Abstract
Consistent gathering of immunotoxic substances on earth is a serious global issue affecting people under pathogenic stress. Organophosphates are among such hazardous compounds that are ubiquitous in nature. They fuel oxidative stress to impair antiviral immune response in living entities. Aside, organophosphates promote cytokine burst and pyroptosis in broncho-alveolar chambers leading to severe respiratory ailments. At present, we witness COVID-19 outbreak caused by SARS-CoV-2. Infection triggers cytokine storm coupled with inflammatory manifestations and pulmonary disorders in patients. Since organophosphate-exposure promotes necroinflammation and respiratory troubles hence during current pandemic situation, additional exposure to such chemicals can exacerbate inflammatory outcome and pulmonary maladies in patients, or pre-exposure to organophosphates might turn-out to be a risk factor for compromised immunity. Fortunately, antioxidants alleviate organophosphate-induced immunosuppression and hence under co-exposure circumstances, dietary intake of antioxidants would be beneficial to boost immunity against SARS-CoV-2 infection.
Keywords: Organophosphate, Oxidative stress, SARS-CoV-2, COVID-19, Antioxidants
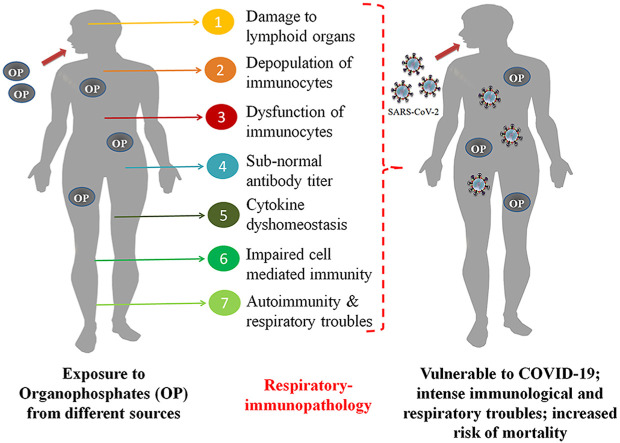
Graphical abstract
1. Introduction
With the advancement of scientific revolution, human beings have made the existing anthropocene more comfortable for their daily life. From agricultural field to the industrial sector, human populations are blessed with the use of modern technologies and equipments, which not only reduce energy for production but also enhance yield at the same time. But the darker side of such advancement includes consistent gathering of detrimental chemicals in the environment contaminating almost every component of biosphere. These chemicals have secured their apparent presence in several drugs, food stuffs, household products, drinking water, agrochemicals and so on. Organophosphates (OPs) are among such hazardous compounds that are being globally used on a regular basis.
OPs are amides, esters, or thiol derivatives of phosphoric acid. These chemicals are extensively used in agriculture, horticulture, forestry, veterinary-medicine, domestic purpose and also for the control of vector-borne diseases. Certain OPs are being used to treat head-lice, scabies and crab-lice in humans (Idriss and Levitt, 2009). In agricultural sector, OPs are extensively applied to eradicate pests including locusts, aphids, leaf miners, fire ants, thrips and caterpillars. These pesticides augment both quantity and quality of agricultural products (Chang et al., 2017). OPs namely tris-(2-chloro, 1-methyl-ethyl) phosphate, tris-(2-chloroethyl) phosphate, tri-n-butyl phosphate, tri-iso-butyl phosphate, triphenylphosphate and tris-(butoxyethyl) phosphate are admired flame retardants and plasticisers at public places (Andresen et al., 2004).
Due to overuse, OP-residues have contaminated drinking water, grains, vegetables, fruits, soft drinks and other food items and hence, it provokes a global health concern (Bala et al., 2017). Unfortunately, traces of OPs are reported in human breast milk that can be perilous to new born infants (Srivastava et al., 2011; Sanghi et al., 2003). Basically, these chemicals block the activity of acetylcholine esterase at synapse leading to disproportionate accrue of neurotransmitter, acetylcholine (Abou-Donia, 2003). Such event drives paralysis and finally death of target organism. Moreover, recent investigations have linked OPs to a nexus of biological responses mediating severe toxic-outcomes (Mandi et al., 2020; Rajak et al., 2018). Adequate studies have suggested the “immunotoxic” potential of OP compounds in human and non-target organisms (Mitra et al., 2019; Noworyta-Głowacka et al., 2012; Oostingh et al., 2009) that might increase the risk of infectious diseases.
Biotransformation of xenobiotics is an integral component of body's detoxification system. Cytochrome (CYP) P450 gene families are major determinants of biotransformation of OPs and other pesticides (Kaur et al., 2017). Genetic polymorphism in CYPs is known to alter the metabolic pathways, induce false cellular response and may provoke false pathological response (Docea et al., 2017). Thus, individual with genetic polymorphism in CYP genes must face less elimination of OP pesticides from the body. CYP polymorphism has been considered as an important risk factor for various pathological conditions induced by chronic organochlorine exposure (Docea et al., 2017). Racial disparity in mortality due to COVID-19 has been reported in the United States, where the mortality rate is 3.6 times higher in African-American population compared to other ethnic individuals (Parpia et al., 2020). It is well known that, CYP2B6 genetic polymorphism is prevalent in African population in comparison to Asian or Caucacian population (Rajman et al., 2017; Bains, 2013). Thus, it can be assumed that, the gene-environment interaction between CYPs and OP exposure might induce oxidative stress (OS) and increase the susceptibility towards SARS-CoV-2 infection through immune suppression. Pesticides like organochlorines impair cellular and humoral immunity that can further augment mortality by infectious diseases (Hayashi et al., 2013; Fournier et al., 1998). Intoxication with cypermethrin impedes antibody forming ability of B-lymphocytes and cell mediated immune responses (Tamang et al., 1998) that may disrupt anti-SARS-CoV-2 defense reactions. Exposure to carbamates is followed by hypersensitivity reactions, autoimmune diseases and even cancers. They often invite immunopathology by inducing mutations in genes encoding for immunoregulatory factors and modifying immune tolerance (Dhouib et al., 2016). Short term exposure to atrazine, a widely used herbicide decreases thymic and spleenic cellularity coupled with subverted native T-helper and cytotoxic T-cells (CTL). It is important to note that, immunotoxic impacts of atrazine can persist for longer duration even after termination of the exposure (Filipov et al., 2005).
OP pesticides are not ideal because they lack target-specificity and often fuel health hazards including immunotoxicity in humans. Nevertheless, agricultural uses of OP pesticides are gaining popularity and they account for more than 30% of global insecticide sales. It is to be noted that, the global market of OP pesticide is expected to exhibit a compound annual growth rate of 5.5% during the forecast period 2018–2023 (https://www.mordorintelligence.com/industry-reports/organophosphate-pesticides-market) and this could enhance human-OP encounter during the current pandemic situation. Unfortunately in many of the developing countries, OPs are being indiscriminately used in agriculture that could further amplify unintentional exposure to these compounds and suppress immunity against viral infections including SARS-CoV-2.
At present, world is struggling to overwhelm outbreak of coronavirus disease-19 (COVID-19) caused by SARS-CoV-2. The disease was first identified in Wuhan of Hubei province, China in December 2019 and acquired the status of pandemic in a brief span of time. Coronavirus-outbreak has marked its footprint on 213 countries and caused more than 1,868,622 fatalities as of January 7, 2021 all over the world (https://covid19.who.int/). The outbreak was declared a Global Sanitary Emergency by World Health Organization (WHO) on January 30, 2020 (WHO, 2020a) and later as a pandemic on March 11, 2020 (WHO, 2020b). Fortunately, scientific community of the planet has had promptly targeted their goals to understand epidemiology, infection-strategies, transmission-dynamics, risk-factors as well as identification of etiological agents of the infection.
To curb SARS-CoV-2 infection, a healthy immune system is obligatory despite of potent vaccine to alleviate morbidities in patients. But unintentional exposure to OP compounds from several sources can rupture the antiviral defense against SARS-CoV-2. Moreover respiratory ailments may also be fueled by OP compounds. Hence, SARS-CoV-2 mediated morbidities and fatalities could be backed by unintentional exposure to OPs in patients.
Current article will cover structure, transmission-pattern and respiratory-immunopathologies of SARS-CoV-2 in infected patients. In addition, immunotoxic impacts of wide-spread OP compounds on human and animal models will also be enumerated citing major in vivo and in vitro findings. At the end, immunoprotective nature of certain antioxidants will be discussed. These antioxidants would be beneficial in mitigating pathologies that may arise following co-exposure to SARS-CoV-2 and OP compounds.
2. SARS-CoV-2: structure & cell-invasion
SARS-CoV-2 virions are spherical, 50–200 nm in diameter and bears polycistronic (+)ssRNA (29,881bp encoding ~9860 amino acids) as the genetic material (Chen et al., 2020). Genome of the virus harbors 11 open reading frames encoding several non-structural (NSP), structural (S, E, M, N) and accessory-proteins (Chan et al., 2020). N protein provides stability to the genomic RNA. It also antagonizes interferon (IFN) response and RNA-silencing in host cell (Cui et al., 2015). M glycoprotein is the most abundant envelope protein that helps to maintain spherical morphology of virion (Neuman et al., 2011). E protein is involved in viral assembly, release and pathogenesis (Nieto-Torres et al., 2014). S (Spike) protein assembles into trimer on virion surface to obtain a distinctive “corona” or crown-like appearance (Wrapp et al., 2020). S protein is comprised of trimeric S1 heads sitting on the top of trimeric S2 stalk. S1 contains a receptor-binding-domain (RBD) that strongly recognizes host angiotensin converting enzyme-2 (ACE-2) receptors. RBD constantly switches between a standing-up position for receptor binding and a lying down position for immune evasion (Shang et al., 2020). S2 harbors a fusion peptide (FP; 5–25 amino acids) and two heptad-repeat (HR1 & HR2) regions involved in fusagenic events between viral envelope and host cell membrane (Henning and Pillat, 2020). S1/S2 interface contains a proprotein convertase (PPC) motif that needs to be activated by proteases for effective entry into host cell (Shang et al., 2020).
Cell invasion by virions is governed by precise interaction between S proteins and ACE-2 receptors on host cell surface. SARS-CoV-2 may also interact with CD147 receptor to invade the target cell (Henning and Pillat, 2020). Binding of S1 to the ACE-2 receptor promotes proteolytic activation of PPC motif at S1/S2 interface via cumulative action of surface proteases such as TMPRSS2 and furin (Hoffmann et al., 2020; Hasan et al., 2020). Such proteolytic activation invokes a conformational change in S2 exposing FP. Hydrophobic amino acid residues of FP insert themselves into the host cell membrane to acquire a hairpin-loop confirmation. Following the event, both HR1 and HR2 domains fold via their hydrophobic grooves into an antiparellel 6-helical bundle to make a stable fusion core (Xia et al., 2020). These key steps pull down the viral membrane in close proximity of host cell membrane to mediate viral-host cell fusion and transfer of genomic RNA therein. Within cytosolic moiety, SARS-CoV-2 virions are replicated, packaged and thereafter exocytosed out of the cell to infect the fresh one (Fig. 1 ).
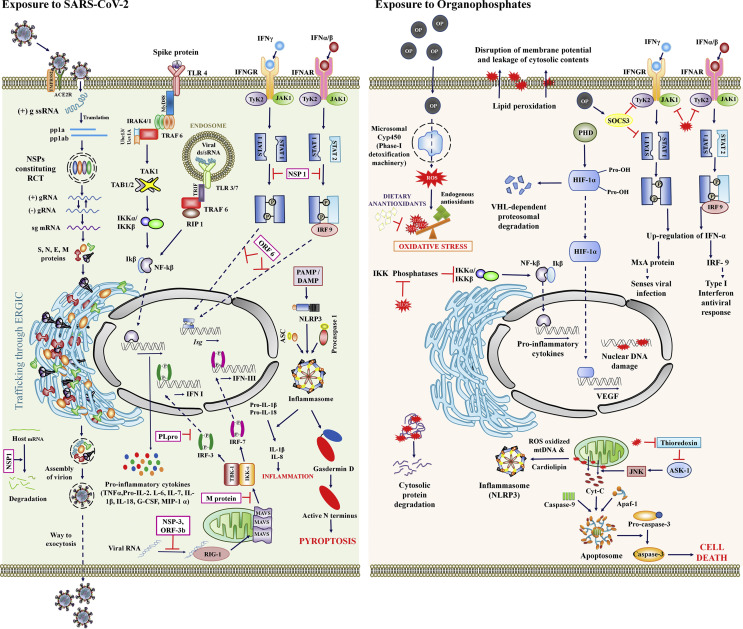
Fig. 1.
Putative immunotoxic mechanism of SARS-CoV-2 and OPs at sub-cellular moiety.
Exposure to SARS-CoV-2 (left panel): SARS-CoV-2 invades host cell via S1/ACE-2 interaction and replicates using replication transcription complex (RCT) within the cytosolic moiety. S1 of spike protein or viral ds/sRNA binds with respective cell surface or endosomal Toll-like receptor (TLR) to fuel downstream signaling cascades involved in activation of NF-kB and synthesis of proinflammatory cytokines. Pathogen associated molecular patterns (PAMPs) and damage associated molecular patterns (DAMPs) are recognized by NLRP3 to induce pyroptosis of infected cells. Several viral proteins viz. NSP1, NSP3, ORF3b, ORF6 and PL-pro target JAK/STAT and RIG-1 pathways to dwarf interferon (IFN)-mediated anti-viral immune response. M protein blocks mitochondrial antiviral signaling protein (MAVS)-dependent activation of kinases to down-regulate IFN production. NSP1 also degrades various host mRNAs, some of them may be crucial for immune reaction against SARS-CoV-2.
Exposure to OP (right panel): Being lipophilic in nature, OP crosses cell membrane and passes through phase-I detoxification machinery to generate massive reactive oxygen species (ROS). Excess ROS and subsequent oxidative stress is the major driver of immunotoxicity. ROS inhibits phosphatases to enhance production of pro-inflammatory cytokines. ROS also stabilizes hypoxia-inducible factor 1-alpha (HIF-1α) by oxidizing prolyl-hydroxylase (PHD) to transcribe vascular endothelial growth factor (VEGF) involved in airway inflammation, airway hyper-responsiveness and lymphocyte dysfunction. ROS induced lipid peroxidation, protein degradation and DNA damage simultaneously trigger necroinflammation. OP activates suppressor of cytokine signaling-3 (SOCS3) to disrupt JAK/STAT mediated anti-viral immune response. Disruption of mitochondrial boundary is promoted by apoptosis signal regulating kinase 1 (ASK-1) which remains inactive as long as it is bound to thioredoxin. ROS oxidizes thioredoxin to encourage apoptosome or inflammasome mediated cellular demise.
3. SARS-CoV-2 & immune response
In the present pandemic milieu, our immune-system provides best defense against the coronavirus infection. SARS-CoV-2 stimulates various components of innate and adaptive immunity that are involved in clearance of viral particles out of the body.
3.1. Innate immune response
Innate immunity constitutes the first line of defense against viral infections. Population of immunocytes of myeloid lineage tends to increase during COVID-19. In a study of 61 COVID-19 patients, blood neutrophil count and neutrophil to lymphocyte ratio were significantly higher in severe cases (Liu et al., 2020). In another study, remarkably higher proportions of activated mast cells and neutrophils were observed in the bronchoalveolar lavage fluid (BALF) of COVID-19 patients indicating active participation of these immunocytes against SARS-CoV-2 (Zhou et al., 2020c). Complement system plays crucial role in innate defense against wide spectrum of pathogens. Gao et al. (2020) have demonstrated that, serum level of complement proteins increases in severe COVID-19 patients compared to mild cases and healthy controls. Additionally, an enrichment in gene expression associated with complement activation and the classical pathway has been observed in infected patients (Xiong et al., 2020). Interferons (IFNs) are signaling molecules produced in response to viral infection to exert strong anti-viral immune response. Unfortunately, SARS-CoV-2 infection dampens the IFN synthesis that could rupture innate defense system (Acharya et al., 2020). Concurrently, SARS-CoV-2 infection triggers profound synthesis of proinflammatory cytokines to execute cytokine storm and pyroptosis. Excessive secretion of proinflammatory chemokines namely IL-1β, IL-2, IL-6, IL-7, G-CSF, IP-10, MCP-1, MIP-1, TNFα and IL1RA hyper-stimulates the innate defense that could exaggerate immunopathologies by several folds in COVID-19 patients. (Blanco-Melo et al., 2020; Chu et al., 2020; Huang et al., 2020).
