Abstract
Background
Exposure to ambient air pollution is related to 4.2 million premature deaths per year worldwide and is associated with a variety of adverse health outcomes, such as respiratory and cardiovascular morbidity. Furthermore, exposure to air pollution can increase human sensitivity to respiratory pathogens via damage to the respiratory tract or via airborne transmission on the surface of particulate matter, and might be an additional factor influencing COVID-19 morbidity and mortality rates. The aim of this study was to examine the association between populations' exposure to air pollution and the morbidity and mortality rates from COVID-19.
Methods
We examined the association between population-weighted long-term exposure to PM2.5 and NOx, and the morbidity and mortality over time following the detection of the first COVID-19 positive case in 36 OECD countries. Pearson and Spearman correlations between daily COVID-19 morbidity and mortality (Jan–Jun 2020) on the 10th, 20th, 40th, 60th and 80th days since first confirmed case in the country, and demographic, health, economic, and environmental data were calculated. Multivariate linear regression were used to examine the associations between demographic, health, economic and air pollution features and the rate of confirmed cases and deaths on the 60th and 80th days following the first confirmed case.
Results
PM2.5 concentrations in 2015–2017 were positively correlated with COVID-19 morbidity and mortality on the 10th, 20th, 40th and 60th days since the first confirmed case in all countries. NOx concentrations in 2015–2017 and country's density (population/Km2) were positively correlated with COVID-19 morbidity and mortality on the 60th day. All multivariate linear regressions consisting PM2.5 concentrations models were statistically significant. Our models also emphasize the importance of the relative number of hospital beds in decreasing the morbidity and mortality of COVID-19.
Conclusions
The adverse health outcomes stemming from long-term exposure to various air pollutants has long been known to the scientific community. According to our results and previously published studies, it appears that long-term exposure to air pollutants concentrations exceeding WHO guidelines, such as PM2.5 and NOx, might exacerbate morbidity and mortality rates from COVID-19. These results should raise a red flag globally among decision makers about the urgent need to reduce air pollution and its harmful effects.
Keywords: COVID-19, PM2.5, NOx, Chronic environmental exposure, Air pollution, Morbidity and mortality
Abbreviations: WHO, World Health Organization; IARC, International Agency for Research on Cancer; PM, Particulate matter; PM2.5, Fine PM with diameter less than 2.5 μm; PM10, PM with a diameter less than 10 μm; NOx, Nitrogen oxides; SOx, Sulfur oxides; VOCs, Volatile organic compounds; NO2, Nitrogen dioxide; NO, Nitrous oxide; COVID-19, The novel coronavirus disease; SARS-CoV-2, The novel coronavirus; GDP, Gross Domestic Product; OECD, Organisation for Economic Cooperation and Development
1. Introduction
According to the World Health Organization (WHO), worldwide 4.2 million premature deaths per year are related to the exposure to ambient air pollution. Overall, in 2016, 91% of the world population was exposed to ambient air pollutants that exceeded WHO guideline limits (World Health Orgnization, 2018). In addition, the International Agency for Research on Cancer (IARC), published an assessment on October 2013 that unanimously classified outdoor air pollution and particulate matter (PM) from outdoor air pollution as carcinogenic to humans (Group 1), based on vast evidence of carcinogenicity in humans and animals, and strong mechanistic evidence including genotoxic effects such as somatic and germ-cell mutations, cytogenetic abnormalities, and DNA damage. In particular, an increased risk of lung cancer was consistently observed in studies that included millions of people across the world (Loomis et al., 2013).
Ample studies show that ambient air pollutants such as PM with diameter less than 10 μm (PM10) and ambient fine PM with diameter less than 2.5 μm (PM2.5), Nitrogen oxides (NOx), Sulfur oxides (SOx), Ozone (O3) and Volatile organic compounds (VOCs) are associated with adverse health outcomes. These effects include respiratory (asthma, chronic obstructive pulmonary disease, pneumonia) and cardiovascular (enhanced thrombosis, elevated arterial blood pressure, and enhanced atherosclerosis) morbidity and premature mortality (Khafaie et al., 2016; World Health Organization, 2006, 2013). Furthermore, recent studies have shown that exposure to ambient air pollution is associated with increased oxidative stress that is the primary cause for the aforementioned morbidities, and may lead to additional morbidities such as diabetes and cancer (Mudway et al., 2020).
