Abstract
This study aimed to assess the impact of coronavirus disease (COVID-19) prevalence in the United States in the week leading to the relaxation of the stay-at-home orders (SAH) on future prevalence across states that implemented different SAH policies. We used data on the number of confirmed COVID-19 cases as of August 21, 2020 on county level. We classified states into four groups based on the 7-day change in prevalence and the state's approach to SAH policy. The groups included: (1) High Change (19 states; 7-day prevalence change ≥50th percentile), (2) Low Change (19 states; 7-day prevalence change <50th percentile), (3) No SAH (11 states: did not adopt SAH order), and (4) No SAH End (2 states: did not relax SAH order). We performed regression modeling assessing the association between change in prevalence at the time of SAH order relaxation and COVID-19 prevalence days after the relaxation of SAH order for four selected groups. After adjusting for other factors, compared to the High Change group, counties in the Low Change group had 33.8 (per 100,000 population) fewer cases (standard error (SE): 19.8, p < 0.001) 7 days after the relaxation of SAH order and the difference was larger by time passing. On August 21, 2020, the No SAH End group had 383.1 fewer cases (per 100,000 population) than the High Change group (SE: 143.6, p < 0.01). A measured, evidence-based approach is required to safely relax the community mitigation strategies and practice phased-reopening of the country.
Keywords: Coronavirus disease prevalence, COVID-19 prevalence, Stay-at-home orders, Reopening
1. Introduction
In the US, the total number of confirmed Coronavirus Disease 2019 (COVID-19) cases has skyrocketed from 30 patients on Mar 1st, 2020 to over 5.6mil on Aug 21st with total deaths exceeding 175 k (Johns Hopkins University and Medicine, 2020). The pandemic has also placed unprecedented challenges on states and local governments across the United States to mitigate the ongoing spread and the possible resurgence of the disease. During the pandemic, a variety of community mitigation policies such as social distancing (e.g., imposing shelter-in-place or stay-at-home (SAH) orders; restricting dine-in at restaurants; closing nonessential business such as bars, entertainment venues, and gyms; banning large social gatherings; and closing public schools) and face-masking have been adopted by the states and localities (Centers for Disease Control and Prevention. Coronavirus Disease, 2019). In the absence of an effective drug treatment or vaccine, such policies are critical to decreasing the mobility patterns and virus transmission rate across different communities. Previous studies have assessed the impact of implementation of such policies on decreasing COVID-19 prevalence, hospitalization, and death rates (Courtemanche et al., 2020; Xu et al., 2020; Badr et al., 2020; VoPham et al., 2020; Lyu and Wehby, 2020; Friedson et al., 2020). But evidence on the proper relaxation of the mitigation policies is not well-developed.
A critical question is an appropriate time for the relaxation of the community mitigation measures. Centers for Disease Control and Prevention (CDC) has recommended a downward trajectory of documented COVID-19 cases or positive tests (as a percent of total tests) within 14 days as the gating indicators to assess the relaxation of the community mitigation measures (The U.S. Department of Health and Human Services. Centers for Disease Control and Prevention, 2020). Despite such recommendations, several states moved forward with the relaxation of the measures without a consistent downward trend (Johns Hopkins University and Medicine, 2020; Boston University School of Public Health, 2020). The surge in the number of daily cases across the US from mid-June to mid-July might partially be attributed to such an approach.
We assessed the impact of COVID-19 prevalence in the week leading to the relaxation of the mitigation measures on future prevalence overall and across counties that implemented different policies for adoption and relaxation of the SAH order.
2. Methods
We used data on the number of cumulative confirmed cases from the COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University at the county-level across the US1 as the numerator and the county resident population as the denominator to calculate COVID-19 prevalence. To address fluctuations in the daily reported number of cases we used the 7-day smoothed change in COVID-19 prevalence at the county-level.
