Abstract
Young Black gay, bisexual, and other men who have sex with men (YB-GBMSM) face multiple psychosocial stressors, and are disproportionately impacted by HIV. Mental health care engagement is a promising avenue for addressing these disparities. To date, rates of mental health service utilization have not been examined specifically in this population. We conducted a retrospective cohort study among YB-GBMSM receiving care in a Ryan White-funded HIV care center that includes co-located HIV and mental health services. Of 435 unique YB-GBMSM patients, mental health concerns were identified in n = 191 (43.9%). Depressive symptoms were the most common concerns identified, followed by substance use, anxiety, and trauma. Among patients with identified mental health concerns who were not previously in mental health care, 79.1% were referred to mental health care, 56.3% set an appointment with a mental health provider, 40.5% were linked to mental health care (attended an initial visit), and 19.6% remained engaged in mental health care. Younger YB-GBMSM (age 18–24 years), who received care in a more integrated pediatric/adolescent part of the center, were more likely to have an appointment set once a concern was identified (χ2 = 7.17; p = 0.007). Even in a setting with co-located HIV and mental health care services, we found significant gaps in engagement at each stage of a newly described mental health care continuum. Implications for intervention at the provider and systems levels are discussed.
Keywords: mental health, Black/African Americans, sexual minorities, HIV/AIDS, health services
Introduction
HIV in the United States disproportionately impacts young Black gay, bisexual, and other men who have sex with men (YB-GBMSM) under the age of 30 years. Among 18- to 24-year-old Black GBMSM, HIV prevalence is estimated to be 26%, in comparison with 3% for young White GBMSM.1 Among those living with HIV, YB-GBMSM have lower rates of engagement at each stage of the HIV care continuum compared with older and non-Black individuals, with critical implications for morbidity, mortality, and public health.2,3
Treatable mental health conditions, including depressive disorders, anxiety disorders, trauma- and stress-related disorders, and substance-related disorders, can contribute to care continuum gaps among people living with HIV (PLH).4–8 In two prior studies of YB-GBMSM living with HIV, depressive symptoms were common (occurring in 47–59%) and associated with lack of HIV viral load suppression.4,5 High levels of trauma and anxiety have also been reported in samples including YB-GBMSM.9–11 Linking YB-GBMSM and other PLH to mental health services is, therefore, critically important for improving HIV care engagement. Cross-sector collaboration between mental health and HIV care services is often challenging.12,13 However, one facilitator of such interdisciplinary collaboration is the federal Ryan White HIV/AIDS Program (Ryan White), which funds HIV care for over half of PLH in the United States and explicitly supports the integration of mental health and HIV care services.14,15 However, real-world implementation of HIV and mental health integration is highly variable,15,16 and it remains unknown to what extent the availability of mental health resources translates into actual service utilization for YB-GBMSM living with HIV.
Amelioration of mental health problems represents an addressable target for interventions aiming to improve HIV care continuum engagement among YB-GBMSM. To our knowledge, no published studies report on mental health service utilization patterns specific to YB-GBMSM living with HIV. However, studies including YB-GBMSM living with HIV (e.g., focusing on youth living with HIV or sexual minority youth more broadly) suggest low rates of mental health service use in this population.17–20 The purpose of this study was to examine rates of mental health service utilization among YB-GBMSM within a large Ryan White-funded center that provides both HIV and mental health care. We sought to describe utilization patterns along a continuum of mental health care engagement, with continuum stages defined in direct correspondence with the mental health service delivery protocols within the center where the study was conducted. These stages included (1) identification of mental health concerns by HIV care providers, (2) referral to mental health care, (3) setting a mental health appointment, (4) linkage to mental health care, and (5) engagement in mental health care. Using a retrospective cohort study sample of YB-GBMSM, mental health care engagement was evaluated at each stage along this continuum.