PM2.5 is naturally emitted in dust storms and forest fires, but is also emitted from anthropogenic activities such as fossil fuel combustion (by transportation vehicles, industrial activities and power generation) and due to excavation and construction activities. One of the most abundant NOx compounds - nitrogen dioxide (NO2) is primarily emitted by road traffic or indoor combustion sources and plays a major role in ground level Ozone formation. It is also often used as a marker for the cocktail of combustion related pollutants such as PM including ultrafine particles (<0.1 μm), nitrous oxide (NO) or benzene (World Health Organization, 2006).
According to WHO, 92% of the world population is exposed to PM2.5 levels that exceed WHO guideline limits (10 μg/m3 annual mean and 25 μg/m3 24 h mean) (World Helath Organizaion, 2018). For example, we recently found that the entire Israeli population is exposed to PM2.5 concentrations that exceed local target values according to the Israeli Clean Air Law and WHO annual mean, with an annual average of 17.8 μg/m3 (Levy et al., 2020). PM2.5 may penetrate the lower respiratory system, pass the lung barrier and enter the blood system. Chronic exposure to this pollutant contributes to the risk of developing cardiovascular and respiratory diseases, and lung cancer (World Health Organization, 2006; World Health Organization, 2018).
WHO NO2 guideline limits are 40 μg/m3 (annual mean) and 200 μg/m3 (1 h mean). At short-term, concentrations exceeding 200 μg/m3 are considered toxic and can cause significant inflammation of the airways. The frequency of symptoms such as bronchitis in asthmatic children and reduced lung function in adults were found to be associated with long-term exposure to NO2 (World Health Organization, 2006, 2018).
Several studies have shown that exposure to ambient air pollution can affect the cilia in the human respiratory tract, which in some cases might become shorter or even missing. This damage affects the cilia ability to clear the respiratory tract (Cao et al., 2020). Exposure to NO2 decreased ciliary beat frequency in healthy subjects reducing mucociliary clearance function of the lower respiratory tract, the lower trachea and the lungs. This negative impacts on the respiratory system's first line of defense, which is in charge of removing mucus-containing pollutants and pathogens outside of the respiratory system, may increase the risk for developing chronic respiratory morbidity and increase sensitivity for respiratory pathogens for people who are chronically exposed to air pollution (Helleday et al., 1995; Blomberg, et al.1999).
In a recent nationwide study, data of 60 million American Medicare beneficiaries over the age of 65 was analyzed. This study showed that a long-term rise of 1 μg/m3 in ambient PM2.5 is associated with an increase of 0.73% in all-cause mortality (Di et al., 2017). Chronic exposure to high levels of air pollutants can lead to the development of chronic inflammatory stimulus even in young healthy adults and have a more significant impact on vulnerable populations. Such an impact might be an additional factor for the recorded elevated morbidity and mortality rates caused by the novel coronavirus (SARS-CoV-2) in several districts of Northern Italy and in Milan in particular, which suffer from heavy air pollution (Conticini et al., 2020; Zoran et al., 2020). Additionally, airborne diffusion via PM aerosols might expand SARS-CoV-2 distribution in heavy air polluted areas, when PM can also serve as a vector, transporting the viruses deeply into the lungs, thus enhancing SARS-CoV-2 virus transmission mechanism (Zoran et al., 2020; Setti et al., 2020).
A new nationwide study that still haven't been peer reviewed, collected data from 3,000 counties in the US (representing 98% of the U.S. population) estimated the relationship between long-term exposure to PM2.5 and the novel coronavirus disease (COVID-19) death rates. It was reported that a rise of 1 μg/m3 in ambient PM2.5 concentrations is associated with an increase of 8% in the COVID-19 death rates (Wu et al., 2020). Another study recently conducted in 355 municipalities (with an average population of approximately 47,000 people) in the Netherlands, showed similar trends when a 1 μg/m3 increase in ambient PM2.5 concentrations was associated with additional 9.4 COVID-19 cases, 3.0 more hospital admissions, and 2.3 more deaths per municipality (Cole et al., 2020).
The aim of this study was to examine the association between populations' chronic exposure to air pollution and COVID-19 morbidity and mortality rates. We examined the associations between weighted exposure to PM2.5 and NOx concentrations, the percentages of population exposed to PM2.5 levels exceeding WHO guideline levels and the morbidity and mortality over time following the detection of the first COVID-19 positive case in 36 OECD countries. We hypothesized that populations living in OECD countries suffering from higher air pollution would have higher morbidity and mortality percentage compared with ones from relatively low air pollution.
2. Methods
2.1. Data collection
We focused on 36 OECD countries (as of March 2020, not including Columbia that joined the OECD in April 2020): Australia, Austria, Belgium, Canada, Chile, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Korea, Latvia, Lithuania, Luxembourg, Mexico, Netherlands, New Zealand, Norway, Poland, Portugal, Slovak Republic, Slovenia, Spain, Sweden, Switzerland, Turkey, the United Kingdom, and the United States.