We obtained the dates on the community mitigation policies from the COVID-19 US State Policy (CUSP) project at the Boston University School of Public Health (reviewed on August 21, 2020) (Boston University School of Public Health, 2020). To address the variation in the type of policies as well as the timing of adopting and relaxing each policy we used the dates for SAH order across different states. The SAH policy had a widespread and strong impact on reducing social interactions due to its nature and the number of people affected compared to other community mitigation policies (Abouk and Heydari, 2020).
To take into account the extent that residents in each community practiced the community mitigation policies we used the social distancing index (SDI) (Maryland Transportation Institute, 2020; Zhang et al., 2020) from the COVID-19 Impact Analysis Platform created by the Maryland Transportation Institute at the University of Maryland. The SDI was an integer from 0– 100 that represented the extent residents and visitors were practicing social distancing. “0” indicated no social distancing was observed in the community, while “100” indicated all residents were staying at home and no visitors were entering the county (Maryland Transportation Institute, 2020; Zhang et al., 2020).
We identified states that both adopted and relaxed the SAH orders (38 states as of August 21, 2020, the time of this analysis). We ranked those states according to the 7-day change in prevalence at the time of SAH order relaxation and divided them by the 50th percentile rank to identify states with a high and low change in prevalence. As of August 21, 2020, 13 states did not adopt a SAH order or did not relax the SAH order. In order to include those states in the analysis we used the midpoint date of the first and the last SAH order adoption (March 28, 2020) and the first and the last SAH order relaxation (May 22, 2020) in other states and included the 7-day change in prevalence on those dates for those 13 states in the analysis. These classifications resulted in four groups of states; (1) High Change group (19 states with the 7-day change in prevalence at 50th percentile and higher), (2) Low Change group (19 states with the 7-day change in prevalence below 50th percentile), (3) No SAH group (11 states that did not adopt a SAH order), and (4) No SAH End group (2 states that did not relax the SAH order). The values presented in the results for states in the No SAH and No SAH End groups should be viewed as approximations of values during the interval where such policies were adopted and relaxed by other states. Using the 50th percentile rank as the cut point for states that both adopted and relaxed the SAH orders helped us to have equal number of states in the High Change and Low Change groups. Additionally, we used the 75th and 90th percentile ranks as the cut points to identify states in the High Change and Low Change groups. Refer to eTable 1 for detailed information on dates for SAH order adoption and relaxation across four groups and the 7-day change in prevalence at the time of SAH order relaxation.
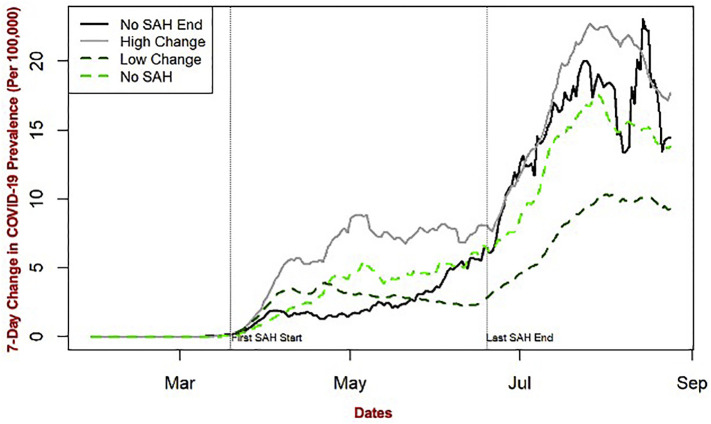
We performed county-level descriptive statistics to assess the prevalence and spread of COVID-19 at the time of SAH order adoption and relaxation across the country and for High Change, Low Change, No SAH, and No SAH End groups. Moreover, we plotted the 7-day change in prevalence for High Change, Low Change, No SAH, and No SAH End groups from February 2020 to the present date (August 21, 2020). We performed linear regression modeling to assess the impact of the 7-day change in prevalence at the time of SAH order relaxation on the COVID-19 prevalence 7, 14, 21, 28 days after the relaxation of SAH order and the current time (i.e. August 21, 2020) for the four selected groups while adjusting for SDI. Furthermore, we performed sensitivity analysis, running the linear regression model after setting the 75th and 90th percentile ranks as the cut points to identify states in the High Change and Low Change groups. Refer to eTables 2 and 3 for results of the linear regression models using the 75th and 90th percentile ranks as the cut point.
