Abstract
Background
During the COVID-19 pandemic, South Korea has achieved perfect universal health coverage (UHC)—all Koreans receive UHC regardless of their socioeconomic status. The current study investigated whether socioeconomic disparities remained in COVID-19 health outcomes under UHC.
Methods
This retrospective, observational study included all 7,590 confirmed COVID-19 patients in South Korea up to 15 May 2020. We used the official medical claim database, and socioeconomic status was estimated by insurance type (National Health Insurance Service [NHIS] beneficiaries and Medical Aid [MA] recipients). Type of insurance is a well-known indicator of socioeconomic status. Prevalence (per one million), mortality rate (per one million), and case fatality rate were calculated. To determine the factors associated with case fatality rate, multivariable logistic regressions were performed.
Findings
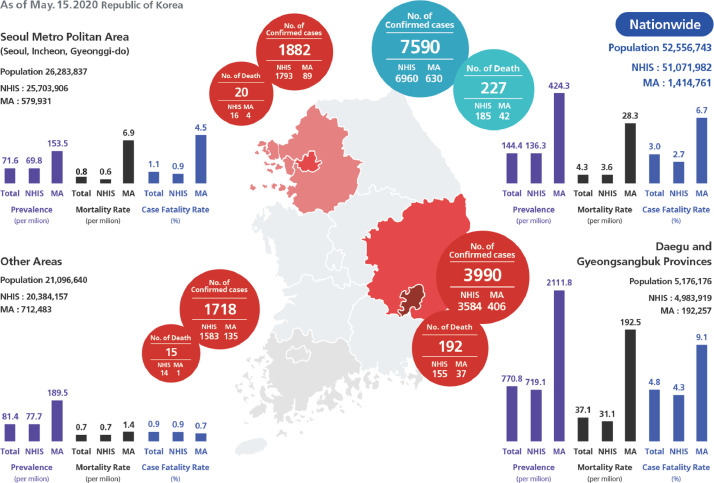
The nationwide prevalence, mortality rate, and case fatality rate of COVID-19 was 144•4, 4•3 and 3•0%, respectively. MA recipients had higher prevalence (424•3 vs 136.3), mortality rate (28•3 vs 3•6), and case fatality rate (6•7 vs 2•7) than NHIS beneficiaries. However, the adjusted analysis showed that the type of insurance was not associated with higher odds of case fatality.
Interpretation
We found socioeconomic disparities in COVID-19 prevalence and fatality despite UHC. However, disparities in fatality were not due to socioeconomic status, but due to the poor underlying health conditions of the people. This result can be explained by a combination of UHC, rapid early testing and treatment, transmission-reducing behaviours, and regional preparedness.
Funding
This research did not receive any funding.
Keywords: SARS-CoV-2, COVID-19, Prevalence, Mortality, Case Fatality, Health disparity
Research in context.
Evidence before this study
In the era of COVID-19, it has been pointed out that there are gaps in the prevalence, level of treatment, and mortality among different ethnicities and socioeconomic classes. Conversely, some argue that, in addition to ethnicity and socioeconomic status, other risk factors, such as old age or underlying illnesses, could also lead to negative outcomes. A study using data from the Worldometer has shown that the case fatality rate of countries with universal health coverage (UHC) during COVID-19 was twice that of countries without UHC (10.5% versus 4.9%, respectively). However, although many countries have UHC, they differ with regard to level of coverage and preparedness of the healthcare system. Therefore, more detailed information on UHC will be helpful in understanding this phenomenon. Another study in Louisiana reported that the Black race was associated with higher risk of hospital admission due to COVID-19, but was not associated with in-hospital mortality. However, the possibility of selection bias for hospital admission existed. During the COVID-19 pandemic, South Korea has achieved a temporary, but perfect universal health coverage model, in terms of the extent of patients and services covered by insurance. In addition, geographic factors could have a large impact on COVID-19 outcomes, because one of the provinces in South Korea experienced a health care system collapse in the early stages of the pandemic. This study was designed to investigate whether there were still socioeconomic disparities in COVID-19 health outcomes in spite of the barrier-free health care condition.
We searched MEDLINE and Google Scholar on 30 July 2020, for articles in English and Korean published in the past 5 years using the terms ‘COVID-19′, ‘disparity’, ‘inequity’ and ‘universal health care’. We found one published study regarding the effect of universal healthcare on COVID-19 outcomes using the data from Worldometer as mentioned above.
Added value of this study
This study is a nationwide study about the effect of universal health coverage on COVID-19 health outcomes. We analysed all COVID-19 confirmed patients in Korea and found that socioeconomic disparities in COVID-19 related health outcomes existed in prevalence, mortality, and case fatality, in spite of the universal health coverage. However, in terms of case fatality, these disparities were not due to socioeconomic status in and of itself, but rather, based on poor underlying health conditions of individuals with lower socioeconomic status. Even in areas where the health care system had collapsed, socioeconomic status was not independently associated with COVID-19 case fatality.
