Abstract
Background
Recent advancements in drilling technology led to a rapid increase in natural gas development (NGD). Air pollution may be elevated in these areas and may vary by drilling type (conventional and unconventional), production volume and gas flaring. Impacts of NGD on paediatric asthma are largely unknown. This study quantifies associations between specific NGD activities and paediatric asthma hospitalizations in Texas.
Methods
We leveraged a database of Texas inpatient hospitalizations between 2000 and 2010 at the zip code level by quarter to examine associations between NGD and paediatric asthma hospitalizations, where our primary outcome is 0 vs ≥1 hospitalization. We used quarterly production reports to assess additional drilling-specific exposures at the zip code-level including drilling type, production and gas flaring. We developed logistic regression models to assess paediatric asthma hospitalizations by zip code-quarter-year observations, thus capturing spatiotemporal exposure patterns.
Results
We observed increased odds of ≥1 paediatric asthma hospitalization in a zip code per quarter associated with increasing tertiles of NGD exposure and show that spatiotemporal variation impacts results. Conventional drilling, compared with no drilling, is associated with odds ratios up to 1.23 [95% confidence interval (CI): 1.13, 1.34], whereas unconventional drilling is associated with odds ratios up to 1.59 (95% CI: 1.46, 1.73). Increasing production volumes are associated with increased paediatric asthma hospitalizations in an exposure–response relationship, whereas associations with flaring volumes are inconsistent.
Conclusions
We found evidence of associations between paediatric asthma hospitalizations and NGD, regardless of drilling type. Practices related to production volume may be driving these positive associations.
Keywords: Natural gas drilling, natural gas production, asthma, children’s health, flaring, environmental health
Key Messages
This study found associations between paediatric asthma hospitalizations and natural gas development.
Associations are similar among unconventional drilling and conventional drilling exposures.
Practices related to production volumes from drilling sites may be a mechanism driving these associations.
The impact of gas flaring on paediatric asthma hospitalizations is unclear.
Introduction
Approximately 4.5 million Texans, or ∼16% of the state’s population, live within 1 mile of at least one oil or gas drilling site.1 Unconventional natural gas development (NGD) activities in shale rock have increased exponentially in the USA from <1% of domestic natural gas production in 2000 to almost 20% in 2010,2 and accounted for 67% of domestic natural gas production by 2017.3 Across the contiguous USA, there are 200 trillion cubic feet of proven shale gas resources with an additional estimated 625 trillion cubic feet of technically recoverable shale gas reserves, thus the industry has significant potential to expand.2,4 Texas is the leading state in unconventional NGD due to its location on multiple shale plays, representing 27% of the domestic market.4 Extensive natural gas is also available in the same regions of Texas via traditional extraction methods, commonly referred to as conventional NGD. Conventional and unconventional NGD often happen in close proximity to each other, thus communities can be exposed to both drilling types.1 Although the number of people living near NGD is increasing, adverse health outcomes associated with this industry are not fully explored.
Recent environmental monitoring studies have found some evidence of decreased air quality near NGD activities, but these campaigns largely focus on unconventional drilling.5–10 Known respiratory irritants associated with NGD processes8–13 include diesel particulate matter,14,15 ozone,16,17 volatile organic compounds18 and polycyclic aromatic hydrocarbons.19,20 Community and regional air quality concerns have not been thoroughly addressed to date.6,11,21,22 Exposure sources that may affect air quality include site construction, truck traffic and natural gas flaring.23–27 Epidemiologic literature thus far has primarily focused on unconventional drilling, but few studies examine conventional drilling and health outcomes.1,28,29 The types of exposure risks are similar between unconventional and conventional NGD but differ in terms of the intensity or quantity of those risks. Unconventional (horizontal) wells are deeper, require more resources, create more liquid and solid waste, and have more wellbores on each pad than conventional (vertical) wells.30,31 However, due to the smaller footprint of conventional wells, there can be many more conventional wells overall.30 This study seeks to fill this knowledge gap by examining exposures from both conventional and unconventional drilling.
Although many studies hypothesize associations between NGD-related air pollution and adverse respiratory outcomes, little literature to date has explicitly examined this relationship, as emphasized in multiple studies.28,29,32–36 Paediatric asthma hospitalizations are a relatively rare occurrence (18.3 per 10 000 children and adolescents <18 years old), but represent a substantial financial burden on patients, families and local healthcare systems.37 Air pollution is an established trigger for asthma exacerbations, including hospitalizations, thus NGD-related air emissions may pose a risk to children’s respiratory health.16,38,39
This study aims to quantify associations between NGD exposure and the odds of at least one paediatric asthma hospitalization per quarter by zip code in Texas in 2000–10, corresponding to the NGD boom. We examine paediatric asthma hospitalization risks at varying drilling intensities across the state, with temporal controls for secular trends and spatial controls for time-invariant unmeasured community-related differences. Furthermore, we examine both conventional and unconventional NGD as well as production and flaring activities to compare paediatric asthma risks associated with each NGD exposure. Additional analyses examine the potentially disproportionate burden of NGD exposure for vulnerable populations.
Methods
Study population and design
We obtained data on individual paediatric asthma hospitalizations from the Inpatient Public Use Data File from the Texas Department of State Health Services for 2000–10.40 Each record represents an asthma hospitalization and indicates the patient’s residential zip code, which we used to assign exposure status to NGD sites. To improve our comparison group, we restricted our analyses to patients whose residential zip code land area is entirely situated on a shale play or basin. This approach is similar to previous work on health impacts of unconventional NGD.41–44
NGD exposure metrics
We obtained data on all newly spudded NGD sites in Texas between 2000 and 2010 through Enverus DrillingInfo, a proprietary database of detailed oil and gas development records in the USA.45 Each unique NGD site (defined as a drilling site that includes natural gas resource extraction on their permit) was assigned to the zip code by its geographic coordinates. We calculated tertiles of cumulative density of NGD sites per square kilometer within a zip code, which is consistent with previous studies.41–44 We further stratified quarterly exposure metrics by permitted drilling type: conventional and unconventional. We define vertical drilling as conventional drilling, and horizontal and directional drilling as unconventional.
Additionally, we obtained detailed information on monthly production and flaring volume in 2000–10 by NGD site from the Railroad Commission of Texas (TXRRC). Previous work notes that the reported flaring volumes are likely inaccurate;46,47 however, these estimates represent the best available approximation that we can calculate during our study period. We believe that these estimates are reasonable for inferring if flaring occurred, but the relative magnitude of flaring is more difficult to determine. We link individual well records to geographic coordinates and aggregate monthly volume into quarters for each zip code. For each drilling site, we linked the TXRRC monthly production data at the individual well to its respective DrillingInfo spud information through standardized ten-digit American Petroleum Institute (API) identifiers. To capture contemporaneous exposures for flaring and production, we linked all newly drilled natural gas wells from 1990 through 2010, thus providing 10 years of existing wells potentially contributing to our exposures prior to our study period and 11 years of newer wells contemporaneous to our study period. TXRRC includes flaring and venting within the same field, thus we treat these two categories as equivalent. We calculated the sum of natural gas production and flaring volumes by zip code-quarter observation. All exposure metrics are described in Table 1.
Table 1.
