Abstract
Background
The recent COVID-19 pandemic pointed out new burdens for researchers on mental health and that evidence-based (EB) studies on vulnerable populations are timely needed. The present paper aims at analysing the impact of suspicious of SARS-COV-2 infection in a cohort of parents presented at 3 major hospitals (spread between north and center of Italy) during the Italian COVID-19 pandemic phase 1.
Methods
Participants of the present cross-sectional, multicenter study were parental couples of children suspected to have COVID-19 who underwent testing with nasopharyngeal swabbing. All subjects were assessed by means of the: Impact of Event Scale-Revised (IES-R), Generalized Anxiety Disorder 7-Item (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) in order to evaluate Post-traumatic stress (PTSS), anxiety, and depressive symptoms, respectively.
Outcomes
Results evidenced that parents whose children tested positive for COVID-19 were more prone to developing PTSS, anxiety and depressive symptoms. The same results emerged for parents who had quarantined as opposed to those who had not. Moreover, patients who suffered economic damage showed a higher prevalence of anxiety and depressive symptoms, whereas PTSS was more common among unemployed subjects and among mothers.
Interpretation
This study identified a mental health strain represented by parenting a child who tested positive for SARS-CoV-2 infection. Further EB research is needed to develop evidence-driven strategies to reduce adverse psychological impacts and related psychiatric symptoms in caregivers of COVID-19 infected children during the next phases of the pandemic.
Keywords: COVID-19, SARS-COV-2, Parents, PTSS, Anxiety, Depression
1. Introduction
Within a few months, the COVID-19 pandemic not only impacted the physical health and financial status of millions of people, but also represented a severe threat for their mental health with a real burden that will only clearly emerge in the long term (Cleland 2020; Galletly 2020; Unützer et al., 2020; Ćosić et al., 2020).
Italy was the first European country to face COVID-19 emergency and one of the most affected; after the first cluster of confirmed cases in the Lombardy Region in late February 2020, the SARS-CoV-2 infection spread to all regions across the country in the following weeks, causing more than 230,000 confirmed cases and more than 33,000 deaths to date. Italians had to rapidly adapt to the emergency measures with restrictions on personal freedom and recommended changes in habits and schedules (Lazzerini and Putoto 2020; Tuite et al., 2020).
The COVID-19 pandemic is likely threatening people's physical health and lives, as well as increasing their stress levels and triggering a wide range of mental health problems (Harper et al., 2020; Pakpour and Griffiths 2020; Taylor and Blackford 2020). In previous exceptional outbreaks of infectious diseases, such as the 2003 Severe Acute Respiratory Syndrome (SARS) or the 2015 Middle East Respiratory Syndrome-CoronaVirus (MERS-CoV) epidemics, features like the contagion risk or the loss of loved ones, in addition to quarantine-related changes in daily habits, were proven to induce the development of psychological distress and different degrees of psychopathological sequelae, experiencing fear and worries, anxiety, depressive symptoms, Post-Traumatic Stress Disorder (PTSD) and Post-Traumatic Stress Symptoms (PTSS) (Rogers et al., 2020).
The outbreak may trigger disturbing feelings of helplessness, fear of death and hopelessness, which frequently arise when people face a real or perceived threat, leading to post-traumatic stress reactions (Pakpour and Griffiths 2020). PTSS refer to symptoms specifically related to traumatic events with characteristic features, including re-experiencing, avoidance, negative alterations in cognition and mood, as well as hyperarousal symptoms (Buselli et al., 2020, Kingston et al., 2016). In this regard, some pieces of evidence have already emerged in the light of the COVID-19 pandemic pointing out significant levels of anxiety, depression and PTSS(Li et al., 2020; Liu et al., 2020; Wang et al., 2020). Noteworthy findings emerged from the first nationwide large-scale survey in the general population of China with the emerging of high levels of peri-traumatic psychological distress (almost 35% of the whole population), with significantly higher rates among females and younger subjects (18–30 years) (Carmassi et al., 2014; Qiu et al., 2020), confirming literature data on the crucial role of specific risk factors, such as age and gender, as vulnerability factors for post-traumatic stress reactions (Carmassi et al., 2020).
Data from two further extensive studies in Chinese general population also revealed high levels of anxiety and depressive symptoms. Particularly, Wang et al. showed that about 17% and 30% of respondents during the initial stage of COVID-19 emergency exhibited moderate to severe depressive and anxiety symptoms, respectively (Wang et al., 2020), whilst Li and colleagues found rates of anxiety or depression or both as high as 20,4% at the peak of the epidemic (Li et al., 2020). Features such as gender, occupation and level of education have been found to influence the development of anxiety and depressive symptoms during the pandemic (Wang et al., 2020).
Illness of one's child is acknowledged to be one of the most destabilizing events for a parent, having a significant impact on parent psychological wellbeing (Carmassi et al., 2018, Corsi et al., 2021). It brings an increased risk of developing a wide range of psychopathological sequelae, such as depression, anxiety and PTSS up to full blown PTSD (van Oers et al., 2014; Carmassi et al. 2017, 2019). All these mental disorders have been associated with diminished quality of life and significant effects on several areas of a person's life, included negative consequences on caregiving role of affected individuals (Kessler et al., 2005; Dell'osso et al., 2014; Carmassi et al., 2017; Muzik et al., 2017).
Despite COVID-19 in children mostly presenting as either asymptomatic or with lighter symptoms than those typically seen in adults, the mere suspicion of COVID-19 infection in children can be a destabilizing event for a parent. Many factors could contribute to the traumatic impact of the event. For instances, the fear of contagion for themselves, which could affect the parenting role (Fontanesi et al., 2020).
The Diagnostical and Statistical Manual of Mental Disorders (DSM) (APA, 2013) itself progressively introduced illness in one's child among the events considered as traumatic. It specifies that the event must be “a medical catastrophe concerning one's child”, a condition that endangers life at the moment highlighting the need for the event to be sudden and dangerous, with attention on the urgency and abruptness of the perceived threat (Carmassi et al., 2018; 2019; Dell'Osso et al., 2018). A review on early traumatic response among parents in the acute period post-diagnosis of a serious illness in their child (within three months), showed that up to one-quarter to one-third of parents experience significant PTSS following the diagnosis of a severe disease in their child (Woolf et al., 2016).
Fear is generally a primitive feeling and arises in the face of a real or perceived threat. Accordingly, the fear of COVID-19 can be thought to have the potential to affect negatively parents mental health and this may hamper the ability of parents to make decisions and to provide adequate emotional support to their children (Landolt et al., 2012; Carmassi et al., 2020).
