Abstract
On January 2020, WHO confirmed the epidemic outbreak of SARS-CoV-2 as a Health Emergency of International Concern. The aim of this meta-meta-analysis is quantifying meta-analytic findings on the association of cardiovascular disease (CVD) comorbidities and COVID-19 severity. Findings suggest that chances of getting severe COVID-19 disease in patients with CVD is greater than those without CVD. Also, prevalence of CVD in patents with COVID-19 is 0.08 (95% CI = 0.07–0.08). The OR as 3.44 indicates that the odds of getting severe COVID-19 is more than 3 times higher in those with CVD. Also, prevalence of hypertension in patient with COVID-19 is 0.27 (95%CI = 0.27–0.28) and the OR as 2.68 indicates that the odds of getting severe COVID-19 in cases with high blood pressure is more than 2.5 times higher than those without hypertension. It is rational to suppose that persons with coronary artery disease are prone to severe viral infection thereby, guideline-directed diagnosis and medical therapy is vital in CVD patients.
Keywords: SARS-CoV-2, COVID-19, Clinical characteristics, Heart damage, Prevalent comorbidity, Underlying disease, Cardiovascular, Hypertension, Meta-meta-analysis
Abbreviations: SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COVID-19, Coronavirus disease-2019; ACS, Acute coronary syndrome; CHD, Coronary heart disease; CVD, Cardiovascular disease; ACE2, angiotensin converting enzyme 2; NHC, National Health Commission of China; ARDS, Acute respiratory distress syndrome; ICU, Intensive care unit
Graphical abstract
1. Introduction
Coronavirus disease-2019 (COVID-19) is a global health emergency caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It has already developed into a pandemic spreading rapidly around the globe (Organization, 2020). SARS-CoV-2 appears to infect the host cells through angiotensin converting enzyme 2 (ACE2) receptors, which are widely expressed not only in epithelial cells of airways, but also in heart and blood vessels. Thus, ACE2-related biological pathways may play a role in heart damage associated with COVID-19. While the clinical presentations of SARS-CoV-2 infection are known by the resulting respiratory symptoms, increasingly studies reported that some patients have developed cardiovascular disorders (Zheng et al., 2020a). Importantly, based on different reports in several countries, people with underlying CVDs present with a substantially greater risk of death from the SARS-COV-2, So, extra care against infection is being urged (Huang et al., 2020). Another phenomenon that plays a key role in COVID-19 is the imbalanced cytokine storm response of type 1/type 2 T helper cells, resulting in fever and multiple organ dysfunction and cardiac injury (Zheng et al., 2020a). Immune system activation may cause plaque vulnerability, contributing to the progress of acute coronary events. The common laboratory abnormalities show that SARS-CoV-2 infection may be related to cellular immunodeficiency, activation of coagulation cascade, liver and kidney damage and myocardial injury (Cui et al., 2020). Due to the poor prognosis, patients with existing cardiovascular disease (CVD) are prone to the adverse effects of COVID-19 infection. According to the National Health Commission of China (NHC), among the confirmed cases of the illness, some patients visited a doctor's office for CV symptoms, palpitations and chest discomfort and tightness rather than respiratory symptoms and signs (high fever and cough), although were later identified and diagnosed with COVID-19). The Prevalence of myocardial damage and its intensity is high in severely ill patients with COVID-19, leading to a higher possibility of in-hospital mortality (Cui et al., 2020). The patients with concomitant heart disease are hypothetically at the greatest risk of contracting the COVID-19 infection. The acute inflammatory response induced by the infection may aggravate cardiac function. We have performed this analysis, using data based searching to identify the proportion of the disease severity and comorbidities such as cardiovascular disorders.
1.1. Cellular mechanisms and physiological consequences
COVID-19 appears to promote the development of CV disorders, such as acute coronary syndrome (ACS), myocardial injury, arrhythmias, and venous thromboembolism. Systemic inflammation related to COVID-19 has been suggested to accelerate the development of subclinical disorders or even lead to de novo CV damage. ACE2, a key part of the renin–angiotensin–aldosterone system (RAAS), which is thought to facilitate cellular coronaviruses entry (Ziegler et al., 2020), leading to myocardial damage, endothelial and microvascular dysfunction, plaque vulnerability, and MI (Guzik et al., 2020). The possible mechanisms of myocardial damage caused by COVID-19 infection are as follows: (1) direct injury: viral infection can directly cause damage to myocardial cells (Knowlton, 2020); (2) immune injury: The resulting over-activation of the immune system produces an extreme immune response and releases a large amount of cytokines (Java et al., 2020; Wiersinga et al., 2020). In addition, the promotion of immune system dysregulation occurs during the distribution of blood pressure, suggesting another mechanism connecting arterial hypertension and COVID-19. CD8+ T cell dysfunction observed in hypertensive patients (Youn et al., 2013), results in insufficient combating viral infections and might be associated with excess cytokine production, augmenting the risk of complications. Effective control of hypertension by medication use can moderately reverse the dysregulation of the immune response in high blood pressure. Arterial hypertension can be considered as the main predictor of disease severity or a causal factor of late deterioration in the disease course, which is characterized by acute respiratory distress syndrome (ARDS) and systemic inflammatory response and/or multiple organ failure syndromes (Lippi et al., 2020). Generally, ACE2 overexpression in failing hearts, suggests an acceptable explanation for higher infection and more mortality in patients with heart failure (Liu et al., 2020b). Also, cellular entry of coronaviruses through ACE2 has associations in vascular instability in infected patients who have pre-existing hypertensive disorders (Guzik et al., 2020).
2. Materials and methods
2.1. Search strategy
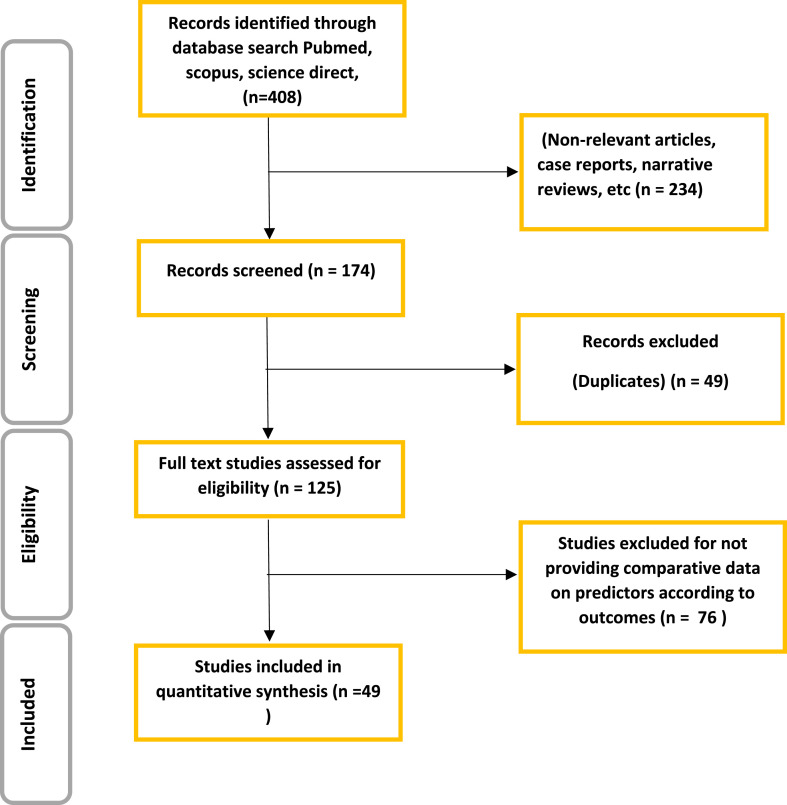
A total of 408 articles were retrieved using the electronic databases: PubMed, SCOPUS and Science direct and the search terms: 2019 novel coronavirus and COVID-19″ and “Cardiovascular Diseases” and “comorbidities, meta-analysis, clinical characteristics and associated MeSH terms. The meta-meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement (PRISMA). A total of 49 articles were finally included in this analysis.