Methods
Setting
The study was conducted at the Grady Infectious Disease Program (IDP), a large, Ryan White-funded comprehensive HIV care center situated within an academically affiliated public hospital system. The Grady IDP is located in Atlanta, Georgia—an urban HIV epicenter in the southeastern United States. The center provides a range of outpatient clinical services, including both HIV care and mental health care. Although HIV and mental health services are co-located in the same facility, approaches to mental health service delivery vary by clinical area. In the pediatric/young adult clinic (serving patients of ages 0–24 years), mental health services are offered on the same floor as medical services. In addition, mental health providers participate alongside their primary care and social work colleagues in weekly multidisciplinary patient care meetings. By contrast, mental health services for adults (patients of ages 25 years and older) are comprised primarily of appointments scheduled separately from HIV primary care visits on a separate floor in the clinic building, although mental health consultation during primary care visits is available upon HIV care provider request. Adult-oriented care providers do not hold weekly multidisciplinary team meetings; communication between primary care and mental health providers occurs on an as-needed basis.
Procedures
There is no automated electronic data capture of patient-recorded mental health symptoms; therefore, we conducted detailed chart reviews to obtain information about mental health service utilization. Trained study staff collected patient data through retrospective electronic medical record abstraction. We abstracted clinical data for all patients who were identified as Black MSM, between the ages of 18–29 years, and with at least one medical visit between November 1, 2017, and October 31, 2018. We then followed the cohort identified and extracted data for the period November 1, 2017–October 31, 2019, to estimate engagement in different stages of the mental health (MH) care continuum.
We defined the respective stages along the mental health care engagement continuum as follows: (1) identification of mental health concerns was indicated by HIV primary care provider documentation in their notes of any mental health symptoms (e.g., depression, anxiety, and adjustment problems) and/or substance use (excluding marijuana or alcohol unless explicitly documented as a clinical problem); (2) referral to mental health care was denoted by HIV provider medical record documentation (an electronic order and/or free text in the provider's assessment/plan) that a referral for mental health services was filed; (3) setting a mental health appointment was identified by appointment date (record of a scheduled visit) listed in the patient clinical record; (4) linkage to mental health care was designated by documentation (record of a completed visit) that a patient completed an initial mental health visit; and (5) engagement in mental health care was signified by documentation of a minimum of two additional completed mental health visits within 6 months of patient completion of an initial mental health visit.
The study received institutional review board approval.
Data analytic plan
Data were entered into an REDCap21 database and exported into SAS (SAS Institute, Inc., Cary, NC), version 9.4, for subsequent statistical analyses. Means, standard deviation (SD), and proportions were used to describe demographic and clinical characteristics of the sample. The mental health continuum was described using proportions, where each stage in the continuum was assessed as a percentage of the previous stage. Finally, achievement of each continuum stage between those aged 18–24 years (who receive care primarily in the more integrated pediatric setting) and those aged 25–29 years was compared using chi-squared statistics.
Results
The total sample included n = 435 unique patients. The mean age of participants was 24.6 years (SD = 2.9 years; Table 1). The mean length of time since HIV diagnosis was 3.2 years (SD = 2.8 years), and mean length of time since initial enrollment in the clinic was 2.1 years (SD = 1.8 years). Most patients did not have public or private insurance outside of Ryan White coverage (71.5%). Approximately half (47.8%) had a suppressed HIV viral load (<200 copies/mL) at the first measurement within the abstraction window, and the mean CD4+ T cell count was 433 cells/mm3. Twenty-one percent had mentions of housing insecurity documented in clinical notes, and 53% were referred to social workers for additional assistance with managing care.
Table 1.