Two of the core symptoms of PTSS, avoidance and hyperarousal, have been put forth in the literature regarding their potential importance as pathogenic mechanisms of distress. Avoidance of external and internal aversive stimuli has been proposed as central for the development and maintenance of psychiatric symptoms in general and of PTSS specifically. Furthermore, avoidance has been identified as a mediator between re-experiencing and general distress in the Cognitive Processing Model. Hyperarousal is a core symptom not only in PTSS, but also in anxiety disorder (Cernvall et al., 2011).
Another important concept that derives from stress models, concerns the female gender. As compared to men, women with trauma exposure exhibit greater sensitivity and lower tolerance to negative emotions (Harper et al., 2020; Pakpour and Griffiths, 2020). Consistently, women seem to have a more sensitized hypothalamus–pituitary–axis than men. Further, women present more cognitive symptoms in response to stress than men, such as self-blame and negative alterations in beliefs (Rogers et al., 2020; Kingston et al., 2016). Women are known to engage to a greater degree in cognitive styles that may put them at greater risk for distress. Repetitive negative thinking and rumination seem to be linked to the development and maintenance of it (Wang et al., 2020; Li et al., 2020; Liu et al., 2020; Qiu et al., 2020). Ruminative thoughts have also been suggested to be a dangerous element able to trigger suicidal behaviors (Qiu et al., 2020; Carmassi et al., 2014).
In light of these conceptual models, the present paper aimed at exploring psychopathological symptoms in caregivers of children tested for probable COVID-19 infection at the Pediatric Emergency Departments of four major hospitals in Italy, in the acute phase of the pandemic. In particular, we paid attention to PTSS, anxiety and depressive symptoms which are the core cluster dimensions of distress. So far, no data have been yet reported regarding the psychological burden among parents of children with suspected infection from SARS-CoV-2 (COVID-19).
2. Methods
2.1. Procedures and study participants
A multicenter, cross-sectional study was designated and conducted in accordance with the STROBE recommendation for observational studies. It was coordinated by clinicians and researchers of the Azienda Ospedaliero-Universitaria Pisana (Pisa) and included clinicians and researchers of the Azienda Ospedaliero-Universitaria Sant’Orsola Malpighi (Bologna) and Fondazione IRCSS Policlinico San Matteo (Pavia). Parents of children with suspected COVID-19 infections, who accessed the Pediatric Emergency Departments of one of these three major University Hospitals and performed a diagnostic assessment for COVID-19 in their children (nasopharyngeal swabbing for SARS-CoV-2), were consecutively recruited for the study and assessed within two weeks of receiving the test results. Enrollment was held between 1st and April 30, 2020.
Exclusion criteria included poor knowledge and understanding of the Italian Language or other limits to verbal communication, and being younger than 18. All eligible parents were asked to provide written informed consent after receiving a complete description of the study and having an opportunity to ask questions. The study received the approval of the Ethics Committee of Area Vasta Nord Ovest Toscana and the other Ethics Committees of the involved Centers.
After eliminating individuals who did not wish to participate, or who were deemed ineligible due to age, language or limits to verbal communication or retirement status, eligible subjects at the baseline were 96, with a response rate of 52,7%.
2.2. Measures
Data on social, demographic and clinical variables were also collected from each participant: age, marital status, employment status, education level, number of children, personal and familiar history of psychiatric disorders, age of the sick children. Additional information regarding social, clinical and demographic variables related to the COVID-19 emergency was also gathered through a specific datasheet. Recruited subjects were assessed using self-report questionnaires: PTSS, depressive as well as anxiety symptoms were measured as follows.
2.2.1. PTSS
PTSS were investigated through the Impact of Event Scale-Revised (IES-R, Weiss & Marmar, 1997 (Weiss et al., 1997)). The IES-R is a 22-item scale measuring three core phenomena of PTSD, i.e., re-experiencing of traumatic events, defensive avoidance and denial of trauma-related memories and emotions. It refers to the applicable prior week. The questionnaire has adequate internal consistency (Cronbach's α for each subscale: intrusion = 0.87 to 0.94, avoidance = 0.84 to 0.97, hyperarousal = .79 to .91), and high test-retest reliability (r = 0.93). Further, internal consistency of the test performed for the current study is excellent (Cronbach's α = 0.92). A score over 24 represents a cutoff for the presence of moderate to severe PTSS. According to the aim of the study, the items referred to the suspected COVID-19 infection of their sons.
2.2.2. Anxiety symptoms
Anxiety symptoms were assessed using the Generalized Anxiety Disorder 7-Item (GAD-7, Spitzer et al., 2006 (Spitzer et al., 2006)). The GAD-7 is a self-assessment questionnaire used as a tool for screening and measuring the severity of anxiety symptoms. In particular, it investigates the frequency of anxiety symptoms in the prior two weeks using a seven-item with a score ranging from 0 = never to 3 = almost every day. The internal consistency of the GAD-7 is excellent (Cronbach's α = 0.92) test-retest reliability is also good (r = 0.83). Cronbach's α tested for the current study is good (Cronbach's α = 0.87). Scores over 10 suggest the presence of moderate to severe anxiety symptoms.
2.2.3. Depressive symptoms
Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9) (Kroenke 2001 (Kroenke et al., 2001)). PHQ-9 is a 9-item self-administered scale measuring depressive symptoms severity in the prior two weeks on a 4-point scale from 0 = not at all to 3 = nearly every day, with the total score ranging from 0 to 27. A cutoff score of 10 has been shown to have a sensitivity of 88% and a specificity of 88% specificity for major depression. The test has adequate internal consistency (Cronbach's α = 0.89), excellent test-retest reliability (r = 0.84) and internal consistency for the current study is also good (Cronbach's α = 0.84).
2.2.4. Statistical analyses
Continuous variables were reported as mean ± standard deviation (SD), whereas categorical variables were reported as percentages. All tests were two-tailed and a p-value <.05 was considered statistically significant. Chi-square test (or Fisher test when appropriate) was used to compare socio-demographical and clinical characteristics, between individuals with and without PTSS, Anxiety and Depressive symptoms. To study all possible effects of socio-demographic variables associated to PTSS, anxiety and depressive symptoms, respectively, in univariate analysis (and their possible interactions) three Decision Tree procedures based on the Chi-squared Automatic Interaction Detection (CHAID) growing method were used. The tree-based classification model can predict the values of the dependent variable based on the values of the independent ones.
Statistical analysis was performed using the Statistical Package for Social Science, version 25.0 (SPSS Inc.).
