Abstract
Purpose of the research
We describe two interventions to screen for SARS-CoV-2 in two squats of exiled persons in France following the diagnosis of symptomatic COVID-19 cases.
Principal results
In squat A, 50 (25%) persons were screened; 19 were found positive, and three accepted a transfer. In squat B, 65 (54%) persons were screened at three different times, and only two were found positive.
Major conclusions
Discrepant outcomes may reflect different levels of sanitation, prevention, and acceptance of interventions. Refusal to be transferred to specific COVID-19 homes if tested positive underscores the importance of local sanitary solutions for all. Cross-curricular strategies addressed to exiled persons are essential means of providing medical and public health solutions designed to deter COVID-19 outbreaks in these populations.
Keywords: COVID-19, Infection, Homeless, Migrant
1. Introduction
France has been markedly affected by the SARS-CoV-2 pandemic, and authorities ordered a lockdown on the 17th of March 2020. Incidence of hospitalisations decreased nationally starting on the 31st of March [1]. Health authorities adopted a strategy of search and isolation of clusters, with extensive testing of symptomatic and closely exposed persons, and isolation of positive cases.
Exiled persons from resource-poor countries, some of whom are dismissed asylum seekers, are a particularly vulnerable population in France. Many live in dire conditions, commonly in squats, due to major social and economic difficulties. These people are difficult to reach, particularly for health-care prevention programs, and given their social conditions, encounter more difficulties in confining [2].
To effectively limit the spread of the SARS-CoV-2 into the community, information, screening, and isolation of index and contact cases in all populations are essential. We report a COVID-19 screening experience in two squats following the diagnosis of symptomatic cases, and present the different efficacy outcomes of these interventions.
2. Methods
Montpellier Métropole is a metropolitan area with approximately 450,000 inhabitants located in the South of France. Medical associations, such as Médecins du monde, monitor squats in Montpellier with the objective of providing assistance in agreement with each squat's representative, who is usually a social worker. The squats are primarily inhabited by exiled people in economic and social hardship. Some are asylum seekers or rebuffed asylum seekers, while others are economic exiles. Since the COVID-19 outbreak, clinical assessment and testing for SARS-CoV-2 on nasopharyngeal swabs have been proposed when appropriate.
Following monitoring, COVID-19 was diagnosed in five moderately symptomatic residents dwelling in two squats. On the 23rd of March 2020, four residents were diagnosed with COVID-19 in squat A, as was one resident in squat B. Spearheaded by “Médecins du Monde”, a strategy to extensively diagnose and confine contaminated individuals, similar to responses to COVID-19 outbreaks in nursing care facilities [3] or cruising ships [4], was planned out. The plan brought together the regional health authorities, medical associations, infectious diseases specialists from the University Hospital, social workers coordinating the squats and local political authorities (representatives of the Mayor's office and the Prefect). Subsequent to decisions reached at these meetings, positive cases were to be monitored, if willing, in a medicalised homeless facility, or else hospitalised according to clinical severity, while negative comorbid residents at risk were to be sheltered in a hotel.
Prior to intervention, accompanied by the social workers, medics repeatedly visited the two squats and gave flyers on COVID-19 symptoms and risks, advice on preventive measures, and information on the testing procedures; they also estimated the number of residents, and enlisted volunteers.
Living conditions and sanitary situations of each squat were recorded, as were demographic data on the screened population. Percentage of residents screened, percentage of residents positive for SARS-CoV-2 and the number of positive cases referred to the COVID shelter were evaluated as outcomes. Oral consent for data use and publication was obtained, and only data useful for clinical care were recorded.
3. Results
The populations screened in squats A and B were mainly young exiles with median ages of 31 and 30 years, respectively (Table 1 ), with an estimated 200 and 120 residents respectively. French speaking people were more frequently present in squat B. In squat A, there were no showers, only one water source and three toilets. In squat B, there were three showers and four toilets, with access to water. Distancing and containment after the first positive case was possible in single rooms and carried out in squat B, whereas following the initial cases, no isolation or barrier measures had been implemented in squat A.
