made to convert to a TDC at the bedside.
Once a patient is identified for whom a bedside TDC is appropriate, the vascular surgery team notifies the operating room, and a cart with required instruments and multiple sizes of TDCs is prepared. Standard catheter lengths are used in each case dependent upon anatomic location: right internal jugular vein – 19 cm; left internal jugular vein – 23cm; femoral vein – 33cm. The procedure is performed at the bedside by the attending vascular surgeon (Fig. 1 A) assisted by one OR nurse, a radiologic technologist, and the patient's ICU nurse. A second operating room nurse remains outside the room to retrieve any supplies that are necessary throughout the procedure. Sedation is managed by the surgeon and the patient's ICU nurse throughout the procedure. All individuals in the patient's room wear lead aprons for the duration of the procedure.
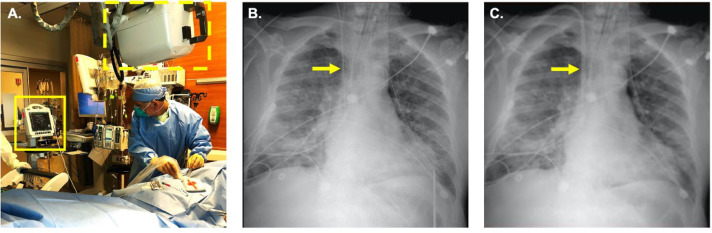
Fig. 1.
Bedside tunneled hemodialysis catheter placement. The surgeon cannulates the internal jugular vein under ultrasound guidance (A, solid box) and confirms placement of the wire (B, arrow) and catheter (C, arrow) in the superior vena cava using plain portable radiographs (A, dotted line).
The patient is left supine in their ICU bed and a flat, wireless radiograph panel is placed under the patient's chest with the radiograph machine positioned above the patient (Fig. 1A) and its monitor positioned for instantaneous view of digital imaging. With the patient supine and in the Trendelenburg position, an ultrasound is used to evaluate the patency of the internal jugular veins. After sterile prep and draping, the Seldinger technique is used to access the internal jugular vein with an .018” wire, which is verified to be in the superior vena cava (SVC) on real-time chest radiograph (Fig. 1B). The .018” wire is converted to a .035” guidewire, the position of which is again confirmed with a radiograph. After infiltration with local anesthesia, a subcutaneous tunnel is developed from the guidewire to the lateral chest, through which the catheter is placed. After dilation of the subcutaneous tissue, a peel-away sheath is advanced over the wire with constant back-and-forth movement of the wire to ensure there is no kinking. A radiograph is occasionally used at this point to verify position of the sheath and is always used if any resistance to advancing the sheath is encountered. The catheter is then advanced through the sheath into the SVC, the position of which is confirmed with a radiograph (Fig. 1C). Flow through each of the catheter ports is verified and a sterile dressing is placed.
Notably, for the first 6 patients for whom bedside TDCs were placed, portable fluoroscopic guidance was used for real-time guidance after the patient was moved from their ICU bed to a fluoroscopy-compatible bed within their ICU room. All subsequent bedside procedures were performed using portable plain radiograph as described above.
RESULTS
From March 1 through June 5, 2020, our institution treated 252 inpatients who were test-positive for SARS-CoV2, 144 (40.9%) of whom required care in the intensive care unit. During this time, our vascular surgery service received 36 consults for HD access in patients who were test- or clinically COVID-19 positive and had not previously required HD. We also were consulted for access in one patient on chronic HD through a left upper extremity arteriovenous fistula who required continuous renal replacement therapy (CRRT), so a temporary catheter was needed.
Characteristics of the 36 patients for whom HD access was needed are summarized in Table I ; the mean age was 65.5 years, the majority were male (80.6%), Black (77.8%), and had a positive COVID-19 test (80.6%). Baseline renal function was available for 28 patients, 16 (57.1%) of whom had a pre-hospital estimated glomerular filtration rate (eGFR) of 60 mL/min/1.73m2 or greater, and one of whom was already on chronic HD.
Table I.