Considering the above facts, it can be speculated that, myeloid cells and complement system play major role to restrict SARS-CoV-2 infection. However, suppressed/delayed IFN-response can dampen early viral control leading to massive efflux of proinflammatory cytokines. Such detrimental consequences promote respiratory illness including pneumonia, bronchitis and acute respiratory distress syndrome (ARDS). Hence, healthy innate immune response is vital to restrain SARS-CoV-2 mediated disease progression.
3.2. Adaptive immune responses
Transition from innate to adaptive immune response is important for clinical progression of coronavirus-infection. T-lymphocytes orchestrate the adaptive immune responses involved in clearance of virally infected cells. NK cells, INF-γ-secreting T-cells and Spike RBD-specific T-cells govern cell mediated immune response against SARS-CoV-2 infection (Ni et al., 2020). Healthy population of cytotoxic CD8-cells is required to eliminate virally infected cells out of the body (Li et al., 2020a). Reduced activation of B-cells and dendritic cells (DCs) are implicated in disease progression and pathological outcome in patients (Wang et al., 2020). Antibody mediated immune response is essential for recovery from COVID-19. Nucleocapsid protein (NP)-specific antibody response was reported in infected patients suggesting their active participation in humoral immune response (Zhou et al., 2020a). Ni et al. (2020) detected the presence of NP- and spike RBD-specific IgM & IgG1 antibodies in sera of newly discharged patients. Preclinical studies with anti-SARS vaccines have detected the presence of neutralizing IgA antibodies in bronchoalveolar lavages (Lu et al., 2010). IgG antibodies are traceable following onset of symptoms (Long et al., 2020).
Hence, the above studies advocate that, healthy population of various immune cells and antibodies are indispensable to eliminate SARS-CoV-2 infection. Injured humoral and cell-mediated immunity can invite disease severity, respiratory immunopathology (Fig. 2 ) and fatal outcome in patients with COVID-19.
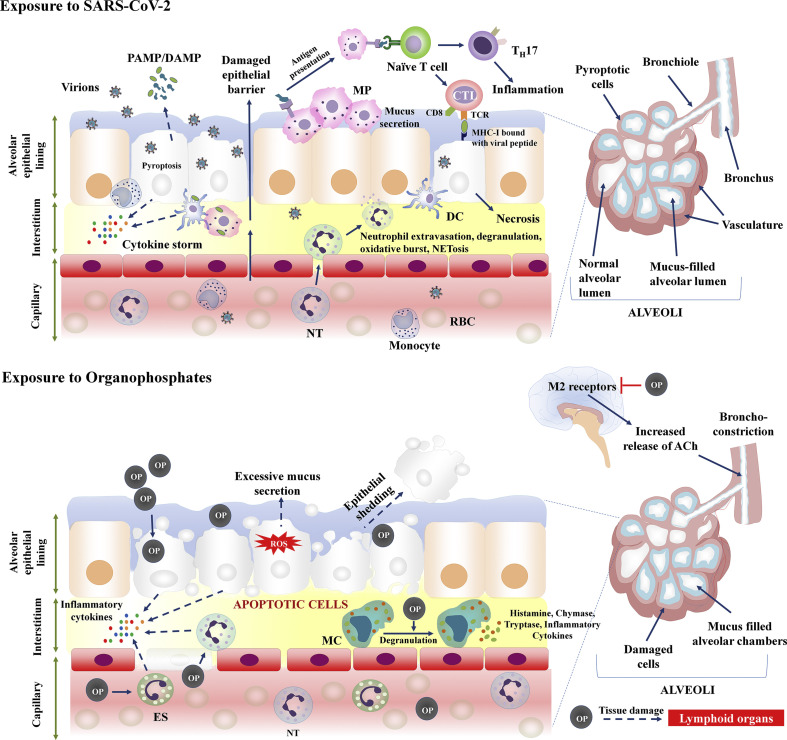
Fig. 2.
Modulation of broncho-alveolar architecture by SARS-CoV-2 and OPs in host.
Exposure to SARS-CoV-2 (upper panel): Viral components fuel necroinflammation of broncho-alveolar cells. PAMPs/DAMPs stimulate macrophages and DCs to release cytokines driving inflammation at respiratory sites. Pyroptosis damages cellular lining and disrupts the epithelial barrier leading to leakage of fluid/mucus at inner faces of broncho-alveolar chambers. This reduces the volume of alveolar-lumen required for oxygen absorption. SARS-CoV-2 invasion attracts neutrophil (NT) extravasation, degranulation of cytosolic contents (HBP, elastase, cathepsins, azurocidin, collagenase, gelatinase) and NETosis to amplify respiratory troubles. Macrophages present viral antigens to naive T-cells of mucosa associated lymphoid tissues. Activated naive T-cells differentiate into CTL and TH17 to exaggerated inflammation and cytotoxicity.
Exposure to OP (lower panel): OP induced ROS and subsequent oxidative stress triggers multiple apoptotic cascades to scrape lung epithelium. Shedding of damaged cells disrupts epithelial barrier. Alongside, OP insists degranulation of mast cells (MCs) to release histamine. Histamine induces goblet cells to secrete excessive mucus in alveolar cups. These events reduce the alveolar-volume interfering with O2 absorption. Additionally, OP contamination invites infiltration of neutrophil and eosinophil (ES) to exert necroinflammation. OP inhibits M2-receptor in brain leading to elevated levels of acetylcholine (ACh). ACh mediates hyper broncho-constriction and dyspnea in human. OP also ignites tissue damage in lymphoid organs, hence may depress immune response against SARS-CoV-2.
4. OP-induced immunotoxicity
Immunotoxicity is defined as an adverse effect on integral components of immune system resulting in immunosuppression or exaggerated immune responses. Immunotoxicity can augment the incidences of being virally infected and/hyper-stimulate the immune components to target body's own healthy tissues. Current evidences have classified these effects into three broad categories namely direct immunotoxicity, hypersensitivity and autoimmunity. OP compounds are potential modulators of immune system. Adequate volume of in vitro (Table 1 ), in vivo (Table 2 ) and direct evidences on human (Table 3 ) have unfolded the immunotoxic feature of OPs and their metabolites. Documented immunotoxicity as imposed by OP compounds on cell culture setups, animal models and human includes the following:
Table 1.
Immunotoxic impacts of organophosphates: In vitro studies.
| Organophosphate tested | Cell type | Immunotoxic Outcome | Reference (s) |
|---|---|---|---|
| Malathion, Chlorpyrifos and Diazinon | Lymphocytes | Increased reactive oxygen species (ROS) and lipid peroxidation in lymphocytes; higher DNA damage; decreased lymphocyte viability; reduced cell proliferation and apoptosis in splenocytes; reduced activity of macrophage lysosomal enzyme and increased production of IL-1β, TNFα and nitric oxide. | Olakkaran et al. (2020); Helali et al. (2016); Battaglia et al. (2010) |
| OP flame retardants: Triphenyl phosphate, Tris (1,3-dichloropropan-2-yl) phosphate, Tributyl phosphate, Tris (2-methylphenyl) phosphate, Tris (2-chloroethyl) phosphate, Tris (2-butoxyethyl) phosphate | Human monocytic leukemia cell line | Reduced cell viability and adhesion property; reduced production of anti-inflammatory cytokines (IL-10 and IL-13) and increased production of proinflammatory cytokines (TNF-α). | Li et al. (2020) |
| Methoxychlor | Murine mast cells | Increased degranulation of mast cells via induction of FcεRI-mediated signal transduction. | Yasunaga et al. (2015) |
| Dimethoate and Chlorpyrifos | Human acute monocytic leukemia cell line THP-1 | Damaged dendrites of dendritic cells; up-regulation of pro- inflammatory cytokines such as IL-1β and IL-8; declined level of protein kinases responsible for cell survival and proliferation. | Schäfer et al. (2013) |
| Diethyldithiophosphate, | Human CD4+ T-lymphocytes | Reduced antigen-induced CD4+ and CD8+ T-cell proliferation; decreased CD25 expression; reduced intracellular secretion of IL-2, IL-10 and IFN-γ. | Esquivel-Sentíes et al. (2010) |
| Chlorpyrifos-oxon | Human blood cultures | Higher levels of pro-inflammatory IFN-γ. | Duramad et al. (2006) |
| Dimethyl 2,2-dichlorovinyl phosphate | NK-92CI cell (an interleukin-2 independent human NK cell line) | Suppressed expression of perforin, granzyme A and granulysin. | Iyer et al. (2017) |
| Dimethyl 2,2-dichlorovinyl phosphate | Human and murine cell lines for NK cells, cytotoxic T lymphocyte (CTL) and lymphokine-activated killer (LAK) cells | Reduced NK, LAK and CTL activities in a dose-dependent manner; significant decrease in granzyme activity. | Tang et al. (2003) |
Table 2.
Immunotoxic impacts of organophosphates: In vivo studies.
| Organophosphate tested | Dose & duration of exposure | Model animal | Immunotoxic outcome | Reference |
|---|---|---|---|---|
| Fenitrothion | 20 mg/kg b.w./day; 30 days |
Male rats | Increased serum levels of TNF-α and IL-2; reduced IgG and IgM antibody titer. | Alam et al. (2019) |
| Chlorpyrifos | 75 mg/L; 3–9 weeks |
Male rats | Significant decrement in macrophage activity, serum lysozyme activity and levels of IL-2 & IL-6; OP-induced oxidative stress and DNA damage in treated lymphocytes. |
Essa et al. (2019) |
| Ethephon | 1995 ppm (1/10th of the oral LD50); 8 weeks |
Mice | Impaired antibody titer and humoral immunity; declined phagocytic activity of polymorphonuclear cells. | Abou-Zeid et al. (2018) |
| Malathion and Parathion methyl | 0.01 LD50 daily (815 ± 28 mg/kg malathion; 25.3 ± 2.6 mg/kg parathion methyl); 30 days |
Albino rats | Reduced activity of neutrophils and NK cells; impaired antibody-dependent cellular cytotoxicity. | Zabrodskii (2018) |
| Diazinon | 10 mg/kg; 30 days |
Male albino rats | Reduced population of lymphocytes and monocytes; sub-optimum level of total serum immunoglobulin titer and hemagglutination; declined blood mononuclear cell proliferation, phagocytic index and blood T-cell subtypes (CD4+ and CD8+). | Hassouna et al. (2015) |
| Chlorpyrifos and Profenofos | Chlorpyrifos: 6.75 mg/kg b.w. Profenofos: 20 mg/kg b.w.; 60 days |
Male rats | Significant increase of TNF-α; reduced levels of IgG and IgM. | Hamza et al. (2013) |
| Parathion | 0.015, 0.15 and 1.5 mg/kg/day; 5 days |
Mice | Decreased production of SRBC-specific IgM antibodies; declined expression of surface antigens in IgM- and germinal center-positive B-cells. | Fukuyama et al. (2011) |
| Phosphamidon | 0.174–1.74 mg/kg b.w.; 28 days |
Male albino rat | Decreased serum antibody titre; significant reduction in leukocyte and macrophage migration. | Suke et al. (2006) |
| Monocrotophos | 0.025 mg/kg b.w.; 6 months |
Sheep | Reduced production of serum globulins and γ globulins and specific Brucella antibodies. | Khurana, & Chauhan (2003) |
| Acephate | 100–500 mg/kg b.w,; 5 min to 24 h |
Female Wistar rats | Low CD4, CD8, B-cell and monocyte contents. | Singh & Jiang (2003) |
| Dimethoate | 7.04–28.2 mg/kg b. w.; 28 days |
Male Wistar rats | Decreased IgM-plaque forming cell content and delayed-type hypersensitivity reaction. | Ȕ;ndeger et al., 2000 |
Table 3.
Effect of organophosphate-exposure on immune health of human.
| Compound | Mode of exposure | Duration of exposure | Immunogenic effects | Reference |
|---|---|---|---|---|
| OP pesticides | Occupational (200 agriculture spray workers) | Chronic | Altered IgE, IgA and IgM in spray workers. | Riaz et al. (2017) |
| Triazophos and acephate | Occupational (71 workers in a unit manufacturing triazophos and acephate) | Chronic | Elevated level of serum IgM compared to control. | Zaidi et al. (2015) |
| Insecticides containing OP and Carbamate | Occupational (55 pesticide sprayers) | Chronic | Significantly reduced antioxidant defense enzymes, IgM and IgG; Up-regulated MDA and TNF levels in exposed group. | Mecdad et al. (2011) |
| Pesticides containing OP | Occupational (64 greenhouse workers) | Chronic | Increased IL-22 concentration and decreased immunocompetence in exposed workers. | Fenga et al. (2014) |
| OP pesticides | Occupational (84 Farm workers) | 1–3 month of exposure | Increased lymphocyte count in farm workers compared with their control counterparts. | Andreadis et al. (2013) |
| OP pesticides | Occupational (20 Workers in pesticide industries) | Chronic | Increased percentage of CD8, decreased CD56, CD4/CD8 ratio and elevated level of IgG. | Osely & Sh (2010) |
| OP agents | Environmental | Chronic exposure | Elevated T-helper 1 (Th1) and T-helper 2 (Th2) cytokines in serum; detected with asthma and wheeze problems. | Duramad et al. (2006) |
| Byproducts of sarin (DIMP and DEMP) | Accidental | Acute exposure | Decreased NK and CTL activity. | Li et al. (2004) |
| Pesticides containing OP | Occupational (304 pesticide applicators in the agricultural farms) | Chronic exposure | Reduced levels of IgM and C4; elevated levels of Neopterin and soluble tumor necrosis factor receptor (sTNF RII); compromised humoral defense system. | Stiller-Winkler et al. (1999) |
| Chlorpyrifos | Environmental | Chronic exposure | Elevated CD26 cells and a higher rate of autoimmunity in exposed groups. | Thrasher et al. (1993) |
| OP pesticides | Occupational (85 individuals working at organophosphate manufacturing unit) | Chronic exposure | Impaired neutrophil chemotaxis, higher upper respiratory tract infection | Hermanowicz & Kossman (1984) |
4.1. Structural damage to lymphoid organs
Immune system is comprised of distinct lymphoid organs that support development, maturation and function of immunocytes. These organs are classified into primary and secondary lymphoid organs. Primary lymphoid organs include red bone marrow and thymus where production, clonal selection and maturation of lymphocytes occur whereas secondary lymphoid tissues such as spleen, lymph nodes, Peyer's patches and mucosa associated lymphoid tissue (MALT) provide space for lymphocyte-antigen interaction. Therefore, these organs can determine the cumulative status of immune health in human and other animals.
Numerous studies have revealed the toxic outcome of OP exposure on lymphoid organs. For instance, dimethoate was reported to reduce thymic cortex and damage thymocytes in rodents (Tiefenbach and Lange, 1980). Handy et al. (2002) monitored the impact of diazinon-exposure on rodent lymphoid tissues. Study indicated that, diazinon promotes necrosis in trabeculae of spleen and thymus coupled with hyperplasia of cortical-medullary zones of lymph nodes. Aside, hyperplasia in red and white-pulp of spleen was also noticed. Intraperitoneal administration of diazinon inflicted atrophy in thymus and spleen with suppressed splenocyte proliferation in C57bl/6 female mice (Neishabouri, 2004). Malathion reduces weight and cellularity of major lymphoid organs in rodents (Ramadan et al., 2017). In a separate study, malathion was responsible for degeneration of spleenic lymphatic follicles and bone marrow cells in juvenile male rats (Ahmed, 2012). Intoxication with other OPs like azamethiphos, chlorfenvinphos, chlorpyrifos-oxon, diazinon-oxon, dichlorvos and malaoxon promotes thymic protein adduction to render functional impairment (Carter et al., 2007). Shahzad et al. (2015) through their study reported chlorpyrifos induced disorganization of follicular patterns, severe congestion, cytoplasmic vacuolation, degeneration and hyperplasia of spleenic reticular cell whereas necrosis in thymic myoid cell. Swiss albino mice exposed to aqueous mixture of profenofos and chloropyrofos for 13 weeks manifested distortion in bone marrow architecture characterized by deformed stromal matrix and stromal cells. Moreover, a quantitative depression in the primitive bone marrow stem cells was evident following OP insult (Chatterjee et al., 2014).