Implications of all the available evidence
Under UHC, people with low socioeconomic status are vulnerable to COVID-19 primarily due to their underlying diseases. Our study also showed the disparities caused by low socioeconomic status itself can be reduced with universal health coverage, even if the health care system collapses. Regarding the risk of COVID-19 infection and death, regional preparedness is one of the key factors affecting outcomes. In response to the pandemic, reducing cost sharing and improving regional preparedness should be considered.
Alt-text: Unlabelled box
As of 25 October 2020, all countries are struggling with the COVID-19 pandemic [1,2], and many people are suffering or dying because of it. As vaccine development is delayed, the pandemic does not seem to be ending in the near future, and various issues induced by the disease have arisen. One of the debates sparked by COVID-19 is that it will exacerbate health disparity. [3], [4], [5] It has been pointed out that there are gaps in prevalence, the level of treatment, and mortality among different ethnicities and socioeconomic classes. [6], [7], [8] The vulnerable are more likely to get infected, less likely to be treated properly, and as a result, more likely to die because of COVID-19. In the United States, it is consistently reported that both incidence and mortality of COVID-19 is higher among Blacks than Whites. [6,8] Some argue that the reason for this imbalance is the population density and public-facing occupations experienced by many Black individuals, making them more susceptible to infection. [6,[9], [10], [11]] Furthermore, the vulnerable are more likely to experience delayed diagnostic testing and insufficient treatment induced by a lack of health insurance, leading to poor prognosis. [12] In addition to ethnicity and socioeconomic status, other risk factors, such as old age or underlying illnesses, could also lead to negative outcomes. [6,8]
During the COVID-19 pandemic, South Korea has achieved a temporary, perfect universal health coverage (UHC) model in terms of the extent of population and services covered by insurance. [13] South Korea has adopted a mandatory universal health care since 1982. Ninety-seven percent of South Koreans are National Health Insurance Service (NHIS) beneficiaries and pay NHIS premiums according to their income levels or property values. The other 3% are Medical Aid (MA) recipients who are unable to pay premiums, so their medical costs are covered by the government through taxes. [14] Both NHIS and MA cover outpatient, inpatient, and prescribed drug costs as well as diagnostic test fees. The out-of-pocket money is normally 20% for NHIS beneficiaries and 0–15% for MA recipients; however, due to the pandemic, the government eliminated all cost sharing associated with health services for COVID-19.
South Korea has followed a ‘Three T Strategy’ (Testing-Tracing-Treatment) to respond to COVID-19. [15] This strategy requires a massive amount of testing in a short time, provides quarantines for confirmed cases in a hospital, and starts treatment as soon as possible. To encourage patients with COVID-19 to be contained and treated, the South Korean government has been waiving the financial burden of patients. All expenses related to COVID-19 is completely free of charge, including testing fees, drugs, hospitalisation, and even some medical services, such as hospital room fee, which are not normally covered by the NHIS or MA. The central government and NHIS paid all costs for medical services of COVID-19. Furthermore, the government reimbursed $450 to $1450 US dollars per month to COVID-19 infected patients according to the length of hospitalisation and number of family members to prevent patients from refusing admission due to the associated fall in income. [16] As a result, the South Korean government has achieved real-world, free of charge, UHC in all streams of COVID-19 response. [17] Theoretically, disparities in health should disappear or be minimised in this health care-related, barrier-free condition.
Although race and ethnicity should be considered as important factors affecting disparities in health outcomes of COVID-19, the main factor affecting disparities in South Korea is socioeconomic status, as South Korea is not a multiracial, multi-ethnic country. Type of insurance (either NHIS beneficiary or MA recipient) is a well-known indicator of socioeconomic status. [18] In addition, geographic factors could have a large impact on COVID-19 outcomes, as evidenced by one of the provinces in South Korea experiencing a health care system collapse in the early stages of the pandemic.
Based on the spread of COVID-19, the regions of South Korea can be divided into three areas. The first one is Daegu and Gyeongsangbuk provinces, which were the epicentres of the COVID-19 outbreak in the early stages of the pandemic. This area had more than 55% of all the COVID-19 patients in South Korea as of May 15, 2020. Many of them are linked to a religious cult (Shincheonji), and therefore difficult to conduct epidemiological investigations on. Furthermore, people who believe in Shincheonji often live in groups; thus, the spread of the disease was very rapid. Although Daegu is a large city with many health care resources, they had little time to prepare, as the disease spread very rapidly. The next region is the Seoul metropolitan area, which has high population density and abundant health care resources. Remaining provinces are classified into the third area, having relatively low population density and below-average health care resources. In contrast to the first area, the other two areas had time to organise systems for quarantine and patient treatment, due to a relatively slow increase of COVID-19 patients in the early stages.
Hence, this study was designed to investigate whether there were still socioeconomic disparities in COVID-19 health outcomes in spite of the barrier-free health care condition in South Korea (i.e. no out-of-pocket expense for diagnosis and treatment related to COVID-19).