2.2. Statistical analysis
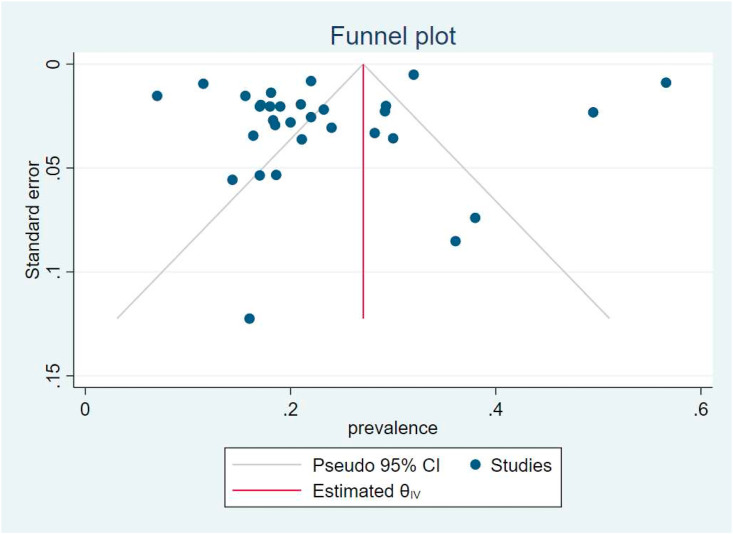
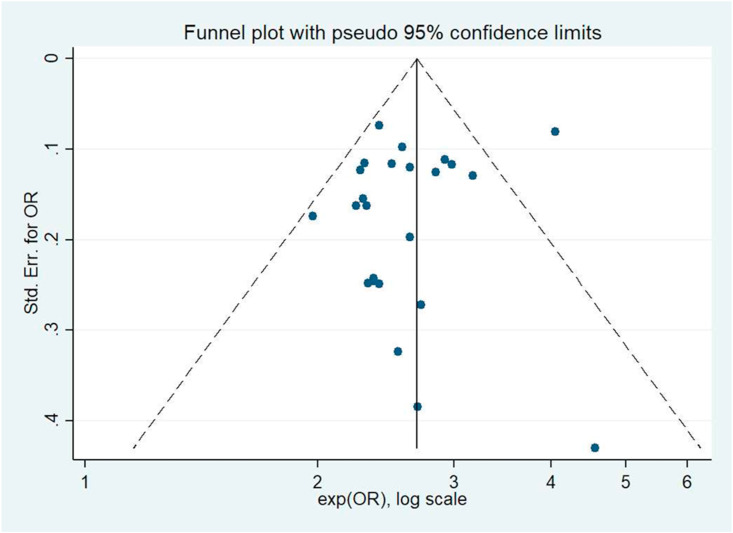
The meta-analysis of single arm studies was performed by statistical software Stata version 14.0 and Open Meta-analyst. We unify all units of variables, and categorized variables are expressed as percentages, and continuous variables are expressed as Means ± SDs. The combined prevalence and 95% CI were determined by a random-effects model.A Meta-analysis of Odds Ratio was performed on the natural logarithm scale and then returned to its original scale. Studies were pooled with fixed-effects meta-analytic models in order to combine odds ratios (OR) and prevalences and their 95% confidence intervals (CIs). Heterogeneity of effect size across trials was established based on I2 more than 0.50. However, as effect sizes were extracted from meta-analysis papers, there was not sufficient information to deal with heterogeneity through subgroup analysis or meta-regression. So in the case of high I2, the results should be interpreted with caution. Publication bias was assessed using funnel plots, as well as, Egger's linear regression test and Begg's rank correlation test. When publication bias was identified, a nonparametric trim and fill method was performed to adjust the publication bias.
3. Results
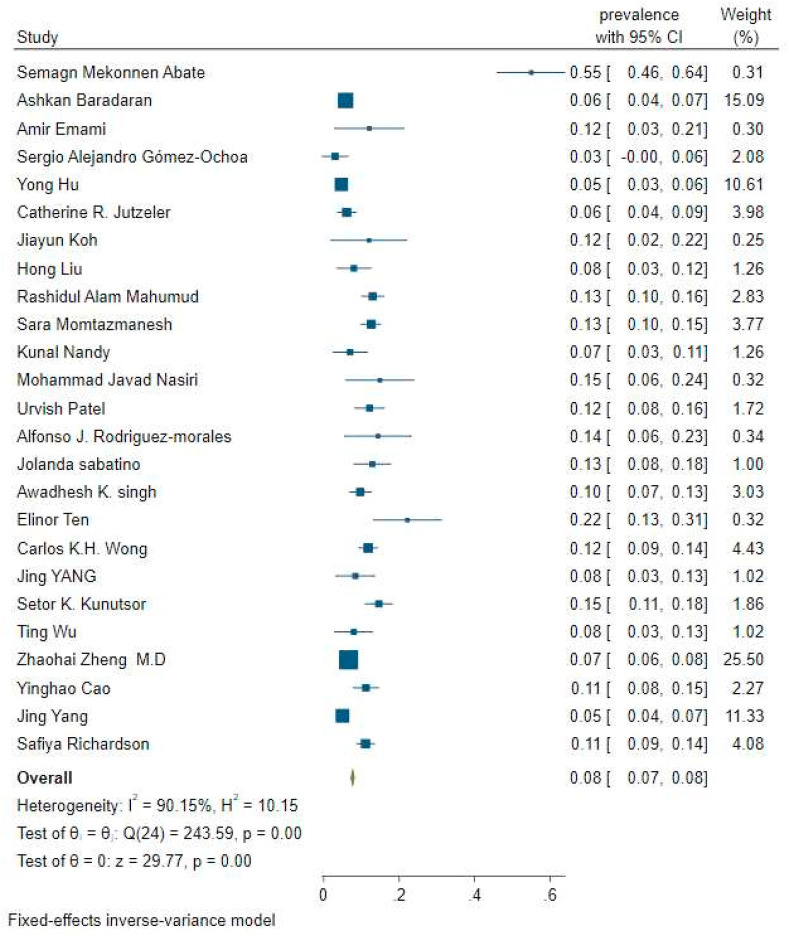
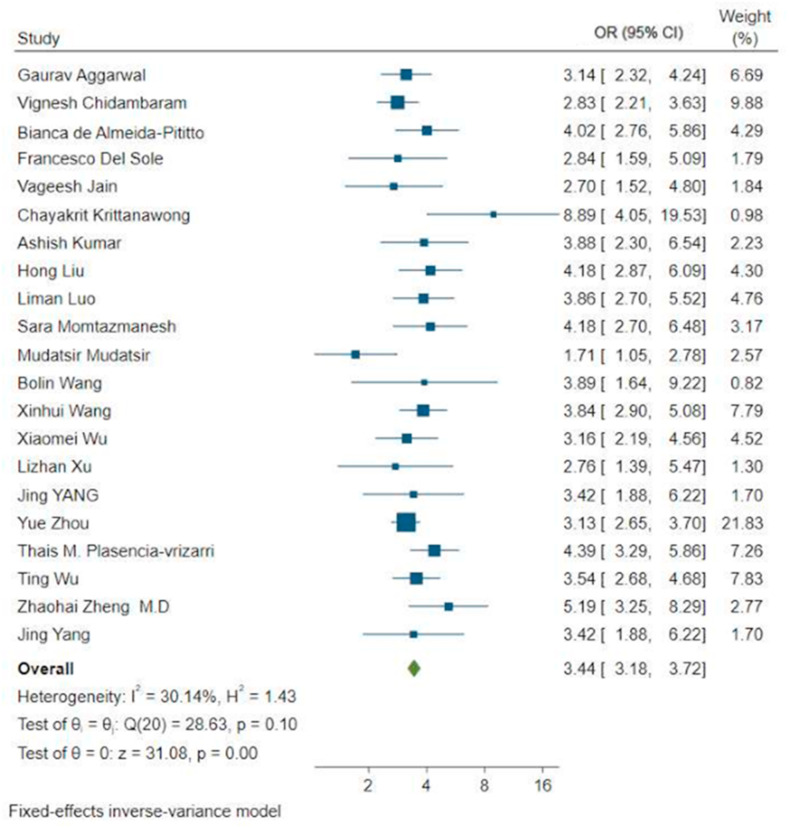
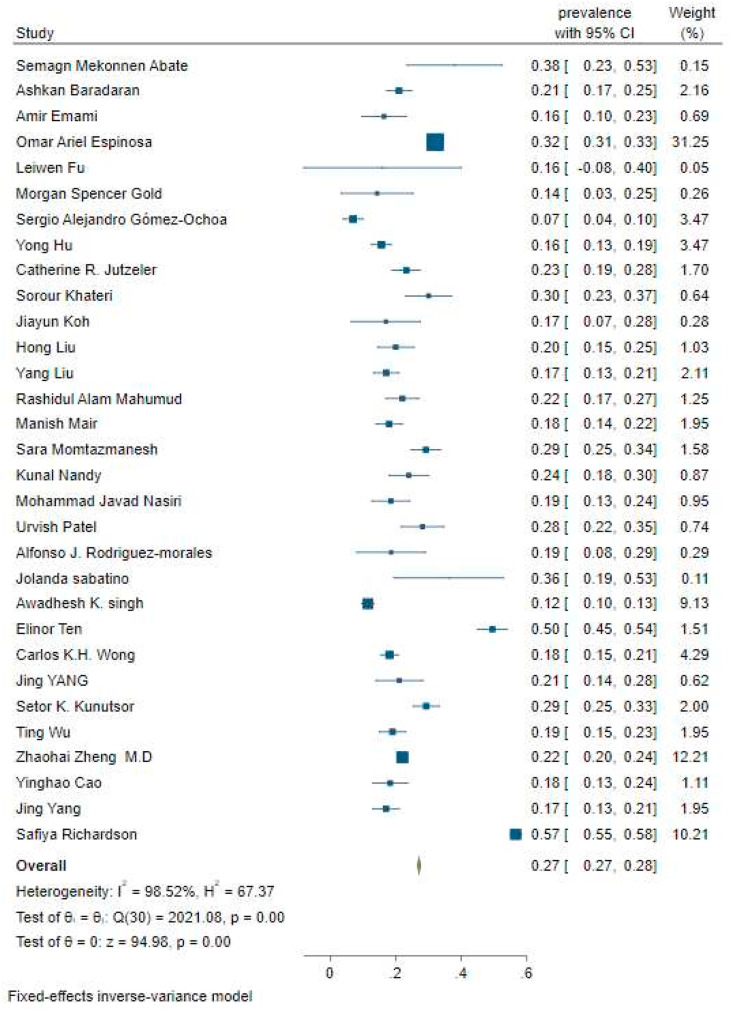