We conducted all analyses using R version 3.3.1. We did not obtain an Institutional Review Board following the policy of our institution for secondary data analysis of publicly available data. This study was funded by the Center for Population Health IT, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health.
3. Results
At the time of SAH order adoption, the mean COVID-19 prevalence was 12.4 per 100,000 population (standard deviation (SD): 30.9) across the country while at the time of SAH order relaxation the prevalence increased to 234.6 per 100,000 (SD: 472.1) and the increase was statistically significant (p < 0.001). The mean 7-day SDI value decreased from 39.2 (SD: 8.7) at the time of SAH order adoption to 28.8 (SD:8.3) at the time of SAH order relaxation and the decrease was statistically significant (p < 0.001). Table 1 presents the confirmed number of COVID-19 cases, prevalence per 100,000 population, the 7-day change in prevalence, and 7-day smoothed SDI for four groups of counties at the time of SAH order adoption and relaxation.
Table 1.
Summary county-level statistics for COVID-19 features by adoption and relaxation of stay-at-home orders.
| High Change Groupa Mean (SD) | Low Change Groupa Mean (SD) | No SAH Groupa Mean (SD) | No SAH End Groupa Mean (SD) | |
|---|---|---|---|---|
| Number (%) of counties | 1229 (39.1%) | 925 (29.4%) | 897 (28.5%) | 91 (2.9%) |
| Stay-at-home Adoptionb | ||||
| Number of cases | 27.1 (129.8) | 38 (346.2) | 6.9 (41.9) | 12.2 (34.5) |
| Prevalence per 100,000 | 19.3 (41.4) | 10.6 (23.6) | 6.1 (17.2) | 1.8 (2.8) |
| 7-day change in prevalence | 2.8 (7.2) | 1.7 (5.7) | 1,1 (4.0) | 0.3 (0.7) |
| 7-day SDI | 39.5 (9.0) | 40.5 (9.2) | 38.0 (7.6) | 34.3 (7.4) |
| Stay-at-home Relaxationb | ||||
| Number of cases | 482.1 (1874.8) | 802.8 (7778) | 172.7 (894.6) | 1063.3 (4662.9) |
| Prevalence per 100,000 | 303.9 (481.4) | 181.5 (374.0) | 202.5 (545.0) | 155.4 (335.8) |
| 7-day change in prevalence | 8.3 (24.7) | 2.4 (9.1) | 4.6 (30.5) | 4.1 (9.1) |
| 7-day SDI | 31.0 (8.2) | 28.7 (8.8) | 25.2 (6.4) | 34.1 (9.0) |
COVID-19: Coronavirus Disease 2019, SD: Standard Deviation, SAH: Stay-at-Home, SDI: Social Distancing Index.
High Change group (counties in 19 states with the 7-day change in COVID-19 prevalence at the time of SAH order relaxation at 50th percentile and higher), Low Change group (counties in 19 states with the 7-day change in prevalence below 50th percentile), No SAH group (counties in 11 states that did not adopt a SAH order), and No SAH End (counties in 2 states that did not relax the SAH order).
The values presented for counties in the No SAH and No SAH End groups should be viewed as approximations of values during the interval where such policies were adopted and relaxed by other states.
Among the more notable findings, at the time of SAH order adoption, counties in the High Change group had a higher statistically significant prevalence and the 7-day change in prevalence compared to counties in the Low Change, No SAH, and No SAH End groups (p < 0.001). By the time of SAH order relaxation, both prevalence and the 7-day change in prevalence for the High Change group were statistically significantly higher than the Low Change (p < 0.001), No SAH (p < 0.001), and the No SAH End groups (p < 0.05).