3. Results
The entire sample comprised 96 parents; 60 (62.5%) mothers and 36 (37.5%) fathers, with a mean age of 40.79 ± 8.22 years. Seventy-five (78.1%) parents were married or cohabiting, 68 (70.8%) had more than one child, a large proportion were unemployed (81, 84.4% and about one third (32, 33.3%) had a university degree.
In the framework of the COVID-19 emergency, 58 parents (60.4%) had a child who tested positive for COVID-19, 16 (16.7%) had a child at risk for medical complications of COVID-19, 39 tested positive themselves for COVID-19, 68 (70.8%) subjects were in quarantine and 21.9% presented a risk for medical complications arising from COVID-19. Furthermore, 22 (22.9%) of the parents reported a family member at risk for medical complications arising from COVID-19, 56 (58.3%) presented a relative or a close one positive to COVID-19 and 17 (17.7%) reported the death of a relative or a close one as a result of the COVID-19 infection.
A total of 38 (39.6%) parents reported moderate to severe PTSS (IES-R score≥24). Specifically, PTSS rates were significantly higher among: (i) mothers than fathers [30 (50%) versus 8 (22.2%), p = .013]; (ii) parents of children who tested positive for COVID-19 as compared to those whose children were negative [34 (89.5%) versus 4 (10.5%), p = .013]; (iii) parents who tested positive for COVID-19 themselves as compared to individuals who tested negative [21 (53.8%) versus 17 (29.8%), p = .033]; (iv) unemployed subjects as compared to employed subjects [10 (66.7%) versus 28 (34.6%), p = .041]; and (v) individuals who received an indication to quarantine as compared to those who had not [35 (51.5%) versus 3 (10.7%), p < .001]. Moreover, the mean age of participants was significantly lower among subjects reporting PTSS symptoms compared to the ones who did not [38.5 ± 8.4 versus 42.3 ± 7.8, p = .028] (see Table 1 ).
Table 1.
Socio-clinical-demographic features of subjects with (N = 38) and without (N = 58) PTSS.
| PTSS N (%) | No PTSS N (%) | p | |
|---|---|---|---|
| Child tested positive for COVID-19 | 34 (89.5) | 24 (41.4) | < .001 |
| Child tested negative for COVID-19 | 4 (10.5) | 34 (58.6) | |
| Mother | 30 (50) | 30 (50) | .013 |
| Father | 8 (22.2) | 28 (77.8) | |
| Married/cohabiting | 34 (45.3) | 41 (54.7) | .054 |
| Unmarried/divorced | 4 (19) | 17 (81) | |
| Child at risk for negative outcomes of COVID-19 (yes) | 9 (56.3) | 7 (43.8) | .225 |
| Child at risk for negative outcomes of COVID-19 (no) | 29 (36.3) | 51 (63.7) | |
| Family member at risk for negative outcomes of COVID-19 (yes) | 9 (40.9) | 13 (59.1) | 1.000 |
| Family member at risk for negative outcomes of COVID-19 (no) | 29 (39.2) | 45 (60.8) | |
| Graduated | 14 (43.8) | 18 (56.3) | .136 |
| Not graduated | 24 (37.5) | 40 (62.5) | |
| Employed | 28 (34.6) | 53 (65.4) | .041 |
| Unemployed | 10 (66.7) | 5 (33.3) | |
| Being at risk for negative outcomes of COVID-19 (yes) | 8 (38.1) | 13 (61.9) | 1.000 |
| Being at risk for negative outcomes of COVID-19 (no) | 45 (60) | 30 (40) | |
| Economic damage due to COVID-19 Emergency (yes) | 13 (32.5) | 27(67.5) | 1.000 |
| Economic damage due to COVID-19 Emergency (no) | 14 (31.8) | 30 (68.2) | |
| Being positive for COVID-19 | 21 (53.8) | 18 (46.2) | .031 |
| Being negative for COVID-19 | 17 (29.8) | 40 (70.2) | |
| Quarantine (yes) | 35 (51.5) | 33 (48.5) | < .001 |
| Quarantine (no) | 3 (10.7) | 25 (89.3) | |
| Relatives or close ones positive for COVID-19 (yes) | 27 (48.2) | 29 (51.8) | .067 |
| Relatives or close ones positive for COVID-19 (no) | 11 (27.5) | 29 (72.5) | |
| Relatives or close one dead of COVID-19 (yes) | 8 (47.1) | 9 (52.9) | .673 |
| Relatives or close one dead of COVID-19 (no) | 30 (38) | 49 (62) | |
| mean ± SD | mean ± SD | ||
| Age | 38.5 ± 8.4 | 42.3 ± 7.8 | .028 |
Results also showed that 39 participants (40.6%) reported moderate to severe anxiety symptoms (GAD-7 score≥10). Rates were significantly higher among parents who had: (i) a child tested positive for COVID-19 as opposed to those without [30 (51.7%) versus 9 (23.7%), p = .012]; (ii) suffered economic damage because of the COVID-19 emergency as opposed to those who had not [19 (47.5%) versus 8 (66.7%), p = .025]; (iii) been quarantined as opposed to those who had not [33 (48.5%) versus 6 (21.4%), p = .026]; and (iv) reported a relative or a close one infected by COVID-19 [29 (51.8%) versus10 (25%), p = .015] (see Table 2 ).
Table 2.
Comparison of socio-clinical-demographic characteristics between subjects with Anxiety symptoms (N = 39) and those without (N = 57).
