Almost 1 year has passed since the first cases of interstitial pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were reported in Wuhan, China.1 Europe and the United States are now facing a second wave of the coronavirus disease 2019 (COVID-19) pandemic, one of the deadliest pandemics of the modern era with more than 1 million deaths and over 60 million confirmed cases throughout the world as of November 30, 2020.2 Since the beginning, COVID-19 has been exerting an unprecedented impact on public health and health care delivery, with critical issues regarding resource allocation, hospital reorganization and prioritization of patients and diseases.3, 4 In times of scarcity of medical resources and persistent pressure on health systems, the early differentiation between high- and low-risk patients is of paramount significance for frontline physicians. Risk stratification is even more crucial for a rapidly evolving and heterogeneous disease like COVID-19, which may swiftly progress from mild constitutional symptoms to severe acute respiratory distress syndrome and multiorgan failure, with frequent involvement of the cardiovascular system.5
Compelling evidence has shown that cardiac troponin elevations are strongly associated with disease severity and hard outcomes in patients with COVID-19, irrespective of the underlying mechanism of cardiovascular involvement. In the study by Calvo-Fernández et al. recently published in Revista Española de Cardiología, the authors evaluated the short-term predictive value of high-sensitivity cardiac-specific troponin-T (hs-cTnT) and N-terminal pro-B-type natriuretic peptide (NT-pro-BNP) assessed at the time of hospital admission in the largest European cohort (n = 872) of laboratory-confirmed COVID-19 patients reported to date.6 hs-cTnT and NT-pro-BNP cutoff serum levels were set, respectively, at > 14 ng/L (which is the 99th percentile upper reference limit, according to the manufacturer) and > 300 pg/mL (which is the recognized threshold for heart failure rule-out in the acute setting).7 Pathological levels of hs-cTnT and NT-pro-BNP were found in 34.6% and 36.2% of the patients, respectively, and proved to be strong independent predictors of mortality and of the composite endpoint of mortality or need for mechanical ventilation in a multivariate Cox regression analysis. Of note, NT-pro-BNP showed an additive value with regards to hs-cTnT, significantly improving the discriminatory power of the statistical models. Furthermore, as shown in table 2 of the supplementary data of the article by Calvo-Fernández et al., the negative predictive value of NT-pro-BNP and hs-cTnT with respect to death and to the composite of death and mechanical ventilation was astonishing at both the 30- and 50-day follow-up.
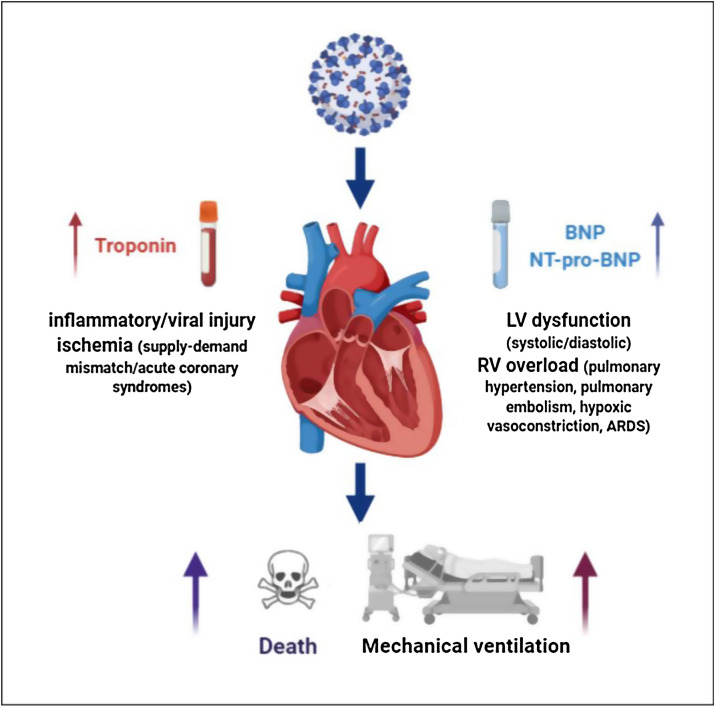
Troponins and natriuretic peptides focus on different aspects of cardiovascular involvement in COVID-19. Troponins are the biomarkers of myocardial injury, which may be due to direct viral damage by SARS-CoV-2 and inflammatory myocarditis in the context of cytokine storm, or myocardial ischemia/infarction as a consequence of oxygen supply-demand imbalance or prothrombotic state with acute coronary syndromes or pulmonary embolisms.5 In contrast, natriuretic peptides are sensitive indicators of hemodynamic cardiac stress, which may be due to ischemic or inflammatory left ventricular systolic/diastolic dysfunction and right heart overload secondary to the pulmonary consequences of the disease (pulmonary embolism, pulmonary hypertension, hypoxic vasoconstriction, acute respiratory distress syndrome).7 Thus, troponins and natriuretic peptides are complementary in the overall evaluation of cardiac involvement in COVID-19 patients (fig. 1 ), as confirmed by the article by Calvo-Fernández et al. Other studies have already assessed the prognostic role of both troponins and natriuretic peptides with similar findings (table 1 ) and, in particular, BNP and NT-pro-BNP were demonstrated to significantly improve the predictive accuracy of troponins in some of them.6, 8, 9, 10, 11, 12, 13 On the other hand, in 2 recent registries, cardiovascular biomarkers failed to provide additional prognostic information after adjustment for baseline clinical characteristics, comorbidities, vital parameters, and laboratory values mirroring multiorgan dysfunction.14, 15 However, these studies focused on a limited sample size and a selected population of critically ill patients, respectively, and also detected higher levels of cardiac biomarkers in patients with worse prognosis.