Daily morbidity and mortality data on COVID-19 in the 36 OECD countries at the period of January 21st to June 7th, 2020 were collected from the World Health Organization (WHO) website (World Health Organization, 2020). For each OECD country, we calculated the following measures: number of confirmed cases, number of deaths, rate of deaths out of the total number of confirmed cases, rate of confirmed cases out of the country population, and rate of deaths out of the country population. These measures were calculated for the 10th, 20th, 40th, 60th and 80th day since the detection of the first COVID-19 positive case in the country.
Numbers of physicians per 100,000 population in 2015–2017 were collected from the World Bank website (The World Bank. Data/Phys, 2018). For the analyses we used the number of physicians in 2017. In case this value was missing, we used the number of physicians in 2016 or in 2015 (the larger value).
Numbers of hospital beds per 100,000 population in 2012–2015 were collected from the World Bank website (The World Bank. Data/Hosp, 2019). In case the 2015 value was missing, we used the number of hospital beds in 2014, and in case the 2014 value was also missing, we used the value of 2012 or 2013 (the larger value).
National percentages of elderly populations (older than 64 years) in 2018 were collected from the World Bank website (The World Bank. Data/Popu, 2018). National population estimates and country sizes (in Km2) were collected from the World Bank website (The World Bank. Data/Popu, 2019). Countries’ densities were calculated by dividing the population sizes by their areas. Data on gross domestic product (GDP) in 2019 were collected from the OECD website (OECD Data/GDP, 2019).
Data on percentages of population exposed to PM2.5 levels exceeding WHO guideline value in 2015–2107 were collected from the World Bank website (The World Bank, 2017a). Population-weighted exposure to PM2.5 (the average level of exposure of a nation's population to PM2.5 concentrations) in 2015–2017 were collected from the World Bank website (The World Bank, 2017b). NOx emission data in 2015–2017 were collected from the OECD website (OECD Data/Air and G em, 2017). National NOx concentrations in 2015–2017 were calculated by dividing the country's NOx emission data by its area.
2.2. Statistical analyses
We calculated correlations between COVID-19 data (morbidities and mortalities) and the demographic, health, economic, and environmental data, on the countries’ data (n=36). In general, the COVID-19 data did not follow a particulate trend: it followed a semi-linear trend in the first days since first positive case, and a semi-exponential trend in the following weeks. We therefore calculated both Pearson correlations (to detect linear associations in the first days) and Spearman correlations (to detect non-linear associations in the following weeks).
In order to better understand the effect of air pollutants chronic exposure on COVID-19 morbidity, we compared the pollutant concentrations in countries with low rates of confirmed cases to pollutant concentrations in countries with high rates of confirmed cases and deaths. This was done by calculating the median of the rates of confirmed cases in the 80th day (out of the entire national populations) and dividing the countries into: “red” countries - countries with rates higher than the median, and “green countries” - countries with rates lower than the median. We used the nonparametric two-sample Kolmogorov-Smirnov test to compare the PM2.5 and NOx concentrations between these two groups of countries.
The level of significance was 0.05 in all analyses.
Multivariate linear regressions were used to examine the associations between demographic, health, economic and air pollution features and the rate of confirmed cases and deaths (out of the entire national population) in the 60th and the 80th days (since the first confirmed case in each country). We used the logarithm value of the mortality and morbidity in the multivariate linear regression. All statistical analyses were performed using Matlab© version R2019b.