Clinical characteristics and hemodialysis catheter placement in test- or clinically-positive COVID-19 patients
| n | 36 | ||
| Age (years) | 65.5 ± 10.5 | ||
| Sex | |||
| Male | 29 (80.6) | ||
| Female | 7 (19.4) | ||
| Race | |||
| White | 7 (19.4) | ||
| Black | 28 (77.8) | ||
| Other | 1 (2.8) | ||
| COVID-19 status | |||
| Test positive | 29 (80.6) | ||
| Clinically positive | 7 (19.4) | ||
| Baseline eGFR (mL/min/1.73m2) | |||
| >60 | 16 (44.4) | ||
| 30–59 | 6 (16.7) | ||
| 15–29 | 4 (11.1) | ||
| <15 | 2 (5.6) | ||
| Unknown | 8 (22.2) | ||
| Patient location | |||
| Medical floor | 2 (5.6) | ||
| Intensive care unit | 34 (94.4) | ||
| Hemodialysis access | |||
| First catheter placement | 36 (100.0) | ||
| Bedside, nontunneled | 19 (52.8) | ||
| Bedside, tunneled | 15 (41.7) | ||
| Operating room, tunneled | 2 (5.6) | ||
| Second catheter placement | 10 (27.8) | ||
| Bedside, tunneled | 9 (90.0) | ||
| Operating room, tunneled | 1 (10.0) | ||
| In-hospital mortality | 23 (63.9) | ||
All values are no. (%) or mean ± standard deviation.
Nineteen patients (52.8%) required emergent HD at the time of consultation, so bedside NTDCs were placed. Two patients were not in the intensive care unit and did not require emergent HD so were taken to the OR for TDC placement. Fifteen patients (41.7%) underwent TDC placement at the bedside as their first HD access and an additional 9 patients had their initial HD access replaced with a TDC at the bedside. Thus, in total, 24 TDCs were placed at the bedside in this series. As above, the first 4 in this series were performed under fluoroscopic guidance while the subsequent 20 were performed with plain radiographs. The median number of plain radiographs taken during insertion was 5 ranging from 1 radiograph (NTDC was converted to TDC over a wire) to 9 radiographs.
One patient with a NTDC required replacement with another NTDC prior to TCD insertion due to clotting. There were no catheter-associated infections observed. Complications were rare in bedside TDC placement. One patient developed pericardial tamponade and pneumothorax during bedside TDC placement requiring emergent pericardial drain and tube thoracostomy insertion. TDC placement was aborted, and the patient was ultimately transitioned to comfort measures. Another patient required removal of the TDC due to positive blood cultures that had been drawn on admission but did not become positive until after bedside placement. After repeat blood cultures were negative, a second bedside TDC was placed.
In-hospital mortality was 63.9% in this cohort. Of the remaining 13 patients, 1 patient was still inpatient at the time this manuscript was submitted and 5 patients had been discharged and no longer required HD. Their TDCs were removed either at the bedside prior to discharge or in follow-up in the vascular surgery office.
DISCUSSION
Here we describe a series of 36 patients with test- or clinically-positive COVID-19 requiring RRT and the use of a system in response to the pandemic for the insertion of 24 TDCs at the bedside under ultrasound and fluoroscopic or plain radiographic guidance.
Our patient series demonstrates that the AKI associated with COVID-19 does not only impact those with pre-infection chronic kidney disease, but also those with normal renal function. Almost half of the patients in this series requiring RRT had a pre-hospital eGFR >60, which signifies normal renal function. Our series also corroborates prior studies that have shown higher rates of mortality among COVID-19 positive patients with AKI. The Centers for Disease Control and Prevention cite mortality related to COVID-19 between <1–27% and a direct relationship with age.26 In line with previous reports,6 , 8 the in-hospital mortality in this series was 63.9%.