| Anxiety Symptoms N (%) | No Anxiety symptoms N (%) | p | |
|---|---|---|---|
| Child tested positive for COVID-19 | 30 (51.7) | 28 (48.3) | .012 |
| Child tested negative for COVID-19 | 9 (23.7) | 29 (76.3) | |
| Mother | 28 (46.7) | 32 (53.3) | .180 |
| Father | 11 (30.6) | 25 (69.4) | |
| Married/cohabiting | 34 (45.3) | 41 (54.7) | .128 |
| Unmarried/divorced | 5 (23.8) | 16 (76.2) | |
| Child at risk for negative outcomes of COVID-19 (yes) | 6 (37.5) | 10 (62.5) | 1.000 |
| Child at risk for negative outcomes of COVID-19 (no) | 33 (41.2) | 47 (58.8) | |
| Family member at risk for negative outcomes of COVID-19 (yes) | 11 (50) | 11 (50) | .440 |
| Family member at risk for negative outcomes of COVID-19 (no) | 28 (37.8) | 46 (62.2) | |
| Graduated | 14 (43.8) | 18 (56.2) | .826 |
| Not graduated | 25 (39.1) | 39 (60.9) | |
| Employed | 8 (61.7) | 7 (38.3) | .421 |
| Unemployed | 31 (46.7) | 50 (53.3) | |
| Being at risk for negative outcomes of COVID-19 (yes) | 5 (23.8) | 16 (76.2) | .128 |
| Being at risk for negative outcomes of COVID-19 (no) | 34 (45.3) | 41 (54.7) | |
| Economic damage due to COVID-19 Emergency (yes) | 19 (47.5) | 21(52.5) | .025 |
| Economic damage due to COVID-19 Emergency (no) | 8 (66.7) | 4 (33.3) | |
| Being positive for COVID-19 | 20 (51.3) | 19 (48.7) | .122 |
| Being negative for COVID-19 | 19 (33.3) | 38 (66.7) | |
| Quarantine (yes) | 33 (48.5) | 35 (51.5) | .026 |
| Quarantine (no) | 6 (21.4) | 22 (78.6) | |
| Relatives or close ones positive for COVID-19 (yes) | 29 (51.8) | 27 (48.2) | .015 |
| Relatives or close ones positive for COVID-19 (no) | 10 (25) | 30 (75) | |
| Relatives or close one dead of COVID-19 (yes) | 7 (41.2) | 10 (58.8) | 1.000 |
| Relatives or close one dead of COVID-19 (no) | 32 (40.5) | 47 (59.5) | |
| mean ± SD | mean ± SD | ||
| Age | 41.6 ± 8.1 | 39.5 ± 8.4 | .219 |
Further, 23 (24%) parents experienced moderate to severe depressive symptoms (PHQ-9 score≥10). Rates were significantly higher among parents who had: (i) a child who tested positive for COVID-19 compared to those who did not [19 (32.8%) versus 4 (10.5%), p = .034]; (ii) suffered economic damage because of the COVID-19 emergency as opposed to those who did not [11 (27.5%) versus 3 (6.8%), p < .001]; and (iv) been quarantined as opposed to those who did not [21 (30.9%) versus 2 (7.1%), p = .027] (see Table 3 ).
Table 3.
Comparison of socio-clinical-demographic characteristics between subjects with Depressive symptoms (N = 23) and those without (N = 73).
| Depressive symptoms N (%) | No depressive symptoms N (%) | p | |
|---|---|---|---|
| Child tested positive for COVID-19 | 19 (32.8) | 39 (67.2) | .024 |
| Child tested negative for COVID-19 | 4 (10.5) | 34 (89.5) | |
| Mother | 18 (30) | 42 (70) | .123 |
| Father | 5 (13.9) | 31 (86.1) | |
| Married/cohabiting | 19 (25.3) | 56 (74.7) | .759 |
| Unmarried/divorced | 4 (19) | 17 (81) | |
| Child at risk for negative outcomes of COVID-19 (yes) | 5 (31.2) | 11 (68.8) | .669 |
| Child at risk for negative outcomes of COVID-19 (no) | 18 (22.5) | 62 (77.5) | |
| Family member at risk for negative outcomes of COVID-19 (yes) | 5 (22.7) | 17 (77.3) | 1.000 |
| Family member at risk for negative outcomes of COVID-19 (no) | 18 (24.3) | 56 (75.7) | |
| Graduated | 9 (28.1) | 23 (71.9) | .673 |
| Not graduated | 14 (21.9) | 50 (71.1) | |
| Employed | 60 (74.1) | 21 (25.9) | .471 |
| Unemployed | 13(86.7) | 2 (13.3) | |
| Being at risk for negative outcomes of COVID-19 (yes) | 4 (19) | 17 (81) | .759 |
| Being at risk for negative outcomes of COVID-19 (no) | 19 (25.3) | 56 (74.7) | |
| Economic damage due to COVID-19 Emergency (yes) | 11 (27.5) | 29(72.5) | < .001 |
| Economic damage due to COVID-19 Emergency (no) | 3 (6.8) | 41 (93.2) | |
| Being positive for COVID-19 | 20 (51.3) | 19 (48.7) | .122 |
| Being negative for COVID-19 | 19 (33.3) | 38 (66.7) | |
| Quarantine (yes) | 21 (30.9) | 47 (69.1) | .027 |
| Quarantine (no) | 2 (7.1) | 26 (92.9) | |
| Relatives or close ones positive for COVID-19 (yes) | 16 (28.6) | 40 (71.4) | .312 |
| Relatives or close ones positive for COVID-19 (no) | 7 (17.5) | 33 (82.5) | |
| Relatives or close one dead of COVID-19 (yes) | 5 (29.4) | 12 (70.6) | .545 |
| Relatives or close one dead of COVID-19 (no) | 18 (22.8) | 61 (77.2) | |
| mean ± SD | mean ± SD | ||
| Age | 41.2 ± 9.3 | 40.7 ± 7.9 | .800 |
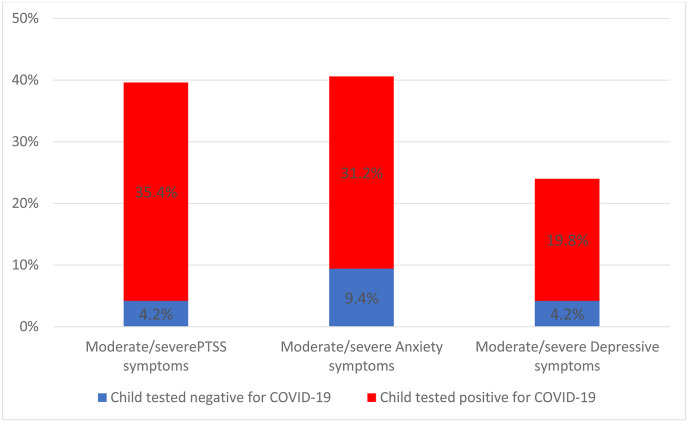
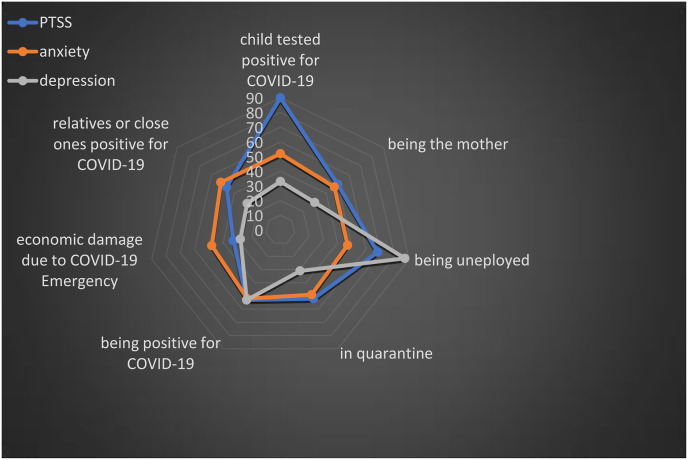
Details concerning rates of moderate-severe PTSS, anxiety and depressive symptoms in the total sample and comparison among parents with a child tested positive or negative for COVID-19 are reported on Fig. 1 . Moreover, socio-demographic and clinical factors influencing mental health outcomes in the study sample are summarized in Fig. 2 .