Natural gas development exposure metrics, definitions and categorical intervals. A total of 1249 zip codes are included in this analysis by quarter between 2000 and 2010; all models are relative to the unexposed group
| Metric | Definition | Low (tertile 1) | Medium (tertile 2) | High (tertile 3) |
|---|---|---|---|---|
| All drilling | Cumulative count of natural gas drilling sites per km2 in a zip code by quarter | (0.0004, 0.017) | (0.017, 0.080) | (0.080, 8.32) |
| Conventional | Cumulative vertical natural gas drilling sites per km2 in a zip code by quarter | (0.0004, 0.011) | (0.011, 0.054) | (0.054, 3.18) |
| Unconventional | Cumulative horizontal or directional natural gas drilling per km2 in a zip code by quarter | (0.0004, 0.012) | (0.012, 0.043) | (0.043, 8.32) |
| Flaring volume | Contemporaneous volume of natural gas flared (MCFa) in a zip code by quarter | (1, 136) | (137, 1649) | (1650, 214 529) |
| Production volume | Contemporaneous volume of natural gas produced (MCF) in a zip code by quarter | (2, 69 618) | (69 621, 706 899) | (706 934, 49 590 692) |
MCF = Thousand cubic feet.
Paediatric asthma hospitalizations
The Inpatient Public Use Data File from the Texas Department of State Health Services contains patient diagnoses at hospital discharge. Individual information includes patient age group, residential zip code and hospitalization quarter. (Patient age or residential zip code may be suppressed if there are <5 total hospitalizations of any diagnoses in a zip code for that quarter. We anticipate that this issue directly impacts fewer than 20 zip codes in our analysis.) Our primary outcome of interest is hospitalizations with a primary diagnosis of asthma (ICD-9-CM 493) by patients in the 1–17 year old age group.48 This diagnosis code shows that the individual was hospitalized due to an asthma exacerbation but does not indicate if this diagnosis is new. To examine heterogeneity by age, we implement stratified models for specific groups: 1–4, 5–9, 10–14 and 15–17 years. Given the rarity of this outcome, we a priori chose to assess paediatric asthma hospitalizations as a binary indicator in a specific zip-quarter-year observation and used descriptive statistics to confirm the distribution of pediatric asthma hospitalizations support this decision.
Additional covariates
To better account for community context, our models include a variety of zip code and county covariates. We include zip code covariates using the baseline 2000 Census data on area in square kilometers, population density of individuals <18 years old, percent of population identifying as non-White race and percent of population identifying as Hispanic.49 We also use National Air Toxics Assessment (NATA) background respiratory hazard index interpolated estimates for 2005 to account for potential differences in environmental respiratory risks among zip codes.50 The 2005 NATA inventory specifically excludes NGD activity, so this index does not remove or reduce any exposures of interest. We include annual county covariates from the Small Area Income and Poverty Estimates such as percent unemployed, percent of population below the poverty line for individuals <18 years old and median household income, which allows us to examine key time-varying socio-economic conditions.51 In addition, we control for existing drilling in our analysis by a count of spudded drilling sites in a zip code in 1990–99.
Statistical analyses
We first examine how the samples vary by intensity according to exposures to any drilling, conventional drilling and unconventional drilling. We then compare spatial and temporal trends in exposure. Within this framework, we estimate a logistic regression at the zip code level with the aforementioned exposure metrics (any drilling, conventional, unconventional, flaring, production) and additional community characteristics (listed above) (Model 1). To demonstrate the impact of temporal and spatial trends, we estimate additional models with year and quarter fixed effects (Model 2) and year, quarter and county fixed effects (Model 3). Temporal fixed effects improve our comparisons to observations within the same time frame, reducing the impact of secular trends in asthma prevalence and treatment on our results. Spatial fixed effects restrict our regression by only comparing zip codes that are within the same county as each other, preventing inappropriate comparisons across the state (e.g. urban downtown Houston to a suburb of Amarillo). Since we believe that the spatial and temporal fixed effects are important to fully capture community variation, we demonstrate the importance of controlling for these confounders via these three model specifications.
In sensitivity analyses, we build on the specifications from Model 3. First, we change our outcome variable to different cut points of hospitalization counts (e.g. ≥2 vs <2) to check the robustness of our results. We ran additional stratified models to examine associations of NGD activity with paediatric asthma hospitalizations for specific vulnerable populations determined a priori: specific age groups, large racial or ethnic minority populations, low household income and rural communities. In further models, we stratified our results by shale play to investigate differences between regions of Texas.
We used Python 3.7 for database construction and Stata 15 for statistical analyses.
Results
Descriptive statistics
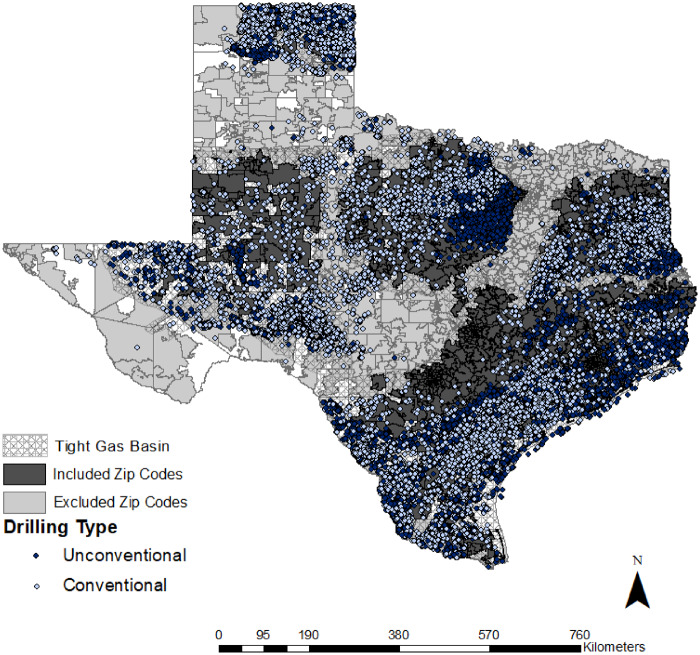
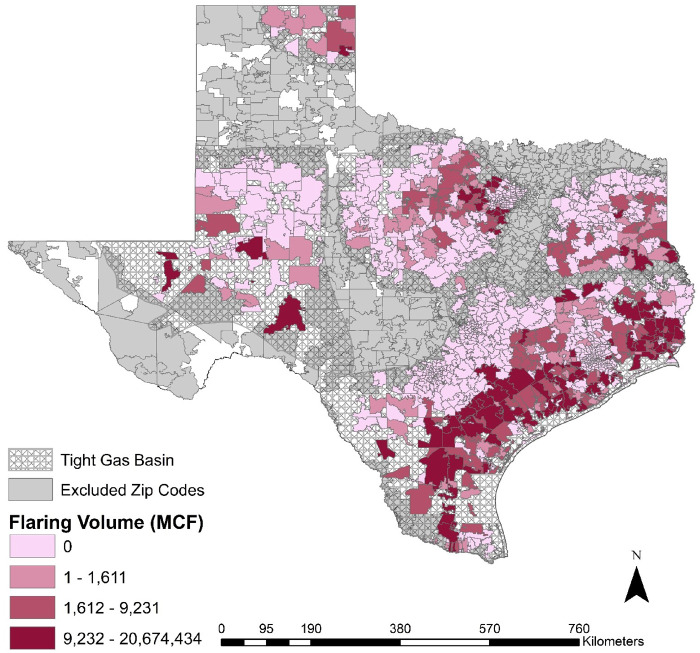
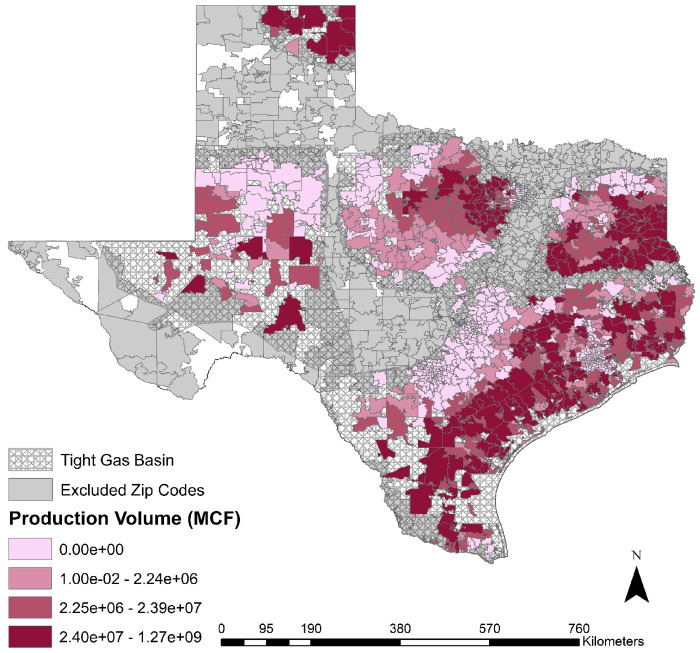
Figures 1–3 demonstrate the cumulative spatial distribution of NGD, flaring and production across Texas, and Supplementary Figure 1, available as Supplementary data at IJE online shows the drilling per year. We have 1249 zip codes, where each contains 11 years of quarterly data, for a total of 54 956 observations in our analysis. A total of 714 zip codes experienced drilling activity during our study period while 535 zip codes did not experience any drilling activity. Of our exposed zip codes, 400 of them experienced both conventional and unconventional drilling. We found 24 333 individual asthma hospitalizations by patients not exposed to NGD compared with 48 589 individual asthma hospitalizations by patients exposed to at least one NGD site (Table 2). Sociodemographic characteristics are similar between the exposed and unexposed patients and communities, except in the unexposed group where the baseline NATA respiratory hazard index is higher, and percent urban population and zip code areas are smaller. We also observed community differences between conventional and unconventional NGD. Conventional NGD occurs in less urban areas, with lower NATA respiratory hazard index and lower median household income compared with unconventional NGD. We demonstrate that the majority of zip code observations contain 0 or 1 asthma hospitalizations (Supplementary Table 1 and 2, available as Supplementary data at IJE online) and note no signs of geographic clustering of asthma hospitalizations by county (Supplementary Figure 2, available as Supplementary data at IJE online). We further examined trends in hospitalizations by age group, finding a slight decrease in hospitalizations per year but similar trends among age groups (Supplementary Figure 3, available as Supplementary data at IJE online).