4.2. Reduced viability and proliferation of immunocytes
Immunocytes are the specialized cells that cater inevitable support to cell mediated and humoral immunity against a wide spectrum of microbial pathogen. These cells include lymphocytes (T-cells, B-cells and NK cells), neutrophils, monocytes/macrophages, DCs and mast cells. T cells are produced from hematopoietic stem cells of bone marrow and undergo selection process with maturation in thymus. Major subtypes of these cells include cytotoxic T-cells (CD8+), helper T cells (CD4+) and regulatory T-cells each having distinct function. Cytotoxic T-cells perform the actual destruction of infected cells whereas helper T-cells assist B lymphocytes to produce antibodies. Regulatory T-cells control the immune response by other lymphocytes. NK cells have their origin in bone marrow and destroy virally infected cells. B-cells are produced and matured in bone marrow and after maturation they populate bone marrow itself, lymph nodes and spleen. Neutrophils and monocytes/macrophages are phagocytes that engulf microorganisms. DCs are antigen-presenting cells that function to process antigenic material and display them to cell surface for presentation to T-lymphocytes therefore acting as a connecting bridge between innate and adaptive immune systems. Mast cells are immunocytes of the myeloid lineage and regulate immune response via degranulation of cytosolic contents like histamine and heparin.
Studies across the world have explored the impact of OPs on survival, development, maturation and proliferation of immunocytes. Liu et al. (2018) have revealed that, exposure to fenitrothion lowers splenic-titer of CD3+, CD4+and CD8+ murine T-cells coupled with increased level of lipid peroxidation and hydroxyl radical. Sonu et al. (2017) analyzed immunotoxic potential of dimethoate on avian lymphocytes. They observed that, dimethoate markedly reduces B and T-lymphocyte proliferation and fuels OS. In an in vitro setting, chlorpyrifos, methyl parathion and malathion have been found to provoke OS and DNA breaks in peripheral blood lymphocytes rendering detrimental impact to immune cells (Ojha and Srivastava, 2014). OFR namely O,O-5- trimethylphosphorothioate impedes CTL production and proliferation (Descotes, 1988). Bagchi et al. (1995) have reported the anti-proliferative effect of chlorpyrifos on T and B-lymphocytes. Intraperitoneal injection of acephate down-regulates the serum CD4, CD8, B-cell and monocyte contents in rodents (Singh and Jiang, 2003). Nain et al. (2011) investigated the effect of malathion on immune system of Japanese quail. They observed bursal atrophy and reduced B-cell density in OP treated birds. Experiment by Gallicchio et al. (1987) showed that, primary metabolites of parathion and malathion generate dose dependent depression in colony formation by granulocyte-macrophage progenitor cells of bone marrow leading to subverted population of active immune cells. In a case study, individuals dealing with chlorpyrifos were reported to have reduced population of CD5+ lymphocytes in their blood samples (Thrasher et al., 1993, 2002). Sub-chronic exposure of the male swiss albino mouse to recommended field dose of thimet (phorate) caused significant decrease in lymphocyte content (Morowati et al., 1997). Similarly, Lima and Vega (2005) reported that, exposure to methyl parathion reduces proliferation of human peripheral blood mononuclear cells.
4.3. Altered activity of immunocytes
Immunocytes have their distinct function to orchestrate cell mediated and humoral immune responses against numerous microbial pathogens including SARS-CoV-2. Nevertheless, studies have fueled global concern regarding the modulation of anti-viral immunity by OP compounds.
Study by Rodgers and Xiong (1997) have revealed that, repeated administration of malathion alters macrophage function and mast cell degranulation in mice. Similarly, exposure to dimethyl 2,2-dichlorovinyl phosphate reduces activity of natural killer (NK) cells, lymphokine-activated killer (LAK) cells and CTL in a dose-dependent manner (Tang et al., 2003). Other OP compounds for instance, triphenylphosphine oxide and tetra-o-cresylpiperazinyl diphosphoamidate hinder monocyte mediated antigen presentation and lymphocyte proliferation in human mononuclear cells (Esa et al., 1988). In a study, Hermanowicz and Kossman (1984) analyzed neutrophil function and prevalence of infections in 85 workers exposed to phosphoorganic pesticides. They observed reduced neutrophil-chemotaxis and adhesion properties in these workers compared to unexposed group. In addition, upper respiratory-tract infection was frequent in exposed workers. In another study, treatment with difenphos and glyphosate suppressed proliferative response of splenocytes towards mitogens; phytohemagglutinin (PHA) and concanavalin A (Con A) in Tilapia nilotica pointing towards injured cell mediated immunity (el-Gendy et al., 1998). Exposure to monocrotophos reduces active splenic macrophages in broiler chicks (Garg et al., 2004). Administration of chlorpyrifos to rats at a dose of 5.0 mg/kg for 28 days suppressed humoral immune response and T-lymphocyte blastogenesis induced by concanavalin A and phytohemagglutinin (Blakley et al., 1999). In vitro exposure of diazinon reduces phagocytic activity of macrophage-like RAW264.7 cells (Ogasawara et al., 2017). Neutrophil function in 40 workers occupationally exposed to OP pesticides was disrupted to some extent (Queiroz et al., 1999). Zabrodskii (2018) found that, chronic intoxication of rats with malathion and parathion methyl (0.01 LD50 daily, for 30 days) significantly reduces the phagocytic-metabolic activity of neutrophils and NK cells. Li et al. (2020b) have reported that, Triphenyl phosphate and Tris (2-butoxyethyl) phosphate partially attenuate the adhesion and phagocytic potential of the THP-1 mϕs. In the same study, Tris (1,3-dichloropropan-2-yl) phosphate was documented to catalyze functional loss of macrophages. Viability of DCs and expression of MHC class II molecules have been down-regulated following Triphenylphosphate and Tris (1,3-dichloroisopropyl) phosphate exposure (Canbaz et al., 2017). Moreover, Tris (1,3-dichloropropan-2-yl) phosphate promotes functional loss of Human THP-1 derived macrophages.
4.4. Sub-normal antibody titer
Healthy antibody titer is essential to curb SARS-CoV-2 infections. Certain OP compounds are responsible for low antibody titer (Li et al., 2000; Fautz and Miltenburger, 1994) and hence can potentially augment the risk for viral infections including COVID-19. Suke et al. (2006) treated albino rats with phosphamidon and measured low serum antibody titer and macrophage migration. In another study, reduced level of IgG plaque forming cells was reported in inbred mice exposed to parathion (Casale et al., 1984). Malathion at noncholinergic doses suppressed generation of rodent IgM and IgG antibodies against sheep red blood cell (SRBC) (Rodgers et al., 1996). A recent study has demonstrated the impaired Th-2 lymphocyte function and IgG production in albino rats acutely intoxicated with malathion (Zabrodskii, 2019). Abou-Zeid et al. (2018) have revealed that, plant growth regulator ethephon decreases serum hemolyzing antibody and immunoglobulin (IgG and IgM) contents against SRBC in mice. 55 workers spraying OP chemicals in agricultural farms had reduced IgM and IgG in their serum indicating higher risk of receiving viral infections (Mecdad et al., 2011). Riaz et al. (2017) have reported elevated IgE titer in OP spray-workers compared to control group. The finding suggests that, exposure to OPs can aggravate allergic reactions that can be detrimental to healthy tissues. Elaimy et al. (2012) have suggested that, exposure to chlorpyrifos can potentially decline IgG level in blood. Diazinon at a dose of 10 mg/kg b.w. lowers hemagglutination titer and the total serum immunoglobulin in male Wister rats (Ibrahim, 2014).
4.5. Dyshomeostasis of cytokine response
Cytokines are endogenous low molecular weight soluble proteins that are produced in response to antigens and function as chemical messengers to drive innate and adaptive immune responses. Two major groups namely proinflammatory and anti-inflammatory cytokines orchestrate controlled immune response. Proinflammatory cytokines are activated in response to antigenic insult and provide effective defense against exogenous pathogens. Nevertheless, overproduction of these mediators fuel intense inflammatory reactions that can be detrimental to multiple organs. In contrast, anti-inflammatory cytokines down-regulate exacerbated inflammatory process and maintain cytokine homeostasis for proper functioning of vital organs. Several literatures have advocated the implication of OPs in dyshomeostasis of cytokine response in cell culture set-ups, animal models and human.
In a very recent study, Tris (2-methylphenyl) phosphate has been reported to inhibit anti-inflammatory cytokines that can disrupt cytokine balance (Li et al., 2020). Decreased immunocompetence with a relevant increase in IL-22 concentration was reported in 64 green-house workers exposed to OP pesticides (Fenga et al., 2014). Diethyldithiophosphate (DEDTP) is a metabolite formed by biotransformation of OP pesticide and has a longer half-life than its parent compound. Esquivel-Sentíes et al. (2010) showed that, human CD4+ T lymphocytes exposed to DEDTP (1–50 μM) had lower secretion of IL-2, IFN-γ and IL-10. Authors suggested that, DEDTP can modulate phosphorylation of suppressor of cytokine signaling-3 (SOCS3) which acts as negative regulator of cytokine signaling. Results from a cytokine/chemokine secretion analysis revealed the proinflammatory properties of Tris (1,3-dichloropropan-2-yl) phosphate, Triphenyl phosphate and Tris (2-butoxyethyl) phosphate (Li et al., 2020). These compounds reduce the production of anti-inflammatory cytokines (IL-10 and IL-13) and trigger the release of proinflammatory cytokine (TNF-α). In another study, exposure to chlorpyrifos suppressed production of IFN-γ, TNF-α and IL-6 following LPS stimulation in mice (Singh et al., 2013). In vitro study by Zhao et al. (2020) has claimed that, malathion can suppress the synthesis of IL-2, IFN-γ, IL-4 and granzyme-B whereas chlorpyrifos is able to decrease the production of IL-6 in splenic lymphocytes.
4.6. Suppressed delayed-type hypersensitivity reaction
Delayed-type hypersensitivity (DTH) is a reflection of cell mediated immune response. Study conducted by Moon et al. (1986) revealed that, subchronic exposure of rodents to certain OP compounds viz. fenitrothion, fenthion and diazinon resulted in marked suppression of DTH and Arthus reaction. Malathion applied epicutaneously for 2 days or over 4 weeks failed to elicit DTH in female BALBc mice pointing towards impaired cell mediated immune response (Cushman and Street, 1983). Immunotoxicological investigation by Undeger et al. (2000) using footpad swelling assay revealed that, dimethoate at a dose of 28.2 mg/kg/day reduced DTH reaction in treated rats. A dose dependent decrease in DTH was also observed following exposure to phosphamidon. Ethephon, at a dose rate of 1995 ppm suppressed DTH response to SRBC as measured by thickness of edema in hind paw in mice (Abou-Zeid et al., 2018). Similar observation was recorded following exposure to diazinon at a dose of 10 mg/kg in male Wister rats (Ibrahim, 2014). In a recent study, acute intoxication of malathion (0.5 LD50) resulted in reduced function of Th1 lymphocytes, DTH reaction and production of IFN-γ in random-bred albino rats. Monocrotophos suppresses DTH reaction, lymphocyte count and lymphocyte stimulation in sheep (Khurana and Chauhan, 2003). Low dose oral exposure to acephate can modulate humoral immune response and DTH response to SRBCs in rodents (Sankhala et al., 2012).
4.7. Autoimmune responses
There is small but evolving body of literature that advocates OP induced autoimmune responses leading to several chronic manifestations. Systemic autoimmunity is measured by anti-nuclear antibodies. OP insecticide diazinon has been positively associated with serum antinuclear antigens in occupationally exposed male farmers (Parks et al., 2019). In another finding, farmers having experience of long-term exposure to diazinon, fenitrothion, methidathion, malathion, chlorpyrifos, parathion and profenofos had elevated level of blood antinuclear antibody. Rheumatoid arthritis (RA) is a systemic autoimmune inflammatory disease. Its incidence of occurrence was higher in fonofos applicators (Meyer et al., 2017). Koureas et al. (2017) conducted a cross sectional study among pesticide sprayers dealing with chlorpyriphos, phosmet and dimethoate in Thessaly (Greece). Multinomial analysis revealed that, frequencies for RA and allergic rhinitis were significantly higher in OP pesticide sprayers compared to control group. Rheumatoid factor (RF) is the autoantibody that targets healthy tissues in the body. Rodgers (1997) has reported that, malathion administration at non-cholinergical doses can potentially increase serum RF and anti-dsDNA antibodies. Moreover, it can exacerbate progression of systemic lupus erythematosus which is an autoimmune disease with diverse clinical and immunological manifestations. Long-term exposure to dichlorvos can promote development of autoimmune hepatitis (Zhao et al., 2015). Thus, OP compounds have certain implications for autoimmunity and organ damage.
5. Mechanism of immunotoxicity: OPs versus SARS-CoV-2
People with under-performing immune system may be at high-risk of receiving SARS-CoV-2 infection. They may also remain infectious for a longer duration than others. Numerous studies have claimed that, OP induced disruption of immune system may intervene antiviral immune responses. OP compounds are the promoters of apoptosis in lymphoid organs. Studies have shown that, OP mediated cell death is triggered by increased levels of pro-apoptotic proteins (Bax and caspase 3) and reduced levels of anti-apoptotic proteins (p-Akt and Bcl2) (Venkatesan et al., 2017). Moreover, OP triggers activation of NF-κB via p53 signaling pathway that further escalates tissue damage (Lee et al., 2014) in lymphoid organs. Cellular demise in thymus, spleen and lymph nodes results in reduced titer of neutralizing antibodies against viral infection (Matter et al., 2011). Immunocytes like NK cell, LAK cell and CTL play crucial role in clearance of virally infected cells by releasing serine proteases (granzymes). OP inhibits activity of these serine proteases to impair cell mediated anti-viral functions. In addition, FasL/Fas pathway is targeted by OP compounds to hinder the activity of killer cells (Li, 2007). OPs injure dendrites of DCs more likely through inhibition of protein kinases such as Akt family or ERK which are essential for cell proliferation and survival (Schäfer et al., 2013). Pro-oxidative impact is exerted via Cytochrome P450 based ROS production. ROS can overwhelm the cellular antioxidant status to manifest OS - a major trigger to necroptosis, pyroptosis, and parthanatos in immunocytes (Robinson et al., 2019). Alongside, ROS mediated disruption of mitochondrial membrane exposes cardiolipin and mtDNA to cytosol thus provoking NLRP3 to compose inflammasome (Iyer et al., 2013). C-reactive proteins are elevated following OP exposure and higher level of this inflammatory marker can contribute to immunosuppression (Yoshida et al., 2020; Taghavian et al., 2016). IFN constitutes the first line of defense against viral infections (Ivashkiv and Donlin, 2014). Inability to mount an effective IFN-response results in systemic infection (Baskin et al., 2009). Efficiency of a virus to evade IFN-response is crucial for viral replication, transcription and onset of pathologies (Iyer et al., 2017). Virions unable to escape IFN-response, usually fail to replicate in host (Iyer et al., 2017). OP promotes IFN-depletion (Singh et al., 2013) and therefore can rupture the protective-shield against viral-attack.