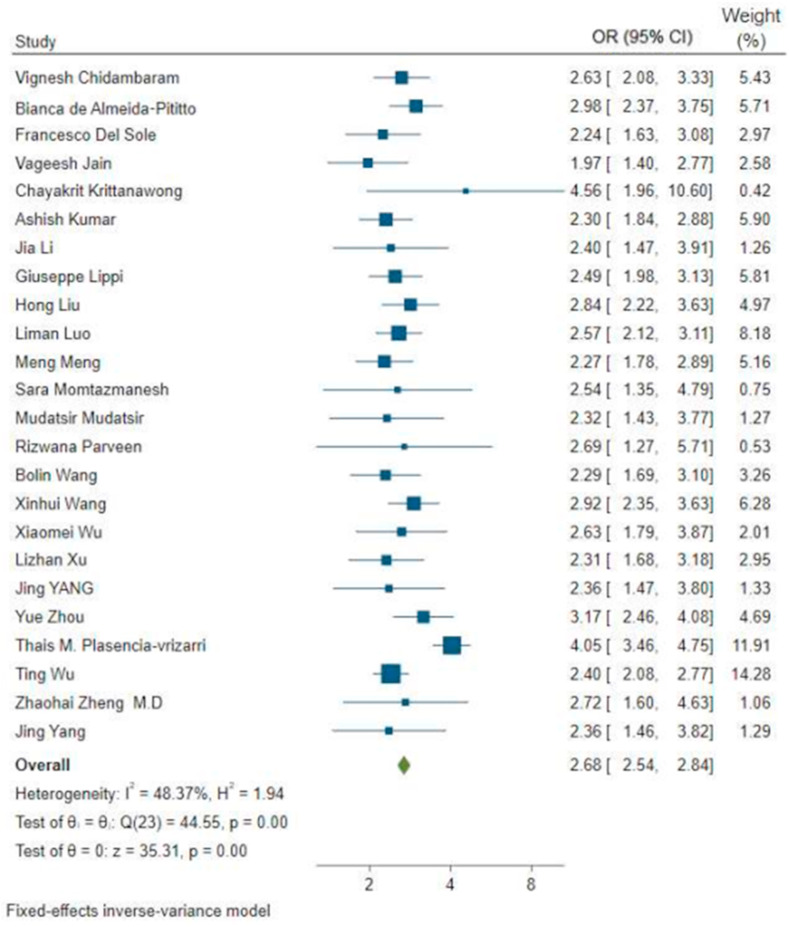
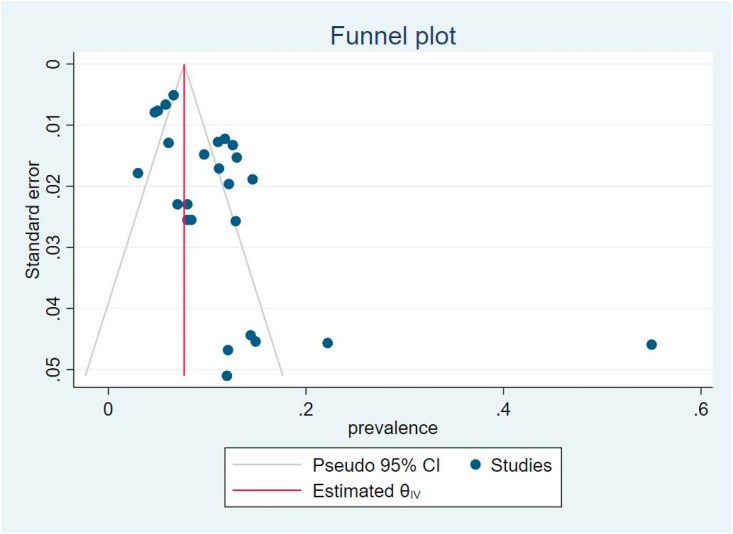
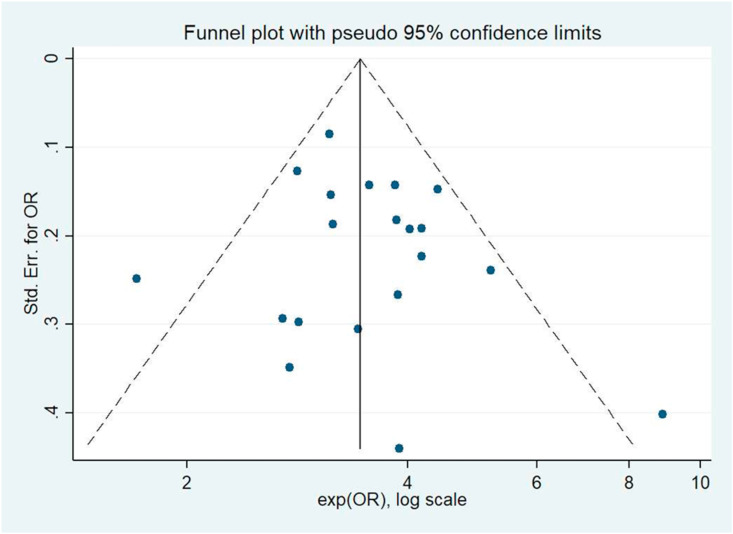
A comprehensive literature search was performed using PubMed, Scopus, and Science Direct from April until December 2020. This meta-meta-analysis included 45 meta-analyses, containing patients with novel coronavirus disease (Table 1, Table 2, Table 3, Table 4 ). The flow chart of articles was illustrated in Fig. 1 . Through this meta-analysis, we found that among all the clinical characteristics of patients with SARS-CoV-2, the prevalence of CVD was 0.08 (Fig. 2 ), OR as 3.44 in severe cases of COVID-19 with CVD in compared to those without CVD (Fig. 4), prevalence of hypertension was 0.27 (Fig. 6) and OR as 2.68 indicates the greater likelihoods of getting severe COVID-19 in hypertensive cases than patients without hypertension (Fig. 8). In addition, Egger's test and Begg's test yielded similar results with funnel plots including: The prevalence of CVD (Egger P = 0.000; Begg P = 0.147) (Fig. 3 ), OR for CVD (Egger P = 0.269; Begg P = 0.628) (Fig. 5 ), prevalence of hypertension (Egger P = 0.000; Begg P = 0.009) (Fig. 7 ), and OR of hypertension (Egger P = 0.133; Begg P = 0.385) (Fig. 9 ). After applying the trim and fill approach the estimated prevalence of CVD didn't significantly change but the estimated prevalence of hypertension increased from 0.27 (0.27–0.28) to 0.323 (0.318–0.328).
