Abstract
Introduction
The importance of receiving an annual influenza vaccine among patients with atherosclerotic cardiovascular disease (ASCVD) is well established. With the rapid community spread and the possibility of another wave of COVID-19 infections in the fall, receiving an influenza vaccine is of particular importance to mitigate the risk associated with overlapping influenza and COVID-19 infections.
Methods
We utilized cross-sectional data from the 2016 to 2019 Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative U.S. telephone-based survey of adults 18 years or older. Race/ethnicity was our exposure of interest. We assessed the relative difference in influenza vaccination by race/ethnicity for each U.S. state in the overall U.S. population and among those with ASCVD as prevalence of receipt of influenza vaccination among Blacks or Hispanics minus prevalence among Whites divided by prevalence among Whites. We used multivariable-adjusted logistic regression models to evaluate the association between socioeconomic risk factors and receipt of influenza vaccination.
Results
The study population consisted of 1,747,397 participants of whom 21% were older than 65 years, 51% women, 63% White, 12% Black, 17% Hispanic, and 9% with history of ASCVD. The receipt of influenza vaccine was 38% in the overall population and 51% among those with self-reported ASCVD, which translates to approximately to 97 million and 12 million US adults, respectively. The receipt of influenza vaccine among individuals with ASCVD was 54% for Whites, 45% for Blacks, and 42% for Hispanics (p<0.001). In the overall U.S. population, the median (interquartile range) relative difference for influenza vaccination between Blacks and Whites was 17% (-27%, -9%) and –22% (-29%, -9%) between Hispanics and Whites across all U.S. states. Among individuals with and without ASCVD, age older than 65 years, greater than college education, higher income, and having a primary care physician were significantly associated with higher odds of receipt of influenza vaccination, while being employed, lack of healthcare coverage, Black race, and delay in healthcare access were significantly inversely associated with having received an influenza vaccine
Conclusions
Only 50% patients with ASCVD receive influenza vaccines. The receipt of influenza vaccination among individuals with ASCVD is lower among Blacks and Hispanics compared to Whites with significant state-level variation. There are important socioeconomic determinants that are associated with receipt of the influenza vaccine.
Keywords: Influenza vaccine, COVID-19, Race/ethnicity, Atherosclerotic cardiovascular disease
1. Introduction
The COVID-19 pandemic has presented numerous challenges to the healthcare system including a high rate of transmission, a high rate of hospitalizations, cardiorespiratory complications often requiring intensive care unit admissions with prolonged length of stay, and until recently, the lack of an effective treatment and vaccine [1], [2], [3].
At the time of the writing of this paper, we are currently in the middle of this year's influenza season, which may be especially challenging given the community spread with COVID-19. This has public health officials especially concerned about two respiratory pathogens circulating this influenza season i.e. influenza and SARS-CoV-2 which may result in increased hospitalizations that could overwhelm the healthcare infrastructure. While clinicians and public health officials stress the importance of receiving annual influenza vaccinations, vaccination rates remain low in the general population and may differ by race/ethnicity [4,5]. These disparities can also be geographic in nature as vaccine hesitancy has been shown to cluster by geography as well [5]. Receiving an influenza vaccine is particularly critical among patients with cardiovascular risk factors and those with atherosclerotic cardiovascular disease (ASCVD) [6].
It is important to evaluate influenza vaccination rates among patients with ASCVD. This information is helpful in the context of COVID-19 where patients with ASCVD are not only more likely to contract this virus but also more likely to be hospitalized and die as a result of it [7]. It is also important to assess socioeconomic determinants of influenza vaccination by race/ethnicity as Blacks and Hispanics have been disproportionately affected by COVID-19 [8]. Lastly, regional variations in influenza vaccination may have ramifications for COVID-19 as well with respect to vaccine distribution.
We therefore evaluate the proportion of the overall U.S. population receiving influenza vaccines, and specifically those with ASCVD. Furthermore, we study the interrelationship between socioeconomic determinants and racial disparities in the receipt of influenza vaccine and assess the geographic variations in such disparities.