Figure 1.
Cumulative spatial distribution of natural gas drilling from 2000 to 2010. Parts of Texas do not have an assigned zip code in 2000, which is shown via the white space. A total of 1249 zip codes are included in this analysis by quarter between 2000 and 2010.
Table 2.
Individual, zip code and county demographic information for hospitalizations by zip code exposure status
| 0 NGD sitesa | ≥1 NGD sites | ≥1 Unconventional NGD sites | ≥1 Conventional NGD sites | |
|---|---|---|---|---|
| Individual | ||||
| Total asthma hospitalizations | 48 589 | 24 333 | 20 356 | 17 844 |
| Age group, years (%) | ||||
| 1–4 | 48.0 | 50.5 | 50.1 | 52.3 |
| 5–9 | 32.5 | 30.5 | 30.9 | 29.2 |
| 10–14 | 15.1 | 14.5 | 14.6 | 14.0 |
| 15–17 | 4.4 | 4.5 | 4.4 | 4.5 |
| Hospitalization quarter (%) | ||||
| 1 (January–March) | 28.8 | 28.1 | 28.0 | 28.5 |
| 2 (April–June) | 20.9 | 20.5 | 20.5 | 20.2 |
| 3 (July–September) | 19.8 | 19.6 | 19.4 | 19.8 |
| 4 (October–December) | 30.6 | 31.8 | 32.1 | 31.6 |
| Zip code | ||||
| Total zip codes | 535 | 714 | 511 | 603 |
| Population <18 years old (mean)b | 3829 | 2725 | 3367 | 2450 |
| Population density <18 years old (people/km2)b | 147.1 | 31.2 | 39.5 | 17.9 |
| Area (km2)b | 127.0 | 389.8 | 386.7 | 437.8 |
| Urban population (%)b | 55.5 | 34.7 | 40.7 | 30.9 |
| Non-White (%)b | 23.0 | 18.6 | 19.7 | 17.8 |
| Hispanic (%) b | 27.1 | 24.1 | 23.3 | 25.2 |
| Respiratory hazard indexc | 1.5 | 1.1 | 1.2 | 1.1 |
| Natural gas drilling sites (sites/km2) | 0 | 0.17 | 0.24 | 0.17 |
| County | ||||
| Median income ($)d | 41 974 | 40 360 | 41 912 | 39 744 |
| Poverty <18 years old (%)d | 22.5 | 24.3 | 23.7 | 24.6 |
| Unemployment rate (%)e | 5.6 | 6.1 | 6.2 | 6.1 |
0 NGD sites, included observations never have sites drilled between 2000 and 2010 in the zip code. ≥1 NGD sites, included observations have at least one site drilled between 2000 and 2010 in the zip code by the instance of the observation. ≥1 Unconventional NGD sites, included observations have at least one unconventionally drilled well in the zip code between 2000 and 2010 at the time of the hospitalization record. ≥1 Conventional NGD sites, included observations have at least one site conventional site drilled between 2000 and 2010 in the zip code by the instance of the observation. Since some zip codes experience both unconventional and conventional drilling during our study period, ≥1 unconventional NGD sites and ≥1 conventional NGD sites are not mutually exclusive categories.
Derived from 2000 U.S. Census population estimates.
Derived from 2005 National Air Toxic Assessment.
Derived from annual 2000–10 U.S. Census Small Area Income and Poverty Estimates.
Derived from annual 2000–10 U.S. Bureau of Labor Statistics.
Figure 2.
Flaring Volume from 2000 to 2010. Parts of Texas do not have an assigned zip code in 2000, which is shown via the white space. A total of 1249 zip codes are included in this analysis by quarter between 2000 and 2010. MCF = Thousand cubic feet.
Figure 3.
Production Volume from 2000 to 2010. Parts of Texas do not have an assigned zip code in 2000, which is shown via the white space. A total of 1249 zip codes are included in this analysis by quarter between 2000 and 2010. MCF = Thousand cubic feet.
Associations of NGD site activities with asthma hospitalizations
Our results demonstrate consistently elevated odds ratios for at least one quarterly paediatric asthma hospitalization for drilling within a zip code (Table 3). In general, Models 1 and 2 yield much higher odds ratios than Model 3, which demonstrates the importance of capturing county-level time-invariant variation.
Table 3.