Fig. 1.
Rates of moderate/severe PTSS, anxiety and depressive symptoms in the total sample (N = 96) and rates of Children tested negative (N = 38) or positive (N = 58) for Covid-19 infection among them.
Fig. 2.
Factors influencing mental health outcomes.
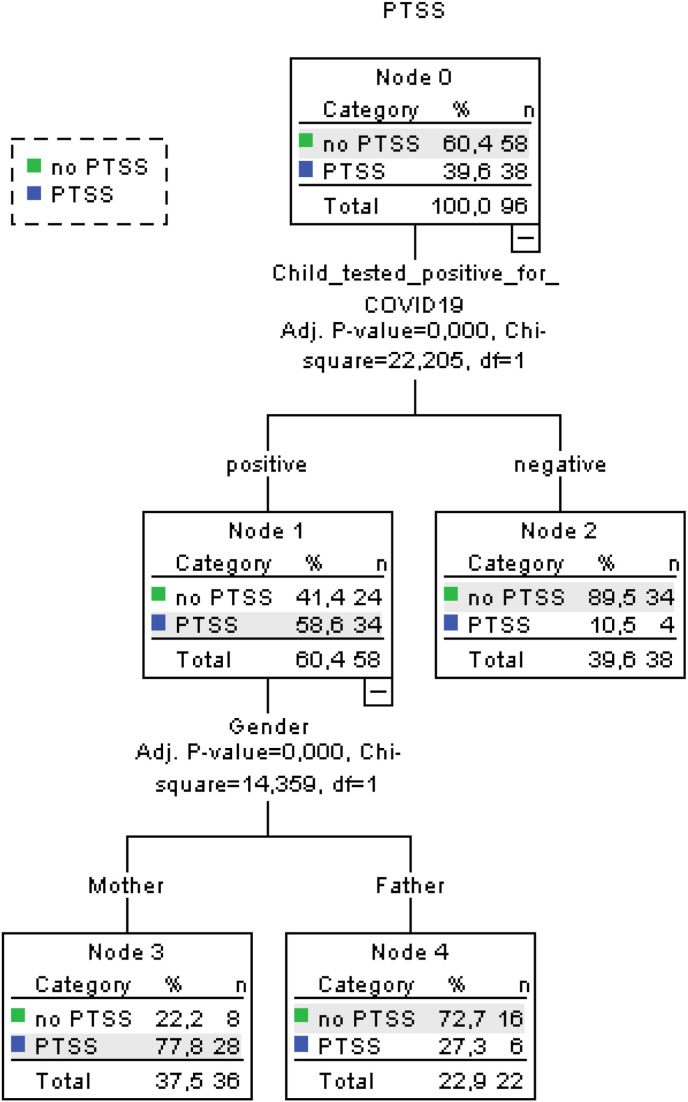
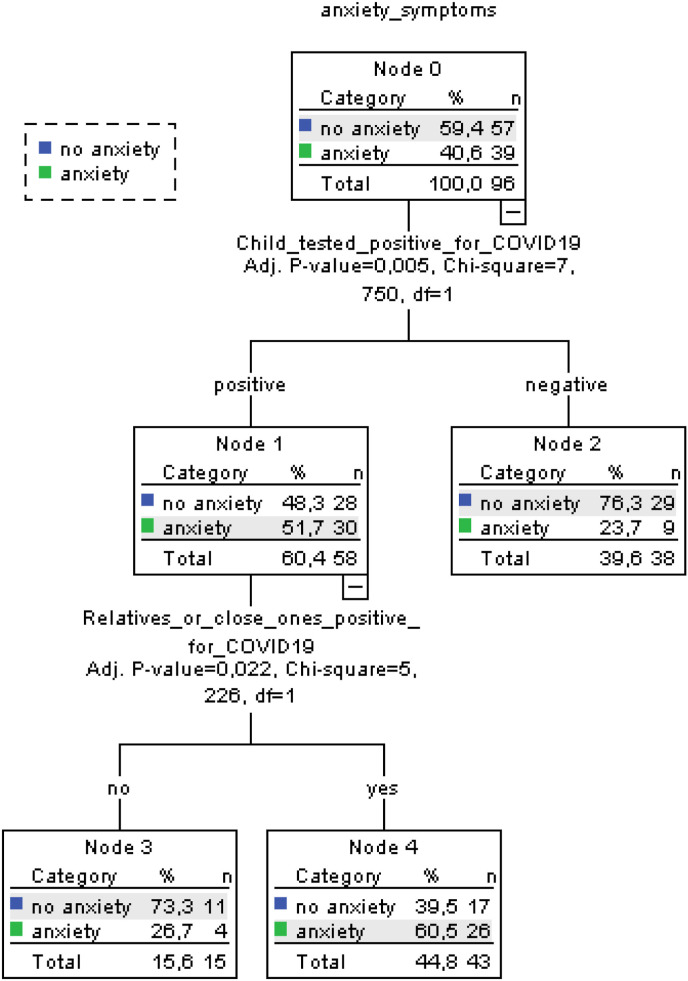
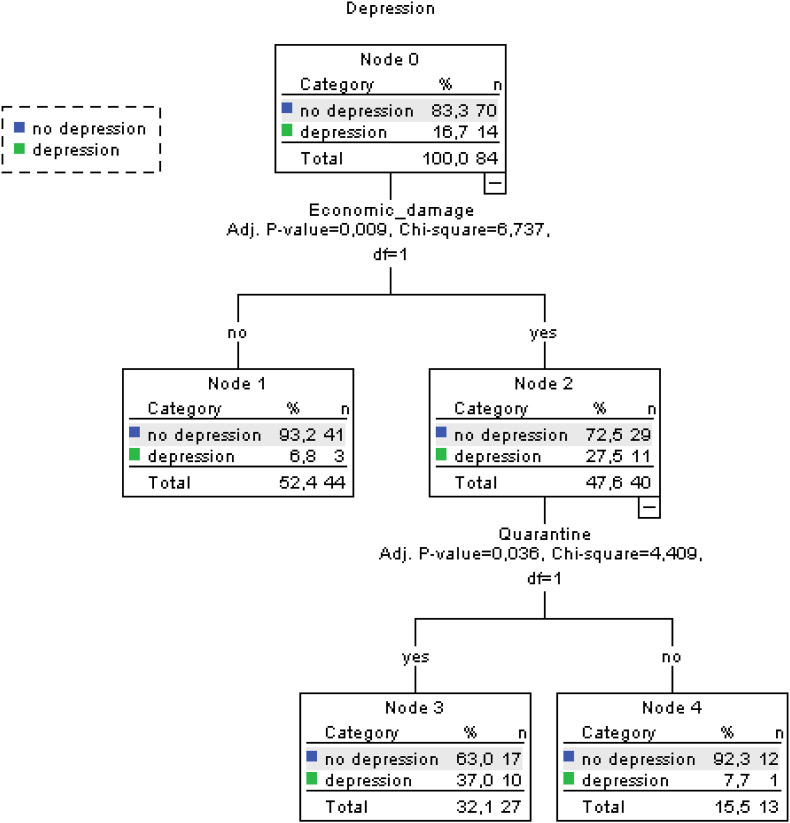
Finally, upon the three Decision Tree procedures, considering PTSS as dependent variable (see Fig. 3 ), parents with a child tested positive for COVID-19 showed significantly higher prevalence rates of PTSS with respect to those whose child tested negative (58,6% vs 10,5%, Chi-square = 22,2, p = .000) and, among the former, mothers with respect to fathers (77,8% vs 27,3%, Chi-square = 14,35, p = .000), This tree-based classification model had an acceptable misclassification risk of the model (value = 0.187). Fig. 4 shows the tree diagram related to anxiety symptoms (acceptable misclassification risk of the model = 0.313): subjects reporting a child tested positive showed significantly higher prevalence of anxiety symptoms with respect to those who had not (51,7% vs 23,7%, Chi-square = 7,75, p = .005) and, among the former, those who referred to also have a relative or close one tested positive for COVID-19 with respect to those without (60,5% vs 26,7%, Chi-square = 5,22, p = .022). Finally, upon the tree diagram considering depressive symptoms (Fig. 5 ): subjects who reported economic damage due to the COVID-19 emergency showed significantly higher prevalence rates of anxiety symptoms with respect to those who did not (27,5% vs 6,8%, Chi-square = 6,73, p = .009) and, among the former, those who had been quarantined (37% vs 7,7%, Chi.square = 4,4, p = .036) (acceptable misclassification risk of the model, value = 0.167).
Fig. 3.
Decision tree showing having a child tested positive for COVID-19 and gender interaction with PTSS symptoms as target variable (PTSS= Post-Traumatic Stress Symptoms).
Fig. 4.
Decision tree showing having a child tested positive for COVID-19 and having relative or close ones positive for COVID-19 interaction with anxiety symptoms as target variable.
Fig. 5.
Decision tree showing suffering economic damage for COVID-19 and quarantine interaction with depressive symptoms as target variable.
4. Discussion
The present study highlights the presence of statistically significantly higher symptoms of PTSS, anxiety and depression among parents whose children tested positive for COVID-19 with respect to parents whose children tested negative during the acute phase of the pandemic in Italy. The same results emerged for parents who had beenquarantined as opposed to those who had not. The findings regarding the other COVID-19 related factors were more uneven and led to different clinical outcomes. In this regard, parents who tested COVID-19 positive themselves, as well as young and unemployed subjects, presented statistically higher rates of PTSS. Subjects who suffered economic loss and experienced a loved one testing positive for COVID-19 presented statistically higher anxiety symptoms as opposed to those who didn't experience the same traumatic events. Further, parents facing economic loss presented also statistically significant higher depressive symptoms as opposed to those who had not.