2. Methods
The Behavioral Risk Factor Surveillance System (BRFSS) survey is established by the Centers for Disease Control and Prevention. BRFSS is a nationwide telephone-based questionnaire survey administered to a random sample that is representative of the U.S. adult residents 18 years and over. The BRFSS is a cross-sectional survey that aims to evaluate chronic health conditions, health-related risk behaviors, and the use of preventive services among U.S adults. The survey is conducted in all 50 U.S. states, the District of Columbia, and the 3 U.S. territories, which makes BRFSS the largest telephone-based survey in the world. We utilized cross-sectional data from the 2016, 2017, 2018, and 2019 BRFSS surveys. The study was exempt from Institutional Review Board approval since it utilized de-identified data from a publicly available dataset.
All variables were self-reported. Participants were considered to have received the influenza vaccine if they answered “Yes” to the question “During the past 12 months, have you had either a flu shot or a flu vaccine that was sprayed in your nose?” ASCVD was identified if participants reported a prior history of coronary heart disease or stroke, based on their response to the following questions: "Has a doctor, nurse, or other health professional ever told you that you had 1) coronary heart disease or myocardial infarction; or 2) a stroke? Self-reported variables in BRFSS have been shown to be valid when compared to other national survey data [9,10].
2.1. Statistical analysis
Prevalence of receipt of influenza vaccine was analyzed using survey weights as the BRFSS utilized design weighting and iterative proportional fitting in order to ensure representativeness of the data to the US population [11]. The results were summarized for the overall study population and among those with history of ASCVD, by race/ethnicity, and U.S. state. We examined temporal trends in receipt of influenza vaccine from 2016 to 2019 in the overall population and for each race/ethnic group. We also used multivariable logistic regression models to study the association between ASCVD, race/ethnicity and receipt of influenza vaccine adjusting for age, sex, education, employment status, income, presence of a primary care physician (PCP), delay in healthcare access, healthcare coverage, hypertension, diabetes mellitus, hyperlipidemia, and cigarette smoking status. We calculated the relative difference in receipt of influenza vaccine by race/ethnicity in each U.S. state as prevalence of receipt of influenza vaccine among Blacks or Hispanics minus the prevalence in Whites and divided by the prevalence in Whites. We then graphically depicted these relative differences across U.S. states using heat maps that were generated by Excel.
In sensitivity analyses, we 1) evaluated the association of socioeconomic determinants and receipt of influenza vaccination in each race/ethnic group; and 2) evaluated the interaction between these determinants and race/ethnicity.
Analyses were conducted using Stata version 16.1 (StataCorp, College Station, Texas) and a two-sided p-value <0.05 was considered statistically significant.
3. Results
3.1. Baseline characteristics
The study population consisted of 1,747,397 participants of whom 21% were older than 65 years, 51% women, 63% White, 12% Black, 17% Hispanic, and 9% with history of ASCVD. At the time of this survey, the U.S. population aged 18 years or older was estimated at 255,200,373 based on U.S. census bureau estimates of the U.S. population. In the overall population, 38% reported receiving influenza vaccination and 51% among those with self-reported ASCVD, which translates to approximately to 97 million and 12 million US adults, respectively.
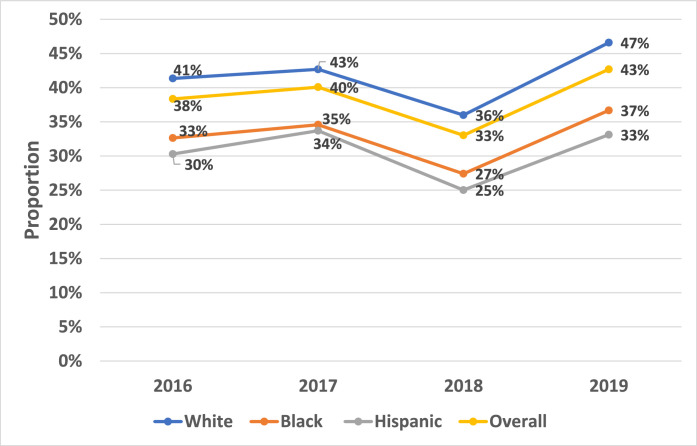
Whites were older, had higher income, a PCP and healthcare coverage, more likely to be educated, but less likely to have delay in healthcare access and be unemployed (Table 1). The proportion of individuals who reported receiving an influenza vaccine in 2016 was 41% among Whites, 33% among Blacks, and 30% among Hispanics. These trends were similar for the years 2017, 2018, and 2019; all p<0.001 (Fig. 1).