Associations among type of drilling activity and odds of ≥1 paediatric asthma hospitalizations per quarter by zip code
| Model Specificationa,b | All drilling | Conventional | Unconventional | Flaring volume | Production volume |
|---|---|---|---|---|---|
| Odds ratio | Odds ratio | Odds ratio | Odds ratio | Odds ratio | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| Model 1: communityc (n = 1249 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 0.99 | 1.07 | 1.49 | 1.18 | 1.03 |
| (0.93, 1.06) | (1.01, 1.15) | (1.39, 1.60) | (1.00, 1.39) | (0.97, 1.10) | |
| Medium | 1.42 | 1.15 | 1.72 | 1.64 | 1.47 |
| (1.34, 1.50) | (1.08, 1.22) | (1.61, 1.84) | (1.40, 1.92) | (1.38, 1.56) | |
| High | 1.28 | 1.14 | 1.66 | 1.38 | 2.03 |
| (1.21, 1.37) | (1.06, 1.22) | (1.53, 1.79) | (1.17, 1.63) | (1.90, 2.17) | |
| Model 2: temporald (n = 1249 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.04 | 1.14 | 1.54 | 1.17 | 1.03 |
| (0.97, 1.11) | (1.07, 1.23) | (1.43, 1.65) | (0.99, 1.38) | (0.96, 1.10) | |
| Medium | 1.52 | 1.23 | 1.79 | 1.55 | 1.48 |
| (1.43, 1.62) | (1.15, 1.31) | (1.67, 1.92) | (1.31, 1.82) | (1.40, 1.58) | |
| High | 1.48 | 1.27 | 1.83 | 1.32 | 2.04 |
| (1.39, 1.58) | (1.17, 1.36) | (1., 1.98) | (1.12, 1.57) | (1.90, 2.18) | |
| Model 3: temporal and spatiale (n = 1249 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.22 | 1.20 | 1.24 | 1.25 | 1.23 |
| (1.12, 1.32) | (1.11, 1.31) | (1.13, 1.35) | (1.02, 1.54) | (1.13, 1.33) | |
| Medium | 1.51 | 1.23 | 1.59 | 1.13 | 1.45 |
| (1.40, 1.64) | (1.13, 1.34) | (1.46, 1.73) | (0.93, 1.38) | (1.34, 1.57) | |
| High | 1.27 | 1.10 | 1.49 | 0.68 | 1.53 |
| (1.16, 1.39) | (0.99, 1.22) | (1.36, 1.64) | (0.55, 0.84) | (1.38, 1.69) | |
Models exclude all zip codes not located on a shale basin or play. Conventional drilling includes a covariate for the cumulative number of unconventional sites drilled in that observation. Unconventional drilling includes a covariate for the cumulative number of conventional sites drilled in that observation.
Zip codes in counties with no variation in the outcome drop out of some analyses due to the county fixed effect included in each model. Full sample includes 1249 zip codes.
Model 1 is adjusted for community characteristics. These models include historical drilling activity in 1990–99, 2005 NATA total respiratory hazard, area of zip code in square kilometers, 2000 population density of people <18 years old by zip code, 2000 census percent Hispanic by zip code, 2000 census percent non-White by zip code, annual county poverty percent <18 years old, annual county unemployment rate and annual county median household income.
Model 2 is the same as Model 1 with the addition of temporal (year and quarter) fixed effects.
Model 3 is the same as Model 2 with the addition of spatial (county) fixed effects.
Since there is substantial variation across time and space in our sample, we focus on the results from Model 3, where this variation is captured. For all drilling, we found that zip codes in the highest tertiles of drilling had on average 27% [95% confidence interval (CI): 1.16, 1.39] higher odds of at least one paediatric asthma hospitalization per quarter, relative to zip codes with no drilling. We see elevated odds ratios in the lowest and medium tertiles at 1.22 (95% CI: 1.12, 1.32) and 1.51 (95% CI: 1.40, 1.64), respectively. Results from models with unconventional drilling yield increased odds across tertiles of 1.24 (95% CI: 1.13, 1.35), 1.59 (95% CI: 1.46, 1.73) and 1.49 (95% CI: 1.36, 1.64), respectively. For conventional drilling, we observed odds ratios of 1.20 (95% CI: 1.11, 1.31), 1.23 (95% CI: 1.13, 1.34) and 1.10 (95% CI: 0.99, 1.22). Models with flaring volume also demonstrate an inverse exposure–response, with zip codes in tertiles of flaring volume having odds ratios of 1.25 (95% CI: 1.02, 1.54), 1.13 (95% CI: 0.93, 1.38) and 0.68 (95% CI: 0.55, 0.84), respectively, relative to zip codes with no reported flaring. Production volume relative to no production yields elevated odds ratios of 1.23 (95% CI: 1.13, 1.33), 1.45 (95% CI: 1.34, 1.57) and 1.53 (95% CI: 1.38, 1.69). We found similar, if attenuated, results in sensitivity analyses using different cut points for hospitalizations for all exposure metrics, except conventional drilling where we no longer observed an association between natural gas development and asthma hospitalizations (Supplementary Table 3, available as Supplementary data at IJE online), and examined co-occurrence of conventional and unconventional drilling via interaction models (Supplementary Table 4, available as Supplementary data at IJE online).
When stratified by age group, associations remain largely similar to the all-ages models across all exposure metrics (Table 4). We then stratified models by specific subgroups of the Texas population that may be differentially burdened by NGD activity at the zip code level, where we use tertiles for population demographics (Table 5). For zip codes with a large Hispanic population (>27.3%), we found elevated risks of an attenuated magnitude with wide CIs, most notably in the unconventional drilling results: odds ratios of 0.92 (95% CI: 0.75, 1.09), 1.40 (95% CI: 1.18, 1.66) and 1.30 (95% CI: 1.08, 1.56). For populations with a large racial minority population, we found similar odds ratios to full models across most exposure metrics. However, we observed lower risks of at least one quarterly paediatric asthma hospitalization in most of our first tertile results. We also found that the flaring results are of a much larger magnitude for the urban population, where we see odds ratios of 1.64 (95% CI: 1.17, 2.30) in the first tertile. In models stratified by shale basin, the associations of all NGD with paediatric asthma do not vary greatly among these geological formations in different parts of the state (Supplementary Table 5, available as Supplementary data at IJE online). In models stratified by years (2000–04; 2005–10), we found that associations are similar with wider CIs (Supplementary Table 6, available as Supplementary data at IJE online).
Table 4.
Stratified models by age group, type of drilling activity and odds of ≥1 paediatric asthma hospitalizations per quarter by zip codea
| Age categoryb | All drilling | Conventional | Unconventional | Flaring volume | Production volume |
|---|---|---|---|---|---|
| Odds ratio | Odds ratio | Odds ratio | Odds ratio | Odds ratio | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| Ages 1–4 years (n = 1247 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.24 | 1.24 | 1.18 | 1.33 | 1.19 |
| (1.14, 1.36) | (1.13, 1.36) | (1.07, 1.30) | (1.08, 1.63) | (1.09, 1.30) | |
| Medium | 1.42 | 1.22 | 1.45 | 1.15 | 1.33 |
| (1.32, 1.54) | (1.12, 1.33) | (1.33, 1.59) | (0.95, 1.39) | (1.22, 1.44) | |
| High | 1.24 | 1.03 | 1.49 | 0.70 | 1.41 |
| (1.14, 1.36) | (0.93, 1.15) | (1.36, 1.63) | (0.57, 0.88) | (1.28, 1.56) | |
| Ages 5–9 years (n = 1230 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.25 | 1.14 | 1.24 | 1.50 | 1.08 |
| (1.13, 1.38) | (1.03, 1.26) | (1.12, 1.39) | (1.21, 1.86) | (0.98, 1.19) | |
| Medium | 1.38 | 1.08 | 1.58 | 1.07 | 1.33 |
| (1.27, 1.51) | (0.98, 1.19 | (1.44, 1.73) | (0.85, 1.32) | (1.22, 1.46) | |
| High | 1.16 | 0.98 | 1.40 | 0.76 | 1.26 |
| (1.06, 1.28) | (0.88, 1.10) | (1.28, 1.55) | (0.60, 0.96) | (1.13, 1.40) | |
| Ages 10–14 years (n = 1213 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.14 | 0.95 | 1.06 | 1.15 | 1.13 |
| (1.01, 1.29) | (0.83, 1.08) | (0.93, 1.21) | (0.89, 1.49) | (1.01, 1.26) | |
| Medium | 1.35 | 1.04 | 1.61 | 1.41 | 1.25 |
| (1.22, 1.49) | (0.93, 1.16) | (1.45, 1.79) | (1.12, 1.78) | (1.13, 1.39) | |
| High | 1.09 | 0,83 | 1.43 | 1.11 | 1.31 |
| (0.98, 1.21) | (0.73, 0.96) | (1.28, 1.59) | (0.86, 1.44) | (1.16, 1.48) | |
| Ages 15–17 years (n = 1082 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.27 | 0.96 | 1.05 | 1.07 | 1.02 |
| (1.07, 1.51) | (0.80, 1.17) | (0.86, 1.28) | (0.74, 1.57) | (0.85, 1.21) | |
| Medium | 1.07 | 0.88 | 1.33 | 0.97 | 1.23 |
| (0.92, 1.24) | (0.74, 1.04) | (1.14, 1.56) | (0.68, 1.38) | (1.05, 1.43) | |
| High | 0.89 | 0.76 | 1.08 | 0.74 | 1.19 |
| (0.76, 1.05) | (0.62, 0.93) | (0.91, 1.28) | (0.51, 1.09) | (0.99, 1.43) | |
Models exclude all zip codes not located on a shale basin or play. Covariates in all models include year, quarter, county, historical drilling activity in 1990–99, 2005 NATA total respiratory hazard, area of zip code in square kilometers, 2000 population density of people <18 years old by zip code, 2000 census percent Hispanic by zip code, 2000 census percent non-White by zip code, annual county poverty percent <18 years old, annual county unemployment rate and annual county median household income. Conventional drilling includes a covariate for the cumulative number of unconventional sites drilled in that observation. Unconventional drilling includes a covariate for the cumulative number of conventional sites drilled in that observation.