1. Methods
1.1. Study design, setting, and population
This retrospective, observational study included all COVID-19 patients who tested positive via reverse transcription polymerase chain reaction (RT-PCR) in South Korea up to 15 May 2020. The Ministry of Health and Welfare as well as the Health Insurance Review and Assessment Service released real-world data of COVID-19 patients to provide supporting evidence for physicians and policymakers. In this dataset, medical utilisation, diagnosis, and treatment of over the past 5 years were collected based on insurance benefit claims. Among them, a total 7590 confirmed COVID-19 patients were included in our analyses. To calculate prevalence, we determined the whole number of NHIS beneficiaries and MA recipients from annual statistics of the NHIS and official statistics of South Korea. There were a total 51,071,982 NHIS beneficiaries and 1484,761 MA recipients. [19]
The Institutional Review Board of the Seoul Metropolitan Government, Seoul National University, Boramae Medical Center (No. 20,200,403/07–2020–12/043) approved this study. The requirement for informed consent was waived, as the study was based on open data sets available to the public.
1.2. Data collection
People who had COVID-19 diagnosis codes (B34.2, B97.2, U18, U18.1, and U07.1) were considered as confirmed COVID-19 patients under the Korean Standard Classification of Diseases and Causes of Death-7 (KCD-7), which is a modified version of the International Classification of Diseases and Related Health Problems, 10th edition (ICD-10). Demographic data (age, sex, insurance type, and regions) were extracted from the dataset. Economic status was estimated using insurance type (i.e. NHIS, MA). Regions were defined as the areas in which the COVID-19 tests were conducted, and categorised into three areas (i.e. Seoul metropolitan area, Daegu and Gyeongsangbuk provinces, and other areas). Chronic medical illnesses, such as hypertension, diabetes mellitus, and dyslipidaemia were defined by the presence of claims for hypertension (I10, I15), diabetes (E10, E118, E119, E13, E149), or hypercholesterolemia (E78) in the past 5 years. Additionally, myocardial infarction (I21, I22), stroke (I60–63), and cancer (C00–97) were also defined by claims of hospitalisation in the past 5 years. Comorbidities were summarised using the Charlson comorbidity index, which is a weighted measure of comorbidity that predicts risk of death within 1 year of hospitalisation. The index includes 17 comorbidity categories, and each condition is assigned a score of 1, 2, 3, or 6. The sum of the index scores is an indicator of disease burden and an estimator of mortality. [20] Treatment outcomes of COVID-19 were classified into three groups (died, hospitalised, and discharged).
1.3. Statistical analysis
We compared characteristics of patients according to region. Baseline characteristics were presented as median with range, mean with standard deviation, or number with percentage. Prevalence (per one million), mortality rate (per one million), and case fatality rate were calculated according to region.
To determine whether socioeconomic status is related to prevalence and case fatality of COVID-19, logistic regressions were performed. The association of socioeconomic status and case fatality were examined with the use of multivariable logistic regressions. Statistical analyses were performed in R software. Statistical significance was defined as two-tailed p-values of < 0•05.
1.4. Role of the funding source
This research did not receive any funding.
2. Results
As of 15 May 2020, a total 7590 COVID-19 patients were confirmed in South Korea. Among them, 3990 (52•6%) lived in Daegu and Gyeongsangbuk provinces, 1882 (24•8%), lived in Seoul metropolitan area, and 1718 (22•6%) lived in other areas. The median age was 47 years, and patients were mostly female (59•2%). Patients in Daegu and Gyeongsangbuk provinces had the highest median age (53 years). Among all 7590 confirmed COVID-19 patients, 6960 (92•7%) were NHIS beneficiaries, and 630 (7•3%) were MA recipients. Daegu and Gyeongsangbuk provinces had a higher percentage of MA recipients (10•2%), and a higher percentage of comorbidities. A total of 227 people (3•0%) died, 1224 (16•1%) were hospitalised, and 6139 (80•9%) were discharged. Daegu and Gyeongsangbuk provinces had a higher number of deaths than any other regions (Table 1).
Table 1.
Characteristics of the patients with confirmed Coronavirus Infectious disease 2019 (Covid-19).*.