3. Results and discussion
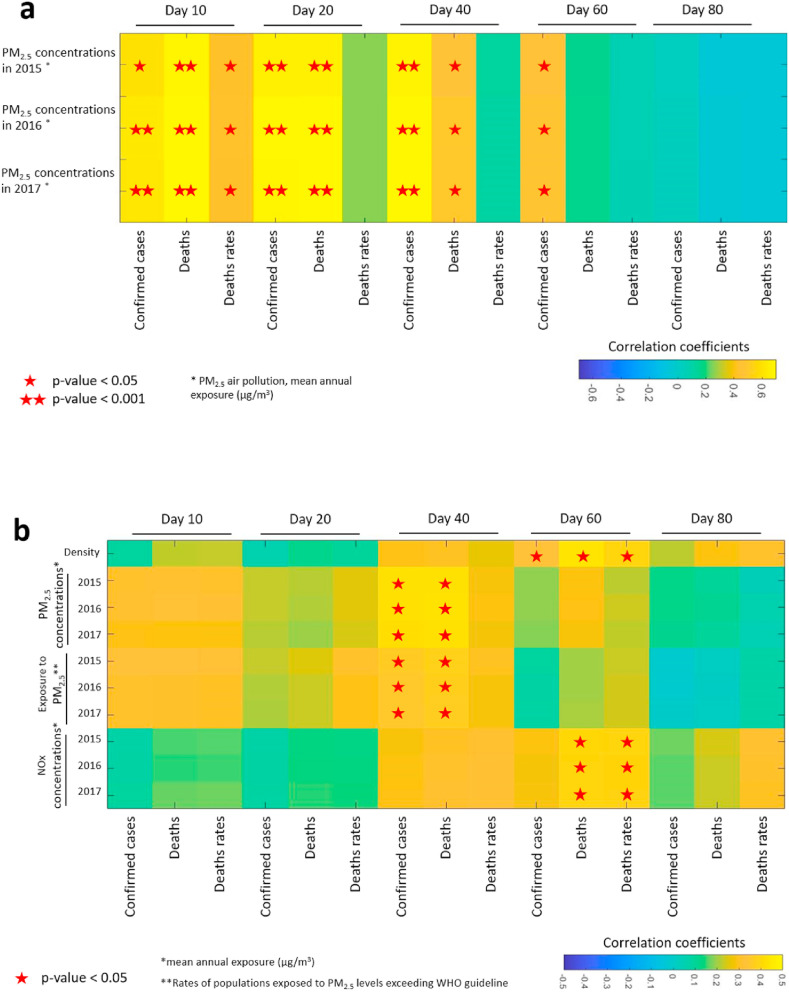
PM2.5 concentrations in 2015, 2016 and 2017 were positively correlated with COVID-19 morbidity (numbers of confirmed COVID-19 cases) and mortality on the 10th, 20th, 40th and 60th days since first confirmed case in every country (p<0.05, Pearson correlations, see Fig. 1 a and supplementary Table S1). This finding is in agreement with the associations between air pollution by PM2.5 and COVID-19 mortality that were found in North Italy and in a nationwide study in the US which associated an increase of 1 μg/m3 in PM2.5 concentrations with an 8% increase in the COVID-19 death rate (Conticini et al., 2020; Wu et al., 2020). In addition to the well-known negative health outcomes of chronic PM2.5 exposure (World Health Organization, World Health Organization, 2006, World Health Organization, 2013), several recent studies postulated that PM aerosols can also serve as a vector transporting bacteria and viruses through airborne diffusion, allowing them to penetrate deeply into the lungs and surpass the multilayer barriers of the respiratory system, thus enhancing SARS-CoV-2 virus transmission mechanism (Zoran et al., 2020; Setti et al., 2020). Such airborne transmission route for COVID-19 was suggested as a possible reason for mass indoor infections in restaurants, buses and fitness centers and in some cases via ventilation systems (Bae et al., 2020; Shen et al., 2020; Lu et al., 2020). Such a route was also recognized by the CDC in 2020 under special circumstances such as: 1. Enclosed spaces in which susceptible people were exposed shortly after an infectious person had left the area; 2. Prolonged exposure to respiratory particles, often generated due to shouting, singing or exercising; 3. Inadequate ventilation that allowed a build-up of suspended respiratory droplets and particles (CDC, 2020). Therefore, future efforts to prevent and control COVID-19 should also consider SARS-CoV-2 airborne spread potential.
Fig. 1.
Correlations between environmental factors (PM2.5 concentrations, PM2.5 exposure exceeding WHO guideline and NOx concentrations in 2105–2017) and COVID-19 morbidity and mortality. 1a – Pearson correlations, 1b – Spearman correlations. Stars indicate the correlation was statistically significant (one star: 0.001<p<0.05, two stars: p≤0.001).
Rates of populations exposed to PM2.5 levels exceeding WHO guideline at 2015–2017 were positively correlated with COVID-19 morbidity and mortality on the 40th day (p<0.05, Spearman correlations, see Fig. 1b). NOx concentrations in 2015–2017 were positively correlated with COVID-19 morbidity and mortality in the 60th day (p<0.05, Spearman correlations, see Fig. 1b). A novel research that analyzed NO2 concentrations from 66 administrative regions in Italy, Spain, France and Germany suggested that long-term exposure to NO2 may be one of the important contributors to COVID-19 fatality in these regions (Ogen, 2020). Additional research, conducted in the Netherlands found a positive statistically significant association between COVID-19 cases and deaths to NO2 levels (Cole et al., 2020).