Demographic and Clinical Characteristics
| Mean (SD) | |
|---|---|
| Age (years) | 24.6 (2.9) |
| Time since HIV diagnosis (years) | 3.2 (2.8) |
| Time since enrolled in this clinic (years) | 2.1 (1.8) |
| Baseline CD4 count (cells/mm3) | 433 (288) |
| n (%) | |
| VL suppressed at baseline | 208 (47.8) |
| Any STI diagnosis | 229 (52.6) |
| Any mention of housing insecurity | 92 (21.2) |
| Any visits with social workers | 231 (53.1) |
| Insurance | |
| Uninsured (Ryan White only) | 311 (71.5) |
| Medicare/Medicaid | 58 (13.3) |
| Private | 66 (15.2) |
SD, standard deviation; STI, sexually transmitted infection; VL, viral load.
HIV care providers identified and documented mental health concerns in 191 (43.9%) patients within our cohort. Of the concerns listed by HIV providers, depressive symptoms were the most common (n = 121; 63.3%), followed by substance use (n = 83, 47.4%), anxiety (n = 45; 25.9%), and trauma-related symptoms (n = 13, 6.8%). Some patients were also referred to mental health services for other reasons, including stress, adjustment, and anger management. Among patients identified as having concerning substance use, methamphetamines and cocaine were most commonly cited, with problematic alcohol use, opiates, and other substances documented less frequently. Concerns identified by HIV providers are given in Table 2. Of note, marijuana use was very common (188 patients)—however, since exclusive marijuana use did not appear to be an indication for mental health referral in any cases, we did not include mentions of marijuana as mental health/substance use concerns (data not shown).
Table 2.
Mental Health Concerns Identified by HIV and Mental Health Care Clinicians
| n (%) | |
|---|---|
| Mental health concerns identified by HIV clinicians (n = 191) | |
| Depression | 121 (63.3) |
| Substance use | 83 (43.4) |
| Methamphetamine | 27 (6.2) |
| Cocaine | 27 (6.2) |
| Alcohol | 21 (4.8) |
| Opiate | 6 (1.4) |
| Other substance | 12 (2.8) |
| Anxiety | 45 (23.5) |
| PTSD/trauma | 13 (6.8) |
| Other | 56 (12.9) |
| Diagnoses made by mental health providers (n = 66) | |
| Depressive disorders | 44 (66.7) |
| Substance use disorders | 30 (45.5) |
| Anxiety disorders | 15 (22.7) |
| Trauma and stressor-related disorders | 11 (16.7) |
| Other diagnoses | 22 (33.3) |
PTSD, post-traumatic stress disorder.
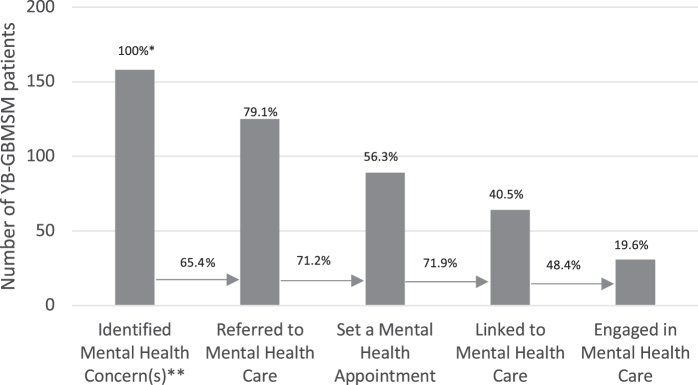
Figure 1 depicts the findings pertaining to the continuum of mental health care engagement. Of note, 33 of the patients with identified mental health concerns who were not newly referred within the abstraction period had previously engaged with mental health care, so that a new referral was not necessarily indicated. For the continuum analysis, we therefore, used a denominator of n = 158 patients who should have gone through the subsequent stages. Seventy-nine percent (n = 125; 79.1%) of the patients with an identified concern were referred to mental health care. Seventy-one percent (71.2%) of patients who were referred actually scheduled an appointment with a mental health provider (n = 89; 56.3% of the patients with identified mental health concern). Seventy-two percent (71.9%) of those scheduled were successfully linked to mental health care (n = 64; 40.5% of patients with an identified concern), and 48.4% of patients who attended an initial mental health visit remained engaged in mental health care (n = 31; 19.6% of patients with an identified mental health concern).