The four-county groups maintained similarly elevated levels of social distancing or SDI at the time of SAH order adoption, which fell by SAH order relaxation. Counties in the No SAH group had the lowest SDI comparing to the other groups at the time of SAH order relaxation. Counties in the No SAH End group maintained a relatively elevated level of SDI from SAH order adoption to SAH order relaxation in other states. They had the highest SDI comparing to the other groups at the time of SAH order relaxation.
Fig. 1 presents the 7-day change in prevalence for counties across the High Change, Low Change, No SAH, and No SAH End groups from February 2020 to the present date (August 21, 2020). The 7-day change in prevalence had a steady increase from mid-April to late June for counties in the High Change, No SAH, and No SAH End groups. But it presented a slight decrease for counties in the Low Change group. From mid-June to the present date the 7-day change in prevalence presented a sharper increase for counties in all four groups with a sharper slope for counties in the High Change group comparing to other groups.
Fig. 1.
The 7-day change in COVID-19 prevalence across four groups of US counties from February to August 2020.
High Change group (counties in 19 states with the 7-day change in COVID-19 prevalence at the time of SAH order relaxation at 50th percentile and higher), Low Change group (counties in 19 states with the 7-day change in prevalence below 50th percentile), No SAH group (counties in 11 states that did not adopt a SAH order), and No SAH End (counties in 2 states that did not relax the SAH order).
COVID-19: Coronavirus Disease 2019, SAH: Stay-at-Home.
The regression modeling of county-level COVID-19 prevalence (Table 2 ) showed that across all counties the 7-day change in prevalence at the time of SAH order relaxation was predictive of eventual levels of prevalence at future time points (e.g., 7 and 14 days after SAH order relaxation, R-squared: 0.339 and 0.369 respectively). For instance, holding county groups and SDI constant an increase in the 7-day change in prevalence at the time of SAH order relaxation resulted in 19.6 cases (per 100,000 population) increase in COVID-19 prevalence 7 days after the relaxation of SAH order and 22.0 cases (per 100,000 population) increase 14 days after the relaxation of SAH order (standard error (SE): 0.5, p < 0.001).
Table 2.
Linear regression model assessing the impact of different factors on COVID-19 prevalence after the relaxation of stay-at-home order.a
| SAH order relaxation + 7 days |
SAH order relaxation + 14 days |
SAH order relaxation + 21 days |
SAH order relaxation + 28 days |
Current Timeb |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SE)c | P-value | Mean (SE)c | P-value | Mean (SE)c | P-value | Mean (SE)c | P-value | Mean (SE)c | P-value | |
| 7-day change in prevalence at the time of relaxation of SAH order | ||||||||||
| 19.6(0.5) | < 0.001 | 22(0.5) | < 0.001 | 23.8(0.6) | < 0.001 | 24.9(0.6) | < 0.001 | 28.7(1.2) | < 0.001 | |
| County Groupsd (High Change group as reference) | ||||||||||
| Low Change group | −33.8(19.8) | < 0.001 | −58.8(20.8) | < 0.001 | −93.4(22.2) | < 0.001 | −124.6(23.3) | < 0.001 | −789.5(46.3) | < 0.001 |
| No SAH Group | −42.8(19.9) | 0.031 | −22.7(21.6) | 0.292 | −32.7(22.7) | 0.150 | −41.4(22.8) | 0.070 | −411.5(46.2) | < 0.001 |
| No SAH End group | −167(60.7) | < 0.01 | −167.5(63.8) | < 0.01 | −181.1(67.4) | 0.070 | −150.5(69.2) | < 0.05 | −383.1(143.6) | < 0.01 |
| Social distancing index | ||||||||||
| 7.0(1.1) | < 0.001 | 7.8(1.2) | < 0.001 | 9.4(1.3) | < 0.001 | 5.1(1.5) | < 0.01 | 7.1(3.1) | < 0.05 | |
| R- squared of model performance | ||||||||||
| 0.339 | 0.369 | 0.381 | 0.398 | 0.250 | ||||||
COVID-19: Coronavirus Disease 2019, SE: Standard Error, SAH: Stay-at-Home.
