Abstract
The COVID-19 pandemic remains a significant problem involving health systems worldwide. Accurate and early detection of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection is critical for minimizing spread and initiating treatment. Among test methods, real-time reverse-transcriptase polymerase-chain-reaction (rRT-PCR) is considered the gold standard. Although this test has high specificity and relatively high sensitivity, the occurrence of falsely negative results in symptomatic patients and/or having a positive CT scan remains a challenge. Sources of error can be pre-analytical (sampling, storage and processing), analytical (RNA extraction, cDNA synthesis and amplification) and post-analytical (interpretation and analysis and test reporting). These potential sources of error and efforts to mitigate are reviewed in this article with an emphasis on the analytical phase.
Keywords: COVID-19, Laboratory errors, rRT-PCR method, SARS-CoV-2
1. Introduction
Coronaviruses are a large family of RNA viruses that cause a wide range of diseases from the common cold to some severe conditions such as Severe Acute Respiratory Syndrome (SARS-CoV) and COVID-19. The first coronavirus was identified in the 1960s. These viruses have an open single-stranded RNA between 26 and 32 kb in length and also have two types of surface proteins that their names derived from feature appearances. Coronaviridae family are divided into four genera, genotypically and serologically: Alpha, Beta, Gamma, and Delta coronaviruses. Coronaviruses are found in both humans and animals so that 30 species of coronaviruses have been identified in human, mammals and birds specimens. Human coronaviruses are categorized in alpha and beta species [1], [2]. The outbreak of class B beta-coronaviruses, a virus with bat origin in 2002–2003 led to SARS-COV and in 2012 and later a camel-origin beta-coronavirus class C led to coronavirus-related Middle East Respiratory Syndrome (MERS) [3]. In late December 2019, a pneumonia in Wuhan, China, was reported, which later turned out to be caused by a coronavirus and was classified by the World Health Organization (WHO) as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) due to its respiratory symptoms [4], [5]. The new 2019 coronavirus has been shown to be a chimeric virus between bat coronavirus and other animals [6]. Studies have shown that the sequence homology between SARS-CoV-2 and SARS-CoV is equal to 79.5% [7], [8].
It has been shown that patients infected with SARS-CoV-2 present some clinical presentations such as fever (High temperature), dry cough, fatigue, Myalgia, shortness of breath, headache, bleeding and diarrhea. Change in laboratory biomarkers such as leukopenia and lymphocytopenia, rise in several enzymes like Aspartate aminotransferase (AST) and Lactate dehydrogenase (LDH), increase in High sensitive troponin I (hs-cTnI) and C-reactive protein (CRP) concentration have been also proved in infected patients. Furthermore, CT scan seems to be helpful in diagnosis of COVID-19 as revealed in previous studies [9], [10]. However, these criteria cannot lead to final confirmation of the COVID-19 because there are some infections with similar symptoms such as influenza and SARS. Therefore, molecular diagnosis through rRT-PCR method and using specific primers and probes is introduced as the gold standard approach to determine and differentiate SARS-CoV-2 from other beta-coronaviruses such as SARS and MERS [11], [12].
PCR is a highly sensitive laboratory technique that has been proved to be applicable in biological and medical sciences and has the ability to provide qualitative and quantitative results. A modification of PCR with diagnostic use is rRT-PCR, which is applied to detect target RNAs in clinical samples specially for diagnosing pathogens in molecular diagnostics laboratories [13], [14].
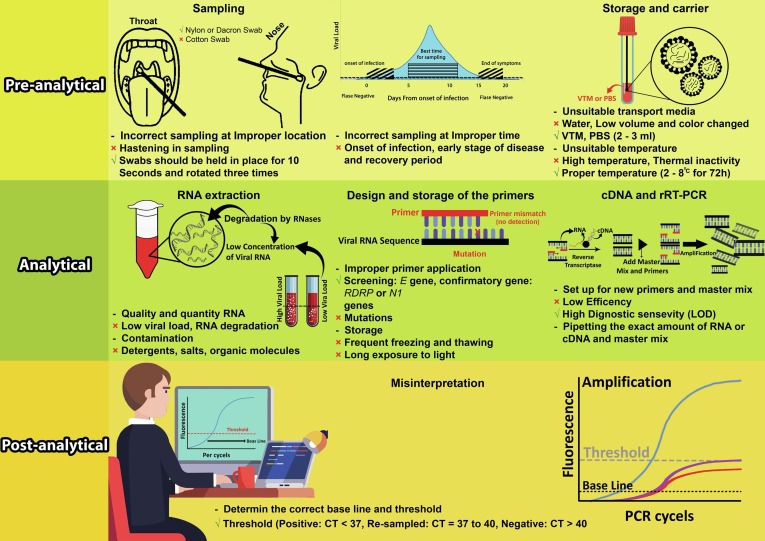
Also, in the COVID-19 pandemic, rRT-PCR technique has been used to detect SARS-CoV-2 genome in biological specimens [12], [15], [16], [17]. Despite the moderate sensitivity and high specificity and being approved by the CDC and WHO as the gold standard test for confirmation of COVID-19, this method has showed a huge number of false negative results that should be highly considered [17]. The results of the test, can be affected by laboratory errors in three different steps including, pre-test errors and factors (pre-analytical) such as sampling method, sampling location, sampling time, sample size, sample transfer and storage errors [18], [19], [20], [21], factors during the test (analytical), such as nucleic acid extraction, cDNA synthesis, and PCR process [17], [22] and finally post-analytical errors such as interpretation and analysis of results and test report (Fig. 1 ) [22]. Therefore troubleshooting and following the guidelines could effectively increase the accuracy and precision of the obtained results. In general, rRT-PCR troubleshooting is explained in three various pre-analytical, analytical, and post-analytical phases (Table 1 ).