Country density (population per Km2) was also positively correlated with COVID-19 morbidity and mortality on the 60th day (p<0.05, Spearman correlation, see Fig. 1b).
Next, we compared the rates of confirmed cases and death rates (out of the entire national population). Country density was positively correlated with the rate of deaths on the 40th day (R=0.33, p=0.05), and with the rate of deaths on the 80th day (R=0.34, p=0.04, Pearson correlation). NOx concentrations in 2015 were positively correlated with the rate of deaths on the 20th day (R=0.36, p=0.03), and on the 40th day (R=0.34, p=0.04). Of note, the numbers of hospital beds were negatively correlated with the rate of confirmed cases on the 80th day (R=−0.34, p=0.04), (Supplementary Table S2). Spearman correlations yielded statistically significant associations between NOx concentrations in 2015–2017 and the rate of deaths on the 60th day (p=0.04), (Supplementary Table S2).
Although modest, these positive associations between the two major air pollutant concentrations, the rates of COVID-19 confirmed cases and mortality rates are not surprising. PM2.5 was previously linked to various negative health outcomes including premature death in patients with cardiovascular or lung disease, non-fatal heart attacks, irregular heartbeats, exacerbated asthma, decrease in lung function, and increased event of inflammation symptoms in the respiratory system, coughing, or difficulties in breathing (EPA, 2019). NO2 was, inter alia, previously linked to heart and cardiovascular diseases (Mann et al., 2002), chronic obstructive pulmonary disease (Euler et al., 1988), and poor lung function in adults (Bowatte et al., 2017). The exposure to NO2 concentrations exceeding the WHO guidelines is significantly associated with respiratory related mortality (Chen et al., 2007) and is also responsible for generating some harmful secondary pollutants such as ground level ozone (O3) (Khoder, 2002).
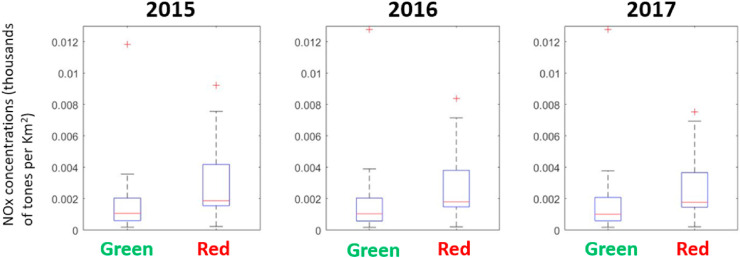
To better understand the effect of air pollutants on COVID-19 morbidity, we calculated the median rate of confirmed COVID-19 cases on the 80th day (per country population) and divided the 36 OECD countries into two lists: countries with rates higher than the median (“red countries”) and countries with rates lower than the median (“green countries”). The “green” list included countries such as Greece, New Zealand and Norway, while the “red” list was comprised of countries such as the UK, Spain and Italy (see list on Supplementary Text S3). Interestingly, all air pollutant parameters (PM2.5 concentrations, rates of populations exposed to PM2.5 levels exceeding WHO guideline and NOx concentrations) were higher in the “red” countries in comparison to the “green” ones. However, while the differences in NOx concentrations between the “red” and “green” countries were statistically significant (NOx concentrations (thousand tones/Km2): 2015 – “green”=1.84, “red”=3.0 p=0.04; 2016 – “green”=1.9, “red”=2.8, p=0.04; 2017 – “green”=1.9, “red”=2.7, p=0.04), (Fig. 2 ), PM2.5 concentrations and its rates of exposure above WHO guidelines were not statistically significant (See Supplementary Fig S1).
Fig. 2.
Boxplots of NOx concentrations (thousands of tones per Km2) in 2015, 2016, and 2017 at “green” and “red” countries. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Multivariate linear regressions were used to examine the associations between demographic, health, economic and air pollution features and the rate of confirmed cases and deaths (out of the entire national population) on the 60th and the 80th days since the first confirmed case in each country. We used the logarithm value of the mortality and morbidity in the multivariate linear regression. While all the multivariate models we built including PM2.5 concentrations were statistically significant, the models including NOx concentrations were not statistically significant.
Our models emphasize the importance of the relative number of hospital beds in decreasing the morbidity and mortality of COVID-19. According to the models, countries with higher relative number of beds per 100,000 population, had lower levels of COVID-19 cases and deaths. Surprisingly, the GDP had a positive (though mild) effect on morbidity and mortality (according to the models, richer countries had higher rates of COVID-19 morbidity and mortality). Although not statistically significant, PM2.5 concentrations (as features) were also positively associated with morbidity and mortality in all the four models (Table 1 ).