FIG. 1.
Continuum of Mental Health Care Engagement. *Percentages on top of the bars indicate proportion of patients at each stage, as a proportion of patients for whom mental health concern is identified. Percentages on the arrows between the bars depict patients who achieved each continuum stage, as a proportion of those who achieved the prior stage. **In this figure, we excluded 33 patients in whom mental health concerns were identified, because they had already been referred to mental health care before the abstraction period.
Comparison of achievement of mental health continuum outcomes between 18- to 24-year-old YB-GBMSM (who received care in the more integrated pediatric setting) and 25–29-year-old patients (Table 3) revealed that younger patients were significantly more likely than older patients to have a mental health appointment scheduled once referred by their HIV clinician (χ2 = 7.17; p = 0.007). There was also a trend toward higher identification of mental health concerns among younger patients (χ2 = 3.6; p = 0.06). When the two age groups were compared by demographic and other clinical characteristics, several other differences emerged: younger patients were more likely to see a social worker (χ2 = 140.11; p < 0.001), have documented housing concerns (χ2 = 11.56; p < 0.001), and to be diagnosed with a sexually transmitted infection (χ2 = 7.06; p = 0.008).
Table 3.
Comparison of Mental Health Continuum Stages by Age Group
| Age 18–24 years | Age 25–29 years | Chi-square | p | |
|---|---|---|---|---|
| Mental health continuum stages | ||||
| Identified mental health concerns | 90/183 (49.2%) | 101/252 (40.1%) | 3.5653 | 0.06 |
| Referred to mental health care | 57/90 (63.3%) | 59/101 (58.4%) | 0.4826 | 0.49 |
| Set a mental health appointment | 48/56 (85.7%) | 35/55 (63.6%) | 7.1706 | 0.007 |
| Linked to mental health care | 34/48 (70.8%) | 25/35 (71.4%) | 0.0035 | 0.95 |
| Engaged in mental health care | 16/34 (47.1%) | 13/27 (48.1%) | 0.0072 | 0.93 |
| Demographic/clinical characteristics | ||||
| Insurance | ||||
| None (Ryan White only) | 140/183 | 171/252 | ||
| (76.5%) | (67.9%) | |||
| Medicare/Medicaid | 20/183 | 38/252 | 3.8899 | 0.143 |
| (10.9%) | (15.1%) | |||
| Private insurance | 23/183 | 43/252 | ||
| (12.6%) | (17.1%) | |||
| Housing concerns | 53/183 | 39/252 | 11.5610 | <0.001 |
| (29.0%) | (15.5%) | |||
| Social work visits | 158/183 | 73/252 | 140.1124 | <0.001 |
| (86.3%) | (29.0%) | |||
| Undetectable viral load at baseline | 86/167 (51.5%) | 124/238 (52.1%) | 0.0143 | 0.905 |
| Any STI diagnosis | 110/183 | 119/252 | 7.0623 | 0.008 |
| (60.1%) | (47.2%) | |||
For those 66 patients who were evaluated by a mental health clinician, two-thirds (66.7%) were diagnosed with depressive disorders or symptoms, and 45% with substance use disorders. Anxiety disorders were diagnosed in 22.7%, and trauma and stress-related disorders in 16.7% of patients. One-third were noted to have other conditions such as adjustment disorders, bipolar disorder, schizophrenia, or grief/bereavement. Mental health and substance-related concerns and diagnoses are given in Table 2.
Discussion
To our knowledge, this is the first study to specifically examine patterns of mental health service utilization among YB-GBMSM living with HIV, a critically important population to target in efforts to end the HIV epidemic in the United States. Our study identified important gaps in mental health care delivery to YB-GBMSM living with HIV, including incomplete identification of mental health problems, lack of referrals to mental health services, and incomplete attendance and engagement with these services even when referrals were made. Notably, these gaps occurred despite the availability of mental health services co-located in the same building as HIV care.