Table 1.
Baseline characteristics of the study population by race/ethnicity.
| Race/Ethnicity |
||||
|---|---|---|---|---|
| White (N = 1309,737; 63%) |
Black (N = 138,279; 12%) |
Hispanic (N = 145,071; 17%) |
Other (N = 120,271; 8%) |
|
| Age (years) | ||||
| 18–34 | 174,457 (25%) | 26,051 (32%) | 45,691 (41%) | 31,903 (39%) |
| 35–44 | 132,796 (14%) | 18,885 (18%) | 28,800 (21%) | 18,970 (20%) |
| 45–54 | 192,474 (16%) | 23,689 (18%) | 25,442 (16%) | 20,179 (15%) |
| 55–64 | 288,145 (18%) | 30,746 (16%) | 21,501 (12%) | 21,744 (13%) |
| ≥65 | 521,865 (26%) | 38,908 (16%) | 23,637 (10%) | 27,475 (13%) |
| Women | 727,232 (51%) | 84,795 (54%) | 79,577 (50%) | 61,384 (50%) |
| Education | ||||
| Less than high school | 63,933 (8%) | 15,303 (14%) | 38,131 (35%) | 9526 (8%) |
| High school – Some college | 721,890 (61%) | 83,681 (66%) | 73,979 (51%) | 64,417 (50%) |
| College graduate | 520,967 (31%) | 38,807 (21%) | 32,203 (14%) | 45,819 (42%) |
| Employment | ||||
| Employed | 638,163 (57%) | 65,260 (56%) | 80,736 (60%) | 63,715 (59%) |
| Unemployed | 191,496 (16%) | 31,427 (22%) | 31,427 (26%) | 24,201 (17%) |
| Student | 26,611 (5%) | 4695 (6%) | 6456 (6%) | 7413 (13%) |
| Retired | 443,597 (23%) | 34,768 (15%) | 18,545 (8%) | 23,196 (11%) |
| Income ≥ $75,000 | 402,181 (41%) | 22,041 (22%) | 19,397 (17%) | 28,687 (40%) |
| Presence of any healthcare coverage | 1230,945 (92%) | 122,511 (86%) | 109,708 (71%) | 108,092 (90%) |
| Presence of a primary care physician | 1125,469 (82%) | 114,534 (77%) | 98,029 (62%) | 91,256 (75%) |
| Delay in healthcare coverage | 126,175 (12%) | 22,719 (18%) | 29,565 (21%) | 17,983 (14%) |
| Influenza vaccine in past 12 months | 585,644 (42%) | 47,301 (33%) | 43,888 (31%) | 43,936 (39%) |
| Current cigarette smoking | 178,800 (17%) | 22,044 (18%) | 17,281 (13%) | 21,765 (14%) |
| Hypertension | 261,599 (34%) | 34,601 (41%) | 21,953 (25%) | 21,197 (25%) |
| Hypercholesterolemia | 234,070 (34%) | 22,474 (29%) | 19,641 (27%) | 17,300 (27%) |
| Diabetes mellitus | 167,907 (11%) | 28,138 (15%) | 20,068 (12%) | 17,997 (10%) |
| Atherosclerotic Cardiovascular Disease | 158,831 (10%) | 16,542 (9%) | 10,636 (6%) | 13,046 (6%) |
All p-values are <0.001.