Zip codes in counties with no variation in the outcome drop out of some analyses due to the county fixed effect included in each model. Full sample includes 1249 zip codes.
Table 5.
Stratified models by demographic characteristics, type of drilling activity and odds of ≥1 paediatric asthma hospitalizations per quarter by zip code
| Demographic categorya,b | All drilling | Conventional | Unconventional | Flaring volume | Production volume |
|---|---|---|---|---|---|
| Odds ratio | Odds ratio | Odds ratio | Odds ratio | Odds ratio | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| >27.3% Hispanicc (n = 439 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.18 | 1.07 | 0.92 | 1.29 | 0.58 |
| (1.00, 1.40) | (0.89, 1.28) | (0.77, 1.09) | (0.94, 1.79) | (0.49, 0.68) | |
| Medium | 1.39 | 1.20 | 1.40 | 1.14 | 0.96 |
| (1.20, 1.61) | (1.03, 1.41) | (1.18, 1.66) | (0.86, 1.52) | (0.82, 1.12) | |
| High | 1.10 | 0.92 | 1.30 | 0.63 | 1.10 |
| (0.94, 1.29) | (0.77, 1.10) | (1.09, 1.56) | (0.46, 0.85) | (0.90, 1.35) | |
| >24.2% Non-Whitec (n = 458 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.31 | 0.95 | 0.94 | 0.86 | 0.94 |
| (1.11, 1.53) | (0.81, 1.12) | (0.79, 1.12) | (0.59, 1.26) | (0.81, 1.10) | |
| Medium | 1.41 | 1.25 | 1.37 | 1.12 | 1.10 |
| (1.23, 1.63) | (1.07, 1.46) | (1.17, 1.59) | (0.79, 1.59) | (0.95, 1.28) | |
| High | 1.06 | 0.84 | 1.17 | 1.04 | 1.32 |
| (0.91, 1.24) | (0.70, 1.01) | (0.99, 1.37) | (0.72, 1.51) | (1.09, 1.59) | |
| <$35 934 Medianc household income (n = 356 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.29 | 1.20 | 1.23 | 1.03 | 1.47 |
| (1.12, 1.49) | (1.03, 1.39) | (1.05, 1.43) | (0.75, 1.42) | (1.25, 1.72) | |
| Medium | 1.37 | 1.13 | 1.69 | 0.90 | 1.67 |
| (1.16, 1.61) | (0.96, 1.35) | (1.42, 2.02) | (0.66, 1.22) | (1.42, 1.96) | |
| High | 1.46 | 1.46 | 1.46 | 0.39 | 1.87 |
| (1.19, 1.79) | (1.18, 1.80) | (1.11, 1.92) | (0.27, 0.57) | (1.52, 2.30) | |
| Rural (0% urban population) (n = 486 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.13 | 1.22 | 1.12 | 0.75 | 1.30 |
| (0.97, 1.31) | (1.04, 1.43) | (0.94, 1.33) | (0.45, 1.25) | (1.10, 1.53) | |
| Medium | 1.29 | 1.31 | 1.25 | 0.87 | 1.46 |
| (1.08, 1.55) | (1.09, 1.56) | (1.02, 1.53) | (0.56, 1.33) | (1.22, 1.75) | |
| High | 1.63 | 1.58 | 1.35 | 0.35 | 1.57 |
| (1.32, 2.01) | (1.29, 1.95) | (1.07, 1.71) | (0.21, 0.59) | (1.26, 1.94) | |
| Urban (>60% urban population) (n = 576 zip codes) | |||||
| None | Ref | Ref | Ref | Ref | Ref |
| Low | 1.41 | 1.14 | 1.18 | 1.64 | 1.47 |
| (1.20, 1.66) | (0.96, 1.34) | (0.98, 1.42) | (1.17, 2.30) | (1.25, 1.72) | |
| Medium | 1.63 | 1.34 | 1.61 | 1.35 | 1.42 |
| (1.44, 1.86) | (1.16, 1.55) | (1.38, 1.87) | (0.98, 1.87) | (1.24, 1.63) | |
| High | 1.42 | 1.21 | 1.74 | 1.19 | 1.57 |
| (1.24, 1.63) | (1.01, 1.44) | (1.52, 2.00) | (0.83, 1.70) | (1.32, 1.88) | |
Models exclude all zip codes not located on a shale basin or play. Covariates in all models include year, quarter, county, historical drilling activity in 1990–99, 2005 NATA total respiratory hazard, area of zip code in square kilometers, 2000 population density of people <18 years old by zip code, 2000 census percent Hispanic by zip code, 2000 census percent non-White by zip code, annual county poverty percent <18 years old, annual county unemployment rate and annual county median household income. Conventional drilling includes a covariate for the cumulative number of unconventional sites drilled in that observation. Unconventional drilling includes a covariate for the cumulative number of conventional sites drilled in that observation.
Zip codes in counties with no variation in the outcome drop out of some analyses due to the county fixed effect included in each model. Full sample includes 1249 zip codes.
Hispanic and minority category cut points correspond to the top tertile of each demographic group by zip code. Household income categories corresponds to the bottom tertile of this demographic group by zip code.
Discussion
We examined associations between NGD and paediatric asthma hospitalizations in a diverse Texas population from 2000 through 2010. These results demonstrate that NGD is associated with paediatric asthma hospitalizations and that conventional drilling poses a similar, if not potentially larger, risk to paediatric asthma patients compared with unconventional drilling. Gas production volume is also associated with increased odds of at least one paediatric asthma hospitalizations in a qualitative exposure–response pattern. Flaring results are inconsistently associated with our asthma outcome, and these results change direction and magnitude. Our results hold across multiple sociodemographic characteristics and age groups. We note that accounting for county fixed effects attenuates all associations, indicating a clear need to account for time-invariant regional characteristics in analyses of NGD in Texas.