Table 1.
Prevalence of CVD.
| Authors | Sample Size | Prevalence (95%CI) |
|---|---|---|
| Semagn Mekonnen Abate (Abate et al., 2020) | 37 studies (24983 patients) | 0.55 (0.46,0.64) |
| Ashkan Baradaran (Baradaran et al., 2020) | 33 studies (9249 patients) | 0.05 (0.04,0.07) |
| Amir Emami (Emami et al., 2020) | 10 studies (76993 patients) | 0.12 (0.04,0.22) |
| Sergio Alejandro Gómez-Ochoa (Gómez-Ochoa et al., 2021) | 97 studies (230,398 patients) | 0.03 (0.01,0.08) |
| Yong Hu (Hu et al., 2020) | 21 studies (47344 patients) | 0.04 (0.031,0.06) |
| Catherine R. Jutzeler (Jutzeler et al., 2020)rowhead | 148 studies (12′149 patients) | 0.06 (0.04,0.09) |
| Jiayun Koh (Koh et al., 2020) | 29 studies (533 patients) | 0.12 (0.03,0.23) |
| Hong Liu (Liu et al., 2020a) | 24studies (10948 patients) | 0.08 (0.03,0.12) |
| Rashidul Alam Mahumud (Mahumud et al., 2020) | 23studies (202,005 patients) | 0.13 (0.1,0.16) |
| Sara Momtazmanesh (Momtazmanesh et al., 2020) | 54 studies | 0.12 (0.1,0.15) |
| Kunal Nandy (Nandy et al., 2020) | 16 studies (3994 patients) | 0.07 (0.04,0.13) |
| Mohammad Javad Nasiri (Nasiri et al., 2020) | 34studies (5057 patients) | 0.14 (0.06,0.23) |
| Urvish Patel (Patel et al., 2020) | 29studies (12,258 patients) | 0.12 (0.08,0.16) |
| Alfonso J. Rodriguez-morales (Rodriguez-Morales et al., 2020) | 19 studies | 0.14 (0.05,0.23) |
| Jolanda sabatino (Sabatino et al., 2020) | 21 studies (77317 patients) | 0.12 (0.08,0.18) |
| Awadhesh K. singh (Awadhesh et al.) | 18studies (558 patients) | 0.09 (0.06,0.12) |
| Elinor Ten (Tan et al., 2020) | 45studies (16,561 patients) | 0.22 (0.13,0.31) |
| Carlos K.H. Wong (Wong et al., 2020) | 76 studies (11,028 patients) | 0.11 (0.09,0.14) |
| Jing YANG (Yang et al., 2020a) | 7studies (1576 patients) | 0.08 (0.03,0.13) |
| Setor K. Kunutsor (Kunutsor and Laukkanen, 2020) | 17 studies (5815 patients) | 0.14 (0.11,0.18) |
| Ting Wu (Wu et al., 2020a) | 73studies (171,108 patients) | 0.08 (0.04,0.14) |
| Zhaohai Zheng M.D (Zheng et al., 2020b) | 13studies (3027 patients) | 0.06 (0.05,0.07) |
| Yinghao Cao (Cao et al., 2020) | 31studies (46,959 patients) | 0.11 (0.07,0.14) |
| Jing Yang (Yang et al., 2020b) | 8 studies (46248 patients) | 0.05 (0.04,0.07) |
| Safiya Richardson (Richardson et al., 2020) | 32studies (310585) | 0.11 (0.08,0.13) |
Table 2.
Odd ratio of CVD.
| Authors | Sample Size | Odd ratio (95%CI) |
|---|---|---|
| Gaurav Aggarwal(Aggarwal et al., 2020) | 18studies (4858 patients) | 1.14 (0.84,1.44) |
| Vignesh Chidambaram(Chidambaram et al., 2020) | 109 studies | 1.04 (0.79,1.28) |
| Bianca de Almeida-Pititto(de Almeida-Pititto et al., 2020) | 40 studies (18.012 patients) | 1.39 (1.01,1.76) |
| Francesco Del Sole(Del Sole et al., 2020) | 12studies (2794 patients) | 1.04 (0.46,1.62) |
| Vageesh Jain(Jain and Yuan, 2020) | 7studies (1813 patients) | 0.99 (0.41,1.56) |
| Chayakrit Krittanawong(Krittanawong et al., 2020) | 13studies (49,076 patients) | 2.18 (1.39,2.97) |
| Ashish Kumar(Kumar et al., 2020) | 58studies (6892 patients) | 1.35 (0.83,1.87) |
| Hong Liu(Liu et al., 2020a) | 24studies (10948 patients) | 1.43 (1.05,1.8) |
| Liman Luo(Luo et al., 2020) | 124 studies | 1.35 (0.99,1.7) |
| Sara Momtazmanesh(Momtazmanesh et al., 2020) | 54 studies | 1.43 (0.99,1.86) |
| Mudatsir Mudatsir(Mudatsir et al., 2020) | 19studies (3578 patients) | 0.53 (0.04,1.02) |
| Bolin Wang(Wang et al., 2020a) | 6studies (1558 patients) | 1.35 (0.49,2.22) |
| Xinhui Wang(Wang et al., 2020b) | 34 studies | 1.34 (1.06,1.62) |
| Xiaomei Wu(Wu et al., 2020b) | 41 studies (5064 patients) | 1.15 (0.78,1.51) |
| Lizhan Xu(Xu et al., 2020) | 20 studies (4062 patients) | 1.01 (0.32,1.69) |
| Jing YANG (Yang et al., 2020b) | 7studies (1576 patients) | 1.22 (0.63,1.82) |
| Yue Zhou(Zhou et al., 2020) | 34studies (16110 patients) | 1.14 (0.97,1.3) |
| Thais M. Plasencia-vrizarri(Plasencia-Urizarri et al., 2020) | 13 studies (99,817 patients) | 1.47 (1.19,1.76) |
| Ting Wu(Wu et al., 2020a) | 73studies (171,108 patients) | 1.26 (0.98,1.54) |
| Zhaohai Zheng M.D(Zheng et al., 2020b) | 13studies (3027 patients) | 1.64 (1.17,2.11) |
| Jing Yang (Yang et al., 2020a) | 8 studies (46248 patients) | 1.22 (0.63,1.82) |
Table 3.