Given that this was a retrospective chart review study, we were not able to directly measure the burden of mental health symptoms in our sample. However, previous studies among YB-GBMSM living with HIV report rates of depressive symptoms ranging from 47% to 59%,4,22 suggesting that the rate of identification of mental health problems in our study (43.9% for multiple psychological symptom categories combined) likely represents under-recognition of psychological symptoms. This gap highlights a need for evidence-based screening practices to improve identification of mental health problems among YB-GBMSM and facilitate subsequent engagement with mental health services.
Our results suggest multiple opportunities for intervention at the clinic and provider levels at each stage along the mental health care continuum to improve mental health care engagement among YB-GBMSM living with HIV. Reasons for the difference between identified mental health concerns and the number of referrals are unclear and worthy of further investigation, but could include limited time during patient encounters, and/or deprioritization of mental health relative to physical health concerns. HIV/primary care providers may benefit from education and/or prompts to increase referral to mental health services when these needs are identified. Streamlining scheduling processes so that referral and scheduling can occur seamlessly in a single step would be one relatively simple way to avoid the next drop off along the continuum. Coordination of mental health and HIV visits, such that a mental health visit does not require an additional trip to the clinic, might be an effective strategy for decreasing the gap between scheduled and attended mental health intake visits, as well as improving attendance at follow-up visits. Similar to what has been used to enhance HIV care engagement, additional support utilizing peer navigators or case managers might also be applied to improving attendance at mental health care visits.
There is also a strong possibility that this gap at the referral stage of the continuum is attributable to patients declining mental health referrals. Prior research has documented unfavorable attitudes toward mental health care utilization among Black Americans more broadly.23–26 In addition, culturally important coping strategies that have developed in response to structural barriers facing Black Americans, such as reliance on church-based services for mental health problems,27,28 high effort coping,29 and masculine self-reliance,30 may paradoxically serve as barriers to help seeking. Recent study has similarly demonstrated the important role of medical mistrust and HIV stigma as barriers to care specifically for sexual minority youth of color.31 These cultural beliefs and stigmas could contribute to lack of enthusiasm and ultimately drop offs in mental health care engagement at each continuum stage, including unwillingness to accept a mental health referral, reticence to follow through on scheduling and attending appointments in mental health, and/or inclination to stop attending mental health visits. Further study examining YB-GBMSM patient perspectives on mental health care, including qualitative studies, would be helpful to tailor interventions and messaging promoting mental health care engagement for this population.
Our findings build on previous study examining mental health service utilization rates. Pence and colleagues previously created a continuum examining mental health service use among PLH meeting criteria for major depressive disorder (MDD). This continuum was based on population-level data and estimation techniques, and included the following stages: prevalence of depression, clinical recognition, initiation of treatment, adequacy of treatment, and treatment response.32 Their study estimated that 45% of MDD cases among PLH are recognized, 40% of the recognized cases get treated adequately, and that once treated adequately, 70% achieve remission of MDD. Although we were unable to capture all of the stages in their continuum through our retrospective study, our results complement this study by examining additional stages (e.g., referral and scheduling), thus adding detail about processes occurring at individual patient, provider, and clinic levels. These details are potentially important for intervention development, as they point out specific steps within a clinic's workflow that could impede or facilitate mental health care for YB-GBMSM living with HIV. In addition, our study included mental health service use across diagnostic categories, as opposed to being limited to depression. Although depressive symptoms were the most common reason for referral in our sample, significant burden of substance use, trauma, and anxiety was noted as well. Future study should aim to further examine differences in mental health service use across diagnostic categories.