Our study examines the most severe asthma cases as indicated by hospitalizations. An asthma hospitalization represents a substantial burden upon the patient and family as well as lost productivity from missed days of school and increased risks for other chronic conditions.52–54 A recent literature review calculates that each paediatric asthma hospitalization costs $3076–$13 612 on average in the USA, thus representing a potential financial strain on the patient and the healthcare system.55 Pollutants associated with NGD, such as particulate matter, sulfur dioxide and volatile organic compounds, have been implicated in increased asthma risks among children.56–58 In addition, there is substantial evidence indicating that outdoor air pollution can trigger asthma among children and adolescents.59–61 Previous studies have linked flaring with increased sulfur dioxide exposure, which has also been associated with asthma exacerbations.56,57,59,60
Our results from unconventional NGD models largely agree with existing literature in direction and magnitude, but most research specifically on asthma to date has used Pennsylvania data.35,43,62 Rasmussen et al.62 examined asthma hospitalizations within the same cohort as Koehler et al.35 and found consistently elevated odds ratios from 1.10 (95% CI: 0.92, 1.30) to 1.74 (95% CI: 1.45, 2.09) using an inverse distance-squared metric for unconventional NGD production only. Koehler et al.35 explored associations between unconventional NGD and mild asthma exacerbations among a sample of people aged 5–90 years and observed mixed results depending on the exposure metrics used. For exposures assigned using an unconventional NGD activity index, they found an increase of up to 3.69 (95% CI: 3.16, 4.30). Willis et al.43 used paediatric hospitalizations in a study design similar to this analysis and found up to a 1.39 (95% CI: 1.14, 1.71) increased risk of asthma hospitalizations across tertiles of unconventional NGD. In the present study using Texas data, we find odds ratios of up to 1.49 (95% CI: 1.36, 1.64) for unconventional NGD in our model that accounts for spatiotemporal variation, which is similar to what has been previously found in Pennsylvania. Unlike the previous work, we consistently find that our middle tertile experiences the highest odds of at least one paediatric asthma exacerbation, but the reasons for this association are unclear.
To date, few studies have examined associations among conventional drilling and asthma. Willis et al.43 examined the effect of co-occurring conventional drilling in Pennsylvania and demonstrated consistent associations between paediatric asthma hospitalizations and tertiles of unconventional drilling density: odds ratios of 1.14 (95% CI: 0.96, 1.35), 1.10 (95% CI: 0.92, 1.31) and 1.37 (95% CI: 1.12, 1.68), controlling for conventional activity. Our models in this analysis yield similar odds ratios of 1.22 (95% CI: 1.12, 1.32) in our lowest tertile, but these associations are much higher in our middle and highest unconventional NGD density zip codes than what was found in the Pennsylvania context. Furthermore, our results also indicate that conventional NGD is associated with paediatric asthma hospitalizations, which corresponds with hypotheses presented in existing commentaries and risk assessments calling for epidemiologic studies to examine both drilling types.1,33
Our results further suggest that production volume may be a relevant exposure pathway by which NGD could affect paediatric asthma. This finding also suggests that production volume by NGD site may correspond to air emissions that are hazardous to respiratory health, which agrees with the findings in Rasmussen et al.62 . Although we cannot examine specific NGD-related emissions, we examined flaring as a potential respiratory irritant from drilling activity. Our results weakly suggest that an increasing flaring volume from an NGD site is associated with an increased risk of at least one asthma hospitalization per quarter in urban areas but protective in rural areas. We also found instances where flaring shows lower odds of at least one asthma hospitalization per quarter after accounting for county, indicating that community context is a large factor. However, due to not including flaring from oil wells, our results may be attenuated. Given the coarse nature of our data, we are also unable to account for finer-scale time-varying sources of air pollution that may be contributing to our results in urban areas. Flaring represents a potential pathway by which children can be exposed to incomplete combustion byproducts that are respiratory irritants, such as polycyclic aromatic hydrocarbons and black carbon, causing concern in many communities.23,26,47 We also note that flaring volumes increased to their highest levels in 2018, so we may be underestimating the impact of this exposure in the present.63
Since we examined a diverse population, we assessed the impact of NGD on paediatric asthma hospitalizations among vulnerable communities prone to environmental inequities. We generally found that vulnerable communities are experiencing higher odds of paediatric asthma hospitalizations in each tertile of drilling, which shows that communities with lower income and more non-White population may be disproportionately burdened with NGD activity or biological responses to the pollution from this activity. This result aligns with existing literature on the demographics of populations residing near drilling sites.64 However, it is worth noting that our conventional drilling exposure model yields inconclusive risk estimates among our communities with high non-White populations. Previous work shows that unconventional NGD occurs in Texas communities with high populations of racial and ethnic minorities as well as low income status,65–68 though little work has been done on conventional drilling exposures. The U.S. Department of Energy is specifically instructed to monitor the impact of the energy sector on these communities, and the current study provides evidence that drilling exposures seem to be inequitably distributed in Texas.69,70 Additional work is needed to ensure that vulnerable communities are more adequately protected from NGD-related air emissions.
This study contains some limitations. First, exposure and outcome metrics were measured at the zip code level, so there is potential for exposure misclassification among patients. We are inherently unable to assess individual environmental exposures (e.g. tobacco smoke; indoor mold) that may be triggers for an exacerbation. However, this study design also allows us to control for unmeasured time-invariant spatial confounding via our county fixed effect and temporal confounding via our year and quarter fixed effects, which should absorb some time-varying unmeasured confounding. We showed that NGD is associated with paediatric asthma at a zip code level, which can inform local policies on NGD. Second, our analysis does not assess drilling sites permitted for only oil extraction. Previous work indicates that flaring occurs at a higher rate for oil sites, so we expect that our flaring models may underestimate the impact of flaring volume on quarterly paediatric asthma hospitalizations. Third, Texas does not maintain an air emissions inventory for NGD, so we cannot examine specific air pollutants that may be driving the results. We overcame this limitation through including gas flaring analysis, thus examining a potential mechanism of exposure that can translate into policy changes, but foud inconsistent results. Fourth, we were unable to examine outpatient visits for paediatric asthma exacerbations using available data. However, we anticipate that hospitalizations represent the most severe response that an asthmatic child or adolescent may have to NGD-related air pollution exposure. Fifth, some literature indicates that the TXRRC reports are likely a substantial underestimate of flaring volumes compared with satellite data,46,47 potentially leading to exposure misclassification in our data and explaining some of our protective associations with this metric. These satellite data are unavailable prior to 2012, thus they cannot be used for historical drilling exposures like those examined in this analysis.23 Sixth, there is considerable variation in zip codes in terms of population and size,71 thus controlling for socio-economic characteristics at the annual county level may be insufficient. Given data availability, we are inherently unable to control for socio-economic status at a finer scale (e.g. individual, zip code).
In conclusion, we found evidence that both unconventional and conventional drilling are associated with paediatric asthma hospitalizations, which has not been previously assessed. Our findings suggest that focusing just on unconventional drilling does not provide a full picture of the potential respiratory health effects of NGD. Additionally, gas production is a source of exposure associated with paediatric asthma. This result increases our confidence in production as a proxy for drilling intensity, an approach used in many existing health studies.62,72–75 Our results do not show consistent associations with flaring volume. However, these results change into large magnitude associations when we examine only urban areas, which provides some support for improving local regulations around when and where gas flaring can occur in cities. Increasing regulatory enforcement on policies such as limits on volume or duration of flaring or restrictions on production output near communities could reduce the impact of drilling on paediatric asthma. Overall, we provide evidence that NGD is associated with decreased respiratory health. Further work on specific air emissions and exposures is needed to determine what aspects of the NGD process drive decreases in respiratory health among local communities.
Supplementary data
Supplementary data are available at IJE online.
Supplementary Material
Funding
This work is supported by the Office of the Director of the National Institutes of Health [grant number DP5OD021338, PI: Hill], the National Institute of Environmental Health Sciences, National Institutes of Health [grant number F31 ES029801, PI: Willis], and the National Center for Advancing Translational Sciences of the National Institutes of Health [grant number TL1TR002371, PI: Morris/Fryer]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Enverus DrillingInfo for access to their proprietary databases for use in this analysis.
Conflict of interest
None declared.