Prevalence of hypertension.
| Author | Sample Size | Prevalence (95%CI) |
|---|---|---|
| Semagn Mekonnen Abate(Abate et al., 2020) | 37 studies (24983 patients) | 0.38 (0.26,0.55) |
| Ashkan Baradaran(Baradaran et al., 2020) | 33 studies (9249 patients) | 0.21 (0.17,0.24) |
| Amir Emami(Emami et al., 2020) | 10 studies (76993 patients) | 0.16 (0.1,0.23) |
| Omar Ariel Espinosa(Espinosa et al., 2020) | 42 studies (98714 patients) | 0.32 (0.31,0.33) |
| Leiwen Fu(Fu et al., 2020) | 43 studies (3600 patients) | 0.16 (0,0.48) |
| Morgan Spencer Gold(Gold et al., 2020) | 33 studies (29,096 patients) | 0.14 (0.06,0.28) |
| Sergio Alejandro Gómez-Ochoa(Gómez-Ochoa et al., 2021) | 97 studies (230,398 patients) | 0.07 (0.04,0.1) |
| Yong Hu(Hu et al., 2020) | 21 studies (47344 patients) | 0.15 (0.12,0.18) |
| Catherine R. Jutzeler(Jutzeler et al., 2020) | 148 studies (12′149 patients) | 0.23 (0.19,0.27) |
| Sorour Khateri(Khateri et al., 2020) | 12 studies (2393 patients) | 0.3 (0.23,0.37) |
| Jiayun Koh(Koh et al., 2020) | 29 studies (533 patients) | 0.17 (0.07,0.28) |
| Hong Liu(Liu et al., 2020a) | 24 studies (10948 patients) | 0.2 (0.15,0.26) |
| Yang Liu(Liu et al., 2020c) | 17 studies (3268 patients) | 0.17 (0.13,0.2) |
| Rashidul Alam Mahumud(Mahumud et al., 2020) | 23studies (202,005 patients) | 0.22 (0.17,0.27) |
| Manish Mair(Mair et al., 2020) | 67 studies (8302 patients) | 0.18 (0.14,0.22) |
| Sara Momtazmanesh(Momtazmanesh et al., 2020) | 54 studies | 0.29 (0.24,0.33) |
| Kunal Nandy(Nandy et al., 2020) | 16 studies (3994 patients) | 0.24 (0.18,0.3) |
| Mohammad Javad Nasiri(Nasiri et al., 2020) | 34 studies (5057 patients) | 0.18 (0.12,0.24) |
| Urvish Patel(Patel et al., 2020) | 29studies (12,258 patients) | 0.28 (0.22,0.35) |
| Alfonso J. Rodriguez-morales(Rodriguez-Morales et al., 2020). | 19 studies | 0.18 (0.08,0.29) |
| Jolanda sabatino(Sabatino et al., 2020) | 21 studies (77317 patients) | 0.36 (0.2,0.53) |
| Awadhesh K. singh(Awadhesh et al. 2020) | 18 studies (558 patients) | 0.11 (0.09,0.13) |
| Elinor Ten(Tan et al., 2020) | 45studies (16,561 patients) | 0.49 (0.44,0.54) |
| Carlos K.H. Wong(Wong et al., 2020) | 76 studies (11,028 patients) | 0.18 (0.15,0.2) |
| Jing YANG (Yang et al., 2020a) | 7studies (1576 patients) | 0.21 (0.13,0.27) |
| Setor K. Kunutsor(Kunutsor and Laukkanen, 2020) | 17 studies (5815 patients) | 0.29 (0.25,0.33) |
| Ting Wu(Wu et al., 2020a) | 73studies (171,108 patients) | 0.19 (0.15,0.23) |
| Zhaohai Zheng M.D(Zheng et al., 2020b) | 13 studies (3027 patients) | 0.22 (0.2,0.23) |
| Yinghao Cao(Cao et al., 2020) | 31studies (46,959 patients) | 0.18 (0.13,0.23) |
| Jing Yang (Yang et al., 2020b) | 8 studies (46248 patients) | 0.17 (0.14,0.22) |
| Safiya Richardson(Richardson et al., 2020) | 32studies (310585) | 0.56 (0.54,0.58) |
Table 4.
Odd ratio of Hypertension.
| Author | Sample Size | Odd ratios (95%CI) |
|---|---|---|
| Vignesh Chidambaram(Chidambaram et al., 2020) | 109 studies | 0.96 (0.73,1.2) |
| Bianca de Almeida-Pititto(de Almeida-Pititto et al., 2020) | 40 studies (18012 patients) | 1.09 (0.86,1.32) |
| Francesco Del Sole(Del Sole et al., 2020) | 12studies (2794 patients) | 0.8 (0.48,1.12) |
| Vageesh Jain(Jain and Yuan, 2020) | 7studies (1813 patients) | 0.67 (0.33,1.01) |
| Chayakrit Krittanawong(Krittanawong et al., 2020) | 13studies (49,076 patients) | 1.51 (0.67,2.35) |
| Ashish Kumar(Kumar et al., 2020) | 58studies (6892 patients) | 0.83 (0.6,1.06) |
| Jia Li(Li et al., 2020) | 12studies (2445 patients) | 0.87 (0.38,1.36) |
| Giuseppe Lippi(Lippi et al., 2020) | 13studies (2893 patients) | 0.91 (0.68,1.13) |
| Hong Liu(Liu et al., 2020a) | 24studies (10948 patients) | 1.04 (0.79,1.28) |
| Liman Luo(Luo et al., 2020) | 124 studies | 0.94 (0.75,1.13) |
| Meng Meng(Meng et al., 2020) | 35 studies (8170 patients) | 0.81 (0.58,1.06) |
| Sara Momtazmanesh(Momtazmanesh et al., 2020) | 54 studies | 0.93 (0.3,1.56) |
| Mudatsir(Mudatsir et al., 2020) | 19studies (3578 patients) | 0.84 (0.35,1.32) |
| Rizwana Parveen(Parveen et al., 2020) | 7studies (2018 patients) | 0.98 (0.23,1.74) |
| Bolin Wang(Wang et al., 2020a) | 6studies (1558 patients) | 0.82 (0.52,1.13) |
| Xinhui Wang(Wang et al., 2020b) | 34 studies | 1.071 (0.85,1.29) |
| Xiaomei Wu(Wu et al., 2020b) | 41 studies (5064 patients) | 0.96 (0.58,1.35) |
| Lizhan Xu(Xu et al., 2020) | 20 studies (4062 patients) | 0.83 (0.51,1.15) |
| Jing YANG(Yang et al., 2020a) | 7studies (1576 patients) | 0.85 (0.39,1.34) |
| Yue Zhou(Zhou et al., 2020) | 34 studies (16,110 patients) | 1.15 (0.9,1.4) |
| Thais M. Plasencia-vrizarri(Plasencia-Urizarri et al., 2020) | 13 studies (99,817 patients) | 1.39 (1.23,1.55) |
| Ting Wu(Wu et al., 2020a) | 73studies (171,108 patients) | 0.87 (0.73,1.02) |
| Zhaohai Zheng M.D(Zheng et al., 2020b) | 13 studies (3027 patients) | 1.0 (0.47,1.53) |
| Jing Yang(Yang et al., 2020b) | 8 studies (46248 patients) | 0.85 (0.37,1.34) |
Fig. 1.
Flow chart of studies selection in this meta-analysis.
Fig. 2.
Forest plot for prevalence of cardiovascular disease in patient with COVID -19. Each square (■) and its horizontal line, respectively, represent the prevalence and its 95% CI for each individual study (the size of the grey square corresponds to the weight of that study in the meta-analysis); the diamond and its horizontal diagonal (◊) show the combined overall prevalence and its 95% CI, respectively. Prevalence of cardiovascular disease in patent with COVID -19 is 0.08 (95%CI = 0.07,0.08, = 89.8%).
Fig. 4.