Fig. 1.
A summarized illustration showing the most important causes which create false results in SARS-CoV-2 molecular diagnosis.
Table 1.
Various causes of generating false results in different laboratory diagnostic steps of SARS-CoV-2.
| Pre-analytical phase |
|
| Analytical phase |
|
| Post-analytical phase |
|
Due to the importance role of clinical laboratories in the management of COVID-19 pandemic, especially in diagnosis and control of disease, it is quite crucial to minimize laboratory errors in order to prevent wasting time, budget and laboratory staff force. In the present review we have summarized the main source of errors leading to wrong results, especially in the level of analytical phase.
2. Pre-analytical errors
It has been shown that pre-analytical errors are an inevitable source of laboratory errors and with regard to SARS-CoV-2 identification these factors are more significant [23], [24]. Therefore, determination and optimizing these errors can entirely improve the analysis process and has a vital role in COVID-19 diagnosis. One of the most important source of errors in pre-analytical level occurs in the sampling step. According to the CDC guidelines, the most important instructions that have a vital role on test result and accuracy and should be fully followed are proper sampling locations including nose and throat, tracheal tube, and sputum and also using standard equipment such as synthetic swabs made of nylon or dacron with aluminum or plastic shaft for sampling. In addition, do not use standard carrier tubes (contains unsuitable virus transport medium) and hastening in specimen collection (swabs should be held in place for 10 s and rotated three times) cause having not enough viral load for testing. It means that the sample has poor quantity and quality [25], [26], [27]. Moreover, the swab which impregnated with contaminants such as glove powder, food debris at the end of the throat, and other substances during the sampling have deteriorating effect on result accuracy [28].
After sampling, the swab should be transferred to a suitable transport medium. A tube containing 2–3 ml of viral transport media (VTM), isotonic saline solution, tissue culture solution and phosphate buffer can be used as a proper media for sample transportation [26]. It has been shown that use of PBS as a transport medium for more than 18 h could negatively impact on genome stability and molecular detection of SARS-CoV-2 compared to VTM [29].
The most important ways to minimize these errors are quick delivery of the swabs into tubes containing transfer medium, rapid transferring of the samples to laboratory and control the temperature and time conditions of the sample (samples must transport at 2–8 °C for 72 h)[25], [26]. Previous studies have reported that inadequate amount of viral load from infected patients in the early stage of disease and recovery period are the main issues for creating false negative results. A study by Basu et al. showed that time and temperature of nasopharyngeal swabs storage had no effect on the reproducibility of the results. However, incorrect sampling and storage could be proposed as important sources for creating wrong results, especially in samples with low viral load [30]. In some cases, despite the positive CT scan evidence suggesting COVID-19, the primary tests of these people were reported to be negative, but in subsequent repetitions, most of them demonstrated positive results until day 5.1 ± 1.5 [31], [32], [33], [34], [35]. Several studies have shown that in early stages of the disease, the virus is mostly located in nose, therefore sampling from throat and throat swabs are more likely to be false negatives in this period, while nasopharyngeal and oropharyngeal swabs are recommended 5 or 6 days after the onset of symptoms [36].
Thermal inactivity of samples in order to protect personnel from contamination can lead to decrease viral load, especially in samples with less amount of the virus, and therefore this preparation is not recommended [37]. Also, it is important to consider whether the patients have received the antiviral drug before sampling or not [17], [21]. Contamination of surfaces, pipettors, and clothes by positive samples, PCR products or positive control vials, can lead to false positive results. To avoid that, different section of a molecular laboratory including sample extraction, preparation of primers and reagents and also rRT-PCR processing must have separate sections [38]. Besides, there is no evidence if sampling time during the day, eating and brushing influence the test accuracy. Finally, it could be concluded that following the recommended methods and protocols (CDC and WHO protocols) in relation with COVID-19 sampling can eliminate numerous errors and eventually increase the accuracy of rRT-PCR results.
3. Analytical errors
In contrast to numerous guidelines and reports on pre-analytical errors, there is a paucity of data about analytical errors in rRT-PCR test for SARS-CoV-2 molecular diagnosis. However, according to previous guidelines on rRT-PCR method, there are useful and applicable information that could be considered for SARS-CoV-2 molecular detection.
One of the important errors occurs in the nucleic acid extraction step and highly impacts on the quantity and quality of the extracted RNA. These criteria can be influenced by the presence of protein and DNA in the extracted sample, and would lead to decreased efficiency of rRT-PCR process. The main contaminating proteins in the nucleic acids extraction process are nucleic acid-binding proteins, which can interfere with the cDNA synthesis reaction and especially the PCR process [39], [40].