| Characteristic | Nationwide (N = 7590) | Daegu and Gyeongsangbuk provinces (N = 3990) | Seoul metropolitan area (N = 1882) | Other areas (N = 1718) |
|---|---|---|---|---|
| Age | ||||
| Median (IQR) - yr | 47•0 (27•0–60•0) |
53•0 (31•0–64•0) |
35•0 (24•0–51•0) |
46•0 (26•0–58•0) |
| Distribution - no. (%) | ||||
| ≤39 yr | 3060 (40•3) | 1298 (32•5) | 1045 (55•5) | 717 (41•7) |
| 40–59 yr | 2509 (33•1) | 1287 (32•3) | 594 (31•6) | 628 (36•6) |
| ≥60 yr | 2021 (26•6) | 1405 (35•2) | 243 (12•9) | 373 (21•7) |
| Sex - no. (%) | ||||
| Female | 4495 (59•2) | 2381 (59•7) | 1101 (58•5) | 1013 (59•0) |
| Male | 3095 (40•8) | 1609 (40•3) | 781 (41•5) | 705 (41•0) |
| Type of insurance - no. (%) | ||||
| National Health Insurance Service Beneficiaries | 6960 (91•7) | 3584 (89•8) | 1793 (95•3) | 1583 (92•1) |
| Medical Aid recipients | 630 (8•3) | 406 (10•2) | 89 (4•7) | 135 (7•9) |
| Comorbidities - no. (%) | ||||
| Hypertension | 1928 (25•4) | 1277 (32•0) | 275 (14•6) | 376 (21•9) |
| Diabetes mellitus | 1776 (23•4) | 1166 (29•2) | 274 (14•6) | 336 (19•6) |
| Dyslipidaemia | 3272 (43•1) | 1980 (49•6) | 597 (31•7) | 695 (40•5) |
| Myocardial infarction | 51 (0•7) | 36 (0•9) | 7 (0•4) | 8 (0•5) |
| Stroke | 280 (3•7) | 235 (5•9) | 19 (1•0) | 26 (1•5) |
| Cancer | 376 (5•0) | 250 (6•3) | 57 (3•0) | 69 (4•0) |
| Median Charlson comorbidity index score (range)† | 1•0 (0•0–2•0) | 1•0 (0•0- 2•0) | 0•0 (0•0- 1•0) | 1•0 (0•0- 1•0) |
| Treatment outcomes - no. (%) | ||||
| Died | 227 (3•0) | 192 (4•8) | 20 (1•1) | 15 (0•9) |
| Hospitalized | 1224 (16•1) | 835 (20•9) | 222 (11•8) | 167 (9•7) |
| Discharged | 6139 (80•9) | 2963 (74•3) | 1640 (87•1) | 1536 (89•4) |
Covid-19 = Coronavirus Infectious Disease 2019.
Percentages may not total 100 because of rounding.
Charlson comorbidity index score, a weighted measure of comorbidity, predict risk of death within 1 year of hospitalization. The index includes 17 comorbidity categories, and each condition is assigned a score of 1, 2, 3, or 6. The sum of the index score is an indicator of disease burden, and an estimator of mortality.
Nationwide prevalence of COVID-19 was 144.4 per one million, mortality rate was 4•3 per one million, and case fatality rate was 3•0%. MA recipients had 3 times higher prevalence (424•3 vs 136•3), 8 times higher mortality rate (28•3 vs 3•6), and 2•5 times higher case fatality rate (6•7 vs 2•7) when compared to NHIS beneficiaries. Daegu and Gyeongsangbuk provinces reported a 5 times higher prevalence (770•8 vs 144•4), 9 times higher mortality rate (37•1 vs 4•3), and 1•5 times higher case fatality rate (4•8 vs 3•0) of COVID-19 when compared to the national mean. In Daegu and Gyeongsangbuk provinces, prevalence of MA recipients was much higher than NHIS beneficiaries (2111•8 vs 719•1); however, the gap was smaller in mortality rate (192•5 vs 31•1) and case fatality rate (9•1 vs 4•3). In the Seoul metropolitan area, prevalence of MA recipients was 2 times higher (153•5 vs 69•8), mortality rate was 11 times higher (0•6 vs 6•9), and case fatality rate was 5 times higher (0•9 vs 4•5) than NHIS beneficiaries (Fig. 1 and Supplementary Table 1 in appendix p 1).
Fig. 1.
Prevalence, Mortality rate, and case fatality rate of Covid-19 in South Korea.
Covid-19 = Coronavirus Infectious Disease 2019. NHIS = National Health Insurance Service beneficiaries. MA =Medical Aid recipients.
* Prevalence (per one million), mortality rate (per one million), and case fatality rate were calculated at the national and regional levels. The whole number of National Health Insurance Service Beneficiaries and Medical Aid recipients was determined from annual statistics of the National Health Insurance Service and official statistics of South Korea. Confirmed cases and number of death were determined by using the official medical database, released from the Ministry of Health and Welfare and Health Insurance Review and Assessment Service in South Korea.
To determine whether socioeconomic status is related to prevalence and case fatality of COVID-19, logistic regressions were performed. Using unadjusted analysis, MA recipients showed higher odds of COVID-19 compared to NHIS beneficiaries (odds ratio [OR], 2•88; 95% confidential interval [CI], 2•66 to 3•13). Daegu and Gyeongsangbuk provinces (OR, 9•52; 95% CI, 8•99 to 10•07) showed higher odds of COVID-19 (Table 2).
Table 2.