The use of NTDCs versus TDCs has been an area of ongoing investigation. It is well known that despite the benefit of being able to place at the bedside without fluoroscopy and initiate dialysis emergently, the use of NTDCs is associated with increased complications such as infection and reduced flow when compared to TDCs.23 , 27., 28., 29., 30. Patients who require initiation of RRT in the ICU are also likely to remain on dialysis for an extended period of time, and ultimately require conversion of NTDC to TDC,23 , 31 , 32 therefore proceeding straight to a TDC has become an attractive strategy.
The COVID-19 pandemic provides significant challenges as the number of patients requiring emergent RRT increased, and the conservation of resources became essential. In our approach, we were able to accomplish the goal of establishing well-functioning dialysis access in patients with COVID-19. Performing insertion at the bedside allowed us to limit the staff required for the procedure in that no transport to the operating room was required, and the management of sedation by the procedure team negated the need for an anesthesia team. We also limited personnel exposure to patients with COVID-19 by, when possible, performing a single stage TDC insertion without the need for conversion of NTDC to TDC. Our initial approach using real-time fluoroscopy at the bedside was abandoned in favor of using portable radiography due to the bulky equipment, and the requirement for moving critically ill patients to fluoroscopy-compatible beds. Not moving patients to the operating room or off their ICU beds also eliminated the need for disconnections from the closed-circuit ventilator, further decreasing staff exposure to SARS-CoV2. The bedside strategy also served to save time that would normally be spent in transport to and from the operating room, as well as provide flexibility for procedure scheduling due to staff and operating room availability.
Importantly, the rate of complication was very low. There were no infectious or thrombotic complications with TDCs, and we only observed one patient who required NTDC replacement due to thrombosis. Only one patient suffered procedural complications, which likely resulted from vascular trauma during insertion of the tear-away sheath over the .035” wire without live fluoroscopic guidance; this is one of the pitfalls of performing TDC insertion without fluoroscopy. Our technique was reviewed and altered to use constant motion of the wire during sheath insertion, and additional radiographs if any resistance was met during the insertion of the tear-away sheath, and no subsequent complications were noted. In fact, as surgeons became more comfortable with this technique, radiography at the time of sheath insertion was frequently omitted.
CONCLUSIONS
Bedside tunneled dialysis catheter placement is a strategy that deserves further investigation and could be considered in critically ill patients who require renal replacement therapy, regardless of COVID-19 status. Given the ongoing surges of the COVID-19 pandemic, the adoption of these strategies could serve to improve the efficiency of care.
Author Contributions
Study design: AW, SN, RM, VD, AU; Data collection: AW, MQ, JE, LM, SN; Manuscript preparation and critical review: AW, MQ, JE, LM, SN, RM, VD, AU
Previous Presentation
This abstract was previously presented in brief at the 2020 American College of Surgeons Quality and Safety Conference, Resident Quality Improvement session.
Funding
No funding was received or used in support of this work.
Acknowledgments
We would like to thank William D. Surkis, MD for assistance with data retrieval.
References
- 1.WHO Timeline - COVID-19 [Internet] [cited 2020 Jun 5] Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline-covid-19.