Figure 1.
Prognostic role of cardiac troponins and natriuretic peptides in COVID-19 patients. ARDS, acute respiratory distress syndrome; BNP, B-type natriuretic peptide; LV, left ventricular; NT-pro-BNP, N-terminal pro-B-type natriuretic peptide; RV, right ventricular.
Table 1.
Main studies demonstrating the prognostic role of cardiac troponin and natriuretic peptides with regards to mortality in hospitalized patients with COVID-19
| Location | Patients, N | Assay used and cutoff | Follow-up | Unadjusted HR or OR (95%CI) for death | Adjusted HR or OR (95%CI) for death | Reference |
|---|---|---|---|---|---|---|
| Wuhan, China | 3219 | hs-cTnI, BNP or NT-pro-BNP (different cutoffs according to different hospital sites) | 28 days | hs-cTnI: 9.59 (6.36-14.47) (NT-pro-)BNP: 5.62 (3.99-7.93) |
hs-cTnI: 7.12 (4.6-11.03) (NT-pro-)BNP: 5.11 (3.5-7.47) |
Qin et al.8 |
| Wuhan, China | 264 | hs-cTnI > 0.020 ng/mL; NT-pro-BNP > 340 pg/mL |
In-hospital | hs-cTnI: 3.48 (1.88-6.43); NT-pro-BNP: 6.33 (2.51-15.95) |
hs-cTnI: 3.08 (1.62-5.88) NT-pro-BNP: 5.78 (2.27-14.68) |
Deng et al.9 |
| Wuhan, China | 54 | NT-pro-BNP > 88.64 pg/mL | In-hospital | hs-cTnI (per 1 ng/mL): 1.86 (1.27-2.72) NT-pro-BNP (per 100 pg/mL): 1.37 (1.22-1.54) |
hs-TnI, (per 0.1 ng/mL): 1.03 (0.57-1.86) NT-pro-BNP (per 100 pg/mL): 1.36 (1.18-1.57) |
Gao et al.10 |
| New York, United States | 1053 | cTnI ≥ 0.34 ng/mL BNP ≥ 295 pg/mL |
30 days | cTnI: 5.47 (3.31-9.04) BNP: 1.94 (1.17-3.22) |
cTnI: 4.38 (2.32-8.28) | Manocha et al.11 |
| Rio de Janeiro, Brazil | 183 | hs-cTnT > 0.014 ng/mL BNP > 100 pg/mL |
In-hospital | - | hs-cTnT: 1.13 (1.05-1.21)* BNP: 1.05 (0.95-1.15)* |
Almeida Junior et al.12 |
| Milan, Italy | 397 | hs-cTnI ≥ 19.6 ng/L BNP ≥ 100pg/mL |
In-hospital | hs-cTnI: 1.9 (1.6-2.3) BNP: 2.8 (2.2-3.7) |
hs-cTnI and BNP: 3.24 (1.06-9.93) | Stefanini et al.13 |
| Barcelona, Spain | 872 | hs-cTnT > 14 ng/L NT-pro-BNP > 300 pg/mL |
30 and 50 days | - | hs-cTnT: 2.91 (1.21-7.04) NT-pro-BNP: 5.47 (2.10-14.26) |
Calvo-Fernández et al.6 |
95%CI, 95% confidence interval; BNP, B-type natriuretic peptide; cTn, cardiac troponin; HR, hazard ratio; hs-cTn, high-sensitivity cardiac troponin; N, number of patients; NT-pro-BNP, N-terminal pro-B-type natriuretic peptide; OR, odds ratio.
Combined outcome of all-cause death or need for mechanical ventilation.
Whatever the underlying mechanisms and pathophysiology of cardiac involvement in COVID-19, a comprehensive early assessment of cardiac biomarkers may be pragmatically used to differentiate high-risk patients—who require intense monitoring and precociously aggressive treatment, from low-risk participants, who may be managed with a strict outpatient follow-up. Thus, in times of paucity of resources and difficulties in priority setting, low-price and widespread cardiac biomarkers may play a decisive role. Moreover, the identification of a significant cardiac involvement might activate a cardiological work-up and a dedicated cardiovascular follow-up with tailored diagnostic and interventional acts during hospitalization or after COVID-19 recovery. As shown by Giustino et al., the echocardiographic characterization of myocardial injury in COVID-19 might further improve risk stratification and guide appropriate management strategies.16
We truly congratulate the authors for this interesting piece of evidence, although a few limitations should be considered.6 First, the observational nature of the study does not prove a causal relationship between cardiac involvement and outcomes. Second, the generalizability of the results may be limited by the single-center nature of the registry. Third, only 75% of patients could be tested for hs-cTnT and 58% for NT-pro-BNP, so selection bias cannot be excluded. However, this work reinforces the role for early systematic surveillance with cardiac biomarkers in a wide population of hospitalized patients with COVID-19.
As the COVID-19 pandemic continues to hit our countries with thousands of hospitalizations and deaths, the availability of low-cost tools with an established predictive value may wisely support frontline physicians in their hard daily choices.
Conflicts Of Interest
None declared.
References
- 1.Fauci A.S., Lane H.C., Redfield R.R. Covid-19 -Navigating the Uncharted. N Engl J Med. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available at: https://covid19.who.int/. Accessed 30 Nov 2020.
- 3.Stefanini G.G., Azzolini E., Condorelli G. Critical Organizational Issues for Cardiologists in the COVID-19 Outbreak: A Frontline Experience From Milan, Italy. Circulation. 2020;141:1597–1599. doi: 10.1161/CIRCULATIONAHA.120.047070. [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez-Leor O., Cid-Álvarez B., Pérez de Prado A., for the Working Group on the Infarct Code of the Interventional Cardiology Association of the Spanish Society of Cardiology Investigators. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience Rev Esp Cardiol. 2020;73:994–1002. doi: 10.1016/j.rec.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giustino G., Pinney S.P., Lala A. Coronavirus and Cardiovascular Disease, Myocardial Injury, and Arrhythmia: JACC Focus Seminar. J Am Coll Cardiol. 2020;76:2011–2023. doi: 10.1016/j.jacc.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calvo-Fernández A., Izquierdo A., Subirana I. Markers of myocardial injury in the prediction of short-term COVID-19 prognosis. Rev Esp Cardiol. 2021;74:576–583. doi: 10.1016/j.rec.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mueller C., McDonald K., de Boer R.A. Heart Failure Association of the European Society of Cardiology Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail. 2019;21:715–731. doi: 10.1002/ejhf.1494. [DOI] [PubMed] [Google Scholar]
- 8.Qin J.J., Cheng X., Zhou F. Redefining Cardiac Biomarkers in Predicting Mortality of Inpatients With COVID-19. Hypertension. 2020;76:1104–1112. doi: 10.1161/HYPERTENSIONAHA.120.15528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng P., Ke Z., Ying B., Qiao B., Yuan L. The diagnostic and prognostic role of myocardial injury biomarkers in hospitalized patients with COVID-19. Clin Chim Acta. 2020;510:186–190. doi: 10.1016/j.cca.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao L., Jiang D., Wen X.S. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res. 2020;21:83. doi: 10.1186/s12931-020-01352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manocha K.K., Kirzner J., Ying X. Troponin and Other Biomarker Levels and Outcomes Among Patients Hospitalized with COVID-19: Derivation and Validation of the HA2T2 COVID-19 Mortality Risk Score. J Am Heart Assoc. 2020:e018477. doi: 10.1161/JAHA.120.018477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almeida Junior G.L.G., Braga F., Jorge J.K. Prognostic Value of Troponin-T and B-Type Natriuretic Peptide in Patients Hospitalized for COVID-19. Arq Bras Cardiol. 2020;115:660–666. doi: 10.36660/abc.20200385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stefanini G.G., Chiarito M., Ferrante G. Humanitas COVID-19 Task Force, Early detection of elevated cardiac biomarkers to optimise risk stratification in patients with COVID-19. Heart. 2020;106:1512–1518. doi: 10.1136/heartjnl-2020-317322. [DOI] [PubMed] [Google Scholar]
- 14.Omland T., Prebensen C., Røysland R. Established Cardiovascular Biomarkers Provide Limited Prognostic Information in Unselected Patients Hospitalized With COVID-19. Circulation. 2020;142:1878–1880. doi: 10.1161/CIRCULATIONAHA.120.050089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metkus T.S., Sokoll L.J., Barth A.S. Myocardial Injury in Severe COVID-19 Compared to Non-COVID Acute Respiratory Distress Syndrome. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.050543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giustino G., Croft L.B., Stefanini G.G. Characterization of Myocardial Injury in Patients With COVID-19. J Am Coll Cardiol. 2020;76:2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]