Our analyses comparing continuum stages by age group (as a proxy for assessing the impact of different HIV–mental health integration strategies) yielded results with implications for service delivery. The biggest difference between the mental health care continua of the two age groups was seen at the stage of scheduling an appointment once a referral had been placed. This result suggests that the closer connection between HIV and mental health clinicians in the pediatric care setting may alleviate some barriers to scheduling appointments, with important downstream effects. In addition, mental health concerns were identified more often in younger patients, although this trend did not quite reach statistical significance. Additional comparisons of younger and older patients demonstrated that younger patients were much more likely to have visited a social worker—although the cross-sectional and retrospective nature of this study limits explanatory speculation regarding this finding, it may be that the social workers are helping to facilitate referral to, and scheduling of mental health appointments. Additional areas to consider for future investigation include the potential role of high burden of psychological distress among younger men recently diagnosed with HIV, differences in pediatric and adult-oriented approaches to care, and the influence of frequent multidisciplinary meetings in helping to identify mental health concerns among the pediatric patients.
Several limitations to this study could impact the interpretation of the results presented here. Given that we utilized a retrospective medical record-based design, we had incomplete information about some patients. Our assessments of mental health concerns and diagnoses are limited to what is identified and documented by clinicians, leading to potential under-reporting. Ideally, our mental health care continuum would have also included a measure of treatment efficacy as the final stage, however, this information is difficult to quantify from examination of mental health clinician notes. Clinic-wide initiatives to promote routine recording of quantitative scores of depressive symptoms or psychological functioning (e.g., the Patient Health Questionnaire-933 or Global Assessment of Functioning34) might help to enable measurement of treatment efficacy in the future.
Treatment of mental health comorbidity has the potential to significantly improve HIV care engagement, and ultimately morbidity and mortality among YB-GBMSM. To realize this promise, however, further study is needed to elicit and address barriers that lead to significant disengagement at each stage of the mental health care continuum. Our findings support the need for further study of both patient- and provider-level barriers to mental health care engagement in HIV care settings to inform tailored interventions to enhance health and well-being for YB-GBMSM.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported by the Emory Center for AIDS Research (P 30 AI050409).
References
- 1. Wejnert C, Hess KL, Rose CE, et al. Age-specific race and ethnicity disparities in HIV infection and awareness among men who have sex with men—20 US cities, 2008–2014. J Infect Dis 2016;213:776–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mugavero MJ, Lin HY, Willig JH, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis 2009;48:248–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hussen SA, Easley KA, Smith JC, et al. Social capital, depressive symptoms, and HIV viral suppression among young Black, gay, bisexual and other men who have sex with men living with HIV. AIDS Behav 2018;22:3024–3032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Menza TW, Choi SK, LeGrand S, et al. Correlates of self-reported viral suppression among HIV-positive, young, Black men who have sex with men participating in a randomized controlled trial of an internet-based HIV prevention intervention. Sex Transm Dis 2018;45:118–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med 2005;10:166–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shacham E, Estlund AL, Tanner AE, et al. Challenges to HIV management among youth engaged in HIV care. AIDS Care 2017;29:182–196 [DOI] [PubMed] [Google Scholar]
- 8. Thompson AB, Gillespie SE, Hood J, et al. Regular marijuana use is associated with poor viral suppression in HIV-infected adolescents and young adults. AIDS Behav 2017;22:1363–1374 [DOI] [PubMed] [Google Scholar]