Table 1.
Linear regression models to predict rates of cases and deaths on the 60th and the 80th day since the first confirmed case, based on demographic, health and economic data, and on PM2.5 concentrations and exposure (percentages of population exposed to PM2.5 levels exceeding WHO guideline value) in 2017*.
| Predicted value | Model p-value | Model RMSE (Root mean square error) | %old | density | GDP | Physician** | Hospital Bed** | PM2.5 concentration 2017 |
PM2.5 exposure 2017 |
|---|---|---|---|---|---|---|---|---|---|
| Rate of cases on day 60 | 0.025 | 0.41 | 0.02 (0.52) | 0.0001 (0.17) | 0.001 (0.06) | 1.69 (0.07) | −0.91 (0.02) | 0.02 (0.17) | 0.0001 (0.96) |
| Rate of deaths on day 60 | 0.037 | 0.39 | 0.05 (0.1) | 0.00005 (0.47) | 0.001 (0.02) | 0.81 (0.39) | −1.0 (0.009) | 0.03 (0.1) | 0.002 (0.53) |
| Rate of cases on day 80 | 0.009 | 0.46 | 0.03 (0.34) | 0.0001 (0.126) | 0.001 (0.02) | 0.23 (0.79) | −1.0 (0.006) | 0.02 (0.17) | −0.002 (0.32) |
| Rate of deaths on day 80 | 0.007 | 0.47 | 0.03 (0.13) | 0.0001 (0.06) | 0.001 (0.04) | 0.06 (0.95) | −1.3 (0.0005) | 0.009 (0.58) | 0.001 (0.65) |
*Regression coefficients (p-values) ** per 10,000 population.
In this preliminary study we show an association between PM2.5 and NOx exposure levels, and a more severe COVID-19 morbidity. This study has several strengths. First, the study focuses on 36 OECD countries, in which the COVID-19 reports are considered as reliable. Second, the population long-term exposure data to PM2.5 and NOx levels at the 36 OECD countries (the base of this study), are considered as highly reliable (OECD, WHO and The World Bank).
Nevertheless, it is important to point out the limitations of the current study: (a) There is a significant difference in the number of tests per 1000 people between different countries, for example: As of August 3rd, 2020, 95.6 tests were performed in Germany per 1000 inhabitants compared to 193.7 in Israel, 171.6 in the US and 144.6 in the UK (Hasell et al., 2020). A different number of tests inevitably results in a different number of patients, which affects both morbidity rates (since unidentified patients may be asymptomatic or experience a mild illness without knowing they have COVID-19) and the COVID-19 related mortality rates recorded in each country. This could also partially explain why we found that richer countries (that naturally have the resources to perform more tests per population) had higher rates of confirmed COVID-19 morbidity and mortality. Another possible explanation could be that richer countries are more polluted than poorer ones. To check this assumption, we further investigated the association between GDP and the PM2.5/NOx concentrations. The results do not support this assumption as all PM2.5 parameters were negatively correlated with GDP (p<0.05), while NOx parameters were not correlated with GDP. Hence, elevated pollution levels do not explain the higher rates of confirmed COVID-19 morbidity and mortality in countries with high GDP. (b) Differences in inclusion policies and the various isolation and quarantine measures taken in response to the epidemic spread in different countries, as well as the population's response to measures taken to reduce the spread of the epidemic (depending on age, socioeconomic variables, geographical area, etc.), have an impact on morbidity and mortality. While some countries have maintained air and land closures, and policies of social exclusion, in other countries, such as the US, no unequivocal policy was formulated at the first stages of the pandemic, or an inclusive policy has been formulated and then changed several weeks later, as in the UK. Therefore, it is possible that the effect of chronic exposure to air pollution fails to be fully reflected in the reported COVID-19 morbidity and mortality in some countries. (c) The available data collected on PM2.5 and NOx exposure levels are updated for the years 2015–2017 only. Further analysis of an additional more up to date database (including the years 2018–2019 and the first quarter of 2020), optimally with a higher resolution, might strengthen our findings.
It should be noted that despite the above limitations, statistically significant results were obtained regarding the association between early chronic exposure of the population to PM2.5 and NOx levels, and the progression of the COVID-19 morbidity and mortality rates.
4. Conclusion
In this study, we show statistically significant multistate associations between the concentrations of the dominant air pollutants PM2.5 and NOx in 36 OECD countries, to morbidity and mortality from COVID-19. The link between air pollution and COVID-19 morbidity and mortality should be further examined, analyzing additional air pollutants levels along a wider timescale and using higher resolutions (counties, cities or quarters) as data allows, to establish the initial link found in this study, and other recently published studies, between chronic exposure to air pollutants and COVID-19 morbidity characteristics.