These findings are in line with some previous evidence on outbreaks where people who had friends or close relatives who contracted SARS were two to three times more likely to develop high levels of PTSS than those who were not exposed to the virus (Boyraz and Legros 2020; Talevi et al., 2020). Nevertheless, literature reports conflicting results about other psychological outcomes related to those who have had close contact with a person who presented COVID-19. A nationwide survey of psychological distress among Italians evidenced that having an acquaintance infected by SARS-COV-2 was associated with increased depression and stress, whereas having an infected relative was associated with increased anxiety. This is perfectly in line with our findings, revealing that parents with children tested positive for COVID-19 show significantly higher anxiety symptoms rates with respect to those with children tested negative and, among the former, those who suffered economic damage due to COVID-19 emergency implications rather than who had not. In contrast, Wang and collaborators reported that neither having an infected acquaintance nor having an infected relative was associated with psychological distress, although their participants showed high levels of concern about the health of their family members (Mazza et al., 2020; Wang et al., 2020).
The only previous study on parents and COVID-19, comparing the psychological status of parents of hospitalized children during the COVID-19 epidemic (EH) with the psychological status of children hospitalized during the non-epidemic period (NEH) highlighted significantly higher anxiety and depressive scores in parents of EH children than those of parents of NEH children (Yuan et al., 2020). This is the first study that highlight that having a child testing positive for COVID-19 negatively influences mental health outcomes for parents, especially for mothers.
The present findings also evidenced how statistically significant gender differences emerged only for PTSS and not for anxiety or depression symptoms. This is perfectly in line with COVID-19 literature that has already highlighted this gender difference for PTSD, but not for anxiety symptoms, among health care workers and among the general adult population. These observations are in contrast with previous literature on others traumatic events where women were more likely to have anxiety than men (Carmassi et al., 2020; Lai et al., 2020; Liu et al., 2020; Sun et al., 2020).
Trauma literature suggests that the risk of PTSD is twice as high among women as among men (Dell'Osso et al., 2011; Carmassi et al., 2014; Boyraz and Legros 2020). Similar results were obtained also in parents of severely ill children where mothers presented higher scores than fathers in each criterion of PTSD with important implications for the future health of the child (Carmassi et al., 2017; Dell’Osso et al., 2018). Interestingly, our results showed significantly higher PTSS rates among parents of a child who tested positive for COVID-19 rather than among those of negative ones and among mothers with respect to fathers. Intrusive memories and re-experiencing may interfere with the family's daily living to such a degree, that commonalities such as a cold, pain, or any other in the children may give rise to extreme fear and anxiety in the parents potentially leading to over-protectiveness of the children. Symptoms of avoidance may potentially interfere with the parents' awareness of symptoms and medical sequelae and interfere with their adherence to following up recommendations (Carmassi et al. 2019, 2020).