Factors associated with prevalence of Covid-19. *.
|
Unadjusted odds ratio* |
||||
|---|---|---|---|---|
| Variable | Nationwide (N = 52,556,743) | Daegu and Gyeongsangbuk provinces (N = 5176,176) | Seoul metropolitan area (N = 26,283,837) | Other areas (N = 21,096,640) |
| Age | ||||
| 40–59 yr vs. ≤39 yr (reference) | 1•14 (1•08–1•20) | 1•41 (1•31–1•53) | 0•81 (0•73–0•89) | 1•17 (1•05–1•30) |
| ≥60 yr vs. ≤39 yr (reference) | 1•44 (1•36–1•53) | 2•11 (1•96–2•28) | 0•59 (0•51–0•67) | 0•99 (0•87–1•12) |
| Sex: female vs. male | 0•69 (0•65–0•72) | 0•68 (0•64–0•73) | 0•71 (0•64–0•77) | 0•71 (0•64–0•78) |
| Type of insurance: National Health Insurance Service Beneficiaries vs Medical Aid recipients |
2•88 (2•66–3•13) | 1•96 (1•77–2•18) | 2•66 (2•15–3•29) | 2•07 (1•74–2•47) |
| Comorbidities† | ||||
| Hypertension: yes vs. no (reference) | 1•11 (1•05–1•16) | 1•69 (1•58–1•81) | 0•56 (0•49–0•64) | 0•88 (0•79–0•99) |
| Diabetes mellitus: yes vs. no (reference) | 3•46 (3•28–3•65) | 4•02 (3•76–4•31) | 2•04 (1•79–2•32) | 2•69 (2•39–3•03) |
| Dyslipidaemia: yes vs. no (reference) | 6•73 (6•44–7•05) | 9•69 (9•11–10•32) | 4•18 (3•80–4•61) | 5•81 (5•27–6•39) |
| Myocardial infarction: yes vs. no (reference) | 1•01 (0•77–1•33) | 1•19 (0•86–1•65) | 0•59 (0•28–1•25) | 0•68 (0•34–1•35) |
| Stroke: yes vs. no (reference) | 2•42 (2•15–2•73) | 4•68 (4•10–5•34) | 0•73 (0•47–1•15) | 0•82 (0•56–1•21) |
| Cancer: yes vs. no (reference) | 1•47 (1•32–1•63) | 2•64 (2•32–3•00) | 0•92 (0•70–1•19) | 1•05 (0•83–1•34) |
| Region | ||||
| Daegu and Gyeongsangbuk province vs Other areas (Reference) | 9•52 (8•99–10•07) | – | – | – |
| Seoul metropolitan area vs Other areas (Reference) | 0•89 (0•83–0•95) | – | – | – |
Covid-19 = Coronavirus Infectious Disease 2019.
Logistic analyses were performed at the national and regional levels.; The whole number of National Health Insurance Service Beneficiaries and Medical Aid recipients was determined from annual statistics of the National Health Insurance Service and official statistics of South Korea.
Charlson comorbidity index score was not included in the analyses due to the lack of information on the whole population.
In terms of case fatality, before adjustment, MA recipients showed higher odds compared to NHIS beneficiaries at the national level (OR, 2•62; 95% CI, 1•85 to 3•70). MA recipients in the Seoul metropolitan area showed the highest odds of case fatality (OR, 5•23; 95% CI, 1•71 to 15•97). In the adjusted analysis, type of insurance was not associated with higher odds of case fatality (OR, 1•43; 95% CI, 0•98 to 2•08; Table 3 and Supplementary Figure 1 in appendix p 2).
Table 3.
Factors associated with case fatality due to Covid-19.
| Case Fatality* |
||||||||
|---|---|---|---|---|---|---|---|---|
|
Unadjusted odds ratio (95% CI) |
Adjusted odds ratio (95% CI)a |
|||||||
| Variable | Nationwide (N = 7590) | Daegu and Gyeongsangbuk provinces (N = 3990) | Seoul metropolitan area (N = 1882) | Other areas (N = 1718) | Nationwide (N = 7590) | Daegu and Gyeongsangbuk provinces (N = 3990) | Seoul metropolitan area (N = 1882) | Other areas (N = 1718) |
| Age | ||||||||
| 40–59 yr vs. ≤39 yr (reference) | 9•81 (2•26–42•66) |
14•26 (1•87–108•54) |
3•53 (0•32–38•97) |
– | 6•25 (1•42–27•62) |
10•20 (1•32–78•61) |
0•68 (0•04–10•98) |
– |
| ≥60 yr vs. ≤39 yr (reference) | 176•36 (43•82–709•73) |
186•95 (26•17–1335•45) |
78•53 (10•40–592•99) |
– | 57•75 (13•85–240•82) |
83•52 (11•39–612•59) |
4•85 (0•38–62•54) |
– |
| Sex: female vs. male | 1•68 (1•29–2•20) |
1•72 (1•29–2•30) |
2•13 (0•87–5•24) |