- 9. Mustanski B, Morgan E, D'Aquila R, et al. Individual and network factors associated with racial disparities in hiv among young men who have sex with men: Results from the RADAR cohort study. J Acquir Immune Defic Syndr 2018;80:24–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kuhns LM, Hotton AL, Garofalo R, et al. An index of multiple psychosocial, syndemic conditions is associated with antiretroviral medication adherence among HIV-positive youth. AIDS Patient Care STDS 2016;30:185–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brown LK, Whiteley L, Harper GW, et al. Psychological symptoms among 2032 youth living with HIV: A multisite study. AIDS Patient Care STDS 2015;29:212–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elkington KS, Robertson AA, Knight DK, et al. HIV/STI service delivery within juvenile community supervision agencies: A national survey of practices and approaches to moving high-risk youth through the HIV care cascade. AIDS Patient Care STDS 2020;34:72–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dunleavy S, Aidala AA,Yomogida M. Medical, mental health, and social service linkage predicts better HIV outcomes: A network analytic approach. AIDS Patient Care STDS 2019;33:538–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Weiser J, Beer L, Frazier EL, et al. Service delivery and patient outcomes in Ryan White HIV/AIDS program-funded and -nonfunded health care facilities in the United States. JAMA Intern Med 2015;175:1650–1659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim S, Ades M, Pinho V, et al. Patterns of HIV and mental health service integration in New York State. AIDS Care 2014;26:1027–1031 [DOI] [PubMed] [Google Scholar]
- 16. Chuah FLH, Haldane VE, Cervero-Liceras F, et al. Interventions and approaches to integrating HIV and mental health services: A systematic review. Health Policy Plan 2017;32(Suppl):iv27–iv47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Salomon EA, Mimiaga MJ, Husnik MJ, et al. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: Implications for age-specific interventions. AIDS Behav 2009;13:811–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Burns MN, Ryan DT, Garofalo R, et al. Mental health disorders in young urban sexual minority men. J Adolesc Health 2015;56:52–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malhotra K, Shim R, Baltrus P, et al. Racial/ethnic disparities in mental health service utilization among youth participating in negative externalizing behaviors. Ethn Dis 2015;25:123–129 [PubMed] [Google Scholar]
- 20. Whiteley LB, Brown LK, Swenson R, Kapogiannis BG, Harper GW. Disparities in mental health care among HIV-infected youth. J Int Assoc Provid AIDS Care 2014;13:29–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hightow-Weidman L, LeGrand S, Choi SK, et al. Exploring the HIV continuum of care among young black MSM. PLoS One 2017;12:e0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Conner KO, Koeske G, Brown C. Racial differences in attitudes toward professional mental health treatment: The mediating effect of stigma. J Gerontol Soc Work 2009;52:695–712 [DOI] [PubMed] [Google Scholar]
- 24. Neighbors HW Jackson JS. The use of informal and formal help: Four patterns of illness behavior in the Black community. Am J Community Psychol 1984;12:629–644 [DOI] [PubMed] [Google Scholar]
- 25. Hankerson SH, Suite D, Bailey RK. Treatment disparities among African American men with depression: Implications for clinical practice. J Health Care Poor Underserved 2015;26:21–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hudson DL, Eaton J, Banks A, Sewell W, Neighbors H. “Down in the sewers”: Perceptions of depression and depression care among African American men. Am J Mens Health 2018;12:126–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Neighbors HW, Musick MA, Williams DR. The African American minister as a source of help for serious personal crises: Bridge or barrier to mental health care? Health Educ Behav 1998;25:759–777 [DOI] [PubMed] [Google Scholar]
- 28. Chatters LM, Mattis JS, Woodward AT, et al. Use of ministers for a serious personal problem among African Americans: Findings from the National Survey of American Life. Am J Orthopsychiatry 2011;81:118–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. James SA. John Henryism and the health of African-Americans. Cult Med Psychiatry 1994;18:163–182 [DOI] [PubMed] [Google Scholar]
- 30. Powell W, Adams LB, Cole-Lewis Y, et al. Masculinity and race-related factors as barriers to health help-seeking among African American men. Behav Med 2016;42:150–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arrington-Sanders R, Hailey-Fair K, Wirtz AL, et al. Role of structural marginalization, HIV stigma, and mistrust on HIV prevention and treatment among young Black Latinx men who have sex with men and transgender women: Perspectives from youth service providers. AIDS Patient Care STDS 2020;34:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pence BW, O'Donnell JK, Gaynes BN. Falling through the cracks: The gaps between depression prevalence, diagnosis, treatment, and response in HIV care. AIDS 2012;26:656–658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Endicott J, Spitzer RL, Fleiss JL, et al. The Global Assessment Scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry1976;33:766–771 [DOI] [PubMed] [Google Scholar]