Forest plot for Odds Ratio for association between cardiovascular disease and severe/nonsevere patient of COVID-19. Each square (■) and its horizontal line, respectively, represent the OR and its 95% CI for each individual study (the size of the grey square corresponds to the weight of that study in the meta-analysis); the diamond and its horizontal diagonal (◊) show the combined overall OR and its 95% CI, respectively. The OR as 3.44 indicates that the odds of getting severe COVID-19 from cardiovascular disease is 3.44 times higher in those without cardiovascular disease. (OR = 3.44 & 95%CI = 3.18–3.72, P = 0.000, = 30.14%).
Fig. 6.
Forest plot for prevalence of hypertension in patient with COVID-19. Each square (■) and its horizontal line, respectively, represent the prevalence and its 95% CI for each individual study (the size of the grey square corresponds to the weight of that study in the meta-analysis); the diamond and its horizontal diagonal (◊) show the combined overall prevalence and its 95% CI, respectively. Prevalence of hypertension in patent with COVID-19 is 0.27 (95%CI = 0.27–0.28, = 98.5%).
Fig. 8.
Forest plot for Odds Ratio for association between hypertension and severe/nonsevere patient of COVID-19. Each square (■) and its horizontal line, respectively, represent the OR and its 95% CI for each individual study (the size of the grey square corresponds to the weight of that study in the meta-analysis); the diamond and its horizontal diagonal (◊) show the combined overall OR and its 95% CI, respectively. The OR as 2.68 indicates that the odds of getting severe COVID -19 from hypertension is 2.68 times higher in those without hypertension. (OR = 2.68 & 95%CI = 2.54–2.84, P = 0.00, = 48.37%).
Fig. 3.
The funnel plot of prevalence for CVD is approximately symmetric that in accord to results of Egger's (P = 0.000) and Begg's (P = 0.147) tests faded the possibility of the potential publication bias. However, to further assess the effect of missing studies on the summary effect, the trim and fill approach was applied and showed that after filling the missing studies the summary effect didn't change significantly. Odd ratio of CVD.
Fig. 5.
The funnel plot of OR for CVD is approximately symmetric that in accord to results of Egger's (P = 0.269) and Begg's (P = 0.628) tests faded the possibility of the potential publication bias. However, to further assess the effect of missing studies on the summary effect, the trim and fill approach was applied and showed that after filling the missing studies the summary effect didn't change significantly. Prevalence of Hypertension.
Fig. 7.
The funnel plot of prevalence for hypertension is approximately symmetric that in accord to results of Egger's (P = 0.000) and Begg's (P = 0.009) tests faded the possibility of the potential publication bias. However, to further assess the effect of missing studies on the summary effect, the trim and fill approach was applied and showed that after filling the missing studies the estimated prevalence of CVD didn't significantly change but estimated prevalence of hypertension increased from 0.27 (0.27–0.28) to 0.323 (0.318–0.328). Odd ratio of Hypertension.
Fig. 9.
The funnel plot of OR for hypertension is approximately symmetric that in accord to results of Egger's (P = 0.133) and Begg's (P = 0.385) tests faded the possibility of the potential publication bias. However, to further assess the effect of missing studies on the summary effect, the trim and fill approach was applied and showed that after filling the missing studies the summary effect didn't change significantly.
Prevalence of CVD.
3.1. Sensitivity analysis
To assess the impact of individual studies on the summary effect the influential anal analysis was performed and the results indicated that none of the summary effects was sensitive to individual studies. In other words, after eliminating of each study, the change in the summary effect was not statistically significant.
4. Discussion
As described in analysis of COVID-19 patients, hypertension and severe myocardial injury contribute to disease severity and mortality of these patients (Nishiura et al., 2020). People with basic CVD are more likely to be infected with the virus, and the virus infection can also lead to the deterioration of basic heart disease. In COVID-19 cases, it is important to recognize the clinical characteristics of patients in order to aid in early and rapid detection of infected persons, as well as to reduce patient mortality. Since many antiviral drugs can cause cardiac insufficiency, arrhythmia or other CV disorders, therefore, during treatment of the disease, especially with antiviral therapy, the risk of cardiac toxicity needs be closely monitored (Sakabe et al., 2013). More attention should be paid to patients with extremely increased cardiac cTnI levels-major plasma biomarker for the identification of myocardial infarction and cell necrosis in an ACS-and new case of arrhythmias (Park et al., 2017). The common laboratory abnormalities demonstrate that 2019-nCoV infection may be associated with cell-mediated immune deficiency, coagulation activation, myocardial injury, and liver and kidney damage. These abnormal laboratory results are similar to those previously reported in patients with MERS-CoV and SARS-CoV infection (Meo et al., 2020). Due to the poor prognosis, patients with CVD are special cases of COVID-19, and the prevention and treatment of cardiovascular events should be deliberated. In this study, we evaluated the results of meta-analyses to collectively re-assessment the basic cardiovascular characteristics in patients with COVID-19. Based on the results, hypertension and cardiovascular comorbidities can be considered as risk factors for persons with severe symptoms of the disease. Apparently, among COVID-19 patients, there were almost 50% diagnosed with chronic diseases, 40% with CV and cerebrovascular disorders, and patients with chronic diseases, such as hypertension, obesity, diabetes, chronic kidney failure and chronic obstructive pulmonary disease, have a developed risk of problems or even death after infection (Yu et al., 2020). Although, most of incorporated studies are single-center, which may show admission bias as well as selection bias. In addition, all of the incorporated studies were retrospective analytical studies, we could not rule out the power of other confounding agents. Most of the studies did not elucidate the guide-line for inclusion criteria, and course and severity of illness. Due to inadequate medical resources, only patients with relatively severe COVID-19 infection were admitted to hospital. Importantly, there may possibly be a selection bias when categorizing factors impact the clinical consequences. Large population-based cohort study of patients with COVID-19 from different countries will be beneficial to recognize the clinical features and risk factors of the disease. Moreover, the history of hypertension cause to alteration in blood vessels structure and disrupts the vascular integrity, and it is more sensitive to develop serious acute illness in severe infection conditions (Zheng et al., 2020b). Therefore, an extreme inflammatory response, along with pre-existing CVD may cause to development of cardiac disease in patients with COVID-19 infection. In other words, COVID-19 patients with CV basic diseases, are suggested to give main concern to treatment, and more attention against the recurrence or augmentation of the original basic pathological disorders (Cao et al., 2020; Channappanavar and Perlman, 2017). Furthermore, results showed that hypertension was related to the severity of COVID-19 infection and in patients with both hypertension and COVID-19, treatment is dependent on their conditions. Seemingly, the intensive care unit (ICU) patients had a greater number of comorbid conditions than those with no ICU admissions. This proposes that comorbidity may be potential risk factors for poor outcome (15). Consequently, a better understanding of the impacts of CVD will be necessary for the management of COVID-19 patients. Some experts suggest that, during the outbreak, people with previous CVD should firmly consume optimized drug regimens in accordance with health center guidance to provide further protection (Ferrario et al., 2005).
5. Conclusion
In conclusion, the present meta-analysis focused on the association between CVD risk and hypertension and severity of COVID-19. Our meta-analysis revealed that CVD and hypertension could be considered as potential risk factors for severity of the disease. Considering the connection exist between chronic CVD and COVID-19, will aid the health sector guide to distinguish high risk people and deliberate the risk factors of deterioration. Diabetes, respiratory system disease, and CVD were known as hypothetically key risk factors that should be encompassed in recommended future vaccination schedule. Collectively, underlying basic diseases such as hypertension and CVD are risk factors for disease progression and development. This is consistent with our analytical results obtained in this paper.
Author contributions
MBN, RY-R and HHM conceived the subject matter and contributed to the design of the work. The search was done by MBN and MA. HHM, MBN, MS and FN contributed to the acquisition, analysis, or interpretation of data for the work. MBN and ZJ wrote the original draft. ZJ illustrated graphical abstract. MBN, RY-R, JR, and MH critically revised the first draft. All authors approved the final version for all aspects of work ensuring integrity and accuracy.
Funding information
Financial support of this study was provided by the Mashhad University of Medical Sciences (Grant 990305).