References
- 1. Czolowski E, Santoro R, Srebotnjak T, Shonkoff S.. Toward consistent methodology to quantify populations in proximity to oil and gas development: a national spatial analysis and review. Environ Health Perspect 2017;125:086004–86011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Energy Information Administration. U.S. Energy Information Administration Annual Energy Outlook. Washington, DC: U.S. Department of Energy; 2017. United State Energy Information Administration (23 April 2017, date last accessed).
- 3.U.S. Energy Information Administration. Hydraulically Fractured Wells Provide Two-Thirds of U.S. Natural Gas Production-Today in Energy; 2016. https://www.eia.gov/todayinenergy/detail.php? id=26112 (29 March 2019, date last accessed).
- 4.U.S. Energy Information Administration. Natural Gas Explained: Where Our Natural Gas Comes From Washington, DC: United States Department of Energy; 2017. [Google Scholar]
- 5. Brown DR, Lewis C, Weinberger BI.. Human exposure to unconventional natural gas development: a public health demonstration of periodic high exposure to chemical mixtures in ambient air. J Environ Sci Health Part A 2015;50:460–72. [DOI] [PubMed] [Google Scholar]
- 6. Allen DT. Emissions from oil and gas operations in the United States and their air quality implications. J Air Waste Manag Assoc 2016;66:549–75. [DOI] [PubMed] [Google Scholar]
- 7. Prenni AJ, Day DE, Evanoski-Cole AR. et al. Oil and gas impacts on air quality in federal lands in the Bakken region: an overview of the Bakken Air Quality Study and first results. Atmos Chem Phys 2016;16:1401–416. [Google Scholar]
- 8. Allshouse WB, McKenzie LM, Barton K, Brindley S, Adgate JL.. Community noise and air pollution exposure during the development of a multi-well oil and gas pad. Environ Sci Technol 2019;53:7126–135. [DOI] [PubMed] [Google Scholar]
- 9. Eisele AP, Mukerjee S, Smith LA. et al. Volatile organic compounds at two oil and natural gas production well pads in Colorado and Texas using passive samplers. J Air Waste Manag Assoc 2016;66 https://www.tandfonline.com/doi/full/10.1080/10962247.2016.1141808. [DOI] [PubMed] [Google Scholar]
- 10.HEI Energy Research Committee. Human Exposure to Unconventional Oil and Gas Development: A Literature Survey for Research Planning. Boston, MA: Health Effects Institute-Energy; 2019. Report No.: Special Report 2. https://hei-energy.org/system/files/hei-energy-exposure-lit-rev-draft.pdf (24 October 2019, date last accessed).
- 11. Walters K, Jacobson J, Kroening Z, Pierce C.. PM2.5 airborne particulates near frac sand operations. J Environ Health 2015;78:8–12. [PubMed] [Google Scholar]
- 12. Bloomdahl R, Abualfaraj N, Olson M, Gurian PL.. Assessing worker exposure to inhaled volatile organic compounds from Marcellus Shale flowback pits. J Nat Gas Sci Eng 2014;21:348–56. [Google Scholar]
- 13. Brantley HL, Thoma ED, Eisele AP.. Assessment of volatile organic compound and hazardous air pollutant emissions from oil and natural gas well pads using mobile remote and on-site direct measurements. J Air Waste Manag Assoc 2015;65:1072–082. [DOI] [PubMed] [Google Scholar]
- 14. Nastos PT, Paliatsos AG, Anthracopoulos MB, Roma ES, Priftis KN.. Outdoor particulate matter and childhood asthma admissions in Athens, Greece: a time-series study. Environ Health 2010;9:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Acciani T, Brandt E, Pastura P, Hershey G, Cras TL.. Low dose diesel exhaust particle exposure exacerbates allergic asthma in young mice. Eur Respir J 2012;40(Suppl 56):P2333. [Google Scholar]
- 16. Zheng X, Ding H, Jiang L. et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS ONE 2015;10:e0138146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Neidell M. Information, avoidance behavior, and health the effect of ozone on asthma hospitalizations. J Hum Resour 2009;44:450–78. [Google Scholar]
- 18. Nurmatov UB, Tagiyeva N, Semple S, Devereux G, Sheikh A.. Volatile organic compounds and risk of asthma and allergy: a systematic review. Eur Respir Rev 2015;24:92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang I-J, Karmaus WJJ, Yang C-C.. Polycyclic aromatic hydrocarbons exposure, oxidative stress, and asthma in children. Int Arch Occup Environ Health 2017;90:297–303. [DOI] [PubMed] [Google Scholar]
- 20. Karimi P, Peters KO, Bidad K, Strickland PT.. Polycyclic aromatic hydrocarbons and childhood asthma. Eur J Epidemiol 2015;30:91–101. [DOI] [PubMed] [Google Scholar]
- 21. Carlton AG, Little E, Moeller M, Odoyo S, Shepson PB.. The data gap: can a lack of monitors obscure loss of clean air act benefits in fracking areas? Environ Sci Technol 2014;48:893–94. [DOI] [PubMed] [Google Scholar]
- 22. Colborn T, Schultz K, Herrick L, Kwiatkowski C.. An exploratory study of air quality near natural gas operations. Hum Ecol Risk Assess Int J 2014;20:86–105. [Google Scholar]
- 23. Elvidge C, Zhizhin M, Baugh K, Hsu F-C, Ghosh T.. Methods for global survey of natural gas flaring from visible infrared imaging radiometer suite data. Energies 2015;9:14. [Google Scholar]
- 24. McCawley M. Air contaminants associated with potential respiratory effects from unconventional resource development activities. Semin Respir Crit Care Med 2015;36:379–87. [DOI] [PubMed] [Google Scholar]
- 25. Goodman PS, Galatioto F, Thorpe N, Namdeo AK, Davies RJ, Bird RN.. Investigating the traffic-related environmental impacts of hydraulic-fracturing (fracking) operations. Environ Int 2016;89-90:248–60. [DOI] [PubMed] [Google Scholar]
- 26. Weyant CL, Shepson PB, Subramanian R. et al. Black carbon emissions from associated natural gas flaring. Environ Sci Technol 2016;50:2075–081. [DOI] [PubMed] [Google Scholar]
- 27. Glazer YR, Davidson FT, Lee JJ, Webber ME.. An inventory and engineering assessment of flared gas and liquid waste streams from hydraulic fracturing in the USA. Curr Sustain Energy Rep 2017;4:219–31. [Google Scholar]
- 28. Shonkoff SB, Hays J, Finkel ML.. Environmental public health dimensions of shale and tight gas development. Environ Health Perspect 2014;122:787–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bamberger M, Oswald RE.. Impacts of gas drilling on human and animal health. New Solut J Solut 2016;22:51–77. [DOI] [PubMed] [Google Scholar]
- 30.Pennsylvania Grade Crude Oil Coalition. Conventional Wells. http://www.pagcoc.org/conventional-wells/ (26 April 2019, date last accessed).