Fig. 1.
Temporal trends in the prevalence of receipt of influenza vaccine in the overall U.S. population and by each race/ethnic group.
3.2. Influenza vaccination and ASCVD
Individuals with ASCVD were 10% more likely to report receiving an influenza vaccine compared to those without ASCVD (odds ratio [95% confidence interval]): 1.10 (1.06,1.15). Among those with ASCVD, the demographic factors that were independently and directly associated with receiving an influenza vaccine were older age, greater than college education, higher income, and having a PCP. In contrast, being employed, lack of healthcare coverage, Black race, and delay in healthcare access were inversely associated with having received an influenza vaccine. These results were similar among patients without prior ASCVD (Table 2).
Table 2.
Odds ratios (95% confidence interval) for the association of demographic factors with receipt of influence vaccine by atherosclerotic cardiovascular disease status.
| Demographic Factors | Odds Ratio (95% Confidence Interval) |
|
|---|---|---|
| Prior ASCVD |
||
| Yes | No | |
| Age ≥ 65 years | 1.75 (1.61,1.90) | 1.80 (1.74,1.87) |
| Female gender | 1.01 (0.94,1.08) | 1.26 (1.23,1.30) |
| Blacks (versus Whites) | 0.83 (0.74,0.93) | 0.79 (0.76,0.82) |
| Hispanics (versus Whites) | 0.99 (0.86,1.15) | 1.00 (0.96,1.05) |
| Greater than college education | 1.43 (1.26,1.62) | 1.46 (1.37,1.55) |
| Being employed | 0.69 (0.62,0.76) | 0.94 (0.90,0.98) |
| Income ≥ $75,000 | 1.33 (1.11,1.58) | 1.30 (1.21,1.40) |
| Lack of healthcare coverage | 0.62 (0.52,0.73) | 0.61 (0.57,0.64) |
| Presence of primary care physician | 2.11 (1.83,2.43) | 1.95 (1.88,2.02) |
| Delay in healthcare access | 0.80 (0.72,0.88) | 0.79 (0.76,0.83) |
Results are adjusted for all above demographic factors in addition to hypertension, diabetes mellitus, hyperlipidemia, and cigarette smoking status.
Among those with ASCVD, influenza vaccination rates were nearly twice among those less than 45 years compared to those 45 years or greater (52% vs. 29%; p<0.001). In multivariable adjusted models, individuals <45 years were 29% less likely to receive an influenza vaccination compared to those ≥45 years: 0.67 (0.57,0.79).
3.3. Influenza vaccine and race/ethnicity among individuals with ASCVD
The unadjusted prevalence of receipt of influenza vaccine among individuals with ASCVD was 54% for Whites, 45% for Blacks, and 42% for Hispanics (p<0.001), which translates to approximately to 8 million, 1 million, and 1.6 million U.S. adults, respectively. In multivariable-adjusted models, Blacks were less likely to have received an influenza vaccine compared to Whites: 0.79 (0.76,0.83) while results for Hispanics were not significant: 1.00 (0.96,1.04).