The adverse health outcomes stemming from long-term chronic exposure to various air pollutants has long been known to the scientific community and decision makers around the world. Despite this, severe ambient air pollution is still responsible for the premature deaths of 4.2 million people around the world annually. According to this study and other recently published studies, it appears that long-term chronic exposure to high concentrations of air pollutants may exacerbate morbidity and mortality rates from COVID-19. These results should raise a red flag among world leaders and decision makers about the urgent need to reduce air pollution and its many harmful effects.
Ambitious goals for promoting the generation and use of renewable energy sources are needed, while dramatically reducing the share of fossil fuels worldwide, alongside a significant acceleration in the electrification rate of public and private transportation and the restriction of private vehicles usage in highly populated areas, together with determined enforcement of air quality regulations and restrictions on air pollutants emissions. In the shadow of the COVID-19 epidemic and in light of the global climate change, an opportunity rises to reduce air pollution alongside with GHGs (Greenhouse gases) emissions. Such actions could likely lead to reduced morbidity and mortality rates from COVID-19, together with post epidemic improved public health, reducing chronic respiratory and cardiovascular morbidity in the general population.
Credit author statement
Z.B.I. – Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing A.L - Conceptualization, Data curation, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank Dr. Tamar Berman for her insightful comments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2021.110723.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bae S., Kim H., Jung T.Y., Lim J.A., Jo D.H., Kang G.S., et al. Epidemiological characteristics of COVID-19 outbreak at fitness centers in cheonan, Korea. J. Kor. Med. Sci. 2020;35(31) doi: 10.3346/jkms.2020.35.e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomberg A., Krishna M.T., Helleday R., Söderberg M., Ledin M.C., Kelly F.J., et al. Persistent airway inflammation but accommodated antioxidant and lung function responses after repeated daily exposure to nitrogen dioxide. Am. J. Respir. Crit. Care Med. 1999;159(2):536–543. doi: 10.1164/ajrccm.159.2.9711068. [DOI] [PubMed] [Google Scholar]
- Bowatte G., Erbas B., Lodge C.J., Knibbs L.D., Gurrin L.C., Marks G.B., et al. Traffic-related air pollution exposure over a 5-year period is associated with increased risk of asthma and poor lung function in middle age. Eur. Respir. J. 2017;50(4) doi: 10.1183/13993003.02357-2016. [DOI] [PubMed] [Google Scholar]
- Cao Y., Chen M., Dong D., Xie S., Liu M. Environmental pollutants damage airway epithelial cell cilia: implications for the prevention of obstructive lung diseases. Thoracic Cancer. 2020;11(3):505–510. doi: 10.1111/1759-7714.13323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center of disease control and prevention CDC Coronavirus disease 2019 (COVID-19) (accessed dec 5th) 2020. https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html#:~:text=Circumstances%20under%20which%20airborne%20transmission,person%20had%20left%20the%20space
- Chen T.M., Kuschner W.G., Gokhale J., Shofer S. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am. J. Med. Sci. 2007;333(4):249–256. doi: 10.1097/MAJ.0b013e31803b900f. [DOI] [PubMed] [Google Scholar]
- Cole M., Ozgen C., Strobl E. Institute of Labor Economics (IZA); Bonn: 2020. Air Pollution Exposure and COVID-19. IZA Discussion Papers, No. 13367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;114465 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Q., Wang Y., Zanobetti A., Wang Y., Koutrakis P., Choirat C., et al. Air pollution and mortality in the Medicare population. N. Engl. J. Med. 2017;376(26):2513–2522. doi: 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euler G.L., Abbey D.E., Hodgkin J.E., Magie A.R. Chronic obstructive pulmonary disease symptom effects of long-term cumulative exposure to ambient levels of total oxidants and nitrogen dioxide in California Seventh-Day Adventist residents. Arch. Environ. Health. 1988;43(4):279–285. doi: 10.1080/00039896.1988.10545950. [DOI] [PubMed] [Google Scholar]
- Hasell J., Ortiz-Ospina E., Mathieu E., Ritchie H., Beltekian D., Roser M. 2020. The Our World in Data COVID-19 Testing Database.https://ourworldindata.org/covid-testing Accessed Aug 4th) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helleday R., Huberman D., Blomberg A., Stjernberg N., Sandström T. Nitrogen dioxide exposure impairs the frequency of the mucociliary activity in healthy subjects. Eur. Respir. J. 1995;8(10):1664–1668. doi: 10.1183/09031936.95.08101664. [DOI] [PubMed] [Google Scholar]