The findings also show that both quarantine and economic loss, which are often associated with each other, had a significant negative impact on mental health of the parents. In particular, the latter highlight the associations between socio-economic status and mental health outcomes, with significantly higher depressive symptoms rates reported by parents who suffered financial loss due to COVID-19 emergency as compared with those who had not and, among these, by those who had been quarantined. These findings corroborate recent evidence on the psychological impact of quarantine (Ben-Ezra et al., 2020; Fiorillo et al., 2020, Orsini et al., 2020). A literature review highlighted how confinement, loss of daily routine, financial loss and social stigma were significant predictors of PTSS and other mental disorders (Sprang and Silman 2013; Boyraz and Legros 2020). Other studies evidenced how financial stressors as well as the social stigma towards individuals with COVID-19 and their families, are even risk factors for suicide (Gunnel et al., 2020; Pompili 2020).It appears evident that anxiety is activated indifferently by many exogenous stimuli, albeit as a consequence of the COVID-19 emergency. On the contrary, unemployment seems to lead more to depressive symptoms as opposed to distress (Brooks et al., 2020).
The results of the current study should be interpreted in light of several limitations. First, the data presented are cross-sectional and based on a limited sample size. Further, the ability to gain insights is highly limited by the lack of sophisticated statistics. Another limitation is that self-reported tools of psychological impact, anxiety, depression and stress may not always be aligned with assessment by mental health professionals. To generalize our considerations and have an adequate view of the phenomena we have to wait for larger -scale prospective, longitudinal studies which are needed to better describe the predictors and trajectory of psychological distress, or even psychiatric disorders, in parents of children positive for SARS-COV-2.
5. Conclusions
Despite the above limitations, this study provides some important findings. We identified a worsening in mental health outcomes in parents of SARS-COV-2 infected children, highlighting that these parents that these parents are at a high risk of showing psychological issues that may lead to imbalances in family units.
Further, parents are both caregivers of the positive child, thus their reaction affect bi-directionally both parents' themselves and children's health, representing an important issue for public health (Carmassi et al., 2020).
The COVID-19 pandemic is a public health emergency of international concern that poses a challenge to psychological resilience. As the pandemic is ongoing, it is important that health care systems and the general public are aware of possible negative mental health outcomes and vulnerable populations. Further research is needed to develop evidence-driven strategies to reduce adverse psychological impacts and related psychiatric symptoms in caregivers of COVID-19 infected children during the next phases of the pandemic.
6. Contribution
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship. All authors gave substantial contribution to the manuscript.
Funding
None.
References
- Ben-Ezra M., Sun S., Hou W.K., Goodwin R. The association of being in quarantine and related COVID-19 recommended and non-recommended behaviors with psychological distress in Chinese population. J. Affect. Disord. 2020;275:66–68. doi: 10.1016/j.jad.2020.06.026. Epub 2020 Jul 2. PMID: 32658825; PMCID: PMC7329674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyraz G., Legros D.N. Coronavirus disease (COVID-19) and traumatic stress: probable risk factors and correlates of posttraumatic stress disorder. J. Loss Trauma. 2020:1–20. doi: 10.1080/15325024.2020.1763556. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buselli rodolfo, Carmassi claudia, Corsi martina, Baldanzi sigrid, Battistini gianmarco, Vhiumiento martina, Massimetti gabriele, Dell’Osso liliana, Cristaudo alfonso. Post-traumatic stress symptoms in an Italian cohort of subjects complaining occupational stress. CNS Spectrums. 2020 doi: 10.1017/S1092852920001595. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Akiskal H.S., Bessonov D., Massimetti G., Calderani E., Stratta P., Rossi A., Dell'Osso L. Gender differences in DSM-5 versus DSM-IV-TR PTSD prevalence and criteria comparison among 512 survivors to the L'Aquila earthquake. J. Affect. Disord. 2014;160:55–61. doi: 10.1016/j.jad.2014.02.028. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Corsi M., Bertelloni C., Pedrinelli V., Massimetti G., Peroni D.G., Bonuccelli A., Orsini A., Dell'Osso L. Post-traumatic stress and major depressive disorders in parent caregivers of children with a chronic disorder. Psychiatr. Res. 2019;279 doi: 10.1016/j.psychres.2019.02.062. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Corsi M., Bertelloni C.A., Carpita B., Gesi C., Pedrinelli V., Massimetti G., Peroni D.G., Bonuccelli A., Orsini A., Dell'Osso L. Mothers and fathers of children with epilepsy: gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatric Dis. Treat. 2018;14:1371–1379. doi: 10.2147/NDT.S158249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Corsi M., Bertelloni C.A., Pedrinelli V., Massimetti G., Peroni D., Bonuccelli A., Orsini A., Dell'Osso L. Post-traumatic stress spectrum symptoms in parents of children affected by epilepsy: gender differences. Seizure. 2020;80:169–174. doi: 10.1016/j.seizure.2020.06.021. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Corsi M., Gesi C., Bertelloni C.A., Faggioni F., Calderani E., Massimetti G., Saggese G., Bonuccelli A., Orsini A., Dell'Osso L. DSM-5 criteria for PTSD in parents of pediatric patients with epilepsy: what are the changes with respect to DSM-IV-TR? Epilepsy Behav. 2017;70(Pt A):97–103. doi: 10.1016/j.yebeh.2017.02.025. [DOI] [PubMed] [Google Scholar]
- Cernvall M., Alaie I., Essen L. The factor structure of traumatic stress in parents of children with cancer: a longitudinal analysis. J. Pediatr. Psychol. 2011;37:448–457. doi: 10.1093/jpepsy/jsr105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland J. Resilience or resistance: a personal response to COVID-19. Med. Educ. 2020;54(7):589–590. doi: 10.1111/medu.14170. [DOI] [PubMed] [Google Scholar]
- Corsi Martina, orsini alessandro, pedrinelli virginia, santangelo andrea, bertelloni carlo antonio, carli niccolò, buselli rodolfo, peroni diego, striano pasquale, dell’osso liliana, carmassi claudia. PTSD in parents of children with severe diseases: a systematic review to face Covid- 19 impact. Italian Journal of Pediatrics. 2021 doi: 10.1186/s13052-021-00957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ćosić K., Popović S., Šarlija M., Kesedžić I. Impact of human disasters and COVID-19 pandemic on mental health: potential of digital psychiatry. Psychiatr. Danub. 2020;32(1):25–31. doi: 10.24869/psyd.2020.25. [DOI] [PubMed] [Google Scholar]