1•26 (0•45–3•49) |
1•74 (1•31–2•31) |
1•75 (1•28–2•39) |
1•81 (0•63–5•19) |
1•46 (0•51–4•22) |
| Type of insurance: National Health Insurance Service Beneficiaries vs Medical Aid recipients | 2•62 (1•85–3•70) |
2•22 (1•53–3•23) |
5•23 (1•71–15•97) |
0•84 (0•11–6•41) |
1•43 (0•98–2•08) |
1•45 (0•97–2•17) |
3•40 (0•78–14•77) |
0•41 (0•05–3•33) |
| Comorbidities | ||||||||
| Hypertension: yes vs. no (reference) | 12•65 (9•11–17•56) |
8•74 (6•15–12•43) |
56•21 (12•97–243•67) |
14•71 (4•13–52•40) |
2•51 (1•73–3•64) |
2•25 (1•51–3•35) |
11•83 (1•76–79•78) |
2•59 (0•69–9•69) |
| Diabetes mellitus: yes vs. no (reference) | 6•21 (4•71–8•19) |
4•71 (3•48–6•38) |
18•57 (6•69–51•52) |
3•65 (1•32–10•15) |
1•31 (0•94–1•83) |
1•30 (0•91–1•88) |
5•33 (1•29–22•01) |
0•57 (0•17–1•93) |
| Dyslipidaemia: yes vs. no (reference) | 4•10 (3•02–5•55) |
3•12 (2•24–4•34) |
6•60 (2•39–18•24) |
5•97 (1•68–21•25) |
0•67 (0•47–0•97) |
0•67 (0•45–0•99) |
0•17 (0•04–0•80) |
1•48 (0•37–5•98) |
| Myocardial infarction: yes vs. no (reference) | 7•20 (3•46–14•97) |
5•85 (2•63–13•02) |
16•28 (1•87–141•84) |
– | 1•29 (0•59–2•83) |
1•48 (0•63–3•44) |
0•42 (0•03–6•35) |
– |
| Stroke: yes vs. no (reference) | 6•57 (4•58–9•44) |
4•17 (2•83–6•16) |
30•78 (9•20–103•00) |
4•79 (0•61–37•87) |
1•12 (0•75–1•66) |
1•13 (0•74–1•72) |
1•37 (0•29–6•39) |
0•65 (0•07–6•04) |
| Cancer: yes vs. no (reference) | 3•75 (2•58–5•47) |
3•01 (1•99–4•55) |
11•6 (4•06–33•12) |
– | 0•86 (0•52–1•40) |
0•99 (0•58–1•67) |
0•29 (0•04–2•34) |
– |
| Charlson comorbidity index score† | 1•35 (1•30–1•40) |
1•30 (1•24–1•36) |
1•51 (1•35–1•70) |
1•26 (1•09–1•44) |
1•17 (1•10–1•25) |
1•14 (1•07–1•22) |
1•46 (1•18–1•80) |
1•31 (0•91–1•88) |
| Region | ||||||||
| Daegu and Gyeongsangbuk province vs Other areas (Reference) | 5•74 (3•38–9•74) |
– | – | – | 3•28 (1•90–5•65) |
– | – | – |
| Seoul metropolitan area vs Other areas (Reference) | 1•22 (0•62–2•39) |
– | – | – | 1•78 (0•89–3•59) |
– | – | – |
Covid-19 = Coronavirus Infectious Disease 2019.
Unadjusted and multivariable logistic analyses were performed at the national and regional levels. Multivariable logistic regression includes age, sex, type of insurance, hypertension, diabetes mellitus, dyslipidaemia, previous myocardial infarction, stroke, cancer, Charlson comorbidity index, and regions.; All death cases in other areas were age over 40 year without myocardial infarction and cancer, thus odds ratios for those groups were not calculated in the areas.
Charlson comorbidity index score, a weighted measure of comorbidity, predict risk of death within 1 year of hospitalization. The index includes 17 comorbidity categories, and each condition is assigned a score of 1, 2, 3, or 6. The sum of the index score is an indicator of disease burden, and an estimator of mortality.
3. Discussion
In this study, with a nationwide data of confirmed COVID-19 patients, we found that socioeconomic disparities in COVID-19-related health outcomes existed in prevalence, mortality, and case fatality, in spite of the UHC. However, based on the results, disparities in COVID-19 deaths were not due to socioeconomic status per se, but due to the demographic characteristics and poor underlying health conditions of individuals with lower socioeconomic status under the UHC. We believe that this result is explained by a combination of UHC, rapid early testing and treatment, transmission-reducing behaviours, and regional preparedness. Even in areas where the health care system had collapsed, socioeconomic status was not independently associated with COVID-19 case fatality.