The linear regression model with the COVID-19 prevalence at 7, 14, 21, 28 days after the relaxation of SAH order and at the current time (i.e. august 21, 2020) as the outcome (dependent variable), using the 50th percentile rank as the cut point to identify states in the High Change and Low Change groups.
Current time refers to the time of completing this study (i.e. august 21, 2020).
The mean and standard errors or the parameter estimates are the coefficients of the regression model for independent variables in the model (i.e., 7-day change in prevalence at the time of relaxation of SAH order, county groups, and social distancing index).
High Change group (counties in 19 states with the 7-day change in COVID-19 prevalence at the time of SAH order relaxation at 50th percentile and higher), Low Change group (counties in 19 states with the 7-day change in prevalence below 50th percentile), No SAH group (counties in 11 states that did not adopt a SAH order), and No SAH End (counties in 2 states that did not relax the SAH order).
Across four categories of counties after adjusting for other factors, comparing to the High Change group, the Low Change group presented statistically significantly lower growth in their prevalence days after the relaxation of SAH order and the difference was larger by time passing. For instance, 14 and 21 days after the relaxation of SAH order the Low Change group had 58.8 and 93.4 fewer cases (per 100,000 population) than High Change group (SE: 19.8 and 20.8, p < 0.01, respectively).
Comparing to the High Change group the No SAH End group presented a statistically significant difference in prevalence days after the relaxation of SAH order. For instance, at the time of completing this study (August 21, 2020) the No SAH End group had 383.1 fewer cases (per 100,000 population) than the High Change group (SE: 143.6, p < 0.01).
4. Discussion
We assessed the county-level COVID-19 prevalence at the time of SAH order adoption and relaxation across four groups of counties that practiced different approaches to reinforcing community mitigation policies (e.g., High Change, Low Change, No SAH, and No SAH End). Since the SAH policies across different states were mostly based on COVID-19 statewide figures we used the state level 7-day change in prevalence at the time of SAH order relaxation to categorize states into four groups.
We assessed the association between prior prevalence and prevalence at future time points across four groups of counties using the 7-day change in prevalence while adjusting for SDI. These attributes reflected a combination of state-level policy decision to relax SAH orders at high vs low levels of change and the extent of social distancing evidenced at the county-level for each time point. Our findings presented the substantial impact of the prior COVID-19 prevalence on the prevalence at future time points across all counties.
Among four groups of counties after adjusting for other factors, counties in states such as West Virginia with lower COVID-19 prevalence at the time of SAH order relaxation (the Low Change group) experienced statistically significantly lower growth in COVID-19 prevalence days after the relaxation of SAH order comparing to counties in states such as Arizona with high prevalence and lack of a downward trend at the time of SAH order relaxation (the High Change group). The difference was even larger at later time points (e.g., 21 and 28 days after SAH order relaxation). In contrast, comparing to High Change group counties in the No SAH End group (California and New Mexico), which experienced a higher number of confirmed cases and relatively high prevalence at the time of SAH order relaxation in other states, presented more growth in COVID-19 prevalence in early days (7 and 14 days after the relaxation of SAH order in other states) but the growth in the prevalence was lower after approximately one incubation period. This pattern was consistent with the theoretical effect of community mitigation policies on COVID-19 spread (Teslya et al., 2020) and the spread of prior epidemics of communicable diseases (Hatchett et al., 2007). Performing sensitivity analysis, setting the cut point at 75th and 90th percentile to identify states in the High Change and Low Change groups, presented the same patterns with counties in the High Change group experiencing statistically significantly higher growth in COVID-19 prevalence days after the relaxation of SAH order compared to the ones in other groups. Other studies observed similar patterns of change in COVID-19 epidemic growth after the implementation of community mitigation policies (Courtemanche et al., 2020; Xu et al., 2020; VoPham et al., 2020; Friedson et al., 2020; Siedner et al., 2020; Tuite et al., 2020).