Similar to OPs, SARS-CoV-2 can be detrimental to immune machinery and convergence of both can worsen the outcome of COVID-19. Virions utilize ACE-2 receptors to invade target cells. However, certain essential oils like geranium and lemon strongly reduces expression of ACE-2 in epithelial cells that can subvert viral invasion (Senthil Kumar et al., 2020). Molecular docking and molecular dynamics studies have revealed that, hesperidin can distort the bound structure of ACE-2 and spike protein fragment that could have potential anti-SARS-CoV-2 implication (Basu et al., 2020). However, many structural, non-structural and accessory proteins of SARS-CoV-2 adopt multiples strategies to modulate cytosolic interactome and subsequent immune function (Fig. 1). For instance, ORF8 down-regulates MHC-I to disrupt antigen presentation by macrophages and DCs (Park, 2020). Indeed a recent literature has demonstrated that, ORF-8 can directly bind to MHC-I molecule at endoplasmic reticulum to drive auto-lysosomal degradation (Zhang et al., 2020b, Zhang et al., 2020a). NSP5 interacts with epigenetic regulator histone deacetylase-2 to modulate MHC-II expression and cytokine production (Gordon et al., 2020). SARS-CoV-2 infection promotes subverted IFN-I synthesis in patients (Acharya et al., 2020). Such response is facilitated by coronavirus PLpro that disrupts IFN genes such as STING–TRAF3–TBK1 complex (Báez-Santos et al., 2015). In addition, other SARS-CoV-2 proteins like NSP13, NSP14, NSP15 and ORF6 have been suggested to antagonize IFN function by suppressing nuclear localization of IRF3 (Yuen et al., 2020). Notably, viral M protein interacts with RIG-1/MDA-5/MAVS signaling pathway to hinder IFN-I and IFN-III production (Zheng et al., 2020). Interestingly, certain essential oil components such as (E,E)-α-farnesene, (E,E)-farnesol and (E)-nerolidol have better binding affinity for SARS-CoV-2 proteins like Mpro and hence could be effective in preventing viral proliferation. Moreover, jensenone, an active ingredient of eucalyptus oil forms complex with proteinase (Mpro/3CLpro) that could restrain SARS-CoV-2 infection and disease severity (Sharma and Kaur, 2020). Structural analysis by cryo–electron microscopy has revealed that, NSP1 binds to and blocks the mRNA entry tunnel in 40s ribosomal subunit that might obstruct RIG-1 dependent innate immune responses (Thoms et al., 2020). SARS-CoV-2 infection injures cell mediated immunity through severe leukopenia and lymphopenia in critical cases of COVID-19 (Tan et al., 2020). Alongside, significant decrement in peripheral CD4+ and CD8+ T lymphocytes has also been diagnosed in patients as the disease progress (Liu et al., 2020). Depopulation and delayed maturation of major immunocytes like T-cells, NK cells, monocyte and DCs in COVID-19 patients are suggestive of immunotoxicity by SARS-CoV-2 (Zhou et al., 2020b). Infection fuels cytokine dyshomeostasis by promoting exaggerated synthesis of proinflammatory cytokines such as IL-2, IL-7, IL-10, G-CSF, IP-10, MCP-1, MIP-1A, and TNFα (Huang et al., 2020; Li et al., 2020). Excess cytokine production culminates into uncontrolled inflammation and autoimmunity that could be injurious to vital organs. It is worth mentioning that, eucalyptol, an active ingredient of eucalyptus oil reduces release of proinflammatory cytokines from monocytes and macrophages without halting their phagocytic properties (Juergens et al., 2020). Cinnamaldehyde bears anti-inflammatory feature as it reduces the levels of proinflammatory cytokines such as TNF-α, IL-6, IL-13 and IL-1β (Huang and Wang, 2017). Therefore, these agents could have implications against SARS-CoV-2 mediated cytokine storm. C-reactive proteins are detected in early stages of COVID-19 (Wang, 2020). Elevated C-reactive proteins could be immuno-suppressive as they inhibit proliferation, activation and function of CD4+ and CD8+ T-cells. In addition, these biopolymers can down-regulate activity of DCs (Yoshida et al., 2020). Gazzaruso et al. (2020) have detected the prevalence of autoimmune markers such as anti-nuclear autoantibodies and lupus anti-coagulant in 45 patients admitted to the hospital for SARS-CoV-2 pneumonia. Zhang et al., 2020b, Zhang et al., 2020a have reported anti-cardiolipin and anti-β2 glycoprotein-1 auto-antibodies in critically ill COVID-19 patients. Thus, onset of SARS-CoV-2 mediated auto-immune responses is confirmatory in these patients.
In summary, OP compounds are immunotoxic since they promotes apoptosis of immunocytes, lower immunoglobulin titer and autoimmune responses in organisms. Similar to OPs, SARS-CoV-2 targets immune system by modulating IFN response, lymphocyte count, cytokine homeostasis and autoimmune reaction. Hence, it is not unreasonable to claim that, co-exposure to both of the agents during the existing pandemic milieu could have altered the disease outcome of patients with COVID-19.
6. Pathohomology shared by OPs & SARS-CoV-2
Striking similarities between pathological outcome of SARS-CoV-2 and OP-exposure can be observed in human. Patients with COVID-19 have been diagnosed with multiple respiratory ailments namely pneumonitis, acute respiratory distress syndrome (ARDS), dyspnea and bronchitis (Chen et al., 2020). Similar pulmonary manifestations are also evident in subjects exposed to OPs. Epidemiological survey by Duramad et al. (2006) revealed increased incidences of asthma in children born to mothers with history of working in OP-contaminated environment. Asthmatic symptoms were also common among villagers undergone occupational exposure to OPs in rural China (Zhang et al., 2002). Valcin et al. (2007) have demonstrated that, individuals dealing with OP pesticides were more prone to develop chronic bronchitis with other respiratory maladies like asthma and emphysema. Hoppin et al. (2009) reported allergic respiratory problems in farmers dealing with OP pesticides. Moreover, OP poisoning promotes bronchoconstriction, pulmonary edema, pneumonia, rhinitis, respiratory muscle-paralysis and acute respiratory-failure posing high risk of death in human (Wang et al., 2010; Marrs, 2001; Ohayo-Mitoko et al., 2000; Deschamps et al., 1994; Senanayake and Karalliedde, 1987).
Surprisingly, certain patients with SARS-CoV-2 infection have been observed to face extra-pulmonary troubles such as cardiac, hepatic, renal, dermatological and neural malfunctions (Giacomelli et al., 2020; Klok et al., 2020; Lin et al., 2020; Mao et al., 2020; Recalcati, 2020; Shi et al., 2020). Similar multi-organ injuries have also been reported following OP-exposure. OP induces neural, cardiac, renal, gastrointestinal and retinal troubles in exposed cases (Zafar et al., 2017; Peter et al., 2014; Anand et al., 2009; Rothlein et al., 2006; Patil et al., 2003).
Thus, above findings unequivocally suggest that, additional exposure to OPs can obviously intensify inflammation, respiratory troubles and even casualties in patients with COVID-19 (Fig. 3 ).
Fig. 3.
Phenotypic outcome imposed by SARS-CoV-2 and OPs in human
SARS-CoV-2 infection produces multiple respiratory troubles namely pneumonitis, acute respiratory distress syndrome (ARDS) and acute bronchitis in patients. In addition subnormal immune status increases the risk for septic shock and secondary infections. Multi-organ failure (cardiac, gastrointestinal, kidney, hepatic, neurological, olfactory, gustatory, ocular & cutaneous) is evident in certain cases. OP-induced necroinflammation at broncho-alveolar sites is the mediator of pulmonary diseases like pneumonitis, emphysema, ARDS, Chronic obstructive pulmonary disease (COPD), bronchitis, asthma and rhinitis. In addition, cellular death in lymphoid tissues promotes immunosuppression. Multi-organ injuries (neural, cardiac, renal, gastrointestinal & retinal) are also reported following OP-exposure. Therefore, OP contamination can intensify health predicaments to several folds and modulate disease outcome in patients with COVID-19.
7. Other toxic effects of OPs
In addition to immunotoxicity, OPs can promote other toxicities by injuring cardiovascular, hepatic as well as renal system of the body. The cardiotoxic effects of OP compounds have been reported in human as well as animal models following acute or chronic exposure (Georgiadis et al., 2018). For instance, accidental exposure to phorate has been reported to provoke sinus tachycardia and electrocardiographic anomalies in patient (Muthu et al., 2014). A hospital-based cross-sectional study in Nepal demonstrated sinus tachycardia, ventricular extrasystole and ventricular fibrillation in OP intoxicated individuals (Laudari et al., 2014). Moreover, Q-T prolongation, malignant tachyarrhythmias, atrial fibrillation and elevated cardiac troponin levels were also evident (Kharoub and Elsharkawy, 2008; Ludomirsky et al., 1982). Notably in China, acute myocardial injuries were predominantly detected in individuals consumed OP pesticides such as dichlorvos, parathion and methamidophos (Chen et al., 2019). Studies using animal models have unfolded the indubitable role of OP-mediated OS in cardiac injury. For example, rats exposed to chlorpyrifos at a dose of 5.4 mg/kg bw for 28 days suffered from altered cardiac antioxidant status, increased lipid peroxidation, degenerated myocardial fibers as well as cytoplasmic vacuolization in cardiomyocytes (Baş and Kalender, 2011). Similar cardiac manifestations involving OS have also been reported following diazinon exposure (Abdou and ElMazoudy, 2010). Other OPs like malathion, dichlorvos, fenthion, propoxur and chlorpyrifos fuel OS and subsequent cardiotoxicity in the form of abnormal electrophysiology, fibrosis, myocardial degeneration, atherosclerosis, infarction, arrhythmia and necrosis in various animal models including zebra fish, rats and rabbits (Imam et al., 2018; Zafiropoulos et al., 2014; Simoneschi et al., 2014; Yavuz et al., 2008). It should be noted that, cardiac tissue is particularly sensitive to peroxidative insults due to its limited antioxidant defenses that can enzymatically counteract hydroxyl radicals (Doroshow et al., 1980). Moreover, anti-cholinesterase activity of OPs could be responsible for fluctuation in heart beat rhythm that may lead to cardiac failure following OP intoxication.
OPs also impose hepatotoxicity by OS-mediated ultrastructural, biochemical, metabolic and mitochondrial damage to liver. Several studies advocate for the fact that, liver is the primary target organ of OP toxicity. Recent findings by Ezzi et al. (2016) suggest that, chlorpyrifos had a dose-dependent detrimental effect on dilated sinusoids, central vein and portal triad in treated rats. Sub-lethal exposure to triazophos triggers infiltration, vacuolization, enlargement of sinusoids and necrosis in hepatic tissue of female albino rats (Sharma and Sangha, 2014). Intriguingly subchronic exposure to methidathion and dimethoate insisted mononuclear cell infiltration in portal areas, sinusoidal dilatation, focal micro-vesicular steatosis and parenchymal degenerations (Gokalp et al., 2003; Sayim, 2007). Besides, hepatomegaly is also evident following OP exposure. There is strong evidence regarding the impacts of OPs on biochemical parameters which are the markers of liver injury. The most common serum biomarkers of liver damage are aspartate transaminase (AST) and alanine transaminase (ALT). Studies have reported that, these markers are increased in response to wide spectrum of OPs such as dimethoate, monocrotophos, methyl parathion, dichlorvos, fenitrothion, omethoate, chlorpyrifos, diazinon and methidathion (Saafi et al., 2011; Goel et al., 2005; Beydilli et al., 2015; Gomes et al., 1999). Therefore, liver injury and some time mortality is obvious following OP exposure and may result from induction of OS (Sethi and Behera, 2016; Lukaszewicz-Hussain, 2013).
It has been widely accepted that, exposure to OPs has a deleterious impact on the renal tissue and subsequently on the renal function of organisms. A recent study by Kaya et al. (2018) has revealed that, fenthion induces degeneration, vacuolization and atrophy in tubular epithelium of rats. Likewise, exposure to methidathion disrupts nephrotic architecture and promotes kidney injury (Sulak et al., 2005). Bidrin is an OP insecticide formulation that triggers ROS mediated tubular cytotoxicity by inducing lipid peroxidation in renal epithelial cells (Poovala et al., 1999). OP induced nephrotoxicity has also been reported in human subjects. For instance, in an OP poisoning case, a 17 year old patient developed acute kidney injury followed by renal failure, necessitating renal replacement therapy (Cavari et al., 2013). Lee et al. (2015) conducted a nationwide population-based cohort study (N = 8924) during 2010–2011 regarding OP intoxication and unfolded that, incidence of acute kidney injury was higher in the patients with OP poisoning than in the controls. Moreover, patients with severe OP poisoning were associated with a substantially increased risk of kidney injury.
Other toxicities in the form of muscle injury, pancreatitis and neurological anomalies have also been reported following OP exposure in human which can further contribute to subverted physiological barrier against SARS-CoV-2 infection and pathogenicity (Chowdhury et al., 2014; Delgado et al., 2004).
8. Antioxidants mitigate OP-induced immunotoxicity
Studies around the globe have confirmed the immunoprotective-potential of certain antioxidants against OP mediated immunotoxicity (Table 4 ). Ahmed et al. (2009) have demonstrated that, treatment with N-acetylcysteine (NAC) and curcumin can mitigate malathion induced apoptosis in peripheral blood mononuclear cells (PBMC).). Supplementary intake of NAC ameliorates fenitrothion induced immunotoxicity for instance reduced levels of IgG and IgM in rats (Alam et al., 2019). Curcumin restores the proliferation of lymphocytes exposed to parathion (Neeraj et al., 2014). Sodhi et al. (2006) have documented that, vitamin E and selenium could be helpful to counteract malathion induced decrement in total immunoglobulins and circulatory immune complexes. Walnut polyphenol normalizes splenic T lymphocyte proliferation following fenitrothion exposure. Moreover, it also helps to optimize T-cell related cytokines viz. Il-2, IL-4 and IFN- γ following fenitrothion insult (Liu et al., 2018). Propolis is a natural product derived from bees and harbors antioxidant property. It is evident that, propolis can ameliorate chlorpyrifos and profenos mediated immune suppression by up-regulating immunoglobulin titer (Hamza et al., 2013). Ascorbic acid helps to maintain optimum levels of lysozyme peroxidase, white blood cells and serum IgM in dimethoate exposed Clarias batrachus (Narra, 2017). Interestingly, L-ascorbic acid reduces acephate induced mortality of phagocytes in Drosophila melanogaster (Rajak et al., 2017). Immunosuppressive impacts of malathion like subnormal levels of immunoglobulins and circulatory immune complexes in chicks were partially ameliorated following supplementary intake of vitamin E and Selenium (Sodhi et al., 2006). Co-administration of green-tea extract is effective in ameliorating ethephon induced immunotoxicity in mice (Abou-Zeid et al., 2018). Exposure to diazinon reduces relative lymphocyte and monocyte counts, immunoglobulin concentration, hemagglutination titer and phagocytic index of lymphocytes. These immunotoxic impacts of diazinon are reversed upon co-administration of hesperidin in rats (Hassouna et al., 2015). In addition to hesperidin, thymoquinone rescues from diazinon mediated immunotoxicity by modulating cytokine levels (Danaei and Karami, 2017). Zinc Oxide (ZnO) nanoparticles can efficiently scavenge free radicals and therefore reduce OS. Aside, ZnO nanoparticles restore macrophage and serum lysozyme activities and cytokine levels that might be disrupted following chlorpyrifos exposure in rats (Essa et al., 2019).
Table 4.