Choosing a proper RNA extraction procedure is a consequential step for a valid real-time PCR result. Currently, three main extraction protocols including automatic extraction, magnetic method and column based method are developed to be used for SARS-CoV-2 RNA extraction. The automatic method has known as the safest and fastest method with minimal staff intervention. However, this method requires special extraction devices which are not available in many laboratories especially in low income countries. Magnetic and column based methods are widely applied in developing countries. The magnetic method does not require a centrifuge and also has a simple operation; nevertheless contamination with magnetic particles could highly affect the PCR process. It was confirmed that the column based method is fast and reproducible, although this process requires centrifugation and also there is a possibility of aerosol contamination through frequent opening and closing of microtubes [41]. Therefore, according to the current crucial conditions, choose of extraction methods and their process must be done carefully.
The quality and quantity of extracted RNA may also be influenced by RNA degradation via endogenous and exogenous ribonuclease enzymes (RNase). Endogenous RNases can be originated from cell lysis and exogenous RNases may derivate from contaminated devices or other surfaces and causes false negative results. Final extract should be dissolved in RNase free water to prevent further degeneration of RNA by these enzymes. Therefore, one of the main sources of error is the presence of these enzymes and as a result a low viral load that further lead to false negative results [42].
There are several agents that negatively impact on PCR efficiency such as glove powder, salts, detergents and organic molecules like phenol and ethanol, therefore should be avoided or minimized in RNA extraction process. Also, it is important to avoid extracted nucleic acid to be exposed to UV radiation that can reduce the sensitivity of the test [28], [42].
To avoid the molecular laboratory environment being affected by aerosols or particles containing virus or viral genome, separate and specific areas must be considered for the equipment (centrifuges, pipettors, etc.) and the consumables (microtubes and pipettor tips and gloves, reagents and even extracted RNA). The workflow should be designed from a clean area to a dirty area [25], [38].
The storage of primers and probes (−20 °C) has major role in the occurrence of errors. Successive freezing and thawing decrease their stability and the efficiency of reaction. The incorrect storage and contamination with fluorescent materials can lead to the diffusion of their color, increase the background color and ultimately reduce their signal to noise. Furthermore, long term light exposure of these oligonucleotides can reduce their efficiency in PCR procedure. The enzymes and master mix should be used and stored according to manufacturer’s instruction and avoid frequent freezing and thawing. Moreover, since the repeated defrosting may lead to inactivity of materials and eventually inhibiting the reaction, it is highly important to prepare master mix after enzymes defrosting on ice [25].
Pipetting the exact amount of extracted RNA and enzyme has major role in cDNA synthesis process [43]. Samples with lower amount of RNA (low viral load, incorrect extraction and incorrect pipetting) can result in higher CT values (CT > 40) and ultimately lead to misinterpretation of the test [25]. Therefore pipetting style, calibration of pipettors and methods of RNA extraction before testing should be qualified and validated [31], [40], [43], [44]. In single-step reactions in which both reverse transcriptase and polymerase processes occur in one tube, the low target value for polymerase activity, misinterpretation and wrong analysis is supposed to occur for samples with low RNA levels [44]. High concentrations of RT enzyme have an inhibitory effect on the amplification phase. Impaired calibration of thermal cyclers can result in non-optimal temperature and cycle times (high or low). Moreover, common problems such as un-calibrated pipettors or low-skilled operators may lead to non-optimal concentration of reaction components [38].
One of the most important reasons for producing false negative results that should be considered is specimens with low viral load which might report negatively, by common rRT-PCR methods. Therefore, it is important to consider other strategies that can overcome the limitations of rRT-PCR method. In a study by Falzone et al. droplet digital PCR (ddPCR) was shown to have more sensitivity and specificity than rRT-qPCR for detecting samples with low viral load. Therefore, to improve COVID-19 diagnosis procedure and also to determine whether a patient has been completely recovered from the disease or not, alternative methods such as ddPCR should be considered [45].
Due to identification of different genes in the SARS-CoV-2 genome and evolution of new rRT-PCR modifications, various organizations and research centers have designed different primers and probes to identify and diagnose COVID-19 (Table 2 ). Identifying SARS-CoV-2 specific sequences is the important goal in diagnosis and cause to specifically differentiate SARS-CoV-2 genome from other viruses with similar genomic regions. One of the most important challenges in SARS-CoV-2 rRT-PCR assay that should not be forgotten is choosing a primer with the highest efficiency. The five regions in the SARS-CoV-2 genome are widely used for designing primer including Nucleocapsids (N), Envelope (E), RNA polymerase-dependent RNA (RdRp), ORF1ab, and Spike (S). It has been proved that ORF1ab, N and RdRp primers have higher sensitivity, specificity and positive predictive value than the others. The occurrence of mutation and recombination in virus genome makes COVID-19 detection quite difficult. To improve method sensitivity and to overcome this issue three main factors including primer concentration, primer degeneration, and design primers for multi-target detection should be more considered. In general, the E gene is used to screen pan-sarbecovirus and the RdRp and the N gene are used to confirm SARS-CoV-2 infection [46]. The related sensitivity and specificity were reported as 96.6% and 100% for Nucleocapsids, 96% and 100% for ORF1ab and 95.7% and 88.9 for RdRp, respectively [47], [48]. Hoang Quoc Cuong and colleagues compared three different sets of primer-probe targeting E gene from TIB-Molbiol, IDT, and Phu Sa using two different PCR mixes including Invitrogen SuperScript III One-Step RT-PCR and LightCycler Multiplex RNA Virus Master. All sets of primer-probes showed highly and relatively similar sensitivity for detecting E gene. The authors proposed that a combination strategy by which different sets of primers are applied should be considered to increase the testing capacity in the screening programs [49].
Table 2.