Our results are consistent with recent studies that reported that socioeconomically vulnerable individuals have a higher risk of contracting COVID-19. In many countries, ethnic minority groups have exhibited a higher risk of COVID-19 infection. [4,11] There are two possible reasons for this phenomenon. First, vulnerable people often have more underlying comorbidities; second, they are more exposed to hazardous environments, such as densely populated neighbourhoods, occupations, and housing conditions. [11] Several studies have attempted to determine if health disparities exist in COVID-19 outcomes, and if so, which factors are associated with these disparities. One study in Louisiana reported that being Black was associated with higher risk of hospital admission due to COVID-19, but was not associated with in-hospital mortality. [8] However, because of the possibility of selection bias, it is doubtful whether these results were accurate. The vulnerable had less chance to be tested and treated due to out-of-pocket cost, and for that reason, those who were hospitalised may have been less vulnerable, resulting in a better prognosis. [12] Since we included all patients in South Korea regardless of socioeconomic status, the results of our analyses are closer to reality. This study confirms previously reported risk factors of COVID-19 infection and death, such as age and other comorbidities, [8,21,22] but also showed different results in the association between socioeconomic status and COVID-19. In our study, socioeconomic status was not an independent risk factor of COVID-19 infection and death. One study showed that during the period of COVID-19, the case fatality rate of countries with UHC was twice that of countries without it (10.5% versus 4.9%, respectively), [23] which may be attributed to a mixture of the effects of several types of UHC. However, although many countries have UHC, they differ with regard to level of coverage and preparedness of the healthcare system. Nevertheless, we assumed that there are three additional reasons for our result. First, with the ‘Three T strategy’ employed by South Korea, early detection and treatment were possible. This strategy lowered basic reproductive number (R0) effectively, starting quarantine and treatment earlier, ultimately lowering mortality. [15,24] Having all COVID-19 diagnoses and treatment aspects free of charge, regardless of income level, effectively supported this strategy, as many previous studies have reported that reducing out-of-pocket costs is an effective intervention for achieving better health outcomes. [12,25,26]
Second, transmission-reducing behaviours, such as wearing a mask, washing hands, and social distancing became routine in South Korea, thereby lowering the incidence rate. [27] Finally, in many regions, spare beds and community treatment centres were prepared to prevent medical system collapse. [28] Without these efforts, socioeconomic status would have affected the incidence, mortality, and case fatality in a manner similar to other reports. [4,11]
Geographic location was also a risk factor of COVID-19 infection and death. In our study, Daegu and Gyeongsangbuk provinces, which experienced a rapid spread of COVID-19 and collapse in the health care system showed an extremely high prevalence and mortality rate. In these areas, COVID-19 spread rapidly because the initial path of transmission was not identified. Additionally, there were mass infections in nursing homes and nursing hospitals; therefore, many patients with underlying comorbidities were infected. [29] Unlike Daegu and Gyeongsangbuk provinces, the Seoul metropolitan area had a slow spread of COVID-19, so there was time to prepare. A rapid response team to prevent community transmission was organised, [15] and hospital beds were secured in case of outbreak.
The current study had several strengths and limitations. Its first major strength is the use of the nationally representative data set, with information on previous medical use for all COVID-19 patients in South Korea. Second, we used data from South Korea, which has essentially become a setting for exploration regarding regional preparedness and the effect of UHC.
Meanwhile, the first limitation of our study is the possibility of inaccurate claim data. However, many studies have shown that claim data are accurate for many diseases. [30] Additionally, to minimise overestimation of comorbidities, myocardial infarction, stroke, and cancer were defined only when hospitalised. Second, since our study used a retrospective design, the sample size or analysis method was not determined before data collection. To address this issue, we did not conduct artificial manipulations, such as cutting data or restricting the period. Third, this study is a cross-sectional study; therefore, we cannot prove causality. As long-term data accumulate in the future, longitudinal analyses will be possible. In this study, we could not adjust for multiple testing, which remained a methodological limitation. Fourth, because of the limitations of the analysis, it was not possible to report the standardised rates for each region. Non-standardised rates are considerably more difficult to compare across regions. Although we have reported stratified results by age, some problems still remain. Finally, laboratory results were not gathered in the dataset; therefore, clinical characteristics were not included in the analyses.
In summary, people with low socioeconomic status have higher risk of COVID-19 fatality primarily due to their underlying diseases under UHC. Our study also showed the disparities caused by low socioeconomic status itself can be reduced with UHC, even if the health care system collapses. Regarding the risk of COVID-19 infection and death, rapid early testing and treatment, transmission-reducing behaviours, and regional preparedness are other key factors associated with positive outcomes. In response to the pandemic, reducing cost sharing, timely testing and treatment, transmission-reducing behaviours, and improving regional preparedness should be considered.
4. Contributors
Jin Yong Lee devised the original study concept and design; Hyejin Lee and Jae-ryun Lee participated in the acquisition of data and had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. Jae-ryun Lee performed statistical analyses and interpreted the data; Jin Yong Lee and Hyemin Jung provided intellectual contributions and critically revised the manuscript; Hyejin Lee and Hyemin Jung wrote the manuscript, which all authors read, edited, and approved prior to submission. Additionally, all authors agreed to accept equal responsibility for the accuracy of the content of the paper.
Declaration of Interests
The authors declare that there are no conflicts of interests.
Acknowledgments
Acknowledgments
The authors would like to acknowledge health care professionals dedicated to treating COVID-19 patients in South Korea, the Ministry of Health & Welfare, and the Health Insurance Review & Assessment Service of South Korea for sharing invaluable national health insurance claims data in a prompt manner.
Data sharing statement
All data used in this study are publicly available. However, the data will be made publicly available on the Health Insurance Review and Assessment Service (https://covid19data.hira.or.kr/).
The corresponding author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported. No important aspects of the study have been omitted, and all discrepancies from the study have been explained.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2020.100088.