3.4. Regional variations in the receipt of influenza vaccine and race/ethnicity among individuals with ASCVD
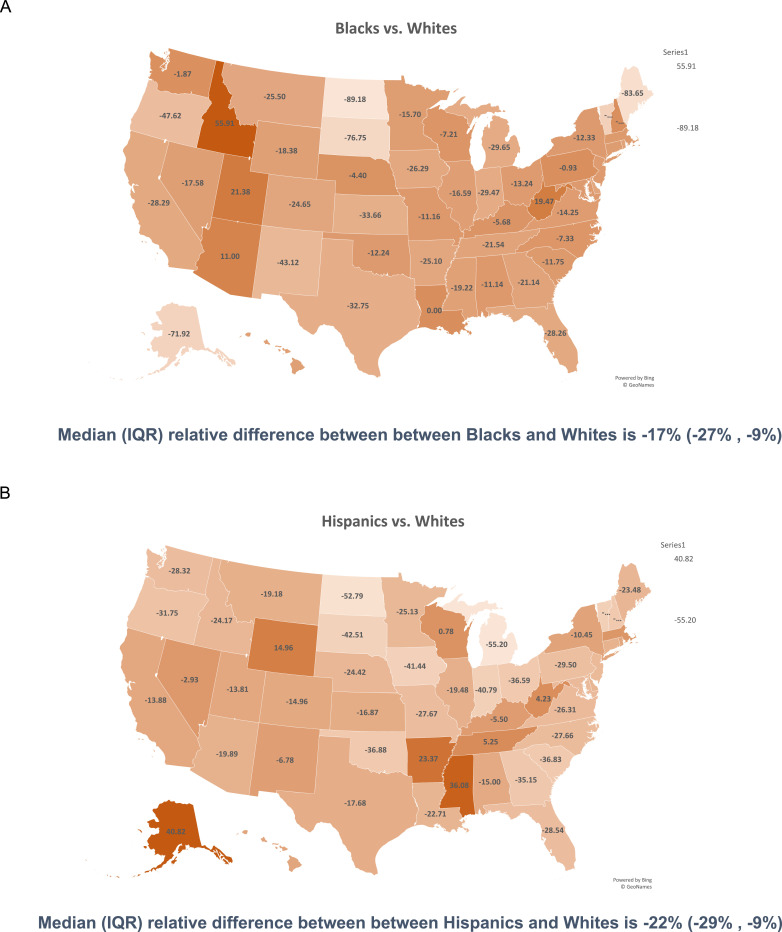
In general, across all U.S. states Blacks and Hispanics reported receipt of influenza vaccine less frequently compared to Whites with significant regional variation (Fig. 2). For example, the prevalence of receipt of influenza vaccine among Blacks was lower than Whites in 46 states with a median (IQR) relative difference of −17% (−27%, −9%) indicating that 50% of the states had at least a 17% relative difference in the receipt of influenza vaccine between White and Black patients with ASCVD (Panel A). The states with the most disparity (i.e. in the bottom 25th percentile of overall relative difference between Blacks and Whites with an overall relative difference of >27%) included Alaska, California, Florida, Indiana, Kansas, Maine, Michigan, New Mexico, North Dakota, Oregon, South Dakota, Texas, and Vermont. The prevalence for the receipt of influenza vaccine among Hispanics was lower than Whites in 43 states with a median (IQR) relative difference of −22% (−29%, −9%) between Hispanics and Whites (Panel B). The states with the most disparity (relative difference of >29%) included Georgia, Indiana, Iowa, Michigan, New Hampshire, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, South Carolina, South Dakota, and Vermont. (Fig. 3).
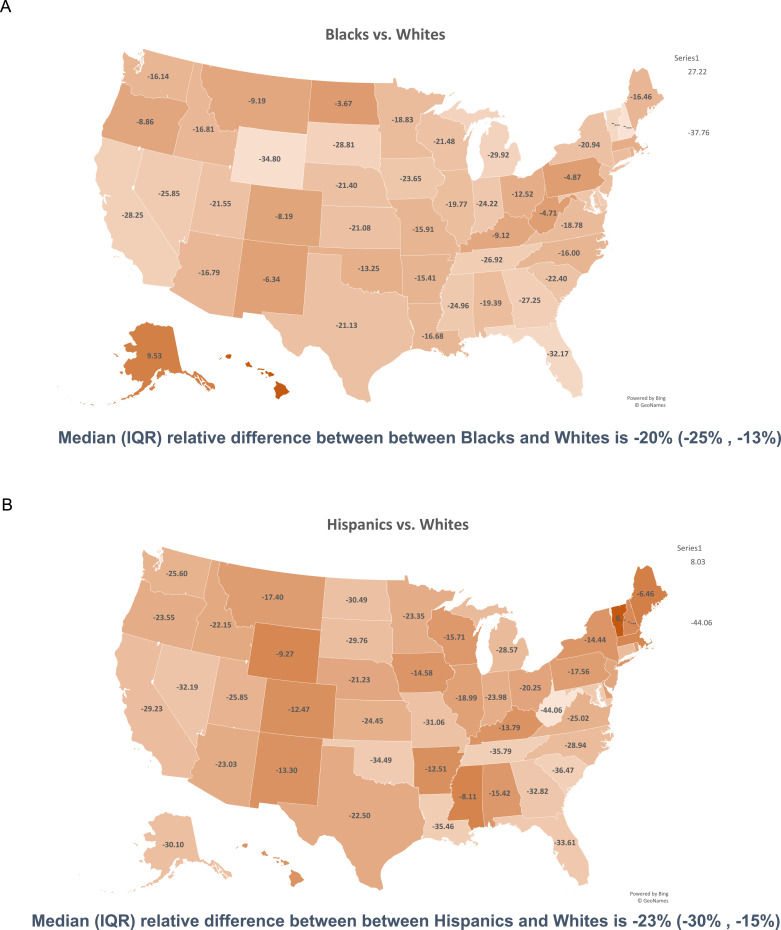
Fig. 2.