Studies reporting protective potential of antioxidants against organophosphate-induced immunotoxicity.
| Organophosphate (dose; duration) | Immunotoxic impacts | Mitigation of immunotoxicity by antioxidant(s) (dose; duration) | Reference |
|---|---|---|---|
| Malathion (20 μM & 100 μM; 24 h) | Triggered apoptosis in cultured peripheral blood mononuclear cells (PBMC) | N-acetyl cysteine (20 μM; 24 h) and curcumin (25 μM; 24 h) prevented malathion-mediated apoptosis in PBMC. | Ahmed et al. (2009) |
| Malathion (10 mg/kg; 60 days) | Decreased total immunoglobulins and circulatory immune complexes in chick | Vitamin E (150 IU/kg; 60 days) and selenium (0.1 mg/kg; 60 days) partially counteracted this effect. | Sodhi et al. (2006) |
| Fenitrothion (Lymphocytes incubated with 100 μL of 10−4M Fenitrothion; 48 h) | Reduced proliferation of cultured Splenic Lymphocytes | Walnut Polyphenol (0.5–10 μg/mL; 48 h) increased proliferation of Fenitrothion exposed splenic T lymphocytes (CD3+ T cells) and T-cell subsets (CD8+ T cells), as well as the secretion of the T-cell related cytokines interleukin (IL)-2, interferon-γ, IL-4 and granzyme B. | Liu et al. (2018) |
| Phosphamidon (0–20 μM; 6–24 h) | Fueled cytochrome c mediated mortality, DNA fragmentation and reduced GSH levels in human PBMCs. | Co-administration of N-acetyl cysteine (20 μM; 6–24 h) and curcumin (25 μM; 6–24 h) attenuated mortality in human PBMCs. | Ahmed et al. (2010) |
| Chlorpyrifos (6.75 mg/kg; 8 weeks) and Profenofos (20 mg/kg; 8 weeks) | Reduced IgG, IgM levels and increased TNF-α level | Propolis (70 mg/kg; 8 weeks) and ginseng (200 mg/kg; 8 weeks) increased IgG and IgM; lowered TNF-α level. | Hamza et al. (2013) |
| Chlorpyrifos (75 mg/L; 3–9 weeks) | Decreased macrophage activity, serum lysozyme activity and levels of interleukin-2 (IL-2) and IL-6 in rats | Co-administration of ZnO nanoparticles (200 mg/L; 3–9 weeks) ameliorated undesirable effects of CPF through elevation of macrophage and serum lysozyme activities, increased the levels of IL-2 and IL-6; corrected the oxidative stress markers. | Essa et al. (2019) |
| Chlorpyrifos (10.6 mg/kg; 17 weeks) | Attributed to neutropenia, lymphopenia, and monocytopenia in Wistar rats | Vitamin C (100 mg/kg; 17 weeks) ameliorated the subnormal count of leucocytes. | Saafi et al., 2011 |
| Diazinon (10 mg/kg; 30 days) | Reduced relative lymphocyte and monocyte counts, immunoglobulin concentration, hemagglutination titer, delayed type hypersensitivity, blood mononuclear cell proliferation, phagocytic index and blood T-cell subtypes (CD4+ and CD8+) in rats | Co-administration of Hesperidin (25 mg/kg; 30 days) was able to normalize most of the hematological and immunological parameters. | Hassouna et al. (2015) |
| Chlorpyrifos (13.5 mg/kg/day; 1–2 weeks) | Decreased lymphocyte viability, neutrophil phagocytic index, total white blood cells count, relative lymphocyte count and IgG concentration | Pre and post-treatment with silymarin (70 mg/kg/day; 1–2 weeks) improved the lymphocyte viability, total white blood cell count and relative lymphocyte count. Silymarin also recovered phagocytic activity of neutrophils and restored IgG level. |
Elaimy et al. (2016) |
| Chlorpyrifos (13.5 mg/kg; 28 days) | Decreased serum antibody titer, leukocyte migration inhibition (LMI) and macrophage migration inhibition (MMI) | Quercetin (3 mg/kg; 15 days) effectively alleviated chlorpyrifos-induced immunotoxicity. | Suke et al. (2018) |
| Diazinon (20 mg/kg; 4 weeks) | Exerted immunotoxicity as indicated by reduced IFN-γ and increased micronucleus indices of IL-10 and IL-4 in rats | Thymoquinone (2.5–10 mg/kg; 4 weeks) normalized the levels of IFN-γ, IL-10, IL-4 and prevented immunotoxicity. | Danaei and Karami (2017) |
| Ethephon (1995 ppm; 2 months) | Leucocytosis, neutrophilia, monocytosis, lymphocytopenia; reduced serum hemolyzing antibody titer, declined phagocytic activity of polymorphonuclear cells were recorded in mice. | Green tea extract (2 g of tea leaves/100 mL; 2 months) normalized lymphocyte count; improved humoral immune response and delayed type hypersensitivity reaction; partially ameliorated phagocytic activity of neutrophils. | Abou-Zeid et al. (2018) |
Therefore, consideration of these antioxidants in diets would be beneficial to sustain a healthy immune system under OP-exposure.
9. Concluding remarks
Evidences cited in the review confirm that, OPs disturb various components of immune machinery that can be opportunistic for viral infections. Moreover, several respiratory difficulties including allergic-asthma, pneumonitis and chronic bronchitis are positively correlated with OP exposure. Further, a healthy immune system is essential to overcome SARS-CoV-2 infection. Hence, pre-exposure to OPs or co-exposure to both deleterious agents might augment inflammatory reactions, pyroptosis and pulmonary shortcomings coupled with higher fatal outcome in COVID-19 patients. OP induced oxidative stress is the major driver of apoptosis in lymphoid organs involved in maturation of lymphocytes and development of antibodies of high affinity against viral antigens. Therefore, OP mediated apoptotic lesions in lymphoid tissues may also dampen the efficacy of potent vaccines to some extent.
Since direct experimental works dissecting the collaborative impacts of OPs and SARS-CoV-2 are still lacking, this article will attract the scientific community across the planet to concentrate on the proposed hypothesis to unveil the synergism between the two threats of human-race. Serious health problems discussed in the current literature will also draw attention of global environment policy makers and concerned government/nongovernment organizations towards the perilous impacts of OP-exposure in human. Alongside, it will insist them to adopt necessary resolutions and amend policies that could limit human contacts with OPs.
Finally, it is important to note that, antioxidants may rescue immune system from detrimental impacts of OP compounds and hence diet rich in antioxidants would be helpful to maintain a good immune system that is essential to overcome COVID-19.
CRediT authorship contribution statement
Prem Rajak: Conceptualization, Writing - original draft, Writing - review & editing, Supervision. Abhratanu Ganguly: Conceptualization, Writing - original draft. Saurabh Sarkar: Conceptualization, Writing - review & editing. Moutushi Mandi: Writing - review & editing. Moumita Dutta: Writing - review & editing. Sayanti Podder: Writing - review & editing. Salma Khatun: Writing - review & editing. Sumedha Roy: Conceptualization, Writing - review & editing, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling editor. Dr. Jose Luis Domingo
References
- Abdou H.M., ElMazoudy R.H. Oxidative damage, hyperlipidemia and histological alterations of cardiac and skeletal muscles induced by different doses of diazinon in female rats. J. Hazard Mater. 2010;182:273–278. doi: 10.1016/j.jhazmat.2010.06.026. [DOI] [PubMed] [Google Scholar]
- Abou-Donia M.B. Organophosphorus ester-induced chronic neurotoxicity. Arch. Environ. Health. 2003;58:484–497. doi: 10.3200/AEOH.58.8.484-497. [DOI] [PubMed] [Google Scholar]
- Abou-Zeid S.M., Allam T.S., El-Bahrawy A., Mohamed M.A. Ameliorating effects of green tea on ethephon-induced immunotoxicity and oxidative stress in mice. Int. J. Pharm. Sci. & Scient. Res. 2018;4:1–9. [Google Scholar]
- Acharya D., Liu G., Gack M.U. Dysregulation of type I interferon responses in COVID-19. Nat. Rev. Immunol. 2020;20:397–398. doi: 10.1038/s41577-020-0346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed O.G. Immune modulating effects of malathion with the role of bradykinin potentiating factor in juvenile male rats. Ibnosina J. Med. B.S. 2012;4:151–169. [Google Scholar]
- Ahmed T., Tripathi A.K., Ahmed R.S., Banerjee B.D. Assessment of phosphamidon-induced apoptosis in human peripheral blood mononuclear cells: protective effects of N-acetylcysteine and curcumin. J. Biochem. Mol. Toxicol. 2010;24:286–292. doi: 10.1002/jbt.20337. [DOI] [PubMed] [Google Scholar]
- Ahmed T., Tripathi A.K., Suke S.G., Kumar V., Ahmed R.S., Das S., Banerjee B.D. Role of HSP27 and reduced glutathione in modulating malathion-induced apoptosis of human peripheral blood mononuclear cells: ameliorating effect of N-acetylcysteine and curcumin. Toxicol. Vitro. 2009;23:1319–1325. doi: 10.1016/j.tiv.2009.07.016. [DOI] [PubMed] [Google Scholar]
- Alam R.T., Imam T.S., Abo-Elmaaty A.M.A., Arisha A.H. Amelioration of fenitrothion induced oxidative DNA damage and inactivation of caspase-3 in the brain and spleen tissues of male rats by N-acetylcysteine. Life Sci. 2019;231:116534. doi: 10.1016/j.lfs.2019.06.009. [DOI] [PubMed] [Google Scholar]
- Anand S., Singh S., Nahar Saikia U., Bhalla A., Paul Sharma Y., Singh D. Cardiac abnormalities in acute organophosphate poisoning. Clin. Toxicol. 2009;47:230–235. doi: 10.1080/15563650902724813. [DOI] [PubMed] [Google Scholar]
- Andreadis1 G., Albanis T., Skepastianos1 P., Andreadou1 E., Avramidis N., Patoucheas D.P. The influence of organophosphate pesticides on white blood cell types and C-reactive protein (CRP) level of Greek farm workers. Fresenius Environ. Bull. 2013;22:2423–2427. [Google Scholar]
- Andresen J.A., Grundmann A., Bester K. Organophosphorus flame retardants and plasticisers in surface waters. Sci. Total Environ. 2004;332:155–166. doi: 10.1016/j.scitotenv.2004.04.021. [DOI] [PubMed] [Google Scholar]
- Báez-Santos Y.M., St John S.E., Mesecar A.D. The SARS‐coronavirus papain‐like protease: structure, function and inhibition by designed antiviral compounds. Antivir. Res. 2015;115:21–38. doi: 10.1016/j.antiviral.2014.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagchi D., Bagchi M., Hassoun E.A., Stohs S.J. 1995. In Vitro and in Vivo. [Google Scholar]
- Bains R.K. African variation at Cytochrome P450 genes: evolutionary aspects and the implications for the treatment of infectious diseases. Evol. Med. Public. Health. 2013:118–134. doi: 10.1093/emph/eot010. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bala R., Dhingra S., Kumar M., Bansal K., Mittal S., Sharma R.K., Wangoo N. Detection of organophosphorus pesticide–Malathion in environmental samples using peptide and aptamer based nanoprobes. Chem. Eng. J. 2017;311:111–116. [Google Scholar]
- Baş H., Kalende Y. Chlorpyrifos induced cardiotoxicity in rats and the protective role of Quercetin and Catechin. GU J. Sci. 2011;24:387–395. [Google Scholar]
- Baskin C.R., Bielefeldt-Ohmann H., Tumpey T.M., Sabourin P.J., Long J.P., García-Sastre A., Tolnay A., Albrecht R., Pyles J.A., Olson P.H., Aicher L.D., Rosenzweig E.R., Murali-Krishna K., Clark E.A., Kotur M.S., Fornek J.L., Proll S., Palermo R.E., Sabourin C.L., Katze M.G. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc. Natl. Acad. Sci. U.S.A. 2009;106:3455–3460. doi: 10.1073/pnas.0813234106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu A., Sarkar A., Maulik U. Molecular docking study of potential phytochemicals and their effects on the complex of SARS-CoV2 spike protein and human ACE2. Sci. Rep. 2020;10:17699. doi: 10.1038/s41598-020-74715-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia C.L., Gogal R.M., Jr., Zimmerman K., Misra H.P. Malathion, lindane, and piperonyl butoxide, individually or in combined mixtures, induce immunotoxicity via apoptosis in murine splenocytes in vitro. Int. J. Toxicol. 2010;29:209–220. doi: 10.1177/1091581809357954. [DOI] [PubMed] [Google Scholar]
- Beydilli H., Yilmaz N., Cetin E.S., Topal Y., Celik O.I., Sahin C., Topal H., Cigerci I.H., Sozen H. Evaluation of the protective effect of silibinin against diazinon induced hepatotoxicity and free-radical damage in rat liver. Iran. Red Crescent Med. J. 2015;17 doi: 10.5812/ircmj.17(4)2015.25310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakley B.R., Yole M.J., Brousseau P., Boermans H., Fournier M. Effect of chlorpyrifos on immune function in rats. Vet. Hum. Toxicol. 1999;41:140–144. [PubMed] [Google Scholar]
- Blanco-Melo D., Nilsson-Payant B.E., Liu W.C., Uhl S., Hoagland D., Møller R., Jordan T.X., Oishi K., Panis M., Sachs D., Wang T.T., Schwartz R.E., Lim L.M., Albrecht R.A., tenOever B.R. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036–1045. doi: 10.1016/j.cell.2020.04.026. e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canbaz D., Logiantara A., van Ree R., van Rijt L.S. Immunotoxicity of organophosphate flame retardants TPHP and TDCIPP on murine dendritic cells in vitro. Chemosphere. 2017;177:56–64. doi: 10.1016/j.chemosphere.2017.02.149. [DOI] [PubMed] [Google Scholar]
- Carter W.G., Tarhoni M., Rathbone A.J., Ray D.E. Differential protein adduction by seven organophosphorus pesticides in both brain and thymus. Hum. Exp. Toxicol. 2007;26:347–353. doi: 10.1177/0960327107074617. [DOI] [PubMed] [Google Scholar]
- Casale G.P., Cohen S.D., DiCapua R.A. The effects of organophosphate-induced cholinergic stimulation on the antibody response to sheep erythrocytes in inbred mice. Toxicol. Appl. Pharmacol. 1983;68:198–205. doi: 10.1016/0041-008x(83)90004-2. [DOI] [PubMed] [Google Scholar]
- Cavari Y., Landau D., Sofer S., Leibson T., Lazar I. Organophosphate poisoning-induced acute renal failure. Pediatr. Emerg. Care. 2013;29:646–647. doi: 10.1097/PEC.0b013e31828e9e45. [DOI] [PubMed] [Google Scholar]
- Chan J.F., Kok K.H., Zhu Z., Chu H., To K.K., Yuan S., Yuen K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microb. Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang M.M.F., Ginjom I.R., Ng S.M. Single-shot ‘turn-off’optical probe for rapid detection of paraoxon-ethyl pesticide on vegetable utilising fluorescence carbon dots. Sensor. Actuator. B Chem. 2017;242:1050–1056. [Google Scholar]
- Chatterjee S., Basak P., Chaklader M., Das P., Pereira J.A., Chaudhuri S., Law S. Pesticide induced alterations in marrow physiology and depletion of stem and stromal progenitor population: an experimental model to study the toxic effects of pesticide. Environ. Toxicol. 2014;29:84–97. doi: 10.1002/tox.20775. [DOI] [PubMed] [Google Scholar]