Table 1.
Characteristics of the residents screened for SARS-CoV-2 (excluding the two social workers).
| No. (%) |
||
|---|---|---|
| Characteristic | Squat A (n = 50) | Squat B (n = 65) |
| Age, mean (SD), y | 31 (16) | 30 (13) |
| Number of persons sharing the same room, mean (SD) | 1.8 (0.7) | 2.2 (1.4) |
| Transfer to COVID-shelter, n (%) | 3 (6) | 0 |
On the 21st of April 2020, a mobile unit for nasopharyngeal testing arrived in squat A. Out of the 75 of the estimated 200 residents who had initially volunteered for testing (Fig. 1 ), 35 actually came to be tested. All in all, 50 persons were tested, as 15 additional subjects agreed to be tested on the day of the intervention (Table 1). Only two tested subjects had a cough (4%). On the 23rd of April, results were handed back to 34 of the 50 tested persons, including 16 of the 19 positive cases, who thereby accounted for 38% of the screened population. The medical team had to leave before having completed its work, the reason being that two residents did not accept their presence on the premises. Other test results were communicated by phone on the 24th and 25th of April. All in all, eight residents, one of whom had tested positive, did not initially receive their results. Three of the positive cases went to the COVID-shelter for homeless persons. Interactions with the medical association were resumed a few weeks later, and two months after screening, six additional toilets and showers were set up. Even though systematic screening was not undergone, no hospitalisations or new cases were diagnosed after our intervention. On the 31st of August 2020, authorities decided to dismantle the squat.
Fig. 1.
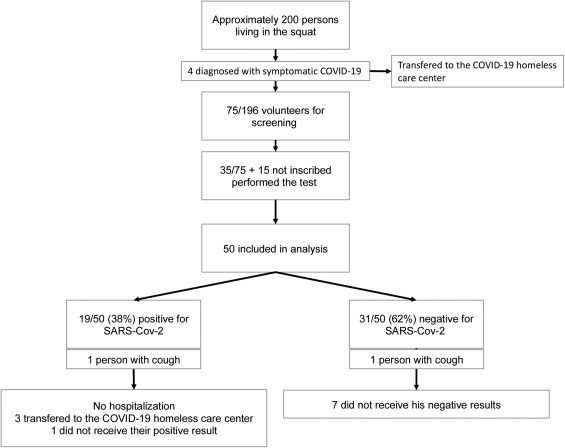
Squat A screening.
In squat B, screening sessions were carried out three times during a period of 14 days. On the 14th of May, 49 persons were screened, and none were found positive (Fig. 2 ). Five days later, ten other persons were tested, and two positive cases were identified. Six more subjects underwent testing ten days later, and the results were negative. All in all, 65 persons were tested (54% of estimated residents), nine of whom were tested twice at different sessions. None of them went to the COVID shelter. Positive cases accounted for 3% of the screened population. Three showers and two toilets were provided in the days following screening, as were masks and sanitisers. Acceptance of the intervention was very good. After which, no new cases were diagnosed and no positive subjects were hospitalised, even though systematic screening of the residents had not been provided.
Fig. 2.
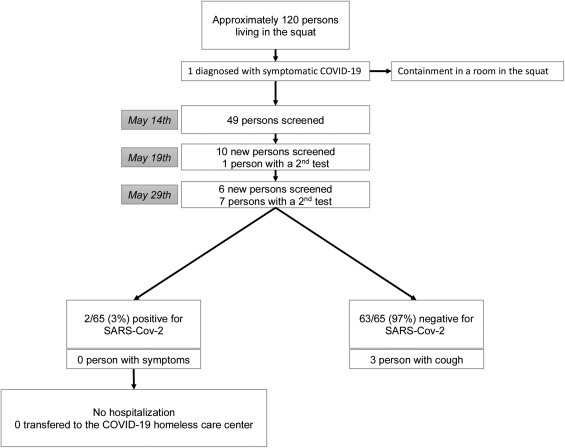
Squat B screening.