- Dell'Osso L., Carmassi C., Massimetti G., Daneluzzo E., Di Tommaso S., Rossi A. Full and partial PTSD among young adult survivors 10 months after the L'Aquila 2009 earthquake: gender differences. J. Affect. Disord. 2011;131(1–3):79–83. doi: 10.1016/j.jad.2010.11.023. [DOI] [PubMed] [Google Scholar]
- Dell'Osso L., Corsi M., Gesi C., Bertelloni C.A., Massimetti G., Peroni D., Bonuccelli A., Orsini A., Carmassi C. Adult Autism Subthreshold Spectrum (AdAS Spectrum) in parents of pediatric patients with epilepsy: correlations with post-traumatic stress symptoms. Compr. Psychiatr. 2018;83:25–30. doi: 10.1016/j.comppsych.2018.02.004. [DOI] [PubMed] [Google Scholar]
- Dell'osso L., Stratta P., Conversano C., Massimetti E., Akiskal K.K., Akiskal H.S., Rossi A., Carmassi C. Lifetime mania is related to post-traumatic stress symptoms in high school students exposed to the 2009 L'Aquila earthquake. Compr. Psychiatr. 2014;55(2):357–362. doi: 10.1016/j.comppsych.2013.08.017. [DOI] [PubMed] [Google Scholar]
- Fiorillo A., Sampogna G., Giallonardo V., Del Vecchio V., Luciano M., Albert U., Carmassi C., Carrà G., Cirulli F., Dell'Osso B., Nanni M.G., Pompili M., Sani G., Tortorella A., Volpe U. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: results from the COMET collaborative network. Eur. Psychiatr. : the journal of the Association of European Psychiatrists. 2020;63(1):e87. doi: 10.1192/j.eurpsy.2020.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S., Roma P., Verrocchio M.C. The effect of the COVID-19 lockdown on parents: a call to adopt urgent measures. Psychol Trauma. 2020 doi: 10.1037/tra0000672. [DOI] [PubMed] [Google Scholar]
- Galletly C. Psychiatry in the COVID-19 era. Aust. N. Z. J. Psychiatr. 2020;54(5):447–448. doi: 10.1177/0004867420920359. [DOI] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J. Suicide risk and prevention during the COVID-19 pandemic. The lancet. Psychiatry. 2020;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addiction. 2020:1–14. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatr. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kingston C., Onwumere J., Keen N., Ruffell T., Kuipers E. Posttraumatic stress symptoms (PTSS) in caregivers of people with psychosis and associations with caregiving experiences. J. Trauma & Dissociation. 2016;17(3):307–321. doi: 10.1080/15299732.2015.1089969. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landolt M.A., Ystrom E., Sennhauser F.H., Gnehm H.E., Vollrath M.E. The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. JCPP (J. Child Psychol. Psychiatry) 2012;53(7):767–774. doi: 10.1111/j.1469-7610.2011.02520.x. [DOI] [PubMed] [Google Scholar]
- Lazzerini M., Putoto G. COVID-19 in Italy: momentous decisions and many uncertainties. Lancet Glob Health. 2020;8(5):e641–e642. doi: 10.1016/s2214-109x(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Long X., Zhang Q., Fang X., Fang F., Lv X., Zhang D., Sun Y., Li N., Hu S., Lin Z., Xiong N. Emerging evidence for neuropsycho-consequences of COVID-19. Curr. Neuropharmacol. 2020 doi: 10.2174/1570159x18666200507085335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J., Li K. Anxiety and depression among general population in China at the peak of the COVID‐19 epidemic. World Psychiatr. 2020;19:249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatr. Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Publ. Health. 2020;17(9) doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M., Morelen D., Hruschak J., Rosenblum K.L., Bocknek E., Beeghly M. Psychopathology and parenting: an examination of perceived and observed parenting in mothers with depression and PTSD. J. Affect. Disord. 2017;207:242–250. doi: 10.1016/j.jad.2016.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsini alessandro, corsi martina, santangelo andrea, riva antonella, peroni diego, foiadelli thomas, savasta salvatore, striano pasquale. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurological Sciences. 2020 doi: 10.1007/s10072-020-04544-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pakpour A., Griffiths M. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders. 2020 [Google Scholar]
- Pompili M. Suicide prevention at the time of covid-19. BMJ. 2020 [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. vol. 33. Published by BMJ; 2020. (A Nationwide Survey of Psychological Distress Among Chinese People in the COVID-19 Epidemic: Implications and Policy Recommendations. Gen Psychiatr, © Author(s) (Or Their Employer(s)) 2020. Re-use Permitted under CC BY-NC. No Commercial Re-use. See Rights and Permissions). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Sun P., Lu X., Xu C., Sun W., Pan B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020;92(6):548–551. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talevi D., Socci V., Carai M., Carnaghi G., Faleri S., Trebbi E., Bernardo A., Capelli F., Pacitti F. Mental health outcomes of the CoViD-19 pandemic. Riv. Psichiatr. 2020;55:137–144. doi: 10.1708/3382.33569. [DOI] [PubMed] [Google Scholar]
- Taylor W.D., Blackford J.U. Mental health treatment for front-line clinicians during and after the coronavirus disease 2019 (COVID-19) pandemic: a plea to the medical community. Ann. Intern. Med. 2020 doi: 10.7326/2FM20-2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuite A.R., Greer A.L., De Keninck S., Fisman D.N. Risk for COVID-19 resurgence related to duration and effectiveness of physical distancing in ontario, Canada. Ann. Intern. Med. 2020 doi: 10.7326/2FM20-2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unützer J., Kimmel R.J., Snowden M. Psychiatry in the age of COVID-19. World Psychiatr. 2020;19:130–131. doi: 10.1002/wps.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oers H.A., Haverman L., Limperg P.F., van Dijk-Lokkart E.M., Maurice-Stam H., Grootenhuis M.A. Anxiety and depression in mothers and fathers of a chronically ill child. Matern. Child Health J. 2014;18(8):1993–2002. doi: 10.1007/s10995-014-1445-8. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5) doi: 10.3390/2Fijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing Psychological Trauma and PTSD. Wilson J.P., Keane T.M., editors. Guilford Press; New York: 1997. The impact of event scale-revised; pp. 399–411. [Google Scholar]
- Woolf C., Muscara F., Anderson V.A., McCarthy M.C. Early traumatic stress responses in parents following a serious illness in their child: a systematic review. J. Clin. Psychol. Med. Settings. 2016;23(1):53–66. doi: 10.1007/s10880-015-9430-y. [DOI] [PubMed] [Google Scholar]
- Yuan R., Xu Q.H., Xia C.C., Lou C.Y., Xie Z., Ge Q.M., Shao Y. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatr. Res. 2020;288:112953. doi: 10.1016/j.psychres.2020.112953. [DOI] [PMC free article] [PubMed] [Google Scholar]