- Khafaie M.A., Yajnik C.S., Salvi S.S., Ojha A. Critical review of air pollution health effects with special concern on respiratory health. Journal of air pollution and health. 2016;1(2):123–136. [Google Scholar]
- Khoder M.I. Atmospheric conversion of sulfur dioxide to particulate sulfate and nitrogen dioxide to particulate nitrate and gaseous nitric acid in an urban area. Chemosphere. 2002;49(6):675–684. doi: 10.1016/s0045-6535(02)00391-0. [DOI] [PubMed] [Google Scholar]
- Levy I., Karakis I., Berman T., Amitay M., Barnett-Itzhaki Z. A hybrid model for evaluating exposure of the general population in Israel to air pollutants. Environ. Monit. Assess. 2020;192(1):4. doi: 10.1007/s10661-019-7960-8. [DOI] [PubMed] [Google Scholar]
- Loomis D., Grosse Y., Lauby-Secretan B., El Ghissassi F., Bouvard V., Benbrahim-Tallaa L., et al. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14(13):1262. doi: 10.1016/s1470-2045(13)70487-x. [DOI] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., et al. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020;26(7):1628–1631. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J.K., Tager I.B., Lurmann F., Segal M., Quesenberry C.P., Jr., Lugg M.M., et al. Air pollution and hospital admissions for ischemic heart disease in persons with congestive heart failure or arrhythmia. Environ. Health Perspect. 2002;110(12):1247–1252. doi: 10.1289/ehp.021101247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudway I.S., Kelly F.J., Holgate S.T. Oxidative stress in air pollution research. Free Radical Biol. Med. 2020;151:2–6. doi: 10.1016/j.freeradbiomed.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD Data/Air and GHG emissions. 2017. https://data.oecd.org/air/air-and-ghg-emissions.htm (Accessed May 24th)
- OECE Data/Gross domestic product (GDP) 2019. https://data.oecd.org/gdp/gross-domestic-product-gdp.htm (Accessed Jun 1th)
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to the coronavirus (COVID-19) fatality rate. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Licen S., Perrone M.G., et al. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ open. 2020;10(9) doi: 10.1136/bmjopen-2020-039338. e039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Y., Li C., Dong H., Wang Z., Martinez L., Sun Z., et al. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in eastern China. JAMA internal medicine. 2020 doi: 10.1001/jamainternmed.2020.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank Data/PM2.5 air pollution, population exposed to levels exceeding WHO guideline value (% of total) 2017. https://data.worldbank.org/indicator/EN.ATM.PM25.MC.ZS Accessed May 26th.
- The World Bank Data/PM2.5 air pollution, mean annual exposure (micrograms per cubic meter) 2017. https://databank.worldbank.org/data/reports.aspx?source=2&series=EN.ATM.PM25.MC.M3 Accessed Jun 12th.
- The World Bank Data/Hospital beds per 1,000 people. 2019. https://data.worldbank.org/indicator/sh.med.beds.zs (Accessed Jun 4th)
- The World Bank Data/Physicians per 1,000 people. 2018. https://data.worldbank.org/indicator/sh.med.phys.zs?name_desc=true (Accessed Jun 4th)
- The World Bank Data/Population total. 2019. https://data.worldbank.org/indicator/sp.pop.totl (Accessed Jun 10th)
- The World Bank Data/Population ages 65 and above (% of total population) 2018. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?end=2018&start=2015 (Accessed Jun 10th)
- United States Environmental Protection Agency (EPA) US EPA; Washington, DC: 2019. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, Dec 2019). EPA/600/R-19/188. [Google Scholar]
- World Health Organization Ambeint (outdoor) Air Pollution. 2018. https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (Accessed Jul 20th)
- World Health Organization . 2006. WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide: Global Update 2005: Summary of Risk Assessment (No. WHO/SDE/PHE/OEH/06.02). World Health Organization.https://apps.who.int/iris/bitstream/handle/10665/69477/WHO_SDE_PHE_OEH_06.02_eng.pdf Accessed Jun 12th) [Google Scholar]
- World Health Organization . The WHO European Centre for Environment and Health; Bonn: 2013. Review of Evidence on Health Aspects of Air Pollution–REVIHAAP Project: Final Technical Report.https://www.euro.who.int/__data/assets/pdf_file/0004/193108/REVIHAAP-Final-technical-report-final-version.pdf Accessed Jun 12th) [Google Scholar]
- World Health Organization Coronavirus disease (COVID-2019) situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed Jun 12th)
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738:139825. doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.