- Chen K.X., Zhou X.H., Sun C.A., Yan P.X. Manifestations of and risk factors for acute myocardial injury after acute organophosphorus pesticide poisoning. Medicine (Baltim.) 2019;98 doi: 10.1097/MD.0000000000014371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Liu W., Zhang Q., Xu K., Ye G., Wu W., Sun Z., Liu F., Wu K., Zhong B., Mei Y., Zhang W., Chen Y., Li Y., Shi M., Lan K., Liu Y. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg. Microb. Infect. 2020;9:313–319. doi: 10.1080/22221751.2020.1725399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury F.R., Bari M.S., Alam M.M., Rahman M.M., Bhattacharjee B., Qayyum J.A., Mridha M.S. Organophosphate poisoning presenting with muscular weakness and abdominal pain-a case report. BMC Res. Notes. 2014;7:140. doi: 10.1186/1756-0500-7-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu H., Chan J.F., Wang Y., Yuen T.T., Chai Y., Hou Y., Shuai H., Yang D., Hu B., Huang X., Zhang X., Cai J., Zhou J., Yuan S., Kok K., To K.K., Chan I.H., Zhang A.J., Sit K., Au W., Yuen K.Y. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin. Infect. Dis. 2020;71:1400–1409. doi: 10.1093/cid/ciaa410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui L., Wang H., Ji Y., Yang J., Xu S., Huang X., Wang Z., Qin L., Tien P., Zhou X., Guo D., Chen Y. The nucleocapsid protein of coronaviruses acts as a viral suppressor of RNA silencing in mammalian cells. J. Virol. 2015;89:9029–9043. doi: 10.1128/JVI.01331-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushman J.R., Street J.C. Allergic hypersensitivity to the insecticide malathion in BALB/c mice. Toxicol. Appl. Pharmacol. 1983;70:29–42. doi: 10.1016/0041-008x(83)90176-x. [DOI] [PubMed] [Google Scholar]
- Danaei G.H., Karami M. Protective effect of thymoquinone against diazinon-induced hematotoxicity, genotoxicity and immunotoxicity in rats. Environ. Toxicol. Pharmacol. 2017;55:217–222. doi: 10.1016/j.etap.2017.09.002. [DOI] [PubMed] [Google Scholar]
- Delgado E., McConnell R., Miranda J., Keifer M., Lundberg I., Partanen T., Wesseling C. Central nervous system effects of acute organophosphate poisoning in a two-year follow-up. Scand. J. Work. Environ. Health. 2004;30:362–370. doi: 10.5271/sjweh.824. [DOI] [PubMed] [Google Scholar]
- Deschamps D., Questel F., Baud F.J., Gervais P., Dally S. Persistent asthma after acute inhalation of organophosphate insecticide. Lancet. 1994;344:1712. doi: 10.1016/s0140-6736(94)90498-7. [DOI] [PubMed] [Google Scholar]
- Descotes J. 2nd (updated. Elsevier; Amsterdam: 1988. Immunotoxicology of Drugs and Chemicals; p. 444. [Google Scholar]
- Dhouib I., Jallouli M., Annabi A., Marzouki S., Gharbi N., Elfazaa S., Lasram M.M. From immunotoxicity to carcinogenicity: the effects of carbamate pesticides on the immune system. Environ. Sci. Pollut. Res. Int. 2016;23:9448–9458. doi: 10.1007/s11356-016-6418-6. [DOI] [PubMed] [Google Scholar]
- Docea A.O., Vassilopoulou L., Fragou D., Arsene A.L., Fenga C., Kovatsi L., Petrakis D., Rakitskii V.N., Nosyrev A.E., Izotov B.N., Golokhvast K.S., Zakharenko A.M., Vakis A., Tsitsimpikou C., Drakoulis N. CYP polymorphisms and pathological conditions related to chronic exposure to organochlorine pesticides. Toxicol. Rep. 2017;4:335–341. doi: 10.1016/j.toxrep.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doroshow J.H., Locker G.Y., Myers C.E. Enzymatic defenses of the mouse heartagainst reactive oxygen metabolites: alterations produced by doxorubicin. J. Clin. Invest. 1980;65:128–135. doi: 10.1172/JCI109642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duramad P., Harley K., Lipsett M., Bradman A., Eskenazi B., Holland N.T., Tager I.B. Early environmental exposures and intracellular TH1/TH2 cytokine profiles in 24-month-old children living in an agricultural area. Environ. Health Perspect. 2006;114:1916–1922. doi: 10.1289/ehp.9306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elaimy I.A., Ibrahim H., Gafaar F.R., Al-Awthan Y.S. Protective and curative effect of silymarin against chlorpyrifos-induced immunotoxicity in rats. Proc. 7th Int. Con. Biol. Sci. (Zool). 2012:99–107. [Google Scholar]
- el-Gendy K.S., Aly N.M., el-Sebae A.H. Effects of edifenphos and glyphosate on the immune response and protein biosynthesis of bolti fish (Tilapia nilotica) J. Environ. Sci. Health B. 1998;33:135–149. doi: 10.1080/03601239809373135. [DOI] [PubMed] [Google Scholar]
- Esa A.H., Warr G.A., Newcombe D.S. Immunotoxicity of organophosphorus compounds. Modulation of cell-mediated immune responses by inhibition of monocyte accessory functions. Clin. Immunol. Immunopathol. 1988;49:41–52. doi: 10.1016/0090-1229(88)90093-1. [DOI] [PubMed] [Google Scholar]
- Esquivel-Sentíes M.S., Barrera I., Ortega A., Vega L. Organophosphorous pesticide metabolite (DEDTP) induces changes in the activation status of human lymphocytes by modulating the interleukin 2 receptor signal transduction pathway. Toxicol. Appl. Pharmacol. 2010;248:122–133. doi: 10.1016/j.taap.2010.07.017. [DOI] [PubMed] [Google Scholar]
- Essa S.S., El-Saied E.M., El-Tawil O.S., Gamal I.M., El-Rahman S.S.A. Nanoparticles of zinc oxide defeat chlorpyrifos-induced immunotoxic effects and histopathological alterations. Vet. World. 2019;12:440–448. doi: 10.14202/vetworld.2019.440-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzi L., Belhadj Salah I., Haouas Z., Sakly A., Grissa I., Chakroun S., Kerkeni E., Hassine M., Mehdi M., Ben Cheikh H. Histopathological and genotoxic effects of chlorpyrifos in rats. Environ. Sci. Pollut. Res. Int. 2016;23:4859–4867. doi: 10.1007/s11356-015-5722-x. [DOI] [PubMed] [Google Scholar]
- Fautz R., Miltenburger H.G. Influence of organophosphorus compounds on different cellular immune functions in vitro. Toxicol. Vitro. 1994;8:1027–1031. doi: 10.1016/0887-2333(94)90238-0. [DOI] [PubMed] [Google Scholar]
- Fenga C., Gangemi S., Catania S., De Luca A., Costa C. IL-17 and IL-22 serum levels in greenhouse workers exposed to pesticides. Inflamm. Res. 2014;63:895–897. doi: 10.1007/s00011-014-0769-6. [DOI] [PubMed] [Google Scholar]
- Filipov N.M., Pinchuk L.M., Boyd B.L., Crittenden P.L. Immunotoxic effects of short-term atrazine exposure in young male C57BL/6 mice. Toxicol. Sci. 2005;86:324–332. doi: 10.1093/toxsci/kfi188. [DOI] [PubMed] [Google Scholar]
- Fournier M., Chevalier G., Nadeau D., Trottier B., Krzystyniak K. Virus-pesticide interactions with murine cellular immunity after sublethal exposure to dieldrin and aminocarb. J. Toxicol. Environ. Health. 1988;25:103–118. doi: 10.1080/15287398809531192. [DOI] [PubMed] [Google Scholar]
- Fukuyama T., Tajima Y., Ueda H., Hayashi K., Kosaka T. Prior exposure to immunosuppressive organophosphorus or organochlorine compounds aggravates the TH1- and TH2-type allergy caused by topical sensitization to 2,4-dinitrochlorobenzene and trimellitic anhydride. J. Immunot. 2011;8:170–182. doi: 10.3109/1547691X.2011.566231. [DOI] [PubMed] [Google Scholar]
- Gallicchio V.S., Casale G.P., Watts T. Inhibition of human bone marrow-derived stem cell colony formation (CFU-E, BFU-E, and CFU-GM) following in vitro exposure to organophosphates. Exp. Hematol. 1987;15:1099–1102. [PubMed] [Google Scholar]
- Gao T., Hu M., Zhang X., Li H., Zhu L., Liu H., Dong Q., Zhang Z., Wang Z., Hu Y., Fu Y., Jin Y., Li K., Zhao S., Xiao Y., Luo S., Li L., Zhao L., Liu J., Zhao H., Liu Y., Yang W., Peng J., Chen X., Li P., Liu Y., Xie Y., Song J., Zhang L., Ma Q., Bian X., Chen W., Liu X., Mao Q., Cao C. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. medRxiv. 2020 doi: 10.1101/2020.03.29.20041962. [DOI] [Google Scholar]
- Garg U.K., Pal A.K., Jha G.J., Jadhao S.B. Haemato-biochemical and immuno-pathophysiological effects of chronic toxicity with synthetic pyrethroid, organophosphate and chlorinated pesticides in broiler chicks. Int. Immunopharm. 2004;4:1709–1722. doi: 10.1016/j.intimp.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Gazzaruso C., Mariani G., Ravetto C., Malinverni L., Tondelli E., Cerrone M., Sala V., Bevilacqua L., Altavilla T., Coppola A., Gallotti P. Lupus anticoagulant and mortality in patients hospitalized for COVID-19. J. Thromb. Thrombolysis. 2020;7:1–7. doi: 10.1007/s11239-020-02335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiadis N., Tsarouhas K., Tsitsimpikou C., Vardavas A., Rezaee R., Germanakis I., Tsatsakis A., Stagos D., Kouretas D. Pesticides and cardiotoxicity. Where do we stand? Toxicol. Appl. Pharmacol. 2018;353:1–14. doi: 10.1016/j.taap.2018.06.004. [DOI] [PubMed] [Google Scholar]
- Giacomelli A., Pezzati L., Conti F., Bernacchia D., Siano M., Oreni L., Rusconi S., Gervasoni C., Ridolfo A.L., Rizzardini G., Antinori S., Galli M. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin. Infect. Dis. 2020;71:889–890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel A., Dani V., Dhawan D.K. Protective effects of zinc on lipid peroxidation, antioxidant enzymes and hepatic histoarchitecture in chlorpyrifos-induced toxicity. Chem. Biol. Interact. 2005;156:131–140. doi: 10.1016/j.cbi.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Gokalp O., Gulle K., Sulak O., Cicek E., Altuntas I. The effects of methidathion on liver: role of vitamins E and C. Toxicol. Ind. Health. 2003;19:63–67. doi: 10.1191/0748233703th176oa. [DOI] [PubMed] [Google Scholar]
- Gomes J., Dawodu A.H., Lloyd O., Revitt D.M., Anilal S.V. Hepatic injury and disturbed amino acid metabolism in mice following prolonged exposure to organophosphorus pesticides. Hum. Exp. Toxicol. 1999;18:33–37. doi: 10.1177/096032719901800105. [DOI] [PubMed] [Google Scholar]
- Gordon D.E., Jang G.M., Bouhaddou M., Xu J., Obernier K., White K.M., et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature [Internet. 2020;583:1–13. doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza R.Z., Diab A.Z., Abd El-Aziz E.A., Hendawy A.A. Immunotoxic effect of organophosphorous insecticides chlorpyrifos, profenofos and possible ameliorative role of Propolis and Ginseng. Biosci. Biotech. Res. Asia. 2013;10:645–651. [Google Scholar]
- Handy R.D., Abd-El Samei H.A., Bayomy M.F., Mahran A.M., Abdeen A.M., El-Elaimy E.A. Chronic Diazinon exposure: pathologies of spleen, thymus, blood cells, and lymph nodes are modulated by dietary protein or lipid in the mouse. Toxicology. 2002;172:13–34. doi: 10.1016/s0300-483x(01)00575-3. [DOI] [PubMed] [Google Scholar]
- Hasan A., Paray B.A., Hussain A., Qadir F.A., Attar F., Aziz F.M., Falahati M. A review on the cleavage priming of the spike protein on coronavirus by angiotensin-converting enzyme-2 and furin. J. Biomol. Struct. Dyn. 2020;22:1–9. doi: 10.1080/07391102.2020.1754293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassouna I., Ibrahim H., Abdel Gaffar F., El-Elaimy I., Abdel Latif H. Simultaneous administration of hesperidin or garlic oil modulates diazinon-induced hemato- and immunotoxicity in rats. Immunopharmacol. Immunotoxicol. 2015;37:442–449. doi: 10.3109/08923973.2015.1081932. [DOI] [PubMed] [Google Scholar]
- Hayashi K., Fukuyama T., Ohnuma A., Tajima Y., Kashimoto Y., Yoshida T., Kosaka T. Immunotoxicity of the organochlorine pesticide methoxychlor in female ICR, BALB/c, and C3H/He mice. J. Immunot. 2013;10:119–124. doi: 10.3109/1547691X.2012.696743. [DOI] [PubMed] [Google Scholar]
- Helali I., Ferchichi S., Maaouia A., Aouni M., Harizi H. Modulation of macrophage functionality induced in vitro by chlorpyrifos and carbendazim pesticides. J. Immunot. 2016;13:745–750. doi: 10.1080/1547691X.2016.1181124. [DOI] [PubMed] [Google Scholar]
- Henning U., Pillat M.M. CD147 as a target for COVID-19 treatment: suggested effects of azithromycin and stem cell engagement. Stem. Cell. Rev. Rep. 2020;16:434–440. doi: 10.1007/s12015-020-09976-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermanowicz A., Kossman S. Neutrophil function and infectious disease in workers occupationally exposed to phosphoorganic pesticides: role of mononuclear-derived chemotactic factor for neutrophils. Clin. Immunol. Immunopathol. 1984;33:13–22. doi: 10.1016/0090-1229(84)90288-5. [DOI] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Müller M.A., Drosten C., Pöhlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppin J.A., Umbach D.M., London S.J., Henneberger P.K., Kullman G.J., Coble J., Alavanja M.C.R., Beane Freeman L.E., Sandler D.P. Pesticide use and adult-onset asthma among male farmers in the Agricultural Health Study. Eur. Respir. J. 2009;34:1296–1303. doi: 10.1183/09031936.00005509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang H., Wang Y. The protective effect of cinnamaldehyde on lipopolysaccharide induced acute lung injury in mice. Cell Mol. Biol. (Noisy-le-grand) 2017;63:58–63. doi: 10.14715/cmb/2017.63.8.13. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim H.M. Immunotoxicity of sub-chronic doses of diazinon in male albino Wister rats. Int. J. Adv. Res. 2014;2:612–621. [Google Scholar]
- Idriss S., Levitt J. Malathion for head lice and scabies: treatment and safety considerations. J. Drugs Dermatol. 2009;8:715–720. [PubMed] [Google Scholar]
- Imam A., Busari M.O., Adana M.Y., Ajibola M.I., Ibrahim A., Sulaimon F.A., Ajao M.S. Subchronic dichlorvos-induced Cardiotoxicity in Wistar rats: mitigative efficacy of Nigella sativa oil. J. Exp. Clin. Anat. 2018;17:60–65. [Google Scholar]
- Ivashkiv L.B., Donlin L.T. Regulation of type I interferon responses. Nat. Rev. Immunol. 2014;14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer S.S., Bibollet-Ruche F., Sherrill-Mix S., Learn G.H., Plenderleith L., Smith A.G., Barbian H.J., Russell R.M., Gondim M.V.P., Bahari C.Y., Shaw C.M., Li Y., Decker T., Haynes B.F., Shaw G.M., Sharp P.M., Borrow P., Hahn B.H. Resistance to type 1 interferons is a major determinant of HIV-1 transmission fitness. Proc. Natl. Acad. Sci. U.S.A. 2017;114:E590–E599. doi: 10.1073/pnas.1620144114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer S.S., He Q., Janczy J.R., Elliott E.I., Zhong Z., Olivier A.K., Sadler J.J., Knepper-Adrian V., Han R., Qiao L., Eisenbarth S.C., Nauseef W.M., Cassel S.L., Sutterwala F.S. Mitochondrial cardiolipin is required for Nlrp3 inflammasome activation. Immunity. 2013;39:311–323. doi: 10.1016/j.immuni.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juergens L.J., Worth H., Juergens U.R. New perspectives for mucolytic, anti-inflammatory and adjunctive therapy with 1,8-cineole in COPD and asthma: review on the new therapeutic approach. Adv. Ther. 2020;37:1737–1753. doi: 10.1007/s12325-020-01279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur G., Jain A.K., Singh S. 2017. CYP/PON Genetic Variations as Determinant of. [DOI] [PubMed] [Google Scholar]
- Kaya Y., Bas O., Hanci H., Cankaya S., Nalbant I., Odaci E., Avni Uydu H., Aslan A. Acute renal involvement in organophosphate poisoning: histological and immunochemical investigations. Ren. Fail. 2018;40:410–415. doi: 10.1080/0886022X.2018.1489289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharoub M.A., Elsharkawy S.A. Mardiotoxicity of acute organophosphate poisoning. Benha M. J. 2008;25(2) https://www.bu.edu.eg/portal/uploads/openLearning/CARDIOTOXICITY%20OF%20ACUTE%20ORGANOPHOSPHATE%20POISONINGabstract_en.pdf [Google Scholar]
- Khurana R., Chauhan R.S. Immunopathological effects of monocrotophos on humoral immune response in sheep. J. Immunol. Immunopathol. 2003;5:54–56. [Google Scholar]
- Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koureas M., Rachiotis G., Tsakalof A., Hadjichristodoulou C. Increased frequency of rheumatoid arthritis and allergic rhinitis among pesticide sprayers and associations with pesticide use. Int. J. Environ. Res. Publ. Health. 2017;14:865. doi: 10.3390/ijerph14080865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudari S., Patowary B.S., Sharma S.K., Dhungel S., Subedi K., Bhattacharya R., Guru-Prasad S., Gangapatnam S. Cardiovascular effects of acute organophosphate poisoning. Asia Pac. J. Med. Toxicol. 2014;3:64–67. [Google Scholar]
- Lee F.Y., Chen W.K., Lin C.L., Lai C.Y., Wu Y.S., Lin I.C., Kao C.H. Organophosphate poisoning and subsequent acute kidney injury risk: a nationwide population-based cohort study. Medicine (Baltim.) 2015;94 doi: 10.1097/MD.0000000000002107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.E., Lim M.S., Park J.H., Park C.H., Koh H.C. Nuclear NF-κB contributes to chlorpyrifos-induced apoptosis through p53 signaling in human neural precursor cells. Neurotoxicology. 2014;42:58–70. doi: 10.1016/j.neuro.2014.04.001. [DOI] [PubMed] [Google Scholar]
- Li G., Fan Y., Lai Y., Han T., Li Z., Zhou P., Pan P., Wang W., Hu X., Zhang O., Wu J. Coronavirus infections and immune responses. J. Med. Virol. 2020;92(4):424–432. doi: 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q. New mechanism of organophosphorus pesticide-induced immunotoxicity. J. Nippon Med. Sch. 2007;74:92–105. doi: 10.1272/jnms.74.92. [DOI] [PubMed] [Google Scholar]
- Li Q., Hirata Y., Piao S., Minami M. The by-products generated during sarin synthesis in the Tokyo sarin disaster induced inhibition of natural killer and cytotoxic T lymphocyte activity. Toxicology. 2000;146:209–220. doi: 10.1016/s0300-483x(00)00174-8. [DOI] [PubMed] [Google Scholar]
- Li X., Li N., Rao K., Huang Q., Ma M. In vitro immunotoxicity of organophosphate flame retardants in human THP-1-derived macrophages. Environ. Sci. Technol. 2020;54:8900–8908. doi: 10.1021/acs.est.0c01152. [DOI] [PubMed] [Google Scholar]
- Li Q., Nakadai A., Takeda K., Kawada T. Dimethyl 2, 2-dichlorovinyl phosphate (DDVP) markedly inhibits activities of natural killer cells, cytotoxic T lymphocytes and lymphokine-activated killer cells via the Fas-ligandFas pathway in perforin-knockout (PKO) mice. Toxicology. 2004;204:41–50. doi: 10.1016/j.tox.2004.05.019. [DOI] [PubMed] [Google Scholar]
- Lima A., Vega L. Methyl-parathion and organophosphorous pesticide metabolites modify the activation status and interleukin-2 secretion of human peripheral blood mononuclear cells. Toxicol. Lett. 2005;158:30–38. doi: 10.1016/j.toxlet.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Lin L., Jiang X., Zhang Z., Huang S., Zhang Z., Fang Z., Gu Z., Gao L., Shi H., Mai L., Liu Y., Lin X., Lai R., Yan Z., Li X., Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- Liu H., Wan Y., Wang Y., Zhao Y., Zhang Y., Zhang A., Weng Q., Xu M. Walnut polyphenol extract protects against fenitrothion-induced immunotoxicity in murine splenic lymphocytes. Nutrients. 2018;10:1838. doi: 10.3390/nu10121838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Zhang R., He G. Hematological findings in coronavirus disease 2019: indications of progression of disease. Ann. Hematol. 2020;99:1421–1428. doi: 10.1007/s00277-020-04103-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Q.X., Tang X.J., Shi Q.L., Li Q., Deng H.J., Yuan J., Hu J.L., Xu W., Zhang Y., Lv F.J., Su K., Zhang F., Gong J., Wu B., Liu X.M., Li J.J., Qiu J.F., Chen J., Huang A.L. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 2020;26:1200–1204. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- Lu B., Huang Y., Huang L., Li B., Zheng Z., Chen Z., Chen J., Hu Q., Wang H. Effect of mucosal and systemic immunization with virus-like particles of severe acute respiratory syndrome coronavirus in mice. Immunology. 2010;130:254–261. doi: 10.1111/j.1365-2567.2010.03231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludomirsky A., Klein H.O., Sarelli P., Becker B., Hoffman S., Taitelman U., Barzilai J., Lang R., David D., DiSegni E., Kaplinsky E. Q-T prolongation and polymorphous ("torsade de pointes") ventricular arrhythmias associated with organophosphorus insecticide poisoning. Am. J. Cardiol. 1982;49:1654–1658. doi: 10.1016/0002-9149(82)90242-9. [DOI] [PubMed] [Google Scholar]
- Lukaszewicz-Hussain A. Involvement of oxidative stress in liver injury after subchronic intoxication with low doses of chlorpyrifos — study on rats. Cent. Eur. J. Med. 2013;8:132–139. [Google Scholar]
- Mandi M., Khatun S., Rajak P., Mazumdar A., Roy S. Potential risk of organophosphate exposure in male reproductive system of a non-target insect model Drosophila melanogaster. Environ. Toxicol. Pharmacol. 2020;74:103308. doi: 10.1016/j.etap.2019.103308. [DOI] [PubMed] [Google Scholar]
- Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrs T.C. In: Organophosphates and Health. Karalliedde L., Feldman S., Henry J., Marrs T., editors. Imperial College Press; London: 2001. Organophosphates: history, chemistry, pharmacology; p. 485. [Google Scholar]
- Matter M.S., Hilmenyuk T., Claus C., Marone R., Schürch C., Tinguely M., Terracciano L., Luther S.A., Ochsenbein A.F. Destruction of lymphoid organ architecture and hepatitis caused by CD4+ T cells. PloS One. 2011;6(9) doi: 10.1371/journal.pone.0024772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mecdad A.A., Ahmed M.H., ElHalwagy M.E.A., Afify M.M.M. A study on oxidative stress biomarkers and immunomodulatory effects of pesticides in pesticide-sprayers. Egypt. J. Forensic Sci. 2011;1:93–98. [Google Scholar]
- Meyer A., Sandler D.P., Beane Freeman L.E., Hofmann J.N., Parks C.G. Pesticide exposure and risk of rheumatoid arthritis among licensed male pesticide applicators in the agricultural health study. Environ. Health Perspect. 2017;125 doi: 10.1289/EHP1013. 077010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra A., Sarkar M., Chatterjee C. Modulation of immune response by organophosphate pesticides: mammals as potential model. Proc. Zool. Soc. 2019;72:13–24. [Google Scholar]
- Moon C.K., Yun Y.P., Lee S.H. Effects of some organophosphate pesticides on the murine immune system following subchronic exposure (II) Arch Pharm. Res. (Seoul) 1986;9:183–187. doi: 10.1007/BF02900004. [DOI] [Google Scholar]
- Morowati M. Inhalation toxicity studies of thimet (phorate) in male Swiss albino mouse, Mus musculus: I. Hepatotoxicity. Environ. Pollut. 1997;96:283–288. doi: 10.1016/s0269-7491(97)00052-3. [DOI] [PubMed] [Google Scholar]
- Muthu V., Dhooria S., Sehgal I.S. A rare manifestation of organophosphorus poisoning: hypothermia with cardiotoxicity. Int. J. Clin. Cardiol. 2014;1 005. [Google Scholar]
- Nain S., Bour A., Chalmers C., Smits J.E.G. Immunotoxicity and disease resistance in Japanese quail (Corturnix coturnix japonica) exposed to malathion. Ecotoxicology. 2011;20:892–900. doi: 10.1007/s10646-011-0657-6. [DOI] [PubMed] [Google Scholar]
- Neeraj K., Anita Y., Sachin G., Kanupriya N.A., Ranjan G. Antigenotoxic effect of curcumin and carvacrol against parathion induced DNA damage in cultured human peripheral blood lymphocytes and its relation to GSTM1 and GSTT1 polymorphism. J. Toxicol. 2014;2014 doi: 10.1155/2014/404236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neishabouri E.Z., Hassan Z., Azizi E., Ostad S. Evaluation of immunotoxicity induced by diazinon in C57bl/6 mice. Toxicology. 2004;196:173–179. doi: 10.1016/j.tox.2003.08.012. [DOI] [PubMed] [Google Scholar]
- Neuman B.W., Kiss G., Kunding A.H., Bhella D., Baksh M.F., Connelly S., Droese B., Klaus J.P., Makino S., Sawicki S.G., Siddell S.G., Stamou D.G., Wilson I.A., Kuhn P., Buchmeier M.J. A structural analysis of M protein in coronavirus assembly and morphology. J. Struct. Biol. 2011;174:11–22. doi: 10.1016/j.jsb.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni L., Ye F., Cheng M.L., Feng Y., Deng Y.Q., Zhao H., Wei P., Ge J., Gou M., Li X., Sun L., Cao T., Wang P., Zhou C., Zhang R., Liang P., Guo H., Wang X., Qin C.F., Chen F., Dong C. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity. 2020;52:971–977. doi: 10.1016/j.immuni.2020.04.023. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieto-Torres J.L., DeDiego M.L., Verdiá-Báguena C., Jimenez-Guardeño J.M., Regla-Nava J.A., Fernandez-Delgado R., Castaño-Rodriguez C., Alcaraz A., Torres J., Aguilella V.M., Enjuanes L. Severe acute respiratory syndrome coronavirus envelope protein ion channel activity promotes virus fitness and pathogenesis. PLoS Pathog. 2014;10 doi: 10.1371/journal.ppat.1004077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noworyta-Głowacka J., Bańkowski R., Siennicka J., Wiadrowska B., Ludwicki J.K. Influence of chlorpyrifos on the profile of subpopulations of immunoactive cells and their phagocytic activity in an experimental in vivo model. Ann. Agric. Environ. Med. 2012;19:483–486. [PubMed] [Google Scholar]
- Ogasawara N., Matsushima M., Kawamura N., Atsumi K., Yamaguchi T., Ochi H., Kusatsugu Y., Oyabu S., Hashimoto N., Hasegawa Y., Ueyama J., Kawabe T. Modulation of immunological activity on macrophages induced by diazinon. Toxicology. 2017;379:22–30. doi: 10.1016/j.tox.2017.01.014. [DOI] [PubMed] [Google Scholar]
- Ohayo-Mitoko G.J.A., Kromhout H., Simwa J.M., Boleij J.S.M., Heederik D. Self reported symptoms and inhibition of acetylcholinesterase activity among Kenyan agricultural workers. Occup. Environ. Med. 2000;57:195–200. doi: 10.1136/oem.57.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojha A., Gupta Y. Study of commonly used organophosphate pesticides that induced oxidative stress and apoptosis in peripheral blood lymphocytes of rats. Hum. Exp. Toxicol. 2017;36:1158–1168. doi: 10.1177/0960327116680273. [DOI] [PubMed] [Google Scholar]
- Olakkaran S., Kizhakke Purayil A., Antony A., Mallikarjunaiah S., Hunasanahally Puttaswamygowda G. Oxidative stress-mediated genotoxicity of malathion in human lymphocytes. Mutat. Res. 2020;849:503138. doi: 10.1016/j.mrgentox.2020.503138. [DOI] [PubMed] [Google Scholar]
- Oostingh G.J., Wichmann G., Schmittner M., Lehmann I., Duschl A. The cytotoxic effects of the organophosphates chlorpyrifos and diazinon differ from their immunomodulating effects. J. Immunot. 2009;6:136–145. doi: 10.1080/15476910902977407. [DOI] [PubMed] [Google Scholar]
- Osely E.ShM. Influence of some pesticides on humoral and cellular immunity of exposed workers in pesticides industries. INIS. 2010 http://inis.iaea.org/search/search.aspx?orig_q=RN:43081200 [Google Scholar]
- Park M.D. Immune evasion via SARS-CoV-2 ORF8 protein? Nat. Rev. Immunol. 2020;20:408. doi: 10.1038/s41577-020-0360-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks C.G., Santos A.S.E., Lerro C.C., DellaValle C.T., Ward M.H., Alavanja M.C., Berndt S.I., Beane Freeman L.E., Sandler D.P., Hofmann J.N. Lifetime pesticide use and antinuclear antibodies in male farmers from the agricultural health study. Front. Immunol. 2019;10:1476. doi: 10.3389/fimmu.2019.01476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parpia A.S., Pandey A., Martinez I., El-Sayed A.M., Wells C.R., Myers L., Duncan J., Collins J., Fitzpatrick M.C., Galvani A.P. Racial disparities in COVID-19 mortality across Michigan, United States. medRxiv. 2020 doi: 10.1101/2020.11.30.20241133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil J.A., Patil A.J., Govindwar S.P. Biochemical effects of various pesticides on sprayers of grape gardens. Indian J. Clin. Biochem. 2003;18:16–22. doi: 10.1007/BF02867362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peter J.V., Sudarsan T.I., Moran J.L. Clinical features of organophosphate poisoning: a review of different classification systems and approaches. Indian J. Crit. Care Med. 2014;18:735–745. doi: 10.4103/0972-5229.144017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poovala V.S., Huang H., Salahudeen A.K. Role of reactive oxygen metabolites in organophosphate-bidrin-induced renal tubular cytotoxicity. J. Am. Soc. Nephrol. 1999;10:1746–1752. doi: 10.1681/ASN.V1081746. [DOI] [PubMed] [Google Scholar]
- Queiroz M.L., Fernandes M.D., Valadares M.C. Neutrophil function in workers exposed to organophosphate and carbamate insecticides. Int. J. Immunopharm. 1999;21:263–270. doi: 10.1016/s0192-0561(99)00006-5. [DOI] [PubMed] [Google Scholar]
- Rajak P., Dutta M., Khatun S., Mandi M., Roy S. Exploringhazards of acute exposure of Acephate in Drosophila melanogaster and search for l-ascorbic acid mediated defense in it. J. Hazard Mater. 2017;321:690–702. doi: 10.1016/j.jhazmat.2016.09.067. [DOI] [PubMed] [Google Scholar]
- Rajak P., Khatun S., Dutta M., Mandi M., Roy S. Chronic exposure to acephate triggers ROS-mediated injuries at organismal and sub-organismal levels of Drosophila melanogaster. Toxicol. Res. 2018;7:874–887. doi: 10.1039/c8tx00052b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramadan G., El-Beih N.M., Ahmed R.S. Aged garlic extract ameliorates immunotoxicity, hematotoxicity and impaired burn-healing in malathion- and carbaryl-treated male albino rats. Environ. Toxicol. 2017;32:789–798. doi: 10.1002/tox.22279. [DOI] [PubMed] [Google Scholar]
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J. Eur. Acad. Dermatol. Venereol. 2020;35:e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- Riaz S., Manzoor F., Mahmood N., Hassan A., Memona H. Serum immunoglobulins (IgA, IgM, IgE) and acetylcholinesterase level determination in agricultural spray workers exposed to organophosphates pesticides in district Gujranwala. GARJAS. 2017;6:374–380. [Google Scholar]
- Robinson N., Ganesan R., Hegedűs C., Kovács K., Kufer T.A., Virág L. Programmed necrotic cell death of macrophages: focus on pyroptosis, necroptosis, and parthanatos. Redox Biol. 2019;26:101239. doi: 10.1016/j.redox.2019.101239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers K., Xiong S. Effect of administration of malathion for 14 Days on macrophage function and mast cell degranulation. Fund. Appl. Toxicol. 1997;37:95–99. doi: 10.1006/faat.1997.2302. [DOI] [PubMed] [Google Scholar]
- Rodgers K.E. Effects of oral administration of malathion on the course of disease in MRL-lpr mice. J. Autoimmun. 1997;10:367–373. doi: 10.1006/jaut.1997.0145. [DOI] [PubMed] [Google Scholar]
- Rothlein J., Rohlman D., Lasarev M. Organophosphate pesticide exposure and neurobehavioral performance in agricultural and non-agricultural Hispanic workers. Environ. Health Perspect. 2006;114:691–696. doi: 10.1289/ehp.8182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saafi E.B., Louedi M., Elfeki A., Zakhama A., Najjar M.F., Hammami M., Achour L. Protective effect of date palm fruit extract (Phoenix dactylifera L.) on dimethoate inducedoxidative stress in rat liver. Exp. Toxicol. Pathol. 2011;63:433–441. doi: 10.1016/j.etp.2010.03.002. [DOI] [PubMed] [Google Scholar]
- Sanghi R., Pillai M.K., Jayalekshmi T.R., Nair A. Organochlorine and organophosphorus pesticide residues in breast milk from Bhopal, Madhya Pradesh, India. Hum. Exp. Toxicol. 2003;22:73–76. doi: 10.1191/0960327103ht321oa. [DOI] [PubMed] [Google Scholar]