Heat map demonstrating the relative difference in prevalence of receipt of an influenza vaccine among Blacks and Hispanics compared to Whites for the overall U.S. population. The relative difference of influenza vaccine was calculated as prevalence of influenza vaccine among Blacks (panel A) or Hispanics (panel B) minus the prevalence in Whites and then divided by the prevalence in Whites.
*For example, in Illinois Blacks were 20% less likely to receive an influenza vaccine compared to Whites whereas Hispanics were 19% less likely.
Fig. 3.
Heat map demonstrating the relative difference in prevalence of receipt of an influenza vaccine among Blacks and Hispanics compared to Whites for individuals with prior self-reported atherosclerotic cardiovascular disease. The relative difference of influenza vaccine was calculated as prevalence of influenza among Blacks (panel A) or Hispanics (panel B) minus the prevalence in Whites and then divided by the prevalence in Whites.
*For example, in Texas Blacks were 33% less likely to receive an influenza vaccine compared to Whites whereas Hispanics were 18% less likely.
3.5. Sensitivity analyses
In sensitivity analyses we found that the direction of the association between socioeconomic determinants and receipt of influenza vaccination was similar for each race/ethnic group (Supplementary Table 1). There was a significant interaction between all socioeconomic determinants (except for gender) and race/ethnicity which could suggest that the association between socioeconomic risk factors and receipt of influenza vaccination is different in non-White race/ethnic groups compared to Whites. In stratified results, the adjusted prevalence of receipt of influenza vaccination remained higher among Whites compared to Blacks and Hispanics in all subgroups except among those with delay in healthcare access where prevalence of influenza vaccination was lower among Whites compared to Hispanics and Blacks (Supplementary Table 2).
4. Discussion
In a nationally representative U.S. sample, only half of patients with ASCVD reported receiving an influenza vaccine. We found that the receipt of influenza vaccine among individuals with ASCVD was lower among Blacks and Hispanics compared to Whites with significant regional variation in this disparity. There are important socioeconomic determinants that are associated with receipt of the influenza vaccine, which may be more significant among Blacks and Hispanics.
The importance of influenza vaccination is well established both for the general population, and especially among patients with prior ASCVD who may benefit from it for secondary prevention [6]. There are known racial disparities in both diagnosis and treatment of ASCVD [12], [13], [14]. We also found that there may be similar disparities in receiving a flu vaccine whereby Blacks and Hispanics with ASCVD were less likely to receive a flu vaccine compared to Whites. These results have special importance in the setting of COVID-19 which has disproportionately affected racial minority groups.