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Abate S.M., Ahmed Ali S., Mantfardo B., Basu B. Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: a systematic review and Meta-analysis. PloS One. 2020;15(7) doi: 10.1371/journal.pone.0235653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aggarwal G., Cheruiyot I., Aggarwal S., Wong J., Lippi G., Lavie C.J., Henry B.M., Sanchis-Gomar F. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: a meta-analysis. Curr. Probl. Cardiol. 2020:100617. doi: 10.1016/j.cpcardiol.2020.100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh Awadhesh K., Clare L. Gillies, Ritu Singh, Akriti Singh, Yogini Chudasama, Briana Coles, Sam Seidu, Francesco Zaccardi, Melanie J. Davies, and Kamlesh Khunti. "Prevalence of co‐morbidities and their association with mortality in patients with COVID‐19: a systematic review and meta‐analysis." Diabetes Obes. Metabol. 22, no. 10 (2020): 1915-1924. [DOI] [PMC free article] [PubMed]
- Baradaran A., Ebrahimzadeh M.H., Baradaran A., Kachooei A.R. Prevalence of comorbidities in COVID-19 patients: a systematic review and meta-analysis. Archives of Bone and Joint Surgery. 2020;8(Suppl. 1):247. doi: 10.22038/abjs.2020.47754.2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Y., Liu X., Xiong L., Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS‐CoV‐2: a systematic review and meta‐analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channappanavar R., Perlman S. Seminars in Immunopathology. vol. 39. Springer; 2017. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology; pp. 529–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chidambaram V., Tun N.L., Haque W.Z., Majella M.G., Sivakumar R.K., Kumar A., Hsu A.T.-W., Ishak I.A., Nur A.A., Ayeh S.K. Factors associated with disease severity and mortality among patients with COVID-19: a systematic review and meta-analysis. PloS One. 2020;15(11) doi: 10.1371/journal.pone.0241541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Tian M., Huang D., Wang X., Huang Y., Fan L., Wang L., Chen Y., Liu W., Zhang K. A 55-day-old female infant infected with 2019 novel coronavirus disease: presenting with pneumonia, liver injury, and heart damage. J. Infect. Dis. 2020;221(11):1775–1781. doi: 10.1093/infdis/jiaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Almeida-Pititto B., Dualib P.M., Zajdenverg L., Dantas J.R., De Souza F.D., Rodacki M., Bertoluci M.C. Severity and mortality of COVID 19 in patients with diabetes, hypertension and cardiovascular disease: a meta-analysis. Diabetol. Metab. Syndrome. 2020;12(1):1–12. doi: 10.1186/s13098-020-00586-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Sole F., Farcomeni A., Loffredo L., Carnevale R., Menichelli D., Vicario T., Pignatelli P., Pastori D. Features of severe COVID‐19: a systematic review and meta‐analysis. Eur. J. Clin. Invest. 2020;50(10) doi: 10.1111/eci.13378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Archives of academic emergency medicine. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- Espinosa O.A., Zanetti A.d.S., Antunes E.F., Longhi F.G., Matos T.A.d., Battaglini P.F. vol. 62. Revista do Instituto de Medicina Tropical de São Paulo; 2020. (Prevalence of Comorbidities in Patients and Mortality Cases Affected by SARS-CoV2: a Systematic Review and Meta-Analysis). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrario C.M., Jessup J., Chappell M.C., Averill D.B., Brosnihan K.B., Tallant E.A., Diz D.I., Gallagher P.E. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- Fu L., Wang B., Yuan T., Chen X., Ao Y., Fitzpatrick T., Li P., Zhou Y., Lin Y., Duan Q. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold M.S., Sehayek D., Gabrielli S., Zhang X., McCusker C., Ben-Shoshan M. COVID-19 and comorbidities: a systematic review and meta-analysis. PGM (Postgrad. Med.) 2020;132(8):749–755. doi: 10.1080/00325481.2020.1786964. [DOI] [PubMed] [Google Scholar]
- Gómez-Ochoa S.A., Franco O.H., Rojas L.Z., Raguindin P.F., Roa-Díaz Z.M., Wyssmann B.M., Guevara S.L.R., Echeverría L.E., Glisic M., Muka T. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021;190(1):161–175. doi: 10.1093/aje/kwaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., Madhur M.S., Tomaszewski M., Maffia P., D'Acquisto F. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Sun J., Dai Z., Deng H., Li X., Huang Q., Wu Y., Sun L., Xu Y. Prevalence and severity of corona virus disease 2019 (COVID-19): a systematic review and meta-analysis. J. Clin. Virol. 2020 doi: 10.1016/j.jcv.2020.104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. 10223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain V., Yuan J.-M. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int. J. Publ. Health. 2020 doi: 10.1007/s00038-020-01390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Java A., Apicelli A.J., Liszewski M.K., Coler-Reilly A., Atkinson J.P., Kim A.H., Kulkarni H.S. The complement system in COVID-19: friend and foe? JCI insight. 2020;5(15) doi: 10.1172/jci.insight.140711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jutzeler C.R., Bourguignon L., Weis C.V., Tong B., Wong C., Rieck B., Pargger H., Tschudin-Sutter S., Egli A., Borgwardt K. medRxiv; 2020. Comorbidities, Clinical Signs and Symptoms, Laboratory Findings, Imaging Features, Treatment Strategies, and Outcomes in Adult and Pediatric Patients with COVID-19: A Systematic Review and Meta-Analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khateri S., Mohammadi H., Khateri R., Moradi Y. The prevalence of underlying diseases and comorbidities in COVID-19 patients; an updated systematic review and meta-analysis. Archives of academic emergency medicine. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- Knowlton K.U. Pathogenesis of SARS-CoV-2 induced cardiac injury from the perspective of the virus. J. Mol. Cell. Cardiol. 2020;147:12–17. doi: 10.1016/j.yjmcc.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh J., Shah S.U., Chua P.E.Y., Gui H., Pang J. Epidemiological and clinical characteristics of cases during the early phase of COVID-19 pandemic: a systematic review and meta-analysis. Front. Med. 2020;7:295. doi: 10.3389/fmed.2020.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krittanawong C., Virk H.U.H., Narasimhan B., Wang Z., Narasimhan H., Zhang H.J., Sun T., Messerli F.H. Coronavirus disease 2019 (COVID-19) and cardiovascular risk: a meta-analysis. Prog. Cardiovasc. Dis. 2020 doi: 10.1016/j.pcad.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Arora A., Sharma P., Anikhindi S.A., Bansal N., Singla V., Khare S., Srivastava A. Clinical features of COVID-19 and factors associated with severe clinical course. a systematic review and meta-analysis. 2020 doi: 10.1007/s12664-020-01058-3. Available at: SSRN 3566166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunutsor S.K., Laukkanen J.A. Cardiovascular complications in COVID-19: a systematic review and meta-analysis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., He X., Zhang W., Li X., Zhang Y., Li S., Guan C., Gao Z., Dong G. Meta-analysis investigating the relationship between clinical features, outcomes, and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Am. J. Infect. Contr. 2020 doi: 10.1016/j.ajic.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Wong J., Henry B.M. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): a pooled analysis. Pol. Arch. Intern. Med. 2020;130(4):304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging and disease. 2020;11(3):668. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Fang Y.-Y., Deng Y., Liu W., Wang M.-F., Ma J.-P., Xiao W., Wang Y.-N., Zhong M.-H., Li C.-H. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chinese Med J. 2020 doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Lu H., Wang W., Liu Q., Zhu C. Clinical risk factors for mortality in patients with cancer and COVID-19: a systematic review and meta-analysis of recent observational studies. Expert review of anticancer therapy1-13. 2020 doi: 10.1080/14737140.2021.1837628. [DOI] [PubMed] [Google Scholar]