- Sankhala L.N., Tripathi S.M., Bhavsar S.K., Thaker A.M., Sharma P. Hematological and immunological changes due to short-term oral administration of acephate. Toxicol. Int. 2012;19:162–166. doi: 10.4103/0971-6580.97217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayim F. Dimethoate-induced biochemical and histopathological changes in the liver of rats. Exp. Toxicol. Pathol. 2007;59:237–243. doi: 10.1016/j.etp.2007.05.008. [DOI] [PubMed] [Google Scholar]
- Schäfer M., Koppe F., Stenger B., Brochhausen C., Schmidt A., Steinritz D., Thiermann H., Kirkpatrick C.J., Pohl C. Influence of organophosphate poisoning on human dendritic cells. Chem. Biol. Interact. 2013;206:472–478. doi: 10.1016/j.cbi.2013.08.011. [DOI] [PubMed] [Google Scholar]
- Senanayake N., Karalliedde L. Neurotoxic effects of organophosphate insecticides: an intermediate syndrome. N. Engl. J. Med. 1987;316:761–763. doi: 10.1056/NEJM198703263161301. [DOI] [PubMed] [Google Scholar]
- Senthil Kumar K.J., Gokila Vani M., Wang C.S., Chen C.C., Chen Y.C., Lu L.P., Huang C.H., Lai C.S., Wang S.Y. Geranium and lemon essential oils and their active compounds downregulate angiotensin-converting enzyme 2 (ace2), a sars-cov-2 spike receptor-binding domain, in epithelial cells. Plants. 2020;9(6):770. doi: 10.3390/plants9060770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi S., Behera R. Acute liver failure due to organophosphorous. Int. J. Gastroenterol. Hepatol. Transpl. Nutr. 2016;1:67–69. [Google Scholar]
- Shahzad A., Khan A., Khan M.Z., Mahmood F., Gul S.T., Saleemi M.K. Immuno-pathologic effects of oral administration of chlorpyrifos in broiler chicks. J. Immunot. 2015;12:16–23. doi: 10.3109/1547691X.2013.866706. [DOI] [PubMed] [Google Scholar]
- Shang J., Wan Y., Luo C., Ye G., Geng Q., Auerbach A., Li F. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. U.S.A. 2020;117:11727–11734. doi: 10.1073/pnas.2003138117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A.D., Kaur I. Jensenone from eucalyptus essential oil as a potential inhibitor of COVID 19 corona virus infection. Res. Rev. Biotech. Biosci. 2020;7:59–66. [Google Scholar]
- Sharma D., Sangha G.K. Triazophos induced oxidative stress and histomorphological changes in liver and kidney of female albino rats. Pestic. Biochem. Physiol. 2014;110:71–80. doi: 10.1016/j.pestbp.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., Gong W., Liu X., Liang J., Zhao Q., Huang H., Yang B., Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoneschi D., Simoneschi F., Todd N.E. Assessment of cardiotoxicity and effects of malathion on the early development of zebrafish (Danio rerio) using computer vision for heart rate quantification. Zebrafish. 2014;11:275–280. doi: 10.1089/zeb.2014.0973. [DOI] [PubMed] [Google Scholar]
- Singh A.K., Jiang Y. Lipopolysaccharide (LPS) induced activation of the immune system in control rats and rats chronically exposed to a low level of the organothiophosphate insecticide. acephate. Toxicol. Ind. Health. 2003;19:93–108. doi: 10.1191/0748233703th181oa. [DOI] [PubMed] [Google Scholar]
- Singh A.K., Parashar A., Singh A.K., Singh R. Pre-natal/juvenile chlorpyrifos exposure associated with immunotoxicity in adulthood in Swiss albino mice. J. Immunot. 2013;10:141–149. doi: 10.3109/1547691X.2012.700653. [DOI] [PubMed] [Google Scholar]
- Sodhi S., Sharma A., Brar R.S. A protective effect of vitamin E and selenium in ameliorating the immunotoxicity of malathion in chicks. Vet. Res. Commun. 2006;30:935–942. doi: 10.1007/s11259-006-2503-5. [DOI] [PubMed] [Google Scholar]
- Sonu A., Kumar A.T., Chauhan R.S. Evaluation of immunotoxicity and oxidative stress due to in vitro exposure of Dimethoate in chicken lymphocytes. J. Immunol. Immunopathol. 2018;20:30–37. [Google Scholar]
- Srivastava S., Narvi S.S., Prasad S.C. Levels of select organophosphates in human colostrum and mature milk samples in rural region of Faizabad district, Uttar Pradesh, India. Hum. Exp. Toxicol. 2011;30:1458–1463. doi: 10.1177/0960327110396525. [DOI] [PubMed] [Google Scholar]
- Stiller-Winkler R., Hadnagy W., Leng G., Straube E., Idel H. Immunological parameters in humans exposed to pesticides in the agricultural environment. Toxicol. Lett. 1999;107:219–224. doi: 10.1016/s0378-4274(99)00050-8. [DOI] [PubMed] [Google Scholar]
- Suke S.G., Ahmed R.S., Tripathi A.K., Chakraborti A., Banerjee B.D. Immunotoxicity of phosphamidon following subchronic exposure in albino rats. Indian J. Exp. Biol. 2006;44:316–320. [PubMed] [Google Scholar]
- Suke S.G., Sherekar P., Kahale V., Patil S., Mundhada D., Nanoti V.M. Ameliorative effect of nanoencapsulated flavonoid against chlorpyrifos-induced hepatic oxidative damage and immunotoxicity in Wistar rats. J. Biochem. Mol. Toxicol. 2018;32 doi: 10.1002/jbt.22050. [DOI] [PubMed] [Google Scholar]
- Sulak O., Altuntas I., Karahan N., Yildirim B., Akturk O., Yilmaz H.R., Delibas N. Nephrotoxicity in rats induced by organophosphate insecticide methidathion and ameliorating effects of vitamins E and C. Pestic. Biochem. Phys. 2005;83:21–28. [Google Scholar]
- Taghavian F., Vaezi G., Abdollahi M., Malekirad A.A. Comparative toxicological study between exposed and non-exposed farmers to organophosphorus pesticides. Cell J. 2016;18:89–96. doi: 10.22074/cellj.2016.3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamang R.K., Jha G.J., Gupta M.K., Chauhan H.V., Tiwary B.K. In vivo immunosuppression by synthetic pyrethroid (cypermethrin) pesticide in mice and goats. Vet. Immunol. Immunopathol. 1988;19:299–305. doi: 10.1016/0165-2427(88)90116-x. [DOI] [PubMed] [Google Scholar]
- Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.Q., Wang Q., Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct. Target Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X., Yin C., Zhang F., Fu Y., Chen W., Chen Y., Wang J., Jia W., Xu A. Measurement of subgroups of peripheral blood T lymphocytes in patients with severe acute respiratory syndrome and its clinical significance. Chin. Med. J. 2003;116:827–830. [PubMed] [Google Scholar]
- Thoms M., Buschauer R., Ameismeier M., Koepke L., Denk T., Hirschenberger M., Kratzat H., Hayn M., Mackens-Kiani T., Cheng J., Straub J.H., Stürzel C.M., Fröhlich T., Berninghausen O., Becker T., Kirchhoff F., Sparrer K.M.J., Beckmann R. Structural basis for translational shutdown and immune evasion by the Nsp1 protein of SARS-CoV-2. Science. 2020;369:1249–1255. doi: 10.1126/science.abc8665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J.D., Madison R., Broughton A. Immunologic abnormalities in humans exposed to chlorpyrifos: preliminary observations. Arch. Environ. Health. 1993;48:89–93. doi: 10.1080/00039896.1993.9938400. [DOI] [PubMed] [Google Scholar]
- Thrasher J.D., Heuser G., Broughton A. Immunological abnormalities in humans chronically exposed to chlorpyrifos. Arch. Environ. Health. 2002;57:181–187. doi: 10.1080/00039890209602934. [DOI] [PubMed] [Google Scholar]
- Tiefenbach B., Lange P. In: Chambers P.L., Klinger W., editors. vol. 4. Springer; Berlin, Heidelberg: 1980. Studies on the action of dimethoate on the immune system. (Further Studies in the Assessment of Toxic Actions. Archives of Toxicology (Supplement)). [DOI] [PubMed] [Google Scholar]
- Ȕndeger U., Institóris L., Siroki O., Nehéz M., Dési I. Simultaneous geno- and immunotoxicological investigations for early detection of organophosphate toxicity in rats. Ecotoxicol. Environ. Saf. 2000;45:43–48. doi: 10.1006/eesa.1999.1844. [DOI] [PubMed] [Google Scholar]
- Valcin M., Henneberger P.K., Kullman G.J., Umbach D.M., London S.J., Alavanja M.C., Sandler D.P., Hoppin J.A. Chronic bronchitis among nonsmoking farm women in the agricultural health study. J. Occup. Environ. Med. 2007;49:574–583. doi: 10.1097/JOM.0b013e3180577768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesan R., Park Y.U., Ji E., Yeo E.J., Kim S.Y. Malathion increases apoptotic cell death by inducing lysosomal membrane permeabilization in N2a neuroblastoma cells: a model for neurodegeneration in Alzheimer's disease. Cell Death Dis. 2017;3:17007. doi: 10.1038/cddiscovery.2017.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C.Y., Wu C.L., Tsan Y.T., Hsu J.Y., Hung D.Z., Wang C.H. Early onset pneumonia in patients with cholinesterase inhibitor poisoning. Respirology. 2010;15:961–968. doi: 10.1111/j.1440-1843.2010.01806.x. [DOI] [PubMed] [Google Scholar]
- Wang F., Hou H., Luo Y., Tang G., Wu S., Huang M., Liu W., Zhu Y., Lin Q., Mao L., Fang M., Zhang H., Sun Z. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI insight. 2020;5 doi: 10.1172/jci.insight.137799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L. C-reactive protein levels in the early stage of COVID-19. Med. Maladies Infect. 2020;50:332–334. doi: 10.1016/j.medmal.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Statement on the second meeting of the international health regulations (2005) emergency committee regarding the outbreak of novel coronavirus (2019-nCoV) 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov accessed 28th September 2020.
- World Health Organization Virtual press conference on COVID-19-11 March 2020. 2020. https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2 29th September 2020.
- Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O., Graham B.S., McLellan J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. (New York, N.Y.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia S., Zhu Y., Liu M., Lan Q., Xu W., Wu Y., Ying T., Liu S., Shi Z., Jiang S., Lu L. Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cell. Mol. Immunol. 2020;17:765–767. doi: 10.1038/s41423-020-0374-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong Y., Liu Y., Cao L., Wang D., Guo M., Jiang A., Guo D., Hu W., Yang J., Tang Z., Wu H., Lin Y., Zhang M., Zhang Q., Shi M., Liu Y., Zhou Y., Lan K., Chen Y. Transcriptomic characteristics of bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg. microbes infect. 2020;9:761–770. doi: 10.1080/22221751.2020.1747363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasunaga S., Nishi K., Nishimoto S., Sugahara T. Methoxychlor enhances degranulation of murine mast cells by regulating FcεRI-mediated signal transduction. J. Immunot. 2015;12:283–289. doi: 10.3109/1547691X.2014.962122. [DOI] [PubMed] [Google Scholar]
- Yavuz T., Altuntas I., Delibas N., Yildirim B., Candir O., Corâ A., Karahan N., Ibrisim E., Kutsal A. Cardiotoxicity in rats induced by methidathion and ameliorating effect of vitamins E and C. Hum. Exp. Toxicol. 2004;23:323–329. doi: 10.1191/0960327104ht456oa. [DOI] [PubMed] [Google Scholar]
- Yoshida T., Ichikawa J., Giuroiu I., Laino A.S., Hao Y., Krogsgaard M., Vassallo M., Woods D.M., Stephen Hodi F., Weber J. C reactive protein impairs adaptive immunity in immune cells of patients with melanoma. J. Immunother. Cancer. 2020;8 doi: 10.1136/jitc-2019-000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen C.K., Lam J.Y., Wong W.M., Mak L.F., Wang X., Chu H., Cai J.P., Jin D.Y., To K.K., Chan J.F., Yuen K.Y., Kok K.H. SARS-CoV-2 nsp13, nsp14, nsp15 and orf6 function as potent interferon antagonists. Emerg. Microb. Infect. 2020;9:1418–1428. doi: 10.1080/22221751.2020.1780953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabrodskii P.F. The effect of chronic intoxication by organophosphate insecticides on the parameters of innate and adaptive immunity and realization of the cholinergic anti-inflammatory pathway. Pharm. Pharmacol. Int. J. 2018;6:418–420. [Google Scholar]
- Zabrodskii P.F. The types of dysfunction of Th1, Th2 lymphocytes after various toxic chemicals acute intoxication. Acta Scientific Microbiol. 2019;2:162–165. [Google Scholar]
- Zafar R., Munawar K., Nasrullah A., Haq S., Ghazanfar H., Sheikh A.B., Khan A.Y. Acute renal failure due to organophosphate poisoning: a case report. Cureus. 2017;9:e1523. doi: 10.7759/cureus.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zafiropoulos A., Tsarouhas K., Tsitsimpikou C., Fragkiadaki P., Germanakis I., Tsardi M., Maravgakis G., Goutzourelas N., Vasilaki F., Kouretas D., Hayes A., Tsatsakis A. Cardiotoxicity in rabbits after a low-level exposure to diazinon, propoxur, and chlorpyrifos. Hum. Exp. Toxicol. 2014;33:1241–1252. doi: 10.1177/0960327114532384. [DOI] [PubMed] [Google Scholar]
- Zaidi S., Bhatnagar V., Patel A.B., Tripathi S., Sinha S., Choudhari R., Shivgotra V. Neurobehavioral, biochemical and immunological manifestations in workers exposed to organophosphate insecticides. Indian J. Biochem. Biophys. 2015;52:305–310. [Google Scholar]
- Zhang L.X., Enarson D.A., He G.X., Li B., Chan-Yeung M. Occupational and environmental risk factors for respiratory symptoms in rural Beijing, China. Eur. Respir. J. 2002;20:1525–1531. doi: 10.1183/09031936.02.00028602. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Zhang J., Chen Y., Luo B., Yuan Y., Huang F., Yang T., Yu F., Liu J., Liu B., Song Z., Chen J., Pan T., Zhang X., Li Y., Li R., Huang W., Xiao F., Zhang H. The ORF8 protein of SARS-CoV-2 mediates immune evasion through potently downregulating MHC-I. bioRxiv. 2020 doi: 10.1101/2020.05.24.111823. [Preprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Cao W., Jiang W., Xiao M., Li Y., Tang N. Profile of natural anticoagulant, coagulant factor and anti-phospholipid antibody in critically ill COVID-19 patients. J. Thromb. Thrombolysis. 2020;50:580–586. doi: 10.1007/s11239-020-02182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao S.X., Zhang Q.S., Kong L., Zhang Y.G., Wang R.Q., Nan Y.M., Kong L.B. Dichlorvos induced autoimmune hepatitis: a case report and review of literature. Hepat. Mon. 2015;15 doi: 10.5812/hepatmon.25469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Zhuang M.W., Han L., Zhang J., Nan M.-L., Zhan P., Kang D., Liu X., Gao C., Wang P.H. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) membrane (M) protein inhibits type I and III interferon production by targeting RIG-I/MDA-5 signaling. Signal Transduct. Target. Ther. 2020;5(299) doi: 10.1038/s41392-020-00438-7. [Preprint] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou R., To K.K., Wong Y.C., Liu L., Zhou B., Li X., Huang H., Mo Y., Luk T.Y., Lau T.T., Yeung P., Chan W.M., Wu A.K., Lung K.C., Tsang O.T., Leung W.S., Hung I.F., Yuen K.Y., Chen Z. Acute SARS-CoV-2 infection impairs dendritic cell and T cell responses. Immunity. 2020;53:864–877. doi: 10.1016/j.immuni.2020.07.026. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Fu B., Zheng X., Wang D., Zhao C., qi Y., Sun R., Tian Z., Xu X., Wei H. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl. Sci. Rev. 2020;7:998–1002. doi: 10.1093/nsr/nwaa041. nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]