- 31. Hill LL, Czolowski ED, DiGiulio D, Shonkoff S.. Temporal and spatial trends of conventional and unconventional oil and gas waste management in Pennsylvania, 1991–2017. Sci Total Environ 2019;674:623–36. [DOI] [PubMed] [Google Scholar]
- 32. Korfmacher KS, Elam S, Gray KM, Haynes E, Hughes MH. Unconventional natural gas development and public health: toward a community-informed research agenda. Rev Environ Health 2014. http://www.degruyter.com/view/j/reveh.ahead-of-print/reveh-2014-0049/reveh-2014-0049.xml; jsessionid=DA6756BB23FC8D3106D6064D0D75FB94. [DOI] [PMC free article] [PubMed]
- 33. Adgate JL, Goldstein BD, McKenzie LM.. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environ Sci Technol 2014;48:8307–320. [DOI] [PubMed] [Google Scholar]
- 34. McKenzie LM, Witter RZ, Newman LS, Adgate JL.. Human health risk assessment of air emissions from development of unconventional natural gas resources. Sci Total Environ 2012;424:79–87. [DOI] [PubMed] [Google Scholar]
- 35. Koehler K, Ellis JH, Casey JA. et al. Exposure assessment using secondary data sources in unconventional natural gas development and health studies. Environ Sci Technol 2018. doi: 10.1021/acs.est.8b00507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Finkel ML, Hays J.. Environmental and health impacts of ‘fracking’: why epidemiological studies are necessary. J Epidemiol Community Health 2015;70:221–22. [DOI] [PubMed] [Google Scholar]
- 37.US Center for Disease Control. Most recent asthma data. 2018. https://www.cdc.gov/asthma/most_recent_data.htm (5 May 2018, date last accessed).
- 38. Li S, Williams G, Jalaludin B, Baker P.. Panel studies of air pollution on children’s lung function and respiratory symptoms: a literature review. J Asthma 2012;49:895–910. [DOI] [PubMed] [Google Scholar]
- 39. Orellano P, Quaranta N, Reynoso J, Balbi B, Vasquez J.. Effect of outdoor air pollution on asthma exacerbations in children and adults: systematic review and multilevel meta-analysis. PLoS ONE 2017;12:e0174050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Texas Department of State Health Services. Texas health care information collection inpatient public use data file. https://www.dshs.texas.gov/thcic/hospitals/Inpatientpudf.shtm (23 January 2018, date last accessed).
- 41. Jemielita T, Gerton GL, Neidell M. et al. Unconventional gas and oil drilling is associated with increased hospital utilization rates. PLoS ONE 2015;10:e0131093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Peng L, Meyerhoefer C, Chou S-Y.. The health implications of unconventional natural gas development in Pennsylvania. Health Econ 2018;27:956–83. [DOI] [PubMed] [Google Scholar]
- 43. Willis MD, Jusko TA, Halterman JS, Hill EL.. Unconventional natural gas development and pediatric asthma hospitalizations in Pennsylvania. Environ Res 2018;166:402–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Denham A, Willis M, Zavez A, Hill E.. Unconventional natural gas development and hospitalizations: evidence from Pennsylvania, United States, 2003–2014. Public Health 2019;168:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.DrillingInfo. 2017. http://info.drillinginfo.com/ (5 December 2017, date last accessed).
- 46. Willyard KA, Schade GW.. Flaring in two Texas shale areas: Comparison of bottom-up with top-down volume estimates for 2012 to 2015. Sci Total Environ 2019;691:243–51. [DOI] [PubMed] [Google Scholar]
- 47. Franklin M, Chau K, Cushing LJ, Johnston JE.. Characterizing flaring from unconventional oil and gas operations in South Texas using satellite observations. Environ Sci Technol 2019;53:2220–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.U.S. Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification. https://www.cdc.gov/nchs/icd/icd9cm.htm (28 June 2018, date last accessed).
- 49.IPUMS NHGIS. National Historical Geographic Information System; 2018. https://www.nhgis.org/ (11 January 2018, date last accessed).
- 50.US EPA O. 2005 National Air Toxics Assessment. US EPA; 2015. https://www.epa.gov/national-air-toxics-assessment/2005-national-air-toxics-assessment (April 5 2019, date last accessed).
- 51.U.S. Census Bureau. Small Area Income and Poverty Estimates Program. https://www.census.gov/programs-surveys/saipe.html (23 January 2018, date last accessed).
- 52. Stridsman C, Dahlberg E, Zandrén K, Hedman L. Asthma in adolescence affects daily life and school attendance–Two cross-sectional population-based studies 10 years apart. Nurs Open2017. [DOI] [PMC free article] [PubMed]
- 53. Adams JY, Sutter ME, Albertson TE.. The patient with asthma in the emergency department. Clinic Rev Allerg Immunol 2011;43:14–29. [DOI] [PubMed] [Google Scholar]
- 54. Nunes C, Pereira AM, Morais-Almeida M.. Asthma costs and social impact. Asthma Res Pract 2017;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Perry R, Braileanu G, Palmer T, Stevens P.. The economic burden of pediatric asthma in the United States: literature review of current evidence. PharmacoEconomics 2019;37:155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cai J, Zhao A, Zhao J. et al. Acute effects of air pollution on asthma hospitalization in Shanghai, China. Environ Pollut 2014;191:139–44. [DOI] [PubMed] [Google Scholar]
- 57. Deger L, Plante C, Jacques L. et al. Active and uncontrolled asthma among children exposed to air stack emissions of sulphur dioxide from petroleum refineries in Montreal, Quebec: a cross-sectional study. Can Respir J 2012;19:97–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Spira-Cohen A, Chen LC, Kendall M, Lall R, Thurston GD.. Personal exposures to traffic-related air pollution and acute respiratory health among Bronx schoolchildren with asthma. Environ Health Perspect 2011;119:559–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Guarnieri M, Balmes JR.. Outdoor air pollution and asthma. Lancet 2014;383:1581–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Strickland MJ, Darrow LA, Klein M. et al. Short-term Associations between Ambient Air Pollutants and Pediatric Asthma Emergency Department Visits. Am J Respir Crit Care Med 2010;182:307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tolbert PE, Mulholland JA, Macintosh DL. et al. Air quality and pediatric emergency room visits for Asthma and Atlanta, Georgia. Am J Epidemiol 2000;151:798–810. [DOI] [PubMed] [Google Scholar]
- 62. Rasmussen S, Ogburn E, McCormack M, Casey J, Bandeen-Roche K, Mercer et al. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA Intern Med 2016;176:1334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.DrillingInfo. OPEC, Flaring, Offshore Drilling, and More. Austin, TX; 2018. (Fundamental Edge). https://info.drillinginfo.com/drillinginfo-explores-leading-international-environmental-and-leasing-issues-affecting-energy-market/ (18 June 2019, date last accessed).
- 64. Zwickl K. The demographics of fracking: a spatial analysis for four U.S. states. Ecol Econ 2019;161:202–15. [Google Scholar]
- 65. Fry M. Urban gas drilling and distance ordinances in the Texas Barnett Shale. Energy Policy 2013;62:79–89. [Google Scholar]
- 66. Fry M, Briggle A, Kincaid J.. Fracking and environmental (in)justice in a Texas city. Ecol Econ 2015;117:97–107. [Google Scholar]
- 67. Murphy T, Brannstrom C, Fry M, Ewers M. Economic-development stakeholder perspectives on boomtown dynamics in the Eagle Ford Shale, Texas. Geogr Rev2016.
- 68. Johnston JE, Werder E, Sebastian D.. Wastewater disposal wells, fracking, and environmental injustice in Southern Texas. Am J Public Health 2016;106:550–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Department of Energy. What is environmental justice? 2016. https://www.energy.gov/lm/services/environmental-justice/what-environmental-justice (29 June 2018, date last accessed).
- 70. Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD.. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff (Millwood) 2011;30:879–87. [DOI] [PubMed] [Google Scholar]
- 71. Grubesic TH, Matisziw TC.. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geogr 2006;5:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Casey JA, Savitz DA, Rasmussen SG. et al. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology2015. [DOI] [PMC free article] [PubMed]
- 73. Hill EL. Shale gas development and infant health: evidence from Pennsylvania. J Health Econ 2018;61:134–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. McKenzie LM, Guo R, Witter RZ, Savitz DA, Newman LS, Adgate JL.. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect 2014;122:412–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Whitworth K, Marshall A, Symanski E.. Drilling and production activity related to unconventional gas development and severity of preterm birth. Environ Health Perspect 2018;126:037006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.