- Luo L., Fu M., Li Y., Hu S., Luo J., Chen Z., Yu J., Li W., Dong R., Yang Y. The potential association between common comorbidities and severity and mortality of coronavirus disease 2019: a pooled analysis. Clin. Cardiol. 2020;43(12):1478–1493. doi: 10.1002/clc.23465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahumud R.A., Kamara J.K., Renzaho A.M. Evidence from a systematic review and meta-analysis; 2020. The Epidemiological Burden of and Overall Distribution of Chronic Comorbidities in Coronavirus Disease-2019 Among 202,005 Infected Patients. Infection1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair M., Singhavi H., Pai A., Singhavi J., Gandhi P., Conboy P., Baker A., Das S. The Laryngoscope; 2020. A Meta‐Analysis of 67 Studies with Presenting Symptoms and Laboratory Tests of COVID‐19 Patients. [DOI] [PubMed] [Google Scholar]
- Meng M., Zhao Q., Kumar R., Bai C., Deng Y., Wan B. Impact of cardiovascular and metabolic diseases on the severity of COVID-19: a systematic review and meta-analysis. Aging (N Y) 2020;12(22):23409. doi: 10.18632/aging.103991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S., Alhowikan A., Al-Khlaiwi T., Meo I., Halepoto D., Iqbal M., Usmani A., Hajjar W., Ahmed N. Novel coronavirus 2019-nCoV: prevalence, biological and clinical characteristics comparison with SARS-CoV and MERS-CoV. Eur. Rev. Med. Pharmacol. Sci. 2020;24(4):2012–2019. doi: 10.26355/eurrev_202002_20379. [DOI] [PubMed] [Google Scholar]
- Momtazmanesh S., Shobeiri P., Hanaei S., Mahmoud-Elsayed H., Dalvi B., Rad E.M. Cardiovascular disease in COVID-19: a systematic review and meta-analysis of 10,898 patients and proposal of a triage risk stratification tool. The Egyptian Heart Journal. 2020;72(1):1–17. doi: 10.1186/s43044-020-00075-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudatsir M., Fajar J.K., Wulandari L., Soegiarto G., Ilmawan M., Purnamasari Y., Mahdi B.A., Jayanto G.D., Suhendra S., Setianingsih Y.A. Predictors of COVID-19 severity: a systematic review and meta-analysis. F1000Research. 2020;9 doi: 10.12688/f1000research.26186.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandy K., Salunke A., Pathak S.K., Pandey A., Doctor C., Puj K., Sharma M., Jain A., Warikoo V. Coronavirus disease (COVID-19): a systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events. Diabetes & Metabolic Syndrome: Clin. Res. Rev. 2020;14(5):1017–1025. doi: 10.1016/j.dsx.2020.06.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasiri M.J., Haddadi S., Tahvildari A., Farsi Y., Arbabi M., Hasanzadeh S., Jamshidi P., Murthi M., Mirsaeidi M. medRxiv; 2020. COVID-19 Clinical Characteristics, and Sex-specific Risk of Mortality: Systematic Review and Meta-Analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H., Jung S.-m., Linton N.M., Kinoshita R., Yang Y., Hayashi K., Kobayashi T., Yuan B., Akhmetzhanov A.R. Multidisciplinary Digital Publishing Institute; 2020. The Extent of Transmission of Novel Coronavirus in Wuhan, China, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization W.H. 2020. Naming the Coronavirus Disease (COVID-19) and the Virus that Causes it. [Google Scholar]
- Park K.C., Gaze D.C., Collinson P.O., Marber M.S. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc. Res. 2017;113(14):1708–1718. doi: 10.1093/cvr/cvx183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parveen R., Sehar N., Bajpai R., Agarwal N.B. Association of diabetes and hypertension with disease severity in covid-19 patients: a systematic literature review and exploratory meta-analysis. Diabetes Res. Clin. Pract. 2020:166. doi: 10.1016/j.diabres.2020.108295. 108295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel U., Malik P., Usman M.S., Mehta D., Sharma A., Malik F.A., Khan N., Siddiqi T.J., Ahmed J., Patel A. Age-adjusted risk factors associated with mortality and mechanical ventilation utilization amongst COVID-19 hospitalizations—a systematic review and meta-analysis. SN comprehensive clinical medicine. 2020;2(10):1740–1749. doi: 10.1007/s42399-020-00476-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plasencia-Urizarri T.M., Aguilera-Rodríguez R., Almaguer-Mederos L.E. Comorbidities and clinical severity of COVID-19: systematic review and meta-analysis. Rev. habanera cienc. 2020:méde3389–e3389. [Google Scholar]
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. Jama. 2020 doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P., Alvarado-Arnez L.E., Bonilla-Aldana D.K., Franco-Paredes C., Henao-Martinez A.F. Travel medicine and infectious disease101623; 2020. Clinical, Laboratory and Imaging Features of COVID-19: A Systematic Review and Meta-Analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatino J., De Rosa S., Di Salvo G., Indolfi C. Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PloS One. 2020;15(8) doi: 10.1371/journal.pone.0237131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakabe M., Yoshioka R., Fujiki A. Sick sinus syndrome induced by interferon and ribavirin therapy in a patient with chronic hepatitis C. Journal of Cardiology Cases. 2013;8(6):173–175. doi: 10.1016/j.jccase.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan E., Song J., Deane A.M., Plummer M.P. Global impact of coronavirus disease 2019 infection requiring admission to the ICU. a systematic review and meta-analysis. Chest. 2020 doi: 10.1016/j.chest.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Li R., Lu Z., Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (N Y) 2020;12(7):6049. doi: 10.18632/aging.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Fang X., Cai Z., Wu X., Gao X., Min J., Wang F. Research; 2020. Comorbid Chronic Diseases and Acute Organ Injuries Are Strongly Correlated with Disease Severity and Mortality Among COVID-19 Patients: a Systemic Review and Meta-Analysis. 2020 2402961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. Jama. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- Wong C.K., Wong J.Y., Tang E.H., Au C.H., Wai A.K. a systematic review and meta-analysis; 2020. Clinical Presentations, Laboratory and Radiological Findings, and Treatments for 11,028 COVID-19 Patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Zuo Z., Kang S., Jiang L., Luo X., Xia Z., Liu J., Xiao X., Ye M., Deng M. Multi-organ dysfunction in patients with COVID-19: a systematic review and meta-analysis. Aging and disease. 2020;11(4):874. doi: 10.14336/AD.2020.0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Liu L., Jiao J., Yang L., Zhu B., Li X. Characterisation of clinical, laboratory and imaging factors related to mild vs. severe covid-19 infection: a systematic review and meta-analysis. Ann. Med. 2020;52(7):334–344. doi: 10.1080/07853890.2020.1802061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Mao Y., Chen G. Risk factors for 2019 novel coronavirus disease (COVID-19) patients progressing to critical illness: a systematic review and meta-analysis. Aging (N Y) 2020;12(12):12410. doi: 10.18632/aging.103383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youn J.-C., Yu H.T., Lim B.J., Koh M.J., Lee J., Chang D.-Y., Choi Y.S., Lee S.-H., Kang S.-M., Jang Y. Immunosenescent CD8+ T cells and CXC chemokine receptor type 3 chemokines are increased in human hypertension. Hypertension. 2013;62(1):126–133. doi: 10.1161/HYPERTENSIONAHA.113.00689. [DOI] [PubMed] [Google Scholar]
- Yu Y., Xu D., Fu S., Zhang J., Yang X., Xu L., Xu J., Wu Y., Huang C., Ouyang Y. Patients with COVID-19 in 19 ICUs in Wuhan, China: a cross-sectional study. Crit. Care. 2020;24:1–10. doi: 10.1186/s13054-020-02939-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J., Li Q., Jiang C., Zhou Y., Liu S. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Yang Q., Chi J., Dong B., Lv W., Shen L., Wang Y. Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler C.G., Allon S.J., Nyquist S.K., Mbano I.M., Miao V.N., Tzouanas C.N., Cao Y., Yousif A.S., Bals J., Hauser B.M. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020 doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]