We found that socioeconomic determinants such as high income and college educations were associated with higher likelihood of receipt of the influenza vaccine, while absence of healthcare coverage and delay in access to healthcare were inversely associated with influenza vaccination. Whites in our study had higher income, a PCP and healthcare coverage, more likely to be educated, but less likely to have delay in healthcare access and be unemployed compared to Blacks and Hispanics. After adjustment for these important socioeconomic factors, Blacks were 21% less likely to report receipt of influenza vaccination compared to Whites while results for Hispanics were no longer significant. Importantly, there was a significant interaction between each of these socioeconomic determinants and race/ethnicity except gender. In stratified analyses the adjusted prevalence of receipt of influenza vaccination remained higher among Whites compared to Blacks and Hispanics suggesting that racial disparities may be even more prominent in vulnerable subgroups of low socioeconomic status.
We also found that racial disparities vary significantly across all U.S. states. As noted, evaluating these disparities at the national scale without paying attention to individual states may dilute significant disparities that may exist at the state level. Although strategies at the national scale to mitigate these disparities might work, the intensity of those efforts needs to tailored based on the relative differences at the state level as noted in our analyses. Our heat maps provide a quick overview that can be used by decision makers to understand the relative disparities that persist in various US states and therefore, the number of resources needed by each state to address these disparities.
Interestingly we also found that influenza vaccination rates were nearly twice higher among older compared to younger adults (<45 years). These results are important given that ASCVD is prevalent in young adults and that secondary prevention measures such as influenza vaccination are effective regardless of age. With reopening of the economy after widespread lockdowns to contain COVID-19, the majority of new COVID diagnoses and hospitalizations are now observed in adults <50 years. This population may be more likely to engage in behaviors such as attending large indoor gatherings and not wearing masks, which increases risk of contracting COVID-19.
With nearing of the influenza season, it is now more important than ever to receive an influenza vaccine given that it may overlap with a second wave of COVID-19. Indeed, we found that nearly half of patients with ASCVD did not receive an influenza vaccine which presents an opportunity for improvement. Such factors may be patient-related (lack of education, misinformation such as anti-vaccine movement, use of homeopathic or alternative medicines) vs. healthcare system-related factors (barriers in obtaining influenza vaccination, poor access to health care as a result of lack of employment). The prevalence of receipt of influenza vaccine and relative differences by race/ethnicity were relatively stable from 2016 to 2019 in our study despite widespread efforts to promote this practice. More quality improvement initiatives and tracking methods are urgently needed to improve adherence to the recommendation that all patients with ASCVD should receive an influenza vaccination. Targeted efforts to increase awareness and compliance with influenza vaccination such as education or incentivization may increase vaccination rates among patients with ASCVD.
With both Influenza and SARS-Cov-2 circulating in the community, there will likely be a higher number of hospitalizations and mortality that has the potential to strain and, possibly, overwhelm the healthcare system and healthcare workers. Obtaining an influenza vaccine may at least partially offset the risk related to influenza virus and decrease hospitalizations [15]. This is especially important since widespread vaccination for COVID-192,3 is not expected until at least the second quarter of 2021. All healthcare professionals should discuss and emphasize with all their patients, especially those with ASCVD, the necessity of being vaccinated for the influenza virus for decreasing risk of illness among themselves and others. With clinic visits now virtual, the telehealth platform can be utilized to promote, educate, and remind patients about the importance of being vaccinated. These efforts should be paralleled by public health officials at every level of government and community partners to ensure widespread adherence and specific targeting of ethnic minorities using culturally tailored messaging. The existing disparities in receiving an influenza vaccine should be systematically addressed so that they can be mitigated to ensure equitable care to all U.S. individuals, particularly minority ethnic groups, who are disproportionately affected with COVID-19. Our state level analyses also provide actionable information as to which states need to address these racial/ethnic disparities in receiving an influenza vaccine, which may be also applicable for COVID-19 vaccine once it becomes available. Ensuring that all parts of the U.S. receive COVID-19 vaccine can help achieve herd immunity to prevent future outbreaks.