Summary of primers use for COVID-19 diagnosis [48].
| Institute | Gene targets | Sequence | Diagnosis criteria |
|---|---|---|---|
| US CDC, USA | Three targets in N gene |
N1: F: GACCCCAAAATCAGCGAAAT R: TCTGGTTACTGCCAGTTGAATCTG P: 5′-FAM-ACCCCGCATTACGTTTGGTGGACC- BHQ1-3′ N2: F: TTACAAACATTGGCCGCAAA R: GCGCGACATTCCGAAGAA P: 5′-FAM-ACAATTTGCCCCCAGCGCTTCAG- BHQ1-3′ N3: F: GGGAGCCTTGAATACACCAAAA R: TGTAGCACGATTGCAGCATTG P: 5′-FAM-AYCACATTGGCACCCGCAATCCTG-BHQ1-3′ |
Negative: no Ct value or Ct value ≥ 40 Positive: Ct value < 37 Gray zone: Ct value range between 37 and 40 |
| National Institute of Infectious Diseases, Japan | Pan-corona and multiple targets, Spike protein | N: F: AAATTTTGGGGACCAGGAAC R: TGGCAGCTGTGTAGGTCAAC P: 5′-FAM-ATGTCGCGCATTGGCATGGA-BHQ1-3′ |
|
| China CDC, China | ORF1ab and N | ORF1ab F:CCCTGTGGGTTTTACACTTAA R: ACGATTGTGCATCAGCTGA P: 5′-FAM-CCGTCTGCGGTATGTGGAAAGGTTATGG-BHQ1-3′ N F: GGGGAACTTCTCCTGCTAGAAT R: CAGACATTTTGCTCTCAAGCTG P: 5′-FAM-TTGCTGCTGCTTGACAGATT-TAMRA-3′ |
Negative: no Ct value or Ct value ≥ 40 Positive: Ct value < 37 Gray zone: CT value range between 37 and 40 |
| Institute Pasteur, Paris, France | nCoV_IP2, nCoV_IP4, E | nCoV_IP2: F: ATGAGCTTAGTCCTGTTG R: CTCCCTTTGTTGTGTTGT P: 5′-FAM-AGATGTCTTGTGCTGCCGGTA-BHQ1-3′ nCoV_IP4: F: GGTAACTGGTATGATTTCG R: CTGGTCAAGGTTAATATAGG P: 5′-FAM-TCATACAAACCACGCCAGG-BHQ1-3′ E: F: ACAGGTACGTTAATAGTTAATAGCGT R: ATATTGCAGCAGTACGCACACA P: 5′-FAM-ACACTAGCCATCCTTACTGCGCTTCG-BHQ1-3′ |
|
| Charité, Germany | RdRP, E, N | RdRp: F: GTGARATGGTCATGTGTGGCGG R: CARATGTTAAASACACTATTAGCATA P: 5′-FAM-CAGGTGGAACCTCATCAGGAGATGC-BBQ-3′ E: F: ACAGGTACGTTAATAGTTAATAGCGT R: ATATTGCAGCAGTACGCACACA P: 5′-FAM-ACACTAGCCATCCTTACTGCGCTTCG-BBQ-3′ |
|
| HKU, Hong Kong SAR | ORF1b-nsp14, N | ORF1b-nsp 14: F: TGGGGYTTTACRGGTAACCT R: AACRCGCTTAACAAAGCACTC P: 5′-FAM-TAGTTGTGATGCWATCATGACTAG- TAMRA-3′ N: F:TAATCAGACAAGGAACTGATTA R: CGAAGGTGTGACTTCCATG P: 5′-FAM-GCAAATTGTGCAATTTGCGG- TAMRA-3′ |
|
| National Institute of Health, Thailand | N | N: F: CGTTTGGTGGACCCTCAGAT R: CCCCACTGCGTTCTCCATT P: 5′-FAM-CAACTGGCAGTAACCA- BHQ1-3′ |
In addition to general criteria that should be considered for primer design such as primers with a length between 16 and 28 nucleotides, a Tm between 50 and 62 °C for a GC content between 45 and 55% that should differ not more than 5 °C, an annealing temperature 5 °C lower than Tm with the best value between 50 and 55 °C, designing primers with at least two G/C bases and no A base in the 3ʹend and finally avoiding primers that could create 3ʹend self-complementary, hair pains and other related issues, there are some specific cautions that could improve the rRT-PCR assay. One important tip by which false negative results could be decreased, is designing primer with a Tm of 60 °C and annealing temperature of 55 °C to be able to amplify genomes with a mismatches. With regards to probe design, the hydrolysis efficiency increases provided that the probe located near the upstream primer. In addition the 5ʹend of primer should not start with a G base. Finally, compared to the loops, the region that is rather to design primer is the stem structures, because of their higher stability [46].