Our findings were consistent with the CDC recommendations (The U.S. Department of Health and Human Services. Centers for Disease Control and Prevention, 2020) and the “Opening Up America Again” plan by the current administration (White House, 2020) for the phased reopening of communities across the country. These findings present the importance of an evidence-based approach to reopening which takes into account the current prevalence and spread of the disease in a community before moving toward relaxation of community mitigation policies. The early relaxation of such policies fails to achieve the desired benefits (Scherbina, 2020). Adoption of community mitigation policies for a long duration in either a sustained manner or with periodic dialing up and down of restrictions would have a better impact to prevent the resurgence of the disease (Tuite et al., 2020). Moreover, when the testing capacity is not high or active contact tracing in a community is not available to control COVID-19 spread, considering a staged relaxation of community mitigation policies and monitoring changes in contacts as an early warning signal might be the next best option (Tuite et al., 2020; Wrighton and Lawrence, 2020; Cheng et al., 2020). While out of the scope of this study cost-benefit analysis has also presented the economic benefits of the timely relaxation of the community mitigation policies for states and local governments (Scherbina, 2020).
The 7-day change in prevalence for four groups of counties over time provided similar findings (Fig. 1). The graph showed an increase in the prevalence across all four groups of counties after the relaxation of SAH orders with the High Change group experiencing the sharpest increase and the Low Change group experiencing the slowest increase in the 7-day change in prevalence. Counties in the No SAH End group (California and New Mexico) had a steady 7-day change in prevalence after the adoption of the SAH order. As early adopters of SAH order, those states appeared to gain larger benefits from their SAH orders (Dave et al., 2020). The graph also showed a sharper increase in the prevalence across all four groups of counites after the relaxation of SAH orders. The upward trend in the No SAH End group is particularly important. It supports the hypothesis that SAH orders and other community mitigation policies would be most effective if they were imposed nationally and the relaxation of such policies in neighboring states (e.g., Oregon, Nevada, and Arizona) possibly resulted in an increase in the prevalence in the states that continued with such mitigation measures (e.g., California and New Mexico). The experience of countries with national coordination of the pandemic to successfully limit the spread of the virus supports the same hypothesis (Bornstein et al., 2020).
In terms of compliance with community mitigation policies counties across the four groups presented elevated levels of SDI at the time of SAH order adoption. The SDI was comparable in the No SAH group at the SAH order adoption midpoint, which implied that individuals practiced social distancing despite a mixed political message and the lack of SAH orders in their states (Badr et al., 2020). The No SAH End group had the lowest SDI at the time of SAH order adoption, those states (California and New Mexico) implemented the SAH order early on and possibly before the threat of COVID-19 was fully conceived by the public, which might explain the slightly lower SDI comparing to other groups. The SDI dropped at the time of SAH order relaxation across four-county groups. The decline in compliance with social distancing policies was the least in the No SAH End group and the most in No SAH group, which supports the impact of policy interventions to maintain adequate behavior change.
The findings of this study should be interpreted with the following limitations in mind. We had access to a limited data set on a population level. The granularity of population level data were not ideal for detecting small or nuanced effects. As more data become available on COVID-19 cases, we expect finer resolution of geographic data, making it necessary to reevaluate and confirm these findings in smaller community levels. The official number of confirmed COVID-19 cases might not include asymptomatic carriers, those who did not seek medical care due to minor disease-related symptoms, and those who were not tested due to lack of available testing or indirect cost (Friedson et al., 2020). Our data did not include information on individual's race, age, and gender, which are critical factors in defining the risk and should be considered in future modeling efforts for COVD-19 prevalence. Additional work is also required to tie in known clinical risk factors and socioeconomic determinants of health to adequately predict the future of the pandemic in relation to mitigation policies and the geographies that are most impacted by the pandemic.
There was variability in methods of reporting COVID-19 cases and data quality across states. There were also fluctuations in the number of confirmed cases and prevalence reported daily across different counties. Each week, we identified a spike in the number of confirmed cases reported on Monday, presumably from labs holding reports over the weekend. To address this issue we used the 7-day change in prevalence. We acknowledge that COVID-19 testing and prevalence are inter-connected and higher testing in specific communities might result in higher disease and lack of adequate testing might lead to spurious results.