Our results should be interpreted in the context of important limitations. All our variables are self-reported and may be prone to measurement error. We could not thoroughly evaluate reasons including beliefs, values, and risk perceptions, as to why someone would or would not receive an influenza vaccine. Our definition of ASCVD did not include patients with peripheral arterial disease or transient ischemic attack, and therefore we may have underestimated the true burden of ASCVD. Lastly, we could not evaluate reasons why specific states demonstrated the largest disparities in influenza vaccination rates.
In conclusion, only 50% patients with ASCVD receive influenza vaccine. The receipt of influenza vaccination among individuals with ASCVD is lower among Blacks and Hispanics compared to Whites with significant variation in this disparity across various U.S states and socioeconomic factors. Efforts are needed to mitigate these disparities and regional differences in disparities to avoid a possible future health crisis that disproportionately affects racial minorities.
Funding
We did not require any funding to conduct this study.
Author disclosures
Salim S. Virani
Grant support: Department of Veterans Affairs, World Heart Federation, Tahir and Jooma Family
Honorarium: American College of Cardiology (Associate Editor for Innovations, ACC.org)
Steering Committee: Patient and Provider Assessment of Lipid Management (PALM) registry at Duke Clinical Research Institute (no financial remuneration).
Dr. Khurram Nasir
Supported by Jerold B. Katz Academy of Translational Research
All other authors report no relevant disclosures.
Author contributions
MAR and SSV contributed to the design of the study, analysis of results, and writing of manuscript
UK, AM, JL, KN, MCA, DM, CMB, LAP contributed to the interpretation of results and writing of the manuscript.
Footnotes
All authors had access to the data and were involved in writing the manuscript
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100150.
Appendix. Supplementary materials
References
- 1.Grein J., Ohmagari N., Shin D. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020;382:2327–2336. doi: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polack F.P., Thomas S.J., Kitchin N. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baden L.R., El Sahly H.M., Essink B. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020 doi: 10.1056/NEJMoa2035389. published online Dec 30. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu D., Qiao Y., Brown N.E., Wang J. Racial and ethnic disparities in influenza vaccination among adults with chronic medical conditions vary by age in the United States. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0169679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall L.L., Xu L., Mahmud S.M., Puckrein G.A., Thommes E.W., Chit A. A map of racial and ethnic disparities in influenza vaccine uptake in the medicare fee-for-service program. Adv Ther. 2020;37:2224–2235. doi: 10.1007/s12325-020-01324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis M.M., Taubert K., Benin A.L. Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. J Am Coll Cardiol. 2006;48:1498–1502. doi: 10.1016/j.jacc.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Clerkin K.J., Fried J.A., Raikhelkar J. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 8.Gross C.P., Essien U.R., Pasha S., Gross J.R., Wang S., Nunez-Smith M. 2020. Racial and ethnic disparities in population level COVID-19 mortality. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pierannunzi C., Hu S.S., Balluz L. A systematic review of publications assessing reliability and validity of the behavioral risk factor surveillance system (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13:49. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li C., Balluz L.S., Ford E.S., Okoro C.A., Zhao G., Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the national health and nutrition examination survey, 20. Prev Med (Baltim) 2012;54:381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 11.CDC. Weighting the BRFSS data; 2017. https://www.cdc.gov/brfss/annual_data/2017/pdf/weighting-2017-508.pdf. (accessed April 17, 2019).
- 12.Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11:238–245. doi: 10.2174/1573403X11666141122220003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kopel J., Perisetti A., Roghani A., Aziz M., Gajendran M., Goyal H. Racial and gender-based differences in COVID-19. Front public Heal. 2020;8:418. doi: 10.3389/fpubh.2020.00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Louis-Jean J., Cenat K., Njoku C.V., Angelo J., Sanon D. Coronavirus (COVID-19) and racial disparities: a perspective analysis. J Racial Ethn Heal Disparit. 2020:1–7. doi: 10.1007/s40615-020-00879-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colquhoun A.J., Nicholson K.G., Botha J.L., Raymond N.T. Effectiveness of influenza vaccine in reducing hospital admissions in people with diabetes. Epidemiol Infect. 1997;119:335–341. doi: 10.1017/s095026889700825x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.