CDC reports primers related to a Nucleocapsid protein associated gene (N gene) known as N1, 2, 3. In contrast, the WHO recommended primers from the RdRp, E and N genes. Therefore, the different types of primers and probes used in various laboratories may have significant effects on the diagnostic accuracy, diagnostic window, sensitivity and specificity of the test [11], [17], [26], [44]. Comparison of two major protocol for efficient diagnosis of SARS-CoV-2 including Charité protocol which targets E, RdRP, and N genes and CDC protocol which is developed to detect three N genes (N1, N2, and N3 genes) revealed worthy information about usefulness of each method. One predictable founding is that the cotton swabs lead to negative results and should not use for sampling. Also N, N2 and N3 assays had no analytical specificity because they made known negative samples amplified. Furthermore, the N1, E and RdRP assays showed better amplification efficiency (93.4%, 86% and 110%, respectively) which indicated their higher diagnostic efficacy. On the other hand the higher diagnostic sensitivity which was determined by measuring the limit of detection (LOD), was observed in N1 (21 copies/reaction) and RdRP (33.7 copies/reaction). Finally, the N1 assay showed more positive results than E, and RdRP. The observation that E assay shows better diagnostic capability than RdRP is inconsistent with this fact that RdRP has better amplification efficiency and LOD as compared to E assay. This issue might be related to the presence of cellular contents which affected the frequency of target gene. In addition, because the N gene sequence located in most subgenomic regions, it has the high expression level and in contrast, the RdRP presents in the ORF1b region and therefor has low expression. All in all, the results of this study showed that the N1 assay has all needed diagnostic criteria to detect SARS-CoV-2, efficiently [50].
Nowadays, mutations in SARS-CoV-2 genome are going to be the most important concern in diagnosis of COVID-19 disease. Studies on the presence of haplotypes and mutations in virus genome have revealed that this viral evolution not only explain the difference in response to individual immunity, severity, pathogenicity, and transmissibility, but also alter diagnostic accuracy of rRT-PCR, which can explain the reason of the mismatch between the primer and probe with the virus genome [51], [52]. In a recent study the effect of genetic variations on the results of rRT-PCR have assessed and also the researchers studied whether how these variations can impact on the sensitivity of the test. They found 11,627 of genome included single nucleotide mutations in the SARS-CoV-2 genome that might impact on PCR assay procedure. About 26% of the variations were high risk and among them 8251 variations would affect the annealing step of the N gene forward primer in National Microbiology Data Center (NMDC) panel assay. Also several variations with much lower importance were reported specially in the RdRp reverse primer, Probe (RdRp_SARSr-P2) or even forward primer biding region of the WHO assay. Although most of these variations would not decrease the sensitivity of PCR procedure in the panel level, due to increase in genome variations and to mitigate the risk of loss in diagnostic efficiency, several targets should be combined in an efficient diagnostic panel for SARS-CoV-2 [53]. Each of above mentioned problems may be considered as errors that lead to false negative results in COVID-19 rRT-PCR testing.
4. Post-analytical errors
There is a paucity of studies which have reported post analytical laboratory errors associated with detection of COVID-19. Nevertheless, these errors may happen during this phase of process. One of the most common sources of error is data misinterpretation by operator. By drawing an accurate diagram for base line and thresholds, curves and appropriate controls and ensuring test sensitivity, the probability of these misinterpretations could be greatly reduced. For example, if the standard curve line slope increase, it leads to decreased efficiency, increased cycle of threshold (CT) and decreased sensitivity of the method. This type of error causes to falsely increase the CT of the curves with low concentration of RNA or cDNA. There is a possibility of pattern destruction, which is usually due to frequent freezing and thawing of standards or use of very low concentration patterns [23], [54].
The amplification curves are important to determine exact baseline and threshold. RRT-PCR results for positive COVID-19 should have a CT less than 40, and the results more than 40 should be considered as negative result. Samples with a CT values of 37–40 must be re-sampled. The first step in troubleshooting results with no typical S shape curve for internal control and a positive or negative results for target genes, is re-analyzing the PCR process. If the results repeated, re-sampling is inevitable. Determining the best threshold depends on the prevalence of the disease in a specific region, so that during the peak period, higher CT can also indicate the disease, but when the prevalence is reduced, CT should be determined low. Real-time PCR is a very sensitive method so that the pipetting, quality of components, calibration of equipment and temperature lead to variable and improper Results. Therefore, uses of internal controls improve the accuracy of PCR process [22], [25], [38], [39].
The efficiency of the real time RT-PCR reaction is a pivotal factor. The optimal efficacy is 90–110%. The efficiency more than 110% can be an inhibitory factor for PCR, which can lead to decrease CT and misinterpretation. The efficiency of less than 90% can be resulted from non-optimal concentrations of primers, magnesium ion, polymerase enzyme and more than 5℃ difference in Tm of the forward and reverse primers, as well as, non-optimal temperature. Altogether, optimal efficiency is necessary to accurate and valuable PCR results and should be considered before data analysis [23], [39], [55].
5. Conclusion
We reviewed some possible source of false-negative or false-positive results. Regarding to the priority of COVID-19 diagnosis, all aspects of error generation (pre-analytical, analytical and post-analytic) should be optimized and comprehensive protocols should be prepared.
As mentioned, pre-analytical errors are considered as the main possible sources of errors in diagnosis of COVID-19. There are several potential factors for pre-analytical errors including, sampling equipment, sampling location and sampling time.
With regards to analytical phase, RNA extraction is the main concern and its quantity and quality can be considered as vital factors in diagnosis; so standard guidelines must be followed. Primer design, its preparation and storage condition along with other PCR components and also pipettor calibration should be performed perfectly. Depending on the type of primer used, the rRT-PCR process should be optimized and if the mutations in the virus genome are reported, new approved primers should be replaced.