Furthermore, there were variations in the type of policies as well as the timing of adopting and relaxing each policy across different states. For instance, New York state did not officially announce the relaxation of the SAH order. But they extended the SAH order up to June 13, 2020, with an order to reevaluate on that date. To be consistent with other research projects assessing the impact of mitigation policies on COVID-19 prevalence we obtained the dates on the community mitigation policies from the CUSP project at the Boston University School of Public Health (Boston University School of Public Health, 2020). The CUSP project referred to the state-wide governor orders for selecting the dates for SAH order adoption and relaxations. The diversity of different mitigation policies across states made the state classification challenging. While we defined a No SAH End group, containing California and New Mexico, by the time of completion of this study all states had some start to a phased reopening. For instance, California was at phase 2 of reopening before tightening restrictions again.
Despite limitations, our findings present the substantial impact of COVID-19 prevalence in the week leading to the relaxation of the mitigation measures on future disease prevalence in a community. These findings could provide evidence to state and local governments across the country regarding the importance of a measured, evidence-based approach to safely relax the community mitigation strategies and practice phased-reopening of the country. These results also confirm the fact that a unified and organized effort across all states would result in more sustainable success to mitigate the ongoing spread of COVID-19 and the possible resurgence of the disease.
Contribution of each author
All authors contributed significantly to the project and writing of the manuscript. All authors reviewed the final paper and provided comments as deemed necessary. EH supervised the development of the analysis plan, reviewed and interpreted the results, and led writing this paper. CK, H-YC, and WT performed the data analysis. HK contributed to setting the overall scope and goal of the project as well as finalizing the manuscript. JW designed the overall scope and goals of the study and supervised the day-to-day operations of the project.
Sources of funding and support
Internal funding from Center for Population Health IT, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States of America.
Declaration of Competing Interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2021.106435.
Appendix A. Supplementary data
Supplementary material
References
- Abouk R., Heydari B. William Paterson University; Wayne (NJ): 2020. The Immediate Effect of COVID-19 Policies on Social Distancing Behavior in the United States[Internet]https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3571421 Apr 8 [last updated 2020 Apr 27] Accessed on September 2, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H.S., Du H., Marshall M., et al. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect. Dis. 2020;20:S1473–S3099. doi: 10.1016/S1473-3099(20)30553-3. 30553-3. Jul 1. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein S.S., Mire R.D., Barrett E.D., et al. The collision of COVID-19 and the U.S. health system. Ann. Intern. Med. 2020:M20–1851. doi: 10.7326/M20-1851. Jun 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boston University School of Public Health . 2020. COVID-19 US State Policy Database (CUSP) https://www.bu.edu/sph/2020/04/01/tracking-covid-19-policies/. Accessed on September 2, 2020. [Google Scholar]
- Centers for Disease Control and Prevention. Coronavirus Disease Community Mitigation Resources. 2019. https://www.cdc.gov/coronavirus/2019-ncov/php/open-america/community-mitigation-concepts.html Updated June 29, 2020. (Accessed on September 2, 2020)
- Cheng S.Y., Wang C.J., Shen A.C., et al. How to safely reopen colleges and universities during COVID-19: experiences from Taiwan. Ann. Intern. Med. 2020;2:M20–2927. doi: 10.7326/M20-2927. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C., Garuccio J., Le A., et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood) 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608.Epub. Jul. (2020 May 14) [DOI] [PubMed] [Google Scholar]