Appendix. Supplementary materials
References
- 1.World Health Organization . 2020. Declared COVID-19 as pandemic. [Google Scholar]
- 2.Gates B. Responding to Covid-19 - a once-in-a-century pandemic? N Engl J Med. 2020;382(18):1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 3.Gray D.M., 2nd, Anyane-Yeboa A., Balzora S., Issaka R.B., May F.P. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat Rev Gastroenterol Hepatol. 2020;17:520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel P., Hiam L., Sowemimo A., Devakumar D., McKee M. Ethnicity and covid-19. BMJ (Clin Res Ed) 2020;369:m2282. doi: 10.1136/bmj.m2282. [DOI] [PubMed] [Google Scholar]
- 5.Wang Z., Tang K. Combating COVID-19: health equity matters. Nat Med. 2020;26(4):458. doi: 10.1038/s41591-020-0823-6. [DOI] [PubMed] [Google Scholar]
- 6.Webb Hooper M., Napoles A.M., Perez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chowkwanyun M., Reed A.L., Jr. Racial health disparities and Covid-19 - caution and context. N Engl J Med. 2020;383(3):199–201. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 8.Price-Haywood E.G., Burton J., Fort D., Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah M., Sachdeva M., Dodiuk-Gad R.P. COVID-19 and racial disparities. J Am Acad Dermatol. 2020;83(1):e35. doi: 10.1016/j.jaad.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yancy C.W. COVID-19 and African Americans. JAMAJAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 11.Av Dorn, Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet North Am Ed. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King J.S. Covid-19 and the need for health care reform. N Engl J Med. 2020;382(26):e104. doi: 10.1056/NEJMp2000821. [DOI] [PubMed] [Google Scholar]
- 13.Were L.P.O. Informality and health: universal health coverage in the era of SDGs. Lancet Glob Health. 2018;6(1):e22–ee3. doi: 10.1016/S2214-109X(17)30458-8. [DOI] [PubMed] [Google Scholar]
- 14.National Health Insurance Service . National Health Insurance Service; 2019. 2018 Medical Aid Statistics. [Google Scholar]
- 15.Na B.J., Park Y., Huh I.S., Kang C.R., Lee J., Lee J.Y. Seventy-two hours, targeting time from first COVID-19 symptom onset to hospitalization. J Korean Med Sci. 2020;35(20):e192. doi: 10.3346/jkms.2020.35.e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korea Center for Disease Control. 2020 (http://ncov.mohw.go.kr/supportPolicyBoardList.do)
- 17.World Health Organization . Health systems financing: the path to universal coverage. World Health Organization; 2010. World health report 2010. Geneva. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim D.W., Byeon K.H., Kim J., Cho K.D., Lee N. The correlation of comorbidities on the mortality in patients with COVID-19: an observational study based on the Korean national health insurance big data. J Korean Med Sci. 2020;35(26):e243. doi: 10.3346/jkms.2020.35.e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Korea National Health Insurance Service . Korea National Health Insurance Service; 2019. 15th National health insurance statistical yearbook; p. 1. [Google Scholar]
- 20.Sundararajan V., Henderson T., Perry C., Muggivan A., Quan H., Ghali W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet North Am Ed. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dongarwar D., Salihu H.M. COVID-19 Pandemic: marked global disparities in fatalities according to geographic location and universal health care. Int J MCH AIDS. 2020;9(2):213–216. doi: 10.21106/ijma.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kang C.R., Lee J.Y., Park Y. Coronavirus disease exposure and spread from Nightclubs, South Korea. Emerg Infect Dis. 2020;26(10):2499–2501. doi: 10.3201/eid2610.202573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woolhandler S., Himmelstein D.U. The relationship of health insurance and mortality: is lack of insurance deadly? Ann Intern Med. 2017;167(6) doi: 10.7326/M17-1403. [DOI] [PubMed] [Google Scholar]
- 26.Griffith K., Evans L., Bor J. The affordable care act reduced socioeconomic disparities in health care access. Health Aff. 2017;36(8):1503–1510. doi: 10.1377/hlthaff.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jang W.M., Jang D.H., Lee J.Y. Social distancing and transmission-reducing practices during the 2019 Coronavirus disease and 2015 Middle East respiratory syndrome Coronavirus outbreaks in Korea. J Korean Med Sci. 2020;35(23):e220. doi: 10.3346/jkms.2020.35.e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kang E., Lee S.Y., Jung H., Kim M.S., Cho B., Kim Y.S. Operating protocols of a community treatment center for isolation of patients with Coronavirus disease, South Korea. Emerg Infect Dis. 2020;26(10):2329–2337. doi: 10.3201/eid2610.201460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Korea Center for Disease Control Ministry of Health and Welfare . Korea Center for Disease Control Ministry of Health and Welfare; 2020. Daily briefing of COVID-19 infection in Korea. [Google Scholar]
- 30.Sathiakumar N., Delzell E., Yun H. Accuracy of medicare claim-based algorithm to detect breast, prostate, or lung cancer bone metastases. Med Care. 2017;55(12):e144–e1e9. doi: 10.1097/MLR.0000000000000539. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.