In post analytical phase, it is essential to use a variety of positive and negative controls to confirm and interpret the obtained results. Therefore, using controls is crucial for every run and the results should analyze according to the controls. Finally, personnel who analyze and interpret the data should have required knowledge and abilities.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Chen Y., Liu Q., Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lau S.K., Lee P., Tsang A.K., Yip C.C., Tse H., Lee R.A., So L.Y., Lau Y.L., Chan K.H., Woo P.C., Yuen K.Y. Molecular epidemiology of human coronavirus OC43 reveals evolution of different genotypes over time and recent emergence of a novel genotype due to natural recombination. J. Virol. 2011;85(21):11325–11337. doi: 10.1128/JVI.05512-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loeffelholz M.J., Tang Y.W. Laboratory diagnosis of emerging human coronavirus infections - the state of the art. Emerg. Microbes Infect. 2020;9(1):747–756. doi: 10.1080/22221751.2020.1745095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coronaviridae V. Study Group of the International Committee on Taxonomy of, The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. “World Health Organization declares Global Emergency: A review of the 2019 Novel Coronavirus (COVID-19)” [Int. J. Surg. 76 (2020) 71-76] Int. J. Surg. 2020;77:217. doi: 10.1016/j.ijsu.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ji W., Li X. Response to comments on “Cross-species Transmission of the Newly Identified Coronavirus 2019-nCoV” and “Codon bias analysis may be insufficient for identifying host(s) of a novel virus”. J. Med. Virol. 2020 doi: 10.1002/jmv.26048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y., Yuan M.L., Zhang Y.L., Dai F.H., Liu Y., Wang Q.M., Zheng J.J., Xu L., Holmes E.C., Zhang Y.Z. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu L., Wang B., Yuan T., Chen X., Ao Y., Fitzpatrick T., Li P., Zhou Y., Lin Y.F., Duan Q., Luo G., Fan S., Lu Y., Feng A., Zhan Y., Liang B., Cai W., Zhang L., Du X., Li L., Shu Y., Zou H. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J. Infect. 2020;80(6):656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., Bleicker T., Brunink S., Schneider J., Schmidt M.L., Mulders D.G., Haagmans B.L., van der Veer B., van den Brink S., Wijsman L., Goderski G., Romette J.L., Ellis J., Zambon M., Peiris M., Goossens H., Reusken C., Koopmans M.P., Drosten C. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro. Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pang J., Wang M.X., Ang I.Y.H., Tan S.H.X., Lewis R.F., Chen J.I., Gutierrez R.A., Gwee S.X.W., Chua P.E.Y., Yang Q., Ng X.Y., Yap R.K., Tan H.Y., Teo Y.Y., Tan C.C., Cook A.R., Yap J.C., Hsu L.Y. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel Coronavirus (2019-nCoV): A Systematic Review. J. Clin. Med. 2020;9(3) doi: 10.3390/jcm9030623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaltenboeck B., Wang C. Advances in real-time PCR: application to clinical laboratory diagnostics. Adv. Clin. Chem. 2005;40:219–259. doi: 10.1016/S0065-2423(05)40006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer G., Muller J., Lunse C.E. RNA diagnostics: real-time RT-PCR strategies and promising novel target RNAs. Wiley Interdiscip. Rev. RNA. 2011;2(1):32–41. doi: 10.1002/wrna.46. [DOI] [PubMed] [Google Scholar]
- 15.Y.H. Jin, L. Cai, Z.S. Cheng, H. Cheng, T. Deng, Y.P. Fan, C. Fang, D. Huang, L.Q. Huang, Q. Huang, Y. Han, B. Hu, F. Hu, B.H. Li, Y.R. Li, K. Liang, L.K. Lin, L.S. Luo, J. Ma, L.L. Ma, Z.Y. Peng, Y.B. Pan, Z.Y. Pan, X.Q. Ren, H.M. Sun, Y. Wang, Y.Y. Wang, H. Weng, C.J. Wei, D.F. Wu, J. Xia, Y. Xiong, H.B. Xu, X.M. Yao, Y.F. Yuan, T.S. Ye, X.C. Zhang, Y.W. Zhang, Y.G. Zhang, H.M. Zhang, Y. Zhao, M.J. Zhao, H. Zi, X.T. Zeng, Y.Y. Wang, X.H. Wang, f.t.Z.H.o.W.U.N.C. Management, E.-B.M.C.o.C.I.E. Research Team, M. Promotive Association for, C. Health, A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version), Mil Med. Res. 7(1) (2020) 4. [DOI] [PMC free article] [PubMed]
- 16.Lippi G., Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin. Chem. Lab. Med. 2020;58(7):1131–1134. doi: 10.1515/cclm-2020-0198. [DOI] [PubMed] [Google Scholar]
- 17.Lippi G., Simundic A.M., Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19) Clin. Chem. Lab. Med. 2020;58(7):1070–1076. doi: 10.1515/cclm-2020-0285. [DOI] [PubMed] [Google Scholar]
- 18.Espy M.J., Uhl J.R., Sloan L.M., Buckwalter S.P., Jones M.F., Vetter E.A., Yao J.D., Wengenack N.L., Rosenblatt J.E., Cockerill F.R., 3rd, Smith T.F. Real-time PCR in clinical microbiology: applications for routine laboratory testing. Clin. Microbiol. Rev. 2006;19(1):165–256. doi: 10.1128/CMR.19.1.165-256.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lippi G., Lima-Oliveira G., Brocco G., Bassi A., Salvagno G.L. Estimating the intra- and inter-individual imprecision of manual pipetting. Clin. Chem. Lab. Med. 2017;55(7):962–966. doi: 10.1515/cclm-2016-0810. [DOI] [PubMed] [Google Scholar]
- 20.G. Lippi, A. von Meyer, J. Cadamuro, A.M. Simundic, C. European Federation of Clinical, P. Laboratory Medicine Working Group for Preanalytical, PREDICT: a checklist for preventing preanalytical diagnostic errors in clinical trials, Clin. Chem. Lab Med. 58(4) (2020) 518–526. [DOI] [PubMed]
- 21.van Zyl G., Maritz J., Newman H., Preiser W. Lessons in diagnostic virology: expected and unexpected sources of error. Rev. Med. Virol. 2019;29(4) doi: 10.1002/rmv.2052. [DOI] [PubMed] [Google Scholar]
- 22.Tang Y.W., Schmitz J.E., Persing D.H., Stratton C.W. Laboratory Diagnosis of COVID-19: Current Issues and Challenges. J. Clin. Microbiol. 2020;58(6) doi: 10.1128/JCM.00512-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kralik P., Ricchi M. A Basic Guide to Real Time PCR in Microbial Diagnostics: Definitions, Parameters, and Everything. Front. Microbiol. 2017;8:108. doi: 10.3389/fmicb.2017.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.G. Lippi, A.M. Simundic, C. European Federation for Clinical, P. Laboratory Medicine Working Group for Preanalytical, The EFLM strategy for harmonization of the preanalytical phase, Clin. Chem. Lab Med. 56(10) (2018) 1660-1666. [DOI] [PubMed]
- 25.Centers for Disease Control and Prevention. Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons Under Investigation (PUIs) for Coronavirus Disease 2019 (COVID-19), 2020. https://www.cdc.gov/coronavirus/2019-ncov/lab/guidelines-clinical-specimens.html (accessed Nov. 5, 2020).
- 26.World Health Organization. Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases: interim guidance, 2020. https://apps.who.int/iris/handle/10665/331329 (accessed 2 March 2020).
- 27.Li Y., Yao L., Li J., Chen L., Song Y., Cai Z., Yang C. Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19. J. Med. Virol. 2020;92(7):903–908. doi: 10.1002/jmv.25786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrader C., Schielke A., Ellerbroek L., Johne R. PCR inhibitors - occurrence, properties and removal. J. Appl. Microbiol. 2012;113(5):1014–1026. doi: 10.1111/j.1365-2672.2012.05384.x. [DOI] [PubMed] [Google Scholar]
- 29.Radbel J., Jagpal S., Roy J., Brooks A., Tischfield J., Sheldon M., Bixby C., Witt D., Gennaro M.L., Horton D.B., Barrett E.S., Carson J.L., Panettieri R.A., Jr., Blaser M.J. Detection of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Is Comparable in Clinical Samples Preserved in Saline or Viral Transport Medium. J. Mol. Diagn. 2020;22(7):871–875. doi: 10.1016/j.jmoldx.2020.04.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Basso D., Aita A., Navaglia F., Franchin E., Fioretto P., Moz S., Bozzato D., Zambon C.F., Martin B., Dal Pra C., Crisanti A., Plebani M. SARS-CoV-2 RNA identification in nasopharyngeal swabs: issues in pre-analytics. Clin. Chem. Lab. Med. 2020;58(9):1579–1586. doi: 10.1515/cclm-2020-0749. [DOI] [PubMed] [Google Scholar]
- 31.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296(2):E32–E40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020;25(5):2000062. doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Errors in Text, Figure, and End Matter, JAMA 323(15) (2020) 1510. [DOI] [PMC free article] [PubMed]
- 34.Feng H., Liu Y., Lv M., Zhong J. A case report of COVID-19 with false negative RT-PCR test: necessity of chest CT. Jpn. J. Radiol. 2020;38(5):409–410. doi: 10.1007/s11604-020-00967-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li D., Wang D., Dong J., Wang N., Huang H., Xu H., Xia C. False-Negative Results of Real-Time Reverse-Transcriptase Polymerase Chain Reaction for Severe Acute Respiratory Syndrome Coronavirus 2: Role of Deep-Learning-Based CT Diagnosis and Insights from Two Cases. Korean J. Radiol. 2020;21(4):505–508. doi: 10.3348/kjr.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., Yu J., Kang M., Song Y., Xia J., Guo Q., Song T., He J., Yen H.L., Peiris M., Wu J. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pan Y., Long L., Zhang D., Yuan T., Cui S., Yang P., Wang Q., Ren S. Potential False-Negative Nucleic Acid Testing Results for Severe Acute Respiratory Syndrome Coronavirus 2 from Thermal Inactivation of Samples with Low Viral Loads. Clin. Chem. 2020;66(6):794–801. doi: 10.1093/clinchem/hvaa091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burkardt H.J. Standardization and quality control of PCR analyses. Clin. Chem. Lab. Med. 2000;38(2):87–91. doi: 10.1515/CCLM.2000.014. [DOI] [PubMed] [Google Scholar]