4. Discussion
Our experience of testing for COVID-19 in squats revealed a high level of asymptomatic disease transmission, particularly in squat A. Monitoring squats and testing only subjects with symptoms may favour inter-resident spread of the virus before the first symptomatic case diagnosis; in addition, prior transmission to comorbid or older residents may occur. The high degree of asymptomatic and paucisymptomatic contaminations in squat A can be explained by the young median ages and the healthy populations residing on the premises. However, systematic and regular screening of squat residents is challenging to organise, and acceptance among exiles may be limited, given that some of them may not have legal resident status. This contrasts with routine surveillance strategies in other settings, such as homeless shelters in the state of Washington (USA) [5]. High transmission rates, particularly in squat A, could also have resulted from dire sanitary conditions, difficulties in achieving adequate confinement, and the time-lapse between the diagnosis of the initial symptomatic cases and the planned screening interventions.
Our experiences underscore low acceptance of the intervention, particularly in squat A, notwithstanding painstaking careful planning and the experience of professionals, and the individual and community benefits of the intervention were correspondingly limited. These results contrast with those reported in a publication on a homeless care facility in Boston [6], in which all of the 408 residents were assessed and tested. Local political authorities were closely involved, and the population was composed of homeless, but not exiled, persons. So it is that context, political engagement, pre-existing sanitary conditions and legal issues are major determinants of the success of these interventions. The difficulty in upgrading sanitary conditions may have contributed to the low acceptance of our intervention in squat A. In addition, some residents may have been wary of any kind of governmental representation, even that of health-care medics, given their fear of impending expulsion procedures of dismissed asylum-seekers. Cultural misrepresentations of COVID-19 [7] might also explain some of our results, particularly in squat A. Meaningful community engagement and community-based interventions are a key element in ensuring that health strategies are widely accepted and reasonably effective.
Other obstacles to controlling outbreaks in our settings include the high mobility of residents, whose frequent moves from one squat to another may entail a high risk of viral spread. Since the end of lockdown, the double objective of caring for patients and controlling the epidemic in these settings may have been rendered even more difficult than was the case during our study.
In conclusion, the COVID-19 outbreak and our experiences underscore the challenges encountered at the individual and the aggregate levels amongst the exiled populations in France. Cross-curricular strategies are essential to appropriate and culture-centered medical and sanitary assistance for COVID-19 diagnosis and management. They will necessitate social and political measures that might help to reduce reducing the prevalence of SARS-CoV-2 and risk of viral spread in this population.
Ethical statement
This retrospective study received the approval of an Institutional review board on the 18th of May 2020.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments
Contribution
All authors contributed to the interventions, data collection, and vow for the exactness of the data submitted in this paper. All authors have approved the final version of the manuscript.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgement
This work did not receive any specific funding
References
- 1.Chêne COVID-19 : point épidémiologique du 30 avril 2020. Sante Publique Fr. 2020 [published online April 30; https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-30-avril-2020] [Google Scholar]
- 2.Bhopal R. COVID-19: undocumented migrants are probably at greatest risk. BMJ. 2020:369. doi: 10.1136/bmj.m1673. [DOI] [PubMed] [Google Scholar]
- 3.Arons M.M., Hatfield K.M., Reddy S.C., et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020 doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baraniuk C. What the Diamond Princess taught the world about COVID-19. BMJ. 2020 doi: 10.1136/bmj.m1632. [m1632] [DOI] [PubMed] [Google Scholar]
- 5.Rogers J.H., Link A.C., McCulloch D., et al. Characteristics of COVID-19 in homeless shelters. Ann Intern Med. 2020 doi: 10.7326/M20-3799. [published online Sept 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baggett T.P., Keyes H., Sporn N., Gaeta J.M. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020 doi: 10.1001/jama.2020.6887. [published online April 27] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hargreaves S., Zenner D., Wickramage K., Deal A., Hayward S.E. Targeting COVID-19 interventions towards migrants in humanitarian settings. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30292-9. [S1473309920302929] [DOI] [PMC free article] [PubMed] [Google Scholar]