- 2.WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020 [Internet] [cited 2020 Jun 5]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 3.Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;0(0) doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng Y, Luo R, Wang K, et al. Kidney impairment is associated with in-hospital death of COVID-19 patients. medRxiv. 2020 doi: 10.1016/j.kint.2020.03.005. Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang G, Hu C, Luo L, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104364. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. 2020. pp. 829–838. Vol. 97, Kidney International. Elsevier B.V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pei G, Zhang Z, Peng J, et al. Renal involvement and early prognosis in patients with COVID-19 PNEUMONIA. J Am Soc Nephrol. 2020;31:1157–1165. doi: 10.1681/ASN.2020030276. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;0(0) doi: 10.1016/j.kint.2020.05.006. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fanelli V, Fiorentino M, Cantaluppi V, et al. Acute kidney injury in SARS-CoV-2 infected patients. Crit Care. 2020;24:155. doi: 10.1186/s13054-020-02872-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soleimani M. Acute kidney injury in SARS-CoV-2 infection: direct effect of virus on kidney proximal tubule cells. Int J Mol Sci. 2020;21 doi: 10.3390/ijms21093275. May 1, 3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diao B, Feng Z, Wang C, et al. Human kidney is a target for novel severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection. medRxiv. 2020;2 doi: 10.1038/s41467-021-22781-1. Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;14:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adapa S, Adapa S, Aeddula NR, et al. COVID-19 and renal failure: challenges in the delivery of renal replacement therapy. J Clin Med Res. 2020;12:276–285. doi: 10.14740/jocmr4160. May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ronco C, Reis T, Husain-Syed F. Management of acute kidney injury in patients with COVID-19. Lancet Respir Med. 2020;8:738–742. doi: 10.1016/S2213-2600(20)30229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirksey L, Vacharajani T, Droz NM, et al. COVID era “essential surgery” dialysis access management considerations. J Vasc Surg. 2020;72:1845–1849. doi: 10.1016/j.jvs.2020.07.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures [Internet]. [cited 2020 Jun 5]. Available from: https://www.facs.org/covid-19/clinical-guidance/triage
- 20.COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation [Internet]. [cited 2020 Jun 5]. Available from: https://www.facs.org/covid-19/clinical-guidance/surgeon-protection
- 21.Society for Vascular Surgery . COVID-19 Vascular Surgery Triage Guidelines. 2020. [Google Scholar]
- 22.Ross SW, Lauer CW, Miles WS, et al. Maximizing the calm before the storm: tiered surgical response plan for novel coronavirus (COVID-19) J Am Coll Surg. 2020;230 doi: 10.1016/j.jamcollsurg.2020.03.019. Jun 11080–1091.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendu ML, May MF, Kaze AD, et al. Non-tunneled versus tunneled dialysis catheters for acute kidney injury requiring renal replacement therapy: a prospective cohort study. BMC Nephrol. 2017;18 doi: 10.1186/s12882-017-0760-x. Dec 4. https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-017-0760-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tunneled Dialysis Catheters Versus Non-tunneled Dialysis Catheters as First-line for Renal Replacement Therapy in the ICU - Full Text View - ClinicalTrials.gov [Internet]. [cited 2020 Jun 14]. Available from: https://clinicaltrials.gov/ct2/show/NCT03496935
- 25.Coronavirus in the U.S.: Latest Map and Case Count - The New York Times [Internet]. [cited 2020 Jun 15]. Available from: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#states
- 26.Bialek S, Boundy E, Bowen V, et al. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. 2020. pp. 343–346. MMWR Morb Mortal Wkly RepMar 27;69(12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weijmer MC, Vervloet MG, ter Wee PM. Compared to tunnelled cuffed haemodialysis catheters, temporary untunnelled catheters are associated with more complications already within 2 weeks of use. Neprhol Dial Transpl. 2004;19:670–677. doi: 10.1093/ndt/gfg581. Mar. [DOI] [PubMed] [Google Scholar]
- 28.Klouche K, Amigues L, Deleuze S, et al. Complications, effects on dialysis dose, and survival of tunneled femoral dialysis catheters in acute renal failure. Am J Kidney Dis. 2007;49:99–108. doi: 10.1053/j.ajkd.2006.09.014. Jan. [DOI] [PubMed] [Google Scholar]
- 29.Vats HS. Complications of catheters: tunneled and nontunneled. Adv Chronic Kidney Dis. 2012;19:188–194. doi: 10.1053/j.ackd.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Asif A, Cherla G, Merrill D, et al. Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int. 2005;67:2399–2406. doi: 10.1111/j.1523-1755.2005.00347.x. [DOI] [PubMed] [Google Scholar]
- 31.Coryell L, Lott JP, Stavropoulos SW, et al. The case for primary placement of tunneled hemodialysis catheters in acute kidney injury. J Vasc Interv Radiol. 2009;20:1578–1581. doi: 10.1016/j.jvir.2009.08.014. Dec. [DOI] [PubMed] [Google Scholar]
- 32.Palevsky PM, Zhang JH, O'Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7–20. doi: 10.1056/NEJMoa0802639. Jul 3. [DOI] [PMC free article] [PubMed] [Google Scholar]