- 39.Kuang J., Yan X., Genders A.J., Granata C., Bishop D.J. An overview of technical considerations when using quantitative real-time PCR analysis of gene expression in human exercise research. PLoS ONE. 2018;13(5) doi: 10.1371/journal.pone.0196438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taylor S.C., Nadeau K., Abbasi M., Lachance C., Nguyen M., Fenrich J. The Ultimate qPCR Experiment: Producing Publication Quality, Reproducible Data the First Time. Trends Biotechnol. 2019;37(7):761–774. doi: 10.1016/j.tibtech.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 41.Ali N., Rampazzo R.C.P., Costa A.D.T., Krieger M.A. Current Nucleic Acid Extraction Methods and Their Implications to Point-of-Care Diagnostics. Biomed. Res. Int. 2017;2017:9306564. doi: 10.1155/2017/9306564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fleige S., Pfaffl M.W. RNA integrity and the effect on the real-time qRT-PCR performance. Mol. Aspects Med. 2006;27(2–3):126–139. doi: 10.1016/j.mam.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Younes N., Al-Sadeq D.W., Al-Jighefee H., Younes S., Al-Jamal O., Daas H.I., Yassine H.M., Nasrallah G.K. Challenges in Laboratory Diagnosis of the Novel Coronavirus SARS-CoV-2. Viruses. 2020;12(6) doi: 10.3390/v12060582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y.C., Chen H., Mubareka S., Gubbay J.B., Chan W.C.W. Diagnosing COVID-19: The Disease and Tools for Detection. ACS Nano. 2020;14(4):3822–3835. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 45.Falzone L., Musso N., Gattuso G., Bongiorno D., Palermo C.I., Scalia G., Libra M., Stefani S. Sensitivity assessment of droplet digital PCR for SARS-CoV-2 detection. Int. J. Mol. Med. 2020;46(3):957–964. doi: 10.3892/ijmm.2020.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li D., Zhang J., Li J. Primer design for quantitative real-time PCR for the emerging Coronavirus SARS-CoV-2. Theranostics. 2020;10(16):7150–7162. doi: 10.7150/thno.47649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mollaei H.R., Afshar A.A., Kalantar-Neyestanaki D., Fazlalipour M., Aflatoonian B. Comparison five primer sets from different genome region of COVID-19 for detection of virus infection by conventional RT-PCR. Iran. J. Microbiol. 2020;12(3):185–193. [PMC free article] [PubMed] [Google Scholar]
- 48.Vogels C.B.F., Brito A.F., Wyllie A.L., Fauver J.R., Ott I.M., Kalinich C.C., Petrone M.E., Casanovas-Massana A., Catherine Muenker M., Moore A.J., Klein J., Lu P., Lu-Culligan A., Jiang X., Kim D.J., Kudo E., Mao T., Moriyama M., Oh J.E., Park A., Silva J., Song E., Takahashi T., Taura M., Tokuyama M., Venkataraman A., Weizman O.E., Wong P., Yang Y., Cheemarla N.R., White E.B., Lapidus S., Earnest R., Geng B., Vijayakumar P., Odio C., Fournier J., Bermejo S., Farhadian S., Dela Cruz C.S., Iwasaki A., Ko A.I., Landry M.L., Foxman E.F., Grubaugh N.D. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT-qPCR primer-probe sets. Nat. Microbiol. 2020;5(10):1299–1305. doi: 10.1038/s41564-020-0761-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cuong H.Q., Hai N.D., Linh H.T., Anh N.H., Hieu N.T., Thang C.M., Thao N.T.T., Lan P.T. Comparison of Primer-Probe Sets among Different Master Mixes for Laboratory Screening of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Biomed. Res. Int. 2020;2020:7610678. doi: 10.1155/2020/7610678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barra G.B., Santa Rita T.H., Mesquita P.G., Jacomo R.H., Nery L.F.A. Analytical Sensitivity and Specificity of Two RT-qPCR Protocols for SARS-CoV-2 Detection Performed in an Automated Workflow. Genes (Basel) 2020;11(10) doi: 10.3390/genes11101183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shen Z., Xiao Y., Kang L., Ma W., Shi L., Zhang L., Zhou Z., Yang J., Zhong J., Yang D., Guo L., Zhang G., Li H., Xu Y., Chen M., Gao Z., Wang J., Ren L., Li M. Genomic Diversity of Severe Acute Respiratory Syndrome-Coronavirus 2 in Patients With Coronavirus Disease 2019. Clin. Infect. Dis. 2020;71(15):713–720. doi: 10.1093/cid/ciaa203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yi H. 2019 Novel Coronavirus Is Undergoing Active Recombination. Clin. Infect. Dis. 2020;71(15):884–887. doi: 10.1093/cid/ciaa219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Penarrubia L., Ruiz M., Porco R., Rao S.N., Juanola-Falgarona M., Manissero D., Lopez-Fontanals M., Pareja J. Multiple assays in a real-time RT-PCR SARS-CoV-2 panel can mitigate the risk of loss of sensitivity by new genomic variants during the COVID-19 outbreak. Int. J. Infect. Dis. 2020;97:225–229. doi: 10.1016/j.ijid.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen P., Huang X. Comparison of analytic methods for quantitative real-time polymerase chain reaction data. J. Comput. Biol. 2015;22(11):988–996. doi: 10.1089/cmb.2015.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gurtler C., Laible M., Schwabe W., Steinhauser H., Li X., Liu S., Schlombs K., Sahin U. Transferring a Quantitative Molecular Diagnostic Test to Multiple Real-Time Quantitative PCR Platforms. J. Mol. Diagn. 2018;20(4):398–414. doi: 10.1016/j.jmoldx.2018.02.004. [DOI] [PubMed] [Google Scholar]