- Dave D.M., Friedson A.I., Matsuzawa K., et al. National Bureau of Economic Research; Cambridge (MA): 2020. When Do Shelter-in-Place Orders Fight COVID-19 Best? Policy Heterogeneity across States and Adoption Time. May. (NBER Working Paper No. 27091). (Accessed on September 2, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedson A.I., McNichols D., Sabia J.J., et al. National Bureau of Economic Research; Cambridge (MA): 2020. Did California’s Shelter in Place Order Work? Early Evidence on Coronavirus-Related Health Benefits.http://ftp.iza.org/dp13160.pdf Apr. (NBER Working Paper No. 26992). Available from. (Accessed on September 2, 2020) [Google Scholar]
- Hatchett R.J., Mecher C.E., Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc. Natl. Acad. Sci. U. S. A. 2007;104(18):7582–7587. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins University and Medicine . JHU; Baltimore (MD): 2020. Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)https://coronavirus.jhu.edu/map.html (Accessed on September 2, 2020) [Google Scholar]
- Lyu W., Wehby G.L. Shelter-in-place orders reduced COVID-19 mortality and reduced the rate of growth in hospitalizations. Health Aff (Millwood) 2020 doi: 10.1377/hlthaff.2020.00719.Online. Jul. 9;101377hlthaff202000719. (ahead of print) [DOI] [PubMed] [Google Scholar]
- Maryland Transportation Institute . 2020. University of Maryland, College Park, USA. University of Maryland COVID-19 Impact Analysis Platform. https://data.covid.umd.edu. Accessed on September 2, 2020. [Google Scholar]
- Scherbina A.D. Brandeis University; Boston (MA): 2020. Determining the Optimal Duration of the COVID-19 Suppression Policy: A Cost-Benefit Analysis [Internet]https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3562053 Mar 24. (Accessed on September 2, 2020) [Google Scholar]
- Siedner M.J., Harling G., Reynolds Z., et al. Massachusetts General Hospital; Boston (MA): 2020. Social Distancing to Slow the U.S. COVID-19 Epidemic: An Interrupted Time-Series Analysis. [published online 2020 April]. https://www.researchgate.net/publication/340518052_Social_distancing_to_slow_the_US_COVID-19_epidemic_an_interrupted_time-series_analysis. Accessed on September 2, 2020. [Google Scholar]
- Teslya A., Pham T.M., Godijk N.G., Kretzschmar M.E., Bootsma M.C.J., Rozhnova G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020;17(7):e1003166. doi: 10.1371/journal.pmed.1003166. Erratum in: PLoS Med. 2020 Dec 4;17(12):e1003499. PMID: 32692736; PMCID: PMC7373263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The U.S. Department of Health and Human Services. Centers for Disease Control and Prevention . 2020. CDC Activities and Initiatives Supporting the COVID-19 Response and the President’s Plan for Opening America Up Again. [published online May 2020]. https://www.cdc.gov/coronavirus/2019-ncov/downloads/php/cdc-activities-initiatives-for-covid-19-response.pdf. Accessed on September 2, 2020. [Google Scholar]
- Tuite A.R., Greer A.L., Keninck S.D., et al. Risk for COVID-19 resurgence related to duration and effectiveness of physical distancing in Ontario, Canada. Ann. Intern. Med. 2020;27:M20–2945. doi: 10.7326/M20-2945. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VoPham T., Weaver M.D., Hart J.E., et al. Effect of social distancing on COVID-19 incidence and mortality in the US. medRxiv. 2020 doi: 10.1101/2020.06.10.20127589. Jun 12;2020.06.10.20127589. (Preprint) [DOI] [Google Scholar]
- White House . White House; Washington (DC): 2020. Opening up America Again.https://www.whitehouse.gov/openingamerica/ (Accessed on September 2, 2020) [Google Scholar]
- Wrighton M.S., Lawrence S.J. Reopening colleges and universities during the COVID-19 pandemic. Ann. Intern. Med. 2020;2:M20–4752. doi: 10.7326/M20-4752. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Hussain S., Lu G., et al. 2020. Associations of Stay-At-Home Order and Face-Masking Recommendation With Trends in Daily New Cases and Deaths of Laboratory-Confirmed COVID-19 in the United States. medRxiv. Jun 29;2020.05.01.20088237. (Preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Ghader S., Pack M., et al. An interactive COVID-19 mobility impact and social distancing analysis platform. medRxiv. 2020 doi: 10.1101/2020